- 1State Key Laboratory of Biotherapy and Cancer Center, West China Hospital, Sichuan University, Chengdu, China
- 2Department of Oncology, West China Hospital, Sichuan University, Chengdu, China
- 3Department of Pathology, West China Hospital, Sichuan University, Chengdu, China
- 4Department of Nuclear Medicine, West China Hospital, Sichuan University, Chengdu, China
- 5Department of Chemistry, University of Washington-Seattle Campus, Seattle, WA, United States
Purpose: The role of 18F-2-fluoro-2-deoxy-D-glucose positron emission tomography/computed tomography (18F-FDG PET/CT) in evaluating bone marrow (BM) involvement (BMI) among patients with extranodal natural killer/T-cell lymphoma (ENKTL) is poorly understood. This study investigated whether PET/CT could replace bone marrow biopsy (BMB) in treatment-naive ENKTL patients.
Methods: Newly diagnosed ENKTL patients (n = 356) who received BMB and PET/CT to evaluate BMI at the time of diagnosis were retrospectively reviewed at West China Hospital between August 2008 and January 2020. The BMI diagnosis was confirmed using BM histology. Clinical characteristics, survival outcomes, and prognostic indicators were summarized and analyzed.
Results: The cohort included 356 cases, of whom 261 were diagnosed with early-stage and 95 with advanced-stage ENKTL by PET/CT before initial treatment. No early-stage patients were identified with BMI by either BMB or PET/CT. Among the advanced-stage patients, 26 were BMB positive, and 12 of 22 patients (54.5%) with positive PET/BM results were also BMB positive. The sensitivity and specificity of PET/CT to detect BMI were 46% and 97%, respectively. The progression-free survival (PFS) and overall survival (OS) of PET/BM-negative patients were markedly longer (p = 0.010 and p = 0.001 for PFS and OS, respectively), which was consistent with the results of the BMB (p = 0.000 for both PFS and OS).
Conclusion: Although 18F-FDG PET/CT showed the potential to replace BMB in the initial staging of early-stage ENKTL patients, baseline PET/CT cannot provide an accurate BMI evaluation for advanced-stage patients. A prospective study is required to confirm the diagnostic performance of BMI identification by PET/CT, along with targeted BMB and MRI for advanced-stage patients.
Introduction
Extranodal natural kill (NK)/T-cell lymphoma (ENKTL) is an aggressive T/NK-cell neoplasm that frequently occurs among Asians and the indigenous populations of Mexico and Central and South America (1). Approximately 73–87% of patients are early-stage (stages I–II), while 13–30% are advanced-stage (stages III–IV) at the time of diagnosis (2, 3). For early-stage patients, radiotherapy combined with asparaginase-containing chemotherapy is established as the initial treatment and is associated with a 59.5–82.9% 5-year progression-free survival (PFS) rate and a 42–85.7% 5-year overall survival (OS) rate (3–7). In contrast, for patients with advanced-stage disease, asparaginase-based chemotherapy is the standard, and the 1-year PFS and OS rates are 38–86% and 57–90% (8–11), respectively. Thus, staging at diagnosis informs both the prognosis of ENKTL patients and the initial treatment strategy.
Determining the bone marrow (BM) status is critical for the initial staging of ENKTL. According to the Ann Arbor (12) and Lugano staging (13) systems, BM involvement (BMI) is associated with stage IV and prognosis is poor (14). BMI is also associated with a higher risk of hemophagocytic syndrome among patients with ENKTL (15, 16). While bone marrow biopsy (BMB) result is the gold standard used to confirm BMI, it is an invasive operation and BMB location may lead to false-negative results. Recently, 18F-FDG PET/CT has been widely used to assist the staging of lymphoma, including ENKTL because NK/T-cell lymphoma is intensely FDG-hypermetabolic (17). In Hodgkin lymphoma (18) and diffuse large B-cell lymphoma (19, 20), PET/CT identified BMI with high sensitivity and specificity. However, the diagnostic and prognostic performance of using PET/CT in assessing BMI among ENKTL patients remains unknown. This study aimed to investigate the concordance between PET/CT and BMB among patients with ENKTL.
Patients and Methods
Patients
Patients enrolled in this study were diagnosed with ENKTL using the World Health Organization classification (21). Those who were ≥ 13 years of age and were diagnosed at West China Hospital between August 2008 and January 2020 were included. Eighty-eight patients from our previous study were also included in this cohort (22). The patients had no other malignancies and received no hematopoietic growth factor injections before PET/CT or BMB. Staging procedures, including whole-body PET/CT and BMB on one side of the iliac crest, were performed for every case.
BMB
Unilateral iliac crest marrow aspirate and trephine biopsy were routinely performed before treatment in all newly diagnosed ENKTL cases. BMB results were obtained from the clinical database and reviewed by experienced hematopathologists at diagnosis. BMB tissue was formalin-fixed, paraffin-embedded, and evaluated morphologically using a hematoxylin–eosin stain. CD3ϵ, CD20, CD56, CD5, Granzyme B staining, and Epstein–Barr virus (EBV)-encoded small RNA in situ hybridization (EBERs) (14) were performed in specific morphologic BMI cases.
PET/CT Imaging and Reporting
All patients underwent whole-body 18F-FDG PET/CT (at least vertex or midbrain to upper thigh or foot) using a combined PET/CT scanner (Gemini GXL with a 16-slice CT component, Philips Corp., Netherlands). After a 6-hour fast and a blood glucose level of <11 mmol/L, patients were given 5.18 MBq of 18F-FDG per kilogram intravenously. After a 60-minute rest period, whole-body CT and PET scans were initiated. CT acquisition data were used for attenuation correction and corrected PET images were reconstructed using the line-of-response method. Syntegra software was applied for image registration and fusion.
PET/CT studies were assessed visually using PET activity in the liver blood pool as a reference. Nuclear medicine specialists carefully and separately reviewed PET/CT data to confirm BMI. The BMI assessed by PET/CT was defined as prominent focal or diffuse homogeneous 18F-FDG uptake in the bone marrow, exceeding that of the normal liver and without an alternative explanation relating to non-oncologic disease, trauma, or procedural history.
Statistical Analysis and Ethics
The patients in this study were followed up by their outpatient oncologist. The diagnostic performance of PET/CT to identify BMI was summarized using the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy, which were calculated using Clopper–Pearson exact confidence limits (23). The PFS and OS were summarized using the Kaplan–Meier method, and the differences were compared using the log-rank test. Univariate logistic regression analysis evaluated variables used to predict the survival of ENKTL patients. Parameters identified as statistically significant risk factors were assessed using multivariate logistic regression analysis. The PFS was calculated from the time of diagnosis to disease progression, recurrence, any cause of death, or last follow-up, and the OS was determined from the time of diagnosis to death for any reason or last follow-up. Survival data were analyzed using SPSS version 25.0 (IBM Corp., Armonk, NY, USA), and a two-sided p <0.05 was considered statistically significant. The study was performed under regulatory requirements and approved by the Ethics Committee of the West China Hospital of Sichuan University.
Results
Patient Characteristics
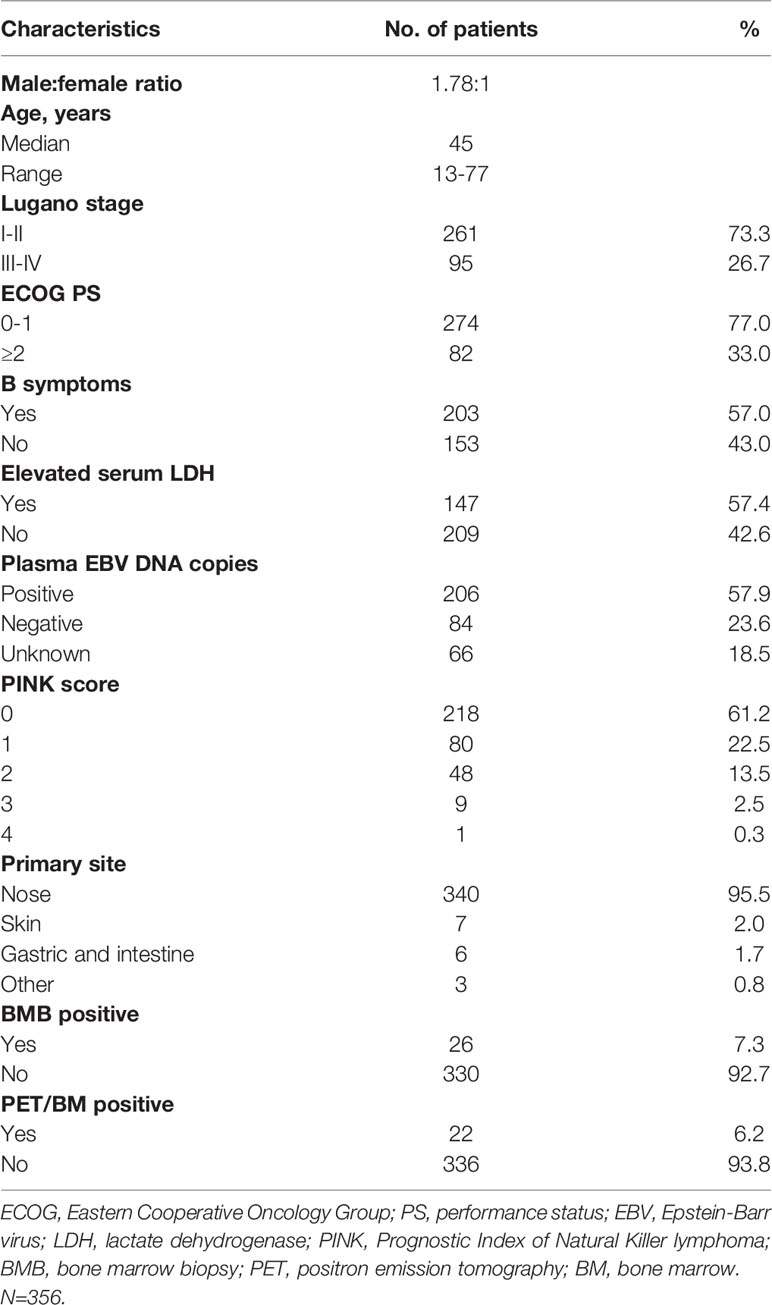
A total of 356 patients who met the study enrollment criteria were included. At diagnosis, the median age was 45 years (range, 13–77 years), and the male-to-female ratio was 1.78. Almost three-quarters (73.3%) of the cases were classified as early-stage and 26.7% were diagnosed as advanced-stage by PET/CT using the Lugano staging system (Table 1). Most of the patients (95.5%) presented with a nasal location as the primary lesion, and other lesions were found in the skin, stomach, and intestine. Using the Prognostic Index of Natural Killer lymphoma (PINK) score evaluation (24), 83.7% of patients were assigned to the low-risk group (Table 1). Using BMB detection and PET/CT scanning, 26 patients (7.3%) had ENKTL cells in the BM using BMB, whereas 22 (6.2%) tested positive by PET/CT. Patients from the BMB-positive group had a higher ratio of performance status ≥2, serum lactate dehydrogenase (LDH), and B symptoms than BMB-negative patients (Table 2).
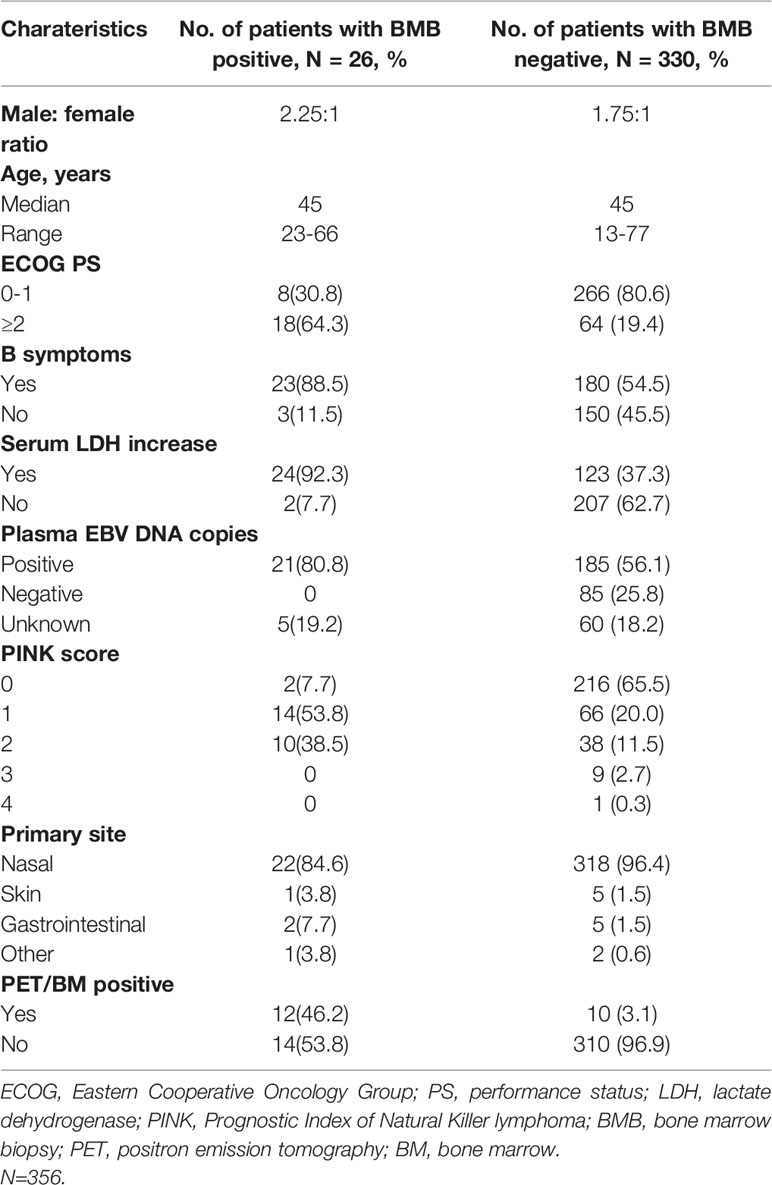
Table 2 Baseline features of patients with bone marrow involvement versus. patients without bone marrow involvement by BMB (n = 356).
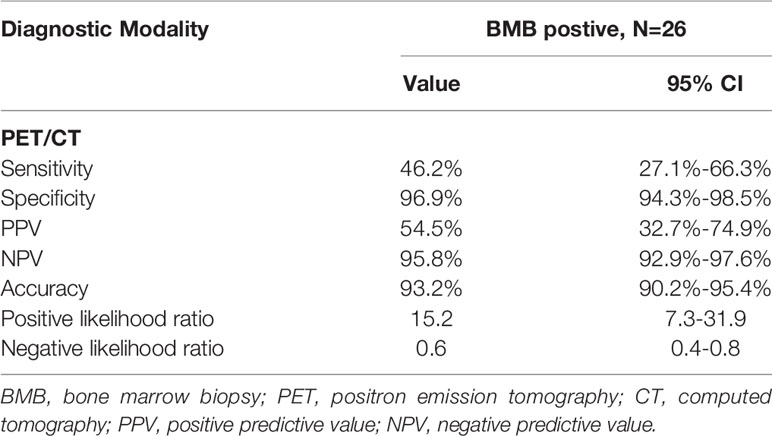
Diagnostic Performance of PET/CT
PET/CT and BMB were used to detect the BM status at the time of diagnosis for 261 early-stage and 95 advanced-stage patients (Figure 1). Among early-stage patients, PET/CT detected that 261/261 (100%) were BM negative. Among advanced-stage patients, 22/95 (23.2%) were PET/BM-positive, and 73/95 (76.8%) were negative. Of the PET/BM-positive cases, 12/22 (54.5%) were BMB positive. Additionally, 14/73 (19.2%) of advanced-stage patients with PET/BM negative were BMB positive. PET/CT detected BMI in 12 of the 26 BMB-positive patients (46.2% sensitivity; Table 3). Of the 330 patients who were PET/BM negative, 320 were also negative using BMB (96.9% specificity; Table 3). The positive predictive value (PPV) and negative predictive value (NPV) of PET/CT for identifying BMI were 54.5% and 95.8%, respectively, and the positive and negative likelihood ratios were 15.2 and 0.6, respectively. The BM examination by PET/CT did not change the clinical stage between early- and advanced-stage and the initial treatment strategy of the cohort.
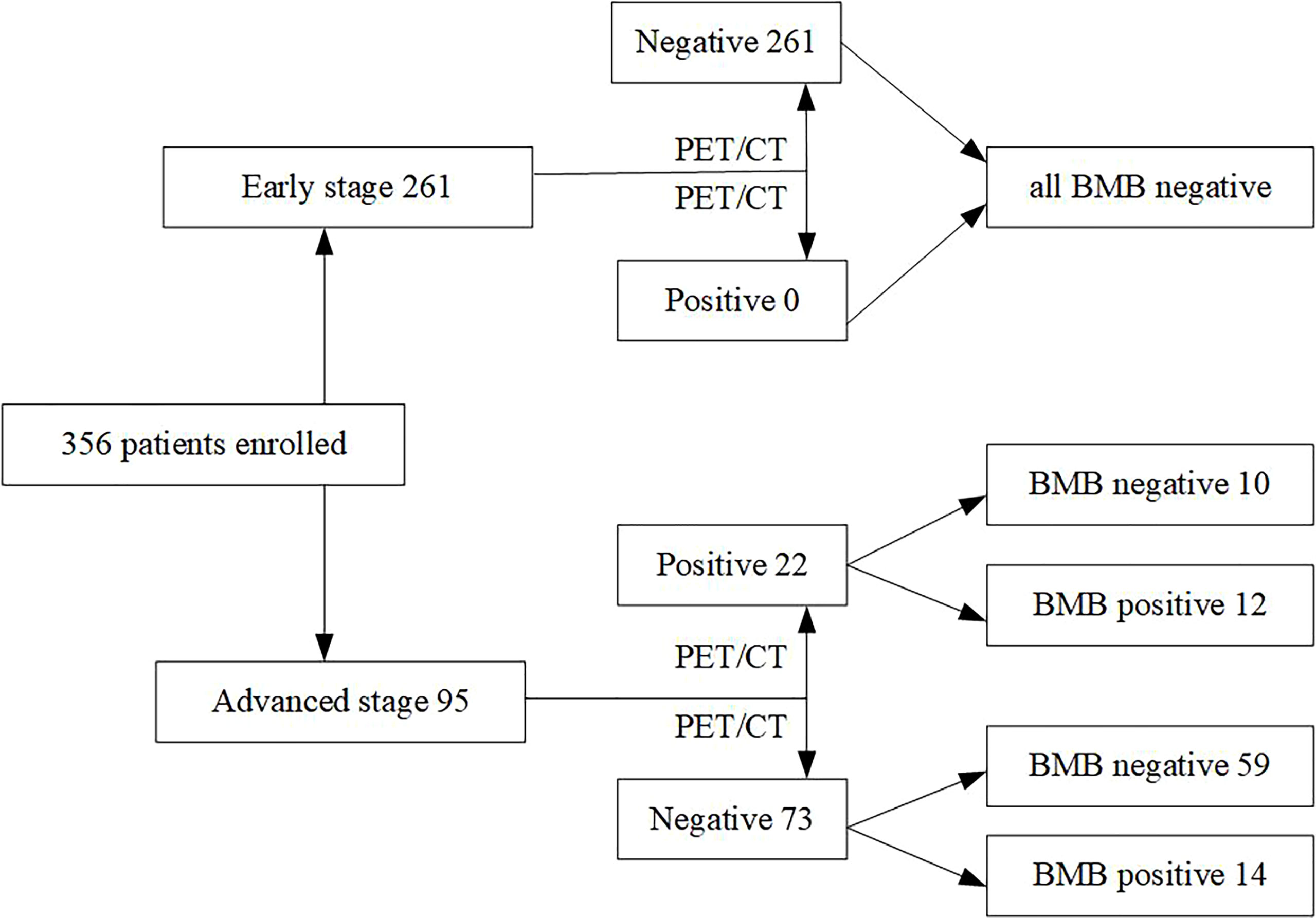
Figure 1 The distribution of bone marrow status as assessed with PET/CT and bone marrow biopsy ENKTL patients.
Prognostic Performance of PET/CT
The median follow-up time for this cohort was 59.0 months (range, 50.1–67.1 months). During this time, the median PFS (mPFS) was 51.0 months (95% CI, 30.0–72.0 months, Figure 2A), and the median OS (mOS) was 144.0 months (95% CI, 61.3–226.7 months, Figure 2B). The BMB-positive group had mPFS of 5.0 months (95% CI, 0.0–10.0 months; p = 0.000) and mOS of 10.0 months (95% CI, 4.3–15.7 months; p = 0.000) (Figures 2C, D). Survival differed significantly between the PET/BM-positive and negative groups (Figures 2E, F). The mPFS was 60.0 months (95% CI, 37.3–82.7 months) for the PET/BM-negative group and only 11.0 months (95% CI, 0.0–22.5 months) for the positive group (p = 0.010). Similarly, the mOS was 144.0 months (95% CI, 61.3–226.7 months) for the PET/BM-negative group and only 12.0 months (95% CI, 0.0–29.5 months) for the PET/BM-positive group (p = 0.001).
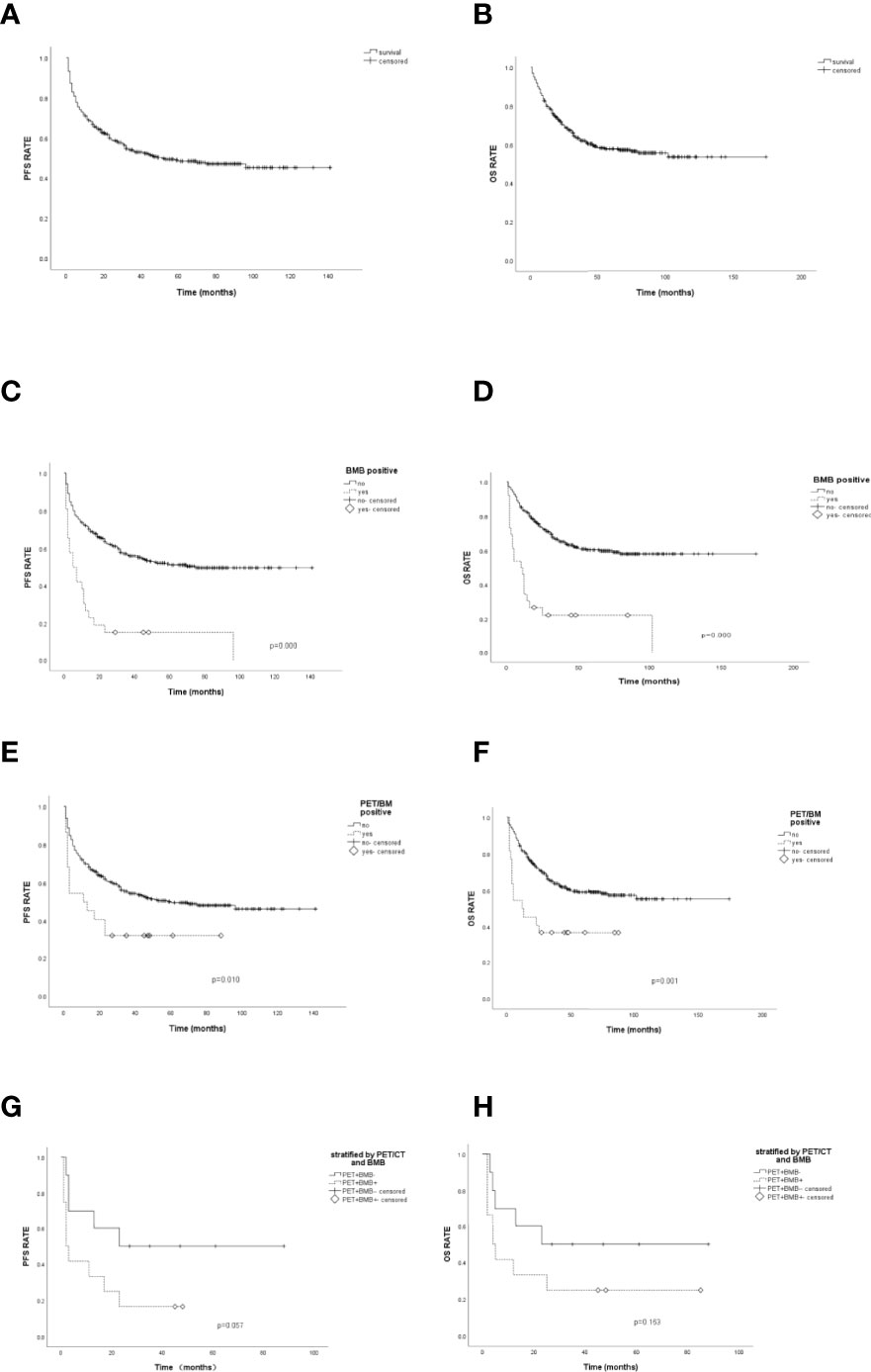
Figure 2 Progression-free survival (PFS) and overall survival (OS) analysis. (A, B): The median PFS (mPFS) and median OS (mOS) of 356 patients was 51.0 months and 144.0 months. (C) The mPFS of bone marrow biopsy (BMB) positive was 5.0 months, and 75.0 months for negative patients, p=0.000. (D). The mOS of BMB positive was 10.0 months, and 144.0 months for negative patients, p=0.000. (E) The mPFS of PET/BM positive was 11.0 months, and 60.0 months for negative patients, p=0.010. (F) The mOS of PET/BM positive was 12.0 months, and 144 months for negative patients, p=0.001. (G) The mPFS of patients with PET/BM false positive (PET+BMB-) and PET/BM true positive (PET+BMB+) were 23.0 months and 2.0 months, respectively, p=0.057. (H) The mOS of patients with PET/BM false and true positive were 23.0 months and 4.0 months, respectively, p=0.163.
Survival outcomes following combined PET/CT and BMB were also investigated. For the PFS evaluation (Figure 2G), the ten PET/BM false positive patients (PET/BM positive but BMB negative, PET+BMB−) had an mPFS of 23.0 months (95% CI not estimated), while PET/BM true positive (both PET/BM-positive and BMB-positive, PET+BMB+) patients had an mPFS of 2.0 months (95% CI, 0.3–3.7 months) (p = 0.057). Similarly, the mOS of PET/BM false positive cases was 23.0 months (95% CI not estimated), while the mOS of PET/BM true positive patients was 4.0 months (95% CI, 0.6–7.4 months) (p = 0.163) (Figure 2H).
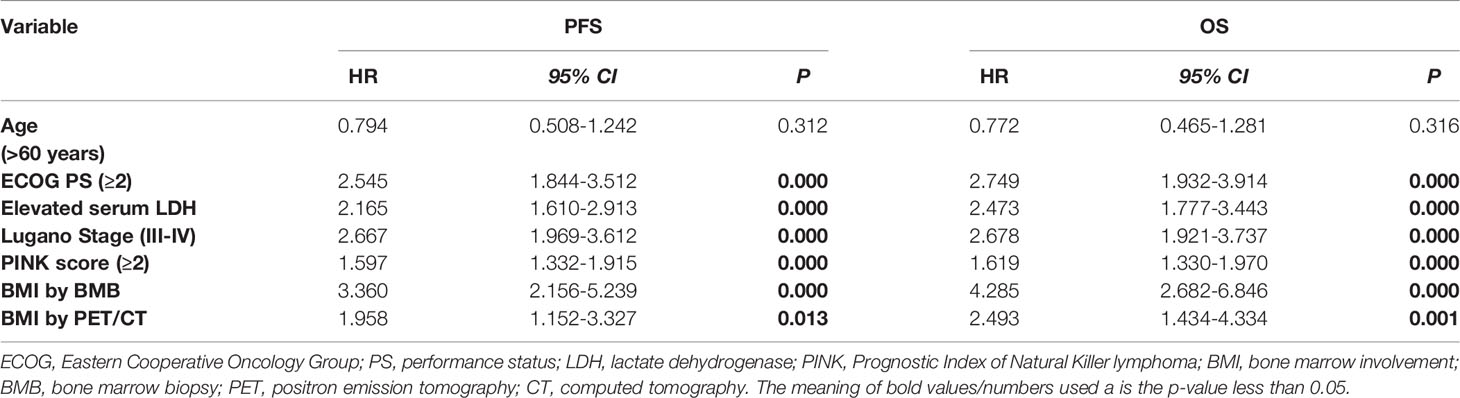
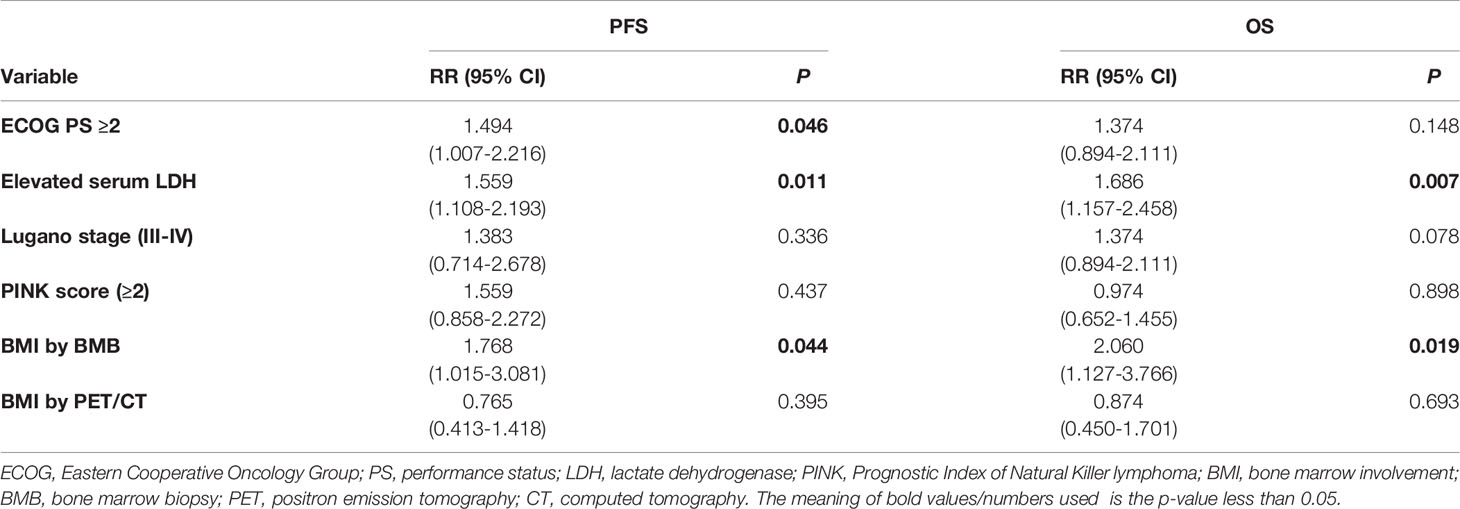
Univariate and multivariate analyses were also performed for this cohort. In the univariate analyses, the Eastern Cooperative Oncology Group (ECOG) performance status (PS) score ≥2, elevated serum LDH, the Lugano stages III–IV, the PINK score ≥2, and BMI using BMB or PET/CT were significantly associated with inferior PFS and OS (Table 4). The parameters identified as statistically significant risk factors (p <0.05) were assessed by multivariate logistic regression and collinearity analysis was performed between the variables in the Cox proportional-hazards model. Patients with an ECOG PS score of ≥2 (RR 1.494, p = 0.046), elevated serum LDH (RR 1.958, p = 0.011), and a positive BMB (RR 1.768, p = 0.044) had inferior PFS, while those with elevated serum LDH (RR 1.686, p = 0.007) and a positive BMB (RR 2.060, p = 0.019) had shorter OS (Table 5).
Discussion
This study evaluated the use of PET/CT to detect BMI and assessed whether it could replace BMB for the initial staging of ENKTL. A positive BMB result was applied as the standard criterion for BMI. The findings showed that while the specificity was 96.9%, the sensitivity was only 46.2%. Like the prognosis performance of BMB, PET/BM-negative patients had better PFS and OS than PET/BM-positive patients. To our knowledge, this is the largest series to date that has examined the ability of PET/CT to detect BMI in ENKTL patients undergoing BMB staging.
By BMB, ENKTL infiltrates the BM in up to 7% of patients (25, 26). In the study cohort, 7.3% of all patients and 27.4% of advanced-stage patients had BMI according to BMB. Because of its high sensitivity, PET/CT has become a frequently used tool for staging, response evaluation, and follow-up after treatment of patients with ENKTL. Suchitra et al. (27) reported that among 60 T/NK-cell lymphoma patients, which only included seven cases of ENKTL, PET/CT had 53.3% sensitivity and 100% specificity to detect BMI. Three published studies have evaluated the use of PET/CT to detect BMI among patients with ENKTL. One study (28) of 55 ENKTL patients showed that 5/12 PET/BM-positive patients were confirmed by BMB and the true positivity and negativity were 100 and 86%, respectively. Another study (22) found that four patients with advanced-stage ENKTL with BMI by PET/CT were BMB positive, indicating a sensitivity and specificity of 100 and 92.8%, respectively. Youngil et al. reported (29) that among 109 patients with T/NK-cell lymphoma, including 46 ENKTL, the sensitivity and specificity of PET/CT for diagnosing BMI in ENKTL were 58.3% and 85.3% by visual analysis.
In this study, the sensitivity of 46.2% was much lower than that reported previously, while the specificity of 96.9% was higher (22, 27, 28). This may be because the sample size used in this study was much larger than that used in previous studies (22, 27, 28). Additionally, the current study diagnosed 26 patients with BMI by BMB and 22 by PET/CT, which was more than five times as many as were identified previously (22). The only true positive results ever reported were also BM positive and contained bone lesions using both PET/CT and BMB (22). Of the 22 patients who were PET/BM positive in this study, the lesion sites included the sternum, ribs, humerus, pelvis, femur, and tibia. However, the BMB was performed only by unilateral iliac crest biopsy, which may cause false-negative results. Future studies should emphasize that BMI locations other than the iliac crest identified by PET/CT should be confirmed by targeted biopsy or complementary magnetic resonance imaging (MRI) in advanced-stage patients.
BMI identified by BMB is an indicator of poor prognosis among ENKTL patients (14, 22, 28). The current study supports prior findings that BMB-positive patients have inferior PFS and OS. However, few studies have assessed the prognosis of PET/BM-positive patients on a large scale. This study found that PET/BM-negative patients also had longer mPFS and mOS than PET/BM-positive patients, supporting the results of smaller sample-sized studies (22, 28). Prognostic performance was also assessed for combined PET/BM and BMB. Although the PET/BM false positives tended to have a better prognosis, the differences were not significant. This may be because, although being the largest to date, the sample size was too small to detect a difference. It is also possible that there were more than 12 PET/BM true positive patients because the targeted BMB and the MRI results were not considered, which may have affected the results. Consistent with previous results (22), BMI detected by PET/CT was associated with inferior survival in the univariate analysis. The significant prognostic difference between PET/BM-positive and negative patients disappeared in the COX proportional hazard model (p = 0.395 for mPFS and p = 0.693 for mOS) but remained for BMB-positive and negative patients, indicating that BMB has a better prognostic performance for BMI than PET/CT.
Based on these findings, we suggest that when PET/CT staging is limited to stages I–II, the BM evaluation by BMB can be omitted on the basis of the strong specificity of PET/CT. Otherwise, the BM evaluation by BMB should be used to exclude false results regardless of the PET/BM status. A future prospective randomized trial should verify these results.
This study had several limitations. First, the BMB was performed only at the iliac crest and for BMI suspected in other locations by PET/CT, like the sternum and femur, targeted BMB or MRI were not conducted, potentially decreasing PET/BM sensitivity. Second, this study was retrospective, so the data are likely to include some selection and information bias. Third, the data included patients receiving a range of first-line treatments that may have an unexpected bias on survival outcomes.
In conclusion, 18F-FDG PET/CT showed the potential to replace BMB for the initial staging of early-stage ENKTL patients, while baseline PET/CT could not provide an accurate BMI evaluation for advanced-stage patients. A prospective study is needed to confirm the diagnostic performance of BMI identification by PET/CT combined with targeted BMB and MRI for advanced-stage patients.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethics Committee of West China Hospital of Sichuan University. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author Contributions
LZ: Conception and design. CY, WW, HZ, and MY: Collection and analysis of data. SZ: Pathological review. RT: PET/CT review. All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Vose J, Armitage J, Weisenburger D. International Peripheral T-Cell and Natural Killer/T-Cell Lymphoma Study: Pathology Findings and Clinical Outcomes. J Clin Oncol (2008) 26:4124–30. doi: 10.1200/JCO.2008.16.4558
2. Au WY, Weisenburger DD, Intragumtornchai T, Nakamura S, Kim WS, Sng I, et al. Clinical Differences Between Nasal and Extranasal Natural Killer/T-Cell Lymphoma: A Study of 136 Cases From the International Peripheral T-Cell Lymphoma Project. Blood (2009) 113:3931–7. doi: 10.1182/blood-2008-10-185256
3. Qi SN, Yang Y, Song YQ, Wang Y, He X, Hu C, et al. First-Line non-Anthracycline-Based Chemotherapy for Extranodal Nasal-Type NK/T-Cell Lymphoma: A Retrospective Analysis From the CLCG. Blood Adv (2020) 4:3141–53. doi: 10.1182/bloodadvances.2020001852
4. Fox CP, Civallero M, Ko Y-H, Manni M, Skrypets T, Pileri S, et al. Survival Outcomes of Patients With Extranodal Natural-Killer T-Cell Lymphoma: A Prospective Cohort Study From the International T-Cell Project. Lancet Haematol (2020) 7:e284–94. doi: 10.1016/S2352-3026(19)30283-2
5. Zhang L, Wang Y, Li X, Li L, Wang X, Sun Z, et al. Radiotherapy vs Sequential Pegaspargase, Gemcitabine, Cisplatin and Dexamethasone and Radiotherapy in Newly Diagnosed Early Natural Killer/T-Cell Lymphoma: A Randomized, Controlled, Open-Label, Multicenter Study. Int J Cancer (2021) 148:1470–7. doi: 10.1002/ijc.33329
6. Zhang L, Jiang M, Xie L, Zhang H, Jiang Y, Yang QP, et al. Five-Year Analysis From Phase 2 Trial of "Sandwich" Chemoradiotherapy in Newly Diagnosed, Stage IE to IIE, Nasal Type, Extranodal Natural Killer/T-Cell Lymphoma. Cancer Med (2016) 5:33–40. doi: 10.1002/cam4.569
7. Bi X-w, Xia Y, Zhang WW, Sun P, Liu PP, Wang Y, et al. Radiotherapy and PGEMOX/GELOX Regimen Improved Prognosis in Elderly Patients With Early-Stage Extranodal NK/T-Cell Lymphoma. Ann Hematol (2015) 94:1525–33. doi: 10.1007/s00277-015-2395-y
8. Wang YQ, Yang Y, Zhuo HY, Zou LQ, Jiang Y, Jiang M. Trial of LVDP Regimen (L-Asparaginase, Etoposide, Dexamethasone, and Cisplatin, Followed by Radiotherapy) as First-Line Treatment for Newly Diagnosed, Stage III/IV Extranodal Natural Killer/T Cell Lymphoma. Med Oncol (Northwood London England) (2015) 32:435. doi: 10.1007/s12032-014-0435-4
9. Li X, Cui Y, Sun Z, Zhang L, Li L, Wang XH, et al. DDGP Versus SMILE in Newly Diagnosed Advanced Natural Killer/T-Cell Lymphoma: A Randomized Controlled, Multicenter, Open-Label Study in China. Clin Cancer Res (2016) 22:5223–8. doi: 10.1158/1078-0432.CCR-16-0153
10. Wang J-H, Wang L, Liu CC, Xia ZJ, Huang HQ, Lin TY, et al. Efficacy of Combined Gemcitabine, Oxaliplatin and Pegaspargase (P-Gemox Regimen) in Patients With Newly Diagnosed Advanced-Stage or Relapsed/Refractory Extranodal NK/T-Cell Lymphoma. Oncotarget (2016) 7:29092–101. doi: 10.18632/oncotarget.8647
11. Yamaguchi M, Kwong Y-L, Kim WS, Maeda Y, Hashimoto C, Suh C, et al. Phase II Study of SMILE Chemotherapy for Newly Diagnosed Stage IV, Relapsed, or Refractory Extranodal Natural Killer (NK)/T-Cell Lymphoma, Nasal Type: The NK-Cell Tumor Study Group Study. J Clin Oncol (2011) 29:4410–6. doi: 10.1200/JCO.2011.35.6287
12. Lister TA, Crowther D, Sutcliffe SB, Glatstein E, Canellos GP, Young RC, et al. Report of a Committee Convened to Discuss the Evaluation and Staging of Patients With Hodgkin's Disease: Cotswolds Meeting. J Clin Oncol (1989) 7:1630–6. doi: 10.1200/JCO.1989.7.11.1630
13. Cheson BD, Fisher RI, Barrington SF, Cavalli F, Schwartz LH, Zucca E, et al. Recommendations for Initial Evaluation, Staging, and Response Assessment of Hodgkin and non-Hodgkin Lymphoma: The Lugano Classification. J Clin Oncol (2014) 32:3059–68. doi: 10.1200/JCO.2013.54.8800
14. Huang W-T, Chang K-C, Huang GC, Hsiao JR, Chen HHW, Chuang SS, et al. Bone Marrow That is Positive for Epstein-Barr Virus Encoded RNA-1 by in Situ Hybridization is Related With a Poor Prognosis in Patients With Extranodal Natural Killer/T-Cell Lymphoma, Nasal Type. Haematologica (2005) 90:1063–9. doi: 10.3324/%25x
15. Jia J, Song Y, Lin N, Liu W, Ping L, Zheng W, et al. Clinical Features and Survival of Extranodal Natural Killer/T Cell Lymphoma With and Without Hemophagocytic Syndrome. Ann Hematol (2016) 95:2023–31. doi: 10.1007/s00277-016-2805-9
16. Li N, Jiang M, Wu WC, Wei WW, Zou LQ. How to Identify Patients at High Risk of Developing Nasal-Type, Extranodal Nature Killer/T-Cell Lymphoma-Associated Hemophagocytic Syndrome. Front Oncol (2021) 11:704962. doi: 10.3389/fonc.2021.704962
17. Moon SH, Cho SK, Kim W-S, Kim S, Ahn Y, Choe Y, et al. The Role of 18F-FDG PET/CT for Initial Staging of Nasal Type Natural Killer/T-Cell Lymphoma: A Comparison With Conventional Staging Methods. J Nucl Med (2013) 54:1039–44. doi: 10.2967/jnumed.112.113399
18. El-Galaly TC, d'Amore F, Mylam K, Brown P, Bøgsted M, Bukh A, et al. Routine Bone Marrow Biopsy has Little or No Therapeutic Consequence for Positron Emission Tomography/Computed Tomography-Staged Treatment-Naive Patients With Hodgkin Lymphoma. J Clin Oncol (2012) 30:4508–14. doi: 10.1200/JCO.2012.42.4036
19. Khan A, Barrington S, Mikhaeel N, Hunt A, Cameron L, Morris T, et al. PET-CT Staging of DLBCL Accurately Identifies and Provides New Insight Into the Clinical Significance of Bone Marrow Involvement. Blood (2013) 122:61–7. doi: 10.1182/blood-2012-12-473389
20. Kaddu-Mulindwa D, Altmann B, Held G, Angel S, Stilgenbauer S, Thurner L, et al. FDG PET/CT to Detect Bone Marrow Involvement in the Initial Staging of Patients With Aggressive non-Hodgkin Lymphoma: Results From the Prospective, Multicenter PETAL and OPTIMAL>60 Trials. Eur J Nucl Med Mol Imaging (2021) 48:3550–9. doi: 10.1007/s00259-021-05348-6
21. Swerdlow SH, Campo E, Harris N, Jaffe ES, Pileri SA, Stein H, et al. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. In: International Agency for Research on Cancer (IARC) 69372 Lyon Cedex 08. France (2017).
22. Wang Y, Xie L, Tian R, Deng Y, Zhang W, Zou L, et al. PET/CT-Based Bone-Marrow Assessment Shows Potential in Replacing Routine Bone-Marrow Biopsy in Part of Patients Newly Diagnosed With Extranodal Natural Killer/T-Cell Lymphoma. J Cancer Res Clin Oncol (2019) 145:2529–39. doi: 10.1007/s00432-019-02957-5
23. Clopper CJ, Pearson ES. The Use of Confidence or Fiducial Limits Illustrated in the Case of the Binomial Biometrika. Biometrika (1934) 26:404–13. doi: 10.1093/biomet/26.4.404
24. Kim S, Yoon D, Jaccard A, Chng W, Lim S, Hong H, et al. A Prognostic Index for Natural Killer Cell Lymphoma After Non-Anthracycline-Based Treatment: A Multicentre, Retrospective Analysis. Lancet Oncol (2016) 17:389–400. doi: 10.1016/S1470-2045(15)00533-1
25. Kim TM, Lee SY, Jeon YK, Ryoo BY, Cho GJ, Hong YS, et al. Clinical Heterogeneity of Extranodal NK/T-Cell Lymphoma, Nasal Type: A National Survey of the Korean Cancer Study Group. Ann Oncol (2008) 19:1477–84. doi: 10.1093/annonc/mdn147
26. Lee J, Kim WS, Park YH, Park SH, Park KW, Kang JH, et al. Nasal-Type NK/T Cell Lymphoma: Clinical Features and Treatment Outcome. Br J Cancer (2005) 92:1226–30. doi: 10.1038/sj.bjc.6602502
27. Sundaram S, Jizzini M, Lamonica D, Attwood K, Gravina M, Hernandez M, et al. Utility of Bone Marrow Aspirate and Biopsy in Staging of Patients With T-Cell Lymphoma in the PET-Era - Tissue Remains the Issue. Leuk Lymphoma (2020) 61:3226–33. doi: 10.1080/10428194.2020.1798950
28. Zhou Z, Chen C, Li X, Li Z, Zhang X, Chang Y, et al. Evaluation of Bone Marrow Involvement in Extranodal NK/T Cell Lymphoma by FDG-PET/Ct. Ann Hematol (2015) 94:963–7. doi: 10.1007/s00277-014-2289-4
Keywords: extranodal NK/T-cell lymphoma, 18F-FDG PET/CT, bone marrow biopsy, bone marrow involvement, diagnosis, prognosis
Citation: Yang C, Wu W, Zhou H, Zhao S, Tian R, Xiang M and Zou L (2022) 18F-FDG PET/CT Plays a Limited Role in Replacing Bone Marrow Biopsy for Newly Diagnosed Advanced-Stage Patients With Extranodal Natural Killer/T-Cell Lymphoma. Front. Oncol. 12:894804. doi: 10.3389/fonc.2022.894804
Received: 12 March 2022; Accepted: 21 June 2022;
Published: 26 July 2022.
Edited by:
Yuqin Song, Peking University, ChinaReviewed by:
Shih-Sung Chuang, Chi Mei Medical Center, TaiwanTanuja Shet, Tata Memorial Hospital, India
Copyright © 2022 Yang, Wu, Zhou, Zhao, Tian, Xiang and Zou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Liqun Zou, aHhsY3l4eUAxNjMuY29t
 Chunli Yang
Chunli Yang Wanchun Wu
Wanchun Wu Huijie Zhou2
Huijie Zhou2 Rong Tian
Rong Tian Liqun Zou
Liqun Zou