
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Oncol., 10 June 2022
Sec. Thoracic Oncology
Volume 12 - 2022 | https://doi.org/10.3389/fonc.2022.889161
 Haiyan Zeng1*
Haiyan Zeng1* Danyang Zheng2,3
Danyang Zheng2,3 Willem J. A. Witlox4
Willem J. A. Witlox4 Antonin Levy5,6
Antonin Levy5,6 Alberto Traverso1
Alberto Traverso1 Feng-Ming (Spring) Kong2,3
Feng-Ming (Spring) Kong2,3 Ruud Houben1
Ruud Houben1 Dirk K. M. De Ruysscher1
Dirk K. M. De Ruysscher1 Lizza E. L. Hendriks7
Lizza E. L. Hendriks7The use of prophylactic cranial irradiation (PCI) for small cell lung cancer (SCLC) patients is controversial. Risk factors for brain metastasis (BM) development are largely lacking, hampering personalized treatment strategies. This study aimed to identify the possible risk factors for BM in SCLC.We systematically searched the Pubmed database (1 January 1995 to 18 January 2021) according to the PRISMA guidelines. Eligibility criteria: studies reporting detailed BM data with an adequate sample size (randomized clinical trials [RCTs]: N ≥50; non-RCTs: N ≥100) in patients with SCLC. We summarized the reported risk factors and performed meta-analysis to estimate the pooled hazard ratios (HR) if enough qualified data (i.e., two or more studies; the same study type; the same analysis method; and HRs retrievable) were available. In total, 61/536 records were eligible (18 RCTs and 39 non-RCTs comprising 13,188 patients), in which 57 factors were reported. Ten factors qualified BM data for meta-analysis: Limited stage disease (LD) (HR = 0.34, 95% CI: 0.17–0.67; P = 0.002) and older age (≥65) (HR = 0.70, 95% CI: 0.54–0.92; P = 0.01) were associated with less BM; A higher T stage (≥T3) (HR = 1.72, 95% CI: 1.16–2.56; P = 0.007) was a significant risk factor for BM. Male sex (HR = 1.24, 95% CI: 0.99–1.54; P = 0.06) tended to be a risk factor, and better PS (0–1) (HR = 0.66, 95% CI: 0.42–1.02; P = 0.06) tended to have less BM. Smoking, thoracic radiotherapy dose were not significant (P >0.05). PCI significantly decreased BM (P <0.001), but did not improve OS in ED-SCLC (P = 0.81). A higher PCI dose did not improve OS (P = 0.11). The impact on BM was conflicting between Cox regression data (HR = 0.59, 95% CI: 0.26–1.31; P = 0.20) and competing risk regression data (HR = 0.74, 95% CI: 0.55–0.99; P = 0.04). Compared to M0–M1a, M1b was a risk factor for OS (P = 0.01) in ED-SCLC, but not for BM (P = 0.19). As regular brain imaging is rarely performed, high-quality data is lacking. Other factors such as N-stage and blood biomarkers had no qualified data to perform meta-analysis. In conclusion, younger age, higher T stage, and ED are risk factors for BM, suggesting that PCI should be especially discussed in such cases. Individual patient data (IPD) meta-analysis and well-designed RCTs are needed to better identify more risk factors and further confirm our findings. Systematic Review Registration: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021228391, identifier CRD42021228391.
Small cell lung cancer (SCLC) accounts for about 13% of newly diagnosed lung cancers worldwide (1). Brain metastases (BM) are a very common metastatic site in SCLC: more than 10% of patients have BM at initial diagnosis, more than 50% will develop BM within 2 years, and up to 80% of all patients are found to have BM at autopsy (2). Patients with SCLC and BM have a dismal survival rate, with a 2-year survival rate below 2% (3). Furthermore, BM have a negative impact on the quality of life (QoL). Prophylactic cranial irradiation (PCI) significantly reduces the incidence of BM in patients with SCLC (4, 5). However, because of potential neurotoxicity (6, 7) and possible limited survival, especially in metastatic SCLC (8, 9), PCI is increasingly questioned. Additionally, stereotactic radiosurgery (SRS) has become more available and may represent an attractive therapeutic alternative (10). As a consequence, SCLC guidelines encourage shared decision making regarding PCI for particular subgroup of patients, such as the elderly, very early stages, or extensive stage disease (ED) (11, 12), However, shared decision making is hampered by the fact that risk factors for BM development are largely unknown in SCLC patients. The specific risk of BM (high vs low) could also be used as a stratification factor to better control confounders in trials evaluating BM prevention strategies such as PCI. Therefore, we performed a systematic review and meta-analysis to summarize the possible risk factors for BM in patients with SCLC to support better management of SCLC patients and a better design of SCLC randomized controlled trials (RCTs).
We conducted this study according to the PRISMA guideline (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) (13) and registered it with PROSPERO (CRD42021228391) (14). We performed a systematic literature search in the PubMed database from 1 January 1995 to the search date (18 January 2021), adhering to the PICO method (15) (Appendix Table 1). The description of these components is presented in (Appendix Table 2). The study eligibility criteria were as follows: 1. SCLC patients without baseline BM; 2. with detailed BM data; 3. had adequate sample size (defined as: retrospective studies or prospective observational/single arm studies [non-RCTs]: N ≥100 patients; RCTs: N ≥50). The detailed criteria are shown in Appendix Table 3. We assessed the “risk of bias” for BM in eligible RCTs using the Revised Cochrane risk-of-bias tool for randomized trials (RoB2) (16, 17). We did not grade non-RCTs separately because of the inherent disadvantages of this type of study.
We extracted data according to our published protocol (14) and reported the following critical items: title, the first author, journal, publication year, study design, recruitment period, sample size, age, performance status (PS), sex, thoracic radiotherapy (TRT), surgery, chemotherapy, PCI, follow-up time, statistical analysis, the results of possible risk factors for BM and OS (numbers of events/patients, hazard ratio [HR], 95% CI, and p-value), and conclusion. We also reported the following items for each RCT: brain magnetic resonance imaging (MRI) or computed tomography (CT) at baseline and before PCI; scheduled brain CT or MRI during follow-up; brain imaging contrast-enhanced or not; BM as primary or secondary outcome. We applied the Web Plot Digitizer (18) to extract survival data from plots if necessary.
Two investigators (HZ and DZ) independently screened the titles, abstracts, methods, and full texts for eligibility; extracted data; and assessed the risk of bias. Any conflicts in each step were resolved through discussion with a third investigator (LH).
Our primary endpoint was BM. When such data were available, we also analyzed OS to further interpret the clinical significance. The effect of the factors on BM and OS was expressed as an HR, being the most appropriate metric for summarizing time-to-event data (19). We first analyzed each factor for BM per study. If two or more studies investigated the factor’s impact on BM with homogenous methodology and outcomes, we performed a meta-analysis with Rev Man 5.4.1 using the EXP[(O − E)/Var] method. If the OS data were not available in one or more studies that were included for the BM meta-analysis, the meta-analysis for OS would not be performed to avoid missing outcome bias. To minimize bias, we used the adjusted rather than the univariate HR if possible. We calculated the observed (O) minus expected (E) number of events and its variance (V) for each study according to the methods of Tierney et al. (20). If similar data were reported by researchers from the same group, only the latest one was included for meta-analysis to avoid data overlapping. Meta-analysis was performed separately for RCTs and non-RCTs to avoid misleading conclusions. A meta-analysis of non-RCTs was not performed if there were sufficient RCTs addressing this issue (21). We used I2 to quantify inter-study heterogeneity, of which 25, 50, and 75% can be considered low, moderate, and high heterogeneity (22). If I2 >50%, we performed a random-effects meta-analysis (23, 24) using R version 4.1.2 with the “meta” package.
The systematic review identified 536 records, of which 61 records met the inclusion criteria (22 records for 18 RCTs comprising 5,060 patients and 39 non-RCTs comprising 8,128 patients [including two prospective observational studies comprising 544 patients]) (Figure 1). All 18 RCTs were published between 1995 and 2019, but only three were from 2010 to 2019 (25–27). As shown in Appendix Tables 4, 5, BM was the primary endpoint in three trials (5, 28–30). Brain MRI/CT was performed before treatment of patients in two trials (27, 31) and before PCI in six trials (9, 26, 28, 30–32). In five trials, brain CT/MRI was scheduled during follow-up (9, 26, 28, 30, 33) and in one trial [PCI85 (28)], the number of performed CT scans at pre-specified time points was mentioned (which indicated low compliance). As regular brain imaging was not performed in most trials, asymptomatic BM will have been missed, which has resulted in a high risk of bias at domain 4 (measurement method) or domain 3 (missing outcome) according to RoB2. Because of that, two RCTs were assessed to be at low risk of bias, while the others were at high risk of bias (Figure 2). The 39 non-RCTs were published from 1995 to 2020, among which 32 were from 2010 to 2020. The study design, characteristics, and treatments of patients are shown in Appendix Table 6.
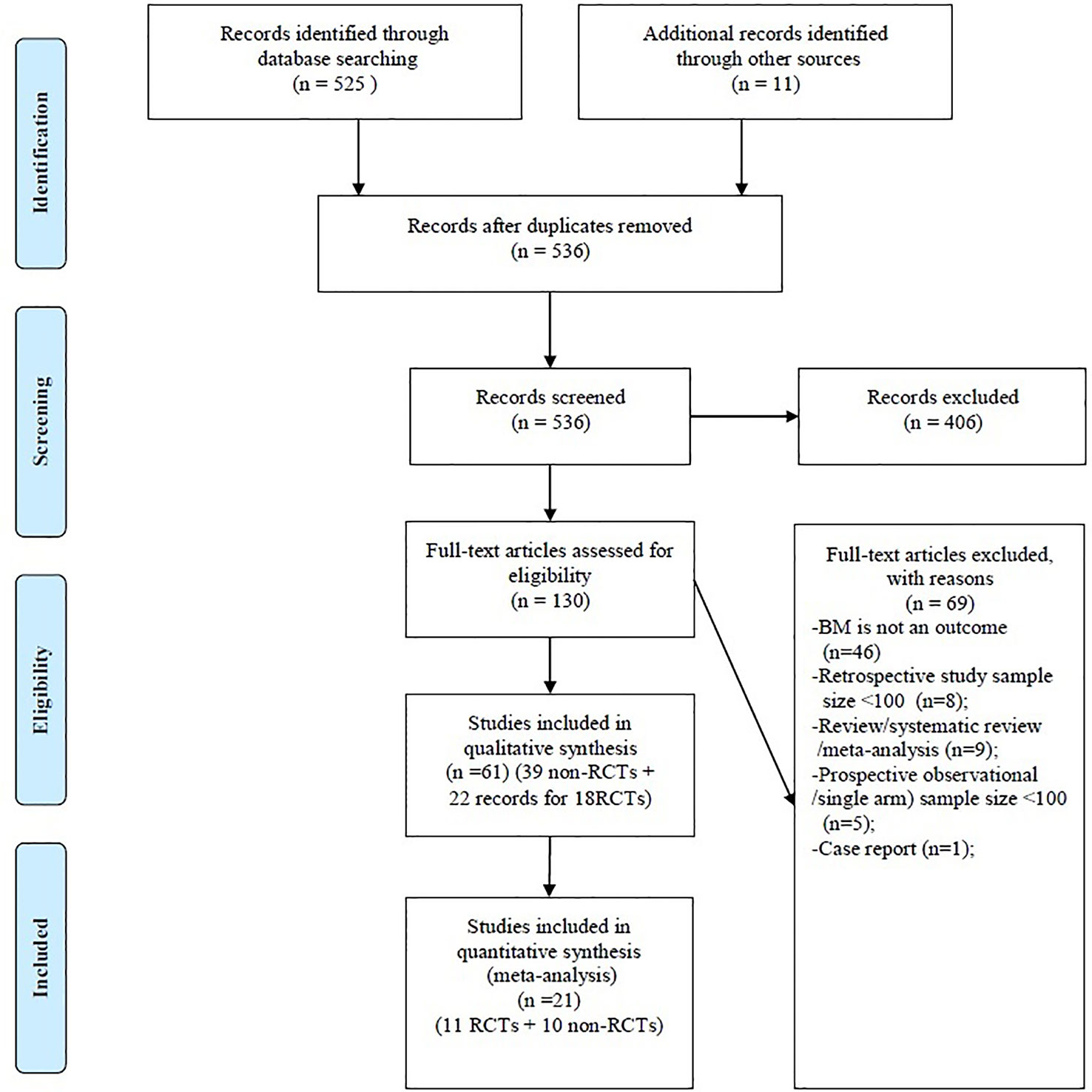
Figure 1 PRISMA flow diagram. BM, brain metastasis; Non-RCTs, non-randomized clinical trials; RCTs, Randomized clinical trials.
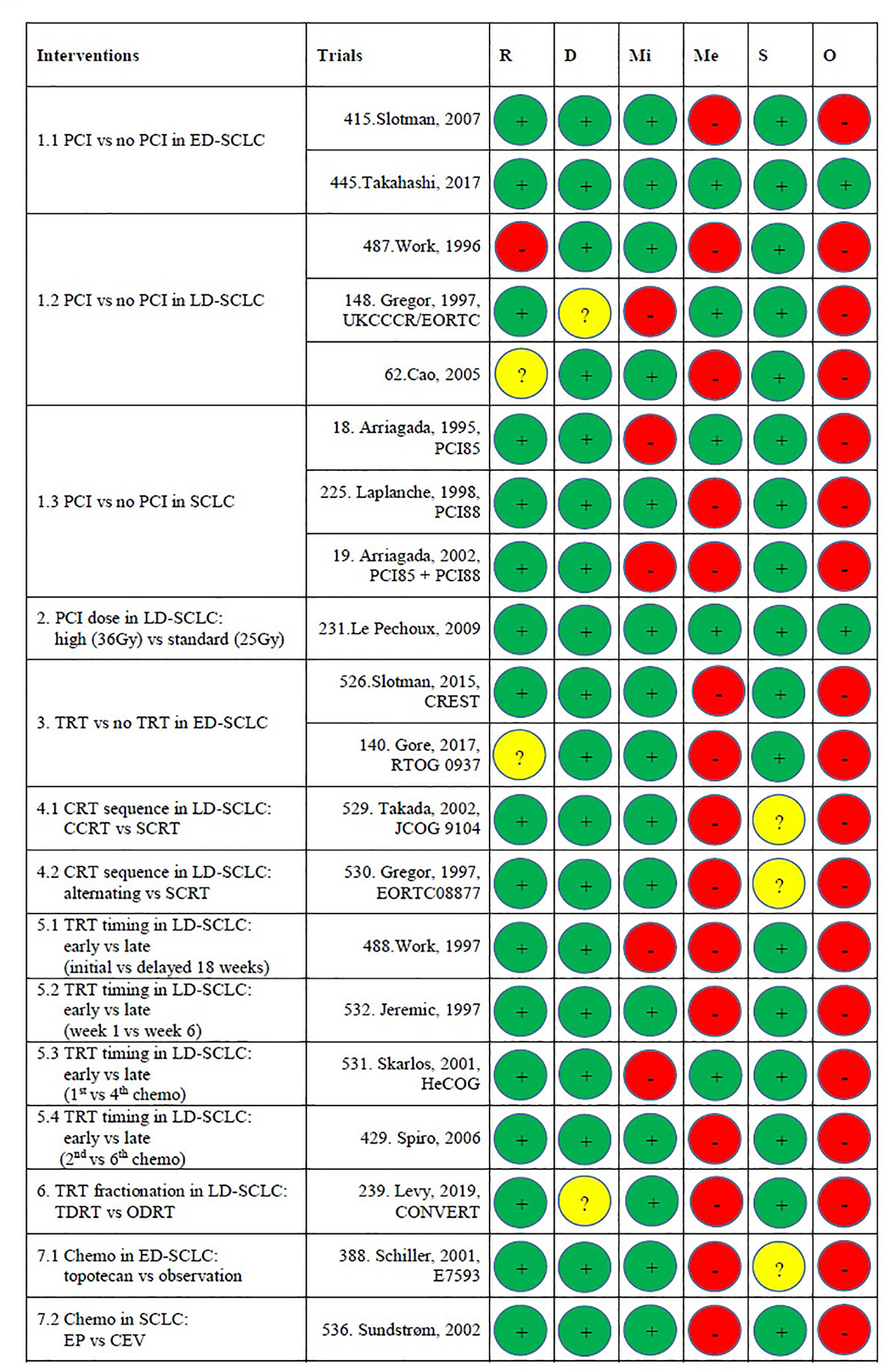
Figure 2 Risk of bias assessments. Risk of bias legend. R, Bias arising from the randomization process; D, Bias due to deviations from intended interventions; Mi, Bias due to missing outcome data; Me, Bias in measurement of the outcome; S, Bias in selection of the reported results; O, Overall risk of bias. Domain 1: Risk of bias arising from the randomization process: The study conducted by Work et al. (34) was at high risk of bias because PCI vs no PCI was not strictly randomized. The study conducted by Cao et al. had “some concerns” because of no information about the random allocation sequence. RTOG 0937 had “some concerns” because baseline age was unbalanced between arms (P = 0.03). The other 16 studies were assessed as at low risk of bias. Domain 2: Risk of bias due to deviations from the intended interventions (effect of assignment to intervention): The CONVERT trial was assessed to have “some concerns” because it is unclear whether there were deviations from the intended intervention that arose because of the trial context. The UKCCCR/EORTC trial was assessed to have “some concerns” since there were deviations from the intended intervention that arose because of the trial context. The others were at low risk. Domain 3: Missing outcome data: This domain is difficult to tell because most trials did not have a regular brain CT/MRI scan plan during the follow-up. In the trials that did have a pre-planned brain CT/MRI scan schedule, only one trial (IPC85) mentioned the compliance at some time point. Readers do not know how many data were missing. The UKCCCR/EORTC trial and HeCOG were at high risk because of no information about missing data. IPC85, the pooled analysis of IPC85+ IPC88, and the study conducted by Work et al. (35) were at high risk because many data were missing but there were no evidence that the result was not biased by missing data. The other 14 studies were at low risk. Domain 4: Risk of bias in measurement of the outcome: 14 studies were judged to be at high risk because the method of measuring the outcome (BM) was inappropriate. They performed brain MRI/CT when patients experience neurological symptoms. The other five trials were at low risk because they had pre-planned brain MRI/CT scan during follow-up. Domain 5: Risk of bias in selection of the reported result: JCOG 9104, E7593, and the trial conducted by Gregor et al. (EORTC) had “some concerns” because of no information about pre-specified analysis plan or selection from multiple eligible analyses. Overall risk of bias: Only the studies conducted by Le Pechoux et al. and Takahashi et al. were judged to be at low risk of bias. The other 17 trials were judged as high risk of bias. This is mainly because of domains 3 and 4. CCRT, concurrent chemoradiotherapy; CEV, cyclophosphamide–epirubicin–vincristine; chemo, chemotherapy; CRT, chemoradiotherapy; ED, extensive-stage disease; EP, etoposide-platinum; LD, limited-stage disease; ODRT, once-daily radiotherapy; PCI, prophylactic cranial irradiation; SCLC, small cell lung cancer; SCRT, sequential chemoradiotherapy; TDRT, twice-daily radiotherapy; TRT, thoracic radiotherapy.
In addition to symptomatic BM, we found that the pre-PCI BM (BM immediately before PCI) was investigated in one study (36) and the first isolated BM event, rather than overall BM during the whole disease course, was analyzed in five studies (37–41). Both the first isolated BM and overall BM were reported in eight papers (28–30, 42–46) and showed that the first isolated BM incidence was lower than the overall BM incidence (Table 1). We only performed meta-analysis for overall BM because this is more relevant than a first isolated BM event.
We also found that the definition of time to BM events varied among studies, which indicates that heterogeneity also exists between RCTs: from the date of initial diagnosis (n = 19) (45, 49, 51, 53, 55, 58–62, 64, 66, 71, 72, 74–76, 78, 81); from the date of randomization (n = 16) (5, 9, 25, 26, 28–32, 34, 35, 41, 46, 68, 79, 80); from the date of treatment initiation (n = 6) (37, 42, 47, 57, 69, 77); from the end of chemoradiotherapy (CRT) (n = 5) (44, 47, 67, 70, 78); from the date of PCI (n = 4) (27, 48, 54, 65); from the date of chemotherapy initiation (n = 3) (33, 38, 39); from the date of TRT initiation (n = 2) (43, 56); from the date of surgery (n = 1) (50); five studies had no information (36, 40, 52, 63, 73), two studies applied two definitions (47, 78).
More importantly, we noticed that the statistical analyses for BM varied considerably: Competing risk regression: n = 12 (47, 56, 60, 73), RCT: N = 8 (5, 9, 26–30, 46); Cox proportional hazard regression: n = 20 (37, 38, 43, 45, 48–53, 55, 57–59, 61, 70), RCT: N = 4 (31, 33, 40, 41); Log-rank test n = 16 (43, 44, 62, 64–66, 72, 74, 75, 78), RCT: N = 6 (25, 32, 34, 35, 68, 79); Logistic regression: n = 3 (36, 54, 63); χ2-test or Fisher exact 2-tailed test: n = 7 (39, 69, 71, 76, 77), RCT: N = 2 (67, 80); Descriptive: n = 2 (42, 81). Statistical analysis for OS was always performed using survival analysis (Kaplan–Meier, Log-rank test, and Cox regression).
In total, 57 factors were reported in all studies, namely, 8 baseline factors, 27 tumor-related factors, and 22 treatment-related factors (Table 1). However, they were investigated in various ways with different participants, such as LD, or ED, or resected SCLC, or patients with PCI. Details are shown in the comments in Table 1. Hence, 10 factors had qualified BM data from 21 studies (11 RCTs + 10 non-RCTs [all were retrospective studies]) and four factors had qualified OS data for meta-analysis (Tables 1, 2).
1. Age: Age was investigated in 18 studies with seven different methods (different age groups, continuous vs group) (Table 1). It was concluded that age was not an independent risk factor for BM or OS in 14 studies (36, 38, 43, 47, 48, 51, 53–57, 59–61). Three studies (49, 51, 52) were eligible to perform BM meta-analysis and showed that patients with advanced age (≥65) had less BM than younger patients (HR = 0.70, 95% CI: 0.54–0.92; P = 0.01) (Figure 3A).
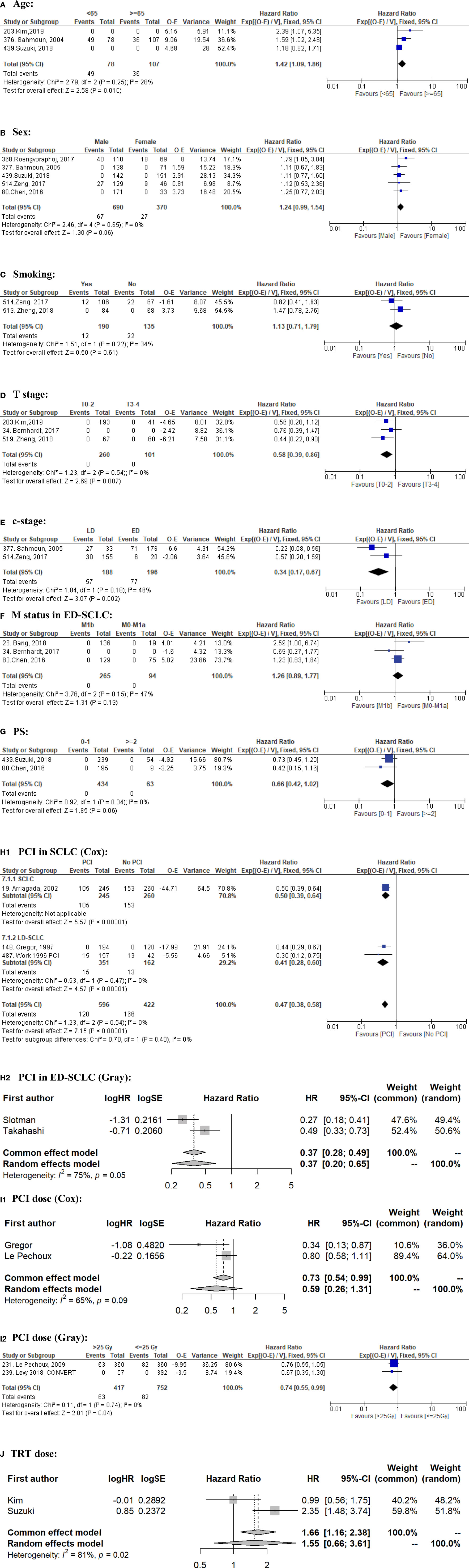
Figure 3 Forrest plots for BM: (A) Age; (B) Sex; (C) Smoking; (D) T stage; (E) c-stage; (F) M status in ED-SCLC; (G) PS; (H1) PCI in SCLC; (H2) PCI in ED-SCLC; (I1) PCI dose (Cox); (I2) PCI dose (Gray); (J) TRT dose. BM, brain metastasis; LD, limited-stage disease; ED, extensive-stage disease; SCLC, small cell lung cancer; PCI, prophylactic cranial irradiation; PS, performance status; TRT, thoracic radiotherapy; O, observed events; E, expected events; V, variance; CI, confidence interval; HR, hazard ratio; SE, standard error.
2. Sex: Sex was investigated in 16 studies. It concluded that sex was not an independent risk factor for BM or OS in 13 studies (36, 38, 47, 49–51, 53–56, 59–61). Five studies (51, 53, 58, 59, 62) were eligible to perform a meta-analysis for BM and showed that male sex tends to be a risk factor for BM (HR = 1.24, 95% CI: 0.99–1.54; P = 0.06) (Figure 3B).
3. Smoking: Smoking was investigated in seven studies. It has been shown that smoking is not a significant risk factor for BM or OS (36, 50, 51, 53, 55, 56, 61). Two studies (53, 55) were eligible to perform meta-analysis for BM and showed that smoking (ever vs never) was indeed not a significant risk factor for BM (HR = 1.13, 95% CI: 0.71–1.79; P = 0.61) (Figure 3C).
1. TNM cT stage: The T stage was investigated in four studies with conflicting conclusions (36, 48, 52, 55). Three studies (48, 52, 55) had qualified BM data for meta-analysis and showed that patients with a higher T stage (T ≥3) had a statistically significantly higher risk of BM than patients with lower T stages (HR = 1.72, 95% CI: 1.16–2.56; P = 0.007) (Figure 3D).
2. c-stage: c-stage was investigated in different ways in 11 studies with conflicting conclusions (38, 39, 51–53, 55, 56, 58, 60, 64, 65) (Table 1). Two studies (53, 58) were eligible to perform meta-analysis for BM and OS. It showed that compared with ED, LD patients had less BM (HR = 0.34, 95% CI: 0.17–0.67; P = 0.002) (Figure 3E) and a better OS (HR = 0.60, 95% CI: 0.37–0.98; P = 0.04) (Figure 4A).
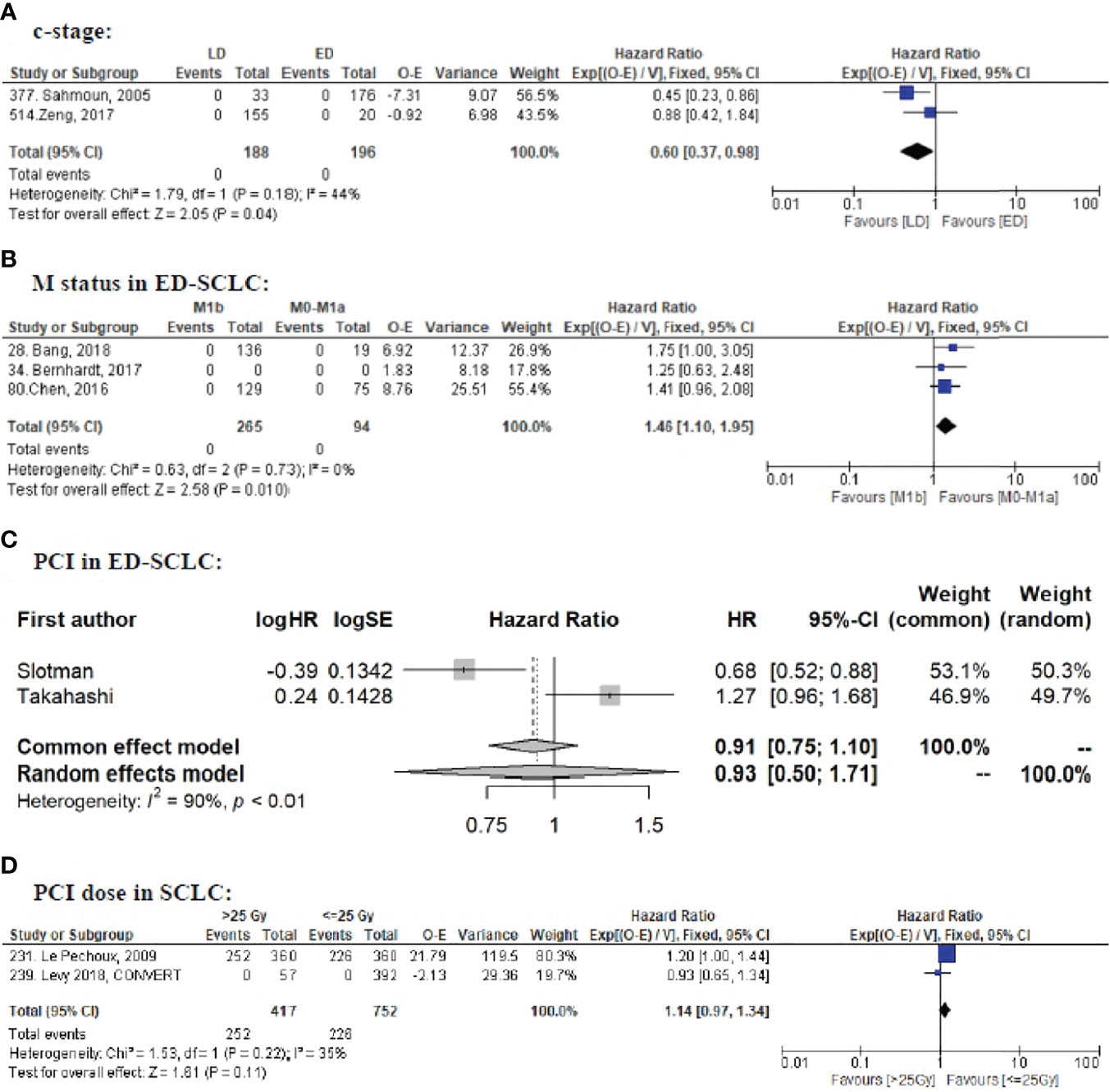
Figure 4 Forrest plots for OS: (A) c-stage; (B) M status in ED-SCLC; (C) PCI in ED-SCLC; (D) PCI dose in SCLC. OS, overall survival; LD, limited-stage disease; ED, extensive-stage disease; SCLC, small cell lung cancer; PCI, prophylactic cranial irradiation; O, observed events; E, expected events; V, variance; CI, confidence interval; HR, hazard ratio; SE, standard error.
3. M-status in ED-SCLC: M status (M1b or M0–M1a) was investigated in patients with ED-SCLC in four studies (54, 59, 61, 48). Three were eligible to perform meta-analysis for BM and OS (48, 59, 61). It showed that M1b was a significant risk factor for OS (HR = 1.46, 95% CI: 1.10–1.95; P = 0.01; Figure 4B) but not for BM (HR = 1.26, 95% CI: 0.89–1.77; P = 0.19; Figure 3F) in ED-SCLC.
4. PS: PS was investigated in 10 studies in different ways. It was concluded that PS was not a significant risk factor for BM or OS in six SCLC studies (38, 51, 52, 54, 55, 63). Two non-RCTs (51, 59) were eligible to perform meta-analysis for BM and showed that better PS (0–1) tended to be associated with less BM (HR = 0.66, 95% CI: 0.42–1.02; P = 0.06) (Figure 3G).
1. PCI vs no PCI: PCI was investigated in 28 studies, including 8 RCTs. Three RCTs had qualified overall BM data for meta-analysis based on Cox regression (29, 34, 68) and showed that PCI significantly decreases BM in SCLC (HR = 0.47, 95% CI: 0.38–0.58; P <0.00001) and LD-SCLC (HR = 0.41, 95% CI: 0.28–0.60; P <0.00001) (Figure 3H1); two had overall BM data based on competing risk regression (5, 9) and also showed that PCI significantly decreased BM in ED-SCLC (HR = 0.37, 95% CI: 0.20–0.65; P = 0.0007) (Figure 3H2); two had OS data (5, 9) and showed that PCI did not significantly improve OS in ED-SCLC (HR = 0.93, 95% CI: 0.50–1.71; P = 0.81) (Figure 4C). Two retrospective studies (72, 73) investigated PCI in LD-SCLC staged with brain MRI and reported controversial conclusions. Meta-analysis was not applicable. Two retrospective studies (74, 75) investigated PCI in resected LD-SCLC and showed that PCI improved OS and decreased BM in resected LD-SCLC but not in p-stage I. Meta-analysis was also not applicable.
2. PCI dose: PCI dose was investigated in four RCTs (27, 30, 34, 68) and three retrospective studies (42, 43, 56). Two RCTs had qualified overall BM data for meta-analysis based on Cox regression (30, 68) and showed that PCI dose (≤25 Gy vs >25 Gy) was not a significant risk factor for BM (HR = 0.59, 95% CI: 0.26–1.31; P = 0.20) (Figure 3I1); two RCTs had overall BM data based on competing risk regression (27, 30) and showed that high dose (>25 Gy) decreased BM more effectively (HR = 0.74, 95% CI: 0.55–0.99; P = 0.04) (Figure 3I2); Two had OS data (27, 30) and showed that higher dose did not significantly improve OS (HR = 1.14, 95% CI: 0.97–1.34; P = 0.11) (Figure 4D).
3. TRT dose: TRT dose (<45 Gy vs ≥45 Gy) was investigated in patients with SCLC in two studies (51, 52) and obtained different conclusions. Meta-analysis showed that high dose (≥45 Gy) was not a significant risk factor for BM (HR = 1.55, 95% CI: 0.66–3.61; P = 0.31) (Figure 3J).
The other 47 factors did not have sufficient qualified data to perform meta-analysis, such as N-stage, number of distant metastasis, and blood biomarkers. Detailed reasons are summarized in Appendix Text 1. Detailed results are provided in Appendix Text 2 along with a brief summary table (Appendix Table 7).
Data on risk factors for BM in SCLC are largely lacking, which makes personalized treatment (e.g., shared decision-making regarding PCI) difficult. It also impairs the design and interpretation of RCTs evaluating PCI. We identified several factors that were associated with a higher risk of BM: higher T-stage, ED, male sex, and younger age. As has already been reported previously (4, 82), we also found that PCI reduced BM incidence significantly, but did not improve OS in ED-SCLC. Of note, most data were derived from studies reporting only the development of symptomatic BM since brain imaging before treatment or during follow-up was rarely performed unless indicated by neurological symptoms, indicating that asymptomatic BM data have been missed; and only two RCTs were at low risk of bias. IPD meta-analysis of RCTs could help reveal more clues.
It is not surprising that ED and higher T stage, which means more advanced tumor load, were risk factors for BM. It is more interesting to note that compared to M0–M1a, M1b was a risk factor for OS but not for BM in patients with ED-SCLC. This could be explained by the aggressive nature of ED-SCLC per se, resulting in a short OS, making M-status factors less relevant than risk factors for BM development.
We also found younger age (<65) as a risk factor for BM. This is probably because younger SCLC patients generally live longer (50, 58) and therefore have more time to experience BM. Of note, the cut-off value of age varied among studies, but only those age <65 had qualified data to perform meta-analysis in our current study.
Similarly, the cut-off value of PS also varied among studies, resulting in only PS ≥2 having qualified data to perform meta-analysis based on two retrospective studies. It showed that worse PS (≥2) tended to be at a higher risk of BM. This is at odds with a secondary analysis of the CONVERT trial showing that poorer PS (1–2 vs 0) patients had a lower risk (HR: 0.54; 95% CI: 0.32–0.90; P = 0.018) of brain progression (27), likely because they die earlier before developing BM (56, 59, 61).
We also showed a marginally significant risk of developing BM in males. This is consistent with former reports illustrating that female patients had better prognosis than males, in SCLC (62), NSCLC (83), or other cancer sites (84). Reasons for this are not clear, but could include lower proliferation indexes (85), lower levels of p-glycoprotein (86, 87), more frequently expressed thyroid transcription factor-1 (TTF-1) (88), and sex hormone patterns (84).
Furthermore, we found that PCI reduced BM in SCLC but did not improve OS in ED-SCLC, which is based on the EORTC phase III trial (5) and the Japanese phase III trial (9). The conflicting results of these two trials have made PCI in ED-SCLC a reviving area of debate. Details of these two RCTs have been thoroughly discussed in other papers (8, 53, 89). Several literature-based meta-analyses reported conflicting OS results after PCI in ED-SCLC (82, 90, 91). Differences might be explained by including different studies, although all those meta-analyses included the aforementioned two RCTs. Interestingly, the meta-analysis results of two RCTs by Maeng et al. were similar to ours (HR = 0.93, 95% CI: 0.50–1.71; P = 0.81) (82). This also indicates that inclusion criteria for meta-analysis are very crucial and that pooling retrospective studies with RCTs could result in misleading conclusions because of the methodological downsides of retrospective studies.
Interestingly, we noticed that the meta-analysis results based on competing risk regression and Cox regression could be different, which indicates that data based on different statistical analysis methods should not be pooled together to perform meta-analysis. In this current study, only PCI dose (≤25 Gy vs >25 Gy) had qualified data to perform meta-analysis for both regressions. The Cox regression data showed that PCI dose was not a significant risk factor for BM (HR = 0.59, 95% CI: 0.26–1.31; P = 0.20), while the competing risk regression data showed that a higher dose (>25 Gy) could prevent BM more effectively (HR = 0.74, 95% CI: 0.55–0.99; P = 0.04). Of note, both analyses contained the same RCT conducted by Le Pechoux et al. (30), in which the results of competing risk regression (HR = 0.76, 95% CI 0.54–1.05, p = 0.10) and Cox regression (HR = 0.80; 95% CI 0.57–1.11; p = 0.18) were similar. It is unknown whether the meta-analysis results of the same trials would be different. We preferred the competing risk result because it treats death without BM as a competing event. We have not found other systematic reviews or meta-analysis answering the same question. IPD meta-analysis is needed to further clarify these data. Since higher doses of PCI did not improve OS significantly, we do not recommend increasing the PCI dose, especially because a higher PCI dose was associated with a higher risk of cognitive decline (7).
PCI best timing is also unknown. Current guidelines do not have a definite consensus on this issue (89). We identified six studies, which had investigated PCI timing (27, 48, 54, 56, 65, 69). The RCT showed that PCI timing was not a significant risk factor for BM or OS in LD-SCLC (27). Two retrospective studies showed that early PCI was more effective in reducing BM (54, 69), but three others showed the opposite (48, 56, 65). As studies investigated PCI timing in different ways, and the definitions of “early” were also different, there was no qualified data to perform meta-analysis. Therefore, it remains unclear what the best PCI timing is. More RCTs or meta-analysis of RCTs is warranted to further answer this question.
Similarly, four RCTs (31–33, 35) and three retrospective studies (52, 55, 56) have reported the impact of TRT timing on BM with different definitions of “early TRT,” which made the meta-analysis not applicable. Therefore, it is unclear whether TRT timing is a risk factor for BM. However, it has already been shown in an IPD meta-analysis that early TRT (within 30 days after the start of chemotherapy) improves OS (2-year survival: OR: 0.73, 95% CI 0.51–1.03, P = 0.07; 5-year survival: OR: 0.64, 95% CI 0.44–0.92, P = 0.02) (92). Consequently, most guidelines recommend starting TRT in the 1st or 2nd cycle of chemotherapy (89).
Risk of bias assessment is essential in systematic reviews and meta-analyses. We assessed the risk of bias for RCTs using the RoB2 tool and noticed that it has its limitations. It assesses the process of data collection and data reporting but does not assess the methods of data analysis. However, inappropriate analysis can lead to different/misleading conclusions. It also does not evaluate trials that were closed earlier, which results in much less powerful conclusions. Therefore, the improvement of the RoB2 tool is needed to assess the risk of bias more thoroughly and help improve the design of RCTs.
As for the non-RCTs, Wells et al. proposed the Newcastle–Ottawa-Scale (NOS) for assessing the quality on a website rather than in a peer-reviewed journal (93). Till now, NOS has been widely used and tends to become increasingly popular for non-RCTs in meta-analysis. However, a discussion in depth showed that the NOS has unknown validity and that using this score may produce arbitrary results (94). Lo et al. also found that the assessment between reviewers and authors of the studies was very different (95). Interestingly, many studies that used the NOS cited this critical discussion instead of the original web-based link (96–99), suggesting that researchers were using the problematic tool even though they were aware of the limitations.
The Cochrane community recommends the Risk Of Bias In Non-randomized Studies of Interventions (ROBINS-I) tool for assessing the risk of bias in non-RCTs of interventions (100). However, in our study, the baseline characteristics and tumor-related factors are not interventions, so ROBINS-I is inappropriate as well. Additionally, since most of the included RCTs were at high risk of bias and all the RCTs in which BM was the primary endpoint did not perform regular brain imaging examinations during follow-up, we decided not to perform risk of bias assessment for non-RCTs because the additional work would not add much value to the current study.
Additionally, current risk of bias assessment tools mainly assesses the risk of bias per study. This is fine for studies that mainly investigate interventions. However, as a meta-analysis aims to identify all related risk factors, it is necessary to assess the risk of bias per factor in each study. Therefore, we assessed the quality of data per factor, mainly focusing on the analysis methods in each study and summarized the possible problems in the comments. In this way, readers can clearly interpret the results.
As far as we are aware, this is the first systematic review and meta-analysis to identify risk factors for BM in SCLC. Most current meta-analyses focused on one aspect, such as PCI or not in SCLC (101), ED-SCLC (82, 90), and resected SCLC (102). Chen et al. conducted a meta-analysis to identify risk factors for BM in NSCLC (97). Unfortunately, they only searched for observational studies instead of RCTs. They used odds ratios (ORs) rather than HRs to measure the effects. Therefore, the conclusions of this study were not comparable to the current study of identifying risk factors for BM in SCLC. We suggest a well-designed study following the PRISMA guidelines and Cochrane handbook before jumping into meta-analysis by simply pooling everything together.
Additionally, we first used a simple and effective method to assess the quality of data before pooling everything together to perform the meta-analysis. That is, only studies of the same type using the same method with proper statistical analysis should be pooled together under the premise that the patients belong to the same category. This will avoid misleading conclusions based on heterogeneous data.
Furthermore, we noticed that many studies retrieved in our search (46, among which 17 were RCTs) did not report BM-related outcomes. Moreover, brain imaging is often lacking in published studies. To evaluate BM risk factors better, it is very crucial to document baseline characteristics, treatment, as well as adequate and regular brain imaging. Brain imaging should be preferred over MRI, as this is the best imaging modality to detect asymptomatic BM. Regular brain imaging is important in clinical trials, as even after a negative baseline brain MRI, in a study by Manapov et al., the second cranial MRI after completion of chemoradiotherapy revealed asymptomatic BM in 11/40 (32.5%) LD-SCLC complete responders (103). In some RCTs (9, 26, 28, 30, 33), MRI was indeed scheduled at specified time points, but it was generally unreported whether these time points were adhered to, which might influence the results. In this study, only one RCT reported the MRI compliance indirectly. Current trials on SCLC patients without BM are assessing whether MRI surveillance could be non-inferior to (hippocampal-avoidance)-PCI in terms of both OS and neurotoxicity (104, 105), in which the regular brain imaging is scheduled. We hope they will also report their compliance data.
We also noticed that many studies which reported BM data did not report OS data. This hampers the interpretation of clinical significance. For example, if a factor (A) is a risk of BM but not for OS, a factor (B) is a risk of both BM and OS, and another factor (C) is a risk of BM but unknown for OS, clinicians will put much higher weight on considering factor B and much less weight on considering C when making an individualized management strategy. Therefore, we suggest researchers report OS data as well when reporting BM data to enhance the clinical application value.
In conclusion, multiple studies evaluated risk factors for SCLC BM, but limited data were qualified to perform a meta-analysis. We found that younger age, higher T stage, and ED were risk factors for BM; suggesting that PCI should be especially discussed in such cases, shared decision making is necessary; and that higher PCI dose is not necessary. IPD meta-analysis and well-designed RCTs with high-quality data are needed to identify more risk factors such as blood biomarkers, and confirm our findings. Regular MRI with contrast-enhancement before PCI and during follow-up is helpful to detect asymptomatic BM, especially for patients with a high risk for BM. The MRI compliance at each pre-specified time point should also be reported in prospective trials. Better collaboration with statisticians is needed in future studies. We suggest emendation of the ROB2 tool to assess the statistical methods as well.
HZ, DDR, and LH conceived this study. HZ and DDR searched papers in Pubmed. HZ and DZ screening the papers from titles to full texts, extracted the data, and assessed the risk of bias. LH checked the screening, extraction and assessments. HZ, WW, and RH analyzed the results. DDR and LH supervised the whole process. HZ, LH, and DDR draft the manuscript. AL, AT, WW, RH, FMK, and DZ made the revisions. All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
This research was supported by the following grant: Scholarship of China Scholarship Council (Grant No.: CSC 201909370087).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We sincerely thank Dr. Yawen Zheng from Department of Radiation Oncology, Jinan Central Hospital, Shandong University, Jinan, China; Dr. Lei Fu from Department of Radiation Oncology, Shandong Cancer Hospital and Institute, Shandong First Medical University (Shandong Academy of Medical Sciences), Jinan, China; Prof. Patricia Tai from Department of Radiation Oncology, Allan Blair Cancer Center, Regina, Canada for their responses to inquiries about the studies. We sincerely thank Fariba Tohidinezhad from Department of Radiation Oncology (Maastro), GROW School for Oncology, Maastricht University Medical Center+, Maastricht, the Netherlands for her help.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2022.889161/full#supplementary-material
1. van Meerbeeck JP, Fennell DA, De Ruysscher DK. Small-Cell Lung Cancer. Lancet (2011) 378:1741–55. doi: 10.1016/s0140-6736(11)60165-7
2. Manapov F, Käsmann L, Roengvoraphoj O, Dantes M, Schmidt-Hegemann NS, Belka C, et al. Prophylactic Cranial Irradiation in Small-Cell Lung Cancer: Update on Patient Selection, Efficacy and Outcomes. Lung Cancer (Auckl) (2018) 9:49–55. doi: 10.2147/lctt.S137577
3. Hall WA, Djalilian HR, Nussbaum ES, Cho KH. Long-Term Survival With Metastatic Cancer to the Brain. Med Oncol (2000) 17:279–86. doi: 10.1007/bf02782192
4. Aupérin A, Arriagada R, Pignon JP, Le Péchoux C, Gregor A, Stephens RJ, et al. Prophylactic Cranial Irradiation for Patients With Small-Cell Lung Cancer in Complete Remission. Prophylactic Cranial Irradiation Overview Collaborative Group. N Engl J Med (1999) 341:476–84. doi: 10.1056/nejm199908123410703
5. Slotman B, Faivre-Finn C, Kramer G, Rankin E, Snee M, Hatton M, et al. Prophylactic Cranial Irradiation in Extensive Small-Cell Lung Cancer. N Engl J Med (2007) 357:664–72. doi: 10.1056/NEJMoa071780
6. Péchoux CL, Sun A, Slotman BJ, De Ruysscher D, Belderbos J, Gore EM. Prophylactic Cranial Irradiation for Patients With Lung Cancer. Lancet Oncol (2016) 17:e277–93. doi: 10.1016/s1470-2045(16)30065-1
7. Zeng H, Hendriks LEL, van Geffen WH, Witlox WJA, Eekers DBP, De Ruysscher DKM. Risk Factors for Neurocognitive Decline in Lung Cancer Patients Treated With Prophylactic Cranial Irradiation: A Systematic Review. Cancer Treat Rev (2020) 88:102025. doi: 10.1016/j.ctrv.2020.102025
8. Crockett C, Belderbos J, Levy A, McDonald F, Le Péchoux C, Faivre-Finn C. Prophylactic Cranial Irradiation (PCI), Hippocampal Avoidance (HA) Whole Brain Radiotherapy (WBRT) and Stereotactic Radiosurgery (SRS) in Small Cell Lung Cancer (SCLC): Where Do We Stand? Lung Cancer (2021) 162:96–105. doi: 10.1016/j.lungcan.2021.10.016
9. Takahashi T, Yamanaka T, Seto T, Harada H, Nokihara H, Saka H, et al. Prophylactic Cranial Irradiation Versus Observation in Patients With Extensive-Disease Small-Cell Lung Cancer: A Multicentre, Randomised, Open-Label, Phase 3 Trial. Lancet Oncol (2017) 18:663–71. doi: 10.1016/s1470-2045(17)30230-9
10. Rusthoven CG, Yamamoto M, Bernhardt D, Smith DE, Gao D, Serizawa T, et al. Evaluation of First-Line Radiosurgery vs Whole-Brain Radiotherapy for Small Cell Lung Cancer Brain Metastases: The FIRE-SCLC Cohort Study. JAMA Oncol (2020) 6:1028–37. doi: 10.1001/jamaoncol.2020.1271
11. Dingemans AC, Früh M, Ardizzoni A, Besse B, Faivre-Finn C, Hendriks LE, et al. Small-Cell Lung Cancer: ESMO Clinical Practice Guidelines for Diagnosis, Treatment and Follow-Up(☆). Ann Oncol (2021) 32:839–53. doi: 10.1016/j.annonc.2021.03.207
12. Simone CB 2nd, Bogart JA, Cabrera AR, Daly ME, DeNunzio NJ, Detterbeck F, et al. Radiation Therapy for Small Cell Lung Cancer: An ASTRO Clinical Practice Guideline. Pract Radiat Oncol (2020) 10:158–73. doi: 10.1016/j.prro.2020.02.009
13. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PloS Med (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097
14. Zeng H, Zheng D, Hendriks L, Kong F-MS, De Ruysscher D. Risk Factors for Brain Metastasis in Patients With Small Cell Lung Cancer: A Systematic Review With Meta-Analysis. PROSPERO (2021) CRD42021228391. Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021228391
15. da Costa Santos CM, de Mattos Pimenta CA, Nobre MR. The PICO Strategy for the Research Question Construction and Evidence Search. Rev Lat Am Enfermagem (2007) 15:508–11. doi: 10.1590/s0104-11692007000300023
16. Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane Handbook for Systematic Reviews of Interventions Version 6.1. Cochrane (2020).
17. Sterne JAC, Savovic J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: A Revised Tool for Assessing Risk of Bias in Randomised Trials. BMJ (2019) 366:l4898. doi: 10.1136/bmj.l4898
18. Web Plot Digitizer. Web Plot Digitizer. Available from: https://automeris.io/WebPlotDigitizer
19. Higginst J, Li T, Deeks J. Chapter 6: Choosing Effect Measures and Computing Estimates of Effect. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (Updated February 2021) (2021).
20. Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical Methods for Incorporating Summary Time-to-Event Data Into Meta-Analysis. Trials (2007) 8:16. doi: 10.1186/1745-6215-8-16
21. Reeves BC, Deeks JJ, Higgins JPT, Shea B, Tugwell P, GA. W. Chapter 24: Including Non-Randomized Studies on Intervention Effects. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (Updated February 2021). Cochrane (2021). Available at: www.training.cochrane.org/handbook.
22. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring Inconsistency in Meta-Analyses. BMJ (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
23. Li Z, Liu Y, Wang J, Zhang C, Liu Y. Effectiveness of Cognitive Behavioural Therapy for Perinatal Depression: A Systematic Review and Meta-Analysis. J Clin Nurs (2020) 29:3170–82. doi: 10.1111/jocn.15378
24. Zhang X, Zhu Z, Jiao W, Liu W, Liu F, Zhu X. Ulinastatin Treatment for Acute Respiratory Distress Syndrome in China: A Meta-Analysis of Randomized Controlled Trials. BMC Pulm Med (2019) 19:196. doi: 10.1186/s12890-019-0968-6
25. Slotman BJ, van Tinteren H, Praag JO, Knegjens JL, El Sharouni SY, Hatton M, et al. Use of Thoracic Radiotherapy for Extensive Stage Small-Cell Lung Cancer: A Phase 3 Randomised Controlled Trial. Lancet (2015) 385:36–42. doi: 10.1016/s0140-6736(14)61085-0
26. Gore EM, Hu C, Sun AY, Grimm DF, Ramalingam SS, Dunlap NE, et al. Randomized Phase II Study Comparing Prophylactic Cranial Irradiation Alone to Prophylactic Cranial Irradiation and Consolidative Extracranial Irradiation for Extensive-Disease Small Cell Lung Cancer (ED SCLC): NRG Oncology RTOG 0937. J Thorac Oncol (2017) 12:1561–70. doi: 10.1016/j.jtho.2017.06.015
27. Levy A, Le Péchoux C, Mistry H, Martel-Lafay I, Bezjak A, Lerouge D, et al. Prophylactic Cranial Irradiation for Limited-Stage Small-Cell Lung Cancer Patients: Secondary Findings From the Prospective Randomized Phase 3 CONVERT Trial. J Thorac Oncol (2019) 14:294–7. doi: 10.1016/j.jtho.2018.09.019
28. Arriagada R, Le Chevalier T, Borie F, Riviére A, Chomy P, Monnet I, et al. Prophylactic Cranial Irradiation for Patients With Small-Cell Lung Cancer in Complete Remission. J Natl Cancer Inst (1995) 87:183–90. doi: 10.1093/jnci/87.3.183
29. Arriagada R, Le Chevalier T, Rivière A, Chomy P, Monnet I, Bardet E, et al. Patterns of Failure After Prophylactic Cranial Irradiation in Small-Cell Lung Cancer: Analysis of 505 Randomized Patients. Ann Oncol (2002) 13:748–54. doi: 10.1093/annonc/mdf123
30. Le Péchoux C, Dunant A, Senan S, Wolfson A, Quoix E, Faivre-Finn C, et al. Standard-Dose Versus Higher-Dose Prophylactic Cranial Irradiation (PCI) in Patients With Limited-Stage Small-Cell Lung Cancer in Complete Remission After Chemotherapy and Thoracic Radiotherapy (PCI 99-01, EORTC 22003-08004, RTOG 0212, and IFCT 99-01): A Randomised Clinical Trial. Lancet Oncol (2009) 10:467–74. doi: 10.1016/s1470-2045(09)70101-9
31. Jeremic B, Shibamoto Y, Acimovic L, Milisavljevic S. Initial Versus Delayed Accelerated Hyperfractionated Radiation Therapy and Concurrent Chemotherapy in Limited Small-Cell Lung Cancer: A Randomized Study. J Clin Oncol (1997) 15:893–900. doi: 10.1200/jco.1997.15.3.893
32. Spiro SG, James LE, Rudd RM, Trask CW, Tobias JS, Snee M, et al. Early Compared With Late Radiotherapy in Combined Modality Treatment for Limited Disease Small-Cell Lung Cancer: A London Lung Cancer Group Multicenter Randomized Clinical Trial and Meta-Analysis. J Clin Oncol (2006) 24:3823–30. doi: 10.1200/jco.2005.05.3181
33. Skarlos DV, Samantas E, Briassoulis E, Panoussaki E, Pavlidis N, Kalofonos HP, et al. Randomized Comparison of Early Versus Late Hyperfractionated Thoracic Irradiation Concurrently With Chemotherapy in Limited Disease Small-Cell Lung Cancer: A Randomized Phase II Study of the Hellenic Cooperative Oncology Group (HeCOG). Ann Oncol (2001) 12:1231–8. doi: 10.1023/a:1012295131640
34. Work E, Bentzen SM, Nielsen OS, Fode K, Michalski W, Palshof T. Prophylactic Cranial Irradiation in Limited Stage Small Cell Lung Cancer: Survival Benefit in Patients With Favourable Characteristics. Eur J Cancer (1996) 32a:772–8. doi: 10.1016/0959-8049(95)00597-8
35. Work E, Nielsen OS, Bentzen SM, Bentzen SM, Fode K, Palshof T. Randomized Study of Initial Versus Late Chest Irradiation Combined With Chemotherapy in Limited-Stage Small-Cell Lung Cancer. Aarhus Lung Cancer Group. J Clin Oncol (1997) 15:3030–7. doi: 10.1200/jco.1997.15.9.3030
36. Chu X, Li S, Xia B, Chu L, Yang X, Ni J, et al. Patterns of Brain Metastasis Immediately Before Prophylactic Cranial Irradiation (PCI): Implications for PCI Optimization in Limited-Stage Small Cell Lung Cancer. Radiat Oncol (2019) 14:171. doi: 10.1186/s13014-019-1371-4
37. Choi M, Lee Y, Moon SH, Han JY, Kim HT, Lee JS. Effect of Accurate Staging Using Positron Emission Tomography on the Outcomes of Prophylactic Cranial Irradiation in Patients With Limited Stage Small-Cell Lung Cancer. Clin Lung Cancer (2017) 18:77–84. doi: 10.1016/j.cllc.2016.06.012
38. Fu L, Liu F, Fu H, Liu L, Yuan S, Gao Y, et al. Circulating Tumor Cells Correlate With Recurrence in Stage III Small-Cell Lung Cancer After Systemic Chemoradiotherapy and Prophylactic Cranial Irradiation. Jpn J Clin Oncol (2014) 44:948–55. doi: 10.1093/jjco/hyu109
39. Nakamura M, Onozawa M, Motegi A, Hojo H, Zenda S, Nakamura N, et al. Impact of Prophylactic Cranial Irradiation on Pattern of Brain Metastases as a First Recurrence Site for Limited-Disease Small-Cell Lung Cancer. J Radiat Res (2018) 59:767–73. doi: 10.1093/jrr/rry066
40. Gregor A, Drings P, Burghouts J, Postmus PE, Morgan D, Sahmoud T, et al. Randomized Trial of Alternating Versus Sequential Radiotherapy/Chemotherapy in Limited-Disease Patients With Small-Cell Lung Cancer: A European Organization for Research and Treatment of Cancer Lung Cancer Cooperative Group Study. J Clin Oncol (1997) 15:2840–9. doi: 10.1200/jco.1997.15.8.2840
41. Takada M, Fukuoka M, Kawahara M, Sugiura T, Yokoyama A, Yokota S, et al. Phase III Study of Concurrent Versus Sequential Thoracic Radiotherapy in Combination With Cisplatin and Etoposide for Limited-Stage Small-Cell Lung Cancer: Results of the Japan Clinical Oncology Group Study 9104. J Clin Oncol (2002) 20:3054–60. doi: 10.1200/jco.2002.12.071
42. Brewster AE, Hopwood P, Stout R, Stout R, Burt PA, Thatcher N, et al. Single Fraction Prophylactic Cranial Irradiation for Small Cell Carcinoma of the Lung. Radiother Oncol (1995) 34:132–6. doi: 10.1016/0167-8140(95)01513-g
43. Rubenstein JH, Dosoretz DE, Katin MJ, Blitzer PH, Salenius SA, Floody PA, et al. Low Doses of Prophylactic Cranial Irradiation Effective in Limited Stage Small Cell Carcinoma of the Lung. Int J Radiat Oncol Biol Phys (1995) 33:329–37. doi: 10.1016/0360-3016(95)00166-v
44. Scotti V, Meattini I, Franzese C, Saieva C, Bertocci S, Meacci F, et al. Radiotherapy Timing in the Treatment of Limited-Stage Small Cell Lung Cancer: The Impact of Thoracic and Brain Irradiation on Survival. Tumori (2014) 100:289–95. doi: 10.1700/1578.17206
45. van der Linden YM, van Kempen ML, van der Tweel I, Vanderschueren RG, Schl�sser NJ, Lammers JW, et al. Prophylactic Cranial Irradiation in Limited Disease Small-Cell Lung Cancer in Complete Remission: A Retrospective Analysis. Respir Med (2001) 95:235–6. doi: 10.1053/rmed.2000.1022
46. Laplanche A, Monnet I, Santos-Miranda JA, Bardet E, Le Péchoux C, Tarayre M, et al. Controlled Clinical Trial of Prophylactic Cranial Irradiation for Patients With Small-Cell Lung Cancer in Complete Remission. Lung Cancer (1998) 21:193–201. doi: 10.1016/s0169-5002(98)00056-7
47. Farooqi AS, Holliday EB, Allen PK, Wei X, Cox JD, Komaki R. Prophylactic Cranial Irradiation After Definitive Chemoradiotherapy for Limited-Stage Small Cell Lung Cancer: Do All Patients Benefit? Radiother Oncol (2017) 122:307–12. doi: 10.1016/j.radonc.2016.11.012
48. Bernhardt D, Adeberg S, Bozorgmehr F, Opfermann N, Hoerner-Rieber J, Repka MC, et al. Nine-Year Experience: Prophylactic Cranial Irradiation in Extensive Disease Small-Cell Lung Cancer. Clin Lung Cancer (2017) 18:e267–71. doi: 10.1016/j.cllc.2016.11.012
49. Sahmoun AE, Case LD, Chavour S, Kareem S, Schwartz GG. Hypertension and Risk of Brain Metastasis From Small Cell Lung Cancer: A Retrospective Follow-Up Study. Anticancer Res (2004) 24:3115–20.
50. Zhu H, Bi Y, Han A, Luo J, Li M, Shi F, et al. Risk Factors for Brain Metastases in Completely Resected Small Cell Lung Cancer: A Retrospective Study to Identify Patients Most Likely to Benefit From Prophylactic Cranial Irradiation. Radiat Oncol (2014) 9:216. doi: 10.1186/1748-717x-9-216
51. Suzuki R, Wei X, Allen PK, Welsh JW, Komaki R, Lin SH. Hematologic Variables Associated With Brain Failure in Patients With Small-Cell Lung Cancer. Radiother Oncol (2018) 128:505–12. doi: 10.1016/j.radonc.2018.05.026
52. Kim TG, Pyo H, Ahn YC, Noh JM, Oh D. Role of Prophylactic Cranial Irradiation for Elderly Patients With Limited-Disease Small-Cell Lung Cancer: Inverse Probability of Treatment Weighting Using Propensity Score. J Radiat Res (2019) 60:630–8. doi: 10.1093/jrr/rrz040
53. Zeng H, Xie P, Meng X, Yuan S, Sun X, Li W, et al. Risk Factors for Brain Metastases After Prophylactic Cranial Irradiation in Small Cell Lung Cancer. Sci Rep (2017) 7:42743. doi: 10.1038/srep42743
54. Chen Y, Li J, Zhang Y, Hu Y, Zhang G, Yan X, et al. Early Versus Late Prophylactic Cranial Irradiation in Patients With Extensive Small Cell Lung Cancer. Strahlenther Onkol (2018) 194:876–85. doi: 10.1007/s00066-018-1307-1
55. Zheng Y, Wang L, Zhao W, Dou Y, Lv W, Yang H, et al. Risk Factors for Brain Metastasis in Patients With Small Cell Lung Cancer Without Prophylactic Cranial Irradiation. Strahlenther Onkol (2018) 194:1152–62. doi: 10.1007/s00066-018-1362-7
56. Zeng H, Li R, Hu C, Qiu G, Ge H, Yu H, et al. Association of Twice-Daily Radiotherapy With Subsequent Brain Metastases in Adults With Small Cell Lung Cancer. JAMA Netw Open (2019) 2:e190103. doi: 10.1001/jamanetworkopen.2019.0103
57. Gong L, Wang QI, Zhao L, Yuan Z, Li R, Wang P. Factors Affecting the Risk of Brain Metastasis in Small Cell Lung Cancer With Surgery: Is Prophylactic Cranial Irradiation Necessary for Stage I-III Disease? Int J Radiat Oncol Biol Phys (2013) 85:196–200. doi: 10.1016/j.ijrobp.2012.03.038
58. Sahmoun AE, Case LD, Santoro TJ, Schwartz GG. Anatomical Distribution of Small Cell Lung Cancer: Effects of Lobe and Gender on Brain Metastasis and Survival. Anticancer Res (2005) 25:1101–8.
59. Chen Y, Li J, Hu Y, Zhang Y, Lin Z, Zhao Z, et al. Prophylactic Cranial Irradiation Could Improve Overall Survival in Patients With Extensive Small Cell Lung Cancer : A Retrospective Study. Strahlenther Onkol (2016) 192:905–12. doi: 10.1007/s00066-016-1038-0
60. Wu AJ, Gillis A, Foster A, Woo K, Zhang Z, Gelblum DY3, et al. Patterns of Failure in Limited-Stage Small Cell Lung Cancer: Implications of TNM Stage for Prophylactic Cranial Irradiation. Radiother Oncol (2017) 125:130–5. doi: 10.1016/j.radonc.2017.07.019
61. Bang A, Kendal WS, Laurie SA, Cook G, MacRae RM. Prophylactic Cranial Irradiation in Extensive Stage Small Cell Lung Cancer: Outcomes at a Comprehensive Cancer Centre. Int J Radiat Oncol Biol Phys (2018) 101:1133–40. doi: 10.1016/j.ijrobp.2018.04.058
62. Roengvoraphoj O, Eze C, Niyazi M, Li M, Hildebrandt G, Fietkau R, et al. Prognostic Role of Patient Gender in Limited-Disease Small-Cell Lung Cancer Treated With Chemoradiotherapy. Strahlenther Onkol (2017) 193:150–5. doi: 10.1007/s00066-016-1073-x
63. Greenspoon JN, Evans WK, Cai W, Wright JR. Selecting Patients With Extensive-Stage Small Cell Lung Cancer for Prophylactic Cranial Irradiation by Predicting Brain Metastases. J Thorac Oncol (2011) 6:808–12. doi: 10.1097/JTO.0b013e31820d782d
64. Seute T, Leffers P, ten Velde GP, Twijnstra A. Neurologic Disorders in 432 Consecutive Patients With Small Cell Lung Carcinoma. Cancer (2004) 100:801–6. doi: 10.1002/cncr.20043
65. Ramlov A, Tietze A, Khalil AA, Knap MM. Prophylactic Cranial Irradiation in Patients With Small Cell Lung Cancer. A Retrospective Study of Recurrence, Survival and Morbidity. Lung Cancer (2012) 77:561–6. doi: 10.1016/j.lungcan.2012.05.101
66. Manapov F, Klöcking S, Niyazi M, Levitskiy V, Belka C, Hildebrandt G, et al. Primary Tumor Response to Chemoradiotherapy in Limited-Disease Small-Cell Lung Cancer Correlates With Duration of Brain-Metastasis Free Survival. J Neurooncol (2012) 109:309–14. doi: 10.1007/s11060-012-0894-4
67. Cao KJ, Huang HY, Tu MC, Pan GY. Long-Term Results of Prophylactic Cranial Irradiation for Limited-Stage Small-Cell Lung Cancer in Complete Remission. Chin Med J (Engl) (2005) 118:1258–62.
68. Gregor A, Cull A, Stephens RJ, Kirkpatrick JA, Yarnold JR, Girling DJ, et al. Prophylactic Cranial Irradiation is Indicated Following Complete Response to Induction Therapy in Small Cell Lung Cancer: Results of a Multicentre Randomised Trial. United Kingdom Coordinating Committee for Cancer Research (UKCCCR) and the European Organization for Research and Treatment of Cancer (EORTC). Eur J Cancer (1997) 33:1752–8. doi: 10.1016/s0959-8049(97)00135-4
69. Sas-Korczyńska B, Korzeniowski S, Wójcik E. Comparison of the Effectiveness of "Late" and "Early" Prophylactic Cranial Irradiation in Patients With Limited-Stage Small Cell Lung Cancer. Strahlenther Onkol (2010) 186:315–9. doi: 10.1007/s00066-010-2088-3
70. Giuliani M, Sun A, Bezjak A, Ma C, Le LW, Brade A, et al. Utilization of Prophylactic Cranial Irradiation in Patients With Limited Stage Small Cell Lung Carcinoma. Cancer (2010) 116:5694–9. doi: 10.1002/cncr.25341
71. Tai P, Assouline A, Joseph K, Stitt L, Yu E. Prophylactic Cranial Irradiation for Patients With Limited-Stage Small-Cell Lung Cancer With Response to Chemoradiation. Clin Lung Cancer (2013) 14:40–4. doi: 10.1016/j.cllc.2012.04.005
72. Eze C, Roengvoraphoj O, Niyazi M, Hildebrandt G, Fietkau R, Belka C, et al. Treatment Response and Prophylactic Cranial Irradiation Are Prognostic Factors in a Real-Life Limited-Disease Small-Cell Lung Cancer Patient Cohort Comprehensively Staged With Cranial Magnetic Resonance Imaging. Clin Lung Cancer (2017) 18:e243–9. doi: 10.1016/j.cllc.2016.11.005
73. Pezzi TA, Fang P, Gjyshi O, Feng L, Liu S, Komaki R, et al. Rates of Overall Survival and Intracranial Control in the Magnetic Resonance Imaging Era for Patients With Limited-Stage Small Cell Lung Cancer With and Without Prophylactic Cranial Irradiation. JAMA Netw Open (2020) 3:e201929. doi: 10.1001/jamanetworkopen.2020.1929
74. Zhu H, Guo H, Shi F, Zhu K, Luo J, Liu X, et al. Prophylactic Cranial Irradiation Improved the Overall Survival of Patients With Surgically Resected Small Cell Lung Cancer, But Not for Stage I Disease. Lung Cancer (2014) 86:334–8. doi: 10.1016/j.lungcan.2014.09.019
75. Xu J, Yang H, Fu X, Jin B, Lou Y, Zhang Y, et al. Prophylactic Cranial Irradiation for Patients With Surgically Resected Small Cell Lung Cancer. J Thorac Oncol (2017) 12:347–53. doi: 10.1016/j.jtho.2016.09.133
76. Nicholls L, Keir GJ, Murphy MA, Mai T, Lehman M. Prophylactic Cranial Irradiation in Small Cell Lung Cancer: A Single Institution Experience. Asia Pac J Clin Oncol (2016) 12:415–20. doi: 10.1111/ajco.12564
77. El Sharouni SY, Kal HB, Barten-Van Rijbroek A, Struikmans H, Battermann JJ, Schramel FM. Concurrent Versus Sequential Chemotherapy and Radiotherapy in Limited Disease Small Cell Lung Cancer: A Retrospective Comparative Study. Anticancer Res (2009) 29:5219–24.
78. Manapov F, Klöcking S, Niyazi M, Oskan F, Niemöller OM, Belka C, et al. Timing of Failure in Limited Disease (Stage I-III) Small-Cell Lung Cancer Patients Treated With Chemoradiotherapy: A Retrospective Analysis. Tumori (2013) 99:656–60. doi: 10.1700/1390.15452
79. Schiller JH, Adak S, Cella D, DeVore RF 3rd, Johnson DH. Topotecan Versus Observation After Cisplatin Plus Etoposide in Extensive-Stage Small-Cell Lung Cancer: E7593–a Phase III Trial of the Eastern Cooperative Oncology Group. J Clin Oncol (2001) 19:2114–22. doi: 10.1200/jco.2001.19.8.2114
80. Sundstrøm S, Bremnes RM, Kaasa S, Aasebø U, Hatlevoll R, Dahle R, et al. Cisplatin and Etoposide Regimen is Superior to Cyclophosphamide, Epirubicin, and Vincristine Regimen in Small-Cell Lung Cancer: Results From a Randomized Phase III Trial With 5 Years' Follow-Up. J Clin Oncol (2002) 20:4665–72. doi: 10.1200/jco.2002.12.111
81. Manapov F, Klöcking S, Niyazi M, Belka C, Hildebrandt G, Fietkau R, et al. Chemoradiotherapy Duration Correlates With Overall Survival in Limited Disease SCLC Patients With Poor Initial Performance Status Who Successfully Completed Multimodality Treatment. Strahlenther Onkol (2012) 188:29–34. doi: 10.1007/s00066-011-0016-9
82. Maeng CH, Song JU, Shim SR, Lee J. The Role of Prophylactic Cranial Irradiation in Patients With Extensive Stage Small Cell Lung Cancer: A Systematic Review and Meta-Analysis. J Thorac Oncol (2018) 13:840–8. doi: 10.1016/j.jtho.2018.02.024
83. Svensson G, Ewers S, Ohlsson O, Olsson H. Gender-Related Survival in Different Stages of Lung Cancer – a Population Study Over 20 Years. Open J Intern Med (2014) 04:47–58. doi: 10.4236/ojim.2014.43008
84. Micheli A, Ciampichini R, Oberaigner W, Ciccolallo L, de Vries E, Izarzugaza I, et al. The Advantage of Women in Cancer Survival: An Analysis of EUROCARE-4 Data. Eur J Cancer (2009) 45:1017–27. doi: 10.1016/j.ejca.2008.11.008
85. Sterlacci W, Tzankov A, Veits L, Oberaigner W, Schmid T, Hilbe W, et al. The Prognostic Impact of Sex on Surgically Resected non-Small Cell Lung Cancer Depends on Clinicopathologic Characteristics. Am J Clin Pathol (2011) 135:611–8. doi: 10.1309/ajcpqf24nywnmvmg
86. Singh S, Parulekar W, Murray N, Feld R, Evans WK, Tu D, et al. Influence of Sex on Toxicity and Treatment Outcome in Small-Cell Lung Cancer. J Clin Oncol (2005) 23:850–6. doi: 10.1200/jco.2005.03.171
87. Davis M. Gender Differences in P-Glycoprotein: Drug Toxicity and Response. J Clin Oncol (2005) 23:6439–40. doi: 10.1200/jco.2005.01.9232
88. Anagnostou VK, Syrigos KN, Bepler G, Homer RJ, Rimm DL. Thyroid Transcription Factor 1 is an Independent Prognostic Factor for Patients With Stage I Lung Adenocarcinoma. J Clin Oncol (2009) 27:271–8. doi: 10.1200/jco.2008.17.0043
89. Zeng H, De Ruysscher DKM, Hu X, Zheng D, Yang L, Ricardi U, et al. Radiotherapy for Small Cell Lung Cancer in Current Clinical Practice Guidelines. J Natl Cancer Center (2022). doi: 10.1016/j.jncc.2022.02.003
90. Ge W, Xu H, Yan Y, Cao D. The Effects of Prophylactic Cranial Irradiation Versus Control on Survival of Patients With Extensive-Stage Small-Cell Lung Cancer: A Meta-Analysis of 14 Trials. Radiat Oncol (2018) 13:155. doi: 10.1186/s13014-018-1101-3
91. Wen P, Wang TF, Li M, Yu Y, Zhou YL, Wu CL. Meta-Analysis of Prophylactic Cranial Irradiation or Not in Treatment of Extensive-Stage Small-Cell Lung Cancer: The Dilemma Remains. Cancer Radiother (2020) 24:44–52. doi: 10.1016/j.canrad.2019.10.001
92. De Ruysscher D, Pijls-Johannesma M, Vansteenkiste J, Kester A, Rutten I, Lambin P. Systematic Review and Meta-Analysis of Randomised, Controlled Trials of the Timing of Chest Radiotherapy in Patients With Limited-Stage, Small-Cell Lung Cancer. Ann Oncol (2006) 17:543–52. doi: 10.1093/annonc/mdj094
93. Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomized Studies in Meta-Analyses. (2022).
94. Stang A. Critical Evaluation of the Newcastle-Ottawa Scale for the Assessment of the Quality of Nonrandomized Studies in Meta-Analyses. Eur J Epidemiol (2010) 25:603–5. doi: 10.1007/s10654-010-9491-z
95. Lo CK, Mertz D, Loeb M. Newcastle-Ottawa Scale: Comparing Reviewers' to Authors' Assessments. BMC Med Res Methodol (2014) 14:45. doi: 10.1186/1471-2288-14-45
96. Wang Y, Li J, Chang S, Dong Y, Che G. Risk and Influencing Factors for Subsequent Primary Lung Cancer After Treatment of Breast Cancer: A Systematic Review and Two Meta-Analyses Based on Four Million Cases. J Thorac Oncol (2021) 16:1893–908. doi: 10.1016/j.jtho.2021.07.001
97. Chen S, Hua X, Jia J, Wu Y, Wei S, Xu L, et al. Risk Factors for Brain Metastases in Patients With non-Small Cell Lung Cancer: A Meta-Analysis of 43 Studies. Ann Palliat Med (2021) 10:3657–72. doi: 10.21037/apm-20-1722
98. Wang N, Tang C, Wang L. Risk Factors for Acquired Stenotrophomonas Maltophilia Pneumonia in Intensive Care Unit: A Systematic Review and Meta-Analysis. Front Med (Lausanne) (2021) 8:808391. doi: 10.3389/fmed.2021.808391
99. Aydh A, Motlagh RS, Alshyarba M, Mori K, Katayama S, Grossmann N, et al. Association of Statins Use and Mortality Outcomes in Prostate Cancer Patients Who Received Androgen Deprivation Therapy: A Systematic Review and Meta-Analysis. Cent Eur J Urol (2021) 74:484–90. doi: 10.5173/ceju.2021.0260
100. Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: A Tool for Assessing Risk of Bias in non-Randomised Studies of Interventions. Bmj (2016) 355:i4919. doi: 10.1136/bmj.i4919
101. Yin X, Yan D, Qiu M, Huang L, Yan SX. Prophylactic Cranial Irradiation in Small Cell Lung Cancer: A Systematic Review and Meta-Analysis. BMC Cancer (2019) 19:95. doi: 10.1186/s12885-018-5251-3
102. Yang Y, Zhang D, Zhou X, Bao W, Ji Y, Sheng L, et al. Prophylactic Cranial Irradiation in Resected Small Cell Lung Cancer: A Systematic Review With Meta-Analysis. J Cancer (2018) 9:433–9. doi: 10.7150/jca.21465
103. Manapov F, Klautke G, Fietkau R. Prevalence of Brain Metastases Immediately Before Prophylactic Cranial Irradiation in Limited Disease Small Cell Lung Cancer Patients With Complete Remission to Chemoradiotherapy: A Single Institution Experience. J Thorac Oncol (2008) 3:652–5. doi: 10.1097/JTO.0b013e3181757a76
104. SWOG S1827 (MAVERICK) Testing Whether the Use of Brain Scans Alone Instead of Brain Scans Plus Preventive Brain Radiation Affects Lifespan in Patients With Small Cell Lung Cancer. (2022).
Keywords: small cell lung cancer, brain metastasis, risk factors, systematic review, meta-analysis
Citation: Zeng H, Zheng D, Witlox WJA, Levy A, Traverso A, Kong F-M(S), Houben R, De Ruysscher DKM and Hendriks LEL (2022) Risk Factors for Brain Metastases in Patients With Small Cell Lung Cancer: A Systematic Review and Meta-Analysis. Front. Oncol. 12:889161. doi: 10.3389/fonc.2022.889161
Received: 03 March 2022; Accepted: 25 April 2022;
Published: 10 June 2022.
Edited by:
Paul Jules Van Houtte, Jules Bordet Institute, BelgiumReviewed by:
Farkhad Manapov, LMU Munich University Hospital, GermanyCopyright © 2022 Zeng, Zheng, Witlox, Levy, Traverso, Kong, Houben, De Ruysscher and Hendriks. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Haiyan Zeng, aGFpeWFuLnplbmdAbWFhc3Ryby5ubA==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.