
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Oncol. , 31 May 2022
Sec. Thoracic Oncology
Volume 12 - 2022 | https://doi.org/10.3389/fonc.2022.855305
This article is part of the Research Topic Epidemiology, Screening and Diagnosis of Lung Cancer View all 24 articles
Background: Familial lung cancer (FLC) accounts for 8% of lung adenocarcinoma. It is known that a few germline mutations are associated with risk increasing and may provide new screening and treatment option. The goal of this study is to identify an FLC gene among three members of an FLC family.
Methods: To uncover somatic and embryonic mutations linked with familial lung cancer, whole exome sequencing was done on surgical tissues and peripheral blood from three sisters in a family diagnosed with pulmonary lung adenocarcinoma (LUAD). At the same time, single-cell RNA sequencing (scRNA-seq) and bulk RNA sequencing data in public databases were enrolled to identify specific gene expression level.
Results: Ataxia Telangiectasia and Rad3-Related Protein (ATR) gene C.7667C >G (p.T2556S) mutation were found in 3 patients with familial lung cancer. Whole-genome sequencing revealed that the three sisters exhibited similar somatic mutation patterns. Besides ATR mutations, common mutated genes (BRCA1, EGFR, and ROS1) that characterize LUAD were also found in 5 tumor samples. Analysis for the ATR expression in LUAD patients by single-cell sequencing data, we found ATR expression of tumor patients at high level in immune cells when compared with normal patients, but the expression of ATR in stromal cells has the opposite result.
Conclusion: We found a germline mutation in the ATR gene in three sisters of a Chinese family affected by familial lung cancer, which may be a genetic factor for lung cancer susceptibility.
Lung adenocarcinoma is the primary cause of cancer-related death worldwide, with an estimated 1.8 million fatalities each year (1). Researchers are still considering possible links involving lung cancer risk. Although smoking is still the leading cause of lung cancer, accounting for 80 to 90 percent of all cases, genetic susceptibility may play a role in lung cancer in some situations (2). Previous studies have demonstrated that genetic susceptibility was thought to be closely related to the development of familial lung cancer (3, 4). However, the risk factors for hereditary lung cancer are unknown at this time. Several research has looked into the function of germline mutations, primarily selected somatic mutations, in lung cancer susceptibility (5–7).
Ataxia Telangiectasia and Rad3 related (ATR) kinase plays a crucial role in the repair of replication-associated DNA damage (8). The study of cell cycle checkpoint signaling through ATR, as well as the related pathways implicated in oncogenesis and cancer progression, has resulted in the discovery and development of effective and selective ATR inhibitors (ATRi) (9). According to recent research of inherited germline mutations in a Chinese population with lung cancer assessed using an NGS, the majority of the discovered germline mutations (85.5 percent) were implicated in DNA damage repair (DDR) pathways (10). There have previously been reports of rare events in lung cancer patients, which may be related to the genetic susceptibility to lung cancer (11). As a high-throughput method, next-generation sequencing (NGS) has become routine in clinical practice and has altered the clinical management of lung cancer (12, 13). This method enables for massively parallel characterization of thousands of cells at the transcriptome level. In this study, we identified an interesting ATR mutation by whole-exome sequencing in three sisters of this family with lung cancers.
The three patients were sisters and were treated successively in the Thoracic Surgery Department of the First Hospital of China Medical University due to lung nodules. We have drawn the pedigree of the lung adenocarcinoma family (Figure 1). The first woman was a 61-year-old female with 40 years of smoking history (II -2), who was diagnosed with micro-invasive adenocarcinoma and invasive adenocarcinoma of two nodules in the upper right lobe (Figures 2A, B). Another 56-year-old female, non-smoker, with 2 nodules in the upper right lobe (II -4), was pathologically confirmed to be adenocarcinoma in situ and invasive adenocarcinoma after surgery (Figures 2C, D). Invasive adenocarcinoma of the right lower lobe (II-5) was diagnosed in a 47-year-old non-smoker sister of the family (Figure 2E). The other members of this family have no history of lung tumor. This study was approved by the ethics committees of the First Hospital of China Medical University. The patient signed written informed consent, and we kept the patient’s identity protection for the duration of the study.
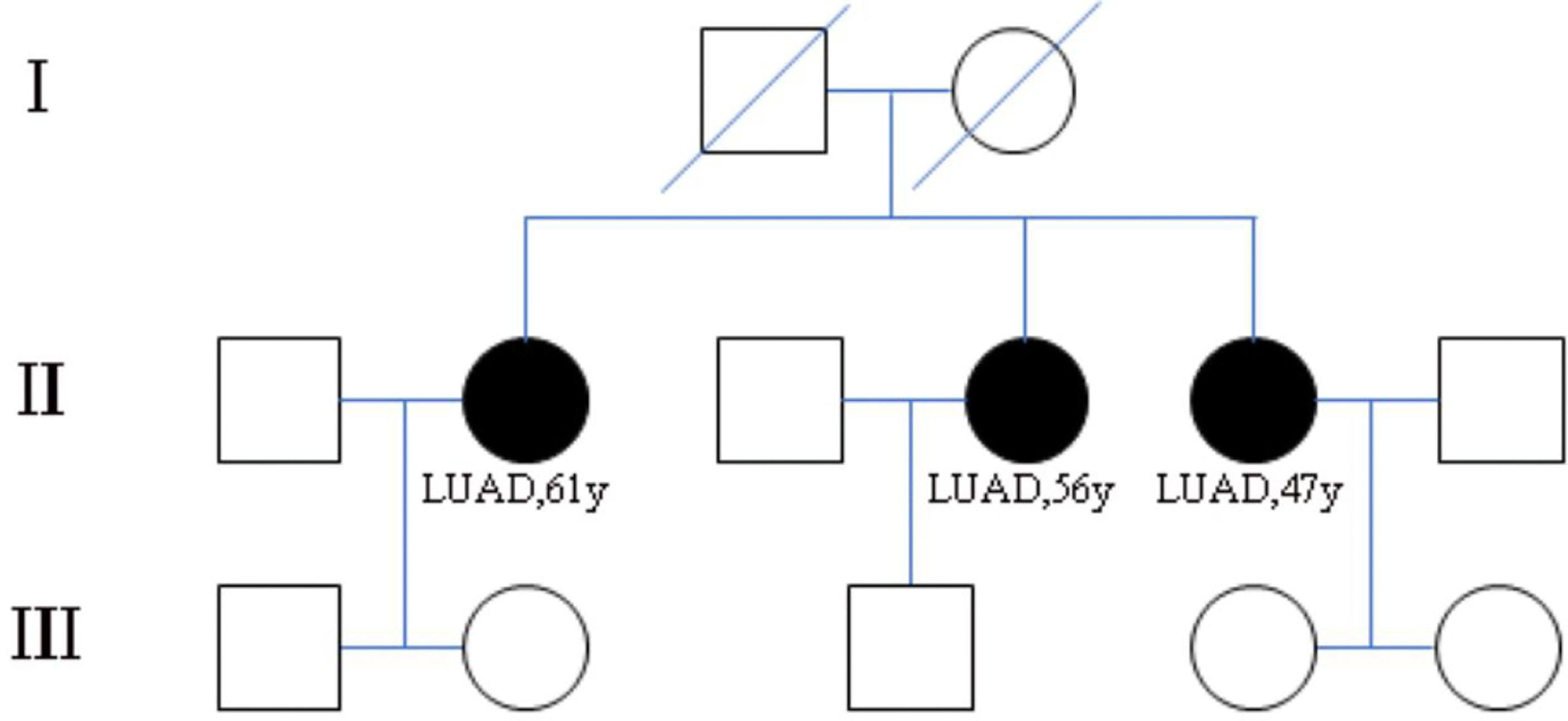
Figure 1 Pedigree of family (case 3) with multiple cases of lung adenocarcinoma. II-2, II-4, II-5 are sisters and have been diagnosed as lung adenocarcinoma. I-1 and I-2 are their parents and have passed away. The other members of this family have no history of lung tumor.
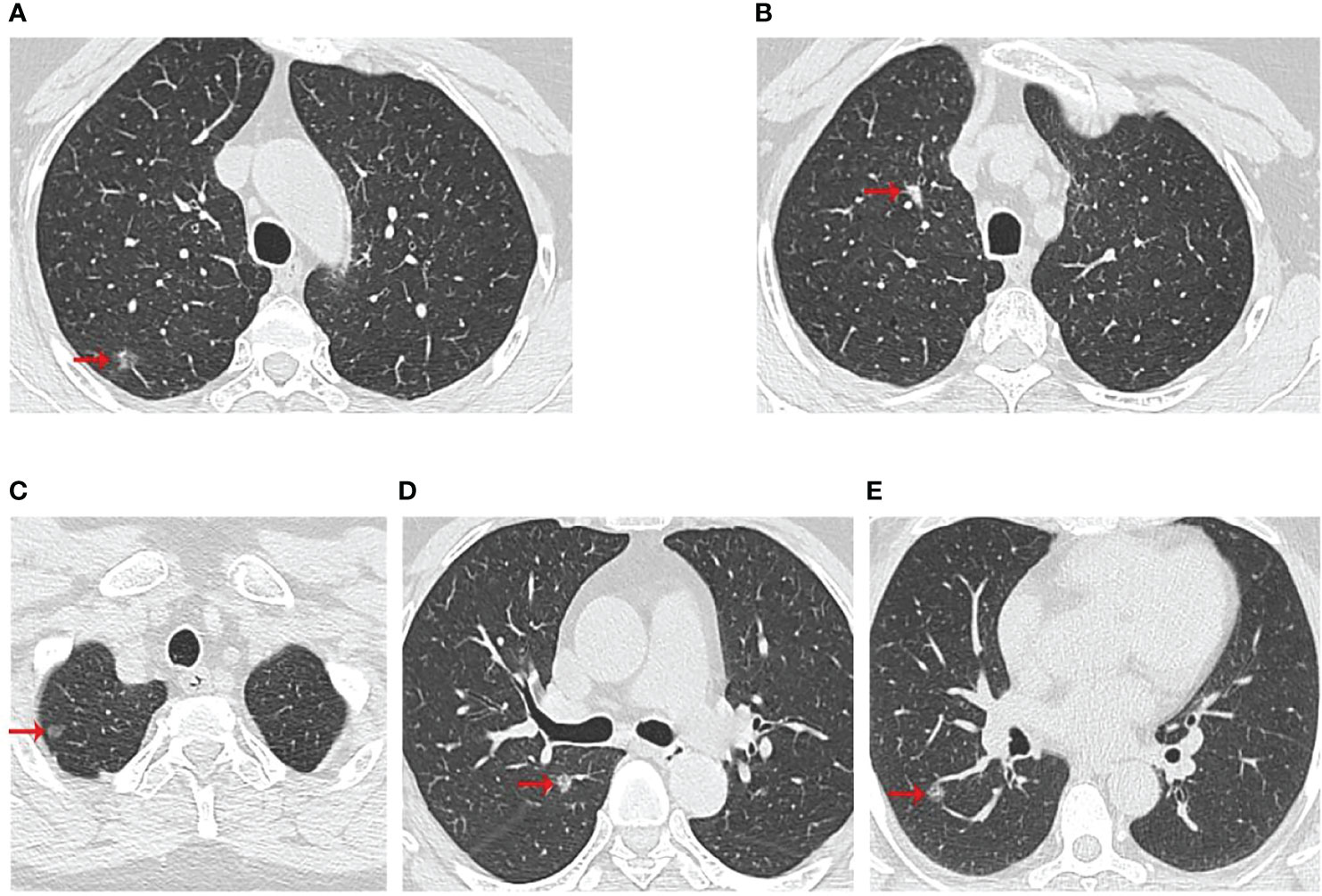
Figure 2 Computed tomographic scan of chest at diagnosis of three patients. (A, B) were II-2 CT scan results, which showed two nodules in the upper right lobe; (C, D) were II-4 CT scan results, which showed two nodules in the upper lobe of the right lung; (E) was II-5 CT scan results with a right lower lobe nodule. The red arrows indicated the location of the lesions.
In total, peripheral blood, cancer, para-cancerous samples, and clinical data of three patients were collected for whole-exome sequencing (WES) in this study. NEBNext dsDNA Fragmentase (NEB, Ipswich, MA, USA) was used to extract and fragment genomic DNA from blood and cancer or para-cancer (normal tissues adjacent to cancer) tissues, followed by DNA end mending. After being detailed, end-repaired DNA segments were ligated with the NEBNext adaptor (NEB, Ipswich, MA, USA). Biotinylated RNA library baits and magnetic beads were coupled with the barcoded library to detect particular areas using the SureSelect Human All Exon V6 Kit (Agilent Technologies, Palo Alto, Calif.). On an Illumina X-ten system, the acquired sequences were amplified further for 150bp paired-end sequencing (Illumina, San Diego, CA, USA). Readings of high quality that passed the Illumina filter were kept for further processing.
Using fastp, raw reads would be processed to make high-quality clean reads (14). To match the clean reads from each sample to the reference genome, the Burrows-Wheeler Aligner (BWA) (15) was employed (GRCh38.p12). The Genome Analysis Toolkit (GATK) (16) was used to call variants for multi-sample analyses. For multi-sample variant calling, local realignment, and base quality score recalibration, Unified Genotyper was employed. To assess the frequency of each SNP, the software package ANNOVAR (17) was used to align and annotate SNPs or InDels.Variants related to diseases were annotated with Clinvar database (http://www.clinvar.com/).
Gene expression profiles of 483 tumor samples and 347 normal samples in LUAD were conducted by GEPIA database (18). RNA-seq data and its relevant clinical information and mutation data of 561 LUAD samples were received from The Cancer Genome Atlas (TCGA) database (https://portal.gdc.cancer.gov/). Survival analysis was conducted by “survival” R package. The “maftools” R package was used to find high-frequency mutation genes. The GEO database (http://www.ncbi.nlm.nih.gov/geo/) was used to download raw UMI counts per gene, as well as the sample and cluster annotations of 11 human LUAD and 11 human normal lung samples from Kim et al’s research (19). The raw counts were normalized using the “scran” R program, and then cluster annotation was performed using the “SingleR” R tool.
We performed whole-exome sequencing on surgical samples and peripheral blood to discover variants associated with familial lung cancer. Then, we applied the following filters for the variants called by whole exome sequencing to identify the most significant germline mutations: (1) all affected family members must have mutations; (2) variations in the SNP databases with a minor allele frequency (MAF) greater than 0.5 percent were eliminated from further research, cause they are more likely to be functional neutral polymorphisms (the SNP databases that we used for filtering are Clinvar from Complete Genomics); (3) the variations must be missense or nonsense mutations or indels that cause in alterations or a shortened protein.; (4) bioinformatics algorithms such as PolyPhen-2 (20), SIFT (21), or MutationTaster must forecast that these mutations are functionally “non-benign” or “intolerable” and are linked to cancer (22). We summarized and annotated the mutation data of three patients (Table 1), and seven candidate variants were discovered in three patients of this family, only the ATR c.7667C>G (p.T2556S) mutation is the most important germline mutation in this family.
Then, the results of somatic mutations in five tumor lesions of three patients were thoroughly studied. The somatic SNV/INDEL mutation spectrum and CNV mutation spectrum of the three lung cancer patients in this investigation were mapped (Supplementary Figure S1). Moreover, we searched the reported driver gene data to screen out the known driver genes in the tumor sample based on Cancer Gene Census (http://cancer.sanger.ac.uk/census), MDG125 (23), SMG127 (24), CDG291 (25) database and we noticed that somatic mutations frequently found in this family, such as EGFR, BRCA1 and ROS1 were also observed (Table 2). Furthermore, new candidate driver genes of lung adenocarcinoma, like PNCK and IP6K2 could also be found in this family (Table 3). Finally, we used MuSiC software (26) to find genes with higher mutation frequencies of the three patients, we found the top thirty high-frequency mutation genes (Figure 3A) and we summarized the mutation information of these genes in the TCGA mutation data, and we found that AMT, BICRA, ARMCX4 are high-frequency mutation genes unique to these three patients (Figure 3B).
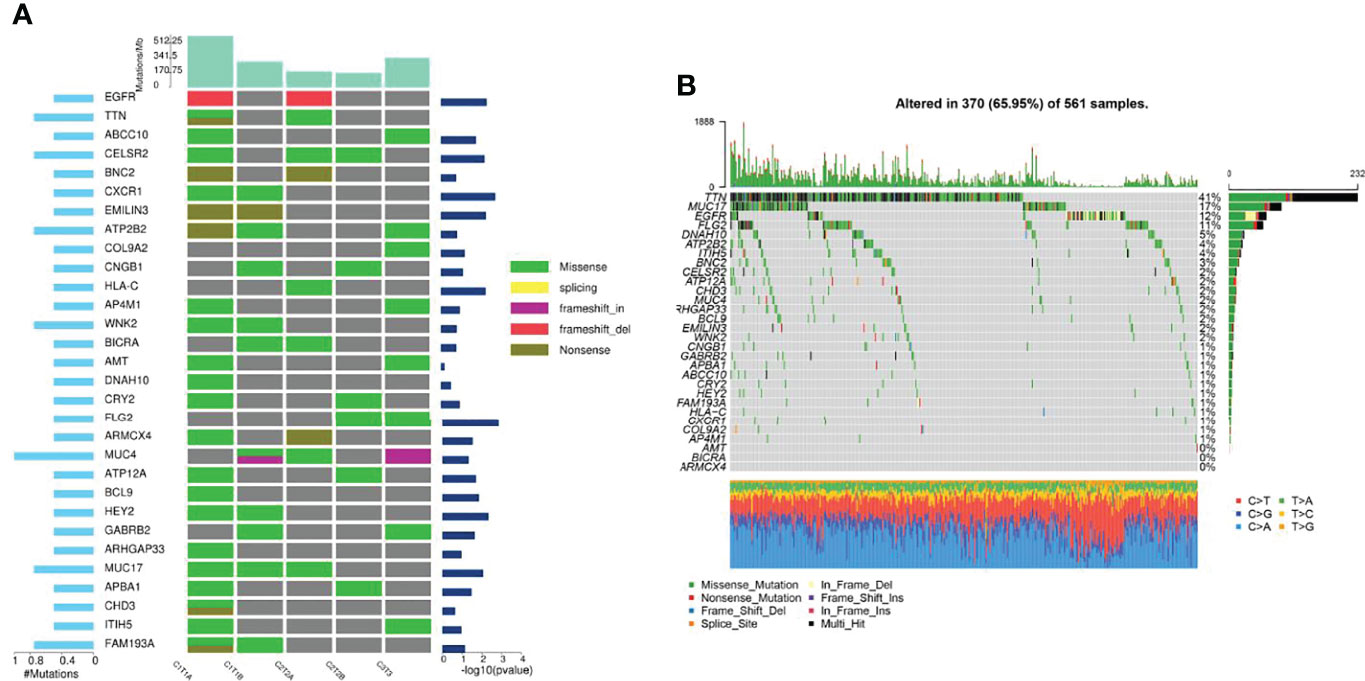
Figure 3 Gene mutation characteristics of three patients and in TCGA database. (A) High-frequency mutation genes of three lung adenocarcinoma patients; (B) Mutation spectrum of high-frequency mutation genes in TCGA mutation data.
ATR is required for maintaining genome integrity during DNA replication and plays a key role in avoiding replication stress at toxic levels, according to previous research. Because of these critical functions, cancers infrequently involve loss-of-function mutations in the ATR pathway, and a subset of tumors with particular mutations is more vulnerable to ATR pathway inhibition than normal cells (27). The underlying mechanism of ATR expression in lung adenocarcinoma requires further study, hence we analyzed ATR related expression and prognosis in cases of lung adenocarcinoma. As demonstrated in Figure 4, the expression of ATR was downregulated in LUAD patients as compared to normal individuals, and the downregulation of ATR expression was related to poor prognosis. Moreover, we used single-cell sequencing data to further explore the expression of ATR in designated cell types of lung adenocarcinoma and found the expression of ATR in stromal cells (Fibroblasts, Epithelial cells, Endothelial cells) of tumor patients is at a lower level when compared with normal patients, but the expression of ATR in the immune cells (Myeloid cells, B lymphocytes, MAST cells) of tumor patients is at a high level, except for T/NK cells (Figure 5).
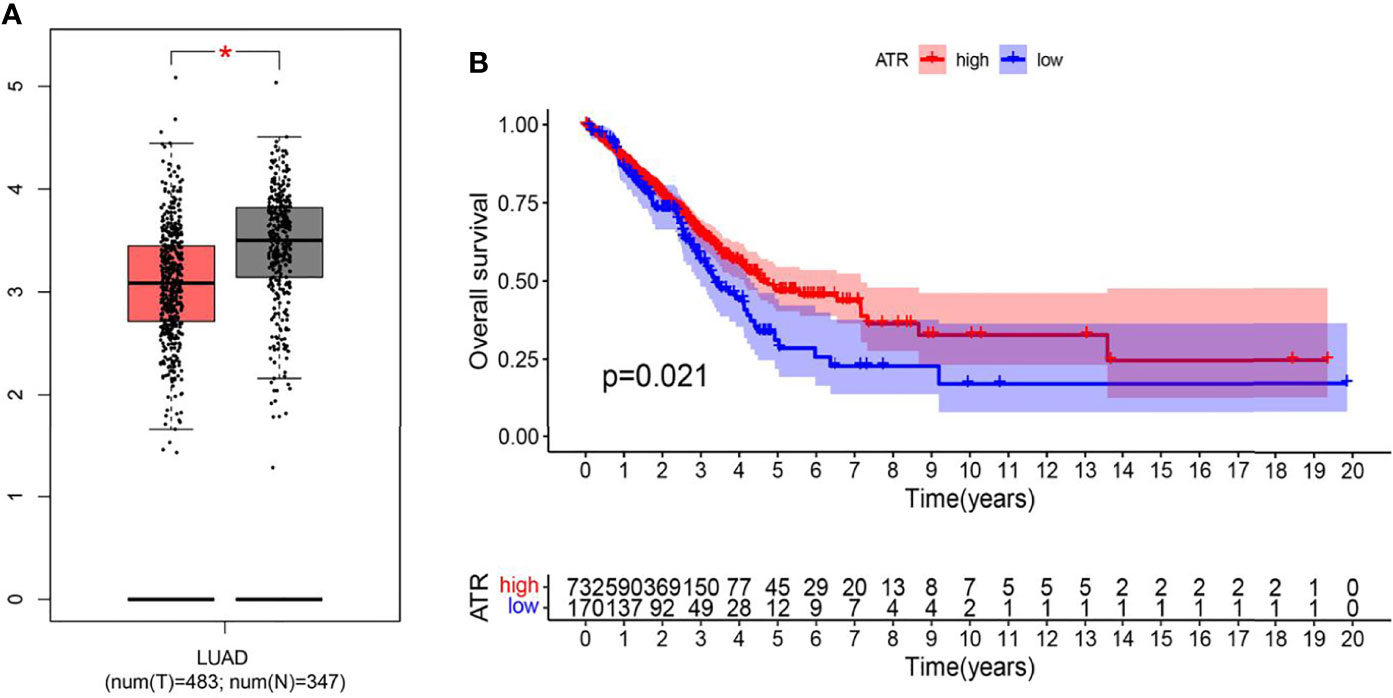
Figure 4 The expression and prognostic differences of ATR in TCGA database. (A) The expression of ATR in LUAD and normal tissues in GEPIA database (Tumor: 483; Normal: 347) (* indicates p < 0.05); (B) Down regulation of ATR is associated with harmful outcome in TCGA database (Tumor: 535; Normal: 59) (p = 0.021).
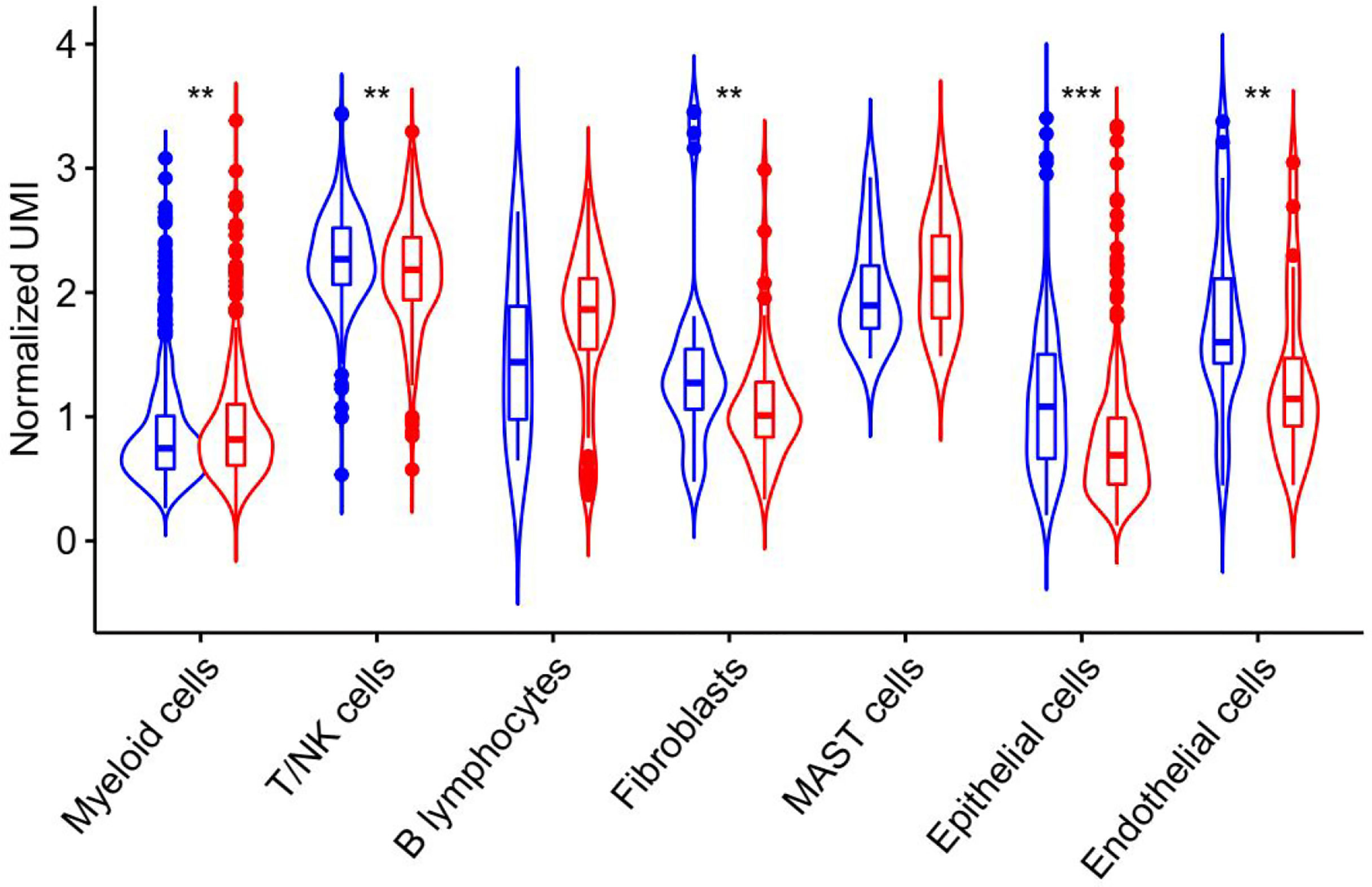
Figure 5 ATR expression in unique molecular identifiers in the indicated cell types from single-cell RNA-Seq data derived from human LUAD specimen. Blue represents the expression of ATR in each component of normal tissue, and red represents the expression of ATR in each component of tumor tissue.
Next, we analyzed the whole-exome sequencing data of 2706 patients to uncover the germline gene mutations in the Chinese LUAD cohort. We then screened out 27 germline gene mutations and listed their mutation frequencies and mutation sites (Table 4). Among the relatively common mutant genes, including MLH1 (1.03474%), BRCA (0.77605%), STK11 (0.62823%), CHEK2 (0.44346%), TP53 (0.44346%), have been reported related to lung cancer. Meanwhile, multiple mutation sites of these germline gene mutations were also revealed. For example, we have detected 3 different mutation sites in the germline mutation of MLH1, including c.649C>T (p.R217C), p.Q701K (c. C2101A), and p.V384D (c.T1151A).
Carcinogenesis is a multi-factor and multi-stage process and gene mutation is an important cause of cancer occurrence and development (28). Germline mutations including somatic mutation and germline mutations. Germline mutations which occur in the reproductive cells, it can be passed on to the next generation, affecting every cell in the next generation. However, most studies on tumor mutations have focused on somatic mutations. The mining and identification of tumor germline mutations are very limited, with only a few cases reported in lung adenocarcinoma. As a result, the identification of novel germline mutations is critical for both fundamental research and clinical cancer treatment (29).
In previous studies, most of the genes with germline mutations in lung adenocarcinoma were typical oncogenes and proto-oncogenes, which included BRCA2, CHECK2, CDKN2, BAP1, EGFR (30–32). The genomic alternations of these genes were thought to be important in familial lung cancer. Then, with the development of high-throughput sequencing data, germline altered variants in other genes (MAST1, CENPE, LCT) (33–35) were identified to exhibit an essential role in the development of lung adenocarcinoma, and they were suspected to be related to the development of lung cancer through whole-exome or genome sequencing of samples from many lung cancer patients.
In this study, we continue to focus on the germline mutation of genes in lung adenocarcinoma and we have identified seven different variants (SMG5, RAB3GAF2, EI24, XDH, PTPRA, ATR, GSTZ1) in three sibling patients suffering from lung cancer. The most significant is a rare somatic mutation in the ATR gene named c.7667C>G (p.T2556S), and this ATR gene variation has never been observed in genome and exome research within combined populations. Then, we analyzed the expression and prognosis of ATR in lung adenocarcinoma. Compared with normal patients, the expression of ATR was down-regulated in LUAD, and the down-regulated expression of ATR was associated with poor prognosis. Furthermore, we employed single-cell sequencing data to investigate the expression of ATR in lung adenocarcinoma cell types. Compared with normal patients, we found that the expression level of ATR in the stromal cells (fibroblasts, epithelial cells, and endothelial cells) of tumor patients was low. In addition to T/NK cells, the expression level of ATR in immune cells (myeloid cells, B lymphocytes, MAST cells) of tumor patients is higher. In view of this, we have reason to believe that germline ATR c.7667C>G (p.T2556S) mutation may lead to familial clusters of lung adenocarcinoma and differentially expressed ATR may play an essential role in the occurrence and development of lung adenocarcinoma. Moreover, based on somatic mutation data, we found common driver gene mutations such as EGFR, BRCA1, ROS1, etc. We predicted 136 new driver gene mutations such as PNCK, IP6K2, CLEC18C, etc. through OncodriveCLUST software (36). These gene mutations may be secondary somatic mutations based on germline ATR c.7667C>G (p.T2556S) mutations, which eventually lead to the occurrence and progression of lung adenocarcinoma.
ATR, as a necessary gene in the DNA damage repair pathway, is involved in the coordination of cell-cycle transitions, DNA replication, DNA repair, and apoptosis (37). Previous studies have shown that germline gene mutations that occur in the DNA damage repair pathway often irreversibly lead to tumors (38, 39). Furthermore, germline abnormalities in DNA repair genes lead to advanced solid tumor (such as prostate, ovarian, pancreatic, and breast cancer) susceptibility to poly ADP ribose polymerase (PARP) inhibitors (40–42). To our knowledge, this is the first such case report confirming the presence of c.7667C>G (p.T2556S), a germline ATR mutation, in a family with three occurrences of lung adenocarcinoma The resulting amino acid mutation, p.Thr2556Ser, was detected in the ATR’s conserved Phosphoinositide 3- and 4-kinase domain, which is involved in biological processes such as cell growth, proliferation, differentiation, motility, survival, and intracellular trafficking (43).
The population frequency in the entire population is 0.0399361 percent, suggesting that this ATR germline mutation may be a genetic susceptibility factor for lung adenocarcinoma. Our findings contribute to the understanding of the genesis and mechanism of lung cancer and may give clues for oncology treatment strategies and cancer prevention.
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: NCBI [accession: PRJNA800743].
The studies involving human participants were reviewed and approved by ethics committees of the First Hospital of China Medical University. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
GB conceived and designed the study, and drafted the manuscript. XG, YX, and YY collected, analyzed and interpreted the experimental data. JL, TL, and XZ revised the manuscript for important intellectual content. All authors contributed to the article and approved the submitted version.
This work was supported by Wu Jieping Medical Foundation (320.6750.2020-17-7).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We are grateful to Nanjing Shihe Gene Bio-Technology Co., Ltd. for providing the whole exome sequencing data of 2706 Chinese LUAD patients. We thanked Home for Researcher for language editing service.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2022.855305/full#supplementary-material
Supplementary Figure 1 | Somatic mutation spectrum of five lesions in three patients. (A, B) Somatic SNV/INDEL mutation spectrum; (C) Somatic CNV mutation spectrum. C1T1A: II-2 tumor A; C1T2A: II-2 tumor B; C2T2A: II-4 tumor A; C2T2B: II-4 tumor B; C3T3: II-5.
1. Sung H, Ferlay J, Siegel R, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA: Cancer J Clin (2021) 71:209–49. doi: 10.3322/caac.21660
2. Alberg A, Brock M, Ford J, Samet J, Spivack S. Epidemiology of Lung Cancer: Diagnosis and Management of Lung Cancer, 3rd Ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest (2013) 143:e1S–e29S. doi: 10.1378/chest.12-2345
3. Bailey-Wilson J, Amos C, Pinney S, Petersen G, De Andrade M, Wiest J, et al. A Major Lung Cancer Susceptibility Locus Maps to Chromosome 6q23-25. Am J Hum Genet (2004) 75:460–74. doi: 10.1086/423857
4. Schwartz A, Ruckdeschel J. Familial Lung Cancer: Genetic Susceptibility and Relationship to Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med (2006) 173:16–22. doi: 10.1164/rccm.200502-235PP
5. Tibaldi C, Giovannetti E, Vasile E, Boldrini L, Gallegos-Ruiz M, Bernardini I, et al. Inherited Germline T790M Mutation and Somatic Epidermal Growth Factor Receptor Mutations in non-Small Cell Lung Cancer Patients. J Thorac Oncol (2011) 6:395–6. doi: 10.1097/JTO.0b013e3182059a6f
6. Oxnard G, Nguyen K, Costa D. Germline Mutations in Driver Oncogenes and Inherited Lung Cancer Risk Independent of Smoking History. J Natl Cancer Institute (2014) 106:djt361. doi: 10.1093/jnci/djt361
7. Lu S, Yu Y, Li Z, Yu R, Wu X, Bao H, et al. EGFR and ERBB2 Germline Mutations in Chinese Lung Cancer Patients and Their Roles in Genetic Susceptibility to Cancer. J Thorac Oncol (2019) 14:732–6. doi: 10.1016/j.jtho.2018.12.006
8. Jackson S, Bartek J. The DNA-damage Response in Human Biology and Disease. Nature (2009) 461:1071–8. doi: 10.1038/nature08467
9. Bradbury A, Hall S, Curtin N, Drew Y. Targeting ATR as Cancer Therapy: A New Era for Synthetic Lethality and Synergistic Combinations? Pharmacol Ther (2020) 207:107450. doi: 10.1016/j.pharmthera.2019.107450
10. Tian P, Cheng X, Zhao Z, Zhang Y, Bao C, Wang Y, et al. Spectrum of Pathogenic Germline Mutations in Chinese Lung Cancer Patients Through Next-Generation Sequencing. Pathol Oncol Res POR (2020) 26:109–14. doi: 10.1007/s12253-019-00771-5
11. Zhang Y, Zhang L, Li R, Chang D, Ye Y, Minna J, et al. Genetic Variations in Cancer-Related Significantly Mutated Genes and Lung Cancer Susceptibility. Ann Oncol (2017) 28:1625–30. doi: 10.1093/annonc/mdx161
12. Puram S, Tirosh I, Parikh A, Patel A, Yizhak K, Gillespie S, et al. Single-Cell Transcriptomic Analysis of Primary and Metastatic Tumor Ecosystems in Head and Neck Cancer. Cell (2017) 171:1611–1624.e1624. doi: 10.1016/j.cell.2017.10.044
13. Azizi E, Carr A, Plitas G, Cornish A, Konopacki C, Prabhakaran S, et al. Single-Cell Map of Diverse Immune Phenotypes in the Breast Tumor Microenvironment. Cell (2018) 174:1293–1308.e1236. doi: 10.1016/j.cell.2018.05.060
14. Chen S, Zhou Y, Chen Y, Gu J. Fastp: An Ultra-Fast All-in-One FASTQ Preprocessor. Bioinf (Oxford England) (2018) 34:i884–90. doi: 10.1093/bioinformatics/bty560
15. Li H, Durbin R. Fast and Accurate Short Read Alignment With Burrows-Wheeler Transform. Bioinf (Oxford England) (2009) 25:1754–60. doi: 10.1093/bioinformatics/btp324
16. Mckenna A, Hanna M, Banks E, Sivachenko A, Cibulskis K, Kernytsky A, et al. The Genome Analysis Toolkit: A MapReduce Framework for Analyzing Next-Generation DNA Sequencing Data. Genome Res (2010) 20:1297–303. doi: 10.1101/gr.107524.110
17. Wang K, Li M, Hakonarson H. ANNOVAR: Functional Annotation of Genetic Variants From High-Throughput Sequencing Data. Nucleic Acids Res (2010) 38:e164. doi: 10.1093/nar/gkq603
18. Tang Z, Li C, Kang B, Gao G, Li C, Zhang Z. GEPIA: A Web Server for Cancer and Normal Gene Expression Profiling and Interactive Analyses. Nucleic Acids Res (2017) 45(1):W98–102. doi: 10.1093/nar/gkx247
19. Kim N, Kim H, Lee K, Hong Y, Cho J, Choi J, et al. Single-Cell RNA Sequencing Demonstrates the Molecular and Cellular Reprogramming of Metastatic Lung Adenocarcinoma. Nat Commun (2020) 11:2285. doi: 10.1038/s41467-020-16164-1
20. Adzhubei I, Schmidt S, Peshkin L, Ramensky V, Gerasimova A, Bork P, et al. A Method and Server for Predicting Damaging Missense Mutations. Nat Methods (2010) 7:248–9. doi: 10.1038/nmeth0410-248
21. Ng P, Henikoff S. Sift: Predicting Amino Acid Changes That Affect Protein Function. Nucleic Acids Res (2003) 31:3812–4. doi: 10.1093/nar/gkg509
22. Schwarz J, Rödelsperger C, Schuelke M, Seelow D. MutationTaster Evaluates Disease-Causing Potential of Sequence Alterations. Nat Methods (2010) 7:575–6. doi: 10.1038/nmeth0810-575
23. Vogelstein B, Papadopoulos N, Velculescu V, Zhou S, Diaz L, Kinzler K. Cancer Genome Landscapes. Sci (N Y NY) (2013) 339:1546–58. doi: 10.1126/science.1235122
24. Kandoth C, Mclellan M, Vandin F, Ye K, Niu B, Lu C, et al. Mutational Landscape and Significance Across 12 Major Cancer Types. Nature (2013) 502:333–9. doi: 10.1038/nature12634
25. Tamborero D, Gonzalez-Perez A, Perez-Llamas C, Deu-Pons J, Kandoth C, Reimand J, et al. Comprehensive Identification of Mutational Cancer Driver Genes Across 12 Tumor Types. Sci Rep (2013) 3:2650. doi: 10.1038/srep02650
26. Dees N, Zhang Q, Kandoth C, Wendl M, Schierding W, Koboldt D, et al. MuSiC: Identifying Mutational Significance in Cancer Genomes. Genome Res (2012) 22:1589–98. doi: 10.1101/gr.134635.111
27. Karnitz L, Zou L. Molecular Pathways: Targeting ATR in Cancer Therapy. Clin Cancer Res Off J Am Assoc Cancer Res (2015) 21:4780–5. doi: 10.1158/1078-0432.CCR-15-0479
28. Curtius K, Wright N, Graham T. An Evolutionary Perspective on Field Cancerization. Nat Rev Cancer (2018) 18:19–32. doi: 10.1038/nrc.2017.102
29. Przytycki P, Singh M. Differential Analysis Between Somatic Mutation and Germline Variation Profiles Reveals Cancer-Related Genes. Genome Med (2017) 9:79. doi: 10.1186/s13073-017-0465-6
30. Abdel-Rahman M, Pilarski R, Cebulla C, Massengill J, Christopher B, Boru G, et al. Germline BAP1 Mutation Predisposes to Uveal Melanoma, Lung Adenocarcinoma, Meningioma, and Other Cancers. J Med Genet (2011) 48:856–9. doi: 10.1136/jmedgenet-2011-100156
31. Thomas A, Xi L, Carter C, Rajan A, Khozin S, Szabo E, et al. Concurrent Molecular Alterations in Tumors With Germ Line Epidermal Growth Factor Receptor T790M Mutations. Clin Lung Cancer (2013) 14:452–6. doi: 10.1016/j.cllc.2013.01.005
32. Wang Y, Mckay J, Rafnar T, Wang Z, Timofeeva M, Broderick P, et al. Rare Variants of Large Effect in BRCA2 and CHEK2 Affect Risk of Lung Cancer. Nat Genet (2014) 46:736–41. doi: 10.1038/ng.3002
33. Renieri A, Mencarelli M, Cetta F, Baldassarri M, Mari F, Furini S, et al. Oligogenic Germline Mutations Identified in Early non-Smokers Lung Adenocarcinoma Patients. Lung Cancer (Amsterdam Netherlands) (2014) 85:168–74. doi: 10.1016/j.lungcan.2014.05.020
34. Clamon G, Bossler A, Abu Hejleh T, Furqan M. Germline Mutations Predisposing to non-Small Cell Lung Cancer. Familial Cancer (2015) 14:463–9. doi: 10.1007/s10689-015-9796-x
35. Tomoshige K, Matsumoto K, Tsuchiya T, Oikawa M, Miyazaki T, Yamasaki N, et al. Germline Mutations Causing Familial Lung Cancer. J Hum Genet (2015) 60:597–603. doi: 10.1038/jhg.2015.75
36. Tamborero D, Gonzalez-Perez A, Lopez-Bigas N. OncodriveCLUST: Exploiting the Positional Clustering of Somatic Mutations to Identify Cancer Genes. Bioinf (Oxford England) (2013) 29:2238–44. doi: 10.1093/bioinformatics/btt395
37. Cimprich K, Cortez D. ATR: An Essential Regulator of Genome Integrity. Nat Rev Mol Cell Biol (2008) 9:616–27. doi: 10.1038/nrm2450
38. Parry E, Gable D, Stanley S, Khalil S, Antonescu V, Florea L, et al. Germline Mutations in DNA Repair Genes in Lung Adenocarcinoma. J Thorac Oncol (2017) 12:1673–8. doi: 10.1016/j.jtho.2017.08.011
39. Wei Y, Wu J, Gu W, Qin X, Dai B, Lin G, et al. Germline DNA Repair Gene Mutation Landscape in Chinese Prostate Cancer Patients. Eur Urol (2019) 76:280–3. doi: 10.1016/j.eururo.2019.06.004
40. Fong P, Boss D, Yap T, Tutt A, Wu P, Mergui-Roelvink M, et al. Inhibition of Poly(ADP-Ribose) Polymerase in Tumors From BRCA Mutation Carriers. New Engl J Med (2009) 361:123–34. doi: 10.1056/NEJMoa0900212
41. Kaufman B, Shapira-Frommer R, Schmutzler R, Audeh M, Friedlander M, Balmaña J, et al. Olaparib Monotherapy in Patients With Advanced Cancer and a Germline BRCA1/2 Mutation. J Clin Oncol (2015) 33:244–50. doi: 10.1200/JCO.2014.56.2728
42. Mateo J, Carreira S, Sandhu S, Miranda S, Mossop H, Perez-Lopez R, et al. Dna-Repair Defects and Olaparib in Metastatic Prostate Cancer. New Engl J Med (2015) 373:1697–708. doi: 10.1056/NEJMoa1506859
Keywords: familiar lung cancer, ATR, sequencing, germline mutation, lung adenocarcinoma
Citation: Bao G, Guan X, Liang J, Yao Y, Xiang Y, Li T and Zhong X (2022) A Germline Mutation in ATR Is Associated With Lung Adenocarcinoma in Asian Patients. Front. Oncol. 12:855305. doi: 10.3389/fonc.2022.855305
Received: 15 January 2022; Accepted: 26 April 2022;
Published: 31 May 2022.
Edited by:
Yutong He, Fourth Hospital of Hebei Medical University, ChinaReviewed by:
Ling Zhao, Harbin Medical University Cancer Hospital, ChinaCopyright © 2022 Bao, Guan, Liang, Yao, Xiang, Li and Zhong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xinwen Zhong, eHd6aG9uZ0BjbXUuZWR1LmNu; Tian Li, Zm1tdWx0QGZveG1haWwuY29t
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.