
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Oncol. , 10 March 2022
Sec. Pharmacology of Anti-Cancer Drugs
Volume 12 - 2022 | https://doi.org/10.3389/fonc.2022.853211
This article is part of the Research Topic Medicinal chemistry of the PARP-1 inhibitor anti-tumor agents and other natural product derivatives View all 4 articles
Niraparib, an oral, potent, highly selective poly (ADP-ribose) polymerase (PARP) inhibitor, has promising clinical benefit for maintenance treatment of patients with ovarian cancer in partial response to platinum-based chemotherapy, especially in patients with BRCA mutation. In publicly available niraparib treatment-related adverse events, gastrointestinal disorders and hematological toxicities were most commonly reported with manageable safety profile. Herein, we first describe a severe and never-reported pulmonary embolism (PE) associated with the use of niraparib in a patient with BRCA mutation advanced high-grade serous ovarian cancer and received anticoagulant therapy after PE. There have been no reports of PE caused by the use of niraparib in patients with advanced high-grade serous ovarian cancer; knowledge of the occurrence of PE after the use of niraparib may assist other clinicians in managing this rare but potentially serious toxic effect.
Niraparib, an oral, potent, highly selective poly (ADP-ribose) polymerase (PARP) inhibitor, has promising clinical benefit for maintenance treatment of patients with ovarian cancer in partial response to platinum-based chemotherapy, especially in patients with BRCA mutation or homologous recombination deficiency (HRD)-positive disease (1, 2). In publicly available niraparib treatment-related adverse events, the most common drug-related treatment-emergent adverse events were anemia and thrombocytopenia, and the most common treatment-emergent serious adverse events were small intestinal obstruction, thrombocytopenia and vomiting.1 Herein, we first describe a severe and never-reported PE associated with the use of niraparib in a patient with BRCA mutant advanced high-grade serous ovarian cancer.
A 55-year-old female patient was diagnosed with advanced high-grade serous ovarian cancer after comprehensive multidisciplinary consultation. Platinum-based chemotherapy was administered as first-line treatment, and the disease was evaluated as partial response. To seek for an effective maintenance therapy, tumor BRCA mutation and HRD status were analyzed using a next-generation sequencing assay in patient providing tissue sample in a CAP-authenticated lab. Subsequently, BRCA2 c.6860G>T (1.85% abundance), CDK12 c.956dupA (22.04% abundance), and ATM c.5692C>T (1.64% abundance) mutations (Figures 1A–C) were detected and confirmed by polymerase chain reaction assay, suggesting PARP inhibitor may show promising clinical benefit for the maintenance treatment.
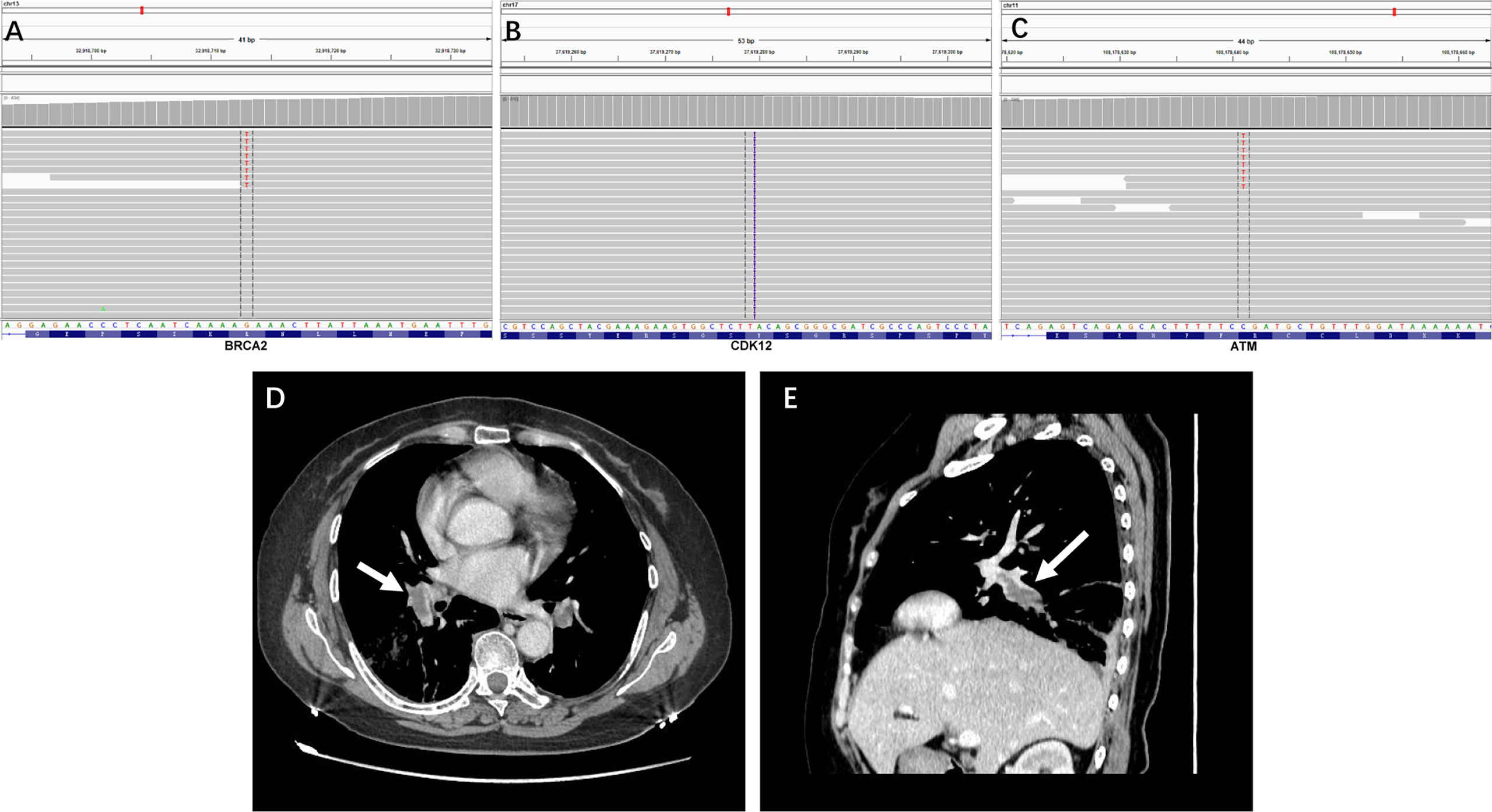
Figure 1 (A–C) The integrative genomics viewer snapshot of BRCA2 c.6860G>T, CDK12 c.956dupA, and ATM c.5692C>T mutation. (D, E) Contrast-enhanced CT revealed dilated pulmonary veins with hypodense filling defect (E), 35.0 × 13.2 mm) highlighting the presence of thrombosis (arrow).
Two months after the ending of the last cycle of chemotherapy, niraparib (200 mg once daily) was administered for the following maintenance treatment; clinical and radiological follow-up within the first 2 months showed no evidence of progression and severe adverse reactions. In the second and a half month of taking niraparib, the patient was presented to the emergency room with the chief complaints of dyspnea, chest pain, and lower abdominal pain that had begun a few days earlier. On presentation, she was mild febrile and had tachycardia with a regular rate. Laboratory studies revealed activated partial thromboplastin time of 22.3 s (normal range (NR), 25.0 to 31.3 s); the serum D-dimer was 23.19 μg/ml (NR < 0.55 µg/ml); and the serum fibrinogen was 4.38 g/L (NR, 2–4 g/L). Other coagulation parameters such as prothrombin time and thrombin time were within normal ranges. Emergency contrast-enhanced computed tomography (CT) revealed dilated pulmonary veins with hypodense filling defect highlighting the presence of thrombosis (Figures 1D, E).
Based on the clinical presentation, CT images, and remarkably increased serum D-dimer and fibrinogen levels, a diagnosis of PE caused by the use of niraparib was made; she was then transported to the high care unit under anticoagulant therapy. Three days after the treatment, CT examination detected the remaining thrombi and her serum D-dimer decreased to 3.66 μg/ml. A week later, she was discharged and discontinued from the use of niraparib; no PE symptoms occurred on the follow-up treatment.
The standard of care for frontline therapy of advanced ovarian cancer is mainly platinum-based chemotherapy in some settings (3, 4). Although most patients respond to initial therapy, most of them will ultimately succumb to the disease. Usually, the recurrence of the disease poorly responds to first- and sometimes even second-line chemotherapy. In this scenario, it is possible that the ovarian cancer inherent resistance may be due to reduced immunosurveillance and drug-resistant cells (5, 6). PARP inhibitors are a new treatment approach for ovarian cancer and other cancers with underlying impaired DNA repair. For instance, PARP inhibitors also bring breakthrough progress in prostate cancer (7). The novel combinations of PARP inhibitors with other anticancer therapies, including inhibitors of VEGF, PD-1, or PD-L1, along with anti-CTLA 4 monoclonal antibodies, are well tolerated and clinically effective (8). In publicly available niraparib treatment-related adverse events, gastrointestinal disorders and hematological toxicities were most commonly reported with manageable safety profile.
PE is a serious complication of surgery and a leading cause of death in women with gynecologic cancer. Serous tubal intraepithelial carcinoma (STIC) is currently considered the precursor lesion of pelvic high-grade serous carcinoma. The incidence of STIC in BRCA1–2 variants was low (9). Early detection and adequate intervention are crucially important in order to prevent PE. In our case, the chief complaints of chest pain and lower abdominal pain suggested the possible presence of deep vein thrombosis. During the thrombosis process, the functions of the coagulation system, anticoagulation system, and fibrinolytic system are activated. D-dimer is a degradation product of fibrin, present in the blood when thrombi are broken down. The level of D-dimer reflects fibrin concentration and is known to have a high positive predictive value. In our case, remarkably increased fibrinogen levels and D-dimer levels suggested the rapid progression of blood coagulation and fibrinolysis. The contrast-enhanced computed tomography revealed dilated pulmonary veins with hypodense filling defect highlighting the presence of thrombosis. Chemotherapy is considered a significant risk factor for cancer-associated thrombosis and may have contributed to its increasing incidence because of the harm on the vascular epithelium (10). In view of niraparib being administered for the maintenance treatment 2 months after the ending of the last cycle of chemotherapy, this eliminated the possibility of the side effect from chemotherapy. Finally, based on the clinical presentation, CT images, and remarkably increased serum D-dimer and fibrinogen levels, a diagnosis of PE caused by the use of niraparib was made.
There are several reports of PE occurring after operation or during chemotherapy in patients with ovarian cancer (11–13). However, confirmed by publicly available niraparib treatment-related adverse events, there have been no reports of PE caused by the use of niraparib in patients with advanced high-grade serous ovarian cancer. In summary, we describe for the first time the occurrence of PE associated with the use of niraparib in a patient with BRCA mutant advanced high-grade serous ovarian cancer. Frankly speaking, we cannot give a detailed mechanism to explain the relationship between the use of niraparib and the occurrence of PE; we hypothesized that off-target inhibition of yet another ubiquitously expressed target may be responsible. Anyway, knowledge of the occurrence of PE after the use of niraparib may assist other clinicians in managing this rare but potentially serious toxic effect.
The datasets for this article are not publicly available due to concerns regarding participant/patient anonymity. Requests to access the datasets should be directed to the corresponding author.
The studies involving human participants were reviewed and approved by the Jiangsu Cancer Hospital. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
We were all involved in the clinical care and management of the patient, collecting the data, and drafting the manuscript. QW and DC collected data and wrote the first draft of the manuscript. YL supervised the work. All authors critically reviewed and approved the final version.
Author DC was employed by Jiangsu Simcere Diagnostics Co. Ltd., Nanjing, China.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2022.853211/full#supplementary-material
1. Moore KN, Secord AA, Geller MA, Miller DS, Cloven N, Fleming GF, et al. Niraparib Monotherapy for Late-Line Treatment of Ovarian Cancer (QUADRA): A Multicentre, Open-Label, Single-Arm, Phase 2 Trial. Lancet Oncol (2019) 20:636–48. doi: 10.1016/S1470-2045(19)30029-4
2. Wu XH, Zhu JQ, Yin RT, Yang JX, Liu JH, Wang J, et al. Niraparib Maintenance Therapy in Patients With Platinum-Sensitive Recurrent Ovarian Cancer Using an Individualized Starting Dose (NORA): A Randomized, Double-Blind, Placebo-Controlled Phase III Trial. Ann Oncol (2021) 32:512–21. doi: 10.1016/j.annonc.2020.12.018
3. Siegel RL, Miller KD, Jemal A. Cancer Statistics, 2018. CA Cancer J Clin (2018) 68:7–30. doi: 10.3322/caac.21442
4. McMeekin DS, Tillmanns T, Chaudry T, Gold M, Johnson G, Walker J, et al. Timing Isn’t Everything: An Analysis of When to Start Salvage Chemotherapy in Ovarian Cancer. Gynecol Oncol (2004) 95:157–64. doi: 10.1016/j.ygyno.2004.07.008
5. Laganà AS, Sofo V, Vitale SG, Triolo O. Epithelial Ovarian Cancer Inherent Resistance: May the Pleiotropic Interaction Between Reduced Immunosurveillance and Drug-Resistant Cells Play a Key Role? Gynecol Oncol Rep (2016) 18:57–8. doi: 10.1016/j.gore.2016.09.004
6. Laganà AS, Colonese F, Colonese E, Sofo V, Salmeri FM, Granese R, et al. Cytogenetic Analysis of Epithelial Ovarian Cancer’s Stem Cells: An Overview on New Diagnostic and Therapeutic Perspectives. Eur J Gynaecol Oncol (2015) 36:495–505.
7. Ghose A, Moschetta M, Pappas-Gogos G, Sheriff M, Boussios S. Genetic Aberrations of DNA Repair Pathways in Prostate Cancer: Translation to the Clinic. Int J Mol Sci (2021) 22:9783. doi: 10.3390/ijms22189783
8. Boussios S, Karihtala P, Moschetta M, Karathanasi A, Sadauskaite A, Rassy E, et al. Combined Strategies With Poly (ADP-Ribose) Polymerase (PARP) Inhibitors for the Treatment of Ovarian Cancer: A Literature Review. Diagn Basel Switz (2019) 9:E87. doi: 10.3390/diagnostics9030087
9. Saccardi C, Zovato S, Spagnol G, Bonaldo G, Marchetti M, Alessandrini L, et al. Efficacy of Risk-Reducing Salpingo-Oophorectomy in BRCA1-2 Variants and Clinical Outcomes of Follow-Up in Patients With Isolated Serous Tubal Intraepithelial Carcinoma (STIC). Gynecol Oncol (2021) 163:364–70. doi: 10.1016/j.ygyno.2021.08.021
10. Shah S, Karathanasi A, Revythis A, Ioannidou E, Boussios S. Cancer-Associated Thrombosis: A New Light on an Old Story. Dis Basel Switz (2021) 9:34. doi: 10.3390/diseases9020034
11. Tasaka N, Minaguchi T, Hosokawa Y, Takao W, Itagaki H, Nishida K, et al. Prevalence of Venous Thromboembolism at Pretreatment Screening and Associated Risk Factors in 2086 Patients With Gynecological Cancer. J Obstet Gynaecol Res (2020) 46:765–73. doi: 10.1111/jog.14233
12. Basaran D, Boerner T, Suhner J, Sassine D, Liu Y, Grisham RN, et al. Risk of Venous Thromboembolism in Ovarian Cancer Patients Receiving Neoadjuvant Chemotherapy. Gynecol Oncol (2021) 163(1):36–40. doi: 10.1016/j.ygyno.2021.07.030
Keywords: Niraparib, pulmonary embolism, BRCA mutation, ovarian cancer
Citation: Wei Q, Chen D-S and Liu Y-H (2022) Case Report: Niraparib-Related Pulmonary Embolism During the Treatment of BRCA Mutant Advanced Ovarian Cancer. Front. Oncol. 12:853211. doi: 10.3389/fonc.2022.853211
Received: 12 January 2022; Accepted: 11 February 2022;
Published: 10 March 2022.
Edited by:
Hongfei Chen, University of South China, ChinaReviewed by:
Nicholas Pavlidis, University of Ioannina, GreeceCopyright © 2022 Wei, Chen and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuan-Hua Liu, eXVhbmh1YWxpdTAyQGhvdG1haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.