- 1Holden Comprehensive Cancer Center, University of Iowa Hospitals and Clinics, Iowa City, IA, United States
- 2Englander Institute for Precision Medicine, Weill Cornell Medical College, New York, NY, United States
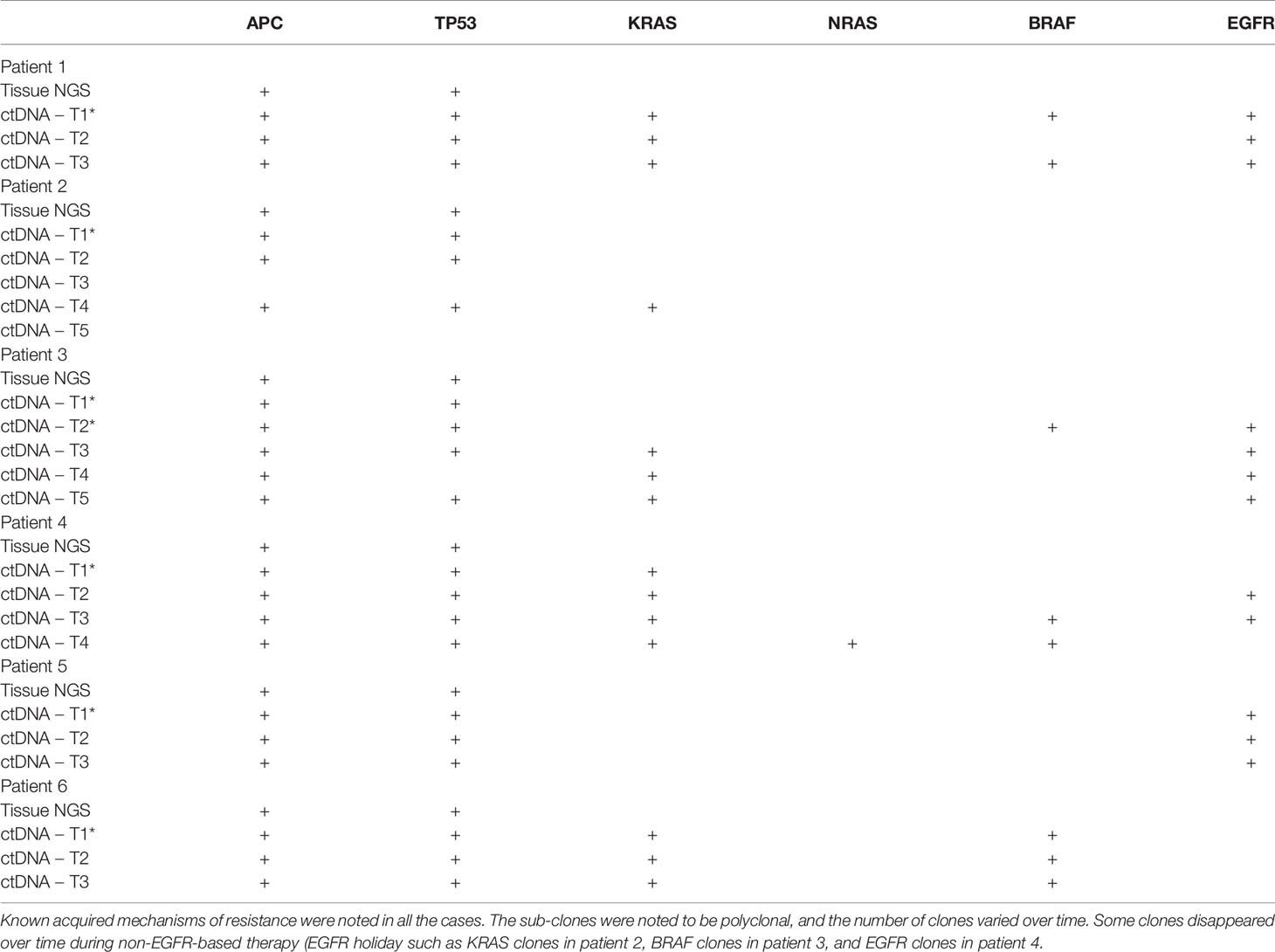
For patients with metastatic RAS/RAF wild-type refractory colorectal cancer, the question of anti-EGFR therapy rechallenge often comes up after initial use. However, not all patients derive benefit. It is now well known that these tumors acquire mechanisms of resistance in the mitogen-activated protein kinase (MAPK) pathway, which can be detected on circulating tumor DNA (ctDNA)-based testing. We present a series of patients who had serial testing post-EGFR blockade showing its feasibility and value. This would have implications for EGFR rechallenge. We reviewed records for patients who were initially noted to be RAS/RAF wild-type on tissue, who received prior anti-EGFR therapy and then subsequently had at least one circulating tumor DNA-based testing. These patients also had tissue-based genomic testing obtained earlier as part of their standard of care, alongside serial ctDNA-based testing that was done later when subsequent lines of therapy were being decided. The median duration of initial prior anti-EGFR therapy was around 10 months. Known acquired mechanisms of resistance were noted in 100% of the cases. These included KRAS, NRAS, extracellular domain mutations in EGFR, and BRAF mutations. Interestingly, the levels of the sub-clones expressed in variant allele fraction percentage varied and decreased over time in relation to timing of the prior EGFR exposure. Additionally, these were noted to be polyclonal, and the number of clones also varied including some disappearing over time during non-EGFR-based therapy (EGFR holiday). Patients’ post-EGFR blockade may have multiple mechanisms of acquired resistance that can be easily detected on non-invasive liquid biopsies. These patients do not benefit from EGFR rechallenge based on the results of the recently reported CRICKET (NCT02296203) and CAVE (NCT04561336) clinical trials. Furthermore, excluding these patients from EGFR rechallenge is already being adopted in prospectively done clinical trials, e.g., the CHRONOS study (NCT03227926). Rechecking the liquid biopsy plasma RAS/RAF status is one thing that may be incorporated into practice with EGFR rechallenge only a consideration if acquired mechanisms of resistance are absent.
Introduction
Advanced colorectal cancer (CRC) patients with a RAS/RAF wild-type status obtain significant benefits from anti-epidermal growth factor receptor antibody (anti-EGFR) therapy in combination with chemotherapy (1–5). Sidedness plays an important role with its approval as first-line therapy only in left-sided tumors, and with subsequent lines among the right-sided tumors (6). Unfortunately, like any targeted therapy, these tumors develop secondary acquired mechanisms of resistance. For patients with metastatic RAS/RAF wild-type refractory colorectal cancer, the question of anti-EGFR therapy rechallenge often comes up after initial use. However, not all patients derive benefit. It is now well known that these tumors acquire mechanisms of resistance in the mitogen-activated protein kinase (MAPK) pathway, which can be detected on circulating tumor DNA (ctDNA)-based testing (6, 7).
Solid tumors change over time and space from clonal evolution, causing significant intra-tumor genetic heterogeneity, contributing resistance to chemotherapy and biologics. When patients have disease progression after first-line combination chemotherapy and anti-EGFR therapy, knowing the mechanism(s) of resistance can be important. Patients who developed resistance to chemotherapy can continue with anti-EGFR therapy with a change in the chemotherapy backbone (8–10). Eventually, patients develop resistance to targeted therapy from selection pressure resulting in disease progression. When patients have a break from targeted therapy, tumors can potentially get resensitized to anti-EGFR therapy by a reduction in clonal selection pressure, as depicted in Figure 1. These patients would potentially derive more benefit from targeted therapy, rather than the broad rechallenge among all patients who are progressing. Rechallenge with anti-EGFR therapy in combination with multiple therapies was evaluated in several retrospective and prospective studies (12–16).
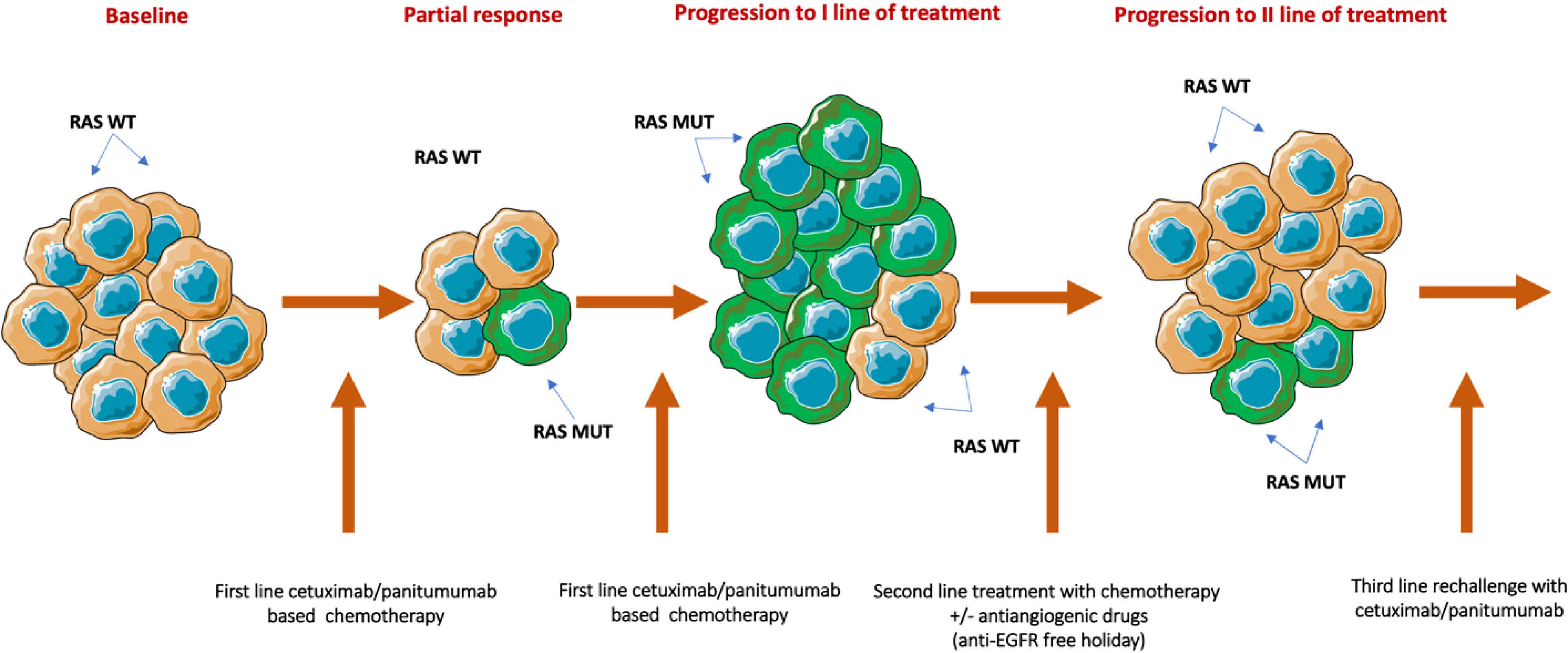
Figure 1 Biological rationale for rechallenge therapy. Treatment with anti-EGFR inhibitors rapidly eliminates RAS WT-sensitive clones and favors the expiation of resistant cancer cells. After disease progression, and due to the administration of a second line of chemotherapy without anti-EGFR monoclonal antibodies, RAS mutant clones progressively decay, inducing the proliferation of RAS WT cell. WT, Wild type; MUT, Mutant;/: Or. [Published with permission from Cancers 2021, 13(8), 1941: open access (11)].
Tissue biopsy to identify the clonal status in the tumor is limited by the procedural risk and availability of enough tissue. Liquid biopsies are gaining importance in capturing tumor heterogeneity, negating the procedural risk. The testing involves circulating or cell-free DNA testing in the circulation, represented by circulating tumor DNA when the origin is from tumor tissue. Liquid biopsy may better assess tumor heterogeneity as ctDNA is released into circulation by the primary tumor and the multiple metastatic sites. Among colorectal cancer patients, various studies have shown that above 20% (17) have difficulty obtaining tissue for molecular analysis, while 15% of patients had no shedding of ctDNA (18–20). Negative ctDNA could be secondary to low tumor volume or the timing of testing, such as post-chemotherapy or postoperative periods. The reliability of liquid biopsy to determine tumor evolution is depicted in the recent CAVE (14), CRICKET (13), and CHRONOS clinical trials (15) and is currently under evaluation in REMARRY/PURSUIT trials (21).
We present a series of patients who had serial testing post EGFR blockade showing its feasibility and value. This would have implications for EGFR rechallenge.
Materials and Methods
This is a retrospective study. After the approval from the Institutional Review Board (IRB), records for patients who were initially noted to be RAS/RAF wild-type on tissue eligible to receive anti-EGFR therapy from 2019 to 2021 were reviewed. We used two commercially available liquid biopsy circulating tumor DNA (ctDNA) platforms that are next-generation sequencing (NGS) based. The choice of the assay was more so due to institutional preference and/or insurance coverage for one assay or the other. Both Tempus xF and Guardant360 assays are CLIA approved. The Guardant360 assay is also US FDA approved. Both assays have numerous validity, concordance, and studies relating to sensitivity and specificity of these assays.
There is little concern regarding the ability of these ctDNA-based platforms with respect to detecting mutations. They are both based on hybrid capture NGS testing, which facilitates broader gene sequencing than hot spot-based NGS amplification with an extensive repertoire for detecting aberrations. Fusions are large gene rearrangements that can also be seen post EGFR challenge. When detected, it is highly specific for these aberrations (22). However, absence of this on the reports does not rule out the presence of fusions (23). This work pertains to more so mutations that were detected post EGFR challenge.
Sequencing and Analysis
G360 (Guardant Health, Redwood City, CA, USA) is a commercially available 74-gene panel plasma-based tumor genomic profiling assay validated to detect a variety of genomic alterations including MSI-H signature (24), single-nucleotide variants, indels, and copy number alterations (amplifications and fusions) (23) in cell-free DNA (cfDNA) from plasma of patients with solid tumors, including colorectal cancer.
The Tempus xF assay (25) assay detects SNVs and indels in 105 genes, CNVs in 8 genes, and chromosomal rearrangements/fusions for 7 genes by DNA-Seq. The average depth of coverage is 5,000 unique reads per 20,000 raw reads.
Patients were followed with ctDNA at multiple variable time points while on therapy for clonal evolution of resistance to anti-EGFR therapy. The resistance was determined through the appearance of mutations in the MAPK pathway (RAS, RAF, and EGFR domain mutations), which are not present during prior ctDNA testing.
Results
Upon reviewing, we found six patients who met the inclusion criteria. Table 1 shows results of the patients’ tissue-based genomic testing in parallel with the serial circulating tumor DNA-based testing that was done during the time of follow-up scans and/or when subsequent lines of therapy were being decided. The median duration of anti-EGFR therapy was around 10 months. Resistance to anti-EGFR therapy is by constitutive activation of EGFR downstream signaling pathways regardless of EGFR blockade predominantly through KRAS, NRAS, BRAF, and extracellular domain mutations in EGFR (26). HER2/ERBB2 aberrations were also noted. As noted in Table 1 the known acquired mechanisms of resistance were noted in 100% of the cases. Interestingly, the levels of the sub-clones expressed in variant allele fraction percentage varied and decreased over time in relation to the timing of the prior EGFR exposure. Additionally, these were noted to be polyclonal, and the number of clones also varied over time. Some clones disappeared over time during the non-EGFR-based therapy (EGFR holiday such as KRAS clones in patient 2, BRAF clones in patient 3, and EGFR clones in patient 4. Anti-EGFR therapy was only attempted in patients who had no known RAS/RAF resistance clones, which did lead to a response lasting 4 months (8 cycles) in 2 of these 6 patients.
Discussion
Precision medicine and utilization of targeted therapy are increasingly gaining importance in the modern therapeutic landscape. ctDNA is gaining significant momentum in aiding important clinical decisions in utilization of the targeted therapies. An earlier study by Ciardiello et al. from the CAPRI-GOIM trial included tissue-based NGS testing to identify patients without downstream mutations depicting benefit with anti-EGFR therapies (27). The combination therapy showed an objective response rate (ORR) of 62.0% (95% CI 55.5%–74.6%) with a median progression-free survival (mPFS) of 11.1 (95% CI 9.2–12.8) months in patients with KRAS and NRAS wild-type tumors. Patients with KRAS or NRAS mutations had a significantly lower ORR of 46.6% (95% CI 39.9–57.5%) with mPFS of 8.9 (95% CI 7.4–9.6) months. Further, retrospectively designed studies show that ctDNA detected KRAS and/or EGFR mutations in patients unresponsive to anti-EGFR treatment (19, 28). The presence of such clones was associated with shorter PFS in comparison with no mutations (3 versus 8 months, P = 0.0004). There were multiple simultaneous mutations in KRAS and EGFR in the ctDNA with a decrease in decline in variable allele frequency (VAF) after stopping the therapy (19). Our study shows a similar evolution of resistance clones with a decline in their VAF by following these patients through their course of anti-EGFR therapy, building further confidence in utilization of ctDNA, a reliable marker for day-to-day clinical decision making (12).
At present, there are several prospective studies that have reported on the importance of determining the RAS/RAF status on the liquid/plasma determining response to targeted therapies. The first landmark observations came from the CRICKET and CAVE clinical trials (29, 30), which both showed a lack of benefit of anti-EGFR therapy in patients who had these acquired mechanisms of resistance detected in plasma. These led to a recent study called CHRONOS that just got reported out and presented at the American Society of Clinical Oncology (ASCO) meeting in June 2021, whereby patients were actually excluded if they had their resistance mechanisms detected in the blood. This led to a clinically meaningful ORR of 30% (95% CI: 12%–47%), a DCR (PR plus SD > 4 months) of 59% (95% CI: 41%–78%), and an mPFS of 16 weeks. Large retrospective series demonstrated ctDNA utilization in detecting NTRK1 (31), RET, and FGFR3 fusions (22) apart from subclonal RAS and EGFR mutations which were hypothesized to contribute to anti-EGFR resistance (32). Such mechanisms need to be studied in prospective fashion to determine treatment implications with specific targeted agents.
Our study reports on the real-time utility and feasibility of incorporating the evaluation of ctDNA liquid RAS/RAF/EGFR and the status of other relevant resistance mutations in blood in patients with prior anti-EGFR exposure and tissue RAS/RAF-wild-type tumor. Given the lack of benefit of anti-EGFR therapy in patients whose liquid biopsies reveal known resistance mechanisms to these drugs, it makes sense not to use these drugs in those patients at that point in time. Given that there is exponential decay that can happen potentially on EGFR holiday, the liquid RAS/RAF/EGFR status could later be rechecked to guide the optimal timing of EGFR rechallenge.
Conclusion
In summary, here we report on a case series illustrating the feasibility of obtaining ctDNA in real time to assess for the presence or absence of acquired resistance mutations. These were present in 100% of the patients initially, with decay over time allowing for rechallenge. With several clinical trials now reporting on the lack of benefit in patients who have these resistance mutations, assessment of this prior to EGFR rechallenge would be a consideration to include in guidelines.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by the University of Iowa Institutional Review Board. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
The authors confirm contribution to the paper as follows: study conception and design: PK; data collection: AC; analysis and interpretation of results: AC; draft manuscript preparation: AC and PK. All authors contributed to the article and approved the submitted version.
Conflict of Interest
Author PMK: Consulting/Advisory Board: Merck/MSD, Servier, Delcath, Foundation Medicine, Taiho (self/institution), Tempus, QED, Eli Lilly, Daiiche Sankyo, Bayer, Incyte, Eisai, Natera, Exact Sciences, Ipsen (institution). Research support to institution: BTG/Boston Scientific, AstraZeneca, Tersera, RenovoRX.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Carrato A, Abad A, Massuti B, Grávalos C, Escudero P, Longo-Muñoz F, et al. First-Line Panitumumab Plus FOLFOX4 or FOLFIRI in Colorectal Cancer With Multiple or Unresectable Liver Metastases: A Randomised, Phase II Trial (PLANET-TTD). Eur J Cancer (2017) 81:191–202. doi: 10.1016/j.ejca.2017.04.024
2. Douillard JY, Siena S, Cassidy J, Tabernero J, Burkes R, Barugel M, et al. Final Results From PRIME: Randomized Phase III Study of Panitumumab With FOLFOX4 for First-Line Treatment of Metastatic Colorectal Cancer. Ann Oncol (2014) 25(7):1346–55. doi: 10.1093/annonc/mdu141
3. Pietrantonio F, Cremolini C, Petrelli F, Di Bartolomeo M, Loupakis F, Maggi C, et al. First-Line Anti-EGFR Monoclonal Antibodies in panRAS Wild-Type Metastatic Colorectal Cancer: A Systematic Review and Meta-Analysis. Crit Rev Oncol Hematol (2015) 96(1):156–66. doi: 10.1016/j.critrevonc.2015.05.016
4. Van Cutsem E, Lenz H-J, Köhne C-H, Heinemann V, Tejpar S, Melezínek I, et al. Fluorouracil, Leucovorin, and Irinotecan Plus Cetuximab Treatment and RAS Mutations in Colorectal Cancer. J Clin Oncol (2015) 33(7):692–700. doi: 10.1200/JCO.2014.59.4812
5. Heinemann V, von Weikersthal LF, Decker T, Kiani A, Vehling-Kaiser U, Al-Batran S-E, et al. FOLFIRI Plus Cetuximab Versus FOLFIRI Plus Bevacizumab as First-Line Treatment for Patients With Metastatic Colorectal Cancer (FIRE-3): A Randomised, Open-Label, Phase 3 Trial. Lancet Oncol (2014) 15(10):1065–75. doi: 10.1016/S1470-2045(14)70330-4
6. NCCN. Colon Cancer (2021). Available at: https://www.nccn.org/professionals/physician_gls/pdf/colon.pdf.
7. Venook AP, Niedzwiecki D, Lenz H-J, Innocenti F, Fruth B, Meyerhardt JA, et al. Effect of First-Line Chemotherapy Combined With Cetuximab or Bevacizumab on Overall Survival in Patients With KRAS Wild-Type Advanced or Metastatic Colorectal Cancer: A Randomized Clinical Trial. JAMA (2017) 317(23):2392–401. doi: 10.1001/jama.2017.7105
8. Blondy S, David V, Verdier M, Mathonnet M, Perraud A, Christou N, et al. 5-Fluorouracil Resistance Mechanisms in Colorectal Cancer: From Classical Pathways to Promising Processes. Cancer Sci (2020) 111(9):3142–54. doi: 10.1111/cas.14532
9. Hammond WA, Swaika A, Mody K. Pharmacologic Resistance in Colorectal Cancer: A Review. Ther Adv Med Oncol (2016) 8(1):57–84. doi: 10.1177/1758834015614530
10. Siravegna G, Mussolin B, Buscarino M, Corti G, Cassingena A, Crisafulli G, et al. Clonal Evolution and Resistance to EGFR Blockade in the Blood of Colorectal Cancer Patients. Nat Med (2015) 21(7):795–801. doi: 10.1038/nm.3870
11. Ciardiello D, Martini G, Famiglietti V, Napolitano S, De Falco V, Troiani T, et al. Biomarker-Guided Anti-Egfr Rechallenge Therapy in Metastatic Colorectal Cancer. Cancers (Basel) (2021) 13(8):3. doi: 10.3390/cancers13081941
12. Santini D, Vincenzi B, Addeo R, Garufi C, Masi G, Scartozzi M, et al. Cetuximab Rechallenge in Metastatic Colorectal Cancer Patients: How to Come Away From Acquired Resistance? Ann Oncol (2012) 23(9):2313–8. doi: 10.1093/annonc/mdr623
13. Cremolini C, Rossini D, Dell’Aquila E, Lonardi S, Conca E, Del Re M, et al. Rechallenge for Patients With RAS and BRAF Wild-Type Metastatic Colorectal Cancer With Acquired Resistance to First-Line Cetuximab and Irinotecan: A Phase 2 Single-Arm Clinical Trial. JAMA Oncol (2019) 5(3):343–50. doi: 10.1001/jamaoncol.2018.5080
14. Martinelli E, Martini G, Famiglietti V, Troiani T, Napolitano S, Pietrantonio F, et al. Cetuximab Rechallenge Plus Avelumab in Pretreated Patients With RAS Wild-Type Metastatic Colorectal Cancer: The Phase 2 Single-Arm Clinical CAVE Trial. JAMA Oncol (2021) 7(10):1529–35. doi: 10.1001/jamaoncol.2021.2915
15. Sartore-Bianchi A, Pietrantonio F, Lonardi S, Mussolin B, Rua F, Fenocchio E, et al. Phase II Study of Anti-EGFR Rechallenge Therapy With Panitumumab Driven by Circulating Tumor DNA Molecular Selection in Metastatic Colorectal Cancer: The CHRONOS Trial. J Clin Oncol (2021) 39(15_suppl):3506–6. doi: 10.1200/JCO.2021.39.15_suppl.3506
16. Sunakawa Y, Nakamura M, Ishizaki M, Kataoka M, Satake H, Kitazono M, et al. RAS Mutations in Circulating Tumor DNA and Clinical Outcomes of Rechallenge Treatment With Anti-EGFR Antibodies in Patients With Metastatic Colorectal Cancer. JCO Precis Oncol (2020) 4):898–911. doi: 10.1200/PO.20.00109
17. Meric-Bernstam F, Brusco L, Shaw K, Horombe C, Kopetz S, Davies MA, et al. Feasibility of Large-Scale Genomic Testing to Facilitate Enrollment Onto Genomically Matched Clinical Trials. J Clin Oncol (2015) 33(25):2753–62. doi: 10.1200/JCO.2014.60.4165
18. Bettegowda C, Sausen M, Leary RJ, Kinde I, Wang Y, Agrawal N, et al. Detection of Circulating Tumor DNA in Early- and Late-Stage Human Malignancies. Sci Trans Med (2014) 6(224):224ra24–224ra24. doi: 10.1126/scitranslmed.3007094
19. Morelli MP, Overman MJ, Dasari A, Kazmi SMA, Mazard T, Vilar E, et al. Characterizing the Patterns of Clonal Selection in Circulating Tumor DNA From Patients With Colorectal Cancer Refractory to Anti-EGFR Treatment. Ann Oncol (2015) 26(4):731–6. doi: 10.1093/annonc/mdv005
20. Strickler JH, Loree JM, Ahronian LG, Parikh AR, Niedzwiecki D, Pereira AAL, et al. Genomic Landscape of Cell-Free DNA in Patients With Colorectal Cancer. Cancer Discov (2018) 8(2):164–73. doi: 10.1158/2159-8290.CD-17-1009
21. Nakajima H, Kotani D, Bando H, Kato T, Oki E, Shinozaki E, et al. REMARRY and PURSUIT Trials: Liquid Biopsy-Guided Rechallenge With Anti-Epidermal Growth Factor Receptor (EGFR) Therapy With Panitumumab Plus Irinotecan for Patients With Plasma RAS Wild-Type Metastatic Colorectal Cancer. BMC Cancer (2021) 21(1):674. doi: 10.1186/s12885-021-08395-2
22. Clifton K, Rich TA, Parseghian C, Raymond VM, Dasari A, Pereira AAL, et al. Identification of Actionable Fusions as an Anti-EGFR Resistance Mechanism Using a Circulating Tumor DNA Assay. JCO Precis Oncol (2019) 3):1–15. doi: 10.1200/PO.19.00141
23. Odegaard JI, Vincent JJ, Mortimer S, Vowles JV, Ulrich BC, Banks KC, et al. Validation of a Plasma-Based Comprehensive Cancer Genotyping Assay Utilizing Orthogonal Tissue- and Plasma-Based Methodologies. Clin Cancer Res (2018) 24(15):3539–49. doi: 10.1158/1078-0432.CCR-17-3831
24. Willis J, Lefterova MI, Artyomenko A, Kasi PM, Nakamura Y, Mody K, et al. Validation of Microsatellite Instability Detection Using a Comprehensive Plasma-Based Genotyping Panel. Clin Cancer Res (2019) 25(23):7035–45. doi: 10.1158/1078-0432.CCR-19-1324
25. Finkle JD, Boulos H, Driessen TM, Lo C, Blidner RA, Hafez A, et al. Validation of a Liquid Biopsy Assay With Molecular and Clinical Profiling of Circulating Tumor DNA. NPJ Precis Oncol (2021) 5(1):63. doi: 10.1038/s41698-021-00202-2
26. Zhao B, Wang L, Qiu H, Zhang M, Sun L, Peng P, et al. Mechanisms of Resistance to Anti-EGFR Therapy in Colorectal Cancer. Oncotarget (2016) 8(3):3980–4000. doi: 10.18632/oncotarget.14012
27. Ciardiello F, Normanno N, Maiello E, Martinelli E, Troiani T, Pisconti S, et al. Clinical Activity of FOLFIRI Plus Cetuximab According to Extended Gene Mutation Status by Next-Generation Sequencing: Findings From the CAPRI-GOIM Trial. Ann Oncol (2014) 25(9):1756–61. doi: 10.1093/annonc/mdu230
28. Vidal J, Muinelo L, Dalmases A, Jones F, Edelstein D, Iglesias M, et al. Plasma ctDNA RAS Mutation Analysis for the Diagnosis and Treatment Monitoring of Metastatic Colorectal Cancer Patients. Ann Oncol (2017) 28(6):1325–32. doi: 10.1093/annonc/mdx125
29. Mayer RJ, Van Cutsem E, Falcone A, Yoshino T, Garcia-Carbonero R, Mizunuma N, et al. Randomized Trial of TAS-102 for Refractory Metastatic Colorectal Cancer. N Engl J Med (2015) 372(20):1909–19. doi: 10.1056/NEJMoa1414325
30. Li J, Qin S, Xu R, Yau TCC, Ma B, Pan H, et al. Regorafenib Plus Best Supportive Care Versus Placebo Plus Best Supportive Care in Asian Patients With Previously Treated Metastatic Colorectal Cancer (CONCUR): A Randomised, Double-Blind, Placebo-Controlled, Phase 3 Trial. Lancet Oncol (2015) 16(6):619–29. doi: 10.1016/S1470-2045(15)70156-7
31. Rolfo C, Drilon A, Hong D, McCoach C, Dowlati A, Lin JJ, et al. NTRK1 Fusions Identified by non-Invasive Plasma Next-Generation Sequencing (NGS) Across 9 Cancer Types. Br J Cancer (2022) 126(3):514–20. doi: 10.1038/s41416-021-01536-1
32. Mauri D, Kamposioras K, Matthaios D, Tolia M, Nixon I, Dambrosio M, et al. Next-Generation Sequencing of Circulating Tumor DNA Can Optimize Second-Line Treatment in RAS Wild-Type Metastatic Colorectal Cancer After Progression on Anti-EGFR Therapy: Time to Rethink Our Approach. Oncol Res Treat (2022) 45(4):216–21. doi: 10.1159/000521845
Keywords: anti-EGFR therapy, ctDNA, rechallenge, metastatic colorectal cancer, cetuximab, panitumumab, tumor heterogeneity, evolution
Citation: Chennamadhavuni A and Kasi PM (2022) Circulating Tumor DNA in Identifying Resistant Sub-Clones Post EGFR Blockade: Implications for EGFR Rechallenge. Front. Oncol. 12:847299. doi: 10.3389/fonc.2022.847299
Received: 01 January 2022; Accepted: 02 May 2022;
Published: 28 June 2022.
Edited by:
Alfonso de Stefano, G. Pascale National Cancer Institute Foundation (IRCCS), ItalyReviewed by:
Francesco Pepe, University of Naples Federico II, ItalyAlessandro Russo, A.O. Papardo, Italy
Copyright © 2022 Chennamadhavuni and Kasi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Pashtoon Murtaza Kasi, cG1rNDAwMUBtZWQuY29ybmVsbC5lZHU=
 Adithya Chennamadhavuni
Adithya Chennamadhavuni Pashtoon Murtaza Kasi
Pashtoon Murtaza Kasi