- 1Department of Obstetrics and Gynecology, Shengjing Hospital of China Medical University, Shenyang, China
- 2Key Laboratory of Maternal-Fetal Medicine of Liaoning Province, Key Laboratory of Obstetrics and Gynecology of Higher Education of Liaoning Province, Shenyang, China
The mammary gland is closely related to the female reproductive system in many aspects, affecting the whole gynecological system. Breast cancer (BC) is the most common malignancy in women and associated with considerable negative effects. Due to various factors including co-pathogenic genetic mutations, environment factors, lifestyle, behavioral factors, treatment regimens and in-creased survival of patients with BC, there is an increased probability of developing additional primary gynecologic cancers such as ovarian cancer (OC), endometrial cancer (EC), and cervical cancer (CC). More and more studies have been conducted in recent years. Multiple primary cancers (MPCs), also known as multiple primary malignancies, refers to two or more different primary cancers in the same patient occurring in the same or different organs or tissues. The pathogenesis of multiple primary cancers is complex and has a negative effect on the prognosis and survival of patients. This review discusses the common types of BC-associated MPCs, namely, BC associated with OC, BC associated with EC and BC associated with CC, as well as risk factors, pathogenesis, treatment, and prognosis of MPCs associated with breast and gynecologic cancers. It provides new intervention and treatment ideas for patients with BC-associated MPCs to improve quality of life and prognosis.
Introduction
Breast cancer (BC) is the most common malignancy in women and is associated with considerable negative effects (1–6). Its 5-year incidence is approximately 43.8 million cases worldwide (7). Despite its increasing incidence in recent years (8), the mortality rate of women with BC has been decreasing (9, 10) due to early screening and continuous improvement in treatment (11).
Multiple primary cancers (MPCs), also known as multiple primary malignancies, refer to two or more different primary cancers in the same patient occurring in the same or different organs or tissues (12). The most common sites are paired organs, especially the breasts, gastrointestinal tract, and thyroid gland (13). Double primary cancer is the most common type of MPCs (14), whereas the incidence of quadruple primary cancer is only <0.1% (15).
The incidence of MPCs associated with BC is also increasing (16) due to increased patient survival (17), genetic susceptibility, environmental interactions, as well as chemotherapy, seriously affecting the quality of life and prognosis of patients. The incidence of a secondary primary cancer after BC is between 4% and 16% (18), which is approximately 17% higher than in healthy women (19), with the most common types being thyroid cancer, gynecological malignancy, etc. (16, 20, 21) (Figure 1). As shown in Figure 1, the blue (22) represents a cohort study of 21, 527 patients with BC at cancer centers in Italy from the European Institute of Oncology. The orange (20) represents a cohort study of patients with BC and other primary cancers in Israel National Cancer Registry between 1992 and 2006. The data does not include follow-up information after 6 months of BC diagnosis. The gray (23) represents patients aged 50 to 59 years with BC and other primary cancers in the SEER Cancer Registry. The data on brain cancer are not available. It can be inferred that the most common gynecologic cancers among the BC-associated MPCs include ovarian cancer(OC), endometrial cancer(EC) and cervical cancer(CC).
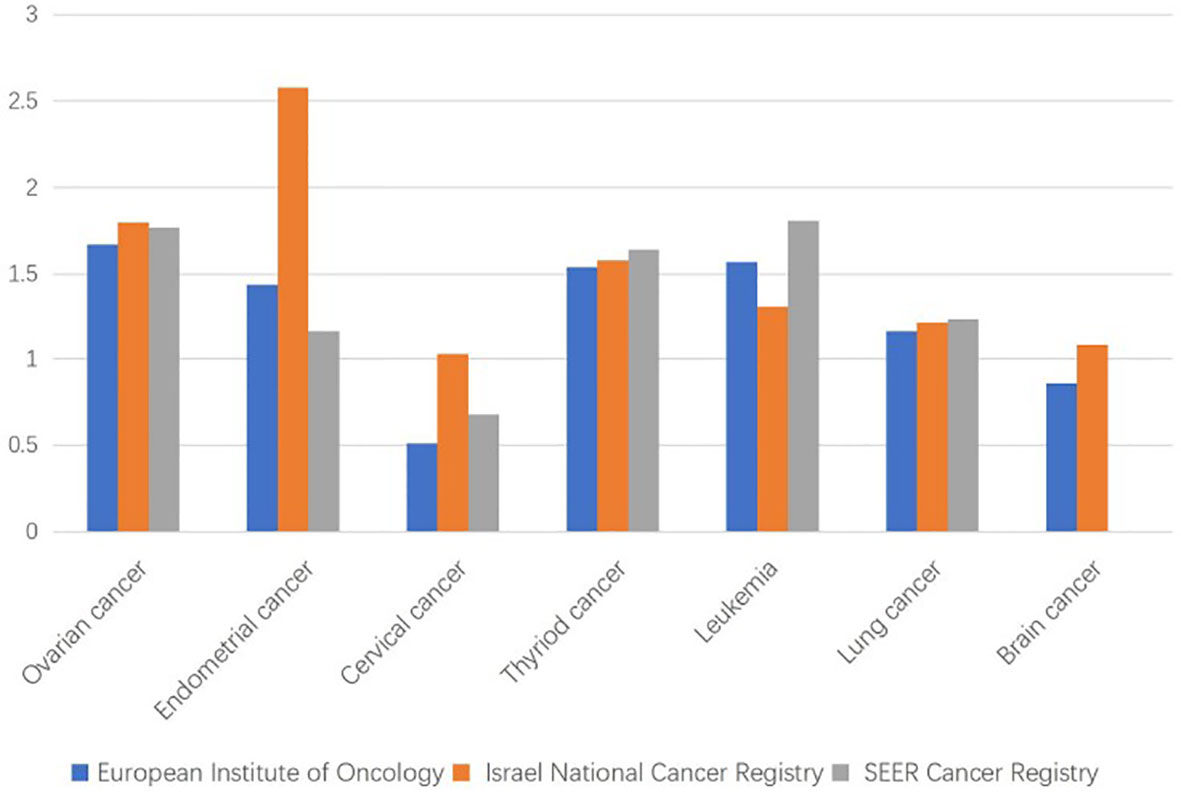
Figure 1 Standardized incidence ratios for common multiple primary cancer sites associated with breast cancer (BC).
The mammary glands are closely related to the female reproductive system; therefore, gynecologic malignancies are also the most common primary cancer after BC (24). Multiple studies have shown that among the MPCs associated with BC, female reproductive malignancies such as OC, EC, and CC are the most common malignancies (25–28), which is consistent with the inference mentioned in the previous paragraph.
In recent years, although evidence about the pathogenesis, treatment, prognosis, and survival in BC associated with gynecologic malignancies has increased, there is still a need for a comprehensive review. In this review, we discuss three common types of MPCs associated with BC, namely, BC associated with OC, EC, and CC, as well as risk factors, pathogenesis, treatment, and prognosis of MPCs associated with breast and gynecologic cancers. The aim is to provide new intervention and treatment ideas for patients with MPCs associated with breast and gynecological malignancies to improve quality of life and prognosis.
MPCs Associated With BC and OC
Early studies have shown that BC is associated with an increased risk of developing OC (29) and that OC is the most common primary malignancy after BC (30). Recently, Nasioudis et al. found that the incidence of BC increases after the incidence of ovarian granulosa cell tumor (31). The risk factors for MPCs are mostly genetic (32). In 1994, Ford et al. established the fact that the carriers of the BRCA-1 mutation are more likely to develop BC and OC (33), and mutations in the BRCA genes are generally linked to BC and OC (34–36). Through large-scale sequencing, Lu et al. recently identified genes including MSH6 and ATM as genes that increase an individual’s susceptibility to BC and OC (37). In the same year, Samadder et al. found that a disease-causing mutation in PALB2 was associated with a medium-high risk of developing BC and OC (38). CDKN2A mutations have also been detected in both cancers (39). Furthermore, Peutz–Jeghers syndrome, which is caused by STK11 mutation, results in malignant changes in the mammary glands and ovaries (13). According to a family-based study conducted in 2020, variations in RAD51C and RAD52D are correlated with an increased risk of developing BC and OC (40). In conclusion, the mutation of some co-pathogenic genes associated with the breasts and ovaries can induce MPCs in these organs.
Regarding the common clinicopathological classification of BC associated with primary OC, studies have reported that BC and epithelial OC have similar risk factors (41). Therefore, patients with one type of cancer have an increased risk of developing other cancers in future. Studies have shown that patients with BRCA1 and BRCA2 mutations are susceptible to developing BC associated with OC, and the probability of developing epithelial-type BC is higher, as is that of developing the histological subtype of serous OC (38, 42–44). Regarding molecular typing, BRCA1-associated BC is of the medullary subtype with a high proportion of negative estrogen and progesterone receptor expression (43, 45). BRCA2-associated BC is similar to luminal-type tumors. Patients with triple-negative BC are more likely to develop primary OC (22). In addition, Bryk et al. reported that the standardized incidence of primary BC in patients with adult granulosa cell tumors (AGCTs) was 1.26 (95% CI: 0.92–1.73) and that of AGCTs after BC was 1.59 (95% CI: 1.04–2.29) (46). Therefore, the prevention and treatment of BC should be considered in the follow-up examination along with identification of patients with AGCT.
Studies show that BC is most likely to develop in the first few years after OC diagnosis (47), and after 10 years, the risk of developing BC is 7.8% (48). Additionally, OC is the most common primary cancer after BC (30). Therefore, regardless of the primary origin, patients with hereditary breast and ovarian cancer should undergo regular screening in the first few years after diagnosis so that timely intervention and treatment are provided to improve prognosis and quality of life (49). Several studies have reported that mastectomy after OC in patients with BRCA mutations reduces the risk of developing BC (45, 48, 50). Thus, prophylactic mastectomy, which reduces the risk of developing BC by 90%, should be considered for BRCA1/2 mutation carriers to improve prognosis (50). In addition to the cancer antigen 125 test (50) performed every 6 months, use of oral contraceptives as well as prophylactic salpingectomy and oophorectomy can lower the risk of developing OC (38, 51, 52). Moreover, prophylactic salpingo-oophorectomy is associated with a reduced risk of developing BC (53).
Regarding treatment type, studies have shown that patients with BRCA mutations who are treated with cisplatin have higher complete response rates than those treated with other chemotherapy regimens (54). Moreover, in recent years, studies have shown that BRAC1 mutations are associated with an increased expression of PD-L1 and PD-1 (55); this suggests that checkpoint inhibitors have an effect on BRCA-associated cancers (43), thereby providing a new treatment approach for MPCs associated with BC and OC.
In conclusion, screening should be regularly performed for patients with genetic mutations who are susceptible to developing primary BC and OC, and prophylactic mastectomy/salpingo-oophorectomy and drug therapy should be considered for risk reduction.
MPCs Associated With BC and EC
EC is a common secondary primary cancer among patients with BC (56), and the causes of this combination of MPCs are complex. In terms of the common pathogenic genes, Guo et al. recently reported that mutations of p53, HER-2, and other genes are related to the incidence of both BC and EC (57). Kim et al. found that IMP3, which is associated with triple-negative BC, is also related to type II EC (58). In addition, Cowden syndrome (also known as multiple hamartoma syndrome) is often associated with thyroid cancer, BC, and EC and is caused by a PTEN mutation, which also increases the risk of developing EC in patients with BC (59), making them susceptible to MPCs (60). Studies have confirmed that the long non-coding RNA, NR2F1-AS1, can promote BC and EC progression (61), becoming a co-pathogenic factor for both types of cancer, and is possibly one of the causes of BC associated with primary EC.
Obesity-related diseases can promote the occurrence and development of BC and EC. It is well known that metabolic syndrome is closely related to EC (62), considering that most patients with metabolic syndrome show signs of obesity. The presence of aromatase in the excessive adipose tissue of patients leads to the transformation of androgens into estrogens (63), resulting in the rise of estrogens in patients; abnormal estrogen levels are also driving factors leading to BC (64). In addition to its effects on estrogen levels, metabolic syndrome can also lead to hyperinsulinemia (65), which can increase the level of insulin-like growth factor-1 (IGF-1). IGF-1 expression was increased in both BC and EC cells (66, 67). The possible mechanism is that the overexpression of insulin growth factor receptor-1R (IGF-1R) or insulin receptor (IR) leads to mitotic signaling and increases the activation of phosphoinositide-3-kinase (PI3)-Akt-mTOR signaling pathway (68), which mediates the development of BC and EC. In addition, insulin resistance and hyperinsulinemia in type II diabetes mellitus patients lead to an increased incidence of BC and EC (69). Therefore, metabolic disorders of obesity-related diseases or a variety of hybrid effects of obesity are possible factors influencing the pathogenesis of MPCs associated with BC and EC.
BC treatment can also affect the development of EC. Tamoxifen, the most commonly used endocrine therapy for patients with hormone receptor-positive BC (70–72), acts as an estrogen antagonist in the breasts and as an agonist in the uterus (73). Therefore, the use of tamoxifen is closely related to the development of EC (74–77). A study in Denmark showed that the relative risk of developing EC in patients with BC who were treated with tamoxifen was 1.5 (78), and the risk increases significantly with the duration of drug use (79). A study claimed that 70.7% of the patients with BC will be diagnosed with EC within 5 years (57). Tamoxifen increases the risk of developing EC by 2–7 fold, and aggressive EC types with poor prognosis have been observed among tamoxifen users (75). The long-term use of tamoxifen resulted in a 59% higher risk of EC-related death in women who had received it for 5 years or more than in women who had not (80). Therefore, timely baseline tamoxifen screening should be performed in these patients (81) through regular transvaginal ultrasound, endometrial examination, and biopsy (82) to lower the threshold (83), diagnose EC, and detect malignant endometrial changes in a timely manner. Because tamoxifen use can lead to poor outcomes, Chlebowski et al. reported that aromatase inhibitors can reduce the incidence of tamoxifen-related EC (84), and they are effective against tamoxifen-resistant BC due to a different mechanism of action (85).
However, genomic analysis showed that tamoxifen-induced endometrial tumors were not different from those in patients who did not receive tamoxifen (86), and other studies have found that patients with ER(−) PR(−) BC who are the least likely to receive tamoxifen also have a significantly increased risk of developing EC (83). This suggests that tamoxifen is not the only risk factor for EC. In addition to genetic mutations and treatment factors, increased body mass index is associated with an increased risk of developing EC in patients with BC (87, 88).
Uzunlulu et al. reported that the incidence of EC in patients with both ER(+) and HR(−) BC was higher than that in the general population and that the clinicopathological characteristics of both are similar (89). This is consistent with the results reported by Guo et al. who found that the incidence of ER(+) and HR(−) BC associated with EC was 0.33% and 0.30%, respectively, which were approximately 16 and 15 times higher than that in the general population (57). Further, EC after BC was a common MPC, and there were no significant differences in the stage or distribution of pelvic or para-aortic metastases compared with those in patients with primary EC alone (57). The effect of the hormone receptor status on the endometrium in patients with BC requires further investigation.
MPCs Associated With BC and CC
CC accounts for 13.4% of all MPCs. The incidence of CC-associated MPC is increasing, most commonly coexisting with BC, lung cancer, and colorectal cancer (90). The development of CC-associated BC is closely related to human papillomavirus (HPV) infection. The high expression of P16, an indicator of HPV transcriptional activity, increases in malignant breast tissues (91). A case study reported that the same high-risk HPV types with biological activity were found in the breast and cervical tissues of some patients with BC or CC, with HPV18 being the most common type (92). The incidence of high-risk HPV infection in BC is four times higher than that of benign BC (93). suggesting that women with HPV infection-associated CC are also at a risk of developing BC. Patients with surgically treated high-grade cervical intraepithelial neoplasia (CIN 2/3) also have an increased risk of developing HPV infection-associated BC and OC (94). In addition to the independent role of HPV, recent studies have found that it may co-infect with Epstein–Barr virus (EBV) to promote the occurrence and progression of CC, BC, as well as other cancers (95), and co-infection of high-risk HPV and EBV possibly plays an important role in the progression of BC through the ERK1/ERK2 and β-catenin signaling pathways (96). Long-term oral contraceptive use also increases the risk of BC and CC in HPV-infected women (97). Therefore, patients with HPV infection who need to take contraceptives over a long period of time should be made aware of this risk. In particularly, BC patients with HPV infection should be vigilant for CC during treatment.
Moreover, it has been reported that PIN1, an enzyme that changes the conformation of phosphoprotein, is overexpressed in malignant tumors such as BC and CC (98), and that patients with PIN1 overexpression are likely to develop MPCs; such patients should be screened for disease in time. In addition, the treatment of BC patients can also cause a second primary cancer. Thong et al. found that alkylating agents in combination with chemotherapy can lead to the development of malignancies (99), which is consistent with the findings of Hughes et al. who discovered that the use of alkylating agents in combination with chemotherapy in patients with BC contributed to the development of CC (100).
There are few reports on the clinical classification and characteristics of CC-associated BC. As for prognostic markers, it has been reported that the expression level of FGD3 mRNA has prognostic value in BC and cervical squamous cell carcinoma (101).
Since BC accounts for a certain proportion of patients with CC, regular follow-up and detection should be performed on the mammary glands and female reproductive organs of patients with CC.
Risk Factors
In recent years, with the increased survival of cancer patients, the incidence of BC-associated MPCs has also been increasing. And is often caused by common risk factors such as genetic and environmental factors, lifestyle and treatment regimens (102, 103). The prognosis has also been reported and common drugs used to treat these cancers could provide new insights into the treatment of BC-associated MPCs. The following are common risk factors.
Genetic Factors
The occurrence and development of tumor is closely related to DNA damage. The presence of co-pathogenic genetic mutations is likely to lead to the occurrence of MPCs associated with breast and gynecologic cancers. The list of genetic mutations and associated syndromes in MPCs associated with breast and gynecologic cancers is shown in Table 1. In addition, a study reported that microsatellite instability is more common in MPCs than in sporadic cancers (104), demonstrating its likely influence on the pathogenesis of MPCs.
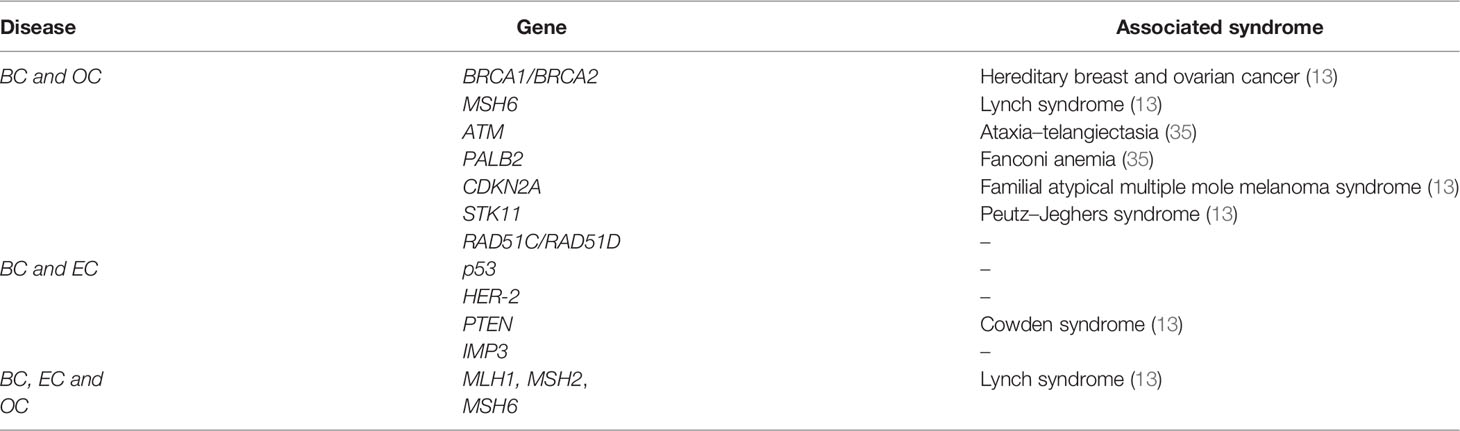
Table 1 List of genetic mutations and associated syndromes in multiple primary malignancies of breast and gynecologic cancers.
Estrogen Factor
Because the mammary gland, uterus, and ovaries have the same estrogen receptors, these areas are simultaneously affected by estrogen-related disturbances. BC is associated with an increased risk of the development of other female reproductive system tumors. Studies have shown that abnormal estrogen levels are closely correlated with BC, EC, OC, and CC in women and are risk factors for many other cancers (85, 105, 106). In addition to abnormal estrogen levels, abnormal estrogen receptor signaling can also contribute to breast, endometrial, and ovarian cancers (106).
Estrogen can lead to different molecular types of BC. One study showed that patients with luminal BC were more likely to develop heterogeneous EC or OC (107), and luminal BC has a strong association with estrogen. If the developmental trend and prognosis of MPCs can be determined by molecular typing of BC, it can provide a clear and efficient treatment plan for these patients.
Lifestyle and Behavioral Factors
Lifestyle and behavioral factors considerably influence the occurrence, development, and treatment of BC-associated MPCs. A high-fat diet can lead to fluctuations in estrogen levels, which can, in turn, lead to the development of OC, BC, and EC (108). Many studies have shown that overweight and obese patients have a higher risk of cancer recurrence (109, 110). For example, most patients with type I EC have metabolic syndrome, which is also associated with BC (111), and bariatric surgery can reduce the risk of developing not only BC but also EC and OC (112). Studies have shown that aromatase in adipose tissue can lead to high estrogen levels, inducing hormone-related cancers such as BC, EC, and OC (113). Adipose tissue is also rich in hormones, cytokines, and other mediators such as leptin and adiponectin, giving rise to a microenvironment that promotes cell proliferation and inflammation (106). Leptin-induced cell signaling cascaded to increase the risk of BC, EC, and OC (114). Therefore, in daily life and in the course of cancer treatment, strict weight management and control should be carried out to maintain the normal metabolism of the body and the normal level of hormones in body, so as to prevent the occurrence of MPCs associated with BC and gynecological cancers.
In addition, smoking is a risk factor contributing to the development of secondary primary cancer (115), and its synergistic relationship with treatment may be associated with the highest risk of secondary primary cancer (109). Quitting smoking after an initial cancer diagnosis may delay the development of secondary primary cancer (116).
Age
In addition to genetic mutations, hormone receptor status, lifestyle and behavioral factors, early age at first diagnosis of BC, and race were also found to be risk factors for primary gynecologic malignancy after BC (117). Young women are more likely to suffer a second primary cancer than women over the age of 50 (118), and second primary cancers of the female reproductive system after BC are also more likely happen to younger women (119). The 10-year survival rate of women aged 20–29 years with BC-associated MPC is approximately 50% lower than that for women with BC alone (23). Therefore, the treatment of these young patients needs additional attention and research.
Treatment Regimens
Treatment is a double-edged sword, it can play a therapeutic role in the first primary cancer, but also can pave the way for the second primary cancer. For example, as mentioned above, tamoxifen, which is used to treat BC, can also cause EC. Otherwise, radiotherapy can also significantly increase the incidence of other primary cancers (109, 120). Berrington de Gonzalez and his team have shown that about 3% of secondary primary cancers in BC survivors are caused by radiation therapy (121), and Grantzau and Overgaard confirmed that patients who have received radiation therapy for BC were 23% more likely to develop another primary cancer (122). Patients with BC who underwent chemotherapy also had a higher standardized incidence of gynecologic malignancies than those who did not undergo chemotherapy (110).
Pathogenesis
To sum up, when the mammary gland and the female reproductive system are exposed to a certain intensity of carcinogenic factors (such as abnormal estrogen levels, terrible lifestyle and behavior patterns, etc.) for a long time, extensive tissue and cells will appear DNA damage, local regional abnormalities and even precancerous lesions (123). The DNA of these cells will be further altered, including oncogene activation and tumor suppressor gene inactivation, by the combined effects of continued oncogenic action or treatment of primary cancer (124) (chemoradiotherapy, hormonal drugs such as tamoxifen, etc.). If the patient has the pathogenic genes associated with BC and gynecologic cancers, the patient is more likely to develop secondary malignant tumors in the final stage, thus forming MPCs with independent and different clonal sources. This indicates that secondary tumors are caused by the human microenvironment similar to that of the first primary cancer, or are closely related to the treatment of the first primary cancer. Simultaneous MPCs can affect the treatment of the first primary cancer in patients. The interaction mechanism between MPCs is complex and diverse, which still needs further research and exploration.
Treatment
BC-associated MPCs is often caused by common risk factors. Therefore, finding the common pathogenic factors and co-therapeutic drugs of these cancers may be a key breakthrough in the treatment of MPCs associated with breast and gynecological cancers. Patients with BC or gynecological cancers should be targeted at the above risk factors for prevention or treatment. Once the second primary cancer is found, radical measures should be taken immediately to intervene in the progression of the disease.
For genetic factors, these patients should be screened for genetic screening, so as to carry out targeted prevention of subsequent cancers. The status of the breasts and reproductive system should be closely monitored during the treatment of patients with BC or gynecologic malignancies, corresponding preventive resection should be carried out when necessary, and radiotherapy or chemotherapy should be carried out according to the condition.
For abnormal estrogen levels, anti-estrogen receptor drugs are widely used to treat these diseases. In recent years, studies have shown that fulvestrant, a selective estrogen receptor degrader, has a strong therapeutic effect in both BC and EC models in vitro and in vivo (125). The use of selective estrogen receptor modulators and selective estrogen receptor degraders to treat MPCs associated with breast and gynecological cancers is undoubtedly a way to improve the prognosis. In addition, studies have found that pigment epithelial derived factor (PEDF) can inhibit the occurrence of tumors in the mammary gland, ovary, endometrium, and other places through the negative regulation of estrogen. PEDF inhibits cell proliferation and reduces cell invasion, and may also prevent drug resistance of BC, EC, and OC by down-regulating estrogen receptors (126).
For obesity, there have been new therapeutic strategies for cancers induced by obesity-related diseases. Multiple studies have shown that metformin can be used as an adjunctive treatment for BC, EC, OC, and other cancers of the female reproductive system, thereby reducing the morbidity and mortality (68, 127–129) (Figure 2). By inhibiting oxidative phosphorylation at the mitochondrial level (OXPHOS), it increases the ratio of adenosine monophosphate (AMP) acid to adenosine triphosphate (ATP) (127), thus activating AMPK and inhibiting several key signaling pathways. For example, activated AMPK inhibits the mTOR signaling pathway and reduces the synthesis of tumor-related proteins (127, 128), thus inhibiting the progression of cancer. It also inhibits IGF-1/IRS-1/PI3K/AKT pathway. It can also lead to the activation of the cellular energy-sensing liver kinase B1 (LKB1)/AMPK pathway. LKB1, as a tumor suppressor, has a negative effect on the occurrence of many tumors (129). In addition, the transcription factor signal converter and transcriptional activator 3 (STAT3) are highly expressed in BC and EC. Metformin can block the phosphorylation of STAT3 and reduce the expression of c-myc, Bcl-2, and other growth promoting targets to inhibit the occurrence and development of these two cancers (127, 128). Therefore, metformin can be used as an effective drug for the treatment of MPCs associated with breast and gynecological cancers, providing a new idea for the treatment of BC-associated MPCs.
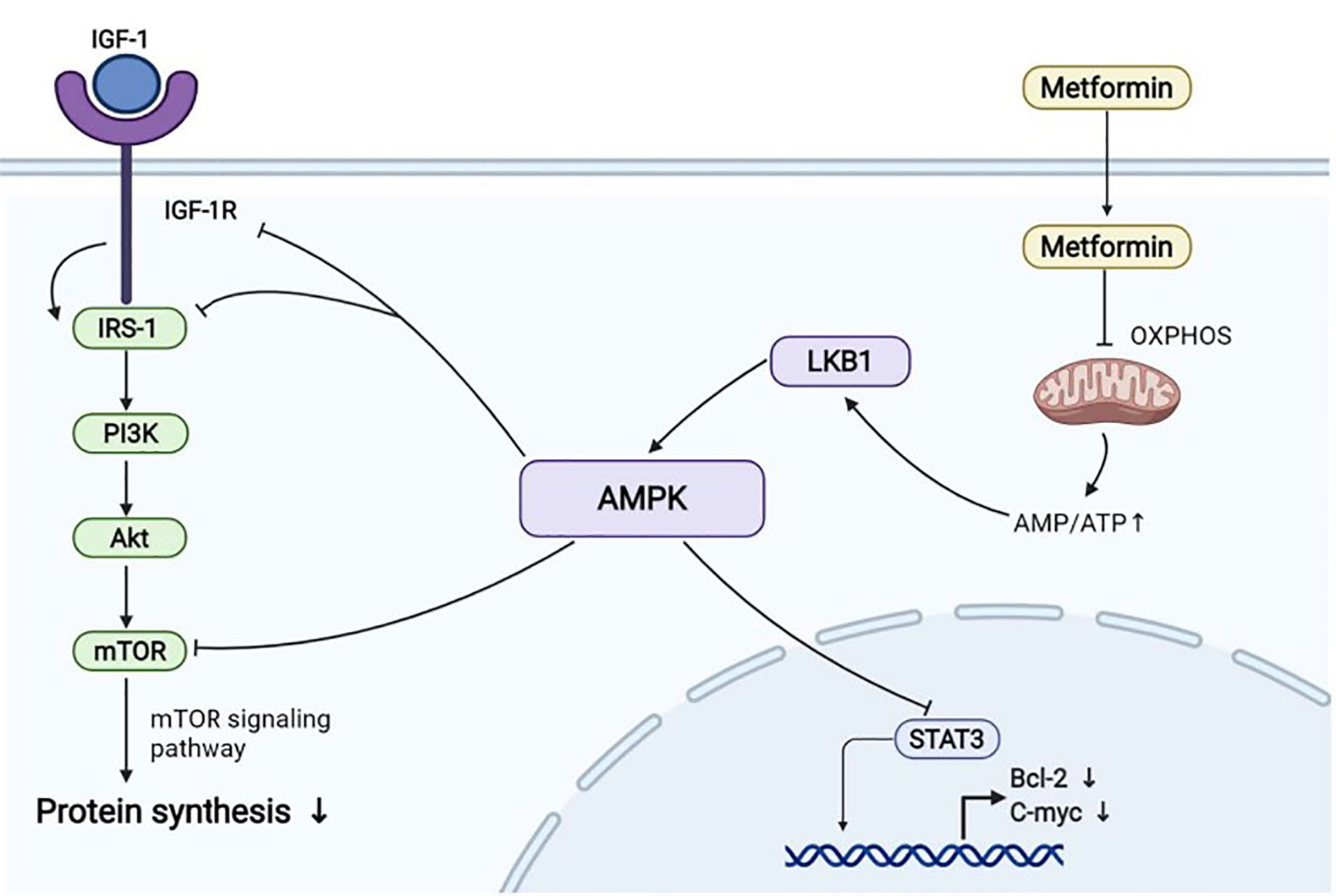
Figure 2 Some of the molecular mechanisms by which metformin inhibits cancer. (Created from BioRender.com.).
In addition to genetic screening and drug therapy, patients should also actively control their weight and quit smoking in time. Young women with BC need additional attention and research.
Otherwise, ibrutinib has been found to have various anti-tumor effects and has been shown to be effective in preclinical studies on OC, BC, and EC cell lines and animal models (130), which is undoubtedly a new treatment option for BC-associated MPCs.
The treatment of patients with MPCs associated with breast and gynecologic cancers is still mainly surgical treatment, supplemented by radiotherapy, chemotherapy, endocrine therapy, and other multidisciplinary comprehensive therapy. Among them, hormone receptor-positive patients should receive endocrine therapy, and through timely, accurate, and suitable treatment, most patients can improve their prognosis and life.
Prognosis
The prognosis of MPCs associated with BC is worse than that of BC alone. The 5-year overall survival rate of BC patients with other primary cancers is about 4.7% lower than that of patients with BC alone (25).
It is worth mentioning that the study by Zhang et al. showed that the 5-year and 10-year overall survival rates of patients with BC after OC were 81.7% and 67.4%, respectively. However, the corresponding overall survival rates of patients with OC without subsequent malignant tumors were 17.0% and 6.5%, respectively (47), which were much lower than those of patients with double primary cancers. This indicates that the prognosis of MPCs is not mainly determined by the number of primary cancers, but by factors such as the patient’s age, cancer stage, pathological type, and malignant degree of the tumor. Individual differences among patients are vast, so the treatment process should be specialized according to the characteristics of different MPCs and patients in order to prolong survival and improve the quality of life.
Discussion
The mammary gland is closely related to the female reproductive system in many aspects, affecting the whole gynecological system. The most common sites of MPCs associated with BC and gynecologic malignancies are the ovary, endometrium, and cervix. Although the incidence of BC associated with gynecologic malignancies is gradually increasing and more studies have been conducted in recent years, further research is required for more insights. The pathogenesis of MPCs is complex and not fully understood. It is related to the patient’s own susceptibility and unhealthy lifestyle, autoimmune deficiency, genetic causes, carcinogenic factors in the surrounding environment, treatment methods such as radiotherapy and chemotherapy. While risk factors such as smoking, alcohol consumption and unhealthy lifestyles can be eliminated, there are uncontrollable and unmodifiable risk factors such as genetic susceptibility and sometimes irreversible effects of anti-cancer treatments.
However, MPCs are often confused with metastasis or recurrence of malignant tumors in clinical practice, and secondary tumors of MPCs are of different clonal origin from primary tumors, while metastatic cancers are the same (123). However, the genetic material and biological behavior of tumor cells may be further changed due to the difference in local microenvironment during the colonization and proliferation of metastases in new sites, resulting in significant differences between their phenotypes and primary sites, which may lead to metastatic cancers misdiagnosis as MPCs, and for MPCs, mutations of selected gene sites may be the same because of tumor homogeneity or the same carcinogen, leading to misdiagnosis as metastatic cancer (131). If clinicians a lack of understanding of MPCs, will be the second primary cancer misdiagnosed as metastatic cancer, treatment strategies are set from the angle of the first primary cancer, and cell biology characteristics of various tumors in MPCs are independent and each are not identical, the treatment methods of different from metastatic carcinoma, so as to delay the best treatment time. Therefore, it is very important to clarify the characteristics of each tumor lesion for the diagnosis and treatment of patients with MPCs.
In addition to the difficulty in distinguishing MPCs from metastatic cancers, there is no unified treatment plan at present due to the complexity of pathogenesis and involved tumors. Some scholars believe that surgical treatment should be performed as soon as possible even if the second primary cancer has surgical characteristics (131). However, because MPCs associated with breast and gynecologic cancer exist in different organs and sites, their histological types are different, the reasons affecting treatment and prognosis are more complex, and patients’ physical and psychological conditions are worse than those of patients with single cancer, surgical treatment may limit the improvement of such patients’ conditions (99). Therefore, radical treatment is mainly used for different primary cancers, and the relevant treatment strategy should also be formulated according to the relevant primary cancer.
Therefore, in future studies, we need to focus on the pathogenesis of MPCs associated with breast and gynecologic cancers, reduce the toxic and side effects of various therapeutic measures, and carefully distinguish MPCs from metastatic cancers. Since there are essential differences in the cloning sources and development of the two, and there are pathogenic genes in patients with MPCs that lead to the occurrence of subsequent cancers, it may be a breakthrough for research to distinguish MPCs from metastatic cancers at the gene level.
For treatment of MPCs, multidisciplinary teams should focus on all risk factors and provide the most adequate management options. Early treatment should be given to patients to reduce the occurrence of MPCs from the source. When MPCs occur, the corresponding treatment plan should be formulated according to the severity of the patient’s disease, and reasonable personalized treatment plan should be provided for the patient. Considering heterogeneity and bias, further studies are needed to analyze clinical prognostic factors in order to establish a staging system for predicting prognosis.
Conclusion
In conclusion, BC associated with OC, BC associated with EC, BC associated with CC are the common types of MPCs associated with breast and gynecologic cancers. Their risk factors include the presence of co-pathogenic genes, abnormal hormone levels, poor lifestyle and behavior habits, age, and treatment regimens of the first primary cancer. The pathogenesis of MPCs is complex and not fully understood and the prognosis of MPCs associated with BC is worse than that of BC alone. In addition, misdiagnosis of MPCs lead to the implementation of the wrong treatment plan and condition assessment, which will adversely impact the treatment of patients. Therefore, postoperative follow-up should be strengthened, various examinations should be improved, preoperative biopsy should be performed, pathological types should be identified, and correct treatment should be given in time. Through the understanding and research of the specific situation of patients with different types of MPCs associated with breast and gynecologic cancers, the corresponding treatment plan should be formulated, so as to achieve the purpose of treating the disease and improving the survival and quality of life of patients.
Author Contributions
Conceptualization SG and XM validation XM writing—original draft preparation SG BW writing—review and editing SG BW ZW JH supervision XM All authors have read and agreed to the published version of the manuscript.
Funding
This review was supported by the National Natural Science Foundation of China (No. 81872123); “Xingliao Talents Program” of Liaoning Province (No.XLYC1902003); Liaoning Provincial Higher Education Innovation Team; Distinguished Professor of Liaoning Province; China Medical University’s 2018 Discipline Construction “Major Special Construction Plan” (No. 3110118029);and Outstanding Scientific Fund of Shengjing Hospital (No. 201601).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Thorat MA, Balasubramanian R. Breast Cancer Prevention in High-Risk Women. Best Pract Res Clin Obstet Gynaecol (2020) 65:18–31. doi: 10.1016/j.bpobgyn.2019.11.006
2. Yang Z, Liu Z, Chang Z, Yan G. MicroRNA-188-5p Inhibits the Progression of Breast Cancer by Targeting Zinc Finger Protein 91. Oncol Rep (2020) 44:1479–88. doi: 10.3892/or.2020.7731
3. Akram M, Iqbal M, Daniyal M, Khan AU. Awareness and Current Knowledge of Breast Cancer. Biol Res (2017) 50:33. doi: 10.1186/s40659-017-0140-9
4. Kolak A, Kamińska M, Sygit K, Budny A, Surdyka D, Kukiełka-Budny B, et al. Primary and Secondary Prevention of Breast Cancer. Ann Agric Environ Med (2017) 24:549–53. doi: 10.26444/aaem/75943
5. Chen K, Beeraka NM, Zhang J, Reshetov IV, Nikolenko VN, Sinelnikov MY, et al. Efficacy of Da Vinci Robot-Assisted Lymph Node Surgery Than Conventional Axillary Lymph Node Dissection in Breast Cancer - A Comparative Study. Int J Med Robot (2021) 17:e2307. doi: 10.1002/rcs.2307
6. D'Alonzo M, Bounous VE, Villa M, Biglia N. Current Evidence of the Oncological Benefit-Risk Profile of Hormone Replacement Therapy. Med (Kaunas) (2019) 55:573-9. doi: 10.3390/medicina55090573
7. Chen K, Lu P, Beeraka NM, Sukocheva OA, Madhunapantula SV, Liu J, et al. Mitochondrial Mutations and Mitoepigenetics: Focus on Regulation of Oxidative Stress-Induced Responses in Breast Cancers. Semin Cancer Biol (2020). doi: 10.1016/j.semcancer.2020.09.012
8. Britt KL, Cuzick J, Phillips KA. Key Steps for Effective Breast Cancer Prevention. Nat Rev Cancer (2020) 20:417–36. doi: 10.1038/s41568-020-0266-x
9. Petri BJ, Klinge CM. Regulation of Breast Cancer Metastasis Signaling by miRNAs. Cancer Metastasis Rev (2020) 39:837–86. doi: 10.1007/s10555-020-09905-7
10. Duffy SW, Vulkan D, Cuckle H, Parmar D, Sheikh S, Smith RA, et al. Effect of Mammographic Screening From Age 40 Years on Breast Cancer Mortality (UK Age Trial): Final Results of a Randomised, Controlled Trial. Lancet Oncol (2020) 21:1165–72. doi: 10.1016/s1470-2045(20)30398-3
11. Alimirzaie S, Bagherzadeh M, Akbari MR. Liquid Biopsy in Breast Cancer: A Comprehensive Review. Clin Genet (2019) 95:643–60. doi: 10.1111/cge.13514
12. Jiao F, Hu H, Wang LW. Quadruple Primary Malignancy Patient With Survival Time More Than 20 Years. World J Gastroenterol (2013) 19:1498–501. doi: 10.3748/wjg.v19.i9.1498
13. Cybulski C, Nazarali S, Narod SA. Multiple Primary Cancers as a Guide to Heritability. Int J Cancer (2014) 135:1756–63. doi: 10.1002/ijc.28988
14. Motuzyuk I, Sydorchuk O, Kovtun N, Palian Z, Kostiuchenko Y. Analysis of Trends and Factors in Breast Multiple Primary Malignant Neoplasms. Breast Cancer (Auckl) (2018) 12:1178223418759959. doi: 10.1177/1178223418759959
15. Noh SK, Yoon JY, Ryoo UN, Choi CH, Sung CO, Kim TJ, et al. A Case Report of Quadruple Cancer in a Single Patient Including the Breast, Rectum, Ovary, and Endometrium. J Gynecol Oncol (2008) 19:265–9. doi: 10.3802/jgo.2008.19.4.265
16. Lee J, Park S, Kim S, Kim J, Ryu J, Park HS, et al. Characteristics and Survival of Breast Cancer Patients With Multiple Synchronous or Metachronous Primary Cancers. Yonsei Med J (2015) 56:1213–20. doi: 10.3349/ymj.2015.56.5.1213
17. Roychoudhuri R, Evans H, Robinson D, Moller H. Radiation-Induced Malignancies Following Radiotherapy for Breast Cancer. Br J Cancer (2004) 91:868–72. doi: 10.1038/sj.bjc.6602084
18. Maxwell KN, Wenz BM, Kulkarni A, Wubbenhorst B, D'Andrea K, Weathers B, et al. Mutation Rates in Cancer Susceptibility Genes in Patients With Breast Cancer With Multiple Primary Cancers. JCO Precis Oncol (2020) 4:PO.19.00301. doi: 10.1200/po.19.00301
19. Molina-Montes E, Requena M, Sanchez-Cantalejo E, Fernandez MF, Arroyo-Morales M, Espin J, et al. Risk of Second Cancers Cancer After a First Primary Breast Cancer: A Systematic Review and Meta-Analysis. Gynecol Oncol (2015) 136:158–71. doi: 10.1016/j.ygyno.2014.10.029
20. Silverman BG, Lipshitz I, Keinan-Boker L. Second Primary Cancers After Primary Breast Cancer Diagnosis in Israeli Women, 1992 to 2006. J Glob Oncol (2017) 3:135–42. doi: 10.1200/jgo.2016.003699
21. Kim BK, Oh SJ, Song JY, Lee HB, Park MH, Jung Y, et al. Clinical Characteristics and Prognosis Associated With Multiple Primary Cancers in Breast Cancer Patients. J Breast Cancer (2018) 21:62–9. doi: 10.4048/jbc.2018.21.1.62
22. Corso G, Veronesi P, Santomauro GI, Maisonneuve P, Morigi C, Peruzzotti G, et al. Multiple Primary non-Breast Tumors in Breast Cancer Survivors. J Cancer Res Clin Oncol (2018) 144:979–86. doi: 10.1007/s00432-018-2621-9
23. Raymond JS, Hogue CJ. Multiple Primary Tumours in Women Following Breast Cancer, 1973-2000. Br J Cancer (2006) 94:1745–50. doi: 10.1038/sj.bjc.6603172
24. Nyqvist J, Parris TZ, Helou K, Sarenmalm EK, Einbeigi Z, Karlsson P, et al. Previously Diagnosed Multiple Primary Malignancies in Patients With Breast Carcinoma in Western Sweden Between 2007 and 2018. Breast Cancer Res Treat (2020) 184:221–8. doi: 10.1007/s10549-020-05822-z
25. Yi M, Cormier JN, Xing Y, Giordano SH, Chai C, Meric-Bernstam F, et al. Other Primary Malignancies in Breast Cancer Patients Treated With Breast Conserving Surgery and Radiation Therapy. Ann Surg Oncol (2013) 20:1514–21. doi: 10.1245/s10434-012-2774-8
26. Hamilton SN, Tyldesley S, Li D, Olson R, McBride M. Second Malignancies After Adjuvant Radiation Therapy for Early Stage Breast Cancer: Is There Increased Risk With Addition of Regional Radiation to Local Radiation? Int J Radiat Oncol Biol Phys (2015) 91:977–85. doi: 10.1016/j.ijrobp.2014.12.051
27. Bazire L, De Rycke Y, Asselain B, Fourquet A, Kirova YM. Risks of Second Malignancies After Breast Cancer Treatment: Long-Term Results. Cancer Radiother (2017) 21:10–5. doi: 10.1016/j.canrad.2016.07.101
28. Lee KD, Chen SC, Chan CH, Lu CH, Chen CC, Lin JT, et al. Increased Risk for Second Primary Malignancies in Women With Breast Cancer Diagnosed at Young Age: A Population-Based Study in Taiwan. Cancer Epidemiol Biomarkers Prev (2008) 17:2647–55. doi: 10.1158/1055-9965.EPI-08-0109
29. Ewertz M, Storm HH. Multiple Primary Cancers of the Breast, Endometrium and Ovary. Eur J Cancer Clin Oncol (1989) 25:1927–32. doi: 10.1016/0277-5379(89)90374-x
30. Rosen PP, Groshen S, Kinne DW, Hellman S. Nonmammary Malignant Neoplasms in Patients With Stage I (T1N0M0) and Stage II (T1N1M0) Breast Carcinoma. A Long-Term Follow-Up Study. Am J Clin Oncol (1989) 12:369–74. doi: 10.1097/00000421-198910000-00001
31. Nasioudis D, Wilson E, Mastroyannis SA, Sisti G, Haggerty AF, Ko EM, et al. Increased Risk of Breast and Uterine Cancer Among Women With Ovarian Granulosa Cell Tumors. Anticancer Res (2019) 39:4971–5. doi: 10.21873/anticanres.13686
32. Chen C, Xu Y, Huang X, Mao F, Shen S, Xu Y, et al. Clinical Characteristics and Survival Outcomes of Patients With Both Primary Breast Cancer and Primary Ovarian Cancer. Med (Baltimore) (2020) 99:e21560. doi: 10.1097/MD.0000000000021560
33. Ford D, Easton DF, Bishop DT, Narod SA, Goldgar DE. Risks of Cancer in BRCA1-Mutation Carriers. Breast Cancer Linkage Consortium. Lancet (London England) (1994) 343:692–5. doi: 10.1016/s0140-6736(94)91578-4
34. Foretová L, Navrátilová M, Svoboda M, Vašíčková P, Sťahlová EH, Házová J, et al. Recommendations for Preventive Care for Women With Rare Genetic Cause of Breast and Ovarian Cancer. Klin Onkol (2019) 32:6–13. doi: 10.14735/amko2019S6
35. Angeli D, Salvi S, Tedaldi G. Genetic Predisposition to Breast and Ovarian Cancers: How Many and Which Genes to Test? Int J Mol Sci (2020) 21:1128-55. doi: 10.3390/ijms21031128
36. Piombino C, Cortesi L, Lambertini M, Punie K, Grandi G, Toss A. Secondary Prevention in Hereditary Breast and/or Ovarian Cancer Syndromes Other Than BRCA. J Oncol (2020) 2020:6384190. doi: 10.1155/2020/6384190
37. Lu HM, Li S, Black MH, Lee S, Hoiness R, Wu S, et al. Association of Breast and Ovarian Cancers With Predisposition Genes Identified by Large-Scale Sequencing. JAMA Oncol (2019) 5:51–7. doi: 10.1001/jamaoncol.2018.2956
38. Samadder NJ, Giridhar KV, Baffy N, Riegert-Johnson D, Couch FJ. Hereditary Cancer Syndromes-A Primer on Diagnosis and Management: Part 1: Breast-Ovarian Cancer Syndromes. Mayo Clin Proc (2019) 94:1084–98. doi: 10.1016/j.mayocp.2019.02.017
39. Shibahara Y, Sugawara Y, Miki Y, Hata S, Takahashi H, Nakamura Y, et al. Analysis of Multiple Primary Cancer Autopsy Cases Associated With Breast Cancer: 2002-2010. Pathol Int (2016) 66:695–700. doi: 10.1111/pin.12484
40. Yang X, Song H, Leslie G, Engel C, Hahnen E, Auber B, et al. Ovarian and Breast Cancer Risks Associated With Pathogenic Variants in RAD51C and RAD51D. J Natl Cancer Inst (2020) 112:1242–50. doi: 10.1093/jnci/djaa030
41. Zheng G, Yu H, Kanerva A, Forsti A, Sundquist K, Hemminki K. Familial Ovarian Cancer Clusters With Other Cancers. Sci Rep (2018) 8:11561. doi: 10.1038/s41598-018-29888-4
42. Ripamonti CB, Manoukian S, Peissel B, Azzollini J, Carcangiu ML, Radice P. Survey of Gynecological Carcinosarcomas in Families With Breast and Ovarian Cancer Predisposition. Cancer Genet (2018) 221:38–45. doi: 10.1016/j.cancergen.2017.12.001
43. Hodgson A, Turashvili G. Pathology of Hereditary Breast and Ovarian Cancer. Front Oncol (2020) 10:531790. doi: 10.3389/fonc.2020.531790
44. Biglia N, Sgandurra P, Bounous VE, Maggiorotto F, Piva E, Pivetta E, et al. Ovarian Cancer in BRCA1 and BRCA2 Gene Mutation Carriers: Analysis of Prognostic Factors and Survival. Ecancermedicalscience (2016) 10:639. doi: 10.3332/ecancer.2016.639
45. Yoshida R. Hereditary Breast and Ovarian Cancer (HBOC): Review of its Molecular Characteristics, Screening, Treatment, and Prognosis. Breast Cancer (2020) 28:1167-80. doi: 10.1007/s12282-020-01148-2
46. Bryk S, Pukkala E, Farkkila A, Heikinheimo M, Unkila-Kallio L, Riska A. Other Primary Malignancies Among Women With Adult-Type Ovarian Granulosa Cell Tumors. Int J Gynecol Cancer (2018) 28:1529–34. doi: 10.1097/IGC.0000000000001333
47. Zhang W, Zhang W, Lin Z, Wang F, Li M, Zhu L, et al. Survival Outcomes of Patients With Primary Breast Cancer Following Primary Ovarian Cancer. Med Sci Monit (2019) 25:3869–79. doi: 10.12659/MSM.914163
48. McGee J, Giannakeas V, Karlan B, Lubinski J, Gronwald J, Rosen B, et al. Risk of Breast Cancer After a Diagnosis of Ovarian Cancer in BRCA Mutation Carriers: Is Preventive Mastectomy Warranted? Gynecol Oncol (2017) 145:346–51. doi: 10.1016/j.ygyno.2017.02.032
49. Modaffari P, Ponzone R, Ferrari A, Cipullo I, Liberale V, D'Alonzo M, et al. Concerns and Expectations of Risk-Reducing Surgery in Women With Hereditary Breast and Ovarian Cancer Syndrome. J Clin Med (2019) 8:313-26. doi: 10.3390/jcm8030313
50. Peters ML, Garber JE, Tung N. Managing Hereditary Breast Cancer Risk in Women With and Without Ovarian Cancer. Gynecol Oncol (2017) 146:205–14. doi: 10.1016/j.ygyno.2017.04.013
51. Alenezi WM, Fierheller CT, Recio N, Tonin PN. Literature Review of BARD1 as a Cancer Predisposing Gene With a Focus on Breast and Ovarian Cancers. Genes (Basel) (2020) 11:856-79. doi: 10.3390/genes11080856
52. Biglia N, D'Alonzo M, Sgro LG, Tomasi Cont N, Bounous V, Robba E. Breast Cancer Treatment in Mutation Carriers: Surgical Treatment. Minerva Ginecol (2016) 68:548–56.
53. Domchek SM, Friebel TM, Singer CF, Evans DG, Lynch HT, Isaacs C, et al. Association of Risk-Reducing Surgery in BRCA1 or BRCA2 Mutation Carriers With Cancer Risk and Mortality. JAMA-J Am Med Assoc (2010) 304:967–75. doi: 10.1001/jama.2010.1237
54. Byrski T, Gronwald J, Huzarski T, Grzybowska E, Budryk M, Stawicka M, et al. Pathologic Complete Response Rates in Young Women With BRCA1-Positive Breast Cancers After Neoadjuvant Chemotherapy. J Clin Oncol (2010) 28:375–9. doi: 10.1200/jco.2008.20.7019
55. Wen WX, Leong CO. Association of BRCA1- and BRCA2-Deficiency With Mutation Burden, Expression of PD-L1/PD-1, Immune Infiltrates, and T Cell-Inflamed Signature in Breast Cancer. PLoS One (2019) 14:e0215381. doi: 10.1371/journal.pone.0215381
56. Jung HK, Park S, Kim NW, Lee JE, Kim Z, Han SW, et al. Development of Second Primary Cancer in Korean Breast Cancer Survivors. Ann Surg Treat Res (2017) 93:287–92. doi: 10.4174/astr.2017.93.6.287
57. Guo JB, Zhang Y, Qian HL, Ma F, Cui XJ, Duan H. The Clinical Characteristics and Prognosis of Endometrial Carcinomas That Occur After Breast Cancer: Does Hormone Receptor Status of Breast Cancer Matter? Arch Gynecol Obstet (2019) 300:1399–404. doi: 10.1007/s00404-019-05318-2
58. Kim HY, Thi HTH, Hong S. IMP2 and IMP3 Cooperate to Promote the Metastasis of Triple-Negative Breast Cancer Through Destabilization of Progesterone Receptor. Cancer Lett (2018) 415:30–9. doi: 10.1016/j.canlet.2017.11.039
59. Ngeow J, Sesock K, Eng C. Breast Cancer Risk and Clinical Implications for Germline PTEN Mutation Carriers. Breast Cancer Res Treat (2017) 165:1–8. doi: 10.1007/s10549-015-3665-z
60. Bubien V, Bonnet F, Brouste V, Hoppe S, Barouk-Simonet E, David A, et al. High Cumulative Risks of Cancer in Patients With PTEN Hamartoma Tumour Syndrome. J Med Genet (2013) 50:255–63. doi: 10.1136/jmedgenet-2012-101339
61. Zhang Q, Li T, Wang Z, Kuang X, Shao N, Lin Y. lncRNA NR2F1-AS1 Promotes Breast Cancer Angiogenesis Through Activating IGF-1/IGF-1r/ERK Pathway. J Cell Mol Med (2020) 24:8236–47. doi: 10.1111/jcmm.15499
62. Yang X, Wang J. The Role of Metabolic Syndrome in Endometrial Cancer: A Review. Front Oncol (2019) 9:744. doi: 10.3389/fonc.2019.00744
63. Hammes SR, Levin ER. Impact of Estrogens in Males and Androgens in Females. J Clin Invest (2019) 129:1818–26. doi: 10.1172/jci125755
64. Clemons M, Goss P. Estrogen and the Risk of Breast Cancer. N Engl J Med (2001) 344:276–85. doi: 10.1056/nejm200101253440407
65. McCracken E, Monaghan M, Sreenivasan S. Pathophysiology of the Metabolic Syndrome. Clin Dermatol (2018) 36:14–20. doi: 10.1016/j.clindermatol.2017.09.004
66. Min DY, Jung E, Kim J, Lee YH, Shin SY. Leptin Stimulates IGF-1 Transcription by Activating AP-1 in Human Breast Cancer Cells. BMB Rep (2019) 52:385–90. doi: 10.5483/BMBRep.2019.52.6.189
67. Majchrzak-Baczmańska D, Malinowski A. Does IGF-1 Play a Role in the Biology of Endometrial Cancer? Ginekol Pol (2016) 87:598–604. doi: 10.5603/gp.2016.0052
68. Roshan MH, Shing YK, Pace NP. Metformin as an Adjuvant in Breast Cancer Treatment. SAGE Open Med (2019) 7:2050312119865114. doi: 10.1177/2050312119865114
69. Giovannucci E, Harlan DM, Archer MC, Bergenstal RM, Gapstur SM, Habel LA, et al. Diabetes and Cancer: A Consensus Report. Diabetes Care (2010) 33:1674–85. doi: 10.2337/dc10-0666
70. Sang YT, Chen B, Song XJ, Li YM, Liang YR, Han DW, et al. circRNA_0025202 Regulates Tamoxifen Sensitivity and Tumor Progression via Regulating the miR-182-5p/FOXO3a Axis in Breast Cancer. Mol Ther (2019) 27:1638–52. doi: 10.1016/j.ymthe.2019.05.011
71. Yao J, Deng K, Huang J, Zeng R, Zuo J. Progress in the Understanding of the Mechanism of Tamoxifen Resistance in Breast Cancer. Front Pharmacol (2020) 11:592912. doi: 10.3389/fphar.2020.592912
72. Liu SS, Li Y, Zhang H, Zhang D, Zhang XB, Wang X, et al. The Erα-miR-575-P27 Feedback Loop Regulates Tamoxifen Sensitivity in ER-Positive Breast Cancer. Theranostics (2020) 10:10729–42. doi: 10.7150/thno.46297
73. Zhao H, Zhou L, Shangguan AJ, Bulun SE. Aromatase Expression and Regulation in Breast and Endometrial Cancer. J Mol Endocrinol (2016) 57:R19–33. doi: 10.1530/JME-15-0310
74. Jeon J, Kim SE, Lee DY, Choi D. Factors Associated With Endometrial Pathology During Tamoxifen Therapy in Women With Breast Cancer: A Retrospective Analysis of 821 Biopsies. Breast Cancer Res Treat (2020) 179:125–30. doi: 10.1007/s10549-019-05448-w
75. Emons G, Mustea A, Tempfer C. Tamoxifen and Endometrial Cancer: A Janus-Headed Drug. Cancers (2020) 12:2535-45. doi: 10.3390/cancers12092535
76. Ignatov A, Ortmann O. Endocrine Risk Factors of Endometrial Cancer: Polycystic Ovary Syndrome, Oral Contraceptives, Infertility, Tamoxifen. Cancers (Basel) (2020) 12:1766-75. doi: 10.3390/cancers12071766
77. Woolas J, Davis M, Rahimi S. Recurrence of Endometrial Cancer in a Hysterectomised Patient Treated With Tamoxifen for Breast Cancer: A Case Report. J R Soc Med (2020) 113:454–6. doi: 10.1177/0141076820961087
78. Andersson M, Jensen MB, Engholm G, Henrik Storm H. Risk of Second Primary Cancer Among Patients With Early Operable Breast Cancer Registered or Randomised in Danish Breast Cancer Cooperative Group (DBCG) Protocols of the 77, 82 and 89 Programmes During 1977-2001. Acta Oncol (2008) 47:755–64. doi: 10.1080/02841860801978921
79. Demoor-Goldschmidt C, de Vathaire F. Review of Risk Factors of Secondary Cancers Among Cancer Survivors. Br J Radiol (2019) 92:20180390. doi: 10.1259/bjr.20180390
80. Jones ME, van Leeuwen FE, Hoogendoorn WE, Mourits MJ, Hollema H, van Boven H, et al. Endometrial Cancer Survival After Breast Cancer in Relation to Tamoxifen Treatment: Pooled Results From Three Countries. Breast Cancer Res (2012) 14:R91. doi: 10.1186/bcr3206
81. Lubian Lopez DM, Orihuela Lopez F, Garcia-Berbel Molina L, Boza Novo P, Pozuelo Solis E, Menor Almagro D, et al. Endometrial Polyps in Obese Asymptomatic Pre and Postmenopausal Patients With Breast Cancer: Is Screening Necessary? Gynecol Oncol (2014) 133:56–62. doi: 10.1016/j.ygyno.2013.12.029
82. Negoiţă M, Terinte C, Mihailovici MS. [Tamoxifen and Endometrial Pathology]. Rev Med Chir Soc Med Nat Iasi (2010) 114:1114–7.
83. Liu J, Jiang W, Mao K, An Y, Su F, Kim BY, et al. Elevated Risks of Subsequent Endometrial Cancer Development Among Breast Cancer Survivors With Different Hormone Receptor Status: A SEER Analysis. Breast Cancer Res Treat (2015) 150:439–45. doi: 10.1007/s10549-015-3315-5
84. Chlebowski RT, Schottinger JE, Shi J, Chung J, Haque R. Aromatase Inhibitors, Tamoxifen, and Endometrial Cancer in Breast Cancer Survivors. Cancer (2015) 121:2147–55. doi: 10.1002/cncr.29332
85. Liang J, Shang Y. Estrogen and Cancer. Annu Rev Physiol (2013) 75:225–40. doi: 10.1146/annurev-physiol-030212-183708
86. Fles R, Hoogendoorn WE, Platteel I, Scheerman CE, de Leeuw-Mantel G, Mourits MJ, et al. Genomic Profile of Endometrial Tumors Depends on Morphological Subtype, Not on Tamoxifen Exposure. Genes Chromosomes Cancer (2010) 49:699–710. doi: 10.1002/gcc.20781
87. Trentham-Dietz A, Newcomb PA, Nichols HB, Hampton JM. Breast Cancer Risk Factors and Second Primary Malignancies Among Women With Breast Cancer. Breast Cancer Res Treat (2007) 105:195–207. doi: 10.1007/s10549-006-9446-y
88. Wijayabahu AT, Egan KM, Yaghjyan L. Uterine Cancer in Breast Cancer Survivors: A Systematic Review. Breast Cancer Res Treat (2020) 180:1–19. doi: 10.1007/s10549-019-05516-1
89. Uzunlulu M, Caklili OT, Oguz A. Association Between Metabolic Syndrome and Cancer. Ann Nutr Metab (2016) 68:173–9. doi: 10.1159/000443743
90. Izmajlowicz B, Kornafel J, Blaszczyk J. Multiple Neoplasms Among Cervical Cancer Patients in the Material of the Lower Silesian Cancer Registry. Adv Clin Exp Med (2014) 23:433–40. doi: 10.17219/acem/37141
91. Lawson JS, Glenn WK, Salyakina D, Delprado W, Clay R, Antonsson A, et al. Human Papilloma Viruses and Breast Cancer. Front Oncol (2015) 5:277. doi: 10.3389/fonc.2015.00277
92. Lawson JS, Glenn WK, Salyakina D, Clay R, Delprado W, Cheerala B, et al. Human Papilloma Virus Identification in Breast Cancer Patients With Previous Cervical Neoplasia. Front Oncol (2016) 5:298. doi: 10.3389/fonc.2015.00298
93. Lawson JS, Glenn WK, Whitaker NJ. Human Papilloma Viruses and Breast Cancer - Assessment of Causality. Front Oncol (2016) 6:207. doi: 10.3389/fonc.2016.00207
94. Preti M, Rosso S, Micheletti L, Libero C, Sobrato I, Giordano L, et al. Risk of HPV-Related Extra-Cervical Cancers in Women Treated for Cervical Intraepithelial Neoplasia. BMC Cancer (2020) 20:972–2. doi: 10.1186/s12885-020-07452-6
95. Gupta I, Jabeen A, Al-Sarraf R, Farghaly H, Vranic S, Sultan AA, et al. The Co-Presence of High-Risk Human Papillomaviruses and Epstein-Barr Virus Is Linked With Tumor Grade and Stage in Qatari Women With Breast Cancer. Hum Vaccines Immunotherapeut (2020) 17:1–8. doi: 10.1080/21645515.2020.1802977
96. Gupta I, Jabeen A, Vranic S, Al Moustafa AE, Al-Thawadi H. Oncoproteins of High-Risk HPV and EBV Cooperate to Enhance Cell Motility and Invasion of Human Breast Cancer Cells via Erk1/Erk2 and β-Catenin Signaling Pathways. Front Oncol (2021) 11:630408. doi: 10.3389/fonc.2021.630408
97. Gierisch JM, Coeytaux RR, Urrutia RP, Havrilesky LJ, Moorman PG, Lowery WJ, et al. Oral Contraceptive Use and Risk of Breast, Cervical, Colorectal, and Endometrial Cancers: A Systematic Review. Cancer Epidemiol Biomarkers Prev (2013) 22:1931–43. doi: 10.1158/1055-9965.Epi-13-0298
98. Choi M-A, Saeidi S, Han H-J, Kim S-J, Kwon N, Kim D-H, et al. The Peptidyl Prolyl Isomerase, PIN1 Induces Angiogenesis Through Direct Interaction With HIF-2alpha. Biochem Biophys Res Commun (2020) 533:995–1003. doi: 10.1016/j.bbrc.2020.08.015
99. Thong MSY, Mols F, Verhoeven RHA, Liu L, Andrykowski MA, Roukema JA, et al. Multiple Primary Cancer Survivors Have Poorer Health Status and Well-Being Than Single Primary Cancer Survivors: A Study From the Population-Based PROFILES Registry. Psycho-Oncology (2013) 22:1834–42. doi: 10.1002/pon.3227
100. Hughes KS, Schnaper LA, Bellon JR, Cirrincione CT, Berry DA, McCormick B, et al. Lumpectomy Plus Tamoxifen With or Without Irradiation in Women Age 70 Years or Older With Early Breast Cancer: Long-Term Follow-Up of CALGB 9343. J Clin Oncol (2013) 31:2382. doi: 10.1200/jco.2012.45.2615
101. Susini T, Renda I. FGD3 Gene as a New Prognostic Factor in Breast Cancer. Anticancer Res (2020) 40:3645–9. doi: 10.21873/anticanres.14353
102. Feller A, Matthes KL, Bordoni A, Bouchardy C, Bulliard JL, Herrmann C, et al. The Relative Risk of Second Primary Cancers in Switzerland: A Population-Based Retrospective Cohort Study. BMC Cancer (2020) 20:51. doi: 10.1186/s12885-019-6452-0
103. Bergfeldt K, Einhorn S, Rosendahl I, Hall P. Increased Risk of Second Primary Malignancies in Patients With Gynecological Cancer. A Swedish Record-Linkage Study. Acta Oncol (1995) 34:771–7. doi: 10.3109/02841869509127185
104. Iioka Y, Tsuchida A, Okubo K, Ogiso M, Ichimiya H, Saito K, et al. Metachronous Triple Cancers of the Sigmoid Colon, Stomach, and Esophagus: Report of a Case. Surg Today (2000) 30:368–71. doi: 10.1007/s005950050602
105. Brown SB, Hankinson SE. Endogenous Estrogens and the Risk of Breast, Endometrial, and Ovarian Cancers. Steroids (2015) 99:8–10. doi: 10.1016/j.steroids.2014.12.013
106. Himbert C, Delphan M, Scherer D, Bowers LW, Hursting S, Ulrich CM. Signals From the Adipose Microenvironment and the Obesity-Cancer Link-A Systematic Review. Cancer Prev Res (Phila) (2017) 10:494–506. doi: 10.1158/1940-6207.CAPR-16-0322
107. Kryzhanivska AE, Dyakiv IB, Kyshakevych I. Clinical and Immunohistochemical Features of Primary Breast Cancer and Metachronous Ovarian and Endometrial Tumors. Exp Oncol (2018) 40:124–7. doi: 10.31768/2312-8852.2018.40(2):124-127
108. Dunneram Y, Greenwood DC, Cade JE. Diet, Menopause and the Risk of Ovarian, Endometrial and Breast Cancer. Proc Nutr Soc (2019) 78:438–48. doi: 10.1017/S0029665118002884
109. Wood ME, Vogel V, Ng A, Foxhall L, Goodwin P, Travis LB. Second Malignant Neoplasms: Assessment and Strategies for Risk Reduction. J Clin Oncol (2012) 30:3734–45. doi: 10.1200/JCO.2012.41.8681
110. Wei JL, Jiang YZ, Shao ZM. Survival and Chemotherapy-Related Risk of Second Primary Malignancy in Breast Cancer Patients: A SEER-Based Study. Int J Clin Oncol (2019) 24:934–40. doi: 10.1007/s10147-019-01430-0
111. Bulsa M, Urasinska E. Triple Negative Endometrial Cancer. Ginekol Polska (2017) 88:212–4. doi: 10.5603/GP.a2017.0040
112. Ishihara BP, Farah D, Fonseca MCM, Nazario A. The Risk of Developing Breast, Ovarian, and Endometrial Cancer in Obese Women Submitted to Bariatric Surgery: A Meta-Analysis. Surg Obes Relat Dis (2020) 16:1596–602. doi: 10.1016/j.soard.2020.06.008
113. Byers T, Sedjo RL. Body Fatness as a Cause of Cancer: Epidemiologic Clues to Biologic Mechanisms. Endocr Relat Cancer (2015) 22:R125–134. doi: 10.1530/erc-14-0580
114. Lipsey CC, Harbuzariu A, Daley-Brown D, Gonzalez-Perez RR. Oncogenic Role of Leptin and Notch Interleukin-1 Leptin Crosstalk Outcome in Cancer. World J Methodol (2016) 6:43–55. doi: 10.5662/wjm.v6.i1.43
115. Jassem J. Tobacco Smoking After Diagnosis of Cancer: Clinical Aspects. Transl Lung Cancer Res (2019) 8:S50–8. doi: 10.21037/tlcr.2019.04.01
116. Romaszko-Wojtowicz A, Bucinski A, Doboszynska A. Impact of Smoking on Multiple Primary Cancers Survival: A Retrospective Analysis. Clin Exp Med (2018) 18:391–7. doi: 10.1007/s10238-018-0498-1
117. Li Z, Wu Q, Song J, Zhang Y, Zhu S, Sun S. Risk of Second Primary Female Genital Malignancies in Women With Breast Cancer: A SEER Analysis. Horm Cancer (2018) 9:197–204. doi: 10.1007/s12672-018-0330-0
118. Molina-Montes E, Pollan M, Payer T, Molina E, Davila-Arias C, Sanchez MJ. Risk of Second Primary Cancer Among Women With Breast Cancer: A Population-Based Study in Granada (Spain). Gynecol Oncol (2013) 130:340–5. doi: 10.1016/j.ygyno.2013.04.057
119. Li Z, Wang K, Shi Y, Zhang X, Wen J. Incidence of Second Primary Malignancy After Breast Cancer and Related Risk Factors-Is Breast-Conserving Surgery Safe? A Nested Case-Control Study. Int J Cancer (2020) 146:352–62. doi: 10.1002/ijc.32259
120. Grantzau T, Overgaard J. Risk of Second non-Breast Cancer After Radiotherapy for Breast Cancer: A Systematic Review and Meta-Analysis of 762,468 Patients. Radiother Oncol (2015) 114:56–65. doi: 10.1016/j.radonc.2014.10.004
121. Berrington de Gonzalez A, Curtis RE, Gilbert E, Berg CD, Smith SA, Stovall M, et al. Second Solid Cancers After Radiotherapy for Breast Cancer in SEER Cancer Registries. Br J Cancer (2010) 102:220–6. doi: 10.1038/sj.bjc.6605435
122. Grantzau T, Overgaard J. Risk of Second non-Breast Cancer Among Patients Treated With and Without Postoperative Radiotherapy for Primary Breast Cancer: A Systematic Review and Meta-Analysis of Population-Based Studies Including 522,739 Patients. Radiother Oncol (2016) 121:402–13. doi: 10.1016/j.radonc.2016.08.017
123. Slaughter DP, Southwick HW, Smejkal W. Field Cancerization in Oral Stratified Squamous Epithelium; Clinical Implications of Multicentric Origin. Cancer (1953) 6:963–8. doi: 10.1002/1097-0142(195309)6:5<963::aid-cncr2820060515>3.0.co;2-q
124. Lee YC, Wang HP, Wang CP, Ko JY, Lee JM, Chiu HM, et al. Revisit of Field Cancerization in Squamous Cell Carcinoma of Upper Aerodigestive Tract: Better Risk Assessment With Epigenetic Markers. Cancer Prev Res (Phila) (2011) 4:1982–92. doi: 10.1158/1940-6207.Capr-11-0096
125. Patel HK, Bihani T. Selective Estrogen Receptor Modulators (SERMs) and Selective Estrogen Receptor Degraders (SERDs) in Cancer Treatment. Pharmacol Ther (2018) 186:1–24. doi: 10.1016/j.pharmthera.2017.12.012
126. Brook N, Brook E, Dass CR, Chan A, Dharmarajan A. Pigment Epithelium-Derived Factor and Sex Hormone-Responsive Cancers. Cancers (Basel) (2020) 12:3483–95. doi: 10.3390/cancers12113483
127. Lee TY, Martinez-Outschoorn UE, Schilder RJ, Kim CH, Richard SD, Rosenblum NG, et al. Metformin as a Therapeutic Target in Endometrial Cancers. Front Oncol (2018) 8:341. doi: 10.3389/fonc.2018.00341
128. Faria J, Negalha G, Azevedo A, Martel F. Metformin and Breast Cancer: Molecular Targets. J Mammary Gland Biol Neoplasia (2019) 24:111–23. doi: 10.1007/s10911-019-09429-z
129. Gadducci A, Biglia N, Tana R, Cosio S, Gallo M. Metformin Use and Gynecological Cancers: A Novel Treatment Option Emerging From Drug Repositioning. Crit Rev Oncol Hematol (2016) 105:73–83. doi: 10.1016/j.critrevonc.2016.06.006
130. Metzler JM, Burla L, Fink D, Imesch P. Ibrutinib in Gynecological Malignancies and Breast Cancer: A Systematic Review. Int J Mol Sci (2020) 21:4154–70. doi: 10.3390/ijms21114154
Keywords: breast cancer, ovarian cancer, endometrial cancer, cervical cancer, multiple primary cancers, primary gynecologic cancer
Citation: Ge S, Wang B, Wang Z, He J and Ma X (2022) Common Multiple Primary Cancers Associated With Breast and Gynecologic Cancers and Their Risk Factors, Pathogenesis, Treatment and Prognosis: A Review. Front. Oncol. 12:840431. doi: 10.3389/fonc.2022.840431
Received: 23 February 2022; Accepted: 16 May 2022;
Published: 08 June 2022.
Edited by:
Ke-Da Yu, Fudan University, ChinaCopyright © 2022 Ge, Wang, Wang, He and Ma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaoxin Ma, bWF4eEBzai1ob3NwaXRhbC5vcmc=
 Shuwen Ge
Shuwen Ge Bo Wang
Bo Wang Zihao Wang1,2
Zihao Wang1,2 Junjian He
Junjian He Xiaoxin Ma
Xiaoxin Ma