Abstract
Background:
Breast reconstruction is a promising surgical technique to improve health-related quality of life (HRQoL) in patients with breast cancer. However, the long-term risk factors associated with HRQoL after breast surgery are still unclear. Our aim was to evaluate breast satisfaction and HRQoL following breast reconstruction to identify clinical factors associated with each domain of BREAST-Q in the long-term.
Methods:
Patient-reported BREAST-Q outcomes were analyzed 1 and 5 years after breast reconstruction in a single-blinded, prospective study. Multiple regression analysis was performed to identify the risk and protective factors associated with BREAST-Q scores. These scores at 1 and 5 years were also compared across three types of operation: mastectomy only, tissue expander/implant (TE/Imp), and a deep inferior epigastric perforator (DIEP) flap.
Results:
Surveys were completed by 141 subjects after 1 year and 131 subjects after 5 years. Compared to mastectomy only, breast reconstruction was significantly associated with greater “Satisfaction with breasts” (TE/Imp, p < 0.001; DIEP, p < 0.001) and “Psychosocial well-being” (TE/Imp, p < 0.001; DIEP, p < 0.001), higher body mass index (BMI) resulted in lower “Satisfaction with breasts” (p = 0.004), and a history of psychiatric or neurological medication was significantly associated with “Physical well-being” at 1-year postoperatively (p = 0.02). At 5 years, reconstructive procedures were significantly positively associated with greater “Satisfaction with breasts” (TE/Imp, p < 0.001; DIEP, p < 0.001) and “Psychosocial well-being” (TE/Imp, p = 0.03; DIEP, p < 0.001), and a bilateral procedure was a significant risk factor for lower “Psychosocial well-being” (p = 0.02).
Conclusions:
The results of this study show that breast reconstruction improves “Satisfaction with Breasts” and “Psychosocial well-being” compared to mastectomy. Among all three types of operation, DIEP gave the best scores at 5 years postoperatively. Thus, autologous reconstruction is recommended for promotion of long-term HRQoL after breast surgery.
Introduction
More than 2 million women worldwide receive a new diagnosis of breast cancer every year (1–3). The number of women surviving breast cancer has increased due to improvements of treatment in many countries, including in Japan (4, 5). Postoperative complications such as lymphoedema, axillary web syndrome (AWS), and fatigue may reduce health-related quality of life (HRQoL) (6–8), but patients also have the opportunity to receive breast reconstruction after mastectomy, which can significantly improve HRQoL (9). Factors associated with HRQoL include satisfaction with appearance, psychological well-being, and physical function. In patients with breast cancer, some studies have shown that aesthetic outcome also influences HRQoL (10, 11).
Multiple questionnaires have been used to measure patient-reported outcomes (PROs) after breast surgery for patients with breast cancer. However, until the turn of the century, few instruments had sufficient evidence for specific use in these patients due to limitations in certain areas, including aesthetics and body perception (12). In 2009, the BREAST-Q questionnaire was developed to meet this need, as a validated PRO measurement specific to breast surgery. Since its release, the BREAST-Q has greatly improved studies of satisfaction with breast surgery from the patient’s perspective (13–16).
Previous studies using the BREAST-Q questionnaire have established that breast reconstruction provides higher levels of patient satisfaction. Most of these studies had short follow-up periods of up to 1 year and limited comparison groups (17–25). In addition, satisfaction with breast reconstruction may change, even over a short period of time (26–28). Long-term satisfaction is important after breast reconstruction, but how satisfaction and HRQoL change years after the initial operation is still unclear.
To investigate these issues further, we performed a long-term prospective survey of patients with breast cancer who underwent breast surgery including breast reconstruction. The objective was to evaluate HRQoL in a Japanese population following breast reconstruction to identify clinical factors that predict higher or lower BREAST-Q scores in long-term survivors.
Material and Methods
Subjects and Experimental Design
We prospectively analyzed clinical data for all consecutive patients with breast cancer who underwent breast reconstruction performed by three surgeons at a single center from January 2016 to April 2017. Patients were enrolled in the study if they fulfilled the following criteria: (1) age ≥18 years, (2) undergoing mastectomy only or first-time unilateral or bilateral post-mastectomy breast reconstruction using a tissue expander/implant (TE/Imp) or a deep inferior epigastric perforator (DIEP) flap, and (3) not meeting exclusion criteria of surgical complications such as implant loss or flap loss that could affect long-term results, death, or a poor understanding of the study due to severe neurological or psychiatric disorders. For power analysis, a 10-point difference in HRQoL (BREAST-Q) score was taken to indicate a clinically relevant difference (minimally important difference: MID) based on a previous study (29). Using alpha of 0.05, a standard deviation of 5-10 points from our previous study (30) and beta of 0.80, at least 34 patients per arm were required for significance. Advice on statistical analysis was provided by Statista (Kyoto, Japan), a medical statistics support company. As the scheduled date of closure was reached, enrollment was stopped in April 2017 before reaching the planned sample size.
Data Collection and Measurements
All subjects provided demographic data. Smoking was divided into past and current. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. Clinical characteristics, type of breast surgery, therapy after mastectomy (radiotherapy, chemotherapy, and/or hormone therapy), and history of psychiatric or neurological illness and medication were obtained from medical records.
BREAST-Q Survey
The BREAST-Q is a validated PRO measure developed at Memorial Sloan Kettering Cancer Center and the University of British Columbia (13, 14). We focused on three BREAST-Q domains: “Satisfaction with breasts”, “Psychosocial well-being”, and “Physical well-being”. Each domain score was obtained by transforming the scale item responses with the Q-score software program. The transformed scores range from 0 to 100 and higher scores indicated greater satisfaction or QOL. The Japanese version of the BREAST-Q survey was administered prior to surgery after consultation with the surgical oncologist and plastic surgeon, and at 1 and 5 years after completion of surgery (31). At these time points, surveys were given to patients at an office visit or mailed to the patient’s home.
Statistical Analysis
Statistical analyses were performed using JMP Pro v.14.0 (SAS Institute Inc., Cary, NC) and SPSS v.26.0 (IBM Corp., Armonk, NY). Continuous variables are shown as the mean ± standard deviation (SD) and categorical variables as a number (percentage). A multiple linear regression model was constructed for identification of significant factors for HRQoL. A Mann-Whitney U test was used to compare data between years, and a post-hoc Tukey test was used for comparison between operative procedures. P < 0.05 was considered to be significant in all analyses.
Ethics Approval
All procedures were approved by the local research ethics committee (Kyoto Prefectural University of Medicine: IRBMED Number ERB-C-563-1) and were conducted in accordance with the Declaration of Helsinki. Informed consent was obtained from all subjects.
Results
Among 213 potential subjects, 8 were excluded due to implant loss (n=1), flap loss (n=2), and difficulty understanding the study because of severe neurological or psychiatric disorders (n=5). All patients received immediate reconstruction. Questionnaire surveys were sent to the home addresses of 205 subjects in the year after the operation. Written informed consent and answers were obtained from 141 at 1 year and 131 at 5 years postoperatively, giving response rates of 68.8% and 63.9%, respectively (Figure 1).
Figure 1
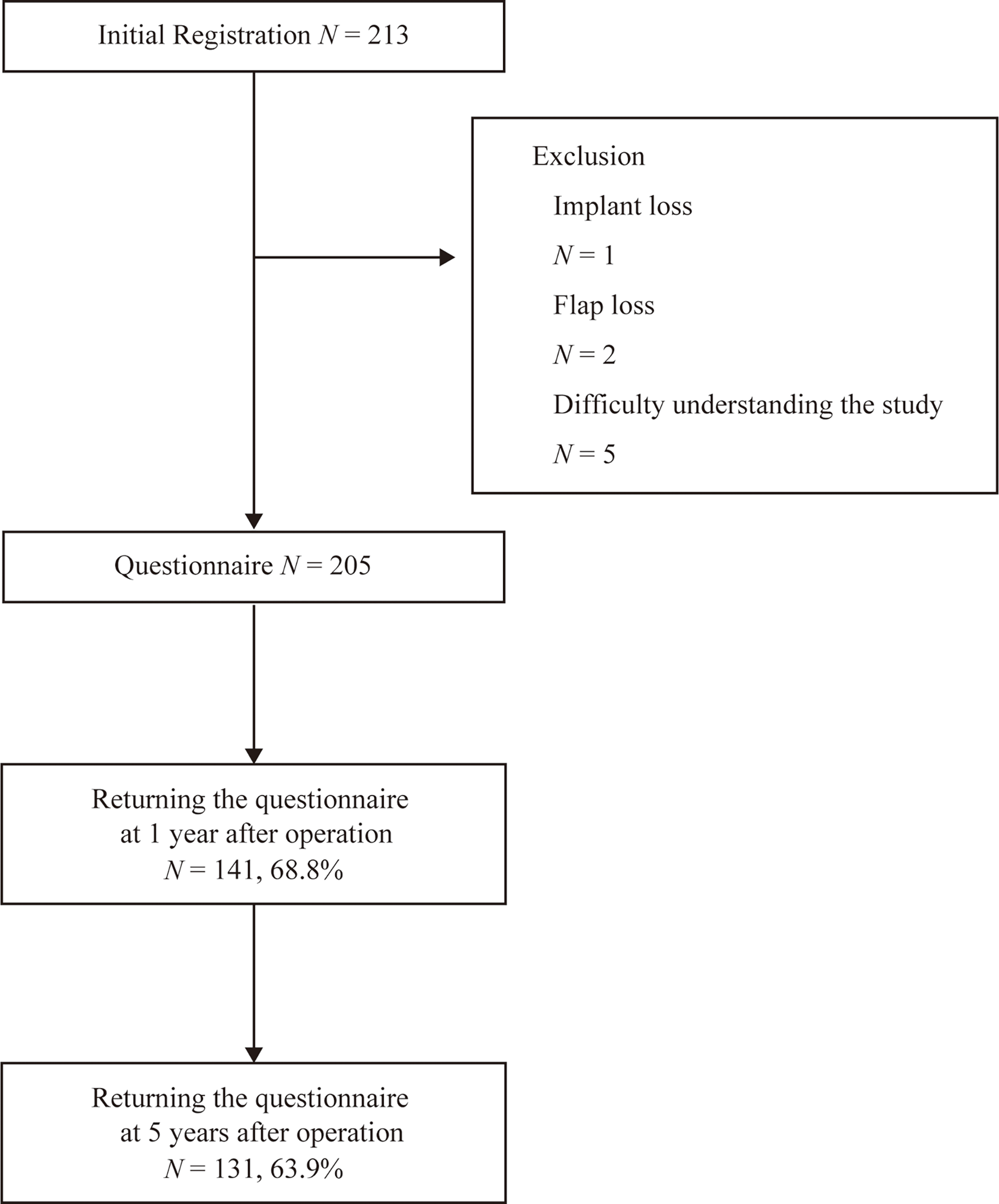
Inclusion and exclusion of subjects.
The demographic and clinical characteristics of the 141 subjects at 1 year and 131 subjects at 5 years are shown in Table 1. The subjects were 53.0 ± 12.9 years old and had a BMI of 22.3 ± 3.41 kg/m2. The surgical procedures were TE/implant reconstruction (27.4%), mastectomy only (35.0%), and DIEP flap reconstruction (37.6%). Most patients underwent unilateral surgery (94.9%).
Table 1
| Item | Responders after 1 year | Responders after 5 years | ||
|---|---|---|---|---|
| N | Percent | N | Percent | |
| Number of patients | 141 | 100% | 131 | 100% |
| Age (years), mean (SD) | 53.2 (13.1) | 52.8 (12.8) | ||
| BMI (kg/m2), mean (SD) | 22.0 (3.41) | 22.2 (3.45) | ||
| Lesion | ||||
| Bilateral | 8 | 5.7% | 7 | 5.3% |
| Unilateral | 133 | 94.3% | 124 | 94.7% |
| Type of operation | ||||
| Mastectomy only | 51 | 36.2% | 45 | 34.4% |
| TE/Imp | 56 | 39.7% | 53 | 40.5% |
| DIEP | 34 | 24.1% | 33 | 25.2% |
| Radiotherapy | ||||
| No | 108 | 76.6% | 99 | 75.6% |
| Yes | 33 | 23.4% | 32 | 24.4% |
| Chemotherapy/hormone therapy | ||||
| No | 78 | 55.3% | 68 | 51.9% |
| Yes | 63 | 44.7% | 63 | 48.1% |
| Smoking | ||||
| Never | 108 | 76.6% | 100 | 76.3% |
| Past | 30 | 21.3% | 29 | 22.1% |
| Current | 3 | 2.1% | 2 | 1.5% |
| Psychotic/neurological medical history or medication | ||||
| No | 133 | 94.3% | 123 | 93.9% |
| Yes | 8 | 5.7% | 8 | 6.1% |
Demographics of the subjects.
SD, Standard deviation; BMI, Body mass index; TE/Imp, tissue expander/implant; DIEP, deep inferior epigastric perforator.
Regression analyses for patient-reported aesthetic satisfaction across 3 domains (“Satisfaction with breasts”, “Psychosocial well-being”, and “Physical well-being”) with mastectomy only, TE/Imp and DIEP at 1- and 5-year follow-up after surgery are listed in Table 2. These data were controlled for age, BMI, laterality, type of operation, radiation, chemotherapy, smoking, and psychotic/neurological medical history or medication.
Table 2
| Independent Variable | Satisfaction with breasts | Psychological well-being | Physical well-being | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Year 1 | Year 5 | Year 1 | Year 5 | Year 1 | Year 5 | |||||||
| Coefficient | P value | Coefficient | P value | Coefficient | P value | Coefficient | P value | Coefficient | P value | Coefficient | P value | |
| Age | 0.03 | 0.73 | 0.12 | 0.23 | 0.06 | 0.55 | -0.07 | 0.51 | -0.12 | 0.24 | -0.78 | 0.49 |
| BMI | -0.20 | 0.004** | -0.07 | 0.40 | -0.07 | 0.39 | -0.02 | 0.85 | 0.01 | 0.91 | 0.17 | 0.08 |
| Lesion | ||||||||||||
| Unilateral | Reference | Reference | Reference | Reference | Reference | Reference | ||||||
| Bilateral | -0.06 | 0.35 | -0.10 | 0.25 | -0.12 | 0.15 | -0.11 | 0.15 | 0.00 | 0.99 | -0.07 | 0.53 |
| Type of Operation | ||||||||||||
| Mastectomy Only | Reference | Reference | Reference | Reference | Reference | Reference | ||||||
| TE/ Imp | 0.61 | < 0.001*** | 0.46 | < 0.001*** | 0.43 | < 0.001*** | 0.25 | 0.03* | 0.02 | 0.88 | -0.08 | 0.53 |
| DIEP | 0.64 | < 0.001*** | 0.64 | < 0.001*** | 0.35 | < 0.001*** | 0.40 | < 0.001*** | 0.17 | 0.11 | -0.09 | 0.43 |
| Preoperative Radiation | ||||||||||||
| No | Reference | Reference | Reference | Reference | Reference | Reference | ||||||
| Yes | 0.02 | 0.79 | 0.10 | 0.26 | 0.01 | 0.87 | 0.12 | 0.17 | 0.08 | 0.37 | 0.16 | 0.10 |
| Chemotherapy | ||||||||||||
| No | Reference | Reference | Reference | Reference | Reference | Reference | ||||||
| Yes | 0.05 | 0.50 | 0.12 | 0.14 | 0.17 | 0.06 | -0.05 | 0.60 | -0.05 | 0.60 | 0.07 | 0.44 |
| Smoking | ||||||||||||
| Never | Reference | Reference | Reference | Reference | Reference | Reference | ||||||
| Past | 0.94 | 0.17 | -0.08 | 0.29 | 0.10 | 0.23 | 0.11 | 0.18 | -0.07 | 0.46 | -0.04 | 0.63 |
| Current | -0.54 | 0.43 | 0.03 | 0.71 | 0.06 | 0.47 | 0.05 | 0.57 | -0.07 | 0.54 | -0.01 | 0.93 |
| Psychotic/Neurological Medical History or Medication | ||||||||||||
| No | Reference | Reference | Reference | Reference | Reference | Reference | ||||||
| Yes | -0.02 | 0.83 | 0.03 | 0.73 | -0.05 | 0.56 | -0.15 | 0.84 | 0.20 | 0.02* | 0.17 | 0.08 |
Multiple regression analysis of factors associated with increased satisfaction or QOL for BREAST-Q domains.
BMI, Body mass index; TE/Imp, tissue expander/implant; DIEP, deep inferior epigastric perforator.
*P < 0.05. **P < 0.005. ***P < 0.001.
At 1-year postoperatively, “Satisfaction with breasts” was significantly impaired in patients with higher BMI (coefficient (β) -0.20, 95% confidence interval (CI) -1.89 to -0.38, p = 0.004). Compared to mastectomy only, TE/Imp and DIEP were both positively associated with “Satisfaction with breasts” (TE/Imp: β -0.61, 95%CI 16.62 to 30.51, p < 0.001; DIEP: β 0.64, 95% CI 21.31 to 35.81, p < 0.001) and “Psychosocial well-being” (TE/Imp: β 0.43, 95% CI 8.71 to 26.80, p < 0.001; DIEP: β 0.35, 95% CI 7.05 to 25.61, p < 0.001) at 1 year. History or medication for a psychotic/neurological condition was associated with greater “Physical well-being” (β 0.20, 95% CI 2.00 to 22.91, p = 0.02) at 1 year. At 5 years, compared to mastectomy only, TE/Imp and DIEP were positively associated with “Satisfaction with breasts” (TE/Imp: β 0.46, 95% CI 7.62 to 21.62, p < 0.001; DIEP: β 0.64, 95% CI 15.82 to 29.52, p < 0.001) and “Psychosocial well-being” (TE/Imp: β 0.25, 95%CI 0.95 to 20.29, p = 0.03; DIEP: β 0.40, 95%CI 9.32 to 28.53, p < 0.001). In addition, “Psychosocial well-being” significantly improved in patients with a bilateral procedure at 5 years (β 0.20, 95% CI -34.31 to -2.90, p = 0.02). No factors were significantly associated with “Physical well-being” at 5 years.
Comparisons of BREAST-Q scores among operative procedures in each year are shown in Figure 2. Mastectomy scored significantly lower than TE/Imp and DIEP for “Satisfaction with breasts” and “Psychosocial well-being” (both p < 0.001) at 1 year (all p < 0.001; Figures 2A, B) and 5 years (all p < 0.001, except p = 0.007 vs. DIEP for “Satisfaction with breasts”; Figures 2D, E). In addition, at 5 years, DIEP scored significantly higher than TE/Imp for “Satisfaction with breasts” (p < 0.001) (Figure 2D). Detailed results are shown in Table S1.
Figure 2
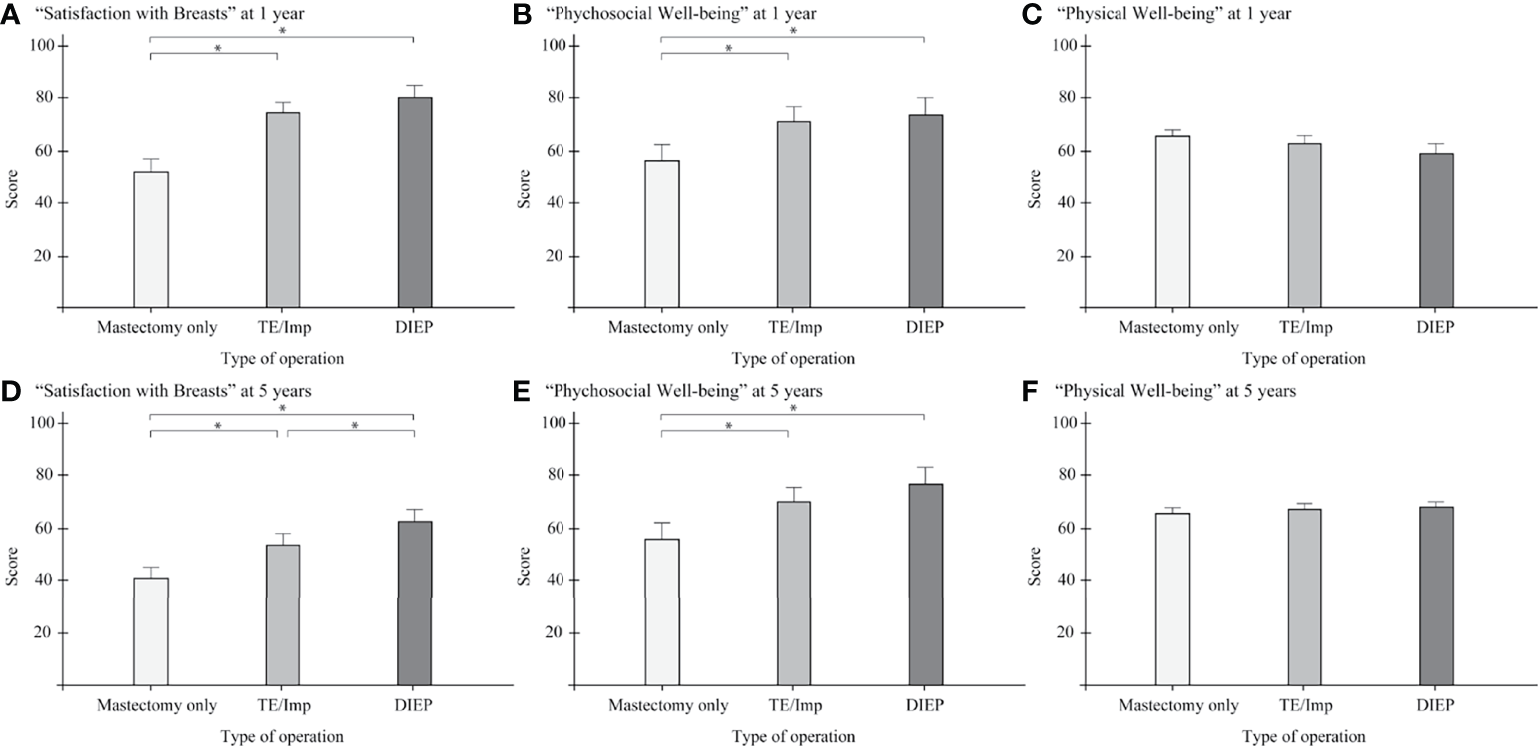
Comparison of BREAST-Q scores among operative procedures in each year, with 95% confidence intervals. (A) “Satisfaction with breasts” at 1 year; (B) “Psychosocial well-being” at 1 year; (C) “Physical well-being” at 1 year; (D) “Satisfaction with breasts” at 5 years; (E) “Psychosocial well-being” at 5 years; (F) “Physical well-being” at 5 years. TE/Imp, tissue expander/implant; DIEP, deep inferior epigastric perforator. *P < 0.05.
Comparisons of BREAST-Q scores between 1- and 5-year follow-up evaluations for each operative procedure are shown in Figure 3. Scores at 5 years were significantly lower than those at 1 year for “Satisfaction with breasts” for all three procedures (mastectomy only, p = 0.012; TE/Imp p < 0.001; DIEP, p < 0.001; Figures 3A, D, G) and for “Physical well-being” for two procedures (TE/Imp, p = 0.007; DIEP, p = 0.008; Figures 3E, H). Detailed results are shown in Table S2.
Figure 3
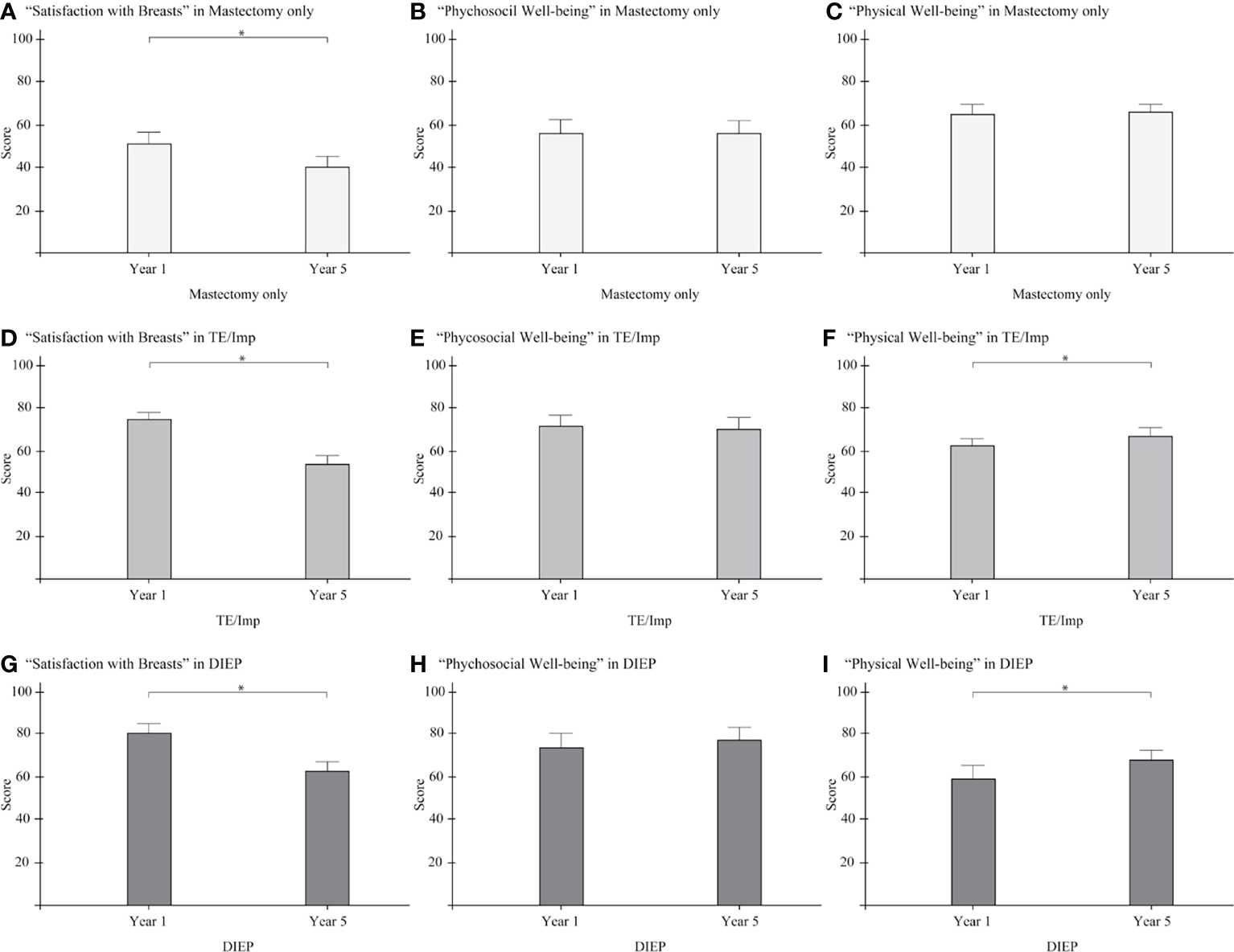
Comparison of BREAST-Q scores in 1- and 5-year follow-up evaluations for three operative procedures, with 95% confidence intervals. (A) “Satisfaction with breasts” in mastectomy only; (B) “Psychosocial well-being” in mastectomy only; (C) “Physical well-being” in mastectomy only; (D) “Satisfaction with breasts” in TE/Imp; (E) “Psychosocial well-being” in TE/Imp; (F) “Physical well-being” in TE/Imp; (G) “Satisfaction with breasts” in DIEP; (H) “Psychosocial well-being” in DIEP; (I) “Physical well-being” in DIEP. TE/Imp, tissue expander/implant; DIEP, deep inferior epigastric perforator. *P < 0.05.
Discussion
In this study, general and aesthetic satisfaction with breast operations including reconstruction were investigated at 1 and 5 years postoperatively in Japanese women. The main finding was that the type of operation was significantly associated with HRQoL-related domains of BREAST-Q at both 1 and 5 years in multivariate analysis. Over time, all surgical procedures had lower scores for “Satisfaction with breasts”, but “Psychosocial well-being” was maintained and “Physical well-being” improved after TE/Imp and DIEP. “Satisfaction with breasts” and “Psychosocial well-being” were lowest for mastectomy only at 1 and 5 years, and “Satisfaction with breasts” at 5 years was best after DIEP.
To our knowledge, there have been few long-term studies of HRQoL after breast surgery. Long-term evaluations of 5 years or more that have been performed are shown in Table 3 (32, 33, 35, 36). In the current study, the response rate and score for “Satisfaction with breasts” declined from postoperative year 1 to year 5. The lower response rate is consistent with previous studies showing a decline in response rate for PROs over time, as patients lose interest in the aesthetic impact of breast surgery (37–41). A lower score at a later time has also been found previously (42, 43) and is due to patients becoming used to the results of reconstruction over time. Thus, the time after the operation is an important factor associated with HRQoL.
Table 3
| Reference | Patient Base | Number of Patients | BREAST-Q Postop Follow-up Period | Scales | Protective factors | Risk factors |
|---|---|---|---|---|---|---|
| Hu et al. (32) | TE/Imp and TRAM | 219 | 6.5 years* | Satisfaction with breasts | TRAM | TE/Imp; early postoperative period |
| Ledibabari et al. (33) | Mammoplasty | 70 | 6 years* | Satisfaction with breasts | None | Obesity |
| Ticha et al. (34) | Implant-based reconstruction, abdominal-based autologous reconstruction, and combined reconstruction (with implant and LD flap or implant and TDAP flap) | 110 | 5 years | Satisfaction with breasts | Abdominal-based autologous reconstruction | None |
| Psychosocial well-being | Abdominal-based autologous reconstruction | None | ||||
| Physical well-being | Abdominal-based autologous reconstruction | None | ||||
| Dominici et al. (35) | Mastectomy, radiotherapy, and autologous flap | 290 | 5.8 years** | Satisfaction with Breasts | None | TE/Imp |
| Psychosocial well-being | None | None | ||||
| Physical well-being | None | Complex reconstruction (vs. autologous) |
Comparison of long-term breast reconstruction studies using BREAST-Q.
TE/Imp, tissue expander/implant; DIEP, deep inferior epigastric perforator; TRAM, transverse rectus abdominis myocutaneous; LD, latissimus dorsi flap; TDAP, thoracodorsal artery perforator flap.
*Mean; **Median.
Among patient factors, higher BMI was significantly negatively associated with “Satisfaction with breasts” at 1-year postoperatively, but not at 5 years. This is consistent with several reports showing that high BMI is an independent risk factor for lower satisfaction (44–46). However, most of these studies did not obtain baseline data using the preoperative module of BREAST-Q. Previous reports have also shown that obese patients tend to have higher rates of postoperative complications. However, in the current study, higher BMI at 5 years was not a risk factor, which suggests that these complications had resolved or that patients had become used to their postoperative status.
Psychotic/neurological medical history or medication was found to be a significant risk factor that lowers “Physical well-being” at 1 year after breast surgery. The questions in the “Physical well-being” domain are related to physical problems, including pain in the chest, back, abdomen or skin. Among psychological factors, preoperative levels of depression, anxiety, and psychological vulnerability to aberrant pain perception have been reported to be significantly associated with greater postoperative pain intensity, which may decrease physical morbidity (47–51). However, in a previous study, we found no significant association of psychotic/neurological medical history or medication with postoperative pain at one year after breast surgery in a similar cohort of Japanese patients to that in the current study (52). Thus, more psychiatrically oriented pain such as chronic postsurgical pain (CPSP) may have a negative effect on “Physical well-being” of patients (53).
A bilateral procedure was significantly associated with “Psychosocial well-being” at 5 years after breast surgery. Several studies focusing on bilateral breast operations have concluded that “Psychosocial well-being” after surgery significantly improves compared to the preoperative level (54, 55). These findings suggest that patients who underwent bilateral reconstruction were more satisfied due to improved symmetry and a superior aesthetic appearance.
Age was not found to be a significant factor associated with HRQoL among breast cancer survivors in the current study. However, this is still controversial because some reports indicate that implant and autogenous tissue techniques are associated with aging processes that can affect aesthetic appearance (56–60), whereas other studies did not find significant age-related differences using BREAST-Q (61–64). Reconstructive surgeons may avoid autologous reconstruction in older women due to complications following longer anesthetic times, but our results indicate that autologous procedures can be viable choices in older patients, given that age is not associated with greater risks and that autologous reconstruction in this population still achieves high HRQoL.
In this study, we focused on general and aesthetic well-being after breast surgery. Postoperative complications such as lymphedema, AWS, and fatigue can lower HRQoL, but intervention through rehabilitation can improve satisfaction (6–8). Risk factors for each complication have been described (65–68) and there are also several predictive methods for the complications. For example, de Sire et al. found that measuring the upper limb volume using a three-dimensional laser scanner was a reliable way to diagnose breast cancer-related lymphedema (69), and Nevola Teixeira et al. established a self-assessment questionnaire for AWS (70). A combination of BREAST-Q and these diagnostic methods is a promising approach for evaluation of complications.
The main strength of the study is the long-term evaluation of PROs for breast reconstruction. There are several limitations in the study. The main limitation was the response rates of 68.8% at 1 year and 63.9% at 5 years. However, these rates are similar to those in previous reports (71–73). Patients were followed for up to 5 years, but with such a long study period some could not be contacted or may have died, and were lost to follow up. It is also possible that there was a non-response bias, since patients who are still thinking about the complications of their breast reconstruction are more likely to respond to a questionnaire. We also did not examine the baseline status of the patients in terms of their well-being and satisfaction, and we were unable to assess changes in BMI in the postoperative period, which may influence patient satisfaction. However, in a retrospective study, Applebaum et al. found no significant change in BMI over time following implant-based or autologous breast reconstruction (74). The current study was also restricted to a single center with a relatively homogeneous patient population and evaluation, which could lead to potential selection bias. Finally, it was difficult to control for variability in operative techniques of surgeons and management of postoperative complications in statistical analysis.
In conclusion, the BREAST-Q score for “Physical well-being” was maintained at 5 years after breast reconstruction, and breast reconstruction procedures were better than mastectomy for “Satisfaction with breasts” and “Psychosocial well-being”. DIEP had the best scores among the three procedures at 5 years postoperatively. Thus, autologous reconstruction using a DIEP flap is recommended in terms of long-term satisfaction after breast surgery. These results are clinically useful for the choice of operative method by surgeons and patients. However, factors such as ethnic and regional differences may affect the results in other cohorts, and further research is required to promote better satisfaction with HRQoL after breast reconstruction.
Funding
Costs related to statistical analysis and manuscript publication were funded through the department of Plastic and Reconstructive Surgery, Kyoto Prefectural University of Medicine.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the ethics committee of Kyoto Prefectural University of Medicine, IRBMED Number ERB-C-563-1. The patients/participants provided their written informed consent to participate in this study.
Author contributions
MS and YS contributed to the conceptualization, methodology, investigation, and revision of the manuscript. MS wrote the original draft. TK and NI contributed to the collection of patient data, the investigation, and revision of the manuscript. IT and NM contributed to the revise of the article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2022.815498/full#supplementary-material
References
1
Heer E Harper A Escandor N Sung H McCormack V Fidler-Benaoudia MM . Global Burden and Trends in Premenopausal and Postmenopausal Breast Cancer: A Population-Based Study. Lancet Glob Health (2020) 8(8):e1027–37. doi: 10.1016/s2214-109x(20)30215-1
2
Nardin S Mora E Varughese FM D'Avanzo F Vachanaram AR Rossi V et al . Breast Cancer Survivorship, Quality of Life, and Late Toxicities. Front Oncol (2020) 10:864. doi: 10.3389/fonc.2020.00864
3
Invernizzi M Kim J Fusco N . Editorial: Quality of Life in Breast Cancer Patients and Survivors. Front Oncol (2020) 10:620574. doi: 10.3389/fonc.2020.620574
4
Nakamura K Okada E Ukawa S Hirata M Nagai A Yamagata Z et al . Characteristics and Prognosis of Japanese Female Breast Cancer Patients: The BioBank Japan Project. J Epidemiol (2017) 27(3S):S58–64. doi: 10.1016/j.je.2016.12.009
5
Saika K Sobue T . Time Trends in Breast Cancer Screening Rates in the OECD Countries. Jpn J Clin Oncol (2011) 41(4):591–2. doi: 10.1093/jjco/hyr044
6
Pappalardo M Starnoni M Franceschini G Baccarani A De Santis G . Breast Cancer-Related Lymphedema: Recent Updates on Diagnosis, Severity and Available Treatments. J Pers Med (2021) 11(5):402. doi: 10.3390/jpm11050402
7
de Sire A Losco L Cisari C Gennari A Boldorini R Fusco N et al . Axillary Web Syndrome in Women After Breast Cancer Surgery Referred to an Oncological Rehabilitation Unit: Which Are the Main Risk Factors? A Retrospective Case-Control Study. Eur Rev Med Pharmacol Sci (2020) 24(15):8028–35. doi: 10.26355/eurrev_202008_22486
8
Invernizzi M de Sire A Lippi L Venetis K Sajjadi E Gimigliano F et al . Impact of Rehabilitation on Breast Cancer Related Fatigue: A Pilot Study. Front Oncol (2020) 10:556718. doi: 10.3389/fonc.2020.556718
9
Dean C Chetty U Forrest AP . Effects of Immediate Breast Reconstruction on Psychosocial Morbidity After Mastectomy. Lancet (1983) 1(8322):459–62. doi: 10.1016/s0140-6736(83)91452-6
10
Heil J Czink E Golatta M Schott S Hof H Jenetzky E et al . Change of Aesthetic and Functional Outcome Over Time and Their Relationship to Quality of Life After Breast Conserving Therapy. Eur J Surg Oncol (2011) 37(2):116–21. doi: 10.1016/j.ejso.2010.11.007
11
Waljee JF Hu ES Ubel PA Smith DM Newman LA Alderman AK . Effect of Esthetic Outcome After Breast-Conserving Surgery on Psychosocial Functioning and Quality of Life. J Clin Oncol (2008) 26(20):3331–7. doi: 10.1200/JCO.2007.13.1375
12
Davies CF Macefield R Avery K Blazeby JM Potter S . Patient-Reported Outcome Measures for Post-Mastectomy Breast Reconstruction: A Systematic Review of Development and Measurement Properties. Ann Surg Oncol (2021) 28(1):386–404. doi: 10.1245/s10434-020-08736-8
13
Pusic AL Klassen AF Scott AM Klok JA Cordeiro PG Cano SJ . Development of a New Patient-Reported Outcome Measure for Breast Surgery: The BREAST-Q. Plast Reconstr Surg (2009) 124(2):345–53. doi: 10.1097/PRS.0b013e3181aee807
14
Cano SJ Klassen AF Scott AM Cordeiro PG Pusic AL . The BREAST-Q: Further Validation in Independent Clinical Samples. Plast Reconstr Surg (2012) 129(2):293–302. doi: 10.1097/PRS.0b013e31823aec6b
15
Cohen WA Mundy LR Ballard TN Klassen A Cano SJ Browne J et al . The BREAST-Q in Surgical Research: A Review of the Literature 2009-2015. J Plast Reconstr Aesthet Surg (2016) 69(2):149–62. doi: 10.1016/j.bjps.2015.11.013
16
Stolpner I Heil J Feißt M Karsten MM Weber WP Blohmer JU et al . Clinical Validation of the BREAST-Q Breast-Conserving Therapy Module. Ann Surg Oncol (2019) 26(9):2759–67. doi: 10.1245/s10434-019-07456-y
17
Nano MT Gill PG Kollias J Bochner MA Malycha P Winefield HR . Psychological Impact and Cosmetic Outcome of Surgical Breast Cancer Strategies. ANZ J Surg (2005) 75(11):940–7. doi: 10.1111/j.1445-2197.2005.03517.x
18
Saulis AS Mustoe TA Fine NA . A Retrospective Analysis of Patient Satisfaction With Immediate Postmastectomy Breast Reconstruction: Comparison of Three Common Procedures. Plast Reconstr Surg (2007) 119(6):1669–76. doi: 10.1097/01.prs.0000258827.21635.84
19
Mosahebi A Ramakrishnan V Gittos M Collier J . Aesthetic Outcome of Different Techniques of Reconstruction Following Nipple-Areola-Preserving Envelope Mastectomy With Immediate Reconstruction. Plast Reconstr Surg (2007) 119(3):796–803. doi: 10.1097/01.prs.0000251999.52374.09
20
Tykkä E Asko-Seljavaara S Hietanen H . Patient Satisfaction With Delayed Breast Reconstruction: A Prospective Study. Ann Plast Surg (2002) 49(3):258–63. doi: 10.1097/01.SAP.0000015487.09561.62
21
Tykkä E Asko-Seljavaara S Hietanen H . Patients' Satisfaction With Breast Reconstruction and Reduction Mammaplasty. Scand J Plast Reconstr Surg Handb Surg (2001) 35(4):399–405. doi: 10.1080/028443101317149363
22
Kovacs L Papadopulos NA Ammar SA Klöppel M Herschbach P Heinrich G et al . Clinical Outcome and Patients' Satisfaction After Simultaneous Bilateral Breast Reconstruction With Free Transverse Rectus Abdominis Muscle (TRAM) Flap. Ann Plast Surg (2004) 53(3):199–204. doi: 10.1097/01.sap.0000120525.86997.52
23
Ramon Y Ullmann Y Moscona R Ofiram E Tamir A Har-Shai Y et al . Aesthetic Results and Patient Satisfaction With Immediate Breast Reconstruction Using Tissue Expansion: A Follow-Up Study. Plast Reconstr Surg (1997) 99(3):686–91. doi: 10.1097/00006534-199703000-00013
24
Simon AM Bouwense CL McMillan S Lamb S Hammond DC . Comparison of Unipedicled and Bipedicled TRAM Flap Breast Reconstructions: Assessment of Physical Function and Patient Satisfaction. Plast Reconstr Surg (2004) 113(1):136–40. doi: 10.1097/01.PRS.0000095939.19970.D5
25
Moscona RA Holander L Or D Fodor L . Patient Satisfaction and Aesthetic Results After Pedicled Transverse Rectus Abdominis Muscle Flap for Breast Reconstruction. Ann Surg Oncol (2006) 13(12):1739–46. doi: 10.1245/s10434-006-9096-7
26
Stolpner I Heil J Riedel F Wallwiener M Schäfgen B Feißt M et al . Long-Term Patient Satisfaction and Quality of Life After Breast-Conserving Therapy: A Prospective Study Using the BREAST-Q. Ann Surg Oncol (2021) 28:8742–51. doi: 10.1245/s10434-021-10377-4
27
Lantz PM Janz NK Fagerlin A Schwartz K Liu L Lakhani I et al . Satisfaction With Surgery Outcomes and the Decision Process in a Population-Based Sample of Women With Breast Cancer. Health Serv Res (2005) 40(3):745–67. doi: 10.1111/j.1475-6773.2005.00383.x
28
Alderman AK Wilkins EG Lowery JC Kim M Davis JA . Determinants of Patient Satisfaction in Postmastectomy Breast Reconstruction. Plast Reconstr Surg (2000) 106(4):769–76. doi: 10.1097/00006534-200009040-00003
29
Howes BH Watson DI Xu C Fosh B Canepa M Dean NR . Quality of Life Following Total Mastectomy With and Without Reconstruction Versus Breast-Conserving Surgery for Breast Cancer: A Case-Controlled Cohort Study. J Plast Reconstr Aesthet Surg (2016) 69(9):1184–91. doi: 10.1016/j.bjps.2016.06.004
30
Shiraishi M Sowa Y Inafuku N . Long-Term Survey of Sexual Well-Being After Breast Reconstruction Using the BREAST-Q in the Japanese Population. Asian J Surg, S1015–9584(22)00108-7. doi: 10.1016/j.asjsur.2022.02.007
31
Saiga M Taira N Kimata Y Watanabe S Mukai Y Shimozuma K et al . Development of a Japanese Version of the BREAST-Q and the Traditional Psychometric Test of the Mastectomy Module for the Assessment of HRQOL and Patient Satisfaction Following Breast Surgery. Breast Cancer (2017) 24(2):288–98. doi: 10.1007/s12282-016-0703-6
32
Hu ES Pusic AL Waljee JF Kuhn L Hawley ST Wilkins E et al . Patient-Reported Aesthetic Satisfaction With Breast Reconstruction During the Long-Term Survivorship Period. Plast Reconstr Surg (2009) 124(1):1–8. doi: 10.1097/PRS.0b013e3181ab10b2
33
Ngaage LM Bai J Gebran S Elegbede A Ihenatu C Nam AJ et al . A 12-Year Review of Patient-Reported Outcomes After Reduction Mammoplasty in Patients With High Body Mass Index. Med (Baltimore) (2019) 98(25):e16055. doi: 10.1097/MD.0000000000016055
34
Ticha P Mestak O Wu M Bujda M Sukop A . Patient-Reported Outcomes of Three Different Types of Breast Reconstruction With Correlation to the Clinical Data 5 Years Postoperatively. Aesthetic Plast Surg (2020) 44(6):2021–9. doi: 10.1007/s00266-020-01926-5
35
Dominici L Hu J Zheng Y Kim HJ King TA Ruddy KJ et al . Association of Local Therapy With Quality-Of-Life Outcomes in Young Women With Breast Cancer. JAMA Surg (2021) 156(10):e213758. doi: 10.1001/jamasurg.2021.3758
36
Ticha P Wu M Mestak O Sukop A . Evaluation of the Number of Follow-Up Surgical Procedures and Time Required for Delayed Breast Reconstruction by Clinical Risk Factors, Type of Oncological Therapy, and Reconstruction Approach. Aesthetic Plast Surg (2021) 46(1):71–82. doi: 10.1007/s00266-021-02580-1
37
Reinholdsson J Kraus-Schmitz J Forssblad M Edman G Byttner M Stålman A . A non-Response Analysis of 2-Year Data in the Swedish Knee Ligament Register. Knee Surg Sports Traumatol Arthrosc (2017) 25(8):2481–7. doi: 10.1007/s00167-015-3969-x
38
Juto H Gärtner Nilsson M Möller M Wennergren D Morberg P . Evaluating non-Responders of a Survey in the Swedish Fracture Register: No Indication of Different Functional Result. BMC Musculoskelet Disord (2017) 18(1):278. doi: 10.1186/s12891-017-1634-x
39
Patel J Lee JH Li Z SooHoo NF Bozic K Huddleston JI 3rd . Predictors of Low Patient-Reported Outcomes Response Rates in the California Joint Replacement Registry. J Arthroplasty (2015) 30(12):2071–5. doi: 10.1016/j.arth.2015.06.029
40
Wang K Eftang CN Jakobsen RB Årøen A . Review of Response Rates Over Time in Registry-Based Studies Using Patient-Reported Outcome Measures. BMJ Open (2020) 10(8):e030808. doi: 10.1136/bmjopen-2019-030808
41
Liu LQ Branford OA Mehigan S . BREAST-Q Measurement of the Patient Perspective in Oncoplastic Breast Surgery: A Systematic Review. Plast Reconstr Surg Glob Open (2018) 6(8):e1904. doi: 10.1097/GOX.0000000000001904
42
Flanagan MR Zabor EC Romanoff A Fuzesi S Stempel M Mehrara BJ et al . A Comparison of Patient-Reported Outcomes After Breast-Conserving Surgery and Mastectomy With Implant Breast Reconstruction. Ann Surg Oncol (2019) 26(10):3133–40. doi: 10.1245/s10434-019-07548-9
43
Santosa KB Qi J Kim HM Hamill JB Wilkins EG Pusic AL . Long-Term Patient-Reported Outcomes in Postmastectomy Breast Reconstruction. JAMA Surg (2018) 153(10):891–9. doi: 10.1001/jamasurg.2018.1677
44
Atisha DM Rushing CN Samsa GP Locklear TD Cox CE Shelley Hwang E et al . A National Snapshot of Satisfaction With Breast Cancer Procedures. Ann Surg Oncol (2015) 22(2):361–9. doi: 10.1245/s10434-014-4246-9
45
O'Connell RL DiMicco R Khabra K O'Flynn EA deSouza N Roche N et al . Initial Experience of the BREAST-Q Breast-Conserving Therapy Module. Breast Cancer Res Treat (2016) 160(1):79–89. doi: 10.1007/s10549-016-3966-x
46
Nelson JA Sobti N Patel A Matros E McCarthy CM Dayan JH et al . The Impact of Obesity on Patient-Reported Outcomes Following Autologous Breast Reconstruction. Ann Surg Oncol (2020) 27(6):1877–88. doi: 10.1245/s10434-019-08073-5
47
Ip HY Abrishami A Peng PW Wong J Chung F . Predictors of Postoperative Pain and Analgesic Consumption: A Qualitative Systematic Review. Anesthesiology (2009) 111(3):657–77. doi: 10.1097/ALN.0b013e3181aae87a
48
Kulkarni AR Pusic AL Hamill JB Kim HM Qi J Wilkins EG et al . Factors Associated With Acute Postoperative Pain Following Breast Reconstruction. JPRAS Open (2017) 11:1–13. doi: 10.1016/j.jpra.2016.08.005
49
Munafò MR Stevenson J . Anxiety and Surgical Recovery. Reinterpreting the Literature. J Psychosom Res (2001) 51(4):589–96. doi: 10.1016/s0022-3999(01)00258-6
50
Khan RS Ahmed K Blakeway E Skapinakis P Nihoyannopoulos L Macleod K et al . Catastrophizing: A Predictive Factor for Postoperative Pain. Am J Surg (2011) 201(1):122–31. doi: 10.1016/j.amjsurg.2010.02.007
51
Pinto PR McIntyre T Almeida A Araújo-Soares V . The Mediating Role of Pain Catastrophizing in the Relationship Between Presurgical Anxiety and Acute Postsurgical Pain After Hysterectomy. Pain (2012) 153(1):218–26. doi: 10.1016/j.pain.2011.10.020
52
Shiraishi M Sowa Y Fujikawa K Kodama T Okamoto A Numajiri T et al . Factors Associated With Chronic Pain Following Breast Reconstruction in Japanese Women. J Plast Surg Handb Surg (2020) 54(5):317–22. doi: 10.1080/2000656X.2020.1780246
53
Weinrib AZ Azam MA Birnie KA Burns LC Clarke H Katz J . The Psychology of Chronic Post-Surgical Pain: New Frontiers in Risk Factor Identification, Prevention and Management. Br J Pain (2017) 11(4):169–77. doi: 10.1177/2049463717720636
54
Klapdor R Weiß C Kuehnle E Kohls F von Ehr J Philippeit A et al . Quality of Life After Bilateral and Contralateral Prophylactic Mastectomy With Implant Reconstruction. Breast Care (Basel) (2020) 15(5):519–26. doi: 10.1159/000505449
55
Wampler AT Powelson IA Homa K Freed GL . BREAST-Q Outcomes Before and After Bilateral Reduction Mammaplasty. Plast Reconstr Surg (2021) 147(3):382e–90e. doi: 10.1097/PRS.0000000000007605
56
Alderman AK Kuhn LE Lowery JC Wilkins EG . Does Patient Satisfaction With Breast Reconstruction Change Over Time? Two-Year Results of the Michigan Breast Reconstruction Outcomes Study. J Am Coll Surg (2007) 204(1):7–12. doi: 10.1016/j.jamcollsurg.2006.09.022
57
Clough KB O'Donoghue JM Fitoussi AD Nos C Falcou MC . Prospective Evaluation of Late Cosmetic Results Following Breast Reconstruction: I. Implant Reconstruction. Plast Reconstr Surg (2001) 107(7):1702–9. doi: 10.1097/00006534-200106000-00010
58
Clough KB O'Donoghue JM Fitoussi AD Vlastos G Falcou MC . Prospective Evaluation of Late Cosmetic Results Following Breast Recon- Struction: II. TRAM Flap Reconstruction. Plast Reconstr Surg (2001) 107:1710–6. doi: 10.1097/00006534-200106000-00011
59
Spear SL Onyewu C . Staged Breast Reconstruction With Saline-Filled Implants in the Irradiated Breast: Recent Trends and Therapeutic Implications. Plast Reconstr Surg (2000) 105(3):930–42. doi: 10.1097/00006534-200003000-00016
60
Yang B Li L Yan W Chen J Chen Y Hu Z et al . The Type of Breast Reconstruction May Not Influence Patient Satisfaction in the Chinese Population: A Single Institutional Experience. PloS One (2015) 10(11):e0142900. doi: 10.1371/journal.pone.0142900
61
Song D Slater K Papsdorf M Van Laeken N Zhong T Hazen A et al . Autologous Breast Reconstruction in Women Older Than 65 Years Versus Women Younger Than 65 Years: A Multi-Center Analysis. Ann Plast Surg (2016) 76(2):155–63. doi: 10.1097/SAP.0000000000000527
62
August DA Wilkins E Rea T . Breast Reconstruction in Older Women. Surgery (1994) 115(6):663–8.
63
Bowman CC Lennox PA Clugston PA Courtemanche DJ . Breast Reconstruction in Older Women: Should Age be an Exclusion Criterion? Plast Reconstr Surg (2006) 118(1):16–22. doi: 10.1097/01.prs.0000220473.94654.a4
64
Santosa KB Qi J Kim HM Hamill JB Pusic AL Wilkins EG . Effect of Patient Age on Outcomes in Breast Reconstruction: Results From a Multicenter Prospective Study. J Am Coll Surg (2016) 223(6):745–54. doi: 10.1016/j.jamcollsurg.2016.09.003
65
Monleon S Murta-Nascimento C Bascuas I Macià F Duarte E Belmonte R . Lymphedema Predictor Factors After Breast Cancer Surgery: A Survival Analysis. Lymphat Res Biol (2015) 13(4):268–74. doi: 10.1089/lrb.2013.0042
66
Martínez-Jaimez P Armora Verdú M Forero CG Álvarez Salazar S Fuster Linares P Monforte Royo C et al . Breast Cancer-Related Lymphoedema: Risk Factors and Prediction Model. J Adv Nurs (2022) 78(3):765–75. doi: 10.1111/jan.15005
67
Tay MRJ Wong CJ Aw HZ . Prevalence and Associations of Axillary Web Syndrome in Asian Women After Breast Cancer Surgery Undergoing a Community-Based Cancer Rehabilitation Program. BMC Cancer (2021) 21(1):1019. doi: 10.1186/s12885-021-08762-z
68
de Sire A Invernizzi M Lippi L Cisari C Özçakar L Franchignoni F . Blurred Lines Between Axillary Web Syndrome and Mondor's Disease After Breast Cancer Surgery: A Case Report. Ann Phys Rehabil Med (2020) 63(4):365–7. doi: 10.1016/j.rehab.2019.04.007
69
de Sire A Losco L Cigna E Lippi L Gimigliano F Gennari A et al . Three-Dimensional Laser Scanning as a Reliable and Reproducible Diagnostic Tool in Breast Cancer Related Lymphedema Rehabilitation: A Proof-of-Principle Study. Eur Rev Med Pharmacol Sci (2020) 24(8):4476–85. doi: 10.26355/eurrev_202004_21030
70
Nevola Teixeira LF Veronesi P Lohsiriwat V Luini A Schorr MC Garusi C et al . Axillary Web Syndrome Self-Assessment Questionnaire: Initial Development and Validation. Breast (2014) 23(6):836–43. doi: 10.1016/j.breast.2014.09.001
71
García-Solbas S Lorenzo-Liñán MÁ Castro-Luna G . Long-Term Quality of Life (BREAST-Q) in Patients With Mastectomy and Breast Reconstruction. Int J Environ Res Public Health (2021) 18(18):9707. doi: 10.3390/ijerph18189707
72
Thorarinsson A Fröjd V Kölby L Ljungdal J Taft C Mark H . Long-Term Health-Related Quality of Life After Breast Reconstruction: Comparing 4 Different Methods of Reconstruction. Plast Reconstr Surg Glob Open (2017) 5(6):e1316. doi: 10.1097/GOX.0000000000001316
73
Gass JS Onstad M Pesek S Rojas K Fogarty S Stuckey A et al . Breast-Specific Sensuality and Sexual Function in Cancer Survivorship: Does Surgical Modality Matter? Ann Surg Oncol (2017) 24(11):3133–40. doi: 10.1245/s10434-017-5905-4
74
Applebaum MA Miller BT Lopez J Doren EL Laronga C Smith PD . Change in Body Mass Index After Breast Reconstruction and Associated Complications. Eplasty (2015) 15:e43.
Summary
Keywords
breast reconstruction, tissue expander, breast implant, DIEP, BREAST-Q, health-related quality of life
Citation
Shiraishi M, Sowa Y, Tsuge I, Kodama T, Inafuku N and Morimoto N (2022) Long-Term Patient Satisfaction and Quality of Life Following Breast Reconstruction Using the BREAST-Q: A Prospective Cohort Study. Front. Oncol. 12:815498. doi: 10.3389/fonc.2022.815498
Received
15 November 2021
Accepted
20 April 2022
Published
23 May 2022
Volume
12 - 2022
Edited by
Mangesh A. Thorat, Guy’s and St Thomas’ NHS Foundation Trust, United Kingdom
Reviewed by
Julio de la Torre, Comillas Pontifical University, Spain; Marco Invernizzi, University of Eastern Piedmont, Italy; Alessandro de Sire, University of Magna Graecia, Italy
Updates
Copyright
© 2022 Shiraishi, Sowa, Tsuge, Kodama, Inafuku and Morimoto.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yoshihiro Sowa, sowawan@koto.kpu-m.ac.jp
This article was submitted to Breast Cancer, a section of the journal Frontiers in Oncology
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.