- 1Department of Health Management Center, West China Hospital, Sichuan University, Chengdu, Sichuan, China
- 2Department of Industrial Engineering and Engineering Management, College of Business, Sichuan University, Chengdu, Sichuan, China
- 3Integrated Care Management Center, West China Hospital, Sichuan University, Chengdu, Sichuan, China
The study aimed to investigate the influencing factors of physicians in recommending low-dose computed tomography (LDCT) for lung cancer screening to high-risk groups. A total of 1767 participants with good knowledge of LDCT were included in a cross-sectional study. Data about physicians’ demographics, perception of barriers on LDCT screening, medical conditions for practicing medicine and the behavior of recommending LDCT were collected by a questionnaire. Physicians who care about the transportation convenience of patients were less likely to recommend LDCT (OR 0.568, 95% CI (0.423 to 0.763), p < 0.05). The physicians who considered LDCT expensive, recommended LDCT less than others (OR 0.308, 95% CI (0.186 to 0.510), p < 0.05). The false positive rate of LDCT can decrease the possibility of physicians’ recommending (OR 0.542, 95% CI (0.387 to 0.758), p < 0.05). The physicians in oncology department and health management center were more likely to recommend LDCT (OR 2.282, 95% CI (1.557 to 3.345); OR 2.476, 95% CI (1.618 to 3.791)). The convenience of transportation, the price, and the\ false positive rate may be the main concerns among physicians on recommending LDCT to high-risk groups. The influencing factors of physicians’ recommending on LDCT was various. Information technology, government support in price and self-improvement of LDCT should be gathered together to break the barriers on physicians’ recommending on LDCT.
1. Introduction
Worldwide, lung cancer is currently the most common cancer, accounting for 11.6% of all cancers and the leading cause of cancer-related mortality, responsible for 18.4% of overall cancer mortality in both men and women (1). Similarly, lung cancer is the most common cancer in China (2), accounting for 20% of all cancers and 27% of all cancer-related death (3). Previous studies, such as US National Lung Screening Trial (NLST) and the German Lung cancer Screening Intervention (LUSI), have shown that lung cancer screening by low-dose computed tomography (LDCT) effectively reduces lung cancer mortality (4, 5). However, the screening benefits are largely dependent on the high-risk population’s attendance. Currently, lung cancer screening is performed in many countries, but the screening compliance is mostly lower than 60% (6, 7). In China, previous studies revealed that lung cancer screening compliance is lower, roughly reaching forty percent (8, 9).
And Since healthcare workers are often the primary source of health-related information for patients (10, 11), and the decision of lung cancer related examinations were always made by pulmonologist, so the physician especially the lung cancer related doctors are likely to play the key role in promoting the screening compliance.
Improving understanding of lung cancer screening knowledge among doctors may increase utilization of LDCT has been proved by many studies (12–14). But we found the perceptions of barriers on screening were similar among the doctors whether aware of the knowledge of LDCT (12). In other words, there is a possibility that doctors who aware of the knowledge of lung cancer will not recommend LDCT to high-risk groups. Therefore, this study is devoted to discuss the factors that influence the recommendation of LDCT to high-risk groups by physicians with good knowledge and which point has rarely been mentioned in previous studies. Understanding the factors influencing the doctors’ recommendation of LDCT can help guide future interventions aimed at promoting the screening rate.
According to some classical theory of framework, some personal factors and organizational factors were deemed to be the main factors to improve doctors’ compliance on recommending LDCT (15). And we combined with existing studies, the sociodemographic characteristics of doctors (16), the perceptions of barriers on LDCT (12) and medical conditions for practicing medicine (17, 18) may influence medical personnel’s medical behavior decision. The mechanisms of human behavior are complex, so we want to combine these factors to discuss how they influence doctors’ behavior.
2. Materials and methods
2.1. Participants
In this cross-sectional study, a convenience sample of physicians at a general hospital who were willing to participate were recruited. These physicians all came from Sichuan Province, China. The majority of them belonged to departments that were related to lung cancer, including the respiratory department, thoracic surgery department, oncology department, and health management center, a few of them from other departments. Excluding the missing date from any of the variables used in the present study, 1767 physicians remained. These physicians had all self-reported they had finished networking learning of lung cancer related knowledge from West China Hospital and had a good self-evaluation about grasping the knowledge of LDCT.
2.2. Survey questionnaire
The survey contained four sections:(1) The doctors’ sociodemographic characteristics, and in this study included gender, age, education, professional title, department, and experience. (2) The doctors’ perception of barriers on LDCT screening, and by combining with existing studies, we find the high price of LDCT (19), false positive rate (20, 21), frequent radiation (22, 23), and its mental impact (24) are major perceptions of barriers on LDCT recommending among doctors. So, we used the four questions “Do you consider the price of low-dose spiral CT expensive?”, “Do you think the false positive rate of LDCT is high?”, “Do you think radiation exposure to LDCT is unacceptable compared with chest X-ray, sputum, and other screening methods?” and “Do you think the mental burden imposed on patients by LDCT is unacceptable?” to measure respectively. And combining with the harsh geography in Sichuan province, we added the convenience of transportation as one more barrier, which was measured by the question “will you consider the convenience of transportation for patients to seek for medical service?”. All items were yes-no questions. (3) Medical conditions for practicing medicine in this study were defined by the availability of LDCT, and hospital level. (4) The behavior of recommending LDCT which was measured by the question “Have you recommended LDCT to high-risk groups in the past 12 months?”. The item was yes-no question.
2.3. Data collection
The Wenjuanxing platform, one of the leading companies in online questionnaire data collection in China, handled data collection. The survey was distributed to the physicians via WeChat (a popular social application in China). Each participant had the right to decide whether to participate in the study and could withdraw from the study at any time. Before the content of the questionnaire was presented, a page showing the objectives of this study and soliciting informed consent from the participants was presented. If the participants provided informed consent, they could continue to complete the questionnaire. Every questionnaire was check by two investigators for logistic errors and missing items. Questionnaires with more than 20% missing items were eliminated. Finally, 1767 complete responses were received.
2.4. Statistical analysis
Data provided by the questionnaires in Wenjuanxing were entered into the Microsoft Excel program and double-checked before analysis. And the data were imported into SPSS 23.0 for statistical analysis. Descriptive statistics, including frequency (n) and percentage (%) were used to express the distribution of data. The variables between the recommendation and no-recommendation groups were compared using the Chi-square method.
And then a multivariable logistic regression analysis was conducted to explore the predictors of the physicians’ recommendation of LDCT to high-risk groups. All variables with a significant association with the recommending behavior in aforementioned univariate tests and other variables had closely relationship with the recommending behavior according to previous studies were into the multivariable logistic regression model. The results of logistic regression are presented as odds ratios (OR) with 95% confidence intervals (CI). We performed Hosmer and Leeshawn’s goodness-of-fit test to identify if our model had a good fit with a P-value >0.05. And a two-tailed P<0.05 was viewed as statistically significant.
3. Results
3.1. The characteristics of participants
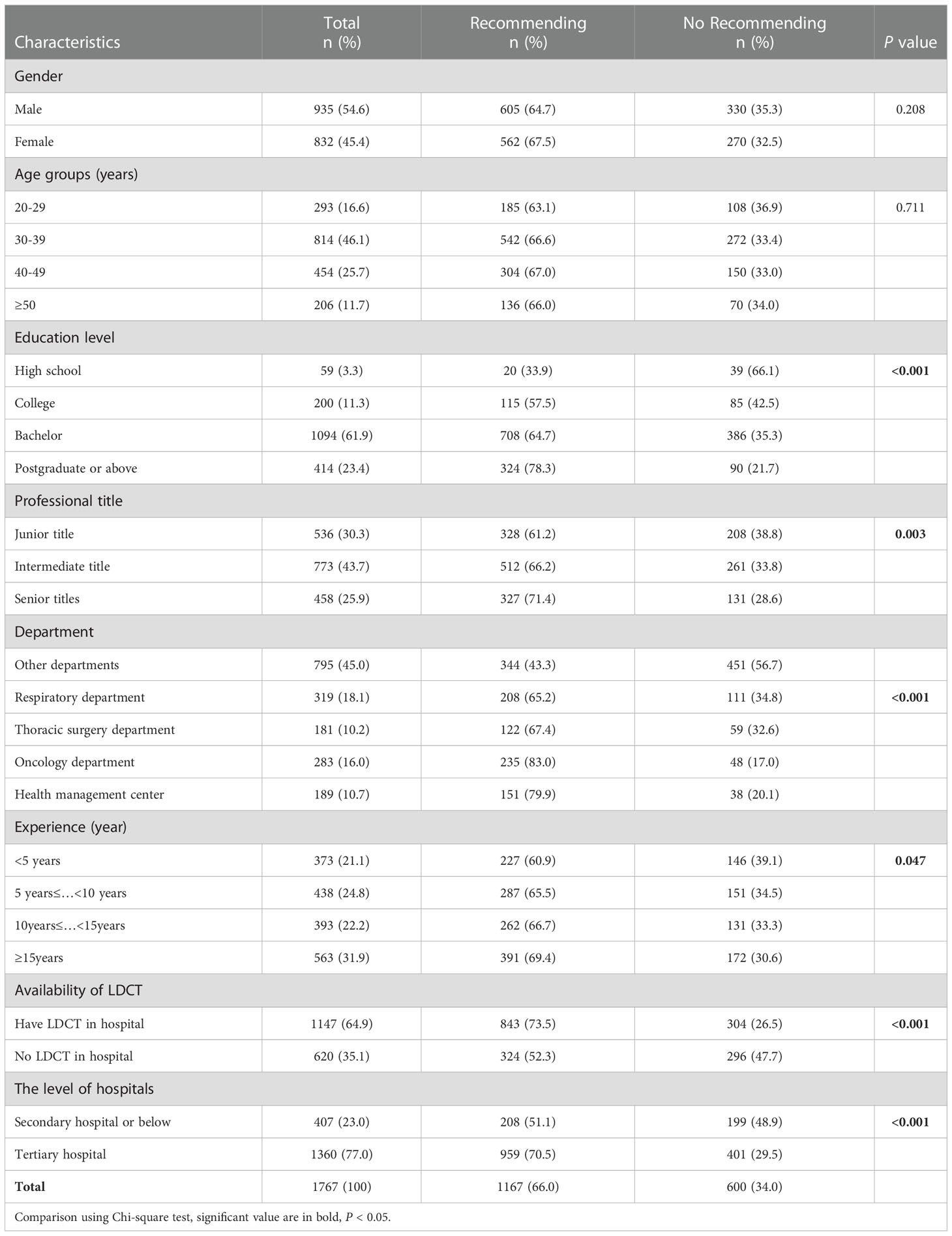
Table 1 shows the result of univariable analysis. Among the 1767 physicians, 66% self-reported that they had recommended LDCT to high-risk groups in past 12 month. There were significant differences in the education level, professional title, department, working experience, availability of LDCT and the level of hospitals (P<0.05). However, no statistically significant differences were found in gender, and age group (P>0.05).
3.2. Perception of barriers on LDCT screening among physicians
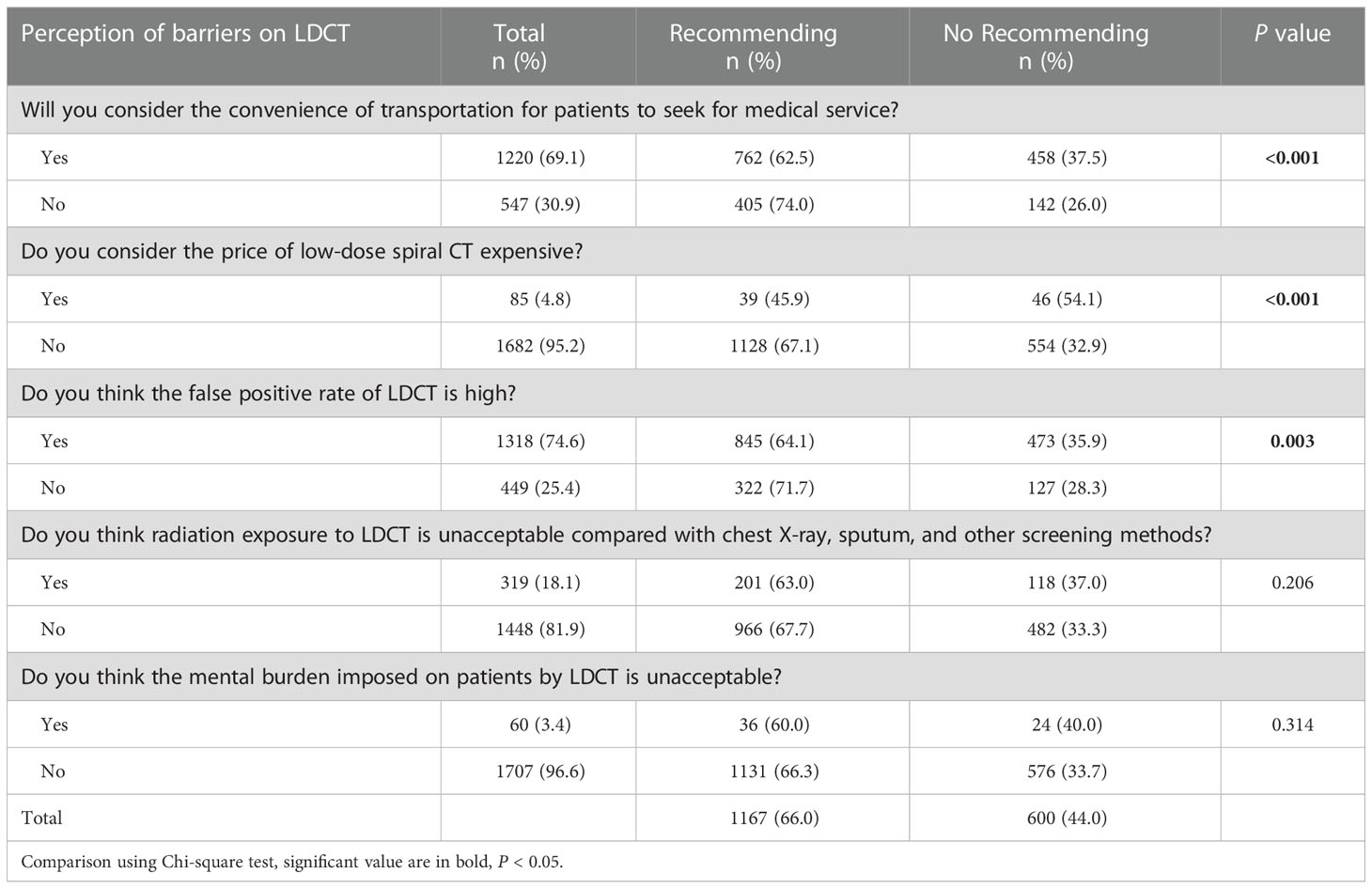
Table 2 shows the result of univariate analysis. The perception of barriers on the convenience of transportation, the price and the false positive rate were statistically significant between two groups of recommendation and no-recommendation(P<0.05). And the difference of two group on the radiation exposure and mental burden were statistically insignificant(P>0.05).
3.3. Multiple-factor analysis
We included all variables in univariate analysis that had a significant association with the recommending behavior, and the all perception of barriers whether statistically significant or not in the univariate analysis for these barriers had been proved by many previous studies (22–24).
Table 3 shows the convenience of transportation (OR=0.568, 95%CI=0.423-0.763), the price of LDCT screening (OR=0.308, 95%CI=0.186-0.510), and the false positive outcome (OR=0.708, 95%CI=0.521-0.961) may be physicians’ main concern on whether recommending LDCT to high-risk groups.
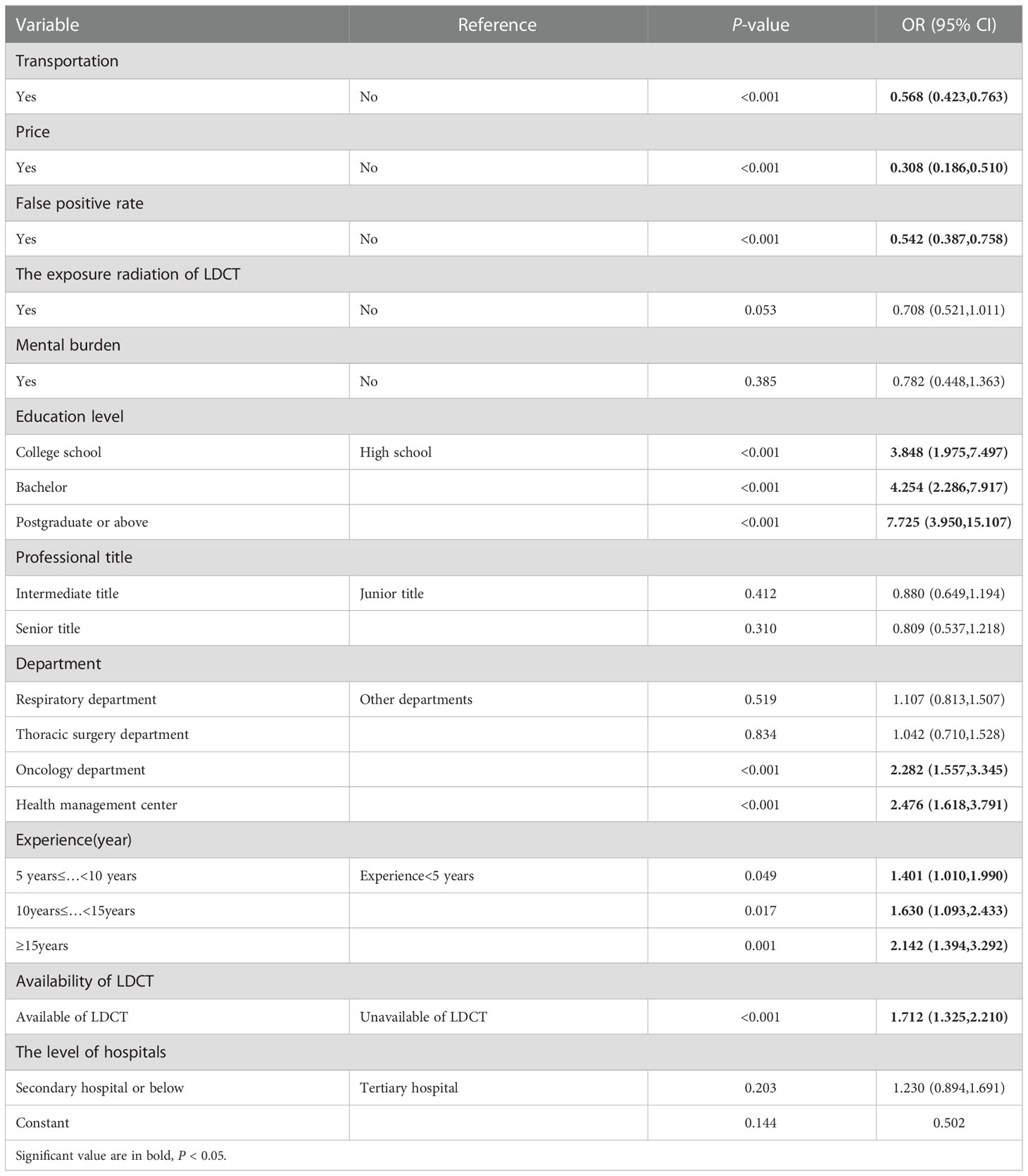
Table 3 The multivariable logistic regression for factors influencing physicians’ recommendation on LDCT to high-risk groups.
The following factors were associated with a higher possibility of recommending LDCT to high-risk groups: higher education level [OR (95%CI):3.848(1.975,7.497),4.254(2.286,7.917), and7.725(3.950,15.107) for college school, Bachelor, and Postgraduate or above, respectively], the longer work experience [OR (95%CI): 1.401(1.010,1.990), 1.630(1.093,2.433), 2.142(1.394,3.292) for different work experience], the availability of LDCT(OR=1.712,95%CI=1.325,2.210). Compared to other departments, the physicians in Oncology department (OR=2.282,95%CI=1.557-3.345) and Health management center (OR=2.476,95%CI=1.618-3.791) were more likely to recommend LDCT to high-risk groups.
4. Discussion
The convenience of transportation was the factors of impact in this study. Sichuan Province, our study region, is located in the transition zone between the Qinghai-Tibet Plateau and the Middle-Lower Yangtze Plain. The northwest region of Sichuan province is mainly composed of plateaus and mountains, with an elevation of more than 4000 meters. The southwest of Sichuan province is Hengduan Mountains, with numerous high mountains and deep valleys. The hostile environment impedes normal traffic. In addition, poor resources and weak financial conditions are found in most regions of Sichuan province. Therefore, the convenience of transportation for medical services may influence the willingness of physicians in Sichuan province to recommend LDCT to high-risk groups. Modern technology may help solve this problem. Advanced 5G wireless communication can be used to gather outstanding experts nationwide for accelerating diagnosis and designing therapeutic regimens.
In China, the price of medical services is uniformly designated by the government according to different grades of hospitals. For instance, in a first-class hospital in grade 3, sputum screening costs RMB75, CXR costs RMB 130.3, and LDCT costs RMB250. The price of LDCT is significantly higher than sputum screening and CXR. LDCT screening may substantially increase national health care expenditures in less developed countries. Previous cost-effectiveness analyses also have not conclusively shown that LDCT is cost-effective (22, 25, 26). And in China lung cancer screening is usually done in an outpatient setting or in a medical examination institution. Although China nearly achieved universal health insurance coverage, the outpatient fees and the fees paid in medical examination institutions are not covered by medical insurance. Therefore, reducing the cost of LDCT or adopting certain medical subsidies for poor individuals may reduce the physicians’ perceptions of barriers on LDCT and may be helpful in improving the early diagnosis of lung cancer. And we found that the cost of LDCT screening to the patient was the also the most often-cites concern among pulmonologists abroad, although some countries has covered the cost of lung cancer screening (27).
LDCT is recognized as a highly sensitive test, which is inevitably accompanied by a high false positive rate. There were many studies had reported enough information to confirmed the high false-positive rate of LDCT screening home and abroad (20, 21, 28, 29). And in this study, the high false-positive rate was also proved to be one of the main perception of barriers on recommending LDCT among physicians in Sichuan province of China. The economic development level of Sichuan Province is not balanced, and residents in most areas are relatively poor. Moreover, due to geographical location, many residents are not convenient to travel to seek for periodically lung cancer screening. So, in addition to unnecessary tests and invasive procedures, the medical burden and the difficulty of seeking for medical service also increased by the false positive outcome among the residents in Sichuan Province. Precise lung cancer screening was desperately needed in such underdeveloped areas.
The mental burden and radiation didn’t influence physicians choose in recommending LDCT or not in this study. LDCT was introduced into China because of its low radiation compared to ordinary CT and which characteristic may be recognized and accepted by majority Chinese physicians. Reasonable and accurate case selection for screening can reduce radiation exposure and unnecessary screening (30). Compared with the serious consequences of lung cancer, the anxiety of high-risk subjects may be not important enough to influence physicians’ recommending.
Physicians in health management center and oncology department were more likely to recommend LDCT to high-risk groups. Physicians in thoracic surgery and respiratory medicine were no different in the likelihood of recommending LDCT compared with other departments. The difference may be related to the different groups they faced. The healthy people and diagnosed population were more likely in health management center and oncology department. And the patients who need to be diagnosed are more likely in Thoracic Surgery and Respiratory Medicine. The fact that low-dose CT does have an impact on the quality of the image which may influence physicians’ judgement can’t be ignored.
Limited by the weak causal inference power of cross-sectional data and given that a convenience sample was used, the generalizability of the result was limited.
5. Conclusion
The convenience of transportation, the price, false positive rate and the quality of image may be the main perception of barriers on recommending LDCT to high-risk groups among physicians in Sichuan province. Information technology, such as 5G wireless communication and mobile CT unit which may allow effective screening for underserved populations, government support in price and self-improvement of LDCT should be gathered together to break the barriers on physicians recommending on LDCT.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by Ethical approval was granted by the Ethical Committee of West China Hospital, Sichuan University. The patients/participants provided their written informed consent to participate in this study.
Author contributions
RL & QC designed the study, these authors contributed equally to this work and should be considered co-first authors. RL, QC, QL and HZ collected, analyzed data. FC, RL and QC wrote the manuscript. All authors contributed to the article and approved the submitted version.
Funding
The study was supported by National Natural Science Foundation of China (71532007, 72042007).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Oudkerk M, Liu S, Heuvelmans MA, Walter JE, Field JK. Lung cancer LDCT screening and mortality reduction - evidence, pitfalls and future perspectives. Nat Rev Clin Oncol (2021) 18(3):135–51. doi: 10.1038/s41571-020-00432-6
2. Yang D, Liu Y, Bai C, Wang X, Powell CA. Epidemiology of lung cancer and lung cancer screening programs in China and the united states. Cancer Lett (2020) 468:82–7. doi: 10.1016/j.canlet.2019.10.009
3. Zheng RS, Sun KX, Zhang SW, Zeng HM, Zou XN, Chen R, et al. [Report of cancer epidemiology in China, 2015]. Zhonghua Zhong Liu Za Zhi (2019) 41(1):19–28. doi: 10.3760/cma.j.issn.0253-3766.2019.01.005
4. The National Lung Screening Trial Research Team, Aberle DR, Adams AM, Berg CD, Black WC, Clapp JD, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. New Engl J Med (2011) 365(5):395–409. doi: 10.1056/NEJMoa1102873
5. Becker N, Motsch E, Trotter A, Heussel CP, Dienemann H, Schnabel PA, et al. Lung cancer mortality reduction by LDCT screening-results from the randomized German LUSI trial. Int J Cancer (2020) 146(6):1503–13. doi: 10.1002/ijc.32486
6. Quaife S, Ruparel M, Dickson J, Beeken RJ, McEwen A, Baldwin DR, et al. Lung screen uptake trial (LSUT): randomized controlled clinical trial testing targeted invitation materials. Am J Respir Crit Care Med (2020) 201(8):965–75. doi: 10.1164/rccm.201905-0946OC
7. Kinsinger LS, Anderson C, Kim J, Larson M, Chan SH, King HA, et al. Implementation of lung cancer screening in the veterans health administration. JAMA Intern Med (2017) 177(3):399–406. doi: 10.1001/jamainternmed.2016.9022
8. Guo L, Zhang S, Liu S, Yang FN, Wu Y, Zheng LY, et al. Compliance of lung cancer screening with low-dose computed tomography and influencing factors in urban area of henan province. Chin J Epidemiol (2020) 41(07):1076–80. doi: 10.3760/cma.j.cn112338-20190730-00564
9. Wen Y, Yu L, Du L, Wei DH, Liu YY, Yang Z, et al. Analysis of low-dose computed tomography compliance and related factors among high-risk population of lung cancer in three provinces participating in the cancer screening program in urban China. Chin J Prev Med (2021) 55(5):633–9. doi: 10.3760/cma.j.cn112150-20201015-01286
10. Rutten LJ, Arora NK, Bakos AD, Aziz N, Rowland J. Information needs and sources of information among cancer patients: a systematic review of research (1980-2003). Patient Educ Couns (2005) 57(3):250–61. doi: 10.1016/j.pec.2004.06.006
11. Raz DJ, Wu GX, Consunji M, Nelson RA, Kim H, Sun CL, et al. The effect of primary care physician knowledge of lung cancer screening guidelines on perceptions and utilization of low-dose computed tomography. Clin Lung Cancer (2018) 19(1):51–7. doi: 10.1016/j.cllc.2017.05.013
12. Iaccarino JM, Clark J, Bolton R, Kinsinger L, Kelley M, Slatore CG, et al. A national survey of pulmonologists' views on low-dose computed tomography screening for lung cancer. Ann Am Thorac Soc (2015) 12(11):1667–75. doi: 10.1513/AnnalsATS.201507-467OC
13. Raz DJ, Wu GX, Consunji M, Nelson R, Sun C, Erhunmwunsee L, et al. Perceptions and utilization of lung cancer screening among primary care physicians. J Thorac Oncol (2016) 11(11):1856–62. doi: 10.1016/j.jtho.2016.06.010
14. Lewis JA, Petty WJ, Tooze JA, Miller DP, Chiles C, Miller AA, et al. Low-dose CT lung cancer screening practices and attitudes among primary care providers at an academic medical center. Cancer Epidemiol Biomarkers Prev (2015) 24(4):664–70. doi: 10.1158/1055-9965.EPI-14-1241
15. Huang J, Liu W, Huang Y. Influencing mechanism of the use behavior of clinical practice guidelines on antimicrobials: evidence from the integration of theory of reasoned action and organizational readiness for change. BMC Med Inform Decis Mak (2022) 22(1):279. doi: 10.1186/s12911-022-02019-w
16. Reynolds L, McKee M. Factors influencing antibiotic prescribing in China: An exploratory analysis. Health Policy (2009) 90(1):32–6. doi: 10.1016/j.healthpol.2008.09.002
17. Horwood J, Cabral C, Hay AD, Ingram J. Primary care clinician antibiotic prescribing decisions in consultations for children with RTIs: A qualitative interview study. Br J Gen Pract (2016) 66(644):e207–13. doi: 10.3399/bjgp16X683821
18. Teixeira Rodrigues A, Roque F, Falcão A, Figueiras A, Herdeiro MT. Understanding physician antibiotic prescribing behaviour: A systematic review of qualitative studies. Int J Antimicrob Agents (2013) 41(3):203–12. doi: 10.1016/j.ijantimicag.2012.09.003
19. Zeng X, Zhou Z, Luo X, Liu Q. Lung cancer screening with low-dose computed tomography: National expenditures and cost-effectiveness. Front Public Health (2022) 10:977550. doi: 10.3389/fpubh.2022.977550
20. Aberle DR, DeMello S, Berg CD, Black WC, Brenda B, Church TR, et al. Results of the two incidence screenings in the national lung screening trial. N Engl J Med (2013) 369(10):920–31. doi: 10.1056/NEJMoa1208962
21. Jonas DE, Reuland DS, Reddy SM, Nagle M, Clark SD, Weber RP, et al. Screening for lung cancer with low-dose computed tomography: Updated evidence report and systematic review for the US preventive services task force. JAMA (2021) 325(10):971–87. doi: 10.1001/jama.2021.0377
22. Carozzi FM, Bisanzi S, Carrozzi L, Falaschi F, Pegna AL, Mascalchi M, et al. Multimodal lung cancer screening using the ITALUNG biomarker panel and low dose computed tomography. Results of the ITALUNG biomarker study. Int J Cancer (2017) 141(1):94–101. doi: 10.1002/ijc.30727
23. Liu C, Xiang X, Han S, Lim HY, Li L, Zhang X, et al. Blood-based liquid biopsy: Insights into early detection and clinical management of lung cancer. Cancer Lett (2022) 524:91–102. doi: 10.1016/j.canlet.2021.10.013
24. Rasmussen JF, Siersma V, Malmqvist J, Brodersen J. Psychosocial consequences of false positives in the Danish lung cancer CT screening trial: A nested matched cohort study. BMJ Open (2020) 10(6):e034682. doi: 10.1136/bmjopen-2019-034682
25. Puggina A, Broumas A, Ricciardi W, Boccia S. Cost-effectiveness of screening for lung cancer with low-dose computed tomography: A systematic literature review. Eur J Public Health (2016) 26(1):168–75. doi: 10.1093/eurpub/ckv158
26. Sun C, Zhang X, Guo S, Liu Y, Zhou L, Shi J, et al. Determining cost-effectiveness of lung cancer screening in urban Chinese populations using a state-transition Markov model. BMJ Open (2021) 11(7):e046742. doi: 10.1136/bmjopen-2020-046742
27. Ersek JL, Eberth JM, McDonnell KK, Strayer SM, Sercy E, Cartmell KB, et al. Knowledge of, attitudes toward, and use of low-dose computed tomography for lung cancer screening among family physicians. Cancer (2016) 122(15):2324–31. doi: 10.1002/cncr.29944
28. Horeweg N, Scholten ET, de Jong PA, Van der Aalst CM, Weenink C, Lammers JW, et al. Detection of lung cancer through low-dose CT screening (NELSON): A prespecified analysis of screening test performance and interval cancers. Lancet Oncol (2014) 15(12):1342–50. doi: 10.1016/S1470-2045(14)70387-0
29. Ji G, Bao T, Li Z, Tang H, Liu D, Yang P, et al. Current lung cancer screening guidelines may miss high-risk population: A real-world study. BMC Cancer (2021) 21(1):50. doi: 10.1186/s12885-020-07750-z
Keywords: influencing factors, low-dose spiral CT, lung cancer screening, recommending willingness, perception of barriers
Citation: Li R, Chai Q, Chen F, Liu Q and Zhang H (2023) Influencing factors of LDCT recommendation by physicians in Sichuan Province, China. Front. Oncol. 12:1049096. doi: 10.3389/fonc.2022.1049096
Received: 29 September 2022; Accepted: 14 December 2022;
Published: 04 January 2023.
Edited by:
Tung-Sung Tseng, Louisiana State University, United StatesReviewed by:
Alexander Nikolaev, Scientific and Practical Clinical Center for Diagnostics and Telemedicine Technologies of the Department of Healthcare of the City of Moscow, RussiaTing Luo, University of California, San Diego, United States
Copyright © 2023 Li, Chai, Chen, Liu and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Feng Chen, Y2hlbmZAc2N1LmVkdS5jbg==
 Ruicen Li
Ruicen Li Qi Chai
Qi Chai Feng Chen3*
Feng Chen3*