
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Oncol. , 25 November 2022
Sec. Surgical Oncology
Volume 12 - 2022 | https://doi.org/10.3389/fonc.2022.1014817
This article is part of the Research Topic Acute Care Surgery, Emergency Surgery, Surgical Outcomes View all 7 articles
Objective: This study used a national sample cohort database to investigate the risk of osteoporotic fractures after gastrectomy is performed for gastric cancer.
Materials and Methods: We used data from the Korea National Health Insurance Service-National Sample Cohort between 2002 and 2019. After performing 1:3 propensity score matching, 28,328 individuals were analysed in the final study (7, 082 cases; 21, 246 controls). Gastrectomy data were extracted from the coded claims data, and osteoporotic fractures were defined as the occurrence of fractures in any of the vertebrae, distal radius, humerus, or hip, according to the 10th version of the International Classification of Diseases. A Cox proportional hazards regression model was generated to investigate the association between gastrectomy and risk of osteoporotic fractures.
Results: Patients with gastric cancer who underwent a gastrectomy had a higher risk of osteoporotic fractures as compared to the general population (men, hazard ratio [HR]: 1.13, 95% confidence interval [CI]: 1.00-1.27; women, HR: 1.18, 95% CI: 1.06-1.30). A significantly higher risk of osteoporotic fractures was observed with surgical resection than with endoscopic resection (men, surgical, HR: 1.28, 95% CI: 1.08-1.52, endoscopic, HR: 1.04, 95% CI: 0.90-1.21; women, surgical, HR: 1.34, 95% CI: 1.11-1.62, endoscopic, HR: 1.13, 95% CI: 1.01-1.27). In men, the risk of hip fracture was the highest among the four fracture sites (HR: 1.18, 95% CI:0.89-1.56), while in women, the risk of vertebral fracture after gastrectomy was the highest (HR: 1.16, 95% CI: 0.99-1.35).
Conclusion: Patients with gastric cancer who underwent gastrectomy had a higher risk of osteoporotic fractures as compared to the general population. This suggests the need for bone metabolism management in patients with gastric cancer to prevent post-gastrectomy complications.
Gastric cancer is the fourth most common cancer worldwide (1) and has been the most common cancer in South Korea since 1999, when the Korea Central Cancer Registry first reported nationwide cancer incidence data (2). Fortunately, through early detection and curative treatment such as gastrectomy, the long-term survival rates increase considerably (3). In South Korea, early diagnosis of gastric cancer leads to a survival rate of over 90% (4). However, the complications associated with gastrectomy cannot be overlooked. Osteoporosis and fractures commonly occur after gastrectomy is performed for gastric cancer (5, 6). Previous studies have reported an incidence of 32-42% for osteoporosis after gastrectomy, and approximately 40% for fractures (7–9). In addition, osteoporotic fractures have been found to increase the socioeconomic burden on individuals and society (10) as well as impair the quality of life (11).
Although several studies have reported a high prevalence of metabolic bone diseases such as osteomalacia and osteoporosis after gastrectomy was performed for gastric cancer (7, 12) a systematic post-surgery management program has not yet been established. While the incidence of osteoporotic fractures is expected to increase due to gastrectomy, the exact incidence has not been confirmed because the hospitals wherein the gastrectomies are performed are usually different from those that diagnose osteoporotic fractures (7). Therefore, longitudinal observational studies on the risk of new-onset osteoporotic fractures have rarely been conducted in South Korea.
The current study aimed to identify the risk of osteoporotic fractures after gastrectomy for gastric cancer using a national sample cohort database. Furthermore, based on the results of this study, we aimed to provide evidence of the need for systematic management to prevent complications after gastrectomy.
This population-based cohort study analysed data from the Korea National Health Insurance Service-National Sample Cohort (NHIS-NSC) database between 2002 and 2019. Since the introduction of universal health coverage in 1989, all South Koreans have been obliged to subscribe to the NHIS; thus, approximately 98% of the total population has been enrolled. The NHIS-NSC database contains data on all cases of Korean healthcare utilisation and information on the sociodemographic characteristics and diagnosis codes as per the International Classification of Diseases, 10th revision (ICD-10). The study protocol was approved by the Institutional Review Board of Yonsei University Health System (IRB Number: Y-2020-0031). The requirement for informed consent was waived owing to the retrospective nature of the study and the lack of any identifiable information in the data.
Of the 47,851,928 individuals in the NHIS-NSC database as of 2002, 46,605,433 individuals were included in the sample cohort after excluding non-citizens. After random sampling, the database included 1,025,340 individuals, accounting for 2.2% of the total population of South Korea (13). The years 2002 and 2003 were designated as washout periods since the first 2-year might be the consequence of pre-existing diseases and the outcome of our study was the newly onset osteoporotic fractures. Moreover, to avoid reverse causality, we excluded those individuals who were found to have osteoporotic fractures within one year after gastrectomy. We then performed 1:3 propensity score matching (matching variables: sex, age, and medical insurance) to include the normal general population who did not undergo gastrectomy as the control group. Consequently, 28,328 individuals in total were analysed in the final study, with 7,082 in the case group and 21, 246 in the control study.
The dependent variable was the risk of osteoporotic fractures, which was defined as the occurrence of fractures in any of the vertebrae (ICD-10 codes S220, S221, S320, M484, and M485), distal radius (ICD-10 codes S525 and S526), humerus (ICD-10 codes S422 and S423), or hip (ICD-10 codes S720 and S721) (14, 15). The main variable of interest was gastrectomy, which included both endoscopic and surgical resections. The date of diagnosis of any of the four types of osteoporotic fractures or the last date of the study period (30 December 2019) was set as the final follow-up date (16).
As covariates, we included sociodemographic variables such as age, medical insurance, income, region, and health status-related variables such as the Charlson Comorbidity Index (CCI), hypertension, and diabetes mellitus. The Korean National Health Insurance System covers the entire population residing within the territory of the Republic of Korea, except for beneficiaries of medical aid. Additionally, the Korean government offers a medical aid program to those who cannot afford to pay for healthcare coverage (17). Taking this into account, medical insurance was classified into three categories i.e., regionally-insured, workplace-insured, and medical aid. Regions were defined using the position value for the relative comparison (PARC) index, which has been widely used to diagnose the level of medical care by region in Korea (18, 19). PARC is an objective indicator used to determine the relative position of medical care in a region in terms of demand, supply, access, use, and quality compared to other regions (18). The PARC value ranges from -1 to 1, the best being 1, the average indicated by 0, and the worst being -1 (19). A PARC value less than -0.33 was classified as a medically vulnerable region. The CCI score is an index for evaluating patient comorbidities, which can be calculated by assigning weights of 1-6 points for 19 comorbidities. Categories of comorbid diseases included in the CCI score consisted of myocardial, vascular, pulmonary, endocrine kidney, gastrointestinal, cancer, immune, and neurologic comorbidities (20). ICD-10 diagnostic codes were used to calculate the CCI scores of the study population for each comorbid disease (21), and CCI scores were classified into two categories i.e., approximately 0-2, and ≥ 3.
Chi-square tests were performed to investigate the general characteristics of the study population. A Cox proportional hazards model was generated to examine the association between gastrectomy and the risk of osteoporotic fractures. Kaplan–Meier survival curves were used to compare survival probabilities between the groups, and a stratified log-rank test was used to compare the Kaplan–Meier curves of the matched cohort (22, 23). The adjusted hazard ratios (HRs) with 95% confidence intervals (CIs) were presented as the key results. For all analyses, we used SAS software (version 9.4; SAS Institute Inc., Cary, NC, USA). Statistical significance was set at p <.05.
Table 1 presents the general characteristics of the study population after propensity score matching in a 1:3 ratio. Among the 28,328 individuals eligible for analysis, 7,082 were part of the case group of gastric cancer patients who underwent gastrectomy, and the remaining 21,246 were part of the control group recruited from the general population. Osteoporotic fractures were found in 1,415 (8.4%) of the 16,904 men and 1,909 (16.7%) of the 11,424 women.
Table 2 shows the results of a Cox proportional hazards regression analysis of the association between gastrectomy and the risk of osteoporotic fractures after controlling for all covariates. Patients with gastric cancer who underwent gastrectomy in the case group had a higher risk of osteoporotic fractures than the general population in the control group (men, HR: 1.13, 95% CI:1.00-1.27; women, HR: 1.18, 95% CI: 1.06-1.30). Among covariates, medical insurance (women, regionally insured, HR: 1.19, 95% CI: 1.08-1.32), income (men, low, HR: 1.19, 95% CI: 1.04-1.36), region (men, vulnerable area, HR: 1.24, 95% CI: 1.08-1.41), and CCI score (men, ≥3, HR: 1.33, 95% CI: 1.15-1.54; women, ≥3, HR: 1.16, 95% CI: 1.03-1.32) were found to be statistically significant factors influencing the risk of osteoporotic fractures.
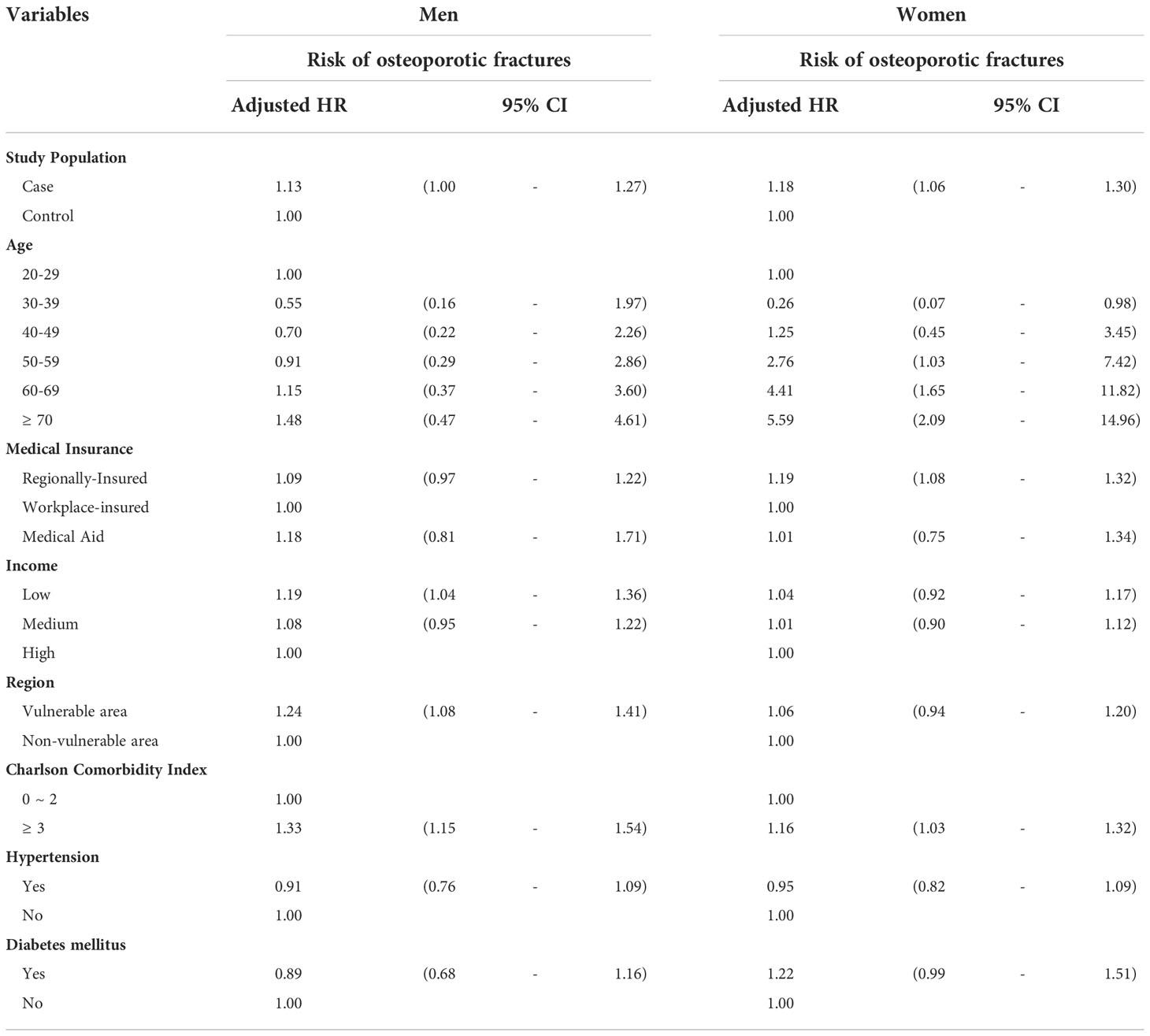
Table 2 Results of Cox proportional hazard regression analysis on the association between gastrectomy and risk of osteoporotic fractures.
Figure 1 presents the Kaplan–Meier survival curves. There were difference in the survival probabilities between patients with osteoporotic fractures after gastrectomy and the control groups during the entire follow-up period (p <.0001 for log-rank test).
Since gastrectomy, which was our main variable of interest, included both endoscopic and surgical resections, we performed a subgroup analysis with stratification by the method of gastrectomy. The results for the same are depicted in Figure 2. As compared to the men in the control group, the risk of osteoporotic fractures in men was 1.04 times higher in those who underwent endoscopic resections (95% CI: 0.90-1.21), and 1.28 times higher in those who underwent surgical resection (95% CI: 1.08-1.52). Similarly, compared to women in the control group, the women who underwent endoscopic resection had a 1.13 times higher risk of osteoporotic fractures (95% CI: 1.01-1.27), and those who underwent surgical resection had a 1.34 times higher risk (95% CI: 1.11-1.62).
Subgroup analysis was performed according to the four osteoporotic fractures sites, and the results are shown in Table 3. In male patients with gastric cancer who underwent gastrectomy, the risk of hip fracture was the highest among the four fracture sites (HR:1.18, 95% CI: 0.89-1.56). In contrast, in women, the risk of vertebral fracture after gastrectomy was the highest (HR: 1.16, 95% CI: 0.99-1.35).
It is well established that metabolic bone diseases can occur as late complications in patients with gastric cancer who undergo gastrectomy (24, 25). Previous studies have reported a decrease in the intestinal absorption of calcium and vitamin D as a cause of bone disorders such as osteoporosis and osteomalacia after gastrectomy (12, 26). In addition, it has also been demonstrated that decreased bone mass after gastrectomy increases the cumulative incidence of fractures (6, 27). In south Korea, an increase in the long-term survival rate after gastrectomy in patients with gastric cancer has led to an anticipated rise in metabolic bone diseases and fractures related to gastrectomy (28); however, only a few studies have explored this yet. Thus, this retrospective observational study attempted to investigate the risk of osteoporotic fractures among possible bone diseases after gastrectomy, using a national health insurance claims data.
The present study had three key findings. First, we found that patients with gastric cancer who underwent gastrectomy were at a higher risk of new-onset osteoporotic fractures than the general population. This is consistent with the results of a study that used the nationwide claims data and showed that osteoporosis and osteoporotic fracture incidences were high in patients within a relatively short period of time after gastrectomy in gastric cancer patients who underwent gastrectomy for 3 years (7). Therefore, our findings suggest that the systematic management of metabolic bone diseases and fractures is necessary immediately after gastrectomy. Second, a significantly higher risk of osteoporotic fracture was observed for surgical resection, as compared with endoscopic resection. This finding was similar to that of a previous meta-analysis, which confirmed that compared to surgical resection, endoscopic resection was associated with similar long-term outcomes and considerable advantages in terms of operation time, hospital stay, costs, and complications (29). While endoscopic resections can be performed on patients with relatively early stage gastric cancer, development in medical technology for wide-scale applications will be required to restore function and reduce complications after resection. Third, we found that men had the highest risk of hip fractures and women the highest risk of vertebral fractures among the four fracture sites. Since several studies have demonstrated that hip and vertebral fractures are associated with increased mortality risk (30, 31), bone metabolism management is vital in patients who undergo gastrectomy.
This study had several limitations. First, because we used retrospective cohort data, we could not adjust for any potential confounding factors that could affect the incidence of osteoporotic fractures, such as nutrients, diet, and exercise. Second, diagnostic inaccuracies in the health insurance claims database may limit the accuracy of the diagnostic information (32). To correct for this, we included both primary and secondary diagnostic codes in the analysis (16). In addition, since we only used ICD-10 coded claims data, we could not control for the severity of osteoporotic fractures. Despite these limitations, our study had certain strengths because we used the most up-to-date national sample cohort database. Due to the representativeness of the data, our results can be generalised to the entire population of South Korea as well as to other countries with similar demographic characteristics. Unlike several previous studies focusing mainly on the association between gastrectomy and osteoporosis occurrence (33, 34), there was a clear difference in that we also considered the risk of osteoporotic fractures and resection methods, and preformed 1:3 propensity score matching. Furthermore, the follow-up period of our data was 18 years, making it possible to infer long-term associations.
In conclusion, our study found a significant relationship between gastrectomy and the risk of osteoporotic fractures using data from the South Korean National Sample Cohort database. Patients with gastric cancer who underwent gastrectomy had a higher risk of osteoporotic fractures than the general population, and this tendency was particularly observed when they underwent surgical resection rather than endoscopic resection. These findings highlight the need to systematically manage bone metabolism immediately after gastrectomy in patients with gastric cancer.
Publicly available datasets were analyzed in this study. This data can be found here: https://nhiss.nhis.or.kr/bd/ab/bdaba000eng.do.
The studies involving human participants were reviewed and approved by the Institutional Review Board of Yonsei University Health System (IRB Number: Y-2020-0031). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
IY made a substantial contribution to the concept or design of the work. IY and KH contributed to the acquisition, analysis, or interpretation of data. SH, E-CP, and S-IJ drafted the article or revised it critically for important intellectual content. All authors contributed to the article and approved the submitted version.
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI20C1130).
We would like to thank the colleagues from the Department of Public Health, Graduate School of Yonsei University provided advice for this manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer (2015) 136(5):E359–E86. doi: 10.1002/ijc.29210
2. Kang MJ, Won Y-J, Lee JJ, Jung K-W, Kim H-J, Kong H-J, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2019. Cancer Res Treatment: Off J Korean Cancer Assoc (2022) 54(2):330. doi: 10.4143/crt.2022.128
3. Chan BA, Jang RW, Wong RK, Swallow CJ, Darling GE, Elimova E. Improving outcomes in resectable gastric cancer: A review of current and future strategies. Oncology (2016) 30(7):635–45.
4. Lee H-J, Han-Kwang Y, Ahn Y-O. Gastric cancer in Korea. Gastric Cancer (2002) 5(3):177. doi: 10.1007/s101200200031
5. Krupski W, Tatara MR, Bury P, Szabelska A, Charuta A, Maciejewski R, et al. Negative effects of total gastrectomy on bone tissue metabolism and volumetric bone mineral density (vBMD) of lumbar spine in 1-year study in men. Medicine (2016) 95(7):e2817. doi: 10.1097/MD.0000000000002817
6. Oh HJ, Lim C-H, Yoon B-H, Yoon SB, Baeg MK, Kim WC, et al. Fracture after gastrectomy for gastric cancer: A long-term follow-up observational study. Eur J Cancer (2017) 72:28–36. doi: 10.1016/j.ejca.2016.11.023
7. Seo GH, Kang HY, Choe EK. Osteoporosis and fracture after gastrectomy for stomach cancer: a nationwide claims study. Medicine (2018) 97(17):e0532. doi: 10.1097/MD.0000000000010532
8. Inoue K, Shiomi K, Higashide S, Kan N, Nio Y, Tobe T, et al. Metabolic bone disease following gastrectomy: Assessment by dual energy X-ray absorptiometry. Br J Surg (1992) 79(4):321–4. doi: 10.1002/bjs.1800790413
9. Lim JS, Kim SB, Bang H-Y, Cheon GJ, Lee J-I. High prevalence of osteoporosis in patients with gastric adenocarcinoma following gastrectomy. World J Gastroenterol: WJG (2007) 13(48):6492. doi: 10.3748/wjg.v13.i48.6492
10. Mohd-Tahir N, Li S. Economic burden of osteoporosis-related hip fracture in Asia: a systematic review. Osteoporosis Int (2017) 28(7):2035–44. doi: 10.1007/s00198-017-3985-4
11. Lips P, van Schoor NM. Quality of life in patients with osteoporosis. Osteoporosis Int (2005) 16(5):447–55. doi: 10.1007/s00198-004-1762-7
12. Morgan D, Paterson C, Woods C, Pulvertaft C, Fourman P. Osteomalacia after gastrectomy: a response to very small doses of vitamin d. Lancet (1965) 286(7422):1089–91. doi: 10.1016/S0140-6736(65)90061-9
13. Lee J, Lee JS, Park S-H, Shin SA, Kim K. Cohort profile: the national health insurance service–national sample cohort (NHIS-NSC), south Korea. Int J Epidemiol (2017) 46(2):e15–e. doi: 10.1093/ije/dyv319
14. Yoo J-I, Ha Y-C, Park KS, Kim R-B, Seo S-H, Koo K-H. Incidence and mortality of osteoporotic refractures in Korea according to nationwide claims data. Yonsei Med J (2019) 60(10):969–75. doi: 10.3349/ymj.2019.60.10.969
15. Kim HY, Ha Y-C, Kim T-Y, Cho H, Lee Y-K, Baek J-Y, et al. Healthcare costs of osteoporotic fracture in Korea: Information from the national health insurance claims database, 2008-2011. J Bone Metab (2017) 24(2):125–33. doi: 10.11005/jbm.2017.24.2.125
16. Kim H, Jeong W, Kim SH, Seo JH, Ryu JS, Kim Y-s, et al. Association between social phobia and the risk of arrhythmia using the Korean national sample cohort: a retrospective cohort study. BMC Psychiatry (2022) 22(1):1–8. doi: 10.1186/s12888-022-03689-6
17. Kim K-H, Park E-C, Hahm M-I. The gap between physicians and the public in satisfaction with the national health insurance system in Korea. J Korean Med Sci (2012) 27(6):579–85. doi: 10.3346/jkms.2012.27.6.579
18. Youn HM, Lee HJ, Park E-C. Position value for relative comparison of healthcare status of Korea in 2018. Health Policy Manage (2021) 31(2):217–24. doi: 10.4332/KJHPA.2021.31.2.217
19. Jang S-I, Nam J-M, Choi J, Park E-C. Disease management index of potential years of life lost as a tool for setting priorities in national disease control using OECD health data. Health Policy (2014) 115(1):92–9. doi: 10.1016/j.healthpol.2013.11.007
20. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J chronic Dis (1987) 40(5):373–83. doi: 10.1016/0021-9681(87)90171-8
21. Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA. New ICD-10 version of the charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol (2004) 57(12):1288–94. doi: 10.1016/j.jclinepi.2004.03.012
22. Austin PC. The use of propensity score methods with survival or time-to-event outcomes: reporting measures of effect similar to those used in randomized experiments. Stat Med (2014) 33(7):1242–58. doi: 10.1002/sim.5984
23. Bland JM, Altman DG. Survival probabilities (the Kaplan-Meier method). Bmj (1998) 317(7172):1572–80. doi: 10.1136/bmj.317.7172.1572
24. Zittel TT, Zeeb B, Maier GW, Kaiser GW, Zwirner M, Liebich H, et al. High prevalence of bone disorders after gastrectomy. Am J Surg (1997) 174(4):431–8. doi: 10.1016/S0002-9610(97)00123-2
25. Eddy RL. Metabolic bone disease after gastrectomy. Am J Med (1971) 50(4):442–9. doi: 10.1016/0002-9343(71)90333-0
26. Deller D, Begley M. Calcium metabolism and the bones after partial gastrectomy: I. clinical features and radiology of the bones. Australas Ann Med (1963) 12(4):282–94. doi: 10.1111/imj.1963.12.4.282
27. Nilsson B, Westlin N. The fracture incidence after gastrectomy. Acta chirurgica Scandinavica (1971) 137(6):533–4.
28. Lee YS, Kim WH, Shin HS, Kang JK, Park IS, Kim CB. Calcium metabolism after gastrectomy in patients with stomach carcinoma-a short-term prospective study-. Korean J Med (1994) 46(6):825–35.
29. Sun W, Han X, Wu S, Yang C. Endoscopic resection versus surgical resection for early gastric cancer: A systematic review and meta-analysis. Medicine (2015) 94(43):e1649. doi: 10.1097/MD.0000000000001649
30. Lee Y-K, Jang S, Lee H, Park C, Ha Y-C, Kim D-Y. Mortality after vertebral fracture in Korea. Osteoporosis Int (2012) 23(7):1859–65. doi: 10.1007/s00198-011-1833-5
31. Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA, Center JR. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. Jama (2009) 301(5):513–21. doi: 10.1001/jama.2009.50
32. Park E. Evaluating the consistency of health insurance claim disease code and medical record and improvement plan. Health Insurance Rev Assess Service (2017).
33. Jeong S-M, Shin DW, Lee JE, Jin S-M, Kim S. Increased risk of osteoporosis in gastric cancer survivors compared to general population control: a study with representative Korean population. Cancer Res Treatment: Off J Korean Cancer Assoc (2019) 51(2):530–7. doi: 10.4143/crt.2018.164
Keywords: gastric cancer, gastrectomy, metabolic bone disease, osteoporotic fracture, cohort study
Citation: Yun I, Hurh K, Jeong SH, Park E-C and Jang S-I (2022) The risk of osteoporotic fractures after gastrectomy: Findings from the Korean national sample cohort database (2002-2019). Front. Oncol. 12:1014817. doi: 10.3389/fonc.2022.1014817
Received: 09 August 2022; Accepted: 31 October 2022;
Published: 25 November 2022.
Edited by:
Pietro Fransvea, Fondazione Policlinico Universitario A. Gemelli, ItalyReviewed by:
Valentina Bianchi, Agostino Gemelli University Polyclinic (IRCCS), ItalyCopyright © 2022 Yun, Hurh, Jeong, Park and Jang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sung-In Jang, SkFOR1NJQHl1aHMuYWM=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.