
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Oncol. , 12 October 2022
Sec. Surgical Oncology
Volume 12 - 2022 | https://doi.org/10.3389/fonc.2022.1011076
This article is part of the Research Topic Case Reports in Surgical Oncology: 2022 View all 56 articles
Introduction: Bronchogenic cyst is a congenital aberration of bronchopulmonary malformation with bronchial-type, pseudostratified cylindrical epithelium. They are usually discovered in the mediastinum and intrapulmonary but are rarely encountered in retroperitoneum. We report a case of the retroperitoneal bronchogenic cyst and perform a literature review to summarize the safety of laparoscopic resection for this rare disease.
Case presentation: We report a 57-year-old woman who was admitted to our hospital with no clinical symptoms and was found by chance to have masses in the adrenal gland area during a routine physical examination. An abdominal CT examination revealed a cystic lesion was found in the left suprarenal region. Afterward, the patient underwent a laparoscopic exploration. Histopathological findings confirmed the diagnosis of a retroperitoneal bronchogenic cyst. The patient recovered uneventfully without signs of recurrence during a 1-year follow-up period.
Conclusion: Bronchogenic cyst is rare in the retroperitoneal region. It should be considered as one of the differential diagnoses of a retroperitoneal neoplasm, especially in the left retroperitoneal region. Laparoscopic surgery is technically feasible and safe for the treatment of patients with a retroperitoneal bronchogenic cyst.
Bronchogenic cysts (BCs) arise from abnormal budding of the foregut during embryogenesis, which is a benign congenital aberration of bronchopulmonary foregut malformation (1). It is typically located within the mediastinum and pulmonary parenchyma. The retroperitoneum is rarely involved (2). Particularly, retroperitoneal bronchogenic cysts(RBCs) tend to occur on the pancreas corpus or left adrenal gland (3). In most cases, BCs are asymptomatic unless they are infected, ruptured into the surrounding cavities, or enlarged enough to compress adjacent structures (4, 5). Cough, fever, pain, and dyspnea are among the most common manifestations (6). Due to the lack of characteristic clinical features, RBCs are often accidentally identified and diagnosed by imaging examinations, such as computed tomography(CT) and magnetic resonance imaging (MRI) (7). However, due to their rarity, location, variable cystic content, and non-specific imaging, they are frequently misinterpreted as cystic teratomas, adrenal tumors, or other benign and malignant retroperitoneal lesions (7–9). Although benign lesions, surgical resection is recommended to establish the diagnosis, alleviate symptoms, and prevent complications or malignant transformation (1, 10). Recently, laparoscopic procedure for RBCs has become increasingly popular for decreased scarring, less complications, shorter hospital stays, and faster recovery. Herein, we present a case of RBC, which was successfully removed through a laparoscopic excision. Additionally, we have performed a literature review to summarize the safety of laparoscopic resection for this rare disease.
On January 4, 2021, a 57-year-old woman was referred to the West China Hospital for evaluation of a left adrenal neoplasm suspected of being an adrenal tumor. The patient had no symptoms and the mass was incidentally discovered on medical examination. There were no obvious abnormalities in her medical history or physical examination. Additionally, she did not have any underlying diseases or take any medications. Routine laboratory investigations such as complete blood counts and liver and kidney function tests were within normal ranges. Specifically, negative results were obtained for all adrenal gland hormones and serum tumor markers (Table 1).
CT showed an ovoid, well-defined, and heterogeneous lesion, measuring 2.2×5.8 cm in her left adrenal area (Figure 1). Based on these CT imaging characteristics, a benign lesion (most likely a cyst) was suspected. To confirm the diagnosis and determine the feature, the cyst was completely removed through the laparoscope.
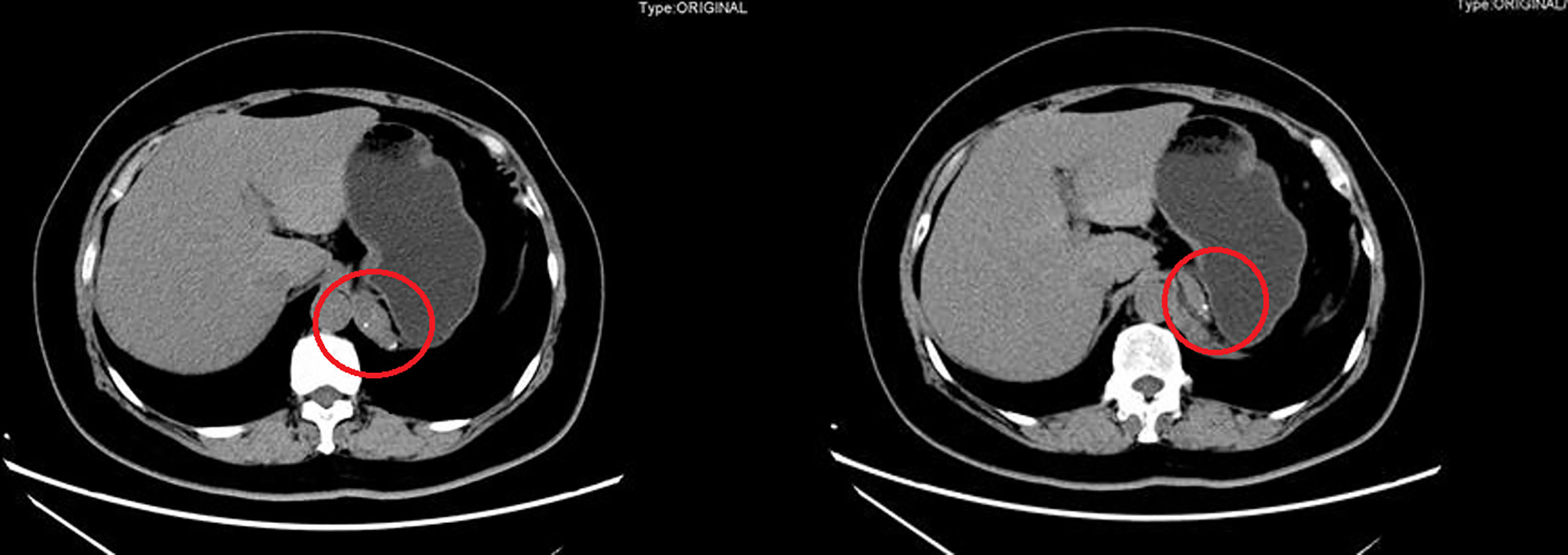
Figure 1 Computed tomography scan showed a 2.2×5.8 cm thin-walled water-attenuated cystic lesion in retroperitoneal region (red circle).
During the surgery, the patient was positioned supine. Using Veress needles, a 1.5-cm incision near the upper navel edge was made to establish pneumoperitoneum with a constant pressure of 13 mm Hg. Four trocars were used: a 5 mm trocar was inserted on the left side of the umbilicus, and two 12 mm trocars were placed below the right costal margin in the midclavicular line and mid-axillary line, respectively. The rest 12 mm trocar was installed under the xiphoid process. The procedure was performed using an ultrasonic surgical aspirator (CUSA; Cavitron Lasersonic Corp., Stamford, CT, USA), an ultrasonic system (Harmonic® scalpel; Ethicon Endo-Surgery, Inc., Cincinnati, OH, USA), and a bipolar clamp coagulation system (ERBE, Tubingen, Germany). Dissociation and exposure of the mass were achieved through the ultrasound knife, along with clamping the blood vessels leading to and from the tumor by a titanium clip. Intraoperatively, a 4×3cm cyst mass was observed behind the head of the pancreas and on the left side of the abdominal aorta, which had an unclear boundary with the surrounding tissues and was closely adhered to the diaphragm. The entire mass was completely removed. Afterward, we repaired the damaged diaphragm and performed complete hemostasis of the wound. The resection specimen was collected in a plastic bag and removed via small incisions around the umbilical cord. An orthopedic drainage tube was inserted into the left retroperitoneal cavity, and slightly bloody fluid was collected. The operation lasted 200 min, and the estimated blood loss was 20 ml with no transfusion.
The postoperative period was uneventful and the patient was discharged on the 6th day after surgery with no complications. CT was repeated regularly after surgery. No recurrence, metastasis, or other complications were observed after one and a half years of follow-up.
Grossly, the cystic lesion measured 60 mm in diameter (Figure 2A). Sectioning revealed yellowish fluid within the white tough tissue. Cystic walls were about 1-2 mm thick with a smooth interior surface (Figure 2B). Pathologically, characteristic pseudostratified columnar epithelium and cartilage were identified in histological specimens (Figure 2C). It was definitively determined that a retroperitoneal bronchogenic cyst existed.

Figure 2 (A) An ovoid, well-defined, and homogeneous cystic lesion. (B) Mucous filled the cystic lesion. (C) Histopathologic section revealed the cyst lined with tall columnar epithelium and cyst wall containing thin smooth muscle bundles, seromucous glands, and mature hyaline cartilage. (Haematoxylin and eosin stain, original magnification, ×200).
BCs are rare cystic lesions, with the prevalence in the general population remaining unknown (11). Men are slightly more prone to them, and they often go undetected until their 30 s or 40 s (12). They originate predominantly in the middle mediastinum and account for 10% to 15% of mediastinal tumors (13). Occasionally, they are identified in the neck, spinal canal, pleural cavity, skin, esophagus, pericardium, and retroperitoneum (1).
BCs originate from an aberrant budding of the tracheobronchial anlage of the primitive foregut between the 3rd and 7th weeks of embryonic development. The pleuroperitoneal membranes completely seal off the pericardioperitoneal canal at the end of the 7th week. Therefore, the abnormal lung buds are pinched off from the tracheobronchial tree by the growing diaphragm and trapped in the abdominal cavity. Eventually, the early lung buds develop into RBCs (14).
First reported by Miller et al. in 1953, RBCs are extremely rare. A thorough search of the PubMed database revealed 88 publications of retroperitoneal bronchogenic cysts reported worldwide in the English literature between 1991-2022. After screening the full texts and pathological results,40 publications reporting on 45 cases with laparoscopic RBC removal were reviewed within the study. A concise summary of the included articles was shown in Table 2.
Laparoscopic resection was first reported in 1997 by Tokuda et al. for 3 cm such cysts (51). This procedure of the cyst has been reported most frequently in China (17cases, 37.8%), followed by Japan (8 cases,17.8%) and the United States (6 cases,13.3%). The finding concerning regional and race differences was consistent with Mike et al. (52) However, it remained unclear whether this represents a real difference in incidence among Asian patients or merely a reporting bias. There exists no discrepancy between the gender who underwent laparoscopic surgery (22 female and 23 male), with an average diagnosis age of 38.6 (range 6-78) years. To date, the largest retroperitoneal bronchial cyst of laparoscopic excision was 10×6cm, as reported by Trehan et al. in 2015 in India (26). Retroperitoneal bronchogenic cysts tend to be found on the left side of the abdomen(37cases,82.2%). The most common location of retroperitoneal bronchogenic cyst is near the left adrenal gland (31cases, 68.9%). Only 4 cases (8.9%) were discovered in the right adrenal gland. The previous review of cases has confirmed this difference (18). Based on Rud et al. (53), the left pericardioperitoneal canal closes later and is larger than the right which can explain why RBCs prefer to be located on the left side. It’s worth noting that nearly half of patients (22cases, 48.9%) find a mass incidentally, with no typical clinical manifestations. Of symptomatic patients, the majority complained of abdominal pain (7 cases, 30.4%) left flank pain (6 cases,26.1%) and a small number complained of thoracic pain and back pain.
Similar literature reviews were successively performed by Cetinkurşun et al. (54), Mike et al. (52), Govaerts et al. (55), and Yuan et al. (18) in 1997, 2005, 2012, and 2021, respectively. The aforementioned studies, however, included a large number of patients undergoing surgery via the open approach. In addition, we enrolled the latest reports from the past two years through a more comprehensive search, and supplemented cases missed by the previous retrieval. Similar conclusions were obtained regarding the clinical characteristics of the disease, including age, symptoms, and predilection sites.
It remains difficult to diagnose RBCs before surgery. CT and MRI are the most helpful imaging modalities (13, 56). Typical CT appearances are sharply defined, homogeneous masses with attenuation coefficients to water density (0 to 20 HU). However, the attenuation coefficients can increase when protein, calcium, or anthracosis pigment are elevated within the cyst, aggravating difficulties in the differential diagnosis (14). MRI reveals the inhomogeneity of RBCs with better clarity than CT, providing a more accurate preoperative diagnosis (56). By now, only histopathology can yield a definitive diagnosis of BCs. Indispensable pathological criteria consist of secretory epithelium along with bronchial glands, smooth muscle, or hyaline cartilage (57). There is still no exact evidence that endocrine or tumor biomarkers are associated with RBCs. In only a few cases were endocrine or tumor biomarker variations recorded (8, 58, 59).
Early surgical excision of RBCs is recommended to clarify a diagnosis, relieve symptoms and prevent complications, even if asymptomatic. Due to reduced operating time, length of stay, and intraoperative blood loss, laparoscope has been increasingly ubiquitous in intraperitoneal surgery. Currently, laparoscopic resection is particularly recommended to clarify the diagnosis and apply for the treatment of retroperitoneal bronchogenic cysts. In addition, laparoscopic resection has been widely used to lessen the economic burden as well as postoperative pain of patients. More than half of patients with RBCs underwent laparoscopic resection and the majority were free of complications during the postoperative course. The present study also found laparoscopy to be safe and reliable. In particular, the retroperitoneal laparoscopic excision, which was first documented by McCrystal et al. in 2002, has gained more and more applications in recent years. Our literature review supports that the retroperitoneal approach is feasible, effective, and less invasive when treating such retroperitoneal cysts. In addition, there are only two articles reporting three cases of robotic surgery applicated to RBC patients (22, 36). Robotic surgery has overcome many limitations of traditional laparoscopic surgery and has improved in terms of dexterity, tremor reduction, and 3-dimensional visualization (60). This enables broader adaptability of robotic surgery in abdominal and retroperitoneal surgical procedures (61). However, due to the high financial cost, the application of robotic resection remains limited (22).
The prognosis of bronchogenic cysts after surgical excision is excellent. No recurrence, malignancy, or other complications are reported in all the literature we reviewed.
To our best knowledge, our review provides the largest case series in the world with such cysts to be resected laparoscopically. In conclusion, we reported a case with an ectopic bronchogenic cyst in the left retroperitoneal region. A literature review suggests that laparoscopic excision is optimal management to establish both diagnosis and treatment. The long-term outcome of this disease is excellent, with no report of recurrence.
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
JL and QF contributed to the study concept and design. HL, JX, and QF contributed to the investigation and writing the original draft. HL, JX, and QF contributed to data collection. QF,JL and ZC revised the paper. All authors contributed to the article and approved the submitted version.
This work was supported by the 2021 Sichuan Science and Technology Plan Project “International cooperation in science and technology innovation/technological innovation cooperation in Hong Kong, Macao and Taiwan“ (2021YFH0095) and Sichuan University from 0 to 1 project (No. 2022SCUH0017).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Limaiem F, Mlika M. Bronchogenic cyst. StatPearls. Treasure Island (FL: StatPearls Publishing Copyright © 2022, StatPearls Publishing LLC (2022).
2. Wu LD, Wen K, Cheng ZR, Alwalid O, Han P. Retroperitoneal bronchogenic cyst in suprarenal region treated by laparoscopic resection: A case report. World J Clin cases (2021) 9(24):7245–50. doi: 10.12998/wjcc.v9.i24.7245
3. Başoğlu M, Karabulut K, Özbalcı GS, Aykun N, Çamlıdağ İ, Güngör BB, et al. Laparoscopic resection of retroperitoneal bronchogenic cyst clinically presenting as adrenal cyst. Turk J Surg (2018), 1–3. doi: 10.5152/turkjsurg.2018.4033
4. Bolton JW, Shahian DM. Asymptomatic bronchogenic cysts: what is the best management? Ann Thorac Surg (1992) 53(6):1134–7. doi: 10.1016/0003-4975(92)90412-W
5. Altieri MS, Zheng R, Pryor AD, Heimann A, Ahn S, Telem DA. Esophageal bronchogenic cyst and review of the literature. Surg Endosc (2015) 29(10):3010–5. doi: 10.1007/s00464-015-4082-4
6. Lateef N, Kuniyoshi J, Latif A, Ahsan MJ, Shaikh K, DeVrieze B, et al. Cardiac tamponade as a complication of bronchogenic cyst. Proc (Bayl Univ Med Cent) (2020) 34(1):172–4. doi: 10.1080/08998280.2020.1795594
7. Tong HX, Liu WS, Jiang Y, Liu JU, Zhou JJ, Zhang Y, et al. Giant retroperitoneal bronchogenic cyst mimicking a cystic teratoma: A case report. Oncol Lett (2015) 9(6):2701–5. doi: 10.3892/ol.2015.3076
8. Wang M, He X, Qiu X, Tian C, Li J, Lv M. Retroperitoneal bronchogenic cyst resembling an adrenal tumor with high levels of serum carbohydrate antigen 19-9: A case report. Med (Baltimore) (2017) 96(31):e7678. doi: 10.1097/MD.0000000000007678
9. Kluger MD, Tayar C, Belli A, Salceda JA, van Nhieu JT, Luciani A, et al. A foregut cystic neoplasm with diagnostic and therapeutic similarities to mucinous cystic neoplasms of the pancreas. Jop (2013) 14(4):446–9. doi: 10.6092/1590-8577/1402
10. Sullivan SM, Okada S, Kudo M, Ebihara Y. A retroperitoneal bronchogenic cyst with malignant change. Pathol Int (1999) 49(4):338–41. doi: 10.1046/j.1440-1827.1999.00869.x
11. Fievet L, Gossot D, de Lesquen H, Calabre C, Merrot T, Thomas P, et al. Resection of bronchogenic cysts in symptomatic versus asymptomatic patients: An outcome analysis. Ann Thorac Surg (2021) 112(5):1553–8. doi: 10.1016/j.athoracsur.2020.05.031
12. Aktoğu S, Yuncu G, Halilçolar H, Ermete S, Buduneli T. Bronchogenic cysts: clinicopathological presentation and treatment. Eur Respir J (1996) 9(10):2017–21. doi: 10.1183/09031936.96.09102017
13. McAdams HP, Kirejczyk WM, Rosado-de-Christenson ML, Matsumoto S. Bronchogenic cyst: imaging features with clinical and histopathologic correlation. Radiology (2000) 217(2):441–6. doi: 10.1148/radiology.217.2.r00nv19441
14. Sumiyoshi K, Shimizu S, Enjoji M, Iwashita A, Kawakami K. Bronchogenic cyst in the abdomen. Virchows Arch A Pathol Anat Histopathol (1985) 408(1):93–8. doi: 10.1007/BF00739965
15. Hu BY, Yu H, Shen J (2022). A retroperitoneal bronchogenic cyst clinically mimicking an adrenal mass: three case reports and a literature review. J. Int. Med. Res. 50 (1):3000605211072664.
16. Tadokoro T, Misumi T, Itamoto T, Nakahara H, Matsugu Y, Ikeda S, et al. (2022). Retroperitoneal bronchogenic cyst resected by single-incision laparoscopic surgery in an adolescent female: A case report. Asian J. Endosc Surg. 15 (1):206–210.
17. Cowan S, Gunawardene A, Davenport E (2021). Retroperitoneal bronchogenic cyst mistaken as an adrenal adenoma. ANZ J. Surg. 91 (7-8):E526–E527.
18. Yuan K, Shu M, Ma Y, Feng W, Ye J, Yuan Y. Ectopic bronchogenic cyst in the retroperitoneal region: a case report and literature review of adult patients. BMC Surg (2021) 21(1):347. doi: 10.1186/s12893-021-01341-w
19. Qingyu J, Xiaolong L, Ruohan Z, Licong M, Zhichao T, Qingwei C, et al. (2021). Computed tomography helps pre-operative evaluation before laparoscopic resection of retroperitoneal bronchogenic cyst: A case report. J. Minim Access Surg. 17 (1):95–97.
20. Wen Y, Chen W, Chen J, He X (2020). Retroperitoneal bronchogenic cyst resembling an adrenal tumor: two case reports and literature review. J. Int. Med. Res. 48 (5):300060520925673.
21. Sinha V, Nandi P, Shankar M, Sardana N (2020). Retroperitoneal bronchogenic cyst: A rare case study. Cureus 12 (9), e10421.
22. Liu Q, Gao Y, Zhao Z, Zhao G, Liu R, Lau WY. Robotic resection of benign nonadrenal retroperitoneal tumors: A consecutive case series. Int J Surg (2018) 55:188–92. doi: 10.1016/j.ijsu.2018.04.013
23. Yoon YR, Choi J, Lee SM, Kim YJ, Cho HD, Lee JW, et al. (2015). Retroperitoneal bronchogenic cyst presenting paraadrenal tumor incidentally detected by (18)F-FDG PET/CT. Nucl. Med. Mol. Imaging. 49 (1):69–72.
24. Bulut G, Bulut MD, Bahadır I, Kotan Ç (2015). Bronchogenic cyst mimicking an adrenal mass in the retroperitoneal region: report of a rare case. Indian J. Pathol. Microbiol. 58 (1):96–98.
25. Jiang X, Zeng H, Gong J, Huang R (2015). Unusual uptake of radioiodine in a retroperitoneal bronchogenic cyst in a patient with thyroid carcinoma. Clin. Nucl. Med. 40 (5):435–436.
26. Trehan M, Singla S, Singh J, Garg N, Mahajan A. A rare case of intraabdominal bronchogenic cyst- a case report. J Clin Diagn Res (2015) 9(11):Pd03–4. doi: 10.7860/JCDR/2015/12949.6761
27. Zhang D, Zhang Y, Liu X, Zhu J, Feng C, Yang C, et al. (2015). Challenge in preoperative diagnosis of retroperitoneal mucinous cyst in a pediatric patient. Int. J. Clin. Exp. Med. 8 (10):19540–19547.
28. Terasaka T, Otsuka F, Ogura-Ochi K, Miyoshi T, Inagaki K, Kobayashi Y, et al. (2014). Retroperitoneal bronchogenic cyst: a rare incidentaloma discovered in a juvenile hypertensive patient. Hypertens. Res. 37 (6):595–597.
29. Cao DH, Zheng S, Lv X, Yin R, Liu LR, Yang L, et al. (2014). Multilocular bronchogenic cyst of the bilateral adrenal: report of a rare case and review of literature. Int. J. Clin. Exp. Pathol. 7 (6):3418–3422.
30. Dong B, Zhou H, Zhang J, Wang Y, Fu Y. (2014). Diagnosis and treatment of retroperitoneal bronchogenic cysts: A case report. Oncol Lett 7 (6):2157–9.
31. Castro R, Oliveira MI, Fernandes T, Madureira AJ (2013). Retroperitoneal bronchogenic cyst: MRI findings. Case Rep. Radiol. 2013:853795.
32. Runge T, Blank A, Schäfer SC, Candinas D, Gloor B, Angst E (2013). A retroperitoneal bronchogenic cyst mimicking a pancreatic or adrenal mass. Case Rep. Gastroenterol. 7 (3):428–432.
33. Cai Y, Guo Z, Cai Q, Dai S, Gao W, Niu Y, et al. (2013). Bronchogenic cysts in retroperitoneal region. Abdom Imaging. 38 (1):211–214.
34. Jannasch O, Büschel P, Wodner C, Seidensticker M, Kuhn R, Lippert H, et al. (2013). Retroperitoneoscopic and laparoscopic removal of periadrenally located bronchogenic cysts–a systematic review. Pol. Przegl Chir. 85 (12):706–713.
35. O'Neal PB, Moore FD, Gawande A, Cho NL, King EE, Moalem J, et al. (2012). Bronchogenic cyst masquerading as an adrenal tumor: a case of mistaken identity. Endocr. Pract. 18 (5):e102–e105.
36. Alguraan Z, Agcaoglu O, El-Hayek K, Hamrahian AH, Siperstein A, Berber E. Retroperitoneal masses mimicking adrenal tumors. Endocr Pract (2012) 18(3):335–41. doi: 10.4158/EP11240.OR
37. Díaz Nieto R, Naranjo Torres A, Gómez Alvarez M, Ruiz Rabelo JF, Pérez Manrique MC, Ciria Bru R, et al. (2010). Intraabdominal bronchogenic cyst. J. Gastrointest Surg. 14 (4):756–758.
38. Inaba K, Sakurai Y, Umeki Y, Kanaya S, Komori Y, Uyama I (2010). Laparoscopic excision of subdiaphragmatic bronchogenic cyst occurring in the retroperitoneum: Report of a case. Surg. Laparosc Endosc Percutan Tech 20 (6):e199–e203.
39. El Youssef R, Fleseriu M, Sheppard BC (2010). Adrenal and pancreatic presentation of subdiaphragmatic retroperitoneal bronchogenic cysts. Arch Surg 145 (3):302–4.
40. Obando J, Merkle E, Bean SM (2009). A retroperitoneal bronchogenic cyst. Clin. Gastroenterol. Hepatol. 7 (8):A24–Ae1.
41. Chung JM, Jung MJ, Lee W, Choi S (2009). Retroperitoneal bronchogenic cyst presenting as adrenal tumor in adult successfully treated with retroperitoneal laparoscopic surgery. Urology 73 (2):442.e13–5.
42. Roma A, Varsegi M, Magi-Galluzzi C, Ulbright T, Zhou M (2008). The distinction of bronchogenic cyst from metastatic testicular teratoma: A light microscopic and immunohistochemical study. Am. J. Clin. Pathol. 130 (2):265–273.
43. Minei S, Igarashi T, Hirano D (2007). A case of retroperitoneal bronchogenic cyst treated by laparoscopic surgery. Hinyokika Kiyo. 53 (3):171–174.
44. Chu PY, Hwang TI, Teng TH, Lee CC (2007). A retroperitoneal bronchogenic cyst successfully treated by laparoscopic surgery. Ann. Saudi Med. 27 (3):199–200.
45. Terry NE, Senkowski CK, Check W, Brower ST (2007). Retroperitoneal foregut duplication cyst presenting as an adrenal mass. Am. Surg. 73 (1):89–92.
46. Ishizuka O, Misawa K, Nakazawa M, Nishizawa O (2004). A retroperitoneal bronchogenic cyst: laparoscopic treatment. Urol Int. 72 (3):269–270.
47. Ishikawa T, Kawabata G, Okada H, Arakawa S, Kamidono S, Fujisawa M (2003). Retroperitoneal bronchogenic cyst managed with retroperitoneoscopic surgery. J. Urol. 169 (3):1078–1079.
48. Hedayati N, Cai DX, McHenry CR (2003). Subdiaphragmatic bronchogenic cyst masquerading as an "adrenal incidentaloma". J. Gastrointest Surg. 7 (6): 802–804.
49. McCrystal DJ, Borzi PA (2002). Retroperitoneoscopic resection of retroperitoneal bronchogenic cysts. Pediatr. Surg. Int. 18 (5-6):375–377.
50. Yamamoto E, Nakayama H, Ozaki N, Kitamura Y, Funatsuka M, Ueda M, et al. (1998). Laparoscopically resected foregut cyst adjacent to the right adrenal gland. Diagn. Ther. Endosc. 5 (1):53–56.
51. Tokuda N, Naito S, Uozumi J, Shimura H, Takayanagi R, Kumazawa J. A retroperitoneal bronchogenic cyst treated with laparoscopic surgery. J Urol (1997) 157(2):619. doi: 10.1016/S0022-5347(01)65220-0
52. Liang MK, Yee HT, Song JW, Marks JL. Subdiaphragmatic bronchogenic cysts: a comprehensive review of the literature. Am Surg (2005) 71(12):1034–41. doi: 10.1177/000313480507101210
53. Rud O, May M, Brookman-Amissah S, Moersler J, Greiner A, Gilfrich C. [Retroperitoneal bronchogenic cyst treated by laparoscopic surgery]. Chirurg (2010) 81(3):243–6. doi: 10.1007/s00104-009-1799-4
54. Cetinkurşun S, Oztürk H, Celasun B, Sakarya MT, Sürer I. Isolate abdominal bronchogenic cyst: A case report. Eur J Pediatr Surg (1997) 7(2):103–5. doi: 10.1055/s-2008-1071064
55. Govaerts K, Van Eyken P, Verswijvel G, Van der Speeten K. A bronchogenic cyst, presenting as a retroperitoneal cystic mass. Rare Tumors (2012) 4(1):e13. doi: 10.4081/rt.2012.e13
56. Murakami R, Machida M, Kobayashi Y, Ogura J, Ichikawa T, Kumazaki T. Retroperitoneal bronchogenic cyst: CT and MR imaging. Abdom Imaging (2000) 25(4):444–7. doi: 10.1007/s002610000019
57. Liang MK, Marks JL. Congenital bronchogenic cyst in the gastric mucosa. J Clin Pathol (2005) 58(12):1344.
58. Choi KK, Sung JY, Kim JS, Kim MJ, Park H, Choi DW, et al. Intraabdominal bronchogenic cyst: report of five cases. Korean J Hepatobil Pancreat Surg (2012) 16(2):75–9. doi: 10.14701/kjhbps.2012.16.2.75
59. Doggett RS, Carty SE, Clarke MR. Retroperitoneal bronchogenic cyst masquerading clinically and radiologically as a phaeochromocytoma. Virchows Arch (1997) 431(1):73–6. doi: 10.1007/s004280050071
60. Giulianotti PC, Coratti A, Angelini M, Sbrana F, Cecconi S, Balestracci T, et al. Robotics in general surgery: personal experience in a large community hospital. Arch Surg (2003) 138(7):777–84. doi: 10.1001/archsurg.138.7.777
Keywords: bronchogenic cysts, laparoscopic surgery, retroperitoneal neoplasm, case report, retroperitoneal bronchogenic cyst
Citation: Li H, Xu J, Feng Q, Cai Z and Li J (2022) Case report: The safety of laparoscopic surgery for the retroperitoneal bronchogenic cyst. Front. Oncol. 12:1011076. doi: 10.3389/fonc.2022.1011076
Received: 03 August 2022; Accepted: 20 September 2022;
Published: 12 October 2022.
Edited by:
Ugo Cioffi, University of Milan, ItalyCopyright © 2022 Li, Xu, Feng, Cai and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jiaxin Li, NDA3NzIzMDgwQHFxLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.