- 1Department of Anesthesiology, West China Hospital of Sichuan University, Chengdu, China
- 2Laboratory of Anesthesia and Critical Care Medicine, National-Local Joint Engineering Research Centre of Translational Medicine of Anesthesiology, West China Hospital of Sichuan University, Chengdu, China
- 3Department of Anesthesiology & Key Laboratory of Birth Defects and Related Diseases of Women and Children, Ministry of Education, West China Second Hospital of Sichuan University, Chengdu, China
Surgical resection is the main curative avenue for various cancers. Unfortunately, cancer recurrence following surgery is commonly seen, and typically results in refractory disease and death. Currently, there is no consensus whether perioperative epidural analgesia (EA), including intraoperative and postoperative epidural analgesia, is beneficial or harmful on cancer recurrence and survival. Although controversial, mounting evidence from both clinical and animal studies have reported perioperative EA can improve cancer recurrence and survival via many aspects, including modulating the immune/inflammation response and reducing the use of anesthetic agents like inhalation anesthetics and opioids, which are independent risk factors for cancer recurrence. However, these results depend on the cancer types, cancer staging, patients age, opioids use, and the duration of follow-up. This review will summarize the effects of perioperative EA on the oncological outcomes of patients after cancer surgery.
Introduction
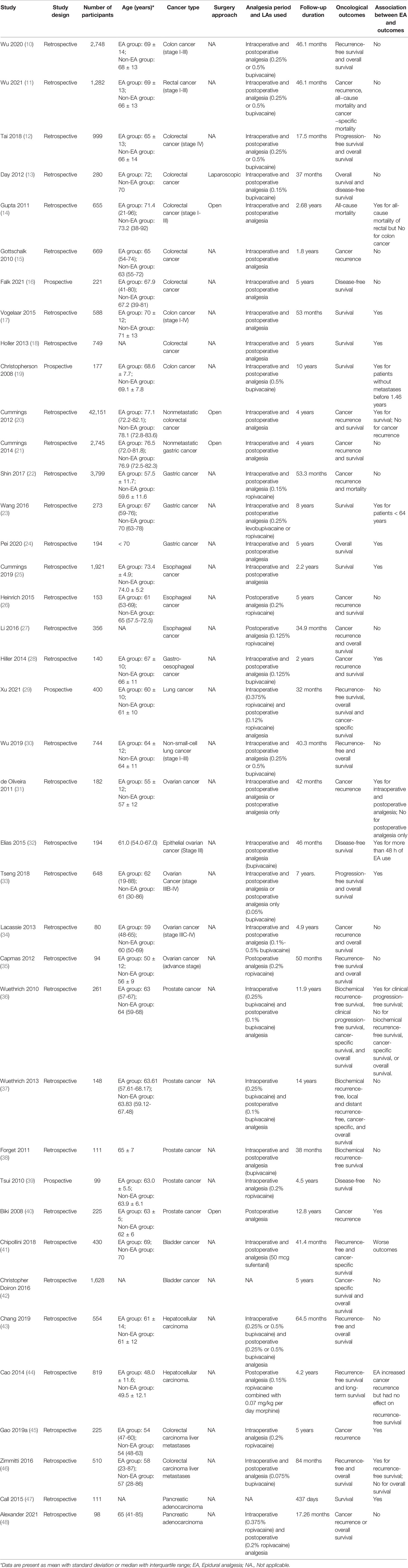
Cancer has become a major cause of death worldwide, while metastasis and/or recurrence is the major cause of death from cancer (1–3). Surgical resection of primary solid tumors remains a cornerstone of cancer treatment (4). However, the surgical process is associated with immunosuppression, which may generate a high vulnerability for tumor worse progression (4–6). Meanwhile, several drugs, such as volatile anesthetics and opioids during perioperative periods were also suggested to be implicated in immunosuppression and cancer recurrence (7). Regional anesthesia (RA), such as epidural anesthesia, spinal aesthesia, paravertebral block, can provide effective pain relief preoperatively (8). The adjunctive use of RA for general anesthesia is believed to decrease the requirement of opioids and general anesthetics consumption, and attenuate surgical-related stress and immunosuppression (9). Therefore, RA is theoretically suggested to have potential impacts on oncological outcomes in patients underwent cancer surgeries. Among various regional techniques in RA, the most commonly used for cancer surgery is perioperative epidural analgesia (EA), including both intraoperative or postoperative use. Currently, there is no definitive consensus whether perioperative EA is beneficial to cancer recurrence and survival. Cancer types and staging may be the major contributors to these inconsistent results. In this review, we summarized the current evidences regarding the effects of perioperative EA on recurrence and survival for various cancer types. Study characteristics were summarized in Table 1.
Effects of Surgery on Cancer Recurrence
Surgical resection is the main curative avenue for various solid cancers (1). Unfortunately, minimal residual disease may be present persistently after treatment, which can cause metastasis and recurrence (49). Meanwhile, the operation and general anesthesia process themself may facilitate the tumor metastasis and recurrence through several ways, such as stress and immune/inflammation responses, and postoperative pain (50–55). Furthermore, tissue damage caused by surgery, especially the local pro-inflammatory and wound-healing responses, were associated with local and distant recurrence (56). Additionally, postoperative pain is suggested as an important contributor to suppress immunity function, thus promoting cancer progression (49, 57). For general anesthesia, inhaled anesthetics and opioids were reported to be related to worse oncological outcomes for cancer surgeries (20). Therefore, the perioperative period represents as a critical timeframe for metastatic progression and cancer recurrence.
Effects of Perioperative EA on Cancer Recurrence
Mounting evidence from both clinical and animal researches indicated that perioperative EA could improve cancer recurrence and survival (17, 28, 31). The underlying mechanism remains elusive, which was mainly attributed to improve immunosuppression via attenuating surgical stress and postoperative pain, reducing requirements for opioid and anesthetics, and direct anti-metastasis effects of local anesthetics (58).
Perioperative EA Attenuates Surgical Stress and Pain
During and/or after the surgical resection of tumor, stress responses and pain are commonly existed and interacted, which may cause immunosuppression, thus promoting cancer recurrence (59, 60). Perioperative EA was reported to attenuate the immunosuppression by inhibiting the stress responses and/or alleviating the perioperative pain (58). Meanwhile, perioperative EA can improve the function of immunity via preserve and/or increase the numbers of immune cells and reduce the plasma concentrations of immune suppressive soluble factors (61–65).
Perioperative EA Reduces Opioid and Anesthetics Requirements
Opioids were suggested to be an important factor that suppress the immune function (66, 67). For example, morphine and remifentanil suppress NK cell activity and T cell differentiation, and promote lymphocyte apoptosis (68–71). Likewise, fentanyl and sufentanil decrease NK cell activity or leukocyte migration (72–74). In addition to opioids, previous studies reported that volatile anesthetics are also independent risk factors of cancer recurrence (75–78). It is well known that perioperative EA significantly reduced the requirements for perioperative opioids and volatile anesthetics use during the cancer surgery, thus influencing the oncological outcomes (58, 79, 80).
Direct Anti-Metastasis Effects of Local Anesthetics
Metastasis is an important factor for cancer recurrence and is the major cause of death from most malignant cancers. During the process of metastasis, tumor cells undergo several steps known as the metastatic cascade. At the primary site, tumor cells escape from the antitumor immune response, invade the surrounding parenchyma and intravasate into blood and/or lymphatic vessels, which allows them to circulate and spread. At the metastatic site, these circulating tumor cells extravasate from the blood and/or lymphatic vessel, survive and proliferate to form the metastatic tumor (3). Local anesthetics used in RA were suggested to directly inhibit the metastasis process (81, 82). For example, lidocaine has anti-growth and anti-metastatic properties towards lung cancer cells (83). Ropivacaine is demonstrated to reduce the proliferation of breast cancer cells and induce the apoptosis processes (84). Although there is no consensus whether different local anesthetics have different effects on the cancer outcomes in vivo, it is suggested that all local anesthetics at high concentrations are toxic to cancer cells in vitro with different potencies (bupivacaine > lidocaine > ropivacaine) (85). The underlying mechanism remains elusive, which may involves ion channels (86–89), inflammatory pathways (90, 91), and cancer stem cells (92, 93).
Effects of Perioperative EA on Certain Cancer Types
In clinic, perioperative EA is commonly used for thoracic and abdominal surgeries due to many advantage aspects, such as postoperative pain management, reducing requirements for anesthetics as well as postoperative complications (58, 94, 95). However, the potential benefit of perioperative EA on cancer recurrence and survival is debated in patients undergoing thoracic and abdominal surgeries, which is suggested most likely related to cancer types. Du et al. evaluated the effects of perioperative EA on the long-term oncological outcomes in elderly patients (60 to 90 years old) with major thoracic and abdominal surgeries. The results found that, compared with general anesthesia alone with postoperative intravenous analgesia, combined epidural-general anesthesia with postoperative epidural analgesia did not improve overall or cancer-specific mortality, or the recurrence-free survival after a median follow-up duration of 66 months (96). Similarly, another retrospective study also did not support an association between postoperative EA use and recurrence-free and overall survival after abdominal cancer surgery (97). One randomized controlled trial (RCT) involving 503 patients also found that postoperative EA use had no effects on cancer-free survival after abdominal cancer surgery (98). The effects of perioperative EA on long-term oncological outcomes were varied for specific cancer surgery.
Effects of Perioperative EA on Colorectal Cancer Surgery
A large number of retrospective studies have evaluated the effects of perioperative EA on oncological outcomes in patients underwent colorectal cancer surgeries, but the results were inconsistent. One study compared the effects of perioperative EA (combined intraoperative and postoperative analgesia) with intravenous opioid analgesia in patients receiving surgery for colon cancer (stage I to III). No association was found between perioperative EA use and cancer recurrence or death with 46.1 months duration of follow-up. However, higher level of preoperative carcinoembryonic antigen, perioperative blood transfusion, advanced cancer stage, and pathological lymphovascular invasion were independent risk factors for cancer recurrence and death in these patients (10). In patients with rectal cancer resection (stage I-III), postoperative EA also did not improve recurrence or mortality with a follow-up duration of 46.1 months when compared to opioids analgesia (11). For patients with stage IV colorectal cancer, one study involving 999 patients showed perioperative EA was not associated with better progression-free or overall survival after surgeries with 17.5 months follow-up (12). In patients underwent laparoscopic colorectal resection for adenocarcinoma, Day et al. showed that postoperative EA had no significant advantage in 5-year overall or disease-free survival than opioids analgesia (13). In contrast, one study revealed that, compared with patient-controlled analgesia, postoperative EA reduces all-cause mortality after open resection of rectal but not colon cancer in patients (14). Furthermore, the results suggested that elder age (>72 years old) and cancer stage (stages 2 and/or 3) were risk factors for death after colon and rectal cancer surgeries. Interestingly, in another study, age was also supposed to be a factor to influence the effects of perioperative EA on oncological outcomes. Gottschalk et al. showed that, although perioperative EA for colorectal cancer surgery did not improve cancer recurrence with a median follow-up time of 1.8 years, a potential benefit was observed in older patients (> 64 years old) (15). Taken together, these findings suggest that the effects of perioperative EA on oncological outcomes after colorectal cancer surgery may be related to the cancer types, stage, patients’ age, and surgery approach, which need further well-designed studies to determine.
Few prospective studies investigated the effects of EA on the cancer recurrence and/or mortality after surgery for colorectal cancer. One multicenter RCT found that, compared with intravenous morphine analgesia, perioperative EA did not improve 5 years disease-free survival in patients underwent colorectal cancer surgery, although perioperative EA significantly reduced postoperative pain during the first 24 h after surgery (16).
However, epidural anesthesia use is also reported beneficial for oncological outcomes in patients after colorectal cancer surgery. One retrospective study revealed that perioperative EA was associated with a better five-year overall survival in patients underwent colorectal cancer surgery. Subgroup analysis also showed that EA contributed to a better overall survival in patients of 80 years and older (17). Another retrospective study also showed that EA improved 5-year survival in patients after colorectal carcinoma surgeries (18).
Christopherson et al. suggested that the potential benefits of perioperative EA depend on cancer staging. They showed that epidural block was associated with enhanced survival in patients without metastases before 1.46 years, but not in patients without metastases after 1.46 years or with metastases (19). Also, Cummings et al. found that perioperative EA improved 5-year survival in patients with nonmetastatic colorectal cancer after open surgery, but did not decrease cancer recurrence (20).
Effects of Perioperative EA on Gastric Cancer Surgery
For gastric cancer surgeries, the results regarding the effects of EA on oncological outcomes were also conflicting. Most evidences suggest that EA use is not associated with better oncological outcomes in patients underwent gastric cancer surgeries. Compared with intravenous analgesia, perioperative EA was not associated with improved recurrence or survival in patients after gastric cancer surgeries (21, 22). Compared with general anesthesia, epidural anesthesia also showed no effects on the long-term survival of patients after gastric cancer surgeries, but the benefit was observed in younger patients (age up to 64) (23). Furthermore, compared with patient-controlled intravenous analgesia, postoperative EA did not provide better short-term outcomes in patients underwent laparoscopic distal gastrectomy for gastric cancer (99). EA was even associated with a longer length of stay for patients underwent open elective gastrectomies for nonmetastatic cancer (100). Currently, only one retrospective study supported an association between EA use and survival after gastric cancer surgery. The results found that the 5-year overall survival rates were higher in patients receiving general anesthesia combined perioperative EA than that receiving general anesthesia alone (24).
Effects of Perioperative EA on Esophageal Cancer
Four studies have evaluated the effects of EA on oncological outcomes after esophageal surgeries (25–28). Heinrich et al. showed that postoperative EA did not improve cancer recurrence, 1-year mortality, or 5-year survival after esophagus cancer surgery, although it significantly decreased postoperative opioid consumption and the duration of ICU hospitalization (26). Li et al. also confirmed the benefits of postoperative EA on the short-term outcomes after esophagectomy for cancer, such as attenuating inflammatory response, reducing the incidence of pneumonia and anastomotic leakage, but did not support an association between postoperative EA use and improved 3-year overall recurrence and survival (27). The other two retrospective studies revealed potential benefits of EA on oncological outcomes of EA, of which one study found that perioperative EA was associated with better cancer recurrence and survival after esophageal surgery with 2-year follow-up (28). The other one showed that perioperative EA was associated with better 90-day survival after esophagectomy. Additionally, compared with transthoracic esophagectomy, the five-year survival rates were higher after transhiatal esophagectomy (25), suggesting that the surgical approach may influence the effects of EA on oncological outcomes. Prospective RCTs are needed to assess whether perioperative EA use can improve the cancer recurrence and/or survival after esophageal cancer surgeries.
Effects of Perioperative EA on Lung Cancer
The current evidences from prospective and retrospective studies do not show a role of perioperative EA use in improving oncological outcomes after lung cancer surgeries. One randomized trial showed that, compared with general anesthesia alone, the combining use with perioperative EA did not improve recurrence-free, overall, or cancer-specific survival in patients after major lung cancer surgery after median follow-up duration of 32 months (29). In patients having non-small-cell lung cancer resection, one retrospective study showed that thoracic epidural analgesia was not associated with better 3-year recurrence-free and overall survival (30). Wu et al. reported that postoperative EA after surgery for non-small cell lung cancer had no association with better 2-year or 5-year recurrence-free survival or overall survival rates. Instead, elder age (≥ 65 years old), male gender, higher body mass index (≥ 25 kg/m2), ASA 4, preoperative blood transfusions, pneumonectomy, and postoperative radiation implicated in decreased recurrence-free survival and overall survival (30). Therefore, perioperative EA use appears to not be a factor for oncological outcomes after lung cancer surgeries.
Effects of Perioperative EA on Ovarian Cancer
The current evidences are conflicting regarding the effects of epidural anesthesia in patients with ovarian cancer surgeries. One study showed that perioperative EA was associated with an increased time to tumor recurrence in patients after ovarian cancer surgery (31). Elias et al. found that the additional use of perioperative EA in general anesthesia was also associated with a lower rate of recurrence in patients with stage III ovarian cancer (32). Tseng et al. reported that perioperative EA was associated with improved progression-free survival (70.8 months follow-up) and overall survival (68.8 months follow-up) in patients with advanced ovarian cancer surgeries (33). However, two studies reported the negative results. One study found that the addition of perioperative EA in general anesthesia did not increase the time to recurrence or overall survival in patients with advanced ovarian cancer surgeries (34). Postoperative EA also did not improve recurrence-free survival and overall survival in patients with advanced-stage ovarian cancer surgery (35).
Effects of Perioperative EA on Prostate Cancer
The potential impacts of perioperative EA on oncological outcomes in patients with surgeries for prostate cancer are debated. Most evidences point that perioperative EA was not associated with better oncological outcomes in these patients. One study showed that, compared with ketorolac-morphine analgesia, intraoperative and postoperative epidural analgesia did not improve biochemical recurrence-free survival (11.8 years follow-up), 5-year and 10-year cancer-specific survival, or 5 year and 10-year overall survival after open radical prostatectomy (36). Wuethrich et al. also reported that general anesthesia combined with perioperative EA did not improve cancer progression or survival after retropubic radical prostatectomy for prostate cancer with 14 years follow-up (37). One retrospective analysis revealed that intraoperative EA was not, but sufentanil administration was associated with an increased risk of cancer recurrence after retropubic radical prostatectomies with a median follow-up of 38 months (38). Similarly, Tsui et al. demonstrated that, compared with general anesthesia alone, combined general anesthesia with intraoperative EA did not improve disease-free survival following radical prostatectomy for adenocarcinoma with 4.5 years follow-up (39). Currently, only one retrospective study investigated the potential effects of postoperative EA on the long-term outcomes after prostate cancer surgeries, and the results showed that postoperative EA improved cancer recurrence for open prostatectomy surgery (40). Recently, Robot-assisted radical prostatectomy (RARP) has been widely used for prostate cancer and show some potential benefits than open radical prostatectomy, such as improved peri-operative outcomes and functional outcomes (101, 102). Emerging evidence showed that, compared with general anesthesia alone, combined general anesthesia and perioperative EA provided better outcomes in patients undergoing RARP, such as attenuating the severity of postoperative diaphragmatic dysfunction (103) and improving intraoperative ventilation/oxygenation (104). However, no studies have yet investigated the effects of perioperative EA on the oncological outcomes after RARP. It is interesting to determine this in future studies.
Effects of Perioperative EA on Bladder Cancer
Limited evidence assessed the effects of EA use on the oncological outcomes after bladder cancer surgeries (105). One study evaluated the influence of EA with sufentanil-based epidural analgesia on cancer outcomes in patients receiving radical cystectomy. The results showed that compared with general anesthesia alone, combined general anesthesia with perioperative EA was associated with worse recurrence and disease-free survival for bladder cancer surgeries with 41.4 months follow-up (41), which may be due to the increased opioids use. In another study, Christopher Doiron et al. reported that EA was not associated with cancer-specific survival or overall survival in patients underwent radical cystectomy for bladder cancer (42).
Effects of Perioperative EA on Hepatocellular Carcinoma
Few studies have evaluated the effects of EA on the oncological outcomes after surgical resection for hepatocellular carcinoma. One retrospective analysis showed no association between perioperative EA use and cancer recurrence or overall survival in patients after surgical resection of hepatocellular carcinoma with a median follow-up time of 64.5 months (43). However, compared with postoperative intravenous analgesia with fentanyl, postoperative EA with morphine increased cancer recurrence and survival but had no effects on recurrence-free survival in patients undergoing resection of hepatocellular carcinoma with a median follow-up time of 4.2 years (44).
Two studies have investigated the association between perioperative EA use and oncological outcomes in patients with colorectal carcinoma liver metastases. Unexpectedly, one study reported that, compared with combined general anesthesia-intraoperative EA, general anesthesia alone may provide a better survival outcome for resected colorectal carcinoma liver metastases with 60 months follow-up (45). However, another study showed that, compared to intravenous analgesia, perioperative EA improved five-year recurrence-free, but not overall survival after colorectal carcinoma liver metastases resection (46).
Effects of Perioperative EA on Pancreatic Cancer
Epidural analgesia has been used widely in patients underwent pancreatic cancer surgeries due to several advantages such as improved pain control, improved infectious and pulmonary complications (106), although it may be contraindicated in elderly patients for increased risk of epidural-induced hypotension or malfunction (107). Currently, limited evidence put insights on the relationship between perioperative EA use and oncological outcomes after pancreatic cancer surgeries. One study investigated the effects of perioperative EA on oncologic outcomes in patients after resection of pancreatic cancer. The results indicated that perioperative EA was associated with prolonged survival in patients underwent resection of pancreatic adenocarcinoma with a median follow-up time of 437 days (47). Whereas, Alexander et al. reported no association between EA use and recurrence or overall survival in patients underwent radical resection of pancreatic adenocarcinoma, although subgroup analysis revealed a trend towards a longer overall survival associated with perioperative EA in patients with better differentiation of pancreatic adenocarcinoma (48). The concentration of LAs may also influence the effects of EA on the oncological outcomes in patients after pancreatic surgery. One retrospective cohort study reported that, compared with low concentration (0.15%-0.25%) of ropivacaine, intraoperative EA with high concentration (0.375%-0.5%) of ropivacaine was associated with improved overall survival in patients underwent pancreatectomy (108).
Conclusion
Although it is generally recognized that perioperative EA has advantages in modulating the surgical stress, inflammatory, and immunological responses in patients after cancer surgeries, no definitive evidence yet support or refute an association between the use of perioperative EA and improved cancer recurrence and/or survival. The effects of perioperative EA on oncological outcomes likely depend on the cancer types, cancer staging, patients’ age, opioids use, and the duration of follow-up. Large prospective multicenter RCTs are needed to assess the role of EA in long-term oncological outcomes for cancer surgeries.
Author Contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Funding
This work was supported by Grant No. 81801117 and 81974164 from the National Natural Science Foundation of China; Grant No. 2021M692276 from China Postdoctoral Science Foundation; and Grant No. 21PJ014 from Medical Science and Technology Project of Sichuan Provincial Health Commission.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Cakmakkaya OS, Kolodzie K, Apfel CC, Pace NL. Anaesthetic Techniques for Risk of Malignant Tumour Recurrence. Cochrane Database Syst Rev (2014) CD008877. doi: 10.1002/14651858.CD008877.pub2
2. Gupta GP, Massagué J. Cancer Metastasis: Building a Framework. Cell (2006) 127:679–95. doi: 10.1016/j.cell.2006.11.001
3. Kitamura T, Qian BZ, Pollard JW. Immune Cell Promotion of Metastasis. Nat Rev Immunol (2015) 15:73–86. doi: 10.1038/nri3789
4. Le-Wendling L, Nin O, Capdevila X. Cancer Recurrence and Regional Anesthesia: The Theories, the Data, and the Future in Outcomes. Pain Med (2016) 17:756–75. doi: 10.1111/pme.12893
5. Cata JP, Bauer M, Sokari T, Ramirez MF, Mason D, Plautz G, et al. 1-2 Effects of Surgery, General Anesthesia, and Perioperative Epidural Analgesia on the Immune Function of Patients With Non-Small Cell Lung Cancer. J Clin Anesth (2013) 25:255–62. doi: 10.1016/j.jclinane.2012.12.007
6. Ramirez MF, Ai D, Bauer M, Vauthey JN, Gottumukkala V, Kee S, et al. Innate Immune Function After Breast, Lung, and Colorectal Cancer Surgery. J Surg Res (2015) 194:185–93. doi: 10.1016/j.jss.2014.10.030
7. Guerrero Orriach JL, Raigon Ponferrada A, Malo Manso A, Herrera Imbroda B, Escalona Belmonte JJ, Ramirez Aliaga M, et al. Anesthesia in Combination With Propofol Increases Disease-Free Survival in Bladder Cancer Patients Who Undergo Radical Tumor Cystectomy as Compared to Inhalational Anesthetics and Opiate-Based Analgesia. Oncol (2020) 98:161–7. doi: 10.1159/000504807
8. Hutton M, Brull R, Macfarlane AJR. 13-9 Regional Anaesthesia and Outcomes. BJA Educ (2018) 18:52–6. doi: 10.1016/j.bjae.2017.10.002
9. O’Riain SC, Buggy DJ, Kerin MJ, Watson RW, Moriarty DC. 13-14 Inhibition of the Stress Response to Breast Cancer Surgery by Regional Anesthesia and Analgesia Does Not Affect Vascular Endothelial Growth Factor and Prostaglandin E2. Anesth Analg (2005) 100:244–9. doi: 10.1213/01.Ane.0000143336.37946.7d
10. Wu HL, Tai YH, Mandell MS, Tsou MY, Yang SH, Chen TH, et al. Effect of Epidural Analgesia on Cancer Prognosis After Colon Cancer Resection: A Single-Centre Cohort Study in Taiwan. BMJ Open (2020) 10:e036577. doi: 10.1136/bmjopen-2019-036577
11. Wu HL, Tai YH, Lin SP, Yang SH, Tsou MY, Chang KY. Epidural Analgesia Does Not Impact Recurrence or Mortality in Patients After Rectal Cancer Resection. Sci Rep (2021) 11:913. doi: 10.1038/s41598-020-79657-5
12. Tai YH, Chang WK, Wu HL, Chan MY, Chen HH, Chang KY. 4-31 The Effect of Epidural Analgesia on Cancer Progression in Patients With Stage IV Colorectal Cancer After Primary Tumor Resection: A Retrospective Cohort Study. PloS One (2018) 13:e0200893. doi: 10.1371/journal.pone.0200893
13. Day A, Smith R, Jourdan I, Fawcett W, Scott M, Rockall T. Retrospective Analysis of the Effect of Postoperative Analgesia on Survival in Patients After Laparoscopic Resection of Colorectal Cancer. Br J Anaesth (2012) 109:185–90. doi: 10.1093/bja/aes106
14. Gupta A, Björnsson A, Fredriksson M, Hallböök O, Eintrei C. Reduction in Mortality After Epidural Anaesthesia and Analgesia in Patients Undergoing Rectal But Not Colonic Cancer Surgery: A Retrospective Analysis of Data From 655 Patients in Central Sweden. Br J Anaesth (2011) 107:164–70. doi: 10.1093/bja/aer100
15. Gottschalk A, Ford JG, Regelin CC, You J, Mascha EJ, Sessler DI, et al. Association Between Epidural Analgesia and Cancer Recurrence After Colorectal Cancer Surgery. Anesthesiol (2010) 113:27–34. doi: 10.1097/ALN.0b013e3181de6d0d
16. Falk W, Magnuson A, Eintrei C, Henningsson R, Myrelid P, Matthiessen P, et al. Comparison Between Epidural and Intravenous Analgesia Effects on Disease-Free Survival After Colorectal Cancer Surgery: A Randomised Multicentre Controlled Trial. Br J Anaesth (2021) 127:65–74. doi: 10.1016/j.bja.2021.04.002
17. Vogelaar FJ, Abegg R, van der Linden JC, Cornelisse HG, van Dorsten FR, Lemmens VE, et al. Epidural Analgesia Associated With Better Survival in Colon Cancer. Int J Colorectal Dis (2015) 30:1103–7. doi: 10.1007/s00384-015-2224-8
18. Holler JP, Ahlbrandt J, Burkhardt E, Gruss M, Röhrig R, Knapheide J, et al. Peridural Analgesia may Affect Long-Term Survival in Patients With Colorectal Cancer After Surgery (PACO-RAS-Study): An Analysis of a Cancer Registry. Ann Surg (2013) 258:989–93. doi: 10.1097/SLA.0b013e3182915f61
19. Christopherson R, James KE, Tableman M, Marshall P, Johnson FE. Long-Term Survival After Colon Cancer Surgery: A Variation Associated With Choice of Anesthesia. Anesth Analg (2008) 107:325–32. doi: 10.1213/ane.0b013e3181770f55
20. Cummings KC 3rd, Xu F, Cummings LC, Cooper GS. A Comparison of Epidural Analgesia and Traditional Pain Management Effects on Survival and Cancer Recurrence After Colectomy: A Population-Based Study. Anesthesiol (2012) 116:797–806. doi: 10.1097/ALN.0b013e31824674f6
21. Cummings KC 3rd, Patel M, Htoo PT, Bakaki PM, Cummings LC, Koroukian S. A Comparison of the Effects of Epidural Analgesia Versus Traditional Pain Management on Outcomes After Gastric Cancer Resection: A Population-Based Study. Reg Anesth Pain Med (2014) 39:200–7. doi: 10.1097/aap.0000000000000079
22. Shin S, Kim HI, Kim NY, Lee KY, Kim DW, Yoo YC. Effect of Postoperative Analgesia Technique on the Prognosis of Gastric Cancer: A Retrospective Analysis. Oncotarget (2017) 8:104594–604. doi: 10.18632/oncotarget.21979
23. Wang J, Guo W, Wu Q, Zhang R, Fang J. Impact of Combination Epidural and General Anesthesia on the Long-Term Survival of Gastric Cancer Patients: A Retrospective Study. Med Sci Monit (2016) 22:2379–85. doi: 10.12659/msm.899543
24. Pei JP, Zhang CD, Liang Y, Zhang C, Wu KZ, Zhao ZM, et al. Effects of Epidural Combined With General Anesthesia Versus General Anesthesia Alone in Gastric Cancer Surgery: A Propensity Score Matching Analysis. Ann Transl Med (2020) 8:473. doi: 10.21037/atm.2020.03.127
25. Cummings Iii KC, Kou TD, Chak A, Schluchter MD, Margevicius S, Cooper GS, et al. Surgical Approach and the Impact of Epidural Analgesia on Survival After Esophagectomy for Cancer: A Population-Based Retrospective Cohort Study. PloS One (2019) 14:e0211125. doi: 10.1371/journal.pone.0211125
26. Heinrich S, Janitz K, Merkel S, Klein P, Schmidt J. 4-10 Short- and Long Term Effects of Epidural Analgesia on Morbidity and Mortality of Esophageal Cancer Surgery. Langenbecks Arch Surg (2015) 400:19–26. doi: 10.1007/s00423-014-1248-9
27. Li W, Li Y, Huang Q, Ye S, Rong T. Short and Long-Term Outcomes of Epidural or Intravenous Analgesia After Esophagectomy: A Propensity-Matched Cohort Study. PloS One (2016) 11:e0154380. doi: 10.1371/journal.pone.0154380
28. Hiller JG, Hacking MB, Link EK, Wessels KL, Riedel BJ. Perioperative Epidural Analgesia Reduces Cancer Recurrence After Gastro-Oesophageal Surgery. Acta Anaesthesiol Scand (2014) 58:281–90. doi: 10.1111/aas.12255
29. Xu ZZ, Li HJ, Li MH, Huang SM, Li X, Liu QH, et al. Epidural Anesthesia-Analgesia and Recurrence-Free Survival After Lung Cancer Surgery: A Randomized Trial. Anesthesiol (2021) 135:419–32. doi: 10.1097/aln.0000000000003873
30. Wu HL, Tai YH, Chan MY, Tsou MY, Chen HH, Chang KY. Effects of Epidural Analgesia on Cancer Recurrence and Long-Term Mortality in Patients After Non-Small-Cell Lung Cancer Resection: A Propensity Score-Matched Study. BMJ Open (2019) 9:e027618. doi: 10.1136/bmjopen-2018-027618
31. de Oliveira GS Jr, Ahmad S, Schink JC, Singh DK, Fitzgerald PC, McCarthy RJ. Intraoperative Neuraxial Anesthesia But Not Postoperative Neuraxial Analgesia Is Associated With Increased Relapse-Free Survival in Ovarian Cancer Patients After Primary Cytoreductive Surgery. Reg Anesth Pain Med (2011) 36:271–7. doi: 10.1097/AAP.0b013e318217aada
32. Elias KM, Kang S, Liu X, Horowitz NS, Berkowitz RS, Frendl G. Anesthetic Selection and Disease-Free Survival Following Optimal Primary Cytoreductive Surgery for Stage III Epithelial Ovarian Cancer. Ann Surg Oncol (2015) 22:1341–8. doi: 10.1245/s10434-014-4112-9
33. Tseng JH, Cowan RA, Afonso AM, Zhou Q, Iasonos A, Ali N, et al. 4-59 Perioperative Epidural Use and Survival Outcomes in Patients Undergoing Primary Debulking Surgery for Advanced Ovarian Cancer. Gynecol Oncol (2018) 151:287–93. doi: 10.1016/j.ygyno.2018.08.024
34. Lacassie HJ, Cartagena J, Brañes J, Assel M, Echevarría GC. The Relationship Between Neuraxial Anesthesia and Advanced Ovarian Cancer-Related Outcomes in the Chilean Population. Anesth Analg (2013) 117:653–60. doi: 10.1213/ANE.0b013e3182a07046
35. Capmas P, Billard V, Gouy S, Lhommé C, Pautier P, Morice P, et al. Impact of Epidural Analgesia on Survival in Patients Undergoing Complete Cytoreductive Surgery for Ovarian Cancer. Anticancer Res (2012) 32:1537–42.
36. Wuethrich PY, Hsu Schmitz SF, Kessler TM, Thalmann GN, Studer UE, Stueber F, et al. Potential Influence of the Anesthetic Technique Used During Open Radical Prostatectomy on Prostate Cancer-Related Outcome: A Retrospective Study. Anesthesiol (2010) 113:570–6. doi: 10.1097/ALN.0b013e3181e4f6ec
37. Wuethrich PY, Thalmann GN, Studer UE, Burkhard FC. Epidural Analgesia During Open Radical Prostatectomy Does Not Improve Long-Term Cancer-Related Outcome: A Retrospective Study in Patients With Advanced Prostate Cancer. PloS One (2013) 8:e72873. doi: 10.1371/journal.pone.0072873
38. Forget P, Tombal B, Scholtès JL, Nzimbala J, Meulders C, Legrand C, et al. Do Intraoperative Analgesics Influence Oncological Outcomes After Radical Prostatectomy for Prostate Cancer? Eur J Anaesthesiol (2011) 28:830–5. doi: 10.1097/EJA.0b013e32834b7d9a
39. Tsui BC, Rashiq S, Schopflocher D, Murtha A, Broemling S, Pillay J, et al. Epidural Anesthesia and Cancer Recurrence Rates After Radical Prostatectomy. Can J Anaesth (2010) 57:107–12. doi: 10.1007/s12630-009-9214-7
40. Biki B, Mascha E, Moriarty DC, Fitzpatrick JM, Sessler DI, Buggy DJ. Anesthetic Technique for Radical Prostatectomy Surgery Affects Cancer Recurrence: A Retrospective Analysis. Anesthesiol (2008) 109:180–7. doi: 10.1097/ALN.0b013e31817f5b73
41. Chipollini J, Alford B, Boulware DC, Forget P, Gilbert SM, Lockhart JL, et al. Epidural Anesthesia and Cancer Outcomes in Bladder Cancer Patients: Is it the Technique or the Medication? A Matched-Cohort Analysis From a Tertiary Referral Center. BMC Anesthesiol (2018) 18:157. doi: 10.1186/s12871-018-0622-5
42. Christopher Doiron R, Jaeger M, Booth CM, Wei X, Robert Siemens D. Is There a Measurable Association of Epidural Use at Cystectomy and Postoperative Outcomes? A Population-Based Study. Can Urol Assoc J (2016) 10:321–7. doi: 10.5489/cuaj.3856
43. Chang WK, Lee MY, Tai YH, Kuo YM, Tsou MY, Chang KY. Does Epidural Analgesia Improve the Cancer Outcome in Hepatocellular Carcinoma After Resection Surgery? A Retrospective Analysis. J Chin Med Assoc (2019) 82:295–9. doi: 10.1097/jcma.0000000000000054
44. Cao L, Chang Y, Lin W, Zhou J, Tan H, Yuan Y, et al. Long-Term Survival After Resection of Hepatocelluar Carcinoma: A Potential Risk Associated With the Choice of Postoperative Analgesia. Anesth Analg (2014) 118:1309–16. doi: 10.1213/ane.0000000000000207
45. Gao H, Meng XY, Wang HQ, Zhu FF, Guo AL, Zhu M, et al. Association Between Anaesthetic Technique and Oncological Outcomes After Colorectal Carcinoma Liver Metastasis Resection. Int J Med Sci (2019) 16:337–42. doi: 10.7150/ijms.28016
46. Zimmitti G, Soliz J, Aloia TA, Gottumukkala V, Cata JP, Tzeng CW, et al. Positive Impact of Epidural Analgesia on Oncologic Outcomes in Patients Undergoing Resection of Colorectal Liver Metastases. Ann Surg Oncol (2016) 23:1003–11. doi: 10.1245/s10434-015-4933-1
47. Call TR, Pace NL, Thorup DB, Maxfield D, Chortkoff B, Christensen J, et al. 16-53 Factors Associated With Improved Survival After Resection of Pancreatic Adenocarcinoma: A Multivariable Model. Anesthesiol (2015) 122:317–24. doi: 10.1097/aln.0000000000000489
48. Alexander A, Lehwald-Tywuschik N, Rehders A, Rabenalt S, Verde PE, Eisenberger CF, et al. Peridural Anesthesia and Cancer-Related Survival After Surgery for Pancreatic Cancer-A Retrospective Cohort Study. Clin Pract (2021) 11:532–42. doi: 10.3390/clinpract11030070
49. Aguirre-Ghiso JA. 18-1 Models, Mechanisms and Clinical Evidence for Cancer Dormancy. Nat Rev Cancer (2007) 7:834–46. doi: 10.1038/nrc2256
50. Bartal I, Melamed R, Greenfeld K, Atzil S, Glasner A, Domankevich V, et al. 21 B 2010 Immune Perturbations in Patients Along the Perioperative Period: Alterations in Cell Surface Markers and Leukocyte Subtypes Before and After Surgery. Brain Behav Immun (2010) 24:376–86. doi: 10.1016/j.bbi.2009.02.010
51. Benish M, Bartal I, Goldfarb Y, Levi B, Avraham R, Raz A, et al. 21 B 2008 Perioperative Use of Beta-Blockers and COX-2 Inhibitors may Improve Immune Competence and Reduce the Risk of Tumor Metastasis. Ann Surg Oncol (2008) 15:2042–52. doi: 10.1245/s10434-008-9890-5
52. Goldfarb Y, Benish M, Rosenne E, Melamed R, Levi B, Glasner A, et al. 21gold 2009 CpG-C Oligodeoxynucleotides Limit the Deleterious Effects of Beta-Adrenoceptor Stimulation on NK Cytotoxicity and Metastatic Dissemination. J Immunother (2009) 32:280–91. doi: 10.1097/CJI.0b013e31819a2982
53. Greenfeld K, Avraham R, Benish M, Goldfarb Y, Rosenne E, Shapira Y, et al. 21 GREEN 2007 Immune Suppression While Awaiting Surgery and Following it: Dissociations Between Plasma Cytokine Levels, Their Induced Production, and NK Cell Cytotoxicity. Brain Behav Immun (2007) 21:503–13. doi: 10.1016/j.bbi.2006.12.006
54. Neeman E, Ben-Eliyahu S. 19 N B 2013 Surgery and Stress Promote Cancer Metastasis: New Outlooks on Perioperative Mediating Mechanisms and Immune Involvement. Brain Behav Immun (2013) 30 Suppl:S32–40. doi: 10.1016/j.bbi.2012.03.006
55. Shahzad MMK, Arevalo JM, Armaiz-Pena GN, Lu C, Stone RL, Moreno-Smith M, et al. 21shah 2018 Stress Effects on FosB and Interleukin-8 (IL8)-Driven Ovarian Cancer Growth and Metastasis. J Biol Chem (2018) 293:10041. doi: 10.1074/jbc.AAC118.004299
56. Pascual M, Alonso S, Parés D, Courtier R, Gil MJ, Grande L, et al. 21 PASCU 2011 Randomized Clinical Trial Comparing Inflammatory and Angiogenic Response After Open Versus Laparoscopic Curative Resection for Colonic Cancer. Br J Surg (2011) 98:50–9. doi: 10.1002/bjs.7258
57. Yücel Y, Barlan M, Lenhardt R, Kurz A, Sessler DI. 21 YUC 2005 Perioperative Hypothermia Does Not Enhance the Risk of Cancer Dissemination. Am J Surg (2005) 189:651–5. doi: 10.1016/j.amjsurg.2005.03.002
58. Hong JY, Lim KT. Effect of Preemptive Epidural Analgesia on Cytokine Response and Postoperative Pain in Laparoscopic Radical Hysterectomy for Cervical Cancer. Reg Anesth Pain Med (2008) 33:44–51. doi: 10.1016/j.rapm.2007.07.010
59. Ben-Eliyahu S. The Promotion of Tumor Metastasis by Surgery and Stress: Immunological Basis and Implications for Psychoneuroimmunology. Brain Behav Immun (2003) 17(Suppl 1):S27–36. doi: 10.1016/s0889-1591(02)00063-6
60. Melamed R, Rosenne E, Shakhar K, Schwartz Y, Abudarham N, Ben-Eliyahu S. Marginating Pulmonary-NK Activity and Resistance to Experimental Tumor Metastasis: Suppression by Surgery and the Prophylactic Use of a Beta-Adrenergic Antagonist and a Prostaglandin Synthesis Inhibitor. Brain Behav Immun (2005) 19:114–26. doi: 10.1016/j.bbi.2004.07.004
61. Deegan CA, Murray D, Doran P, Moriarty DC, Sessler DI, Mascha E, et al. Anesthetic Technique and the Cytokine and Matrix Metalloproteinase Response to Primary Breast Cancer Surgery. Reg Anesth Pain Med (2010) 35:26–31490–5. doi: 10.1097/AAP.0b013e3181ef4d05
62. Li MH, Xu ZZ, Huang SM, Li T, Li XY, Wang DX. 26-47 Effect of Combined Epidural Anaesthesia on Tumor-Infiltrating Lymphocytes in Lung Adenocarcinoma: A Prospective Exploratory Sub-Analysis. Hepatogastroenterology (2018) 61:1142–7. doi: 10.1111/aas.13068
63. Liu K, Liming T, Wang J, Yang HH, Ren J. Effect of Combined General/Epidural Anesthesia on Postoperative NK Cell Activity and Cytokine Response in Gastric Cancer Patients Undergoing Radical Resection. Randomized Controlled Trial (2014) 61:1142–7.
64. Zhu J, Zhang XR, Yang HJM. Effects of Combined Epidural and General Anesthesia on Intraoperative Hemodynamic Responses, Postoperative Cellular Immunity, and Prognosis in Patients With Gallbladder Cancer: A Randomized Controlled Trial. Med (Baltimore) (2017) 96:e6137. doi: 10.1097/MD.0000000000006137
65. Xu YJ, Chen WK, Zhu Y, Wang SL, Miao CH. 26-48 Effect of Thoracic EpiduralAnaesthesia on Serum Vascular Endothelial Growth Factor C and Cytokinesin Patients Undergoing Anaesthesia and Surgery for Colon Cancer. Br J Anaesth (2014) 113(Suppl 1):149–55. doi: 10.1093/bja/aeu148
66. Boland JW, Pockley AG. Influence of Opioids on Immune Function in Patients With Cancer Pain: From Bench to Bedside. Br J Pharmacol (2018) 175:2726–36. doi: 10.1111/bph.13903
67. Gach K, Wyrębska A, Fichna J, Janecka A. The Role of Morphine in Regulation of Cancer Cell Growth. Naunyn Schmiedebergs Arch Pharmacol (2011) 384:221–30. doi: 10.1007/s00210-011-0672-4
69. Mei G, Jie S, Jin W, Qian YJI. Morphine, But Not Ketamine, Decreases the Ratio of Th1/Th2 in CD4-Positive Cells Through T-Bet and GATA3. Inflammation (2012) 35:1069–77. doi: 10.1007/s10753-011-9413-6
70. Sacerdote P, Bianchi M, Gaspani L, Manfredi B, Maucione A, Terno G, et al. The Effects of Tramadol and Morphine on Immune Responses and Pain After Surgery in Cancer Patients. Anesth Analg (2000) 90:1411–4. doi: 10.1097/00000539-200006000-00028
71. Sacerdote P, Gaspani L, Rossoni G, Panerai AE, Bianchi MJII. Effect of the Opioid Remifentanil on Cellular Immune Response in the Rat. Int Immunopharmacol (2001) 1:713–9. doi: 10.1016/S1567-5769(01)00005-4
72. Gong L, Qin Q, Lei Z, Ouyang W, Li YJ. Effects of Fentanyl Anesthesia and Sufentanil Anesthesia on Regulatory T Cells Frequencies. Int J Clin Exp Pathol (2014) 7:7708–16.
73. Hofbauer R, Moser D, Salfinger H, Frass M, Kapiotis S. 14-57 Sufentanil Inhibits Migration of Human Leukocytes Through Human Endothelial Cell Monolayers. Anesth Analg (1998) 87:1181–5. doi: 10.1097/00000539-199811000-00038
74. Shavit Y, Ben-Eliyahu S, Zeidel A, Beilin B. 14-55 Effects of Fentanyl on Natural Killer Cell Activity and on Resistance to Tumor Metastasis in Rats. Dose and Timing Study. Neuroimmunomodulation (2004) 11:255–60. doi: 10.1159/000078444
75. Ecimovic P, McHugh B, Murray D, Doran P, Buggy DJ. Effects of Sevoflurane on Breast Cancer Cell Function. Vitro Anticancer Res (2013) 33:4255–60.
76. Fan L, Wu Y, Wang J, He J, Han X. Sevoflurane Inhibits the Migration and Invasion of Colorectal Cancer Cells Through Regulating ERK/MMP-9 Pathway by Up-Regulating miR-203. Eur J Pharmacol (2019) 850:43–52. doi: 10.1016/j.ejphar.2019.01.025
77. Jun IJ, Jo JY, Kim JI, Chin JH, Kim WJ, Kim HR, et al. Impact of Anesthetic Agents on Overall and Recurrence-Free Survival in Patients Undergoing Esophageal Cancer Surgery: A Retrospective Observational Study. Sci Rep (2017) 7:14020. doi: 10.1038/s41598-017-14147-9
78. Jun R, Gui-he Z, Xing-xing S, Hui Z, Li-xian X. Isoflurane Enhances Malignancy of Head and Neck Squamous Cell Carcinoma Cell Lines: A Preliminary Study. Vitro Oral Oncol (2011) 47:329–33. doi: 10.1016/j.oraloncology.2011.03.002
79. Guay J, Kopp S. Epidural Pain Relief Versus Systemic Opioid-Based Pain Relief for Abdominal Aortic Surgery. Cochrane Database Syst Rev (2016) 1:CD005059. doi: 10.1002/14651858.CD005059.pub4
80. Wu CL, Cohen SR, Richman JM, Rowlingson AJ, Courpas GE, Cheung K, et al. Efficacy of Postoperative Patient-Controlled and Continuous Infusion Epidural Analgesia Versus Intravenous Patient-Controlled Analgesia With Opioids: A Meta-Analysis. (2005) 103:1079–88. doi: 10.1097/00000542-200511000-00023
81. Gao J, Hu H, Wang XJ. Clinically Relevant Concentrations of Lidocaine Inhibit Tumor Angiogenesis Through Suppressing VEGF/VEGFR2 Signaling. C.C.Pharmacol (2019) 83:1–31. doi: 10.1007/s00280-019-03815-4
82. Yang J, Li G, Bao K, Liu W, Zhang Y, Ting W, et al. 1-32 Ropivacaine Inhibits Tumor Angiogenesis via Sodium-Channel-Independent Mitochondrial Dysfunction and Oxidative Stress. J Bioenerg Biomembr (2019) 51:231–8. doi: 10.1007/s10863-019-09793-9
83. Sun H, Sun Y. Lidocaine Inhibits Proliferation and Metastasis of Lung Cancer Cell via Regulation of miR-539/EGFR Axis. Artif Cells Nanomed Biotechnol (2019) 47:2866–74. doi: 10.1080/21691401.2019.1636807
84. Zhao L, Han S, Hou J, Shi W, Zhao Y, Chen Y. The Local Anesthetic Ropivacaine Suppresses Progression of Breast Cancer by Regulating miR-27b-3p/YAP Axis. Aging (Albany NY) (2021) 13:16341–52. doi: 10.18632/aging.203160
85. Liu H, Dilger JP, Lin J. 11 Effects of Local Anesthetics on Cancer Cells. Pharmacol Ther (2020) 212:107558. doi: 10.1016/j.pharmthera.2020.107558
86. Baptista-Hon DT, Robertson FM, Robertson GB, Owen SJ, Rogers GW, Lydon EL, et al. 11 BAP 2014 Potent Inhibition by Ropivacaine of Metastatic Colon Cancer SW620 Cell Invasion and NaV1.5 Channel Function. Br J Anaesth (2014) 113 Suppl 1:i39–48. doi: 10.1093/bja/aeu104
87. Brisson L, Driffort V, Benoist L, Poet M, Counillon L, Antelmi E, et al. 1-29 NaV1.5 Na⁺ Channels Allosterically Regulate the NHE-1 Exchanger and Promote the Activity of Breast Cancer Cell Invadopodia. J Cell Sci (2013) 126:4835–42. doi: 10.1242/jcs.123901
88. Djamgoz MBA, Fraser SP, Brackenbury WJ. 11 DJA 2019 In Vivo Evidence for Voltage-Gated Sodium Channel Expression in Carcinomas and Potentiation of Metastasis. Cancers (Basel) (2019) 11:1675. doi: 10.3390/cancers11111675
89. Jiang Y, Gou H, Zhu J, Tian S, Yu L. 11 JIANG 2016 Lidocaine Inhibits the Invasion and Migration of TRPV6-Expressing Cancer Cells by TRPV6 Downregulation. Oncol Lett (2016) 12:1164–70. doi: 10.3892/ol.2016.4709
90. Piegeler T, Schläpfer M, Dull RO, Schwartz DE, Borgeat A, Minshall RD, et al. 1-34 Clinically Relevant Concentrations of Lidocaine and Ropivacaine Inhibit Tnfα-Induced Invasion of Lung Adenocarcinoma Cells In Vitro by Blocking the Activation of Akt and Focal Adhesion Kinase. Br J Anaesth (2015) 115:784–91. doi: 10.1093/bja/aev341
91. Tohme S, Simmons RL, Tsung AJCR. 11 TOH 2017 Surgery for Cancer: A Trigger for Metastases. Cancer Res (2017) 77:1548. doi: 10.1158/0008-5472.CAN-16-1536
92. Lang A, Horin SB, Picard O, Fudim E, Amariglio N, Chowers YJI. 11 LAN 2010 Lidocaine Inhibits Epithelial Chemokine Secretion via Inhibition of Nuclear Factor Kappa B Activation. Immunobiology (2010) 215:304–13. doi: 10.1016/j.imbio.2009.05.006
93. Ni J, Xie T, Xiao M, Wei X, Wang LJB, Communications BR. Amide-Linked Local Anesthetics Preferentially Target Leukemia Stem Cell Through Inhibition of Wnt/β-Catenin. Biochem Biophys Res Commun (2018) 503:956–62. doi: 10.1016/j.bbrc.2018.06.102
94. Carli F, Mayo N, Klubien K, Schricker T, Trudel J, Belliveau P. Epidural Analgesia Enhances Functional Exercise Capacity and Health-Related Quality of Life After Colonic Surgery: Results of a Randomized Trial. Anesthesiol (2002) 97:540–9. doi: 10.1097/00000542-200209000-00005
95. Feltracco P, Bortolato A, Barbieri S, Michieletto E, Serra E, Ruol A, et al. Perioperative Benefit and Outcome of Thoracic Epidural in Esophageal Surgery: A Clinical Review. Dis Esophagus (2018) 31:1–14. doi: 10.1093/dote/dox135
96. Du YT, Li YW, Zhao BJ, Guo XY, Feng Y, Zuo MZ, et al. Long-Term Survival After Combined Epidural-General Anesthesia or General Anesthesia Alone: Follow-Up of a Randomized Trial. Anesthesiol (2021) 135:233–45. doi: 10.1097/aln.0000000000003835
97. Binczak M, Tournay E, Billard V, Rey A, Jayr C. Major Abdominal Surgery for Cancer: Does Epidural Analgesia Have a Long-Term Effect on Recurrence-Free and Overall Survival? Ann Fr Anesth Reanim (2013) 32:e81–88. doi: 10.1016/j.annfar.2013.02.027
98. Myles PS, Peyton P, Silbert B, Hunt J, Rigg JR, Sessler DI. 4-28 Perioperative Epidural Analgesia for Major Abdominal Surgery for Cancer and Recurrence-Free Survival: Randomised Trial. BMJ (2011) 342:d1491. doi: 10.1136/bmj.d1491
99. Kikuchi S, Kuroda S, Nishizaki M, Matsusaki T, Kuwada K, Kimura Y, et al. Comparison of the Effects of Epidural Analgesia and Patient-Controlled Intravenous Analgesia on Postoperative Pain Relief and Recovery After Laparoscopic Gastrectomy for Gastric Cancer. Surg Laparosc Endosc Percutan Tech (2019) 29:405–8. doi: 10.1097/sle.0000000000000605
100. Pesco J, Young K, Nealon K, Fluck M, Shabahang M, Blansfield J. Use and Outcomes of Epidural Analgesia in Upper Gastrointestinal Tract Cancer Resections. J Surg Res (2021) 257:433–41. doi: 10.1016/j.jss.2020.08.018
101. Kishikawa H, Suzuki N, Suzuki Y, Hamasaki T, Kondo Y, Sakamoto A. Effect of Robot-Assisted Surgery on Anesthetic and Perioperative Management for Minimally Invasive Radical Prostatectomy Under Combined General and Epidural Anesthesia. J Nippon Med Sch (2021) 88:121–7. doi: 10.1272/jnms.JNMS.2021_88-304
102. Seo HJ, Lee NR, Son SK, Kim DK, Rha KH, Lee SH. Comparison of Robot-Assisted Radical Prostatectomy and Open Radical Prostatectomy Outcomes: A Systematic Review and Meta-Analysis. Yonsei Med J (2016) 57:1165–77. doi: 10.3349/ymj.2016.57.5.1165
103. Oh YJ, Lee JR, Choi YS, Koh SO, Na S. Randomized Controlled Comparison of Combined General and Epidural Anesthesia Versus General Anesthesia on Diaphragmatic Function After Laparoscopic Prostatectomy. Minerva Anestesiol (2013) 79:1371–80.
104. Hong JY, Lee SJ, Rha KH, Roh GU, Kwon SY, Kil HK. Effects of Thoracic Epidural Analgesia Combined With General Anesthesia on Intraoperative Ventilation/Oxygenation and Postoperative Pulmonary Complications in Robot-Assisted Laparoscopic Radical Prostatectomy. J Endourol (2009) 23:1843–9. doi: 10.1089/end.2009.0059
105. Rahman SN, Cao DJ, Flores VX, Monaghan TF, Weiss JP, McNeil BK, et al. Impact of Neuraxial Analgesia on Outcomes Following Radical Cystectomy: A Systematic Review. Urol Oncol (2021) 39:100–8. doi: 10.1016/j.urolonc.2020.10.073
106. Simpson RE, Fennerty ML, Colgate CL, Kilbane EM, Ceppa EP, House MG, et al. Post-Pancreaticoduodenectomy Outcomes and Epidural Analgesia: A 5-Year Single-Institution Experience. J Am Coll Surg (2019) 228:453–62. doi: 10.1016/j.jamcollsurg.2018.12.038
107. Axelrod TM, Mendez BM, Abood GJ, Sinacore JM, Aranha GV, Shoup M. Peri-Operative Epidural may Not be the Preferred Form of Analgesia in Select Patients Undergoing Pancreaticoduodenectomy. J Surg Oncol (2015) 111:306–10. doi: 10.1002/jso.23815
Keywords: epidural analgesia, cancer recurrence, cancer survival, cancer surgeries, oncological outcomes
Citation: Zhang D, Jiang J, Liu J, Zhu T, Huang H and Zhou C (2022) Effects of Perioperative Epidural Analgesia on Cancer Recurrence and Survival. Front. Oncol. 11:798435. doi: 10.3389/fonc.2021.798435
Received: 20 October 2021; Accepted: 10 December 2021;
Published: 05 January 2022.
Edited by:
Oliver Kepp, INSERM U1138 Centre de Recherche des Cordeliers (CRC), FranceReviewed by:
Juan Chipollini, University of Arizona, United StatesZhi-Fu Wu, Kaohsiung Medical University, Taiwan
Copyright © 2022 Zhang, Jiang, Liu, Zhu, Huang and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Cheng Zhou, emhvdWNAMTYzLmNvbQ==; Han Huang, aGFuLmh1YW5nQHNjdS5lZHUuY24=
†These authors have contributed equally to this work
 Donghang Zhang
Donghang Zhang Jingyao Jiang
Jingyao Jiang Jin Liu
Jin Liu Tao Zhu
Tao Zhu Han Huang3*
Han Huang3* Cheng Zhou
Cheng Zhou