- 1Radiation Oncology, Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS) Azienda Ospedaliero-Universitaria di Bologna, Bologna, Italy
- 2Department of Experimental, Diagnostic and Specialty Medicine—Alma Mater Studiorum Bologna University, Bologna, Italy
- 3Università Cattolica del Sacro Cuore, Dipartimento Universitario Diagnostica per immagini, Radioterapia Oncologica ed Ematologia, Roma, Italy
- 4Fondazione Policlinico Universitario “A. Gemelli” Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS), Dipartimento di Diagnostica per Immagini, Radioterapia Oncologica ed Ematologia, Roma, Italy
- 5Radiotherapy Unit, Gemelli Molise Hospital, Catholic University of Sacred Heart, Campobasso, Italy
- 6Medical Physic Unit, Gemelli Molise Hospital, Catholic University of Sacred Heart, Campobasso, Italy
- 7Medical Physics Unit, Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS) Azienda Ospedaliero-Universitaria di Bologna, Bologna, Italy
- 8Service of Radiology, Imaging Institute of Southern Switzerland, Ente Ospedaliero Cantonale (EOC), Lugano, Switzerland
Aim: The efficacy of low-dose fractionated radiotherapy (LDFRT) and chemotherapy (CHT) combination has large preclinical but little clinical evidence. Therefore, the aim of this review was to collect and analyze the clinical results of LDRT plus concurrent CHT in patients with advanced cancers.
Methods: A systematic literature search was conducted on PubMed using the PRISMA methodology. Only studies based on the combination of LDFRT (< 1 Gy/fraction) and CHT were included. Endpoints of the analysis were tumor response, toxicity, and overall survival, with particular focus on any differences between LDFRT-CHT and CHT alone.
Results: Twelve studies (307 patients) fulfilled the selection criteria and were included in this review. Two studies were retrospective, one was a prospective pilot trial, six were phase II studies, two were phase I trials, and one was a phase I/II open label study. No randomized controlled trials were found. Seven out of eight studies comparing clinical response showed higher rates after LDFRT-CHT compared to CHT alone. Three out of four studies comparing survival reported improved results after combined treatment. Three studies compared toxicity of CHT and LDFRT plus CHT, and all of them reported similar adverse events rates. In most cases, toxicity was manageable with only three likely LDFRT-unrelated fatal events (1%), all recorded in the same series on LDFRT plus temozolomide in glioblastoma multiforme patients.
Conclusion: None of the analyzed studies provided level I evidence on the clinical impact of LDFRT plus CHT. However, it should be noted that, apart from two small series of breast cancers, all studies reported improved therapeutic outcomes and similar tolerability compared to CHT alone.
Systematic Review Registration: www.crd.york.ac.uk/prospero/, identifier CRD42020206639.
Introduction
Conventionally fractionated curative radiotherapy (RT) is delivered in 1.8–2.0 Gy daily fractions. Conversely, low-dose fractionated RT (LDFRT) is defined as the use of very small dose per fraction (< 1.0 Gy). In some experimental models, LDFRT resulted more effective than predicted by the linear quadratic model in terms of improved cell kill (1, 2). In particular, in vitro experiments showed this phenomenon in several cell lines (3–5). Interestingly, the higher efficacy of LDFRT was confirmed in human cells by several laboratories using different assay techniques, conditions of cell growth, handling, and irradiation (1). On the contrary, a relative tumor cell radiation resistance was recorded when higher doses per fraction were used (6). The low-dose hyper-radiation sensitivity (HRS) phenomenon has been interpreted on the basis of a threshold effect in radiation-induced damage repair. In fact, DNA-repair mechanisms are triggered only above certain dose levels, while lower doses are ineffective in arresting irradiated cells in the G2 cell-cycle phase (7, 8).
The peculiar efficacy of LDFRT has been interpreted also on the basis of immunological mechanisms. For example, Klug and colleagues (9) reported that local LDFRT produces efficient recruitment of tumor-specific T cells in human pancreatic carcinomas with T-cell-mediated tumor rejection and prolonged survival in otherwise immune refractory spontaneous and xenotransplant mouse tumor models. The authors used one single fraction with doses ranging between 0.5 and 6.0 Gy. They observed that the number of intratumoral T lymphocytes was higher after irradiation with the lowest dose (0.5 Gy) (9). Based on this preclinical evidence, LDFRT was tested also in a clinical study (10).
Concurrent chemoradiation is a standard treatment option in several tumors since CHT is able to act as a radiosensitizer. Interestingly, when delivered as LDFRT, also RT may act as a chemosensitizer. This peculiar synergistic effect of LDFRT and CHT was demonstrated by several preclinical studies, in different cell lines, and using different drugs such as cisplatin, carboplatin, docetaxel, and paclitaxel (11–15). It is worth noting that LDFRT-induced toxicity is significantly lower compared to conventional fractionation or hypofractionation. This higher tolerability allows LDFRT to be associated with “full-dose” CHT, with a clear benefit in terms not only of local response but also of systemic tumor control (16).
Considering these aspects, interest in the combination of LDFRT with CHT in the clinical management of cancer patients grew. LDFRT was proposed as a new systemic agent labeled with an “r” (e.g., gemcitabine plus LDFRT: rG) (17). Although some preliminary studies suggested the effectiveness of this combination (16, 17), randomized trials, meta-analyses, and systematic reviews on this topic are lacking. Therefore, the aim of this review was to collect and analyze the results of LDFRT plus CHT, currently available in literature, in terms of tumor response, clinical outcomes, and treatment tolerability.
Methods And Materials
Our systematic review protocol was registered (registration number: CRD42020206639) within the International Prospective Register of Systematic Reviews (PROSPERO, www.crd.york.ac.uk/prospero/) on 31 August 2020.
Inclusion Criteria
Human studies of any design, without limitations in terms of the number of enrolled patients, and based on LDFRT plus CHT combination, were included. Studies based on LDFRT without concurrent CHT were excluded. No restriction about total delivered dose, biological effective dose (BED), and RT technique was imposed.
Outcome Measures
We reported the main findings of the analyzed papers with particular focus on clinical tumor response, overall survival, and treatment-related toxicity. Moreover, any differences between LDFRT-CHT and CHT alone were recorded and reported.
Bibliographic Search
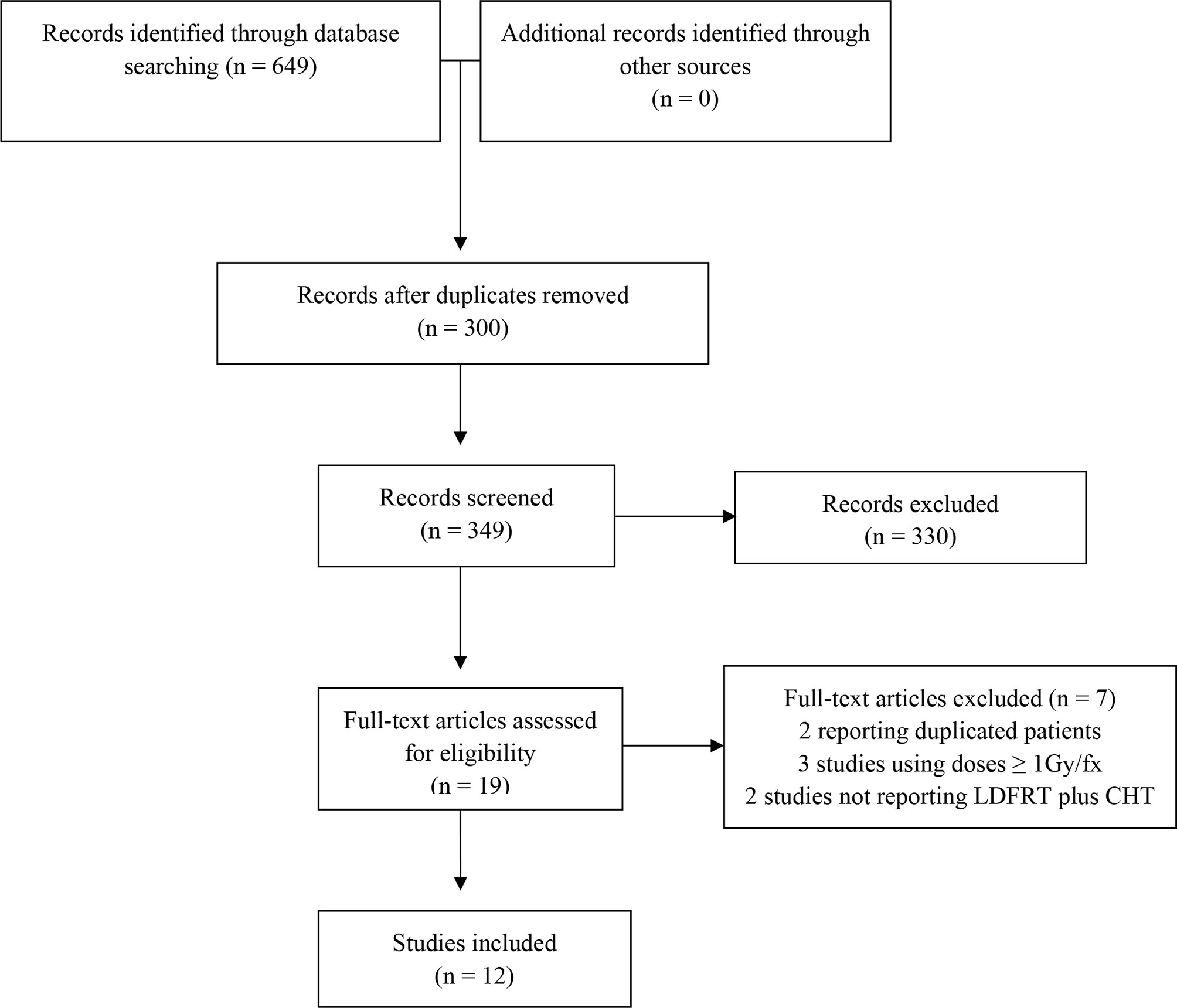
We conducted a search based on PubMed from the earliest date to 20 May 2020. In our review, we considered only studies published in the English language. We used various combinations of the subsequent terms in PubMed such as low-dose, radiotherapy, ultra-fractionation, hyper-radiation-sensitivity, chemosensitization, concurrent, and chemotherapy. Finally, the following two search strategies were used in PubMed: i) low-dose[All Fields] AND (“radiotherapy”[Subheading] OR “radiotherapy”[All Fields] OR “radiotherapy”[MeSH Terms]) AND concurrent[All Fields] AND (“drug therapy”[Subheading] OR (“drug”[All Fields] AND “therapy”[All Fields]) OR “drug therapy”[All Fields] OR “chemotherapy”[All Fields] OR “drug therapy”[MeSH Terms] OR (“drug”[All Fields] AND “therapy”[All Fields]) OR “chemotherapy”[All Fields]); and ii) “hyper radiation sensitivity” OR ((“ultrafractionation” OR “ultrafractionated”) AND (“radiotherapy” OR “irradiation” OR “radiation”)) OR (“chemosensitization” AND (“radiotherapy” OR “irradiation” OR “radiation”)). We found 396 studies with the first strategy and 253 with the second one. We removed duplicates, and we made the first selection based on titles and abstracts. Moreover, a further search through the references of the selected studies was performed. After reading the full-text articles, six studies were excluded: three used the term “ultrafractionation” or “low-dose RT,” but the delivered dose/fraction was ≥ 1 Gy; two studies did not use LDFRT plus CHT combination, and one study reported duplicated patients. Finally, 12 articles fulfilled our criteria (16–27).
Study Selection and Quality Assessment
We used the PRISMA guidelines as a guide to select the items to be included within the review (28, 29). Title, abstract, and keywords of the identified articles were independently analyzed by two researchers (ES, AZ), and disagreements were solved by the senior author (AM). Potentially eligible studies were retrieved, and full-text evaluation was performed based on the inclusion and exclusion criteria by two different authors (ES, AZ) with disagreements resolved by consensus-based discussion. Subsequently, the following data were collected independently by two authors (ES, MB) from each article, with disagreements resolved by the senior author (AM): authors’ name and year of publication, study design, accrual period, patients and setting, treatment (LDFRT and CHT), and main outcomes. Papers were evaluated based on the ROBINS-I Risk of Bias tool (30). Two reviewers (ES, AZ) assessed the quality of the included studies, and discrepancies were resolved on agreement.
Results
Search Results
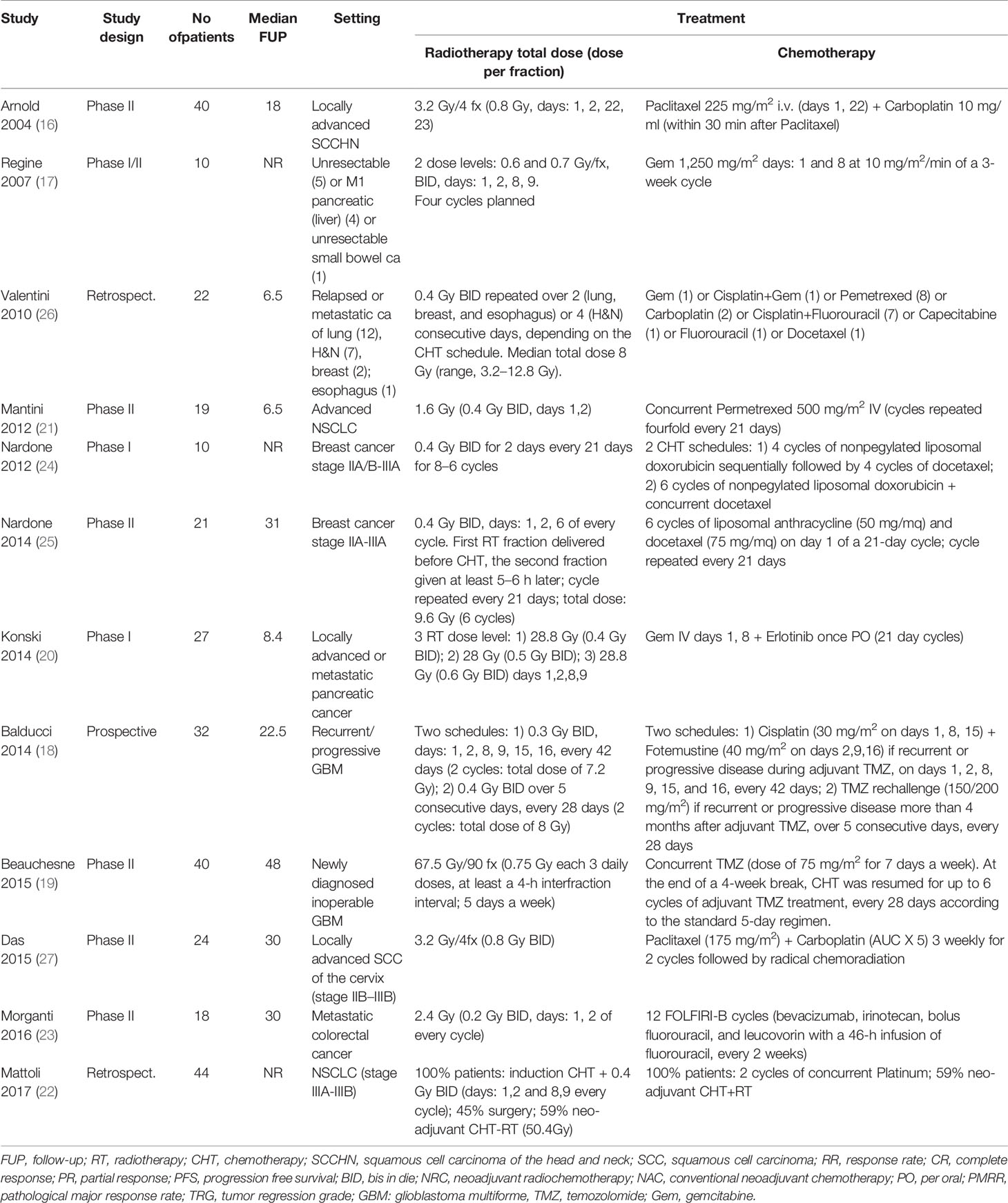
Twelve articles (16–27) including 307 patients fulfilled the inclusion criteria for this review. Accrual period of all the studies ranged from 2000 to 2014. Details on the analyzed studies are reported in Table 1, while the flowchart of the literature search process is shown in Figure 1.
Study Design and Risk of Bias
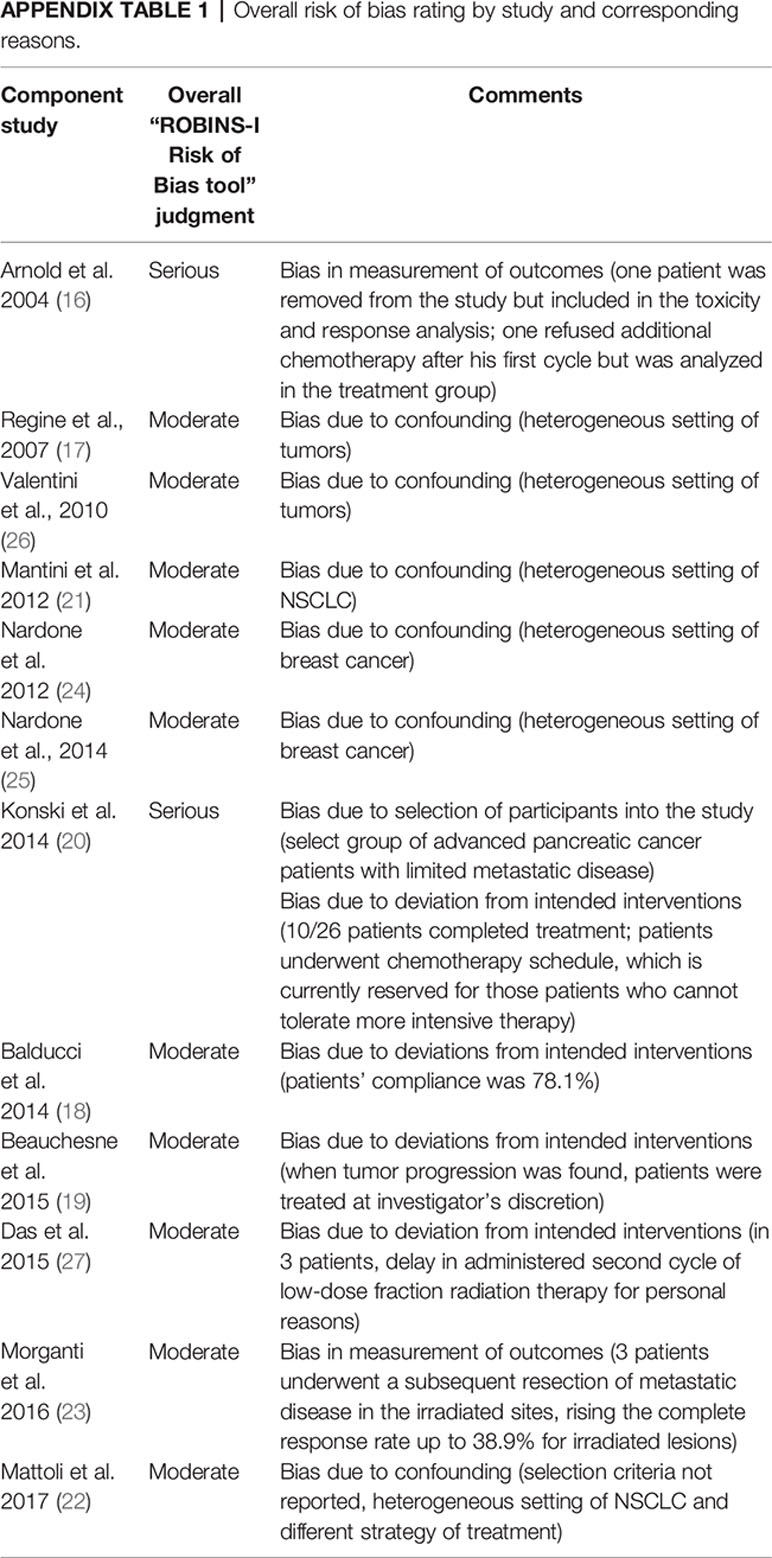
Two studies were retrospective (22, 26), one was a prospective pilot trial (18), six were phase II studies (16, 19, 21, 23, 25, 27), two were phase I trials (20, 24), and one was a phase I/II open label study (17). No randomized controlled trials were found. All were considered to own moderate to serious risk of bias according to the ROBINS-I tool (30). Appendix 1 shows the risk of bias rating per study based on the ROBINS-I tool.
Analysis of the Selected Studies
Treated Tumors
The characteristics and stage of primary tumors in the analyzed papers are shown in Table 1.
Patients and Treatment
Patients’ median age ranged from 21 to 84 years (median 57.6) (16–18, 20, 22–26). Median follow-up ranged from 6.5 to 48 months (median: 22.5 months). The RT total dose ranged from 1.6 to 67.5 Gy. CHT was based on different schedules depending on tumor features. RT details and CHT schedules are shown in Table 1.
Evaluations
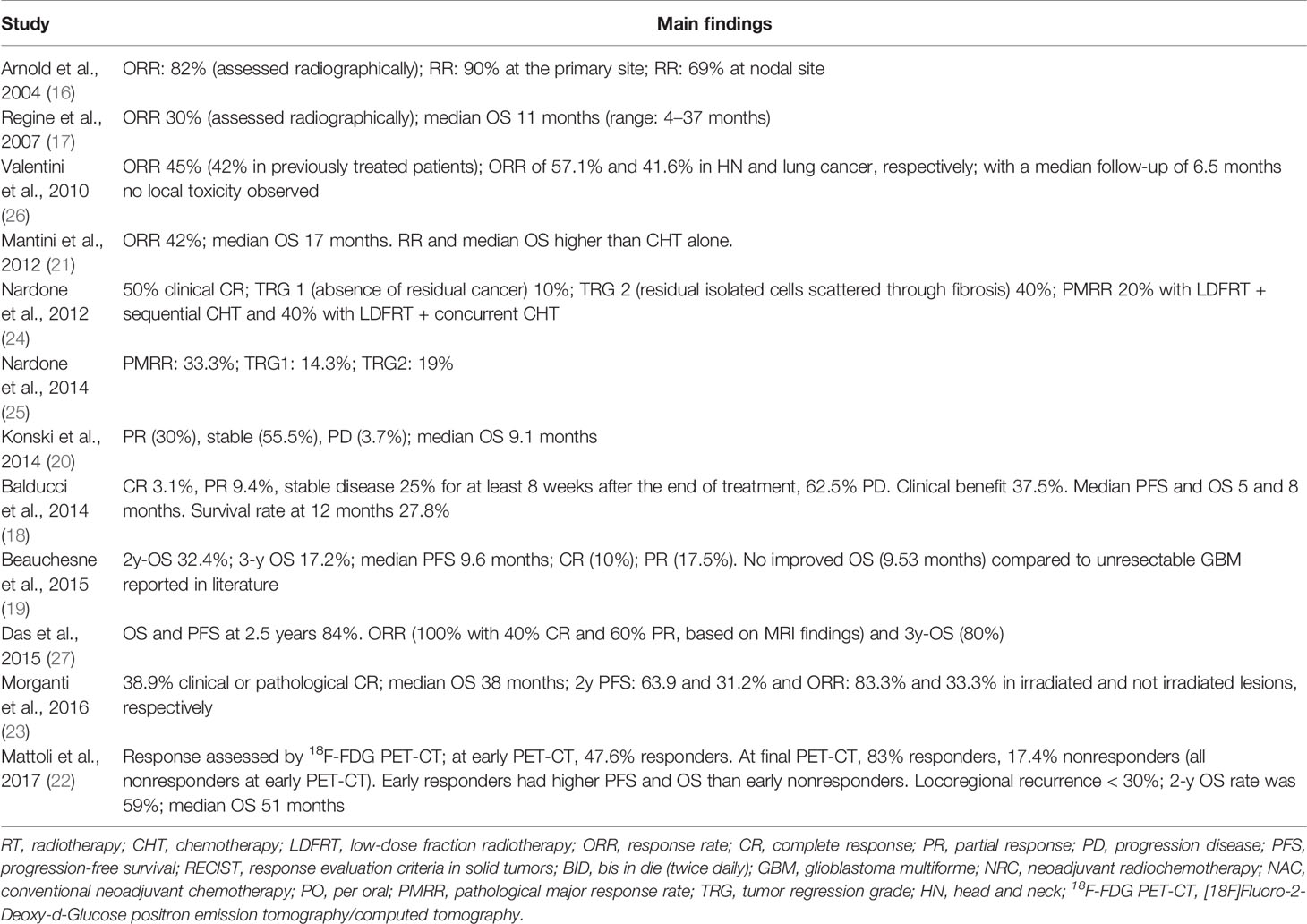
Response was reported in different ways in all the studies (16–27), while overall survival (OS) rates were reported in six studies (18, 19, 21–23, 27). Toxicity was reported in 11 studies (16–21, 23–27), mainly using the Common Toxicity Criteria for Adverse Events scale (31).
Treatment Results
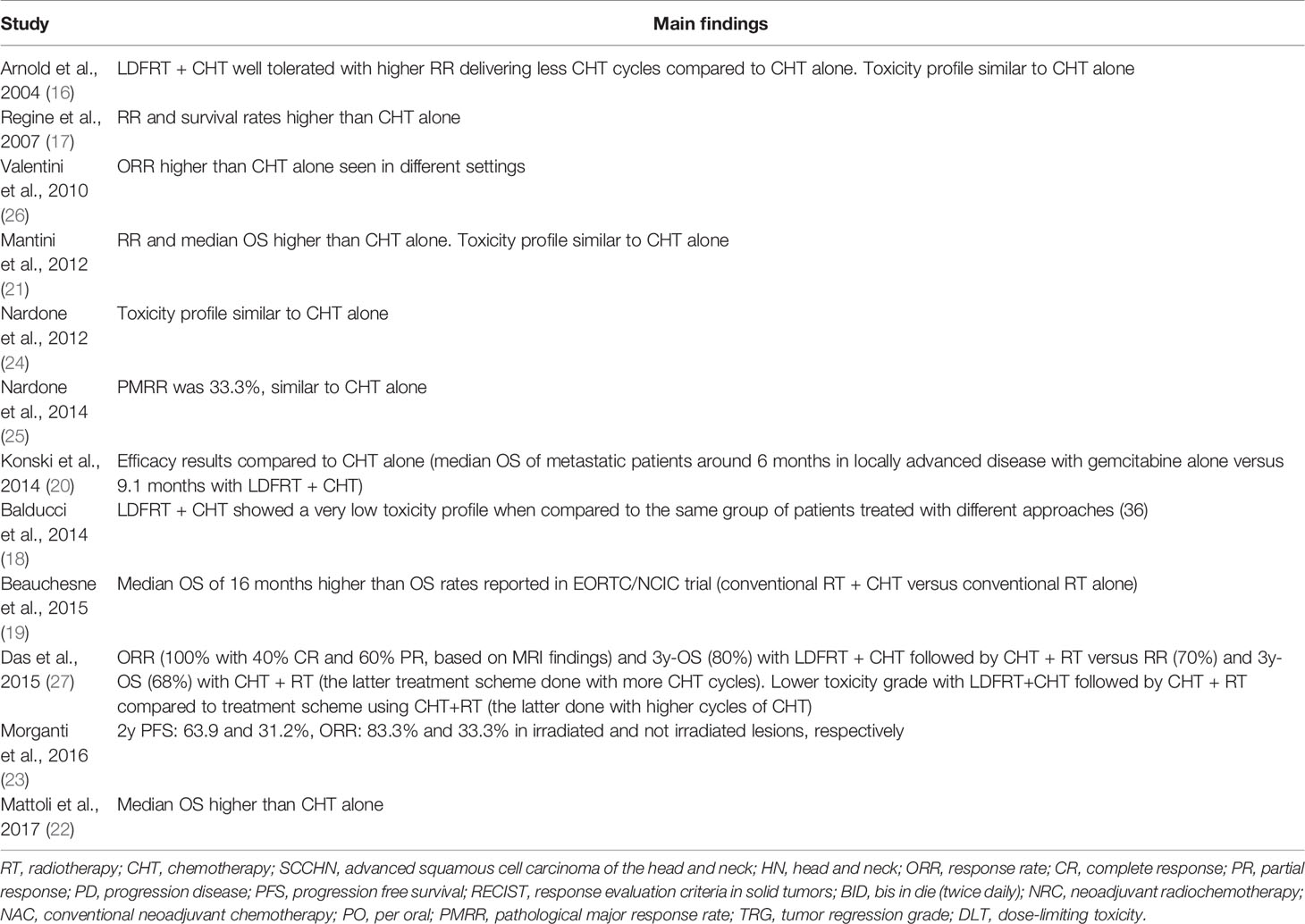
Toxicity results are shown in Table 2. In most studies, the treatment was reasonably tolerated, despite obvious differences due to the different used CHT regimens (16–21, 23–27). In the phase II trial conducted by Beauchesne et al. (19) on LDFRT plus temozolomide in glioblastoma multiforme (GBM), three cases of fatal adverse events were reported: one due to hematological toxicity and two due to pulmonary infections. Moreover, Regine and colleagues (17), in their trial on gemcitabine plus LDFRT in pancreatic and small bowel cancers, reported one grade 3 infection out of six patients treated with 0.6 Gy/fraction and one grade 3 infection and one grade 3 diarrhea out of four patients treated with 0.7 Gy/fraction. Table 3 reports details on tumor response and outcome. The results are very inhomogeneous as expected considering the different treated tumors and clinical settings.
Comparisons
Among all the studies included in our review, only Morganti and colleagues compared irradiated (LDFRT) and non-irradiated sites in patients with metastatic colorectal cancer treated with FOLFIRI-Bevacizumab (23). The authors reported 83.4% and 33.3% overall response rate (ORR) in irradiated and non-irradiated metastases, respectively (p: 0.02). Moreover, the 2-year progression rate was 63.9% and 31.2% in irradiated and non-irradiated sites, respectively (p: 0.08) (23). In other publications, the results of LDFRT-CHT were compared to those of CHT alone as reported in other studies (Table 4) (16–22, 24–27).
Discussion
To the best of our knowledge, this is the first review of clinical studies on combined LDFRT plus CHT. Five studies compared clinical response rates after LDFRT-CHT with literature data on CHT in similar patients, reporting higher ORR rates (16, 21, 23, 26, 27). Similarly, four studies compared OS after LDFRT-CHT and reported improved outcome compared to CHT alone (17, 19, 20, 22). Finally, four studies compared toxicity after LDFRT plus CHT versus CHT alone reporting similar adverse event rates (16, 21, 24, 25). Interestingly, clinical findings regarding LDFRT-CHT were published in 12 studies between 2004 and 2017, and no further studies were published thereafter. The lack of prospective studies, moreover with no control groups, could explain the disinterest in this combined modality therapy.
However, in most cases, the analyzed studies included only patients undergoing LDFRT plus CHT, without direct comparisons with patients undergoing CHT alone. In fact, differences were almost always tested against CHT results from other published studies.
Arnold et al. (16) reported higher ORR (90%), in advanced head and neck squamous cell carcinoma treated with LDFRT plus CHT, compared to literature data (55–75%) on similar patients treated with the same drug combination (carboplatin plus paclitaxel) (32–35). Regine et al. (17) reported prolonged OS after LDFRT plus gemcitabine, in locally advanced pancreatic adenocarcinoma, compared to literature data (36, 37) on gemcitabine alone (median OS: 11 months versus 4.8–5.6 months, respectively). Konski et al. (20) reported on locally advanced pancreatic cancer, with or without small burden metastatic disease, recording improved OS after LDFRT plus erlotinib and gemcitabine (9.1 months) compared to a study on erlotinib and gemcitabine alone (6.2 months) (38). Mattoli et al. (22) reported prolonged median OS in stage IIIA-IIIB non-small cell lung cancer treated with LDFRT plus concurrent induction CHT compared to another study (39) based on induction CHT alone in a similar patient population (median OS: 51 months versus 12.5 months, respectively). Beauchesne et al. published the results of their phase II trial (19) on inoperable GBM treated with LDFRT plus temozolomide reporting 16 months median OS. Surprisingly, this result is at least comparable with the outcome (median OS: 14.6 months) recorded in the EORTC/NCIC trial after standard RT plus temozolomide in patients with resected disease (40). Mantini et al. (21) reported 42% ORR and 17 months median OS in stage III-IV non-small cell lung cancer treated with LDFRT plus concurrent pemetrexed. These results were better compared to 9.1% ORR and 8.3 months median OS recorded in a similar patient population treated with pemetrexed alone (41). Valentini et al. (26) reported higher response rates in patients with lung (ORR: 41.6%) and head and neck cancer (ORR: 57%) treated with LDFRT-CHT compared to literature data on lung (ORR: 5–10%) (42, 43) and head and neck tumors (ORR: 10–35%) (44–47) treated with CHT alone (similar regimens). Das et al. (27) reported 100% ORR and 100% 2-year OS in locally advanced carcinoma of the uterine cervix treated with LDFRT plus induction CHT followed by radical chemoradiation. These figures were higher compared to the ones registered in a similar patient population treated with the same CHT induction regimen followed by standard chemoradiation (48). Only two studies did not show improved results after LDFRT plus CHT compared to CHT alone. In fact, Nardone et al. (24, 25) treated stage IIA/B-IIIA breast cancer patients with LDFRT plus CHT and reported similar response rates compared to CHT alone. However, it should be noted that the sample size of these studies was particularly small, with only 10 (24) and 21 patients (25) enrolled, respectively.
In terms of toxicity, Arnold et al. (16), Nardone et al. (24, 25), and Mantini et al. (21) reported similar toxicity profile in patients treated with LDFRT plus CHT compared to studies on CHT alone. Moreover, Balducci et al. (18) reported lower toxicity rates with LDFRT plus CHT compared to similar patient groups with recurrent GBM (49, 50) treated with several different approaches (second-line CHT, re-irradiation, re-resection). The worse complications recorded in the analyzed papers were reported in Beauchesne et al.’s (19) and Regine et al.’s studies (17). The first series included GBM patients treated with LDFRT plus temozolomide. Three cases of fatal adverse events were recorded: one after severe hematological toxicity and two due to pulmonary infections (19). It should be noted that these complications are not uncommon in patients treated with temozolomide alone. In particular, pneumonitis can occur when prophylactic treatment against pneumocystis carinii infections is not prescribed. In the second study, based on LDFRT plus gemcitabine in pancreatic and small bowel cancers, two grade 3 infections and one grade 3 diarrhea were reported (17). The irradiation of the entire upper abdomen could almost partially explain these adverse events.
A comparison within the same study between LDFRT-CHT and CHT was reported only by Morganti et al. As previously described, after CHT based on the FOLFIRI-bevacizumab regimen, the ORR rate was 83.4% in metastatic lesions undergoing LDFRT and 33.3% in non-irradiated lesions (p: 0.02) (23).
This review has several limitations including lack of randomized trials, heterogeneity of the study design with inclusion of two retrospective studies (22, 26), small sample size with a median number of 23 patients per study (range: 6-44) and four studies with less than 20 patients, and heterogeneity in terms of tumor and treatment characteristics. More specifically, the outcome results reported in two phase I (24) and phase I/II (17) trials, each enrolling only 10 patients, must be interpreted with caution due to the very small sample size. The usefulness of a literature review with these limitations could be debatable. However, due to lack of evidence from large prospective trials, we considered it useful to review the available data. Furthermore, it should be emphasized the uniformity between the analyzed series in terms of results, since all studies reported better outcomes after LDFRT-CHT compared to CHT alone, apart from two small studies on breast cancer (24, 25).
Based on the low level of evidence of the selected studies, the use of LDFRT-CHT in current clinical practice does not seem justified. However, especially in advanced cancers resistant to systemic therapies, enrollment of patients in prospective studies would be useful.
Further studies in this field could have the following design or aims: (i) randomized comparison between LDFRT-CHT versus CHT alone; (ii) definition of the optimal dose and fractionation in LDFRT-CHT; (iii) definition of the optimal CHT regimens in this setting; and (iv) evaluation of LDFRT plus immunotherapy combination, given some evidence on the immune-enhancement effect of LDFRT (51).
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Author Contributions
Conception and design: ES, FC, AZ, and AM. Data extraction from included studies: ES, FC, GM, FD, and AGM. Analysis and interpretation of data: ES, FD, SCi, LS, MB, SR, SCa, and AM. Manuscript writing: all authors. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2021.748200/full#supplementary-material
References
1. Joiner MC, Marples B, Lambin P, Short SC, Turesson I. Low-Dose Hypersensitivity: Current Status and Possible Mechanisms. Int J Radiat Oncol Biol Phys (2001) 49(2):379–89. doi: 10.1016/s0360-3016(00)01471-1
2. Lambin P, Marples B, Fertil B, Malaise EP, Joiner MC. Hypersensitivity of a Human Tumour Cell Line to Very Low Radiation Doses. Int J Radiat Biol (1993) 63(5):639–50. doi: 10.1080/09553009314450831
3. Joiner MC. Induced Radioresistance: An Overview and Historical Perspective. Int J Radiat Biol (1994) 65(1):79–84. doi: 10.1080/09553009414550111
4. Wouters BG, Sy AM, Skarsgard LD. Low-Dose Hypersensitivity and Increased Radioresistance in a Panel of Human Tumor Cell Lines With Different Radiosensitivity. Radiat Res (1996) 146(4):399–413. doi: 10.2307/3579302
5. Marples B, Lambin P, Skov KA, Joiner MC. Low Dose Hyper-Radiosensitivity and Increased Radioresistance in Mammalian Cells. Int J Radiat Biol (1997) 71(6):721–35. doi: 10.1080/095530097143725
6. Lambin P, Malaise EP, Joiner MC. Might Intrinsic Radioresistance of Human Tumour Cells be Induced by Radiation? Int J Radiat Biol (1996) 69(3):279–90. doi: 10.1080/095530096145832
7. Marples B, Wouters BG, Joiner MC. An Association Between the Radiation-Induced Arrest of G2-Phase Cells and Low-Dose Hyper-Radiosensitivity: A Plausible Underlying Mechanism? Radiat Res (2003) 160(1):38–45. doi: 10.1667/rr3013
8. Marples B, Wouters BG, Collis SJ, Chalmers AJ, Joiner MC. Low-Dose Hyper-Radiosensitivity: A Consequence of Ineffective Cell Cycle Arrest of Radiation-Damaged G2-Phase Cells. Radiat Res (2004) 161(3):247–55. doi: 10.1667/rr3130
9. Klug F, Prakash H, Huber PE, Seibel T, Bender N, Halama N, et al. Low-Dose Irradiation Programs Macrophage Differentiation to an iNOS/M1 Phenotype That Orchestrates Effective T Cell Immunotherapy. Cancer Cell (2013) 24(5):589–602. doi: 10.1016/j.ccr.2013.09.014
10. Beauchesne P. Three-Times Daily Ultrafractionated Radiation Therapy, a Novel and Promising Regimen for Glioblastoma Patients. Cancers (Basel) (2013) 5(4):1199–211. doi: 10.3390/cancers5041199
11. Chendil D, Oakes R, Mohiuddin M, Alcock RA, Gallicchio VS, Ahmed MM, et al. Low Dose Fractionated Radiation Enhances the Radiosensitization Effect of Paclitaxel in Colorectal Tumor Cells With Mutant P53. Cancer (2000) 89(9):1893–900. doi: 10.1002/1097-0142(20001101)89:9<1893::aid-cncr4>3.3.co;2-2
12. Dey S, Spring PM, Arnold S, Valentino J, Chendil D, Regine WF, et al. Low-Dose Fractionated Radiation Potentiates the Effects of Paclitaxel in Wild-Type and Mutant P53 Head and Neck Tumor Cell Lines. Clin Cancer Res (2003) 9(4):1557–65.
13. Gupta S, Koru-Sengul T, Arnold SM, Devi GR, Mohiuddin M, Ahmed MM, et al. Low-Dose Fractionated Radiation Potentiates the Effects of Cisplatin Independent of the Hyper-Radiation Sensitivity in Human Lung Cancer Cells. Mol Cancer Ther (2011) 10(2):292–302. doi: 10.1158/1535-7163.MCT-10-0630
14. Spring PM, Arnold SM, Shajahan S, Brown B, Dey S, Lele SM, et al. Low Dose Fractionated Radiation Potentiates the Effects of Taxotere in Nude Mice Xenografts of Squamous Cell Carcinoma of Head and Neck. Cell Cycle (2004) 3(4):479–85. doi: 10.4161/cc.3.4.786
15. Beauchesne PD, Bertrand S, Branche R, Linke SP, Revel R, Dore JF, et al. Human Malignant Glioma Cell Lines Are Sensitive to Low Radiation Doses. Int J Cancer (2003) 105(1):33–40. doi: 10.1002/ijc.11033
16. Arnold SM, Regine WF, Ahmed MM, Valentino J, Spring P, Kudrimoti M, et al. Low-Dose Fractionated Radiation as a Chemopotentiator of Neoadjuvant Paclitaxel and Carboplatin for Locally Advanced Squamous Cell Carcinoma of the Head and Neck: Results of a New Treatment Paradigm. Int J Radiat Oncol Biol Phys (2004) 58(5):1411–7. doi: 10.1016/j.ijrobp.2003.09.019
17. Regine WF, Hanna N, Garofalo MC, Doyle A, Arnold S, Kataria R, et al. Low-Dose Radiotherapy as a Chemopotentiator of Gemcitabine in Tumors of the Pancreas or Small Bowel: A Phase I Study Exploring a New Treatment Paradigm. Int J Radiat Oncol Biol Phys (2007) 68(1):172–7. doi: 10.1016/j.ijrobp.2006.11.045
18. Balducci M, Diletto B, Chiesa S, D'Agostino GR, Gambacorta MA, Ferro M, et al. Low-Dose Fractionated Radiotherapy and Concomitant Chemotherapy for Recurrent or Progressive Glioblastoma: Final Report of a Pilot Study. Strahlenther Onkol (2014) 190(4):370–6. doi: 10.1007/s00066-013-0506-z
19. Beauchesne P, Quillien V, Faure G, Bernier V, Noel G, Quetin P, et al. A Concurrent Ultra-Fractionated Radiation Therapy and Temozolomide Treatment: A Promising Therapy for Newly Diagnosed, Inoperable Glioblastoma. Int J Cancer (2016) 138(6):1538–44. doi: 10.1002/ijc.29898
20. Konski A, Meyer JE, Joiner M, Hall MJ, Philip P, Shields A, et al. Multi-Institutional Phase I Study of Low-Dose Ultra-Fractionated Radiotherapy as a Chemosensitizer for Gemcitabine and Erlotinib in Patients With Locally Advanced or Limited Metastatic Pancreatic Cancer. Radiother Oncol (2014) 113(1):35–40. doi: 10.1016/j.radonc.2014.08.014
21. Mantini G, Valentini V, Meduri B, Margaritora S, Balducci M, Micciché F, et al. Low-Dose Radiotherapy as a Chemo-Potentiator of a Chemotherapy Regimen With Pemetrexed for Recurrent Non-Small-Cell Lung Cancer: A Prospective Phase II Study. Radiother Oncol (2012) 105(2):161–6. doi: 10.1016/j.radonc.2012.09.006
22. Mattoli MV, Massaccesi M, Castellucci A, Scolozzi V, Mantini G, Calcagni ML, et al. The Predictive Value of 18F-FDG PET-CT for Assessing the Clinical Outcomes in Locally Advanced NSCLC Patients After a New Induction Treatment: Low-Dose Fractionated Radiotherapy With Concurrent Chemotherapy. Radiat Oncol (2017) 12(1):4. doi: 10.1186/s13014-016-0737-0
23. Morganti AG, Cellini F, Mignogna S, Padula GDA, Caravatta L, Deodato F, et al. Low-Dose Radiotherapy and Concurrent FOLFIRI-Bevacizumab: A Phase II Study. Future Oncol (2016) 12(6):779–87. doi: 10.2217/fon.15.350
24. Nardone L, Valentini V, Marino L, De Santis MC, Terribile D, Franceschini G, et al. A Feasibility Study of Neo-Adjuvant Low-Dose Fractionated Radiotherapy With Two Different Concurrent Anthracycline-Docetaxel Schedules in Stage IIA/B-IIIA Breast Cancer. Tumori (2012) 98(1):79–85. doi: 10.1700/1053.11503
25. Nardone L, Diletto B, De Santis MC, D' Agostino GR, Belli P, Bufi E, et al. Primary Systemic Treatment and Concomitant Low Dose Radiotherapy for Breast Cancer: Final Results of a Prospective Phase II Study. Breast (2014) 23(5):597–602. doi: 10.1016/j.breast.2014.06.005
26. Valentini V, Massaccesi M, Balducci M, Mantini G, Micciché F, Mattiucci GC, et al. Low-Dose Hyperradiosensitivity: Is There a Place for Future Investigation in Clinical Settings? Int J Radiat Oncol Biol Phys (2010) 76(2):535–9. doi: 10.1016/j.ijrobp.2009.02.075
27. Das S, Subhashini J, Rami Reddy JK, KantiPal S, Isiah R, Oommen R, et al. Low-Dose Fractionated Radiation and Chemotherapy Prior to Definitive Chemoradiation in Locally Advanced Carcinoma of the Uterine Cervix: Results of a Prospective Phase II Clinical Trial. Gynecol Oncol (2015) 138(2):292–8. doi: 10.1016/j.ygyno.2015.05.020
28. Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. PRISMA-P Group. Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015: Elaboration and Explanation. BMJ (2015) 350:g7647. doi: 10.1136/bmj.g7647
29. Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, et al. The PRISMA Extension Statement for Reporting of Systematic Reviews Incorporating Network Meta-Analyses of Health Care Interventions: Checklist and Explanations. Ann Intern Med (2015) 162(11):777–84. doi: 10.7326/M14-2385
30. Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: A Tool for Assessing Risk of Bias in Non-Randomised Studies of Interventions. BMJ (2016) 355:i4919. doi: 10.1136/bmj.i4919
31. Common Terminology Criteria for Adverse Events (CTCAE). Available at: https://ctep.cancer.gov/protocoldevelopment/electronic_applications/ctc.htm (Accessed 26 December 2020).
32. Vokes EE, Stenson K, Rosen FR, Kies MS, Rademaker AW, Witt ME, et al. Weekly Carboplatin and Paclitaxel Followed by Concomitant Paclitaxel, Fluorouracil, and Hydroxyurea Chemoradiotherapy: Curative and Organ-Preserving Therapy for Advanced Head and Neck Cancer. J Clin Oncol (2003) 21(2):320–6. doi: 10.1200/JCO.2003.06.006
33. Bouillet T, Morere J, Depreaux G. Phase II Study of Paclitaxel (P) Twice a Week as a Radiosensitizer, After Paclitaxel-Carboplatin (C) Induction in Stage III-IV Head and Neck Carcinoma. Proc Am Soc Clin Oncol (1999) 18:403a. doi: 10.1016/S0959-8049(99)81076-4
34. Dunphy FR, Dunleavy TL, Harrison BR, Trinkaus KM, Kim HJ, Stack BC Jr, et al. Induction Paclitaxel and Carboplatin for Patients With Head and Neck Carcinoma. Analysis of 62 Patients Treated Between 1994 an 1999. Cancer (2001) 91(5):940–8. doi: 10.1002/1097-0142(20010301)91:5<940::AID-CNCR1083>3.0.CO;2-A
35. Machtay M, Rosenthal DI, Hershock D, Jones H, Williamson S, Greenberg MJ, et al. Penn Cancer Center Clinical Trials Group. Organ Preservation Therapy Using Induction Plus Concurrent Chemoradiation for Advanced Resectable Oropharyngeal Carcinoma: A University of Pennsylvania Phase II Trial. J Clin Oncol (2002) 20(19):3964–71. doi: 10.1200/JCO.2002.11.026
36. Storniolo AM, Enas NH, Brown CA, Voi M, Rothenberg ML, Schilsky R. An Investigational New Drug Treatment Program for Patients With Gemcitabine: Results for Over 3000 Patients With Pancreatic Carcinoma. Cancer (1999) 85(6):1261–8. doi: 10.1002/(SICI)1097-0142(19990315)85:6<1261::AID-CNCR7>3.0.CO;2-T
37. Burris HA 3rd, Moore MJ, Andersen J, Green MR, Rothenberg ML, Modiano MR, et al. Improvements in Survival and Clinical Benefit With Gemcitabine as First-Line Therapy for Patients With Advanced Pancreas Cancer: A Randomized Trial. J Clin Oncol (1997) 15(6):2403–13. doi: 10.1200/JCO.1997.15.6.2403
38. Moore MJ, Goldstein D, Hamm J, Figer A, Hecht JR, Gallinger S, et al. National Cancer Institute of Canada Clinical Trials Group. Erlotinib Plus Gemcitabine Compared With Gemcitabine Alone in Patients With Advanced Pancreatic Cancer: A Phase III Trial of the National Cancer Institute of Canada Clinical Trials Group. J Clin Oncol (2007) 25(15):1960–6. doi: 10.1200/JCO.2006.07.9525
39. Ardizzoni A, Grossi F, Scolaro T, Giudici S, Foppiano F, Boni L, et al. Induction Chemotherapy Followed by Concurrent Standard Radiotherapy and Daily Low-Dose Cisplatin in Locally Advanced Non-Small-Cell Lung Cancer. Br J Cancer (1999) 81(2):310–5. doi: 10.1038/sj.bjc.6990693
40. Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, et al. European Organisation for Research and Treatment of Cancer Brain Tumor and Radiotherapy Groups; National Cancer Institute of Canada Clinical Trials Group. Radiotherapy Plus Concomitant and Adjuvant Temozolomide for Glioblastoma. N Engl J Med (2005) 352(10):987–96. doi: 10.1056/NEJMoa043330
41. Hanna N, Shepherd FA, Fossella FV, Pereira JR, De Marinis F, von Pawel J, et al. Randomized Phase III Trial of Pemetrexed Versus Docetaxel in Patients With Non-Small-Cell Lung Cancer Previously Treated With Chemotherapy. J Clin Oncol (2004) 22(9):1589–97. doi: 10.1200/JCO.2004.08.163
42. Shepherd FA, Dancey J, Ramlau R, Mattson K, Gralla R, O'Rourke M, et al. Prospective Randomized Trial of Docetaxel Versus Best Supportive Care in Patients With Non-Small-Cell Lung Cancer Previously Treated With Platinum-Based Chemotherapy. J Clin Oncol (2000) 18(10):2095–103. doi: 10.1200/JCO.2000.18.10.2095
43. Fossella FV, DeVore R, Kerr RN, Crawford J, Natale RR, Dunphy F, et al. Randomized Phase III Trial of Docetaxel Versus Vinorelbine or Ifosfamide in Patients With Advanced Non-Small-Cell Lung Cancer Previously Treated With Platinum-Containing Chemotherapy Regimens. The TAX 320 Non-Small Cell Lung Cancer Study Group. J Clin Oncol (2000) 18(12):2354–62. doi: 10.1200/JCO.2000.18.12.2354. Erratum in: J Clin Oncol. (2004); 22(1):209. PMID: 10856094.
44. Forastiere AA, Metch B, Schuller DE, Ensley JF, Hutchins LF, Triozzi P, et al. Randomized Comparison of Cisplatin Plus Fluorouracil and Carboplatin Plus Fluorouracil Versus Methotrexate in Advanced Squamous-Cell Carcinoma of the Head and Neck: A Southwest Oncology Group Study. J Clin Oncol (1992) 10(8):1245–51. doi: 10.1200/JCO.1992.10.8.1245
45. Forastiere AA, Leong T, Rowinsky E, Murphy BA, Vlock DR, DeConti RC, et al. Phase III Comparison of High-Dose Paclitaxel + Cisplatin + Granulocyte Colony-Stimulating Factor Versus Low-Dose Paclitaxel + Cisplatin in Advanced Head and Neck Cancer: Eastern Cooperative Oncology Group Study E1393. J Clin Oncol (2001) 19(4):1088–95. doi: 10.1200/JCO.2001.19.4.1088
46. Gibson MK, Li Y, Murphy B, Hussain MH, DeConti RC, Ensley J, et al. Eastern Cooperative Oncology Group. Randomized Phase III Evaluation of Cisplatin Plus Fluorouracil Versus Cisplatin Plus Paclitaxel in Advanced Head and Neck Cancer (E1395): An Intergroup Trial of the Eastern Cooperative Oncology Group. J Clin Oncol (2005) 23(15):3562–7. doi: 10.1200/JCO.2005.01.057
47. Soulieres D, Senzer NN, Vokes EE, Hidalgo M, Agarwala SS, et al. Multicenter Phase II Study of Erlotinib, an Oral Epidermal Growth Factor Receptor Tyrosine Kinase Inhibitor, in Patients With Recurrent or Metastatic Squamous Cell Cancer of the Head and Neck. J Clin Oncol (2004) 22(1):77–85. doi: 10.1200/JCO.2004.06.075
48. McCormack M, Kadalayil L, Hackshaw A, Hall-Craggs MA, Symonds RP, Warwick V, et al. A Phase II Study of Weekly Neoadjuvant Chemotherapy Followed by Radical Chemoradiation for Locally Advanced Cervical Cancer. Br J Cancer (2013) 108(12):2464–9. doi: 10.1038/bjc.2013.230
49. Niyazi M, Siefert A, Schwarz SB, Ganswindt U, Kreth FW, Tonn JC, et al. Therapeutic Options for Recurrent Malignant Glioma. Radiother Oncol (2011) 98(1):1–14. doi: 10.1016/j.radonc.2010.11.006
50. Gilbert MR. Recurrent Glioblastoma: A Fresh Look at Current Therapies and Emerging Novel Approaches. Semin Oncol (2011) 38(Suppl;4):S21–33. doi: 10.1053/j.seminoncol.2011.09.008
51. Reissfelder C, Timke C, Schmitz-Winnenthal H, Rahbari NN, Koch M, Klug F, et al. A Randomized Controlled Trial to Investigate the Influence of Low Dose Radiotherapy on Immune Stimulatory Effects in Liver Metastases of Colorectal Cancer. BMC Cancer (2011) 11:419. doi: 10.1186/1471-2407-11-419
Keywords: chemo-sensitization, low-dose radiotherapy, systematic review, clinical trials, combined modality treatment
Citation: Scirocco E, Cellini F, Zamagni A, Macchia G, Deodato F, Cilla S, Strigari L, Buwenge M, Rizzo S, Cammelli S and Morganti AG (2021) Clinical Studies on Ultrafractionated Chemoradiation: A Systematic Review. Front. Oncol. 11:748200. doi: 10.3389/fonc.2021.748200
Received: 27 July 2021; Accepted: 25 October 2021;
Published: 16 November 2021.
Edited by:
Alessio Bruni, University Hospital of Modena, ItalyReviewed by:
Elvira V. Grigorieva, Institute of Molecular Biology and Biophysics (RAS), RussiaAndra Valentina Krauze, National Cancer Institute, United States
Copyright © 2021 Scirocco, Cellini, Zamagni, Macchia, Deodato, Cilla, Strigari, Buwenge, Rizzo, Cammelli and Morganti. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Erica Scirocco, ZXJpY2Euc2Npcm9jY29Ac3R1ZGlvLnVuaWJvLml0
†These authors share senior authorship
 Erica Scirocco
Erica Scirocco Francesco Cellini
Francesco Cellini Alice Zamagni
Alice Zamagni Gabriella Macchia
Gabriella Macchia Francesco Deodato5
Francesco Deodato5 Milly Buwenge
Milly Buwenge Stefania Rizzo
Stefania Rizzo Silvia Cammelli
Silvia Cammelli Alessio Giuseppe Morganti
Alessio Giuseppe Morganti