- 1Department of Medical Oncology, Fudan University Shanghai Cancer Center, Shanghai, China
- 2Department of Oncology, Shanghai Medical College, Fudan University, Shanghai, China
- 3Department of Pathology, Fudan University Shanghai Cancer Center, Shanghai, China
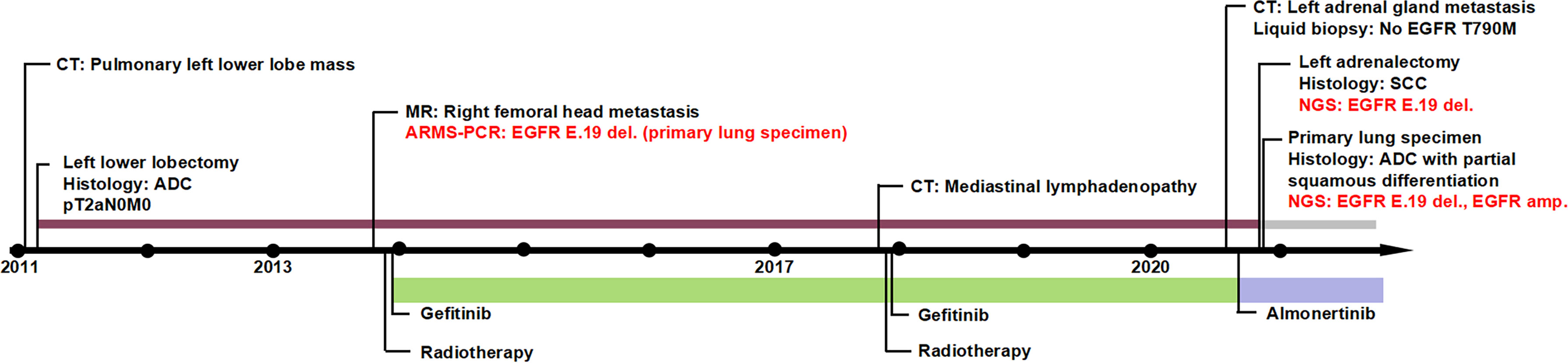
The histological transformation from epidermal growth factor receptor (EGFR)-mutated adenocarcinoma (ADC) to squamous cell carcinoma (SCC) after tyrosine kinase inhibitor (TKI) treatment is rare. We present a case of a patient who transitioned from early-stage primary lung ADC with partial squamous differentiation, EGFR mutation and amplification, to adrenal gland metastasis as SCC with EGFR amplification disappearance 115-months after surgery, during which gefitinib and local radiotherapy were utilized for the metastasis in the right femoral head and mediastinal lymph nodes. This case might indicate a possible mechanism of EGFR inhibition resistance with SCC transition and EGFR amplification loss from the initially well-responding ADC, especially those with SCC or partial squamous differentiation. The optimal post-progression therapy for ADC-SCC patients is challenging and further studies are needed.
Introduction
The development of targeted therapy has significantly advanced the treatment of non-small cell lung cancer patients. Epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors (TKIs) have been well supported as beneficial treatments for EGFR-mutated lung cancer patients (1, 2).
Despite an initial favorable response to EGFR-TKIs, patients typically experience disease progression within 9 to 12 months (3). The reported drug resistance mechanisms include, but are not limited to acquisition of the EGFR T790M mutation in exon 20, MET amplification, PIK3CA mutation, HER2 amplification, and small cell histological transformation (4, 5).
The rare phenomenon of transformation from lung adenocarcinoma (ADC) to squamous cell carcinoma (SCC) during EGFR inhibition treatment has also been described as a possible mechanism involving the acquired resistance to EGFR-TKIs (6–8). Herein, we present a new case of EGFR-mutant (exon 19 deletion) and EGFR-amplified early-stage lung ADC, in which histology revealed partial squamous differentiation, undergoing transformation into metastatic SCC with the disappearance of EGFR amplification subsequent to a long-term standard sequential treatment involving surgery, local radiotherapy, and treatment with the first-generation EGFR-TKI, gefitinib.
Case Description
A 54-year-old man with no smoking history presented with persistent cough in January 2011. Thoracic computed tomography (CT) demonstrated a pulmonary left lower lobe mass. The patient underwent a left lower lobectomy with mediastinal lymph node dissection. The tumor size was 4.0 × 3.5 × 3.5 cm with no lymph node metastasis (pT2aN0M0) and was histologically diagnosed as an adenocarcinoma. No adjuvant chemotherapy or radiotherapy was performed.
Two years after the operation, metastasis in the right femoral head was detected by magnetic resonance imaging (MRI) (Figure 1A). A deletion at exon 19 of the EGFR gene was identified by Sanger sequencing in a surgical specimen of the primary lung carcinoma. The patient started radiotherapy for the right femoral head metastasis followed by gefitinib treatment with 250 mg/day in December 2013 and showed a partial response. Mediastinal lymphadenopathy was detected by CT in December 2017 (Figure 1B). There was no disease progression to other sites. The patient refused endobronchial ultrasound-guided needle aspiration (EBUS-TBNA) of the mediastinal masses. Given the absence of EGFR T790M mutation detection in the liquid biopsy sample, he continued with gefitinib treatment and received radiotherapy for the mediastinal lymph nodes in January 2018. A partial response was achieved.
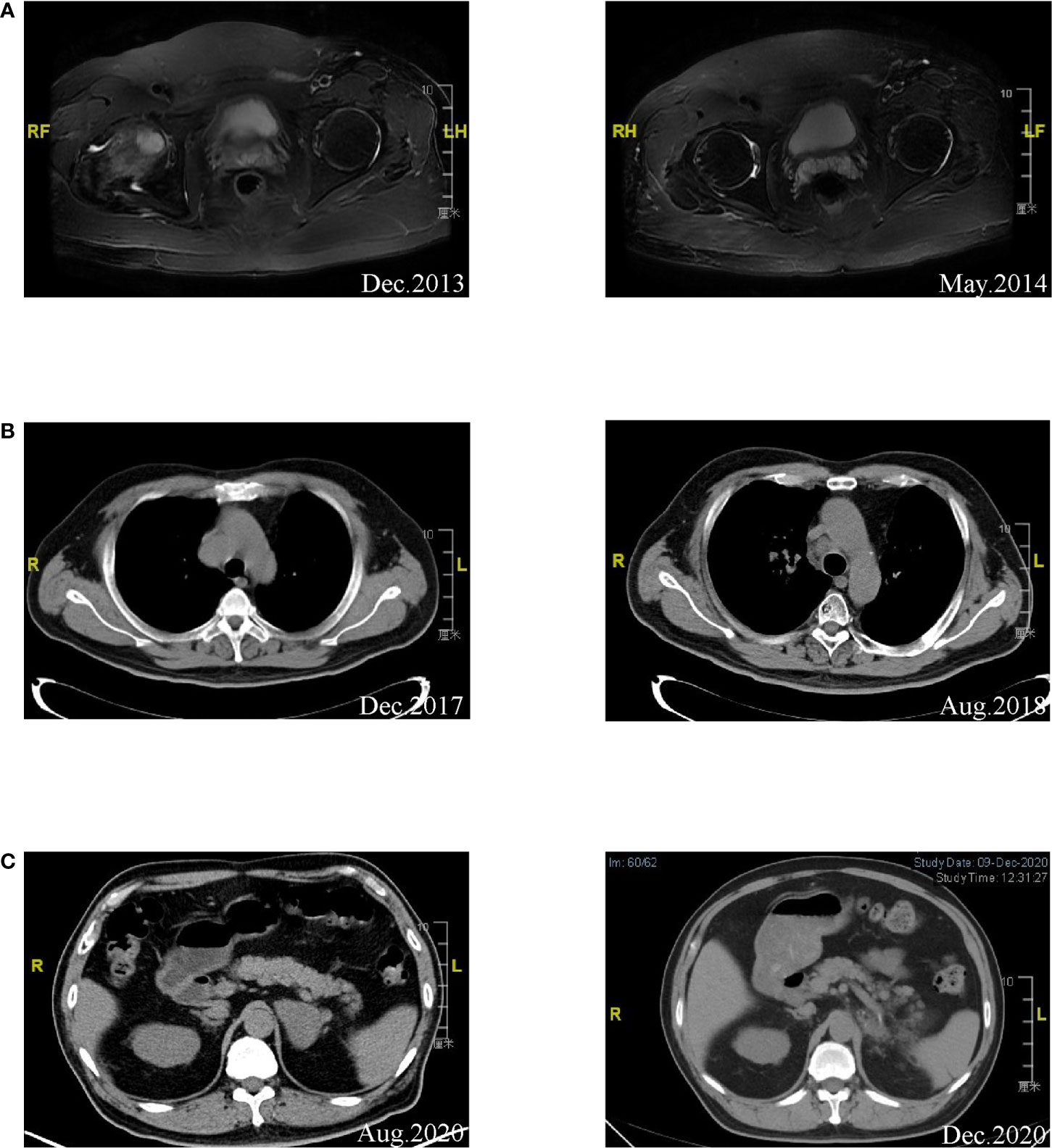
Figure 1 (A) Left: MRI of right femoral head indicating metastasis diagnosis. Right: A partial response was achieved after radiotherapy and gefitinib treatment. (B) Left: Disease progression was found in mediastinal lymph nodes by CT. Right: A partial response was achieved after continued gefitinib treatment and radiotherapy. (C) Left: Metastasis was detected in the left adrenal gland. Right: CT image of the patient after left adrenalectomy was performed.
Disease progression was revealed by CT showing a metastasis in the left adrenal gland in August 2020 (Figure 1C). The patient then received treatment with the third-generation EGFR-TKI almonertinib at 110 mg/day in August 2020 and showed stable disease. Left adrenalectomy was performed in October 2020. Squamous cell carcinoma histology was identified from the left adrenal gland specimen by immunohistochemistry, which was TTF-1 and NapsinA negative, P40 partially positive, and CK7 positive (Figures 2A–C). The sample was subjected to a sequencing study using FoundationOne CDx (an FDA-approved 324-gene panel assay), and the results showed an EGFR exon 19 deletion (delE746_A750, allele frequency [AF]: 26.68%). Histopathological re-examination of the surgical sample from the resected primary lung carcinoma revealed adenocarcinoma with partial squamous differentiation (less than 5%), which was partially positive for TTF-1, NapsinA, and CK5/6, focally positive for P40, and CK7 positive (Figures 2D–F). Sequencing results of the initial lung specimen demonstrated the same EGFR 19del (delE746_A750, AF: 80.37%) and EGFR amplification (copy number [CN]: 30).
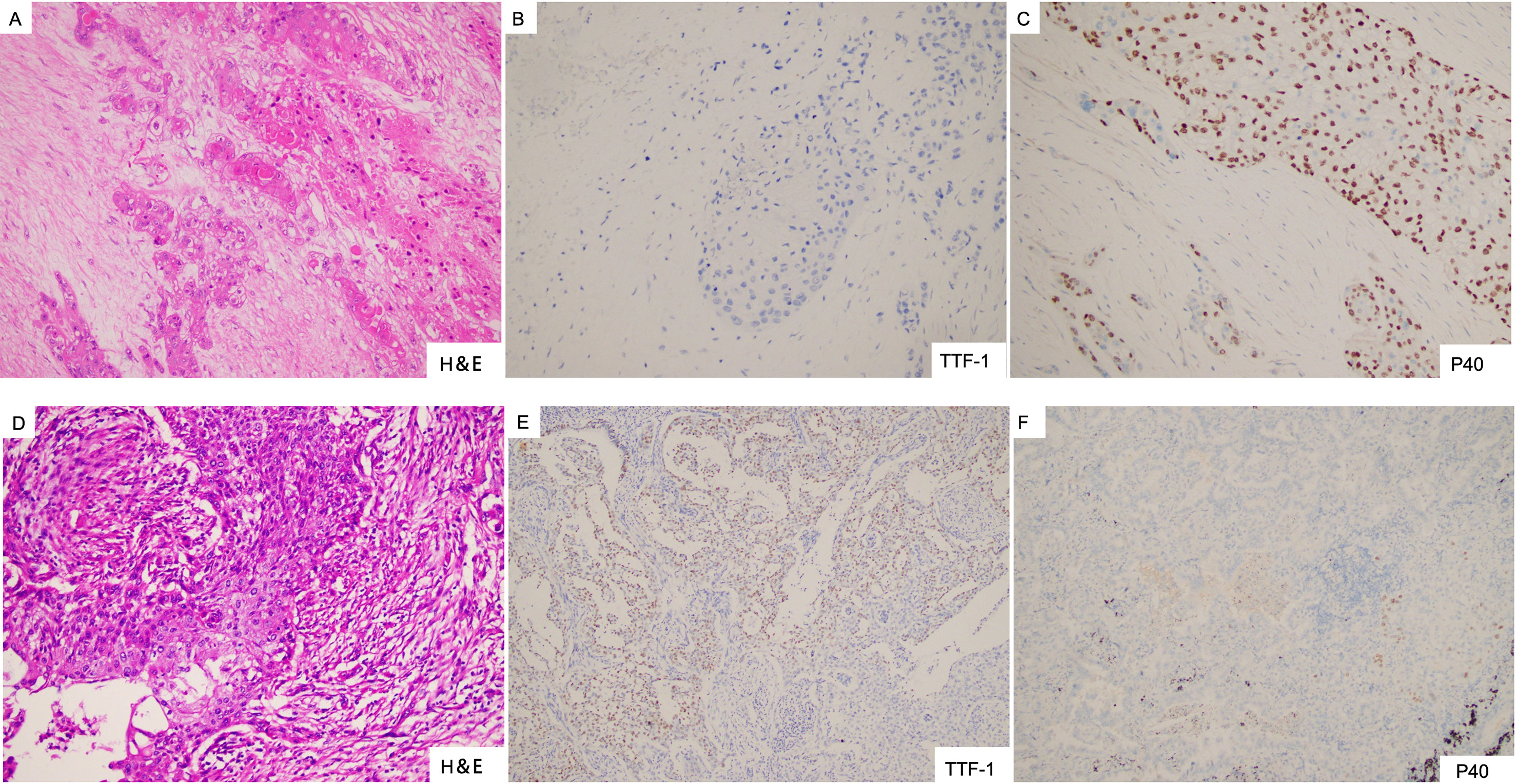
Figure 2 (A–C) Left adrenal gland specimen showing squamous cell carcinoma with negative staining for TTF-1 and partially positive staining for P40. (D–F) Resected lung sample showing adenocarcinoma with partial squamous differentiation, expressing focally positive TTF-1 and P40.
The timeline illustrating this patient’s medical history and treatment is presented in Figure 3. The patient is currently continuing almonertinib monotherapy and the disease is stable.
Discussion
The mechanisms underlying of ADC-SCC transformation during treatment with EGFR inhibitors remain unclear. A possible explanation is that ADC and SCC co-existed in the original tumor and only the SCC component progressed following after EGFR-TKI treatment (9). In this case, pathological and immunohistochemical results revealed the transformation from lung adenocarcinoma with partial squamous differentiation to metastatic SCC, which may support this assumption. There is also a possibility that pluripotent tumor stem cells acquire a divergent phenotype under the pressure of TKI (7). We considered a second primary tumor unlikely because the original EGFR deletion in exon 19 was maintained following the SCC transition in this patient.
Previous studies show that, live kinase B1 (LKB1) inactivation can promote gradual transition from lung ADC to SCC in mouse model (10), leading to drug resistance through metabolic alteration (11). Transition of ADC-SCC with disease progression was also observed in lung cancer patients treated with chemotherapy and immunotherapy (12, 13), indicating that ADC-SCC transition might be a common drug-resistance mechanism. To better understand the link between ADC-SCC transition and EGFR inhibition resistance, further experimental validation is required.
The simultaneous occurrence of ADC-SCC transformation and EGFR inhibition resistance is rare. To date, there have been only 22 reported cases including our patient, and their characteristics are summarized in Table 1. Based on the available information, most patients described were female (72.7%) and the median age was 62 years (range, 40 to 79 years). In most cases, the histological transition was found at the lung recurrence site. This case is unique to present the ADC-SCC transition in the adrenal gland metastasis, which has never been reported before.
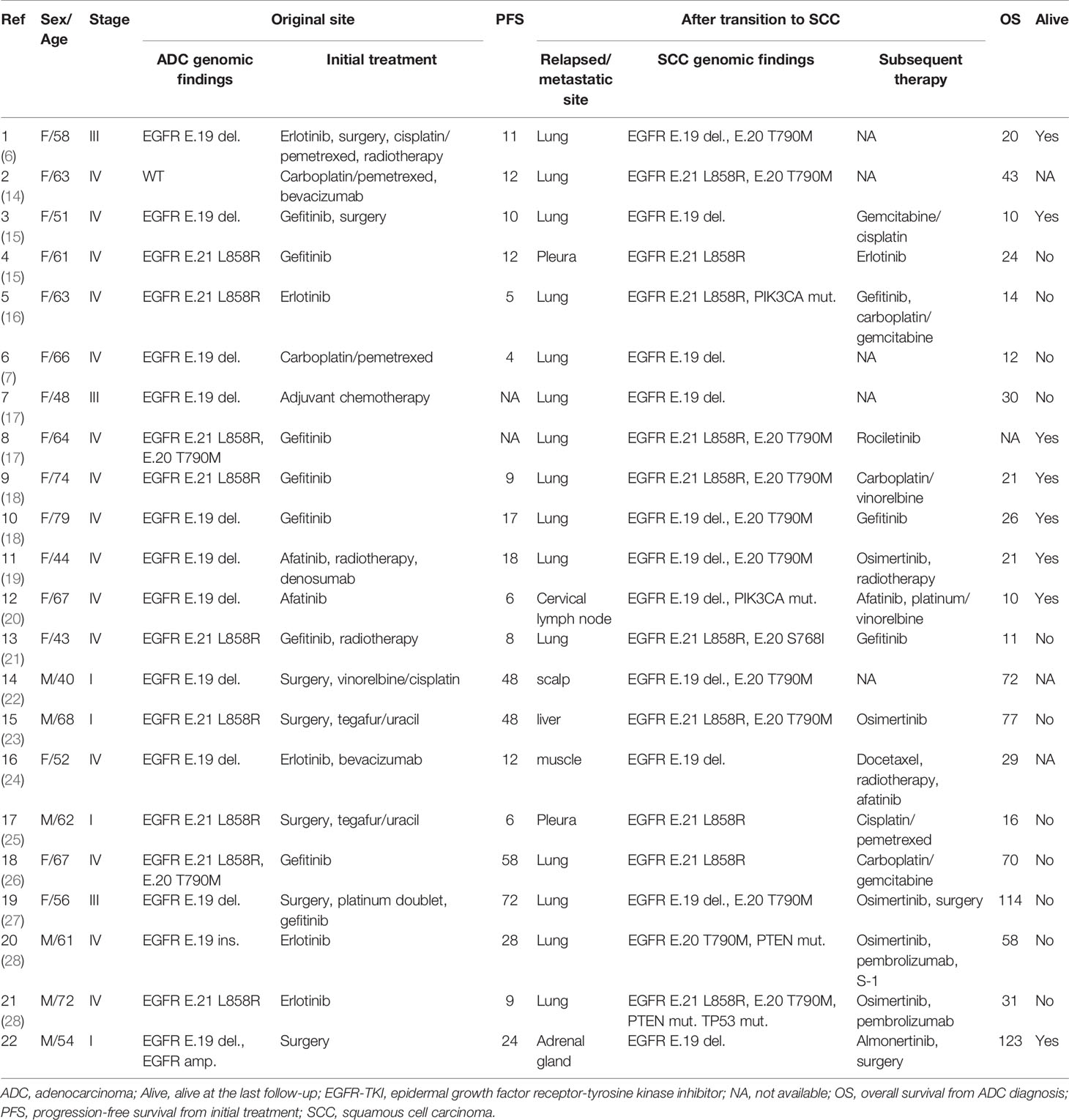
Table 1 Characteristics of patients with transition to SCC from primary lung ADC after EGFR-TKIs treatment.
According to Table 1, approximately half of the patients developed EGFR T790M as an acquired resistance mechanism to EGFR-TKI therapy. Other genomic alterations included the acquired mutations in EGFR S768I, PIK3CA, PTEN, TP53. We describe the first reported histologic evolution of ADC to SCC combined with the disappearance of EGFR amplification.
In this case, sequencing analysis of the primary lung carcinoma demonstrated EGFR deletion in exon 19 (AF: 80.37%) and EGFR amplification (CN: 30). There is evidence indicating that lung ADC patients with higher EGFR mutation abundance benefit more from EGFR-TKIs (29). Further, high EGFR copy number has been associated with better clinical outcomes in EGFR-mutant patients treated with EGFR-TKI (30, 31). Studies have shown that EGFR amplifications usually impact mutated but not wild-type alleles (31), which is likely to increase EGFR mutation abundance and render cancer cells more sensitive to EGFR inhibition. These may explain why the effectiveness of gefitinib and local radiotherapy was sustained for up to 48 months for the first metastasis in the right femoral head, and up to 32 months for the second metastasis in the mediastinal lymph nodes.
A limitation of this report was that no biopsy of the lesions was performed for the first and second metastases. Therefore, we cannot exclude the assumption that ADC-SCC transition had already occurred before the detection of the adrenal gland metastasis.
EGFR-mutated patients resistant to TKIs with a changed phenotype to SCC show poor prognosis with a median overall survival of only 3.5 months (26). The management of transformed SCC after TKI resistance is controversial. According to Table 1, selected treatment strategies include combining chemotherapy or radiotherapy, surgery, third-generation TKI, and immunotherapy. To date, this patient has been treated with almonertinib for 8 months with stable disease. Further studies in EGFR-mutant patients with TKI resistance and ADC-SCC transformation are needed to specify the underlying mechanisms and to optimize the individualized post-progression therapy.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics Statement
Ethical review and approval were not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
JW and JL designed the study drafted the manuscript. YL and CL collected and analyzed the patient data. QL and JL contributed to the literature research. JW reviewed and edited the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study was sponsored by the Natural Science Foundation of Shanghai (grant number: 19ZR1410400).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank Lifeng Wang (Dian Diagnostics) for critical but constructive comments on this paper.
Abbreviations
AF, allele frequency; ADC, adenocarcinoma; CT, computed tomography; CN, copy number; EGFR, epidermal growth factor receptor; MRI, magnetic resonance imaging; SCC, squamous cell carcinoma; TKI, tyrosine kinase inhibitor.
References
1. Lynch TJ, Bell DW, Sordella R, Gurubhagavatula S, Okimoto RA, Brannigan BW, et al. Activating Mutations in the Epidermal Growth Factor Receptor Underlying Responsiveness of Non-Small-Cell Lung Cancer to Gefitinib. New Engl J Med (2004) 350(21):2129–39. doi: 10.1056/NEJMoa040938
2. Shepherd FA, Rodrigues Pereira J, Ciuleanu T, Tan EH, Hirsh V, Thongprasert S, et al. Erlotinib in Previously Treated Non-Small-Cell Lung Cancer. New Engl J Med (2005) 353(2):123–32. doi: 10.1056/NEJMoa050753
3. Riely GJ, Yu HA. Egfr: The Paradigm of an Oncogene-Driven Lung Cancer. Clin Cancer Res an Off J Am Assoc Cancer Res (2015) 21(10):2221–6. doi: 10.1158/1078-0432.Ccr-14-3154
4. Sequist LV, Waltman BA, Dias-Santagata D, Digumarthy S, Turke AB, Fidias P, et al. Genotypic and Histological Evolution of Lung Cancers Acquiring Resistance to EGFR Inhibitors. Sci Trans Med (2011) 3(75):75ra26. doi: 10.1126/scitranslmed.3002003
5. Yu HA, Arcila ME, Rekhtman N, Sima CS, Zakowski MF, Pao W, et al. Analysis of Tumor Specimens At the Time of Acquired Resistance to EGFR-TKI Therapy in 155 Patients With EGFR-Mutant Lung Cancers. Clin Cancer Res an Off J Am Assoc Cancer Res (2013) 19(8):2240–7. doi: 10.1158/1078-0432.Ccr-12-2246
6. Scher KS, Saldivar JS, Fishbein M, Marchevsky A, Reckamp KL. EGFR-Mutated Lung Cancer With T790M-Acquired Resistance in the Brain and Histologic Transformation in the Lung. J Natl Compr Cancer Netw JNCCN (2013) 11(9):1040–4. doi: 10.6004/jnccn.2013.0126
7. Levin PA, Mayer M, Hoskin S, Sailors J, Oliver DH, Gerber DE. Histologic Transformation From Adenocarcinoma to Squamous Cell Carcinoma as a Mechanism of Resistance to EGFR Inhibition. J Thorac Oncol (2015) 10(9):e86–e8. doi: 10.1097/JTO.0000000000000571
8. Soria JC, Felip E, Cobo M, Lu S, Syrigos K, Lee KH, et al. Pathological Transition as the Arising Mechanism For Drug Resistance In Lung Cancer. Cancer Commun (2015) 16(8):897–907. doi: 10.1016/s1470-2045(15)00006-6
9. Hou S, Zhou S, Qin Z, Yang L, Han X, Yao S, et al. Evidence, Mechanism, and Clinical Relevance of the Transdifferentiation From Lung Adenocarcinoma to Squamous Cell Carcinoma. Am J Pathol (2017) 187(5):954–62. doi: 10.1016/j.ajpath.2017.01.009
10. Han X, Li F, Fang Z, Gao Y, Li F, Fang R, et al. Transdifferentiation of Lung Adenocarcinoma in Mice With Lkb1 Deficiency to Squamous Cell Carcinoma. Nat Commun (2014) 5:3261. doi: 10.1038/ncomms4261
11. Li F, Han X, Li F, Wang R, Wang H, Gao Y, et al. Lkb1 Inactivation Elicits a Redox Imbalance to Modulate Non-Small Cell Lung Cancer Plasticity and Therapeutic Response. Cancer Cell (2015) 27(5):698–711. doi: 10.1016/j.ccell.2015.04.001
12. Le T, Sailors J, Oliver DH, Mayer M, Hoskin S, Gerber DE. Histologic Transformation of EGFR Mutant Lung Adenocarcinoma Without Exposure to EGFR Inhibition. Lung Cancer (2017) 105:14–6. doi: 10.1016/j.lungcan.2017.01.005
13. Hsu CL, Chen KY, Kuo SW, Chang YL. Histologic Transformation in a Patient With Lung Cancer Treated With Chemotherapy and Pembrolizumab. J Thorac Oncol (2017) 12(6):e75–e6. doi: 10.1016/j.jtho.2017.02.006
14. Bugano DDG, Kalhor N, Zhang J, Neskey M, William WN. Squamous-Cell Transformation in A Patient With Lung Adenocarcinoma Receiving Erlotinib: Co-occurrence With T790M Mutation. Cancer Treat Commun (2015) 4:34–6. doi: 10.1016/j.ctrc.2015.03.007
15. Hsieh MS, Jhuang JY, Hua SF, Chou YH. Histologic Evolution From Adenocarcinoma to Squamous Cell Carcinoma After Gefitinib Treatment. Ann Thoracic Surg (2015) 99(1):316–9. doi: 10.1016/j.athoracsur.2014.02.075
16. Kuiper JL, Ronden MI, Becker A, Heideman DA, van Hengel P, Ylstra B, et al. Transformation to a Squamous Cell Carcinoma Phenotype of an EGFR-Mutated NSCLC Patient After Treatment With An EGFR-tyrosine Kinase Inhibitor. J Clin Pathol (2015) 68(4):320–1. doi: 10.1136/jclinpath-2015-202866
17. Haratani K, Hayashi H, Watanabe S, Kaneda H, Yoshida T, Takeda M, et al. Two Cases of EGFR Mutation-Positive Lung Adenocarcinoma That Transformed Into Squamous Cell Carcinoma: Successful Treatment of One Case With Rociletinib. Ann Oncol (2016) 27(1):200–2. doi: 10.1093/annonc/mdv495
18. Jukna A, Montanari G, Mengoli MC, Cavazza A, Covi M, Barbieri F, et al. Squamous Cell Carcinoma “Transformation” Concurrent With Secondary T790m Mutation in Resistant Egfr-Mutated Adenocarcinomas. J Thorac Oncol (2016) 11(4):e49–51. doi: 10.1016/j.jtho.2015.12.096
19. Bruno R, Proietti A, Alì G, Puppo G, Ribechini A, Chella A, et al. Squamous Cell Transformation and EGFR T790M Mutation as Acquired Resistance Mechanisms in a Patient With Lung Adenocarcinoma Treated With A Tyrosine Kinase Inhibitor: A Case Report. Oncol Lett (2017) 14(5):5947–51. doi: 10.3892/ol.2017.6913
20. Clery E, Pisapia P, Feliciano S, Vigliar E, Marano A, De Luca C, et al. There is Still A Role for Cytology in the ‘Liquid Biopsy’ Era. A Lesson From a TKI-Treated Patient Showing Adenocarcinoma to Squamous Cell Carcinoma Transition During Disease Progression. J Clin Pathol (2017) 70(9):798–802. doi: 10.1136/jclinpath-2017-204370
21. Longo L, Mengoli MC, Bertolini F, Bettelli S, Manfredini S, Rossi G. Synchronous Occurrence of Squamous-Cell Carcinoma “Transformation” and EGFR Exon 20 S768I Mutation as a Novel Mechanism of Resistance in EGFR-Mutated Lung Adenocarcinoma. Lung Cancer (2017) 103:24–6. doi: 10.1016/j.lungcan.2016.11.012
22. Park HK, Seo Y, Choi YL, Ahn MJ, Han J. Metastatic Squamous Cell Carcinoma From Lung Adenocarcinoma After Epidermal Growth Factor Receptor Tyrosine Kinase Inhibitor Therapy. J Pathol Trans Med (2017) 51(4):441–3. doi: 10.4132/jptm.2016.10.18
23. Izumi H, Yamasaki A, Ueda Y, Sumikawa T, Maeta H, Nakamoto S, et al. Squamous Cell Carcinoma Transformation From EGFR-Mutated Lung Adenocarcinoma: A Case Report and Literature Review. Clin Lung Cancer (2018) 19(1):e63–e6. doi: 10.1016/j.cllc.2017.10.005
24. Sato M, Matsui A, Shimoyama Y, Omote N, Morise M, Hase T, et al. An EGFR-Mutated Lung Adenocarcinoma Undergoing Squamous Cell Carcinoma Transformation Exhibited A Durable Response to Afatinib. Internal Med (Tokyo Japan) (2018) 57(23):3429–32. doi: 10.2169/internalmedicine.0999-18
25. Shinohara S, Ichiki Y, Fukuichi Y, Honda Y, Kanayama M, Taira A, et al. Squamous Cell Carcinoma Transformation From Adenocarcinoma as An Acquired Resistance After the EGFR TKI Therapy in (EGFR-Mutated) Non-Small Cell Lung Cancer. J Thorac Dis (2018) 10(7):E526–E31. doi: 10.21037/jtd.2018.06.83
26. Roca E, Pozzari M, Vermi W, Tovazzi V, Baggi A, Amoroso V, et al. Outcome of EGFR-Mutated Adenocarcinoma NSCLC Patients With Changed Phenotype to Squamous Cell Carcinoma After Tyrosine Kinase Inhibitors: A Pooled Analysis With an Additional Case. Lung Cancer (2019) 127:12–8. doi: 10.1016/j.lungcan.2018.11.016
27. Haruki T, Nakanishi A, Matsui S, Kidokoro Y, Kubouchi Y, Takagi Y, et al. Transformation From Adenocarcinoma to Squamous Cell Carcinoma Associated With Long-Term Administration of EGFR-Tkis. Mol Clin Oncol (2020) 13(6):82. doi: 10.3892/mco.2020.2152
28. Uruga H, Fujii T, Nakamura N, Moriguchi S, Kishi K, Takaya H. Squamous Cell Transformation as A Mechanism of Acquired Resistance to Tyrosine Kinase Inhibitor in EGFR-mutated Lung Adenocarcinoma: A Report of Two Cases. Respirol Case Rep (2020) 8(2):e00521. doi: 10.1002/rcr2.521
29. Zhou Q, Zhang XC, Chen ZH, Yin XL, Yang JJ, Xu CR, et al. Relative Abundance of EGFR Mutations Predicts Benefit From Gefitinib Treatment for Advanced Non-Small-Cell Lung Cancer. J Clin Oncol Off J Am Soc Clin Oncol (2011) 29(24):3316–21. doi: 10.1200/jco.2010.33.3757
30. Ruiz-Patino A, Castro CD, Ricaurte LM, Cardona AF, Rojas L, Zatarain-Barron ZL, et al. Egfr Amplification and Sensitizing Mutations Correlate With Survival in Lung Adenocarcinoma Patients Treated With Erlotinib (Mutp-Clicap). Target Oncol (2018) 13(5):621–9. doi: 10.1007/s11523-018-0594-x
Keywords: lung adenocarcinoma, histological transformation, resistance to gefitinib, EGFR mutation, EGFR amplification, targeted therapy
Citation: Liao J, Li Y, Liu C, Long Q and Wang J (2021) Case Report: EGFR-Positive Early-Stage Lung Adenocarcinoma Transforming to Squamous Cell Carcinoma After TKI Treatment. Front. Oncol. 11:696881. doi: 10.3389/fonc.2021.696881
Received: 18 April 2021; Accepted: 24 May 2021;
Published: 08 June 2021.
Edited by:
Mantang Qiu, Peking University People’s Hospital, ChinaReviewed by:
Rong Yin, Jiangsu Key Laboratory of Molecular and Translational Cancer Research, ChinaPaola Massimi, International Centre for Genetic Engineering and Biotechnology, Italy
Copyright © 2021 Liao, Li, Liu, Long and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jialei Wang, bHV3YW5namlhbGVpQDEyNi5jb20=
 Jiatao Liao1,2
Jiatao Liao1,2 Yuan Li
Yuan Li Jialei Wang
Jialei Wang