- 1Bone Marrow Transplantation Program, Department of Internal Medicine, American University of Beirut Medical Center, Beirut, Lebanon
- 2Cancer Research Institute, Department of Internal medicine, Hematology/Oncology Division, American University of Beirut Medical Center, Beirut, Lebanon
- 3Faculty of Sciences, Lebanese University, Beirut, Lebanon
- 4Department of Nursing, Naef. K. Basile Cancer Institute, American University of Beirut Medical Center, Beirut, Lebanon
- 5Division of Hematology/Oncology, Department of Internal Medicine, American University of Beirut Medical Center, Beirut, Lebanon
Background: The Coronavirus Disease 2019 (COVID-19) was declared a pandemic by WHO in March 2020. The first case of COVID-19 was identified in Lebanon on the 21st of February 2020, amid a national economic crisis. As the numbers of cases increased, ICU admissions and mortality rose, which led hospitals across Lebanon to take certain safety measures to contain the virus. The Naef K. Basile Cancer Institute (NKBCI) at the American University of Beirut Medical Center handles oncology outpatient visits and outpatient treatment protocol infusions. The aim of this study is to evaluate the efficacy of the safety measures put forth by the NKBCI early in the pandemic.
Methods: Oncology patients are amongst the immunosuppressed population, who are at greatest risk of contracting COVID-19 and consequently suffering its complications. In this manuscript, we evaluated the precautionary measures implemented at the NKBCI of AUBMC from March 1st to May 31st of 2020, by surveying oncology patients on the telephone who had live and virtual appointments in both the oncology outpatient clinics and infusion unit. We conducted a prospective study of 670 oncology patients who had appointments at the NKBCI during this period and used their answers to draw responses about patient satisfaction towards those safety measures.
Results: Our results involved 387 responses of oncology patients who visited the NKBCI during the period of March 1st to May 31st of 2020. 99% of our respondents gave a rating of good to excellent with these new measures. The option of online consultation was given to 35% in the hematology group compared to 19% in those with solid tumors (p=0.001). From the total, 15% of patients opted for the telemedicine experience as a new implemented strategy to provide patient-centered medical care. Of this group of patients, 22% faced problems with connectivity and 19% faced problems with online payment.
Conclusion: NKBCI was competent in following the WHO guidelines in protecting the oncology patient population. Feedback collected from the surveys will be taken into account by the committee of the NKBCI to develop new safety measures that can better control viral spread while providing patient-centered medical care.
Introduction
On February 21, 2020, the first case of coronavirus disease 2019 (COVID-19) was identified in Lebanon. This occurred amid a backdrop of political and economic turmoil that began in October 2019, when a banking crisis and a civil uprising pushed the country into an economic crisis (1). By mid-March, when the infection count reached 99 cases, the government declared “public mobilization,” issued stay-at-home orders, and closed the borders, with full lockdown of nonessential services (1). [Graph demonstrating the prevalence of COVID-19 in Lebanon during the period of early outbreak of February – June illustrated in annex (2)].
The Coronavirus Disease 2019 (COVID-19) was first recognized in December 2019 in Wuhan, China after reported cases of clusters of viral pneumonia (3). This respiratory virus causes a mild respiratory illness in 81% of affected patients, whereas 14% develop a severe illness requiring hospitalization with supplemental oxygen, and 5% progress to respiratory failure with multi-organ dysfunction (3–6).
Elderly patients, and those with comorbidities have been reported to be at a higher risk of mortality and morbidity once infected (7). Oncology patients, who are more often than not, immunosuppressed as a result of treatment from their primary disease, are at a greater risk of developing severe complications to the COVID-19 infection, with a 4-7 (average 5.6%) proposed case fatality rate (7). Cancer patients were suggested to be at a 3.5 times higher risk of severe COVID-19 disease compared to the general population (7, 8). The receipt of chemotherapy or cancer surgery was shown to be a risk factor for ICU admissions, intensive ventilation and death in COVID-19 patients (8). However, many oncology patients are postponing their clinic visits and treatment sessions due to fear of contracting the virus in overcrowded areas of the hospitals, which may hinder their care and treatment plans (9, 10).
In this manuscript, we conducted a study to address the preparation of the American University of Beirut Medical Center Oncology clinics and infusion unit, to face the COVID- 19 pandemic during the first three months of the outbreak. The Naef K. Basile Cancer Institute (NKBCI) is part of the American University of Beirut Medical Center (AUBMC). The institute handles oncology outpatient visits including outpatient chemotherapy and other regular treatment protocol infusions. AUBMC, and in turn NKBCI, are centers of care to multiple patients residing inside and outside of Lebanon.
The issuance of temporary restrictions on travel within and between countries to limit the spread of the virus has affected cancer patients seeking essential medical care. The aforementioned has blurred the lines between two healthcare necessities, protecting vulnerable cancer patients from COVID-19 and providing medical help against their disease. The NKBCI had taken additional COVID-19 response measures, along with those already implemented by AUBMC, to precisely cater to the needs of vulnerable cancer patients.
The aim of this study is to assess the measures implemented by the Hematology and Oncology Division at AUBMC, a tertiary care center in Lebanon against the challenges posed by the COVID-19 pandemic, and to incorporate the feedback of patients into the future development of these measures to better contain the virus. These measures and modifications include but are not limited to clinic interventions, remote work, patient-centered modifications, staff operations, public communication and cancer funds.
Modifications in clinic interventions include screening patients regarding recent travel and interaction with a COVID-19 infected individual ahead of their appointments, deferring appointments of patients who had recently traveled or were in contact with a COVID-19 patient and limiting entry into ACC (AUBMC Halim and Aida Daniel Academic and Clinical Center) to a single door with temperature checkpoints. Modifications in remote work include providing online consultations through WEBEX as an alternative to Hematology and Oncology clinic visits and providing physicians with remote access to hold meetings through WEBEX. Multidisciplinary tumor boards are being held in the same manner.
Patient-centered modifications include designating a separate visitor elevator to oncology patients entering ACC, laying floor markings to ensure a minimum of 2 m distance between individuals at the clinic and infusion unit check in and checkout points, decreasing the number of allowed visitors accompanying patients and deferring non-acute autologous BMT patients.
Modifications in staff operations include reducing the number of personnel in the medical team visiting the patients, emphasizing the use of PPE, appropriate hand hygiene and disinfection (4, 5, 10) and allowing staff to work from home. Public communication include live Facebook interviews to educate oncology patients and updates on AUBMC’s website about COVID-19 precautions. Modifications in NKBCI cancer funds include supporting as many outpatients and inpatients as possible.
Methodology
This is a prospective study conducted in the NKBCI of AUBMC on patients who visited the outpatient clinics and infusion unit during the first three months of the outbreak. IRB approval was received on July 3rd, 2020. The primary objective of the study includes evaluating the effectiveness of precautionary strategies implemented at NKBCI to reduce risk of COVID-19 infections amongst patients and health care workers. The secondary objective of the study includes incorporating feedback from patients to improve precautionary measures against COVID-19 in the future.
The inclusion criteria include all patients who have had an appointment at the NKBCI (clinics and infusion units) between March 1st and May 31st of 2020. Online and in-person appointments were included. There were no exclusion criteria. Many of these patients have chronic conditions and therefore had repeat appointments during these three months, as well as follow up visits after June.
Patients were identified from the AUBMC records of patients who have visited the NKBCI outpatient clinic and infusion unit through the HIS portal on (https://his.aub.edu.lb/). Each patient’s primary physician was contacted and informed of the study prior to approaching their patient. The primary physician or their nurse contacted the patients, introduced them to the study and got their willingness to participate, after which the research team proceeded with reaching out to the patients.
A 20-question survey was created in English and translated to Arabic and French. It was administered to identified patients after their verbal consent had been taken over the telephone. The patients were given the option to either fill the survey over the phone or online through Limesurvey based on their preferences. Those 20 questions were developed by the committee responsible for the new safety measures in NKBCI, in accordance with WHO guidelines in effectively controlling viral transmission (4, 5, 11). Co-authors piloted the design and checked the feasibility and validity of the questions.
The surveys were conducted over the telephone, in a quiet and private environment in the NKBCI Research Office, with a single research member involved in the phone call. These surveys were conducted by one postdoctoral research fellow at the NKBCI, one nurse at the NKBCI, one volunteering doctor at AUBMC and one volunteering student. Individual informed consent was obtained during the period of July 20th, 2020 to September 18th, 2020. Answers were collected on a standardized excel sheet that comprised the survey questionnaire. [Survey Questionnaire (20 questions) illustrated in annex].
Ethical Considerations
The Institutional Review Board at the American University of Beirut approved the study. The participants provided oral and written consent to participate in the study. The study does not involve any diagnostic or therapeutic intervention and there was no risk of harm to the patients. When consenting patients, the research assistant explained to them that study participation was merely for observational purposes and there was no influence on their future management in the hospital.
Statistical Analysis
Following the completion of the surveys on all the respondents, the information was collected, and a simple descriptive analysis was performed. This was done using proportions and percentages for categorical variables and means and medians for continuous variables.
Numerical variables were summarized by their median, mean, standard deviation and range. Questionnaires variables were binary and restricted to yes/no answers; these categorical variables were described by counts and relative frequencies.
Crosstabs in the form of 2x2 tables were plotted to identify correlations of all variables collected in the questionnaire to be compared by visit time, gender, Hematology Patient and residence. The chi square test was referred to for correlations between categorical variables; alternatively, Fischer exact test was used when tables had cells with low counts.
Analysis was performed using SPSS software IBM v.25; a p value < 0.05 was considered statistically significant in all analyses.
Results
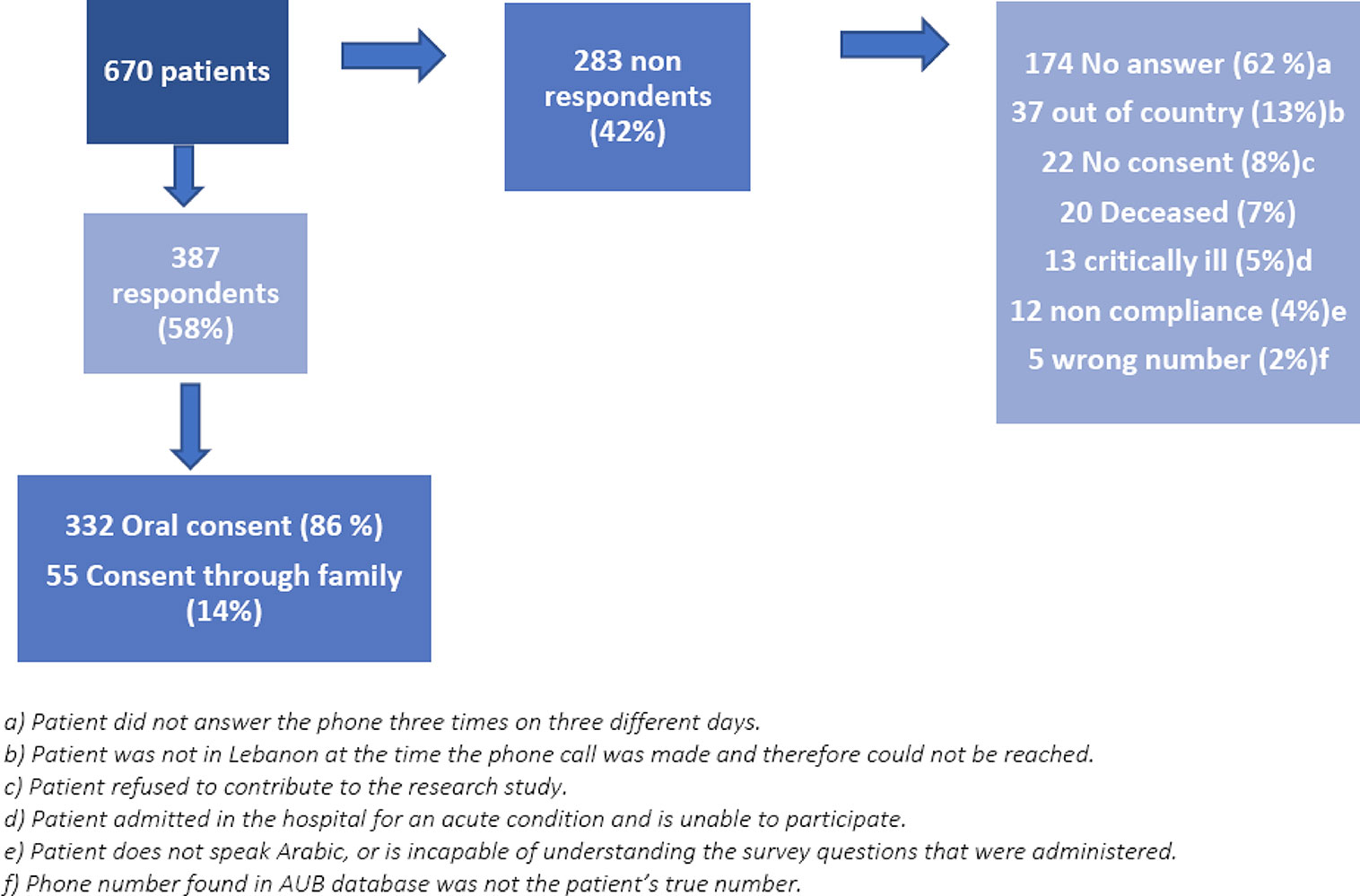
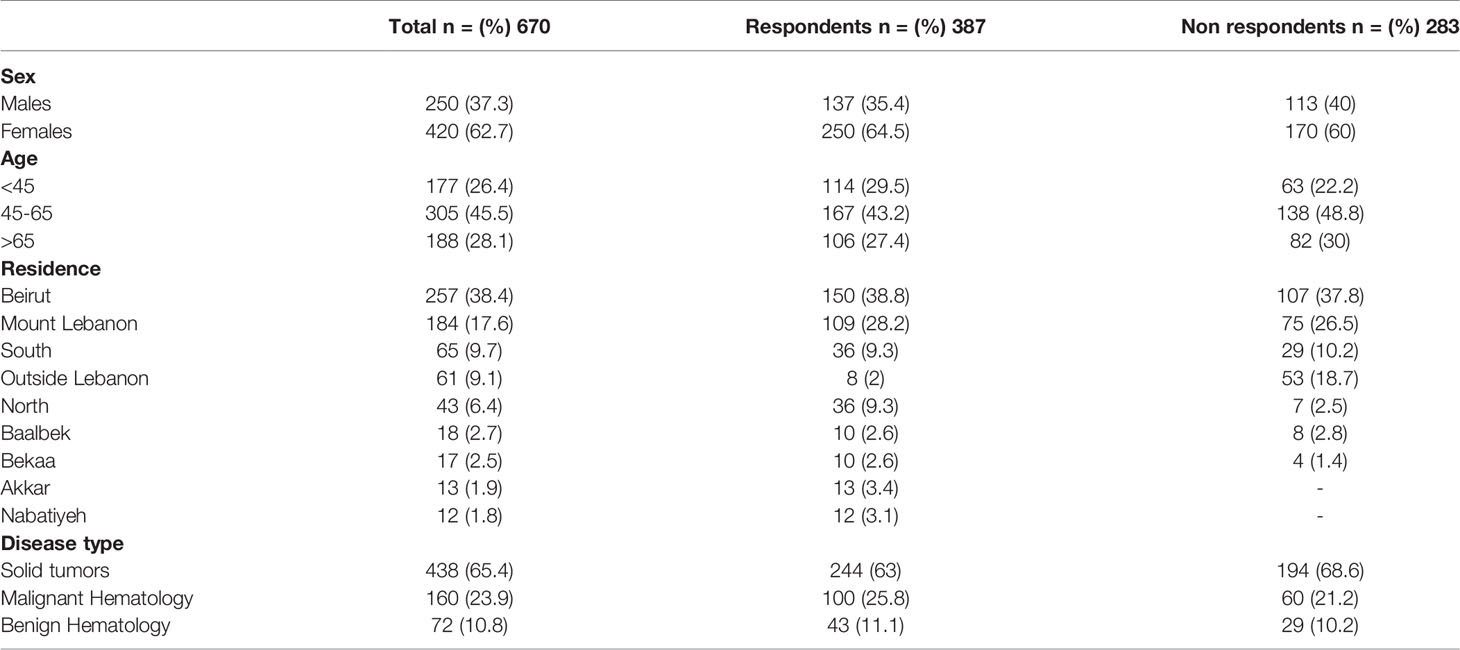
A total of 670 patients who had live and online appointments at the NKBCI (clinics and infusion unit) between March 1st and May 31st, 2020, were contacted; however, only a total of 387 responses were received (Figure 1). [Patient characteristics illustrated in Table 1].
Most respondents had visited the NKBCI during March (195, 50%); Lebanon’s first nation-wide lockdown was implemented during that same month in light of increasing COVID-19 infections. The increased numbers seen in March were prior to the strict precautionary regulations implemented by both the hospital and the country, when patients and staff were less concerned about the virus. [Prevalence of visitors across March, April, May, during the early outbreak illustrated in annex].
Most patients’ ages ranged between 45 and 65 years of age (167, 43%) with a mean age of 55 years. [Distribution of age ranges across respondents illustrated in annex].
The higher numbers seen in March can be attributed to the less strict measures taken prior to the peak of the pandemic, and the less vigilance amongst patients and health care workers. Lebanon’s first nation-wide lockdown was implemented during that same month in light of increasing COVID-19 infections. The higher ratio of women to men can be attributed to the greater prevalence of breast cancer amongst oncology diagnoses, compared to other malignancies. Also, women are more willing to participate in surveys and give feedback. [Distribution of sex ratio amongst respondents illustrated in annex].
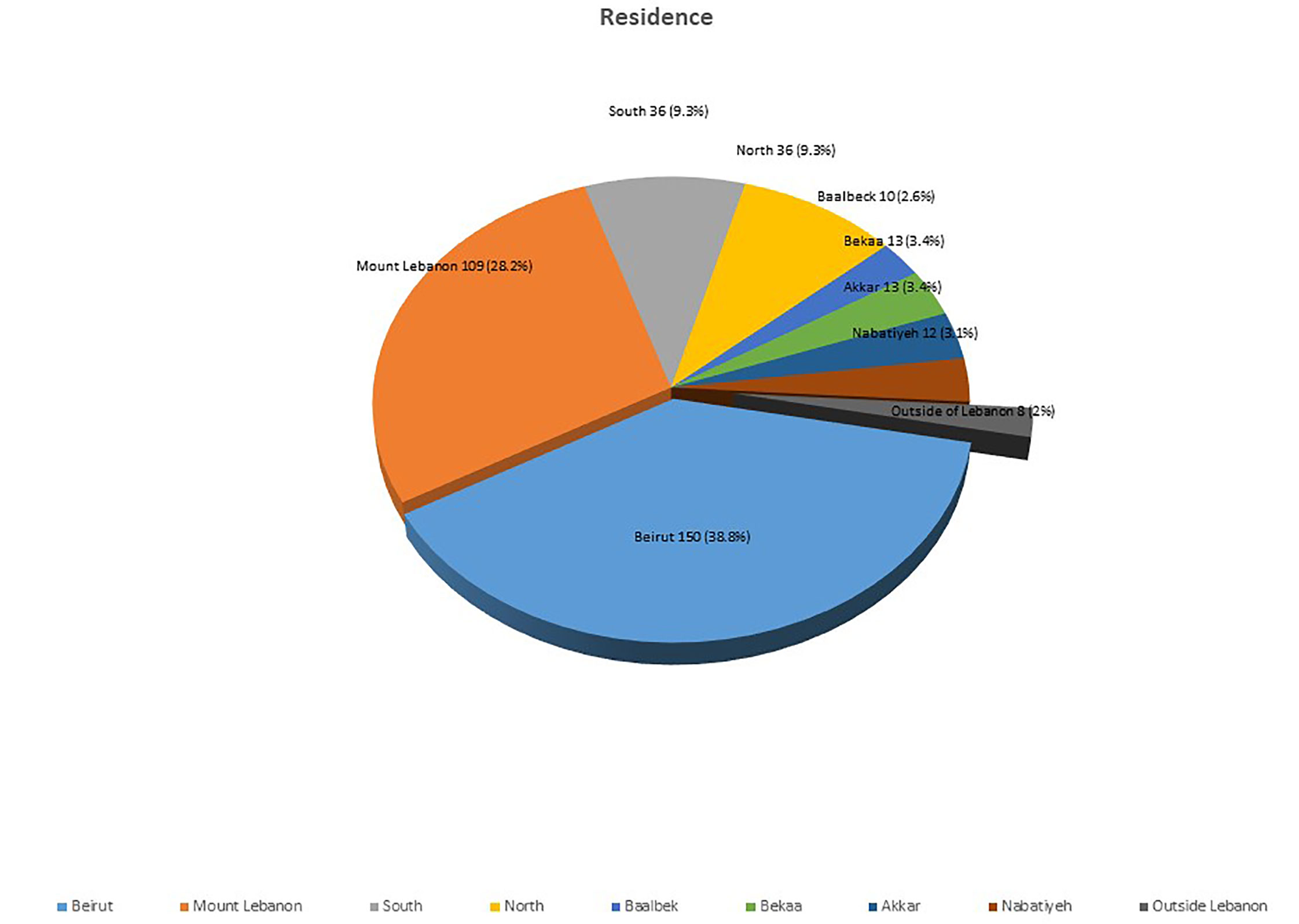
370, 98% of respondents were scattered throughout Lebanon, with the remaining 8 (2%) of respondents having a primary residence outside of Lebanon. Interestingly, the majority of patients reside in Beirut (150, 39%) and Mount Lebanon (109, 28%). The small number of 2% of respondents being outside of Lebanon raises the issue of how the COVID-19 pandemic has placed travel restrictions on Lebanese living abroad and foreigners who usually travel to Lebanon to seek health care and cancer treatment. [Primary residence of respondents illustrated in Figure 2].
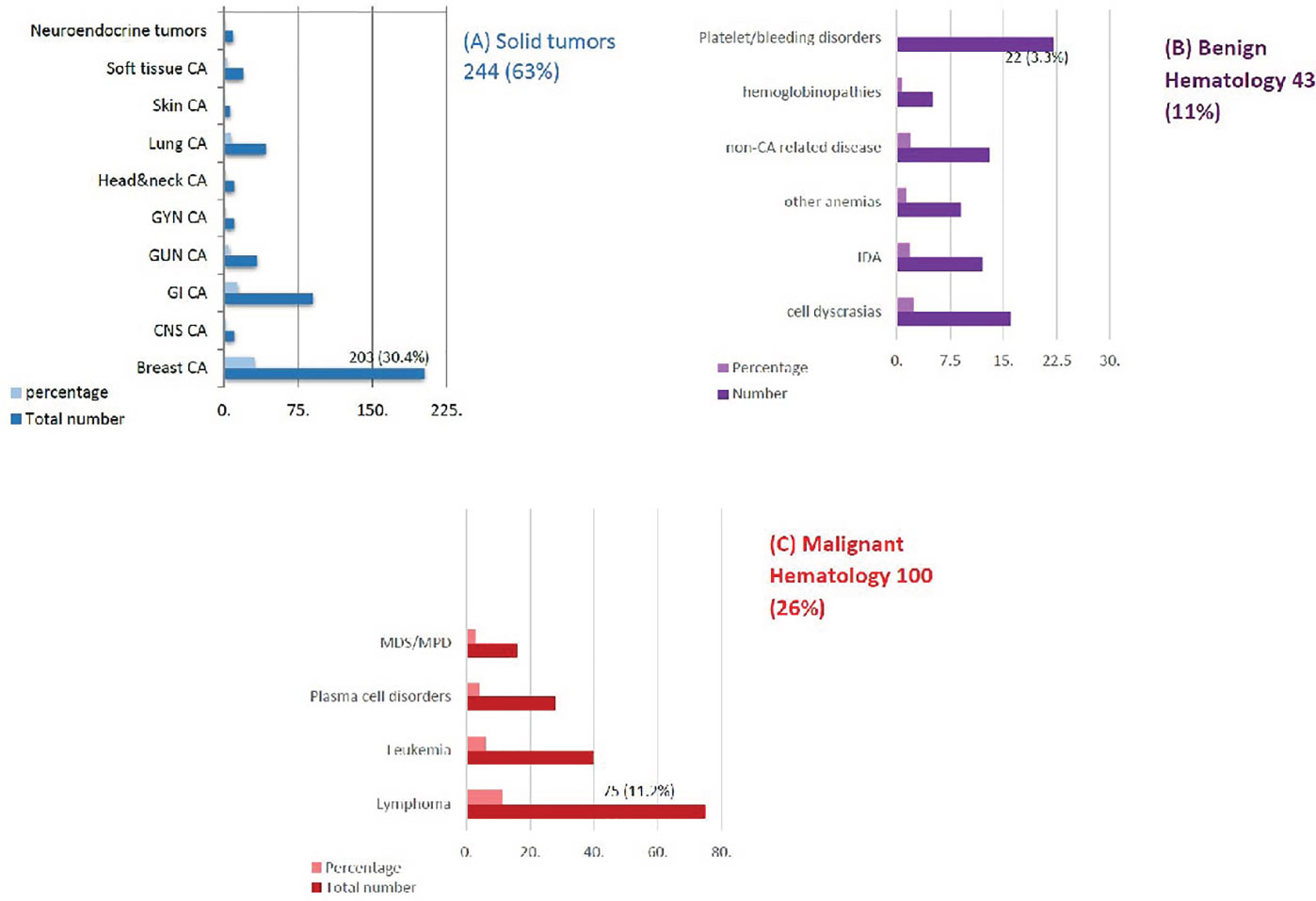
The patients’ respective primary diseases were identified; solid tumor patients comprised the largest patient cluster at 244 (63%) followed by benign and malignant hematology at 43 (11%) and 100 (26%), respectively. [Classification of Oncology Diagnoses of respondents at NKBCI illustrated in Figure 3].
Survey questionnaire results with values of positive and negative respondents (20 questions) illustrated in Table 2.
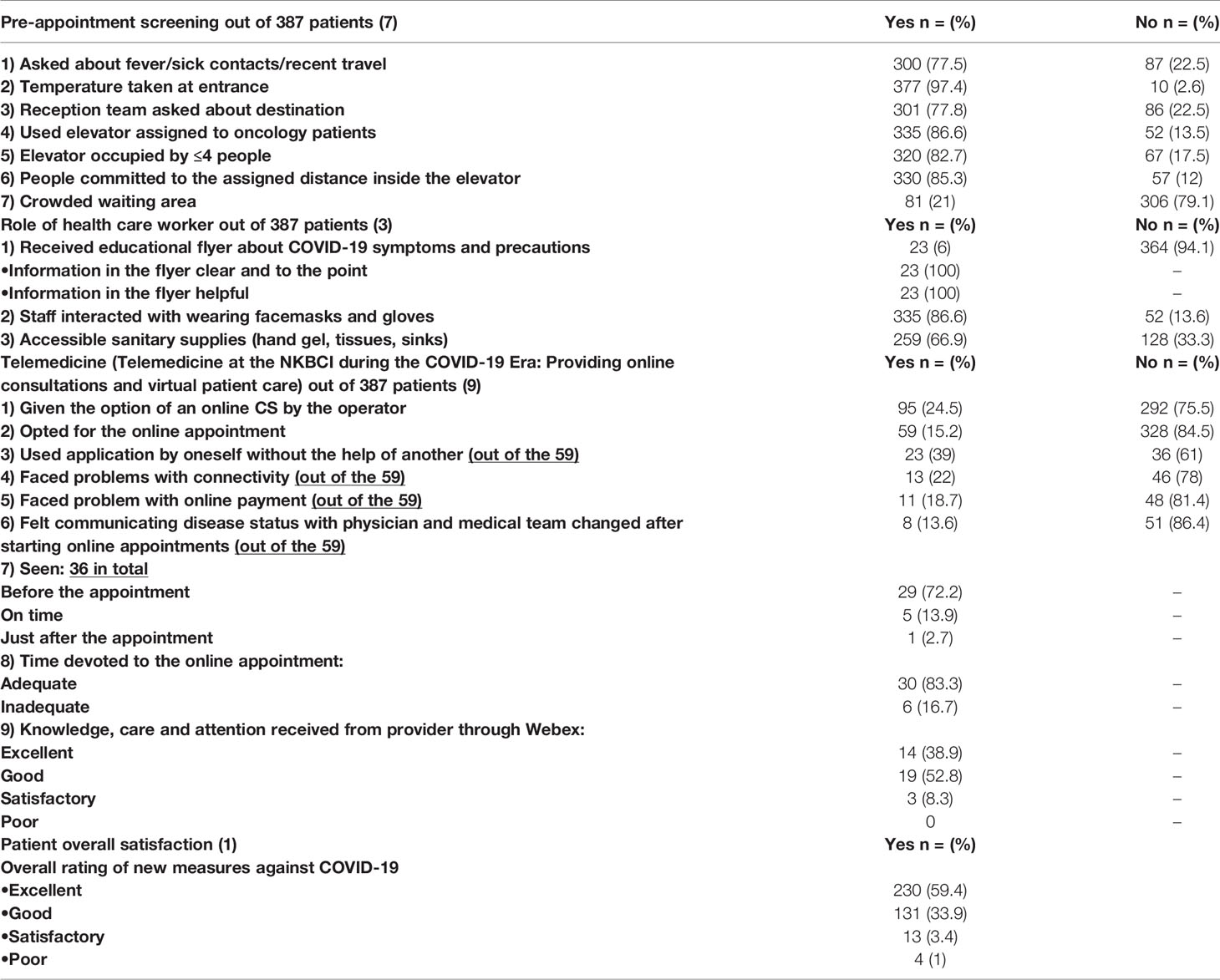
Table 2 Survey questionnaire results with values of positive and negative respondents (20 questions).
The majority of respondents reported being screened for travel history, fever or sick contacts prior to their appointments (300, 78%). An overwhelming majority noted passing through a temperature check before entering the NKBCI (377, 97%). Most patients used the elevator reserved for oncology patients (335, 86.6%), and noted a successful implementation of social distancing in that relatively small space. A relatively significant proportion mentioned overcrowding in waiting areas (81, 21%). A few received a COVID-19 educational pamphlet (23, 6%), 100% of whom found the information clear and helpful.
52, 14% stated that staff was not wearing facemasks and gloves, and close to 130, 34% denied the presence of accessible sanitary supplies including hand sanitizers, tissues, sinks or soap. A quarter of respondents was offered the option of an online consultation (95, 25%) and close to two thirds of those patients chose that option (59, 15%). Of those respondents, half were comfortable using the application by themselves (23, 39%), but close to one-third found trouble with connectivity (13, 22%) and payment (11, 19%) and noted a negative change in communicating their disease with their physician (8, 14%). [Demonstration of positive and negative feedback by respondents illustrated in annex].
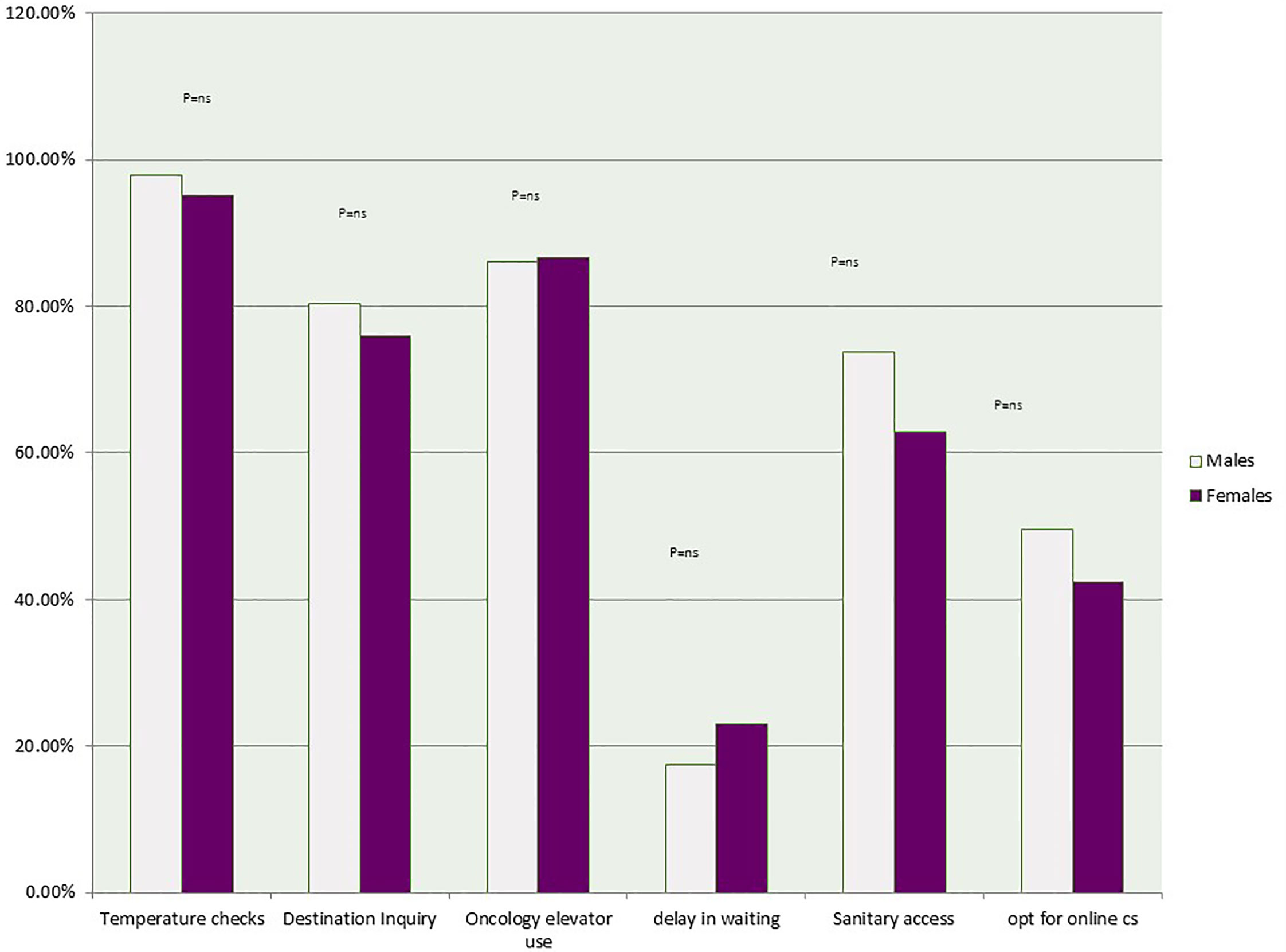
Males reported better pre-appointment measures compared to females, with 98% in temperature checking, 80% in being asked about their destination (compared to 95% and 76% respectively in females). Females reported greater use of specified oncology elevators (87% compared to 86% in males) and greater waiting times (23% compared to 18% in males). There was no statistical difference in relation to sex ratio and pre-appointment measures. Females reported that they had a harder time accessing sanitary supplies compared to males (63% vs 74% in males).
Females in this study were less likely to opt for the online appointment (at 42% compared to 50% in males). This could be attributed to the vast majority of breast cancer patients at NKBCI that need physical examinations. The greater numbers seen with female dissatisfaction compared to males could be due to the greater willingness of females to give detailed feedback to improve measures on the phone, the fact that most females bring along with them hand gel and tissues and therefore are less vigilant to sanitary supplies around them and that most females would prefer physical encounters rather than online consultations in the category of breast cancer population.
[Demonstration of precautionary strategies implemented by NKBCI as per sex difference illustrated in Figure 4].
Discussion
As of July, Lebanon has faced an exponential increase in COVID-19 positive cases. There have been approximately 85,000 cases and 670 deaths in the first few months of the pandemic (12). Interpretation of the data yielded results that can be used to evaluate the efficacy of the new safety measures at AUBMC. This study focused on the Naef K. Basile Cancer Institute at AUBMC, which provides medical care to Hematology and Oncology patients. Given the vulnerability of the oncology patient population, extra measures had been made effective at the NKBCI to ensure patient safety and to avoid COVID-19 infections as well as the fatal complication sequelae that can arise. Though we have no direct measure of the effectiveness of these measures on our population, there is an overall sense of adequate compliance. None of the patients was infected with COVID-19 at the time of the survey. 2 patients (0.5%) had tested positive for COVID-19 during the early outbreak of the virus and not when the study was conducted, with only mild symptoms and no hospital admissions. One patient was a 54-year-old female with Sigmoid Cancer and the other was a 45-year-old female with acquired eosinophilia. The fewer COVID-19 cases seen in oncology clinics in the beginning of the pandemic are due to the fact that this group of patients is at a greater fear of contracting the virus and therefore follows stricter precautionary measures overall compared to the general population (7).
Our results show that the COVID-19 safety strategies were not strongly implemented in the beginning of the pandemic wave in Lebanon (early March), where patients reported lack of supervised elevators and temperature checks at the entrance. These strategies grew stronger towards the end of March. 5 patients (1%) however, personally suggested that strategies were much stronger early in the outbreak. This could be attributed to the leniency of the protective measures towards the summer and the lifting of the national lockdown in July (1). 37% of patients reported better measures in April compared to 29% in March (p=0.003).
Precautionary measures were not implemented in the valet parking areas, where patients complained about the crowded groups posing a risk of COVID-19 transmission. 6 patients (2%) were dissatisfied with the parking service, which is the first point of contact with the hospital premises. There was no statistical difference between patient satisfaction to the measures at NKBCI and their gender or place of primary residence. 35% of patients in the hematology group compared to 19% in those with solid tumors were given the option of an online consultation (p=0.001), likely due to the higher risk of myelosuppression associated with hematology patients.
The majority of responses showed an adherence to social distancing guidelines on hospital premises and the equally important temperature checks. Overcrowding in waiting rooms seems to be a persistent issue. Fewer staff that are currently working during the pandemic have allowed for greater delay times at waiting desks. A future strategy to mitigate this issue would be stricter visitor policies, or on-boarding more staff with effective social distancing measures in order to reduce waiting times (13). This increase in waiting time during the outbreak has shown to be more prominent than the pre-pandemic era.
COVID-19 educational pamphlets should have been administered at a larger scale as evidenced by the small number of patients who was given information booklets; however, this is accompanied by the risk of physical contact with surfaces that could harbor the virus. This topic can be addressed by introducing electronic means of spreading information about the virus, rather than data in hard copy that can allow for viral transmission along surfaces. Alternating seats are amongst the new social distancing measures taken by hospitals. Although this can help reduce the risk of transmission of the virus, the elderly and the cachectic population (common amongst oncology patients) might be forced to remain standing during waiting hours. There must be more seats available to accommodate all the patients that will be seen in the clinic, whilst still practicing effective social distancing (14).
Telemedicine (TM) has become the platform of patient-centered care in the pandemic. Telemedicine permits mildly ill patients to get the supportive care they need while minimizing their exposure to other acutely ill patients (15). The implementation of the new EPIC EHR system at AUBMC in November 2018 made way to new opportunities in remote patient-centered care and telemedicine. Only 59 (15%) reported to have used telemedicine during the pandemic. 14 patients (24%) who opted for virtual appointments would like to continue online consultations in a COVID free era. Some of these patients gave reasons such as distant residence and a long drive to get to the hospital, delayed waiting times in the emergency department, delay on the phone to schedule a live appointment, etc. Some would opt for an online appointment if they had the means to use technology at home (lack of computer for example). Others would not opt for an online appointment because of the need to be examined personally by their primary physician (particularly breast cancer patients).
Unfortunately for the economic crisis in Beirut, 11 patients (19%) were unable to pay for the online appointment via the Internet and could only pay in cash the next time they would visit the hospital. This raises the issue about putting such patients’ lives at risk by bringing them personally to the hospital to make a payment, when the primary purpose of telemedicine is to limit their exposure to COVID-19. The Internet connection in Lebanon is also problematic. 13 patients (22%) complained about the inability to continue with their online consultation due to connection problems, and as such would choose to see the doctor live for their next appointment.
Telemedicine can pose the risk of ineffective history taking. From our respondents who underwent an online consultation, 3 patients (5%) did not get asked about fever, sick contacts or recent travel during initial history taking because they did not need to come to the hospital. Those patients are predisposed to a significant amount of immunosuppression and therefore, it is important to thoroughly screen for viral symptoms, even if they have virtual appointments and do not need to physically come to the hospital. For patients who only undergo continuous chemotherapy and immunotherapy in the infusion unit of NKBCI, online consultations are inapplicable to them, and therefore they could not contribute to this part of the study.
Bone marrow transplant centers have been particularly affected during the pandemic. Non-urgent auto transplants were postponed during the COVID-19 era, however, inpatient transplant care during the pandemic was not addressed in this study. Patients undergoing transplants were not surveyed due to their incapability to participate in their critical conditions. To protect individuals from SARS-CoV-2 infections, it can only be recommended that maximum emphasis should be placed on personal protection (16, 17). Recommendations for donor screening and detailed medical history (including travel history, exposure to COVID-19 etc.) should be followed (16–20).
The data collected from the patients can be used to draw an effective action plan. The feedback received from patients who had appointments at the NKBCI during the beginning of the pandemic is necessary to help implement new effective strategies in the future control of COVID-19. The online portal for patients must be improved so as not to face difficulties with payment or connection during virtual consultations. More stuff must be hired to control crowded waiting areas while still implementing social distancing and safety measures. Elevators should be kept supervised throughout the pandemic and not only during national lockdown measures. There should be a greater supply of sanitary supplies throughout the hospital premises and not only inside clinics. The number of seats in waiting areas can be increased to allow the frail population to rest while waiting, all whilst still practicing effective social distancing. There must be greater supervision in the valet parking areas. The frequency of use of electronic means of communication must be increased (information leaflets, medication prescription, laboratory tests, medical reports etc.) to limit the transmission of the virus via surfaces. A higher proportion of successful, problem-free virtual encounters should be the goal in the near future. A history of travel to a highly affected area is likely to become irrelevant as part of the pre-screening protocol as more areas have become affected. TM can be used for ongoing management of other chronic diseases such as asthma and immunodeficiency disorders, as individuals with these conditions are particularly susceptible to COVID-19, and medication compliance and disease optimization are important ways to mitigate severity (15).
The strengths of the study include the fact that this is the first survey done in the region, at one of the top tertiary medical centers in Lebanon and the Middle East that provides elite patient care, to assess the changes made during the COVID-19 pandemic. In addition, the study was conducted in a single center, homogenous population using a big sample number of 670 oncology patients. The limitation of the study is that it solely relies on a telephone based source. Another limitation is that a big number of 263 did not respond (excluding the deceased). The study was done over a short duration of the first three months of the outbreak, therefore; only limited information could be obtained. The study can be extended over 12 months to incorporate a bigger sample of patients, and to study the changes in precautionary strategies as the pandemic advances.
Conclusion
The above recommendations will be taken into account by the committee of the NKBCI to develop new safety measures that can better control viral spread amongst the oncology patient population, while maintaining best patience care in the hospital. The study can be extended over the next 12 months to evaluate the efficacy of these new precautionary strategies in accordance with the change in COVID-19 behavior across the year.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Ethics Statement
The Institutional Review Board at the American University of Beirut approved the study. The participants provided oral and written consent to participate in the study.
Author Contributions
JC created the concept of the study, wrote, revised and edited the manuscript. SW was involved in data collection, statistical analysis and writing the manuscript. NG, FC, MS, and SC contributed to data collection. NS, AB, and AT read, revised and commented on the manuscript, and approved the submitted version. All authors contributed to the article and approved the submitted version.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2021.685107/full#supplementary-material
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Khoury P, Azar E, Hitti E. Covid-19 Response in Lebanon: Current Experience and Challenges in a Low-Resource Setting. JAMA (2020) 324(6):548–9. doi: 10.1001/jama.2020.12695
2. Bizri AR, Khachfe HH, Fares MY, Musharrafieh U. Covid-19 Pandemic: An Insult Over Injury for Lebanon. J Community Health (2020) 46:1–7. doi: 10.1007/s10900-020-00884-y
3. Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (Covid-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. Jama (2020) 323(13):1239–42. doi: 10.1001/jama.2020.2648
4. Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Di Napoli R. Features, Evaluation, and Treatment of Coronavirus. StatPearls. Treasure Island (FL: StatPearls Publishing Copyright © 2020, StatPearls Publishing LLC (2020).
5. Sun P, Lu X, Xu C, Sun W, Pan B. Understanding of COVID-19 Based on Current Evidence. J Med Virol (2020) 92(6):548–51. doi: 10.1002/jmv.25722
6. Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. New Engl J Med (2020) 382(13):1199–207. doi: 10.1056/NEJMoa2001316
7. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. New Engl J Med (2020) 382(18):1708–20. doi: 10.1056/NEJMoa2002032
8. Liang W, Guan W, Chen R, Wang W, Li J, Xu K, et al. Cancer Patients in SARS-CoV-2 Infection: A Nationwide Analysis in China. Lancet Oncol (2020) 21(3):335–7. doi: 10.1016/S1470-2045(20)30096-6
9. Bodey GP. Unusual Presentations of Infection in Neutropenic Patients. Int J Antimicrobial Agents (2000) 16(2):93–5. doi: 10.1016/S0924-8579(00)00241-7
10. Garnica M, Valetim MR, Furtado P, Moreira MC, Bigni R, Vinhas S, et al. Covid-19 in Hematology: Data From a Hematologic and Transplant Unit. Hematol Transfusion Cell Ther (2020) 42(4):293–9. doi: 10.1016/j.htct.2020.08.004
11. MacIntyre CR, Wang Q. Physical Distancing, Face Masks, and Eye Protection for Prevention of COVID-19. Lancet (2020) 395(10242):1950–1. doi: 10.1016/S0140-6736(20)31183-1
12. Kattan C, Badreddine H, Rassy E, Kourie HR, Kattan J. The Impact of the Coronavirus Pandemic on the Management of Cancer Patients in Lebanon: A Single Institutional Experience. Future Oncol (2020) 16(17):1157–60. doi: 10.2217/fon-2020-0313
13. Hu L-Q, Wang J, Huang A, Wang D, Wang J. Covid-19 and Improved Prevention of Hospital-Acquired Infection. Br J Anaesth (2020) 125(3):e318–9. doi: 10.1016/j.bja.2020.05.037
14. Lee IK, Wang CC, Lin MC, Kung CT, Lan KC, Lee CT. Effective Strategies to Prevent Coronavirus disease-2019 (Covid-19) Outbreak in Hospital. J Hosp Infect (2020) 105(1):102–3. doi: 10.1016/j.jhin.2020.02.022
15. Portnoy J, Waller M, Elliott T. Telemedicine in the Era of COVID-19. J Allergy Clin Immunol In Pract (2020) 8(5):1489–91. doi: 10.1016/j.jaip.2020.03.008
16. Waghmare A, Abidi MZ, Boeckh M, Chemaly RF, Dadwal S, El Boghdadly Z, et al. Guidelines for COVID-19 Management in Hematopoietic Cell Transplantation and Cellular Therapy Recipients. Biol Blood Marrow Transplant (2020) 26(11):1983–94. doi: 10.1016/j.bbmt.2020.07.027
17. Ljungman P, Mikulska M, de la Camara R, Basak GW, Chabannon C, Corbacioglu S, et al. The Challenge of COVID-19 and Hematopoietic Cell Transplantation; EBMT Recommendations for Management of Hematopoietic Cell Transplant Recipients, Their Donors, and Patients Undergoing CAR T-Cell Therapy. Bone Marrow Transplant (2020) 55(11):2071–6. doi: 10.1038/s41409-020-0919-0
18. Ardura M, Hartley D, Dandoy C, Lehmann L, Jaglowski S, Auletta JJ, et al. Addressing the Impact of the Coronavirus Disease 2019 (Covid-19) Pandemic on Hematopoietic Cell Transplantation: Learning Networks as a Means for Sharing Best Practices. Biol Blood Marrow Transplant (2020) 26(7):e147–60. doi: 10.1016/j.bbmt.2020.04.018
19. Algwaiz G, Aljurf M, Koh M, Horowitz MM, Ljungman P, Weisdorf D, et al. Real-World Issues and Potential Solutions in Hematopoietic Cell Transplantation During the COVID-19 Pandemic: Perspectives From the Worldwide Network for Blood and Marrow Transplantation and Center for International Blood and Marrow Transplant Research Health Services and International Studies Committee. Biol Blood Marrow Transplant (2020) 26(12):2181–9. doi: 10.1016/j.bbmt.2020.07.021
Keywords: COVID-19, NKBCI, oncology, AUBMC, interventions, satisfaction
Citation: El Cheikh J, El Warrak S, Ghaoui N, Al Chami F, Shahbaz M, Chehayeb S, Saghir N, Bazarbachi A and Taher A (2021) Implemented Interventions at the Naef K. Basile Cancer Institute to Protect Patients and Medical Personnel From COVID Infections: Effectiveness and Patient Satisfaction. Front. Oncol. 11:685107. doi: 10.3389/fonc.2021.685107
Received: 24 March 2021; Accepted: 07 May 2021;
Published: 10 June 2021.
Edited by:
Alessandro Isidori, AORMN Hospital, ItalyReviewed by:
Michele Malagola, University of Brescia, ItalyClaudio Cerchione, Istituto Scientifico Romagnolo per lo Studio e il Trattamento dei Tumori (IRCCS), Italy
Copyright © 2021 El Cheikh, El Warrak, Ghaoui, Al Chami, Shahbaz, Chehayeb, Saghir, Bazarbachi and Taher. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jean El Cheikh, amU0NkBhdWIuZWR1Lmxi
 Jean El Cheikh
Jean El Cheikh Samantha El Warrak
Samantha El Warrak Nohra Ghaoui
Nohra Ghaoui Farouk Al Chami2
Farouk Al Chami2 Nagi Saghir
Nagi Saghir Ali Bazarbachi
Ali Bazarbachi Ali Taher
Ali Taher