- 1Department of Surgical Oncology and General Surgery, Key Laboratory of Precision Diagnosis and Treatment of Gastrointestinal Tumors, Ministry of Education, The First Affiliated Hospital of China Medical University, Shenyang, China
- 2Department of Thoracic Surgery, The First Affiliated Hospital of China Medical University, Shenyang, China
Background: The clinical pathology of gastric signet-ring cell carcinoma (SRC) is still unclear. This meta-analysis was performed to evaluate the difference in biological behavior and prognosis between SRC and non-signet ring cell carcinoma (NSRC).
Methods: A total of 58 eligible studies were analyzed using RevMan and other auxiliary software. Biological behaviors were compared based on odds ratio (OR) and mean difference (MD). Hazards ratio (HR) was calculated for prognosis based on Kaplan–Meier curves.
Results: Totally, 28,946 SRC patients were compared with 81,917 NSRC patients. Compared with NSRC patients, lower male: female ratio (OR = 0.53, P < 0.01), younger age (MD = −4.89, P < 0.01), more middle location (OR = 1.64, P < 0.01), more depressed type at early stage (OR = 1.31, P < 0.05), higher incidence of Borrmann type IV (OR = 1.96, P < 0.01), less lymph node metastasis at early stage (OR = 0.78, P < 0.05), better prognosis at early stage (HR = 0.59, P < 0.01), and worse prognosis at advanced stage (HR = 1.19, P < 0.01) were associated with SRC patients.
Conclusion: The prognosis of SRC at early stage is better than other types of gastric cancer, while that of SRC at advanced stage is relatively poorer.
Introduction
Signet-ring cell carcinoma (SRC) is associated with unique histological features based on microscopic observation of the tumor cells rather than on biological behavior. Gastric SRC has been categorized as the “undifferentiated type” by Sugano et al. (1), the “diffused type” by Lauren et al. (2), the “infiltrative type” by Ming et al. (3), and “high grade type” by UICC. Several studies have shown that SRC is associated with a high rate of peripheral metastasis and poor prognosis (4–9); however, a few studies have indicated that SRC has a better outcome than other types of gastric cancer (GC) (10, 11). Meanwhile, several studies have demonstrated that the difference in survival rates between SRC and non-signet ring cell carcinoma (NSRC) is statistically insignificant (12, 13). Additionally, multiple studies have also indicated that early stage gastric SRC has a higher five-year survival rate than NSRC (14, 15). Here, we aimed to elucidate the difference in biological behavior between SRC and NSRC.
This meta-analysis compared the biological behavior and prognosis between SRC and NSRC patients, including gender, tumor location, lymph node metastasis (LNM), age, chemotherapy, tumor size, macroscopic type, and overall survival.
Methods
Population
All patients were diagnosed with GC.
Intervention and Comparator
Exposure Group
Patients who were diagnosed with SRC based on pathological analyses.
Control Group
Patients who were diagnosed with NSRC based on pathological analyses.
Outcomes
Biological behavior and prognosis.
Study Design
This meta-analysis complied with the PRISMA statement. All the included studies were primary research studies. There were no language restrictions.
Search Strategy
The Web of Science, PubMed, and Embase databases were searched from initiation until November 2020 as follows: “((“gastric” [Title/Abstract] OR “stomach” [Title/Abstract]) AND (((“cancer” [Title/Abstract] OR “tumor” [Title/Abstract]) OR “carcinoma” [Title/Abstract]) OR “neoplasm” [Title/Abstract])) AND ((“signet ring cell” [Title/Abstract] OR “signet-ring cell” [Title/Abstract]) OR “signet cell” [Title/Abstract])”, including both published and unpublished articles. There were no language restrictions. The articles were retrieved by more than three independent investigators and compiled.
Inclusion and Exclusion Criteria
The criteria for study enrollment were as follows: [1] Based on the WHO classification, SRC was classified when more than 50% cancer cells were predominantly SRC. [2] All studies related to the prognosis and biological behavior of gastric SRC were included. [3] All studies that showed differences in the biological behavior and prognosis between SRC and NSRC were included. [4] All the included studies were primary research articles. [5] If the same research team reported multiple studies during the same time period, only the latest article or that with complete data was included.
Studies without full text or efficacious data were excluded. Additionally, case reports and editorials were not included.
Data Extraction and Quality Assessment
The following data were extracted from the included studies: publication year, name of the first author, country of author, sample size, and clinicopathological features (e.g., sex ratio, mean age, tumor location, tumor size, chemotherapy, macroscopic type, LNM, and overall survival). However, owing to insufficient data, other variables of clinicopathological features (e.g., venous invasion, peritoneal dissemination, and ulceration) were not extracted or analyzed. Engauge Digitizer 4.1 was employed to distinguish the survival curve and extract hazard ratio (HR) of overall survival (data not shown).
Statistical Analysis
All data were analyzed using Review manager 5.3 and Stata 12.0. Heterogeneity was detected by chi-square test. P-value >0.10 was considered as homogeneous, otherwise as heterogeneous. Moreover, the I2 index was used to assess heterogeneity, and I2 >50% was considered as statistically significant. For homogeneous affirmation, the fixed effects model was selected; otherwise, a random effects model was adopted. The odds ratio (OR), mean difference (MD), and hazard ratio (HR) were calculated, and publication bias was assessed by Egger’s test.
Result
Search Result
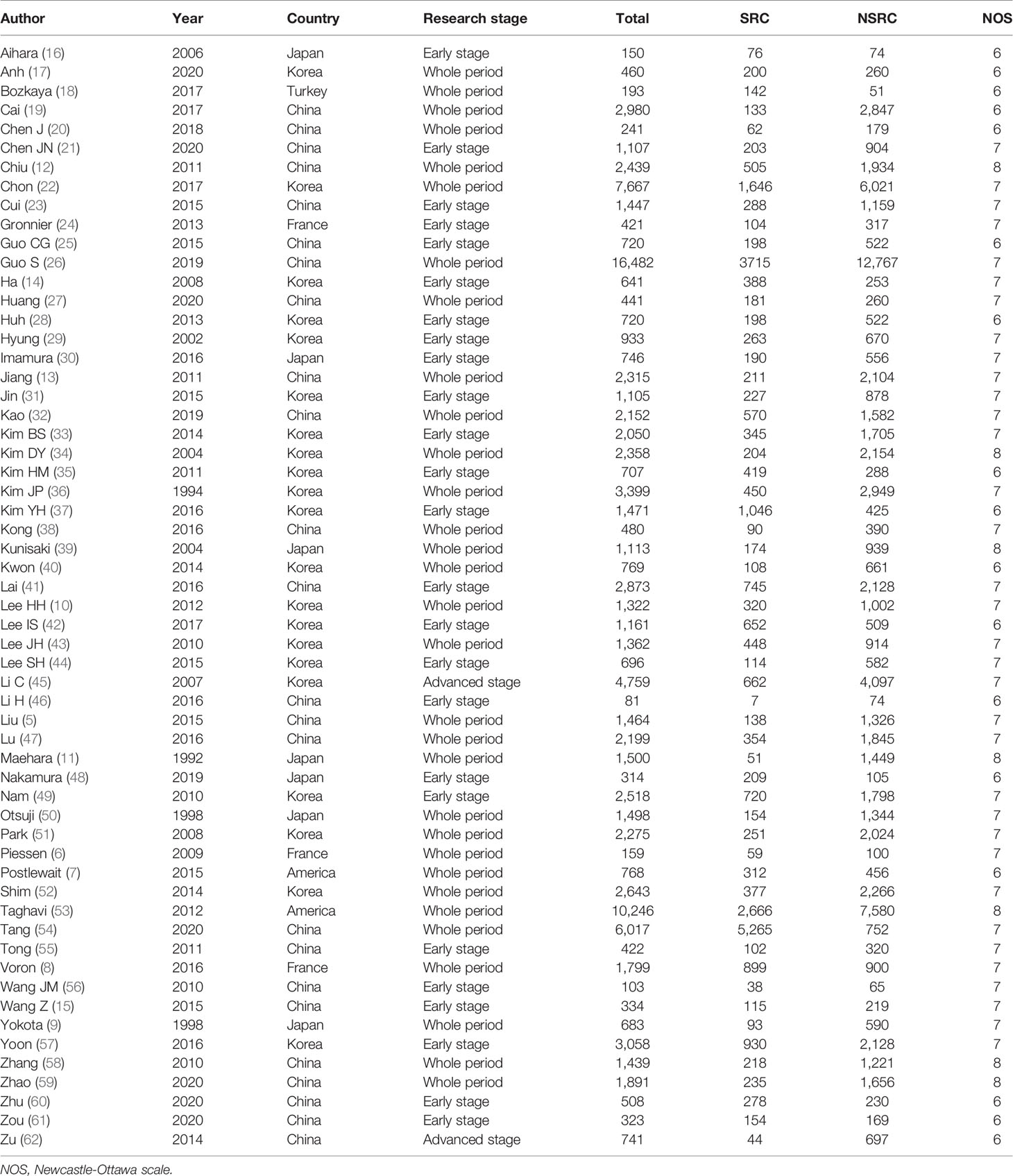
A total of 4,093 studies were retrieved from PubMed, Web of Science, and Embase. After reading the abstracts, we further assessed the full text of 80 studies; we could not obtain the full text for nine studies; 13 contained no usable and reliable data. Finally, 58 eligible studies (5–62) were included in this meta-analysis (Figure 1), among which 31 reported the entire period of patients with SRC or NSRC, 25 focused on early GC, and two reported advanced GC regarding both SRC and NSRC (Table 1). The study population of SRC (28,946) was much smaller than that of NSRC (81,917).
Quality assessment was conducted with Newcastle–Ottawa scale based on three indexes (a maximum of nine points): selection, comparability, and exposure. Among the 58 included studies, 17 scored six points, 34 scored seven points, and seven scored eight points. Based on the threshold of six points, all the studies were eligible.
Clinicopathological Characteristics
The percentage of male patients of SRC was substantially less than that of NSRC (OR = 0.53, 95%CI = 0.49–0.58, P < 0.01; Figure 2). The mean age of SRC patients was substantially younger than that of NSRC patients, at both early and advanced stages (MD = −4.89, 95%CI = −5.85–3.94, P < 0.01; Figure 3). No statistical difference in tumor size of SRC between SRC and NSRC was observed, irrespective of early GC (EGC) or advanced GC (AGC) (total: MD = −1.68, 95%CI = −8.48–5.11, P = 0.63; EGC: MD = 0.55, 95%CI = −0.58–1.67, P = 0.34; AGC: MD = 3.71, 95%CI = −0.24–7.67, P = 0.07; Figure 4). SRC was found to potentially occur at the middle location of the stomach, irrespective of EGC or AGC (OR = 1.64, 95%CI = 1.45–1.85, P < 0.01; Figure 5). Microscopic analysis found that early stage SRC was associated with more depressed type than NSRC (OR = 1.31, 95%CI = 1.03–1.66, P < 0.05; Figure 6A). Moreover, an increased number of incidences with Borrmann type IV at the advanced stage was noted in SRC patients than that in NSRC patients (OR = 1.96, 95%CI = 1.45–2.66, P < 0.01; Figure 6B). However, no marked difference in LNM among advanced-stage SRC and NSRC was found (OR = 1.15, 95%CI = 0.74–1.80, P = 0.53, Figure 7C); while in all the GC cases or EGC cases, SRC was associated with less LNM, in comparison with NSRC (total: OR = 0.78, 95%CI = 0.63–0.96, P < 0.01; EGC: OR = 0.64, 95%CI = 0.52–0.79, P < 0.01; Figures 7A, B). Moreover, 10 studies employed chemotherapy, while no marked difference in the chemotherapy rate was found between SRC and NSRC (OR = 0.95, 95%CI = 0.70–1.27, P = 0.85; Figure 8).
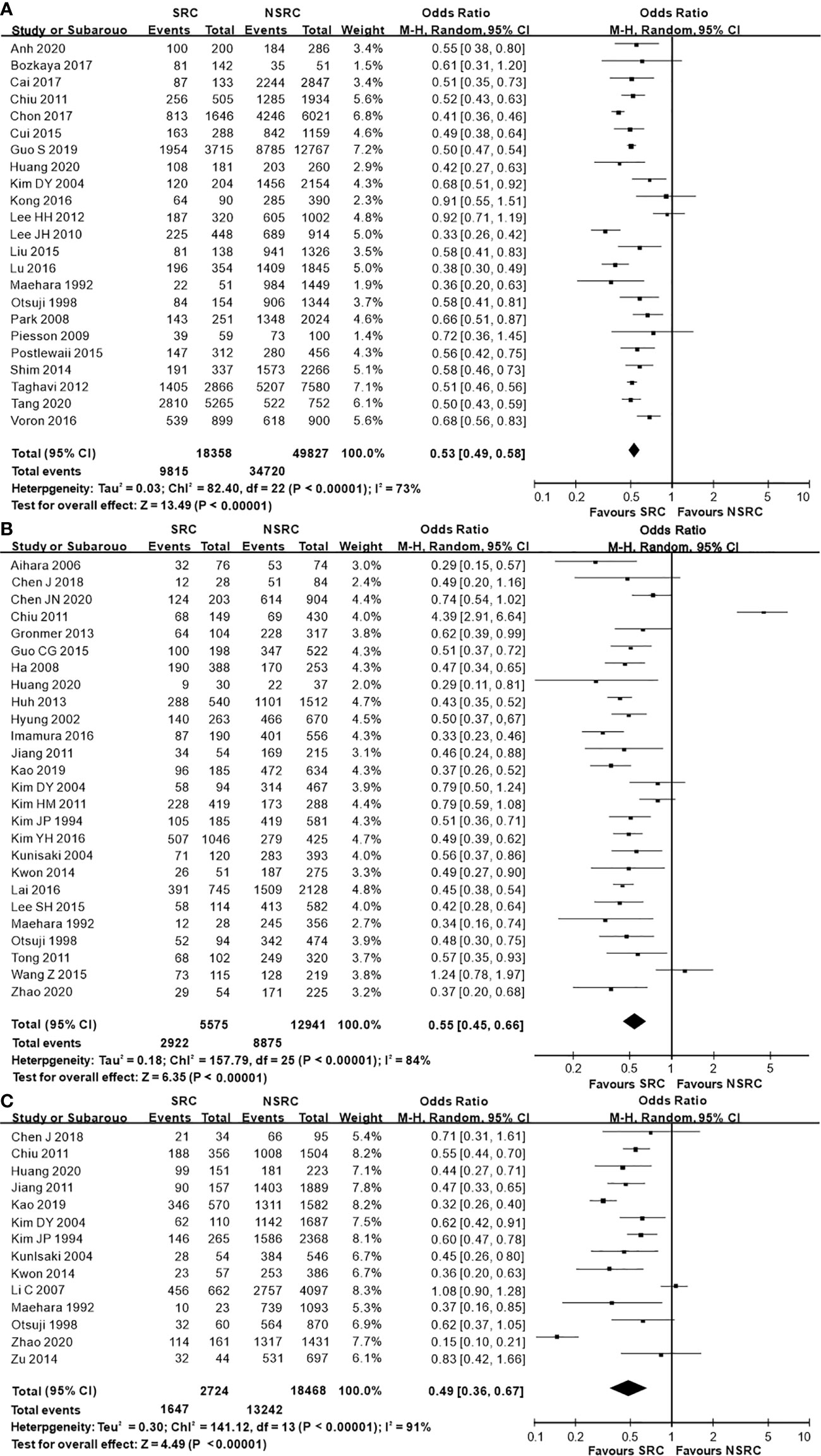
Figure 2 Forest plot displaying the results of the meta-analysis. (A) Odds ratio for the male ratio of patients with SRC and NSRC. (B) Odds ratio for male ratio at early stage. (C) Odds ratio for male ratio at advanced stage.
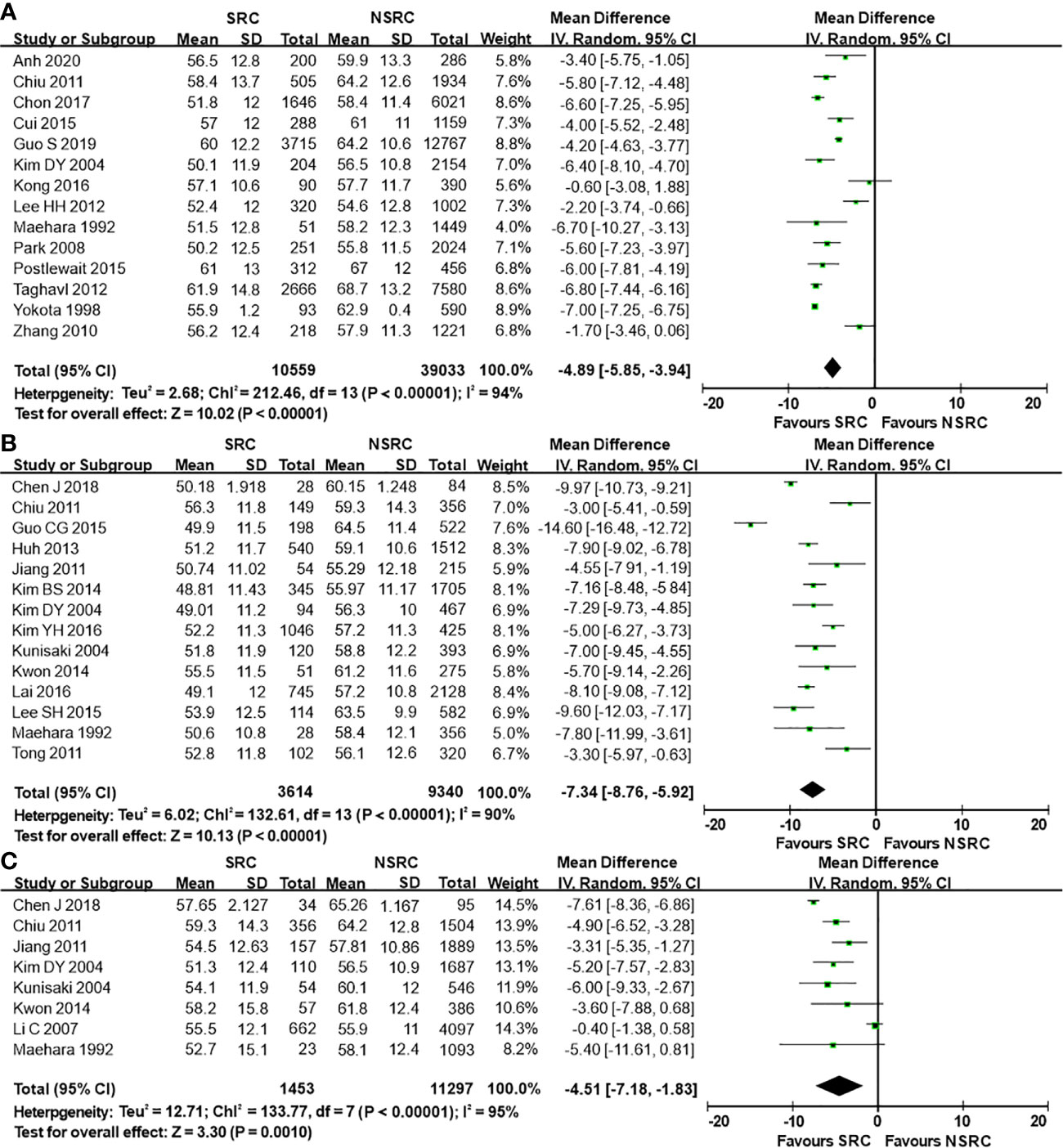
Figure 3 Forest plot displaying the results of meta-analysis. (A) Mean difference for mean age of patients with SRC and NSRC. (B) Mean difference for mean age at early stage. (C) Mean difference for mean age at advanced stage.
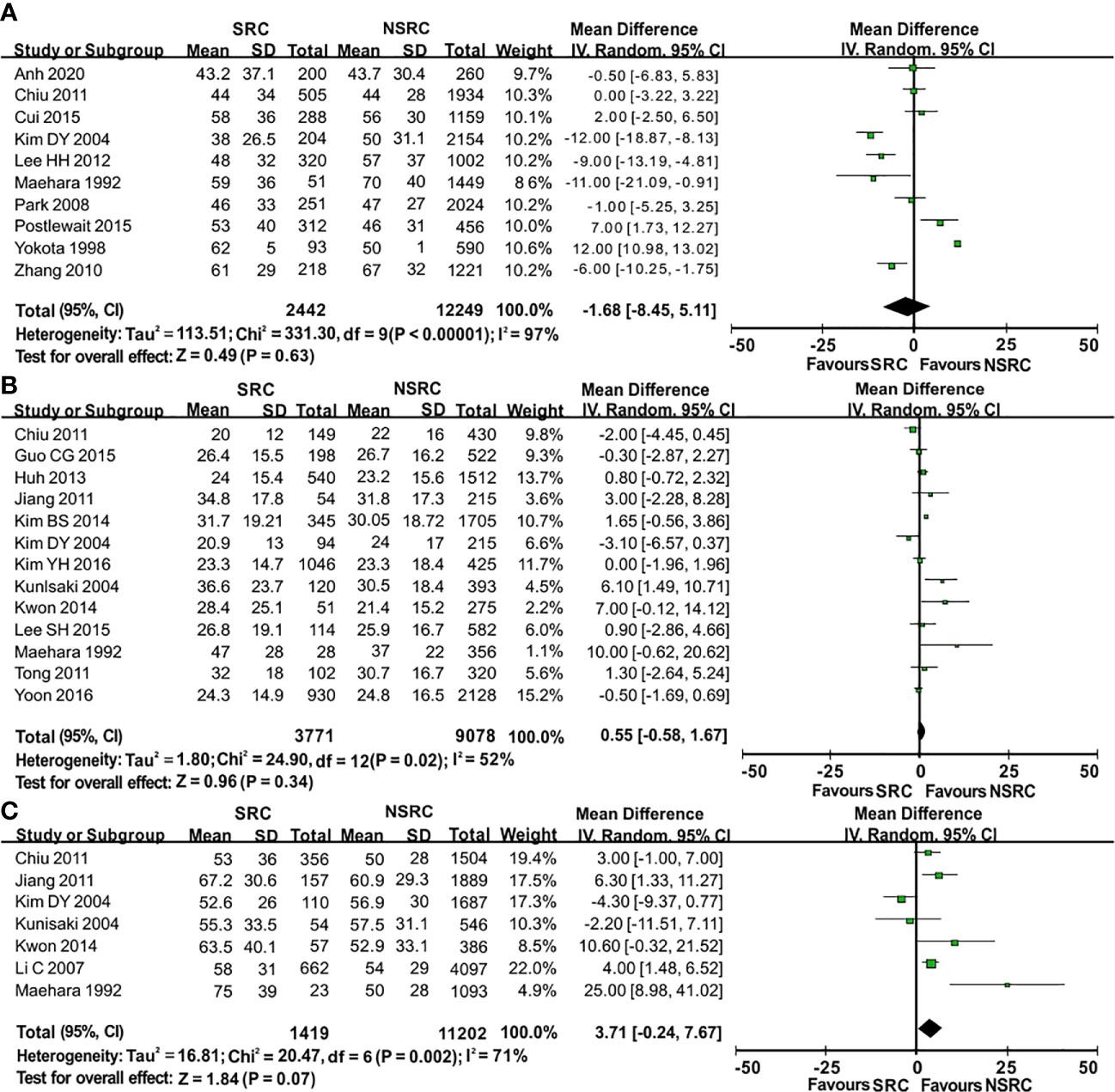
Figure 4 Forest plot displaying the results of meta-analysis. (A) Mean difference for tumor size of patients with SRC and NSRC. (B) Mean difference for tumor size at early stage. (C) Mean difference for tumor size at advanced stage.
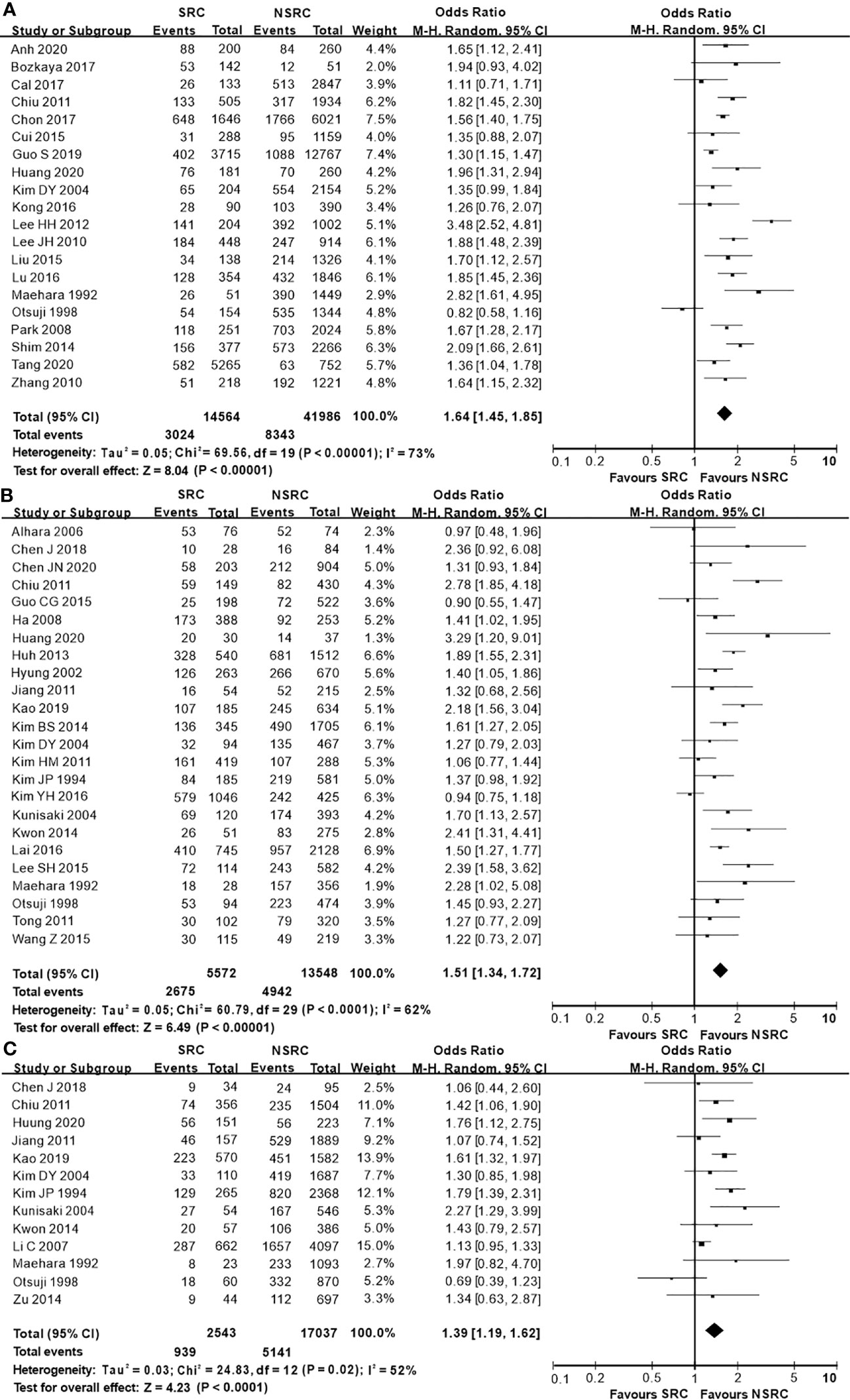
Figure 5 Forest plot displaying the results of meta-analysis. (A) Odds ratio for middle location of patients with SRC and NSRC. (B) Odds ratio for middle location at early stage. (C) Odds ratio for middle location at advanced stage.
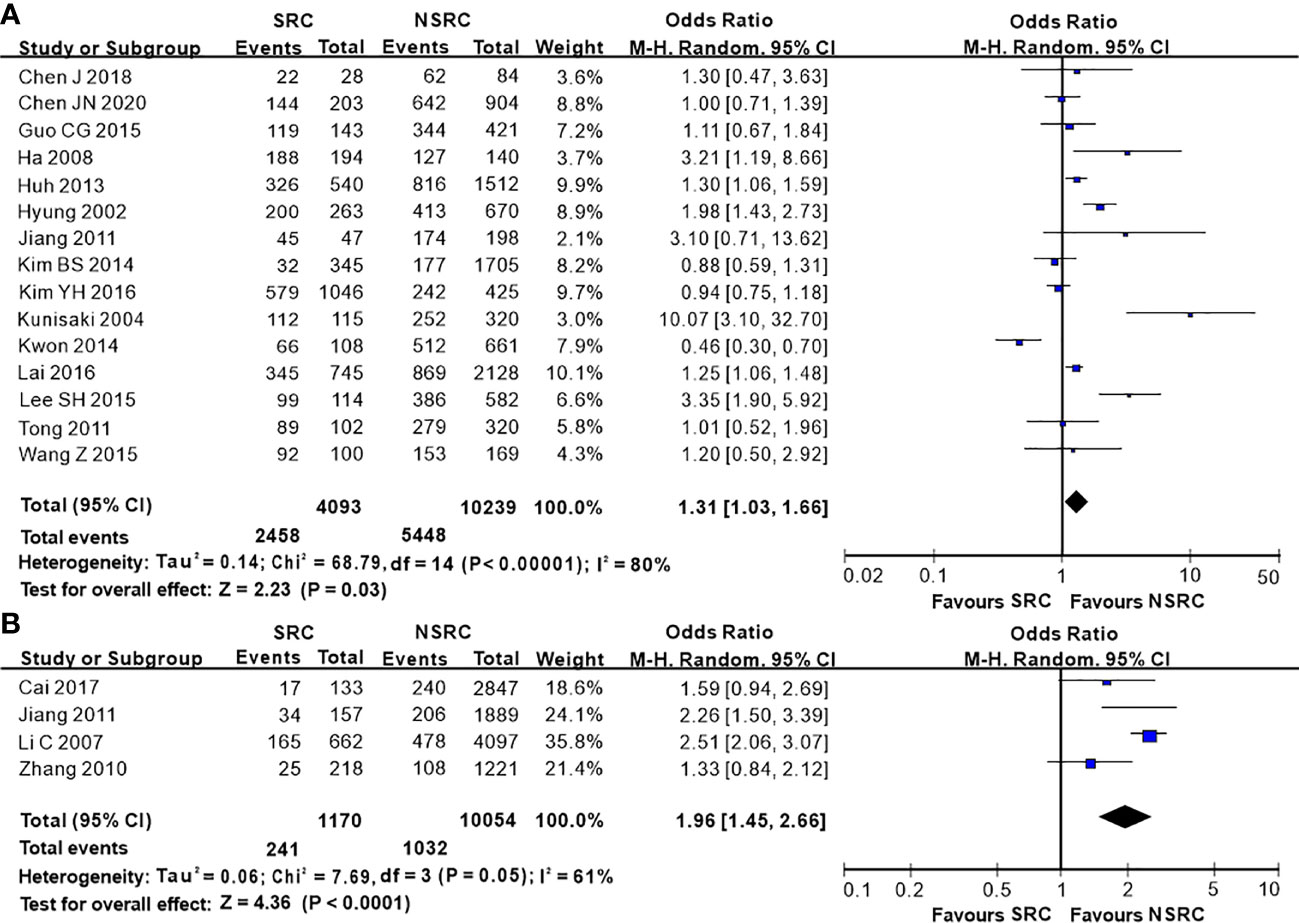
Figure 6 Forest plot displaying the results of meta-analysis. (A) Odds ratio for depressed type of patients with SRC and NSRC at early stage. (B) Odds ratio for Borrmann IV at advanced stage. (DT, depressed type; B-4, Borrmann IV).
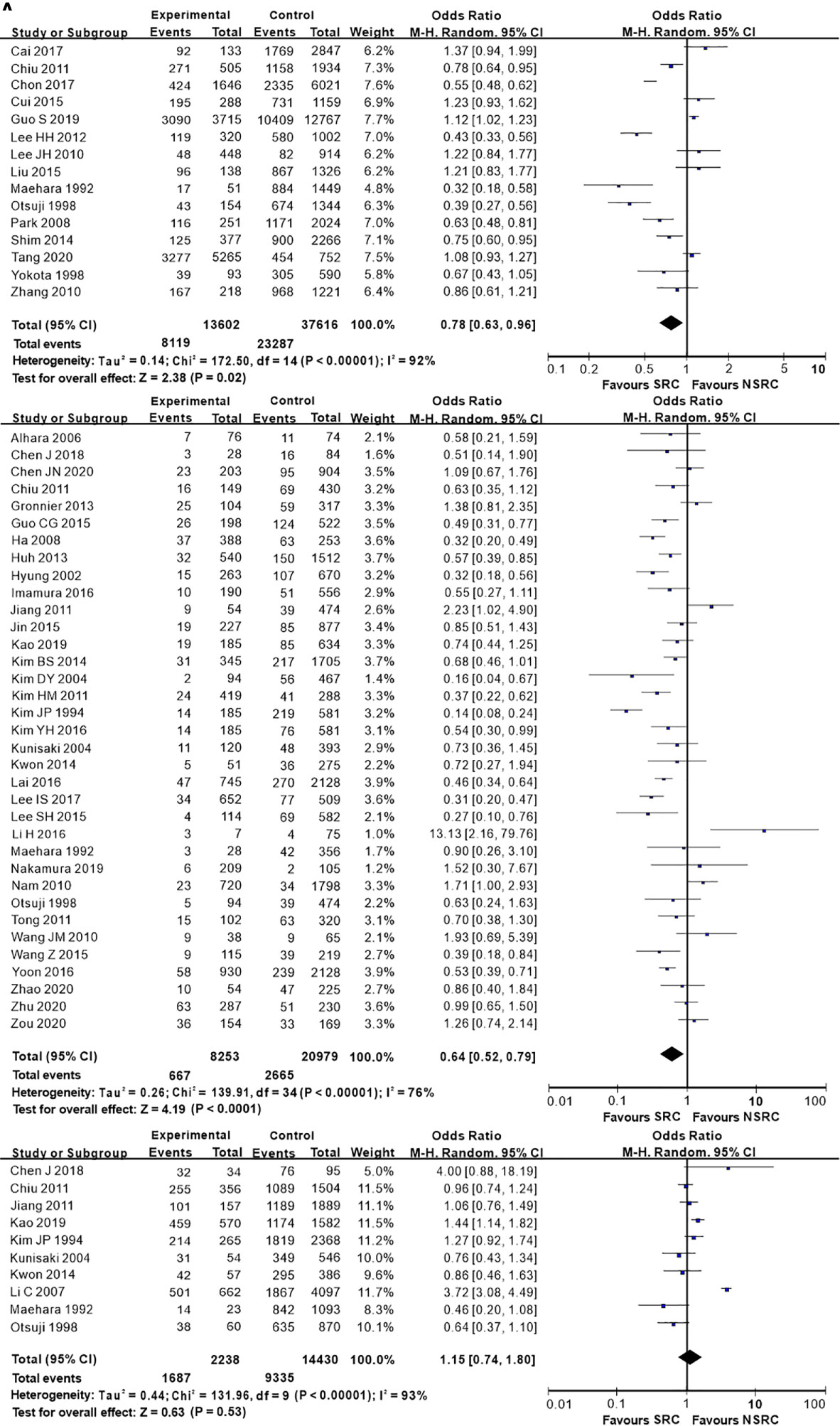
Figure 7 Forest plot displaying the results of meta-analysis. (A) Odds ratio for lymph node metastasis of patients. (B) Odds ratio for lymph node metastasis at early stage. (C) Odds ratio for lymph node metastasis at advanced stage. (LNM, lymph node metastasis).
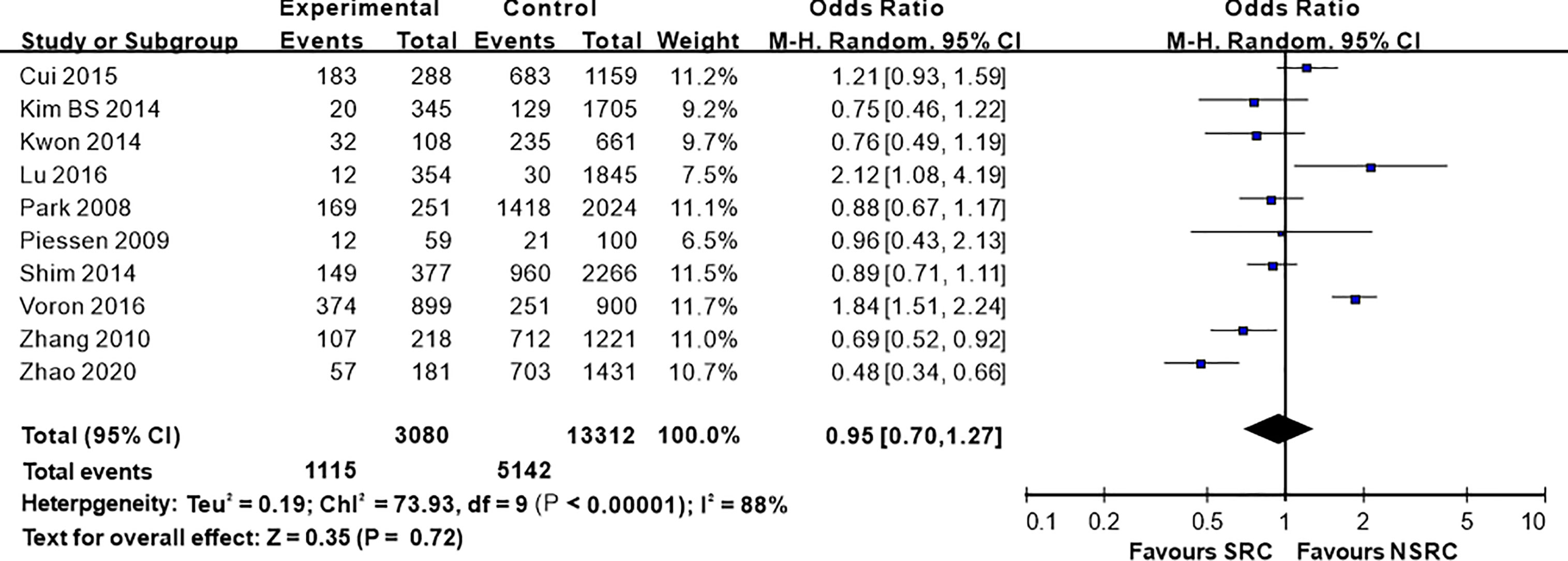
Figure 8 Forest plot displaying the results of meta-analysis. Odds ratio for chemotherapy rate of patients with SRC and NSRC.
Prognosis
No statistically significant difference was noted in the overall survival between SRC and NSRC patients (HR = 1.07, 95%CI = 0.94–1.22, P = 0.285; Figure 9A). Early stage SRC exhibited better prognosis than NSRC (HR = 0.59, 95%CI = 0.45–0.79, P < 0.01; Figure 9B), while advanced-stage SRC exhibited poorer prognosis than NSRC (HR = 1.19, 95%CI = 1.13–1.27, P < 0.01; Figure 9C).
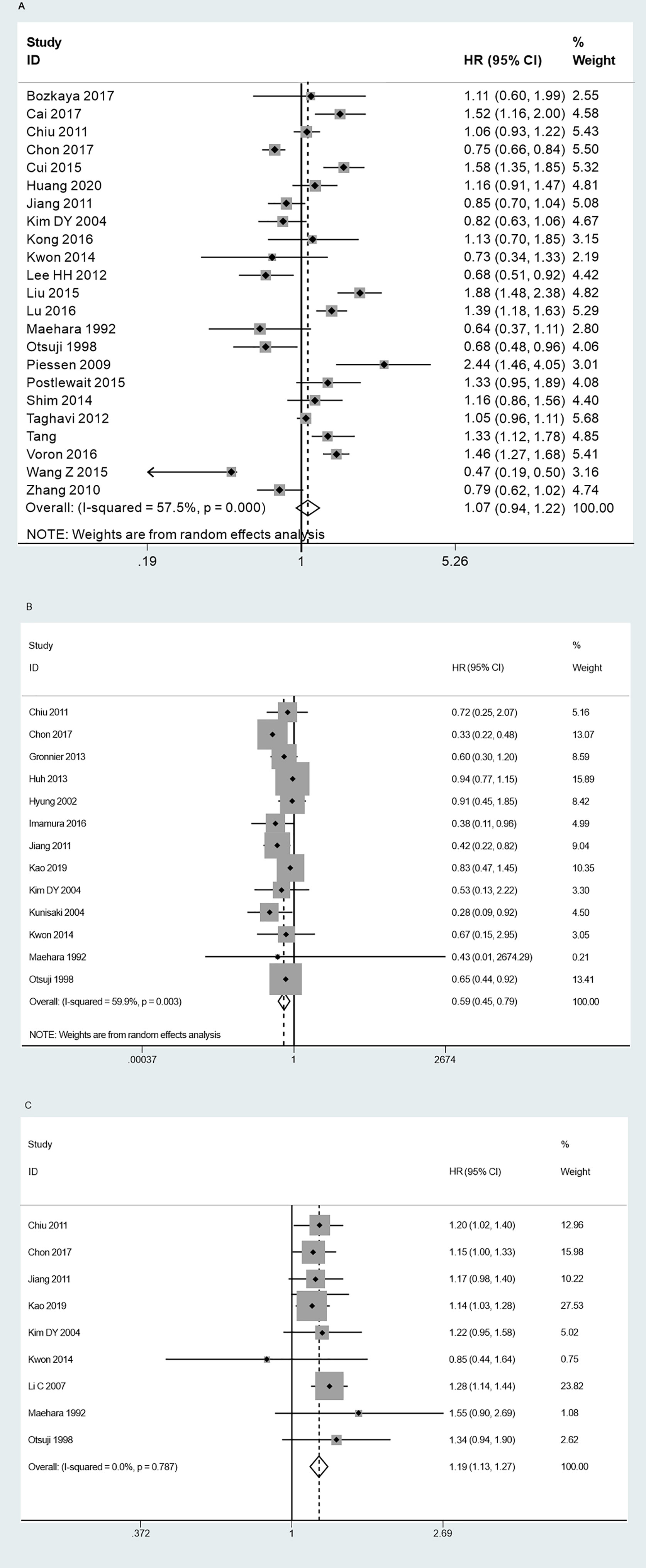
Figure 9 Forest plot displaying the results of meta-analysis. (A) Hazard ratio for overall survival of patients. (B) Hazard ratio for overall survival at early stage. (C) Hazard ratio for overall survival at advanced stage.
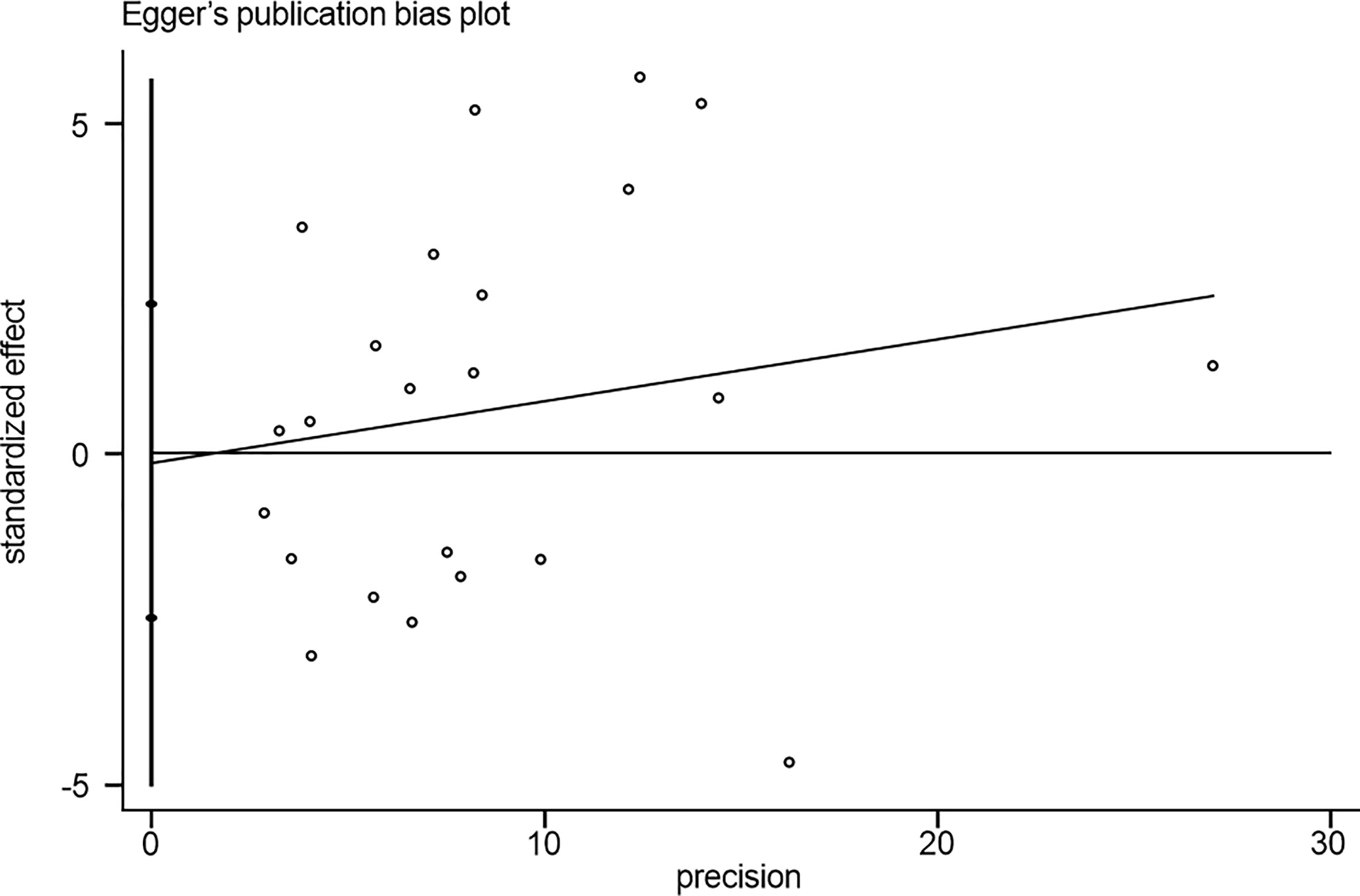
Publication Bias
No noticeable publication bias was observed based on the results of Egger’s test (P = 0.416; Figure 10).
Discussion
SRC is a highly malignant carcinoma mucocellulare. Abundant mucin in the cytoplasm of SRC drives the nuclei to one side of the cells, inducing a ring-like cell conformation (9). Approximately 1% of SRC occurs in organs including colon, urinary tract, gallbladder, pancreas, breast, and stomach. Previous studies have shown that SRC accounts for 8 to 30% of all gastric neoplasms (63). The global incidence of GC has recently declined, while that of gastric SRC is continually increasing (64). Although the included studies in this meta-analysis have reported the clinicopathological features of gastric SRC, the results are unclear.
Here, we found that gastric SRC was relatively frequently diagnosed in females; however, the underlying explanation for such an association has not yet been determined. Several studies have demonstrated the potential role of over-expressed estrogen in SRC, which has been associated with frequent metastasis in the uterus or ovary in SRC patients (65). Furthermore, Kim et al. found a substantially poorer overall survival in female SRC patients than in the male patients, especially those with advanced GC and aged ≤45 years (66). Here, the mean age of SRC patients was substantially younger than that of NSRC patients. The typical intracytoplasmic mucin, compressed nuclei in the corner, the tendency to be larger and sprawl superficially to mucosal and submucosal layers have ensured the early diagnosis of SRC at the early stage or younger age. Postlewait and Yokota claimed that the tumor size of NSRC was smaller than that of SRC. However, our study found no marked difference in the tumor size between the two groups (7, 9). Compared with NSRC, SRC was more commonly found in the middle location of the stomach; meanwhile, no marked difference between upper and lower locations was observed (data not shown). Thus, considering the macroscopic features of EGC, we suggested that SRC had more depressed type than NSRC. For AGC, Borrmann type IV was more commonly found in SRC than NSRC, which probably contributed to the poor outcome.
LNM is known to play a marked role in GC research. Our study implied that SRC was associated with less LNM than NSRC, especially for EGC, while no noticeable relationship was observed for AGC. Unlike other histological types, the correlation between the increased rate of LNM in SRC and the tumor size is not recognized (29). Due to the CDH1 mutation, early SRC was associated with a less aggressive state (67). SRC is thought to arise in the undifferentiated stem cell in lamina propria of gland neck. At the early stage, SRC was found to widely spread in the mucous layer and slowly to submucosal layer than NSRC. When SRC spread into the submucosa, it rapidly metastasized (68).Wang et al. reported that SRC was associated with less ulceration than NSRC, which was considered a major predictor for LNM (15).
The difference in prognosis between SRC and NSRC remains debatable. However, several studies have shown that SRC was associated with worse prognosis than NSRC (5, 23). However, Lee and Maehara reported the opposite results (10, 11). Our study indicated that the overall survival of SRC patients was insignificantly different from that of NSRC patients. The improved survival reported by several studies was probably related to the younger age of the SRC patients at presentation. Early stage SRC was associated with less LNM, and thus, it had better prognosis than NSRC. As a matter of fact, most of the included studies displayed that early stage SRC patients had a higher five-year survival rate. We extracted HR from the Kaplan–Meier curves, and the outcome was significant. Several studies have indicated that advanced-stage SRC was associated with poorer prognosis than NSRC (9, 50), while other studies could not find such an association (13, 34). The current study indicated that the poor prognosis of SRC was accompanied by the lower overall survival rate, as compared to NSRC. Consequently, early diagnosis and detection were crucial to improve the overall survival of gastric SRC. Furthermore, less invasive strategies, such as endoscopic submucosal dissection (ESD) and endoscopic mucosal resection (EMR), have been suggested for early stage GC to improve the quality of life of the patients. However, the Japanese GC treatment guidelines state that ESD was not feasible for the undifferentiated histology type of GC (69), which leads to controversial opinions on ESD for SRC treatment. Recent studies have reported dissimilar outcomes of ESD therapy for SRC (70). One study reported that ESD resulted in a higher rate of en bloc resection and complete resection on SRC than the poorly differentiated types of GC (35), which suggested that ESD might be preferred for EGC patients diagnosed with SRC. On the other hand, curative resection has been suggested for extended lymph node dissection for AGC. Furthermore, the effect of chemotherapy, either neoadjuvant of adjuvant, on SRC is still controversial (71, 72). Turgeon demonstrated that surgery resulted in a higher five-year overall survival rate than perioperative, neoadjuvant, and adjuvant therapy for stage I SRC patients (73). The chemosensitivity of SRC is related to the CLDN18-ARHGAP26/6 fusion (74). Compared with NSRC, SRC is speculated to be more chemo-resistant to conventional drugs, such as 5-FU and platinum (13, 23, 75). However, Pernot suggested that SRC possesses high sensitivity to taxane-based chemotherapeutic drugs or antiangiogenics (64). To improve the treatment strategy and prognosis is the important point of SRC.
This study has several limitations. First, most of the included studies were conducted in China, Korea, or Japan. The discrepancy in diet, heredity, and environment between Asia and other continents could have influenced the outcome. Second, no RCTs were included in this meta-analysis, and all the studies were retrospective analyses, which may result in a risk of bias. Third, since the HR was calculated from the data or extrapolated from the Kaplan–Meier curves, it was associated with reduced reliability. Finally, heterogeneity was high in the statistics process, which could lead to unavoidable biases. Therefore, additional data are essential to increase the quality and reliability of this meta-analysis.
Conclusion
Gastric SRC is associated with more female patients, younger patients, more occurrence at middle location of the stomach, more depressed type (EGC), higher incidence of Borrmann type IV (AGC), and less LNM (EGC) than NSRC. The prognosis of early stage SRC is better than that of other GC types, while the prognosis of SRC at the advanced stage was poor. Thus, SRC exhibits specific biological features and differential prognosis compared with NSRC, which may facilitate the development of tailored therapeutic strategy and individualized treatment.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Author Contributions
SZ and C-GJ designed this study. SZ, LL, and KZ performed search and collected data. J-CZ and C-GJ re-checked the data. SZ and YT performed analysis. LL and SZ wrote the manuscript. C-GJ reviewed the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the General Project of Liaoning Provincial Education Department (JCZR2020004).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Abbreviations
SRC, signet-ring cell carcinoma; NSRC, non signet-ring cell carcinoma; OR, odds ratio; HR, hazard ratio; CI, confidence interval; UICC, Union for International Cancer Control; GC, gastric cancer; EGC, early gastric cancer; AGC, advanced gastric cancer; LNM, lymph node metastasis.
References
1. Sugano H, Nakamura K, Kato Y. Pathological Studies of Human Gastric Cancer. Acta Pathologica Japonica (1982) 32(Suppl 2):329–47.
2. Lauren P. The Two Histological Main Types of Gastric Carcinoma: Diffuse and So-Called Intestinal-Type Carcinoma. An Attempt at a Histo-Clinical Classification. Acta Pathologica Microbiologica Scandinavica (1965) 64:31–49. doi: 10.1111/apm.1965.64.1.31
3. Ming SC. Gastric Carcinoma. A Pathobiological Classification. Cancer (1977) 39(6):2475–85. doi: 10.1002/1097-0142(197706)39:6<2475::aid-cncr2820390626>3.0.co;2-l
4. Bu Z, Zheng Z, Li Z, Wu X, Zhang L, Wu A, et al. Clinicopathological and Prognostic Differences Between Mucinous Gastric Carcinoma and Signet-Ring Cell Carcinoma. Chin J Cancer Res (2013) 25(1):32–8. doi: 10.3978/j.issn.1000-9604.2013.01.05
5. Liu X, Cai H, Sheng W, Yu L, Long Z, Shi Y, et al. Clinicopathological Characteristics and Survival Outcomes of Primary Signet Ring Cell Carcinoma in the Stomach: Retrospective Analysis of Single Center Database. PloS One (2015) 10(12):e0144420. doi: 10.1371/journal.pone.0144420
6. Piessen G, Messager M, Leteurtre E, Jean-Pierre T, Mariette C. Signet Ring Cell Histology is an Independent Predictor of Poor Prognosis in Gastric Adenocarcinoma Regardless of Tumoral Clinical Presentation. Ann Surg (2009) 250(6):878–87. doi: 10.1097/SLA.0b013e3181b21c7b
7. Postlewait LM, Squires MH, 3rd, Kooby DA, Poultsides GA, Weber SM, Bloomston M, et al. Prognostic Value of Signet-Ring Cell Histology in Resected Gastric Adenocarcinoma. Ann Surg Oncol (2015) 22(Suppl 3):S832–9. doi: 10.1245/s10434-015-4724-8
8. Voron T, Messager M, Duhamel A, Lefevre J, Mabrut JY, Goere D, et al. Is Signet-Ring Cell Carcinoma a Specific Entity Among Gastric Cancers? Gastric cancer: Off J Int Gastric Cancer Assoc Jpn Gastric Cancer Assoc (2016) 19(4):1027–40. doi: 10.1007/s10120-015-0564-2
9. Yokota T, Kunii Y, Teshima S, Yamada Y, Saito T, Kikuchi S, et al. Signet Ring Cell Carcinoma of the Stomach: A Clinicopathological Comparison With the Other Histological Types. Tohoku J Exp Med (1998) 186(2):121–30. doi: 10.1620/tjem.186.121
10. Lee HH, Song KY, Park CH, Jeon HM. Undifferentiated-Type Gastric Adenocarcinoma: Prognostic Impact of Three Histological Types. World J Surg Oncol (2012) 10:254. doi: 10.1186/1477-7819-10-254
11. Maehara Y, Sakaguchi Y, Moriguchi S, Orita H, Korenaga D, Kohnoe S, et al. Signet Ring Cell Carcinoma of the Stomach. Cancer (1992) 69(7):1645–50. doi: 10.1002/1097-0142(19920401)69:7<1645::aid-cncr2820690702>3.0.co;2-x
12. Chiu CT, Kuo CJ, Yeh TS, Hsu JT, Liu KH, Yeh CN, et al. Early Signet Ring Cell Gastric Cancer. Digestive Dis Sci (2011) 56(6):1749–56. doi: 10.1007/s10620-010-1487-8
13. Jiang CG, Wang ZN, Sun Z, Liu FN, Yu M, Xu HM. Clinicopathologic Characteristics and Prognosis of Signet Ring Cell Carcinoma of the Stomach: Results From a Chinese Mono-Institutional Study. J Surg Oncol (2011) 103(7):700–3. doi: 10.1002/jso.21878
14. Ha TK, An JY, Youn HK, Noh JH, Sohn TS, Kim S. Indication for Endoscopic Mucosal Resection in Early Signet Ring Cell Gastric Cancer. Ann Surg Oncol (2008) 15(2):508–13. doi: 10.1245/s10434-007-9660-9
15. Wang Z, Zhang X, Hu J, Zeng W, Zhou Z. Clinicopathological Features and Outcomes in Patients Undergoing Radical Resection for Early Gastric Cancer With Signet Ring Cell Histology. J Visceral Surg (2015) 152(6):357–61. doi: 10.1016/j.jviscsurg.2015.09.021
16. Aihara R, Mochiki E, Kamiyama Y, Ohno T, Asao T, Kuwano H. Matrilsin Expression is a Useful Marker of Submucosal Invasion and Lymph Node Metastasis in Early Stage Signet Ring Cell Carcinoma of the Stomach. J Surg Oncol (2006) 93(6):491–7. doi: 10.1002/jso.20439
17. Ahn H, Chung WC, Kim YJ, Ryu S, Lim E. Clinical Outcomes of Mucinous Gastric Carcinomas Compared With non-Mucinous and Signet Ring Cell Carcinomas. Korean J Gastroenterol = Taehan Sohwagi Hakhoe chi (2020) 76(6):297–303. doi: 10.4166/kjg.2020.098
18. Bozkaya Y, Erdem GU, Ozdemir NY, Demirci NS, Hocazade C, Yazici O, et al. Comparison of Clinicopathological and Prognostic Characteristics in Patients With Mucinous Carcinoma and Signet Ring Cell Carcinoma of the Stomach. Curr Med Res Opin (2017) 33(1):109–16. doi: 10.1080/03007995.2016.1239192
19. Cai L, Li Y, Yang X, Wang W, Guo M, Lian X, et al. Is the Signet Ring Cell Histological Type a Positive Prognostic Factor for Gastric Adenocarcinoma After D2 Radical Gastrectomy? Int J Clin Exp Pathol (2017) 10(10):10489–94.
20. Chen J, Cai R, Ren G, Zhao J, Li H, Guo C, et al. Differences in Clinicopathological Characteristics and Computed Tomography Findings Between Signet Ring Cell Carcinoma and Nonsignet Ring Cell Carcinoma in Early and Advanced Gastric Cancer. Cancer Med (2018) 7(4):1160–9. doi: 10.1002/cam4.1417
21. Chen JN, Wang QW, Zhang QW, Tang ZR, Li XB. Poorly Differentiated is More Significant Than Signet Ring Cell Component for Lymph Node Metastasis in Mixed-Type Early Gastric Cancer: A Retrospective Study From a Large-Volume Hospital. Surg Endoscopy (2020) 35(4):1558–65. doi: 10.1007/s00464-020-07532-5
22. Chon HJ, Hyung WJ, Kim C, Park S, Kim JH, Park CH, et al. Differential Prognostic Implications of Gastric Signet Ring Cell Carcinoma: Stage Adjusted Analysis From a Single High-Volume Center in Asia. Ann Surg (2017) 265(5):946–53. doi: 10.1097/sla.0000000000001793
23. Cui J, Liang H, Deng J, Ding X, Wang X, Zhang L, et al. [Clinicopathological Features and Prognostic Analysis of Patients With Signet Ring Cell Gastric Carcinoma]. Zhonghua zhong liu za zhi [Chinese J Oncol] (2015) 37(5):367–70.
24. Gronnier C, Messager M, Robb WB, Thiebot T, Louis D, Luc G, et al. Is the Negative Prognostic Impact of Signet Ring Cell Histology Maintained in Early Gastric Adenocarcinoma? Surgery (2013) 154(5):1093–9. doi: 10.1016/j.surg.2013.05.020
25. Guo CG, Zhao DB, Liu Q, Zhou ZX, Zhao P, Wang GQ, et al. Risk Factors for Lymph Node Metastasis in Early Gastric Cancer With Signet Ring Cell Carcinoma. J Gastroint Surg (2015) 19(11):1958–65. doi: 10.1007/s11605-015-2915-z
26. Guo S, Shang MY, Dong Z, Zhang J, Wang Y, Zheng ZC, et al. Clinicopathological Features and Prognostic Analysis of Signet Ring Cell Gastric Carcinoma: A Population-Based Study. Trans Cancer Res (2019) 8:1918–30. doi: 10.21037/tcr.2019.09.06
27. Huang KH, Chen MH, Fang WL, Lin CH, Chao Y, Lo SS, et al. The Clinicopathological Characteristics and Genetic Alterations of Signet-Ring Cell Carcinoma in Gastric Cancer. Cancers (2020) 12(8):2318. doi: 10.3390/cancers12082318
28. Huh CW, Jung DH, Kim JH, Lee YC, Kim H, Kim H, et al. Signet Ring Cell Mixed Histology may Show More Aggressive Behavior Than Other Histologies in Early Gastric Cancer. J Surg Oncol (2013) 107(2):124–9. doi: 10.1002/jso.23261
29. Hyung WJ, Noh SH, Lee JH, Huh JJ, Lah KH, Choi SH, et al. Early Gastric Carcinoma With Signet Ring Cell Histology. Cancer (2002) 94(1):78–83. doi: 10.1002/cncr.10120
30. Imamura T, Komatsu S, Ichikawa D, Kawaguchi T, Kosuga T, Okamoto K, et al. Early Signet Ring Cell Carcinoma of the Stomach is Related to Favorable Prognosis and Low Incidence of Lymph Node Metastasis. J Surg Oncol (2016) 114(5):607–12. doi: 10.1002/jso.24377
31. Jin EH, Lee DH, Jung SA, Shim KN, Seo JY, Kim N, et al. Clinicopathologic Factors and Molecular Markers Related to Lymph Node Metastasis in Early Gastric Cancer. World J Gastroenterol (2015) 21(2):571–7. doi: 10.3748/wjg.v21.i2.571
32. Kao YC, Fang WL, Wang RF, Li AFY, Yang MH, Wu CW, et al. Clinicopathological Differences in Signet Ring Cell Adenocarcinoma Between Early and Advanced Gastric Cancer. Gastric Cancer: Off J Int Gastric Cancer Assoc Jpn Gastric Cancer Assoc (2019) 22(2):255–63. doi: 10.1007/s10120-018-0860-8
33. Kim BS, Kim BS, Oh ST, Yook JH. Signet Ring Cell Type and Other Histologic Types: Differing Clinical Course and Prognosis in T1 Gastric Cancer. Surg (US) (2014) 155(6):1030–5. doi: 10.1016/j.surg.2013.08.016
34. Kim DY, Park YK, Joo JK, Ryu SY, Kim YJ, Kim SK, et al. Clinicopathological Characteristics of Signet Ring Cell Carcinoma of the Stomach. ANZ J Surg (2004) 74(12):1060–4. doi: 10.1111/j.1445-1433.2004.03268.x
35. Kim HM, Pak KH, Chung MJ, Cho JH, Hyung WJ, Noh SH, et al. Early Gastric Cancer of Signet Ring Cell Carcinoma Is More Amenable to Endoscopic Treatment Than is Early Gastric Cancer of Poorly Differentiated Tubular Adenocarcinoma in Select Tumor Conditions. Surg Endoscopy (2011) 25(9):3087–93. doi: 10.1007/s00464-011-1674-5
36. Kim JP, Kim SC, Yang HK. Prognostic Significance of Signet Ring Cell Carcinoma of the Stomach. Surg Oncol (1994) 3(4):221–7. doi: 10.1016/0960-7404(94)90037-x
37. Kim YH, Kim JH, Kim H, Kim H, Lee YC, Lee SK, et al. Is the Recent WHO Histological Classification for Gastric Cancer Helpful for Application to Endoscopic Resection? Gastric Cancer: Off J Int Gastric Cancer Assoc Jpn Gastric Cancer Assoc (2016) 19(3):869–75. doi: 10.1007/s10120-015-0538-4
38. Kong P, Wu R, Yang C, Geng Q, Liu J, Chen S, et al. Prognostic Impact of the Signet Ring Cell Type in Node-Negative Gastric Cancer. Sci Rep (2016) 6:26313. doi: 10.1038/srep26313
39. Kunisaki C, Shimada H, Nomura M, Matsuda G, Otsuka Y, Akiyama H. Therapeutic Strategy for Signet Ring Cell Carcinoma of the Stomach. Br J Surg (2004) 91(10):1319–24. doi: 10.1002/bjs.4637
40. Kwon CH, Kim YK, Lee S, Kim A, Park HJ, Choi Y, et al. Gastric Poorly Cohesive Carcinoma: A Correlative Study of Mutational Signatures and Prognostic Significance Based on Histopathological Subtypes. Histopathology (2018) 72(4):556–68. doi: 10.1111/his.13383
41. Lai JF, Xu WN, Noh SH, Lu WQ. Effect of World Health Organization (WHO) Histological Classification on Predicting Lymph Node Metastasis and Recurrence in Early Gastric Cancer. Med Sci Monitor (2016) 22:3147–53. doi: 10.12659/MSM.897311
42. Lee IS, Lee S, Park YS, Gong CS, Yook JH, Kim BS. Applicability of Endoscopic Submucosal Dissection for Undifferentiated Early Gastric Cancer: Mixed Histology of Poorly Differentiated Adenocarcinoma and Signet Ring Cell Carcinoma Is a Worse Predictive Factor of Nodal Metastasis. Surg Oncol (2017) 26(1):8–12. doi: 10.1016/j.suronc.2016.12.001
43. Lee JH, Choi IJ, Kook MC, Nam BH, Kim YW, Ryu KW. Risk Factors for Lymph Node Metastasis in Patients With Early Gastric Cancer and Signet Ring Cell Histology. Br J Surg (2010) 97(5):732–6. doi: 10.1002/bjs.6941
44. Lee SH, Jee SR, Kim JH, Seol SY. Intramucosal Gastric Cancer: The Rate of Lymph Node Metastasis in Signet Ring Cell Carcinoma is as Low as That in Well-Differentiated Adenocarcinoma. Eur J Gastroenterol Hepatol (2015) 27(2):170–4. doi: 10.1097/meg.0000000000000258
45. Li C, Kim S, Lai JF, Hyung WJ, Choi WH, Choi SH, et al. Advanced Gastric Carcinoma With Signet Ring Cell Histology. Oncology (2007) 72(1-2):64–8. doi: 10.1159/000111096
46. Li H, Huo ZB, Chen SB, Li H, Wu DC, Zhai TS, et al. Feasibility Study on Expanded Indication for Endoscopic Submucosal Dissection of Intramucosal Poorly Differentiated Early Gastric Cancer. World J Gastroenterol (2016) 22(29):6736–41. doi: 10.3748/wjg.v22.i29.6736
47. Lu M, Yang Z, Feng Q, Yu M, Zhang Y, Mao C, et al. The Characteristics and Prognostic Value of Signet Ring Cell Histology in Gastric Cancer: A Retrospective Cohort Study of 2199 Consecutive Patients. Medicine (2016) 95(27):e4052. doi: 10.1097/md.0000000000004052
48. Nakamura R, Omori T, Mayanagi S, Irino T, Wada N, Kawakubo H, et al. Risk of Lymph Node Metastasis in Undifferentiated-Type Mucosal Gastric Carcinoma. World J Surg Oncol (2019) 17:32. doi: 10.1186/s12957-019-1571-2
49. Nam MJ, Oh SJ, Oh CA, Kim DH, Bae YS, Choi MG, et al. Frequency and Predictive Factors of Lymph Node Metastasis in Mucosal Cancer. J Gastric Cancer (2010) 10(4):162–7. doi: 10.5230/jgc.2010.10.4.162
50. Otsuji E, Yamaguchi T, Sawai K, Takahashi T. Characterization of Signet Ring Cell Carcinoma of the Stomach. J Surg Oncol (1998) 67(4):216–20. doi: 10.1002/(sici)1096-9098(199804)67:4<216::Aid-jso2>3.0.Co;2-b
51. Park JM, Jang YJ, Kim JH, Park SS, Park SH, Kim SJ, et al. Gastric Cancer Histology: Clinicopathologic Characteristics and Prognostic Value. J Surg Oncol (2008) 98(7):520–5. doi: 10.1002/jso.21150
52. Shim JH, Song KY, Kim HH, Han SU, Kim MC, Hyung WJ, et al. Signet Ring Cell Histology Is Not an Independent Predictor of Poor Prognosis After Curative Resection for Gastric Cancer: A Propensity Analysis by the KLASS Group. Medicine (2014) 93(27):e136. doi: 10.1097/md.0000000000000136
53. Taghavi S, Jayarajan SN, Davey A, Willis AI. Prognostic Significance of Signet Ring Gastric Cancer. J Clin Oncol: Off J Am Soc Clin Oncol (2012) 30(28):3493–8. doi: 10.1200/jco.2012.42.6635
54. Tang CT, Chen Y, Zeng C. Prognostic Analysis of Gastric Signet Ring Cell Carcinoma and Mucinous Carcinoma: A Propensity Score-Matched Study and Competing Risk Analysis. Aging (2020) 12:22059–77. doi: 10.18632/aging.104048
55. Tong JH, Sun Z, Wang ZN, Zhao YH, Huang BJ, Li K, et al. Early Gastric Cancer With Signet-Ring Cell Histologic Type: Risk Factors of Lymph Node Metastasis and Indications of Endoscopic Surgery. Surgery (2011) 149(3):356–63. doi: 10.1016/j.surg.2010.07.006
56. Wang JM, Zhou LY, Lin SR, Ding SG. Characteristics and Risk Factors of Lymphatic Metastasis in Early Gastric Cancer. Zhonghua nei ke za zhi [Chinese J Internal Med J (2010) 49(4):297–300.
57. Yoon HJ, Kim YH, Kim JH, Kim H, Kim H, Park JJ, et al. Are New Criteria for Mixed Histology Necessary for Endoscopic Resection in Early Gastric Cancer? Pathol Res Pract (2016) 212(5):410–4. doi: 10.1016/j.prp.2016.02.013
58. Zhang M, Zhu G, Zhang H, Gao H, Xue Y. Clinicopathologic Features of Gastric Carcinoma With Signet Ring Cell Histology. J Gastroint Surg (2010) 14(4):601–6. doi: 10.1007/s11605-009-1127-9
59. Zhao B, Lu H, Luo R, Bao S, Mei D, Xu H, et al. Different Clinicopathologic Features and Prognostic Significance of Signet Ring Cell Histology in Early and Locally Advanced Gastric Cancer Patients. Clinics Res Hepatol Gastroenterol (2021) 45(1):101454. doi: 10.1016/j.clinre.2020.05.006
60. Zhu ZL, Shi HP, Beeharry MK, Feng TN, Yan M, Yuan F, et al. Expanding the Indication of Endoscopic Submucosal Dissection for Undifferentiated Early Gastric Cancer Is Safe or Not? Asian J Surg (2020) 43(4):526–31. doi: 10.1016/j.asjsur.2019.08.006
61. Zou Y, Wu L, Yang Y, Shen X, Zhu C. Risk Factors of Tumor Invasion and Node Metastasis in Early Gastric Cancer With Undifferentiated Component: A Multicenter Retrospective Study on Biopsy Specimens and Clinical Data. Ann Trans Med (2020) 8(6):360. doi: 10.21037/atm.2020.02.42
62. Zu H, Wang H, Li C, Xue Y. Clinicopathologic Characteristics and Prognostic Value of Various Histological Types in Advanced Gastric Cancer. Int J Clin Exp Pathol (2014) 7(9):5692–700.
63. Ellithi M, Elnair R, Abdullah HM. Clinical Characteristics and Outcomes of Signet Ring Cell Carcinoma of the Stomach: A Retrospective Analysis of SEER Database. J Clin Oncol (2020) 38(15):suppl: e16572. doi: 10.1200/JCO.2020.38.15_suppl.e16572
64. Pernot S, Voron T, Perkins G, Lagorce-Pages C, Berger A, Taieb J. Signet-Ring Cell Carcinoma of the Stomach: Impact on Prognosis and Specific Therapeutic Challenge. World J Gastroenterol (2015) 21(40):11428–38. doi: 10.3748/wjg.v21.i40.11428
65. Matsui M, Kojima O, Kawakami S, Uehara Y, Takahashi T. The Prognosis of Patients With Gastric Cancer Possessing Sex Hormone Receptors. Surg Today (1992) 22(5):421–5. doi: 10.1007/bf00308791
66. Kim HW, Kim JH, Lim BJ, Kim H, Kim H, Park JJ, et al. Sex Disparity in Gastric Cancer: Female Sex Is a Poor Prognostic Factor for Advanced Gastric Cancer. Ann Surg Oncol (2016) 23(13):4344–51. doi: 10.1245/s10434-016-5448-0
67. Fitzgerald RC, Hardwick R, Huntsman D, Carneiro F, Guilford P, Blair V, et al. Hereditary Diffuse Gastric Cancer: Updated Consensus Guidelines for Clinical Management and Directions for Future Research. J Med Genet (2010) 47(7):436–44. doi: 10.1136/jmg.2009.074237
68. Sugihara H, Hattori T, Fukuda M, Fujita S. Cell Proliferation and Differentiation in Intramucosal and Advanced Signet Ring Cell Carcinomas of the Human Stomach. Virchows Pathol Anat Histopathol (1987) 411(2):117–27. doi: 10.1007/bf00712735
69. Japanese Gastric Cancer Treatment Guidelines 2010 (Ver. 3). Gastric Cancer: Off J Int Gastric Cancer Assoc Jpn Gastric Cancer Assoc (2011) 14(2):113–23. doi: 10.1007/s10120-011-0042-4
70. Kwak DS, Min YW, Lee JH, Kang SH, Jang SH, Lee H, et al. Outcomes of Endoscopic Submucosal Dissection for Early Gastric Cancer With Undifferentiated-Type Histology: A Clinical Simulation Using a non- Selected Surgical Cohort. Gut Liver (2018) 12(3):263–70. doi: 10.5009/gnl17247
71. Jiang L, Ma Z, Ye X, Kang W, Yu J. Clinicopathological Factors Affecting the Effect of Neoadjuvant Chemotherapy in Patients With Gastric Cancer. World J Surg Oncol (2021) 19(1):44. doi: 10.1186/s12957-021-02157-x
72. Li Y, Zhu Z, Ma F, Xue L, Tian Y. Gastric Signet Ring Cell Carcinoma: Current Management and Future Challenges. Cancer Manage Res (2020) 12:7973–81. doi: 10.2147/cmar.S268032
73. Turgeon MK, Gamboa AC, Rupji M, Lee RM, Switchenko JM, El-Rayes BF, et al. Should Signet Ring Cell Histology Alter the Treatment Approach for Clinical Stage I Gastric Cancer? Ann Surg Oncol (2021) 28(1):97–105. doi: 10.1245/s10434-020-08714-0
74. Shu Y, Zhang W, Hou Q, Zhao L, Zhang S, Zhou J, et al. Prognostic Significance of Frequent CLDN18-ARHGAP26/6 Fusion in Gastric Signet-Ring Cell Cancer. Nat Commun (2018) 9(1):2447. doi: 10.1038/s41467-018-04907-0
Keywords: gastric neoplasm, signet-ring cell carcinoma, prognosis, meta-analysis, biological behavior
Citation: Zhao S, Lv L, Zheng K, Tian Y, Zheng J-C and Jiang C-G (2021) Prognosis and Biological Behavior of Gastric Signet-Ring Cell Carcinoma Better or Worse: A Meta-Analysis. Front. Oncol. 11:603070. doi: 10.3389/fonc.2021.603070
Received: 05 September 2020; Accepted: 11 June 2021;
Published: 30 June 2021.
Edited by:
Valeria Barresi, University of Verona, ItalyReviewed by:
Maria Bencivenga, University of Verona, ItalyYang Li, Chinese Academy of Medical Sciences and Peking Union Medical College, China
Copyright © 2021 Zhao, Lv, Zheng, Tian, Zheng and Jiang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Cheng-Gang Jiang, ZGVhbmppYW5nY2dAMTYzLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Shuai Zhao1†
Shuai Zhao1† Cheng-Gang Jiang
Cheng-Gang Jiang