- Hematology Unit, University of Siena, Azienda Ospedaliero Universitaria Senese, Siena, Italy
Multiple myeloma survival has significantly improved in recent years, due to novel agents that are available for treatment. The anti-CD38 monoclonal antibody Daratumumab is particularly efficient for patients with relapse/refractory disease, and many studies have shown its unprecedented efficacy also as a first treatment. However, to avoid the incidence of infusion reactions, long infusion schedules of 8 h at first dose and 4 h in the following doses are required, which can reduce the compliance of patients and health care professionals. A reduced infusion time of 90 min has been reported previously, but data are missing on the prolonged safety of this over time as well as the efficacy of this approach. In this work, we investigate the safety of 484 rapid Daratumumab infusions given early after the second dose over a 22 months period in 39 myeloma patients.
Introduction
Multiple myeloma (MM) is a plasma cell disorder, the prognosis of which has dramatically improved in the last years thanks to new immunomodulatory drugs (IMIDs), proteasome inhibitors (PIs), and monoclonal antibodies (mAbs), in relapsed/refractory disease and at diagnosis (1–6). Daratumumab, a CD38 antagonist, is a human immunoglobulin G1 kappa (IgG1κ) monoclonal antibody that binds CD38 expressed on the cell surface in a variety of hematological malignancies, including myeloma, lymphomas, and leukemias, as well as on other cell types and tissues with various expression levels. Daratumumab acts through different mechanisms of action including an immune-mediated effect: i) antibody-dependent cytotoxicity (ADC), ii) complement-dependent cytotoxicity (CDC), and iii) antibody-dependent cellular phagocytosis (ADCP). It can also cause apoptosis through a direct antitumor effect or it can act as an immune modulator to decrease immunosuppression or infuence CD38 enzymatic inhibition. When Daratumumab was used as a single drug in relapsed/refractory MM patients who previously received a median of four lines of therapy, it led to an unprecedented response of 31% (ORR) and a median OS of 20.1 months (7). CASTOR and POLLUX studies demonstrated that the addition of Daratumumab to bortezomib and lenalidomide, respectively, prolonged PFS and OS in the relapsed refractory setting (8, 9). Daratumumab combinations with pomalidomide and carfilzomib have been used for relapsed refractory disease, and other combinations are now approved also at diagnosis (10–14). In particular, the combination with pomalidomide and dexamethasone has been tested in a cohort of heavily pretreated patients, giving an ORR of 60% (17% CR or better), while Daratumumab combined with carfilzomib and dexamethasone did not reach PFS at a median follow-up of 17 months. In the Alcyone trial (12) Daratumumab–VMP (velcade, melphalan, prednisone) compared to VMP alone showed a superior PFS (36.4 vs 19.3 months, respectively) and OS (78% vs 68.9%, respectively, at 40 months of follow up) in newly diagnosed MM patients (NDMM) that were not eligible for transplantation. Furthermore, the MAIA study (13) showed the superiority of Daratumumab in NDMM patients when comparing Dara–Rd (Daratumumab, Revlimid, Dexamethasone) with Rd alone. PFS was superior for Dara–Rd vs Rd (not reached vs 31.9 months), with 24% of minimal residual disease (MRD) showing negativity in the Dara–Rd group. Finally, the Cassiopeia study (14) evaluated Daratumumab–VTD (velcade, thalidomide, Dexamethasone) vs VTD in NDMM patients in pre-transplant induction therapy and post-transplant consolidation. Dara–VTD was superior in terms of the depth of response (MRD negativity of 64% vs 44%) and PFS (93% vs 85% at 18 months). These studies showed the good tolerability of daratumumab; however, due to the expression of CD38 on airway smooth muscle cells, infusion-related reactions (IRRs) are very common at the first dose, accounting for about 40% of patients and presenting with symptoms (cough, wheezing, rhinorrhea) similar to those of allergic rhinitis. Daratumumab as a monotherapy or when combined with revlimid dexamethasone is given intravenously (IV), every week for 8 weeks, then every 2 weeks for 16 weeks, and then every month, while the Dara–Velcade regimen (DVd) is given weekly with 9 doses, then every 3 weeks with 5 doses, and then every 4 weeks (15). It is worthy of note that the infusion duration is particularly long for the first infusion (7 h), with median durations of 4.3 and 3.5 h for second and other infusions, respectively. Moreover, if an infusion-related reaction presents, the infusion may take longer, worsening the patient’s quality of life and also affecting the planning of daily practice for physicians and nurses. Splitting the first dose over two days reduces the length of each infusion (4 h each), although the patient has to come to the hospital twice. Strategies to reduce the infusion time have been reported (16): in one study, the authors showed safety in 28 patients with MM with an infusion time of 90 min starting from a dose >10 in the majority of cases. In 11 out of 28 patients, a 90 min infusion was given from the third dose. No report, however, has been made regarding the prolonged safety of rapid Daratumumab infusions over time, nor regarding the efficacy of the drug with this modified schedule. It is worthy of note that the subcutaneous formulation has been tested in many trials and is about to be introduced in clinical practice (17).
Materials and Methods
Patient Characteristics
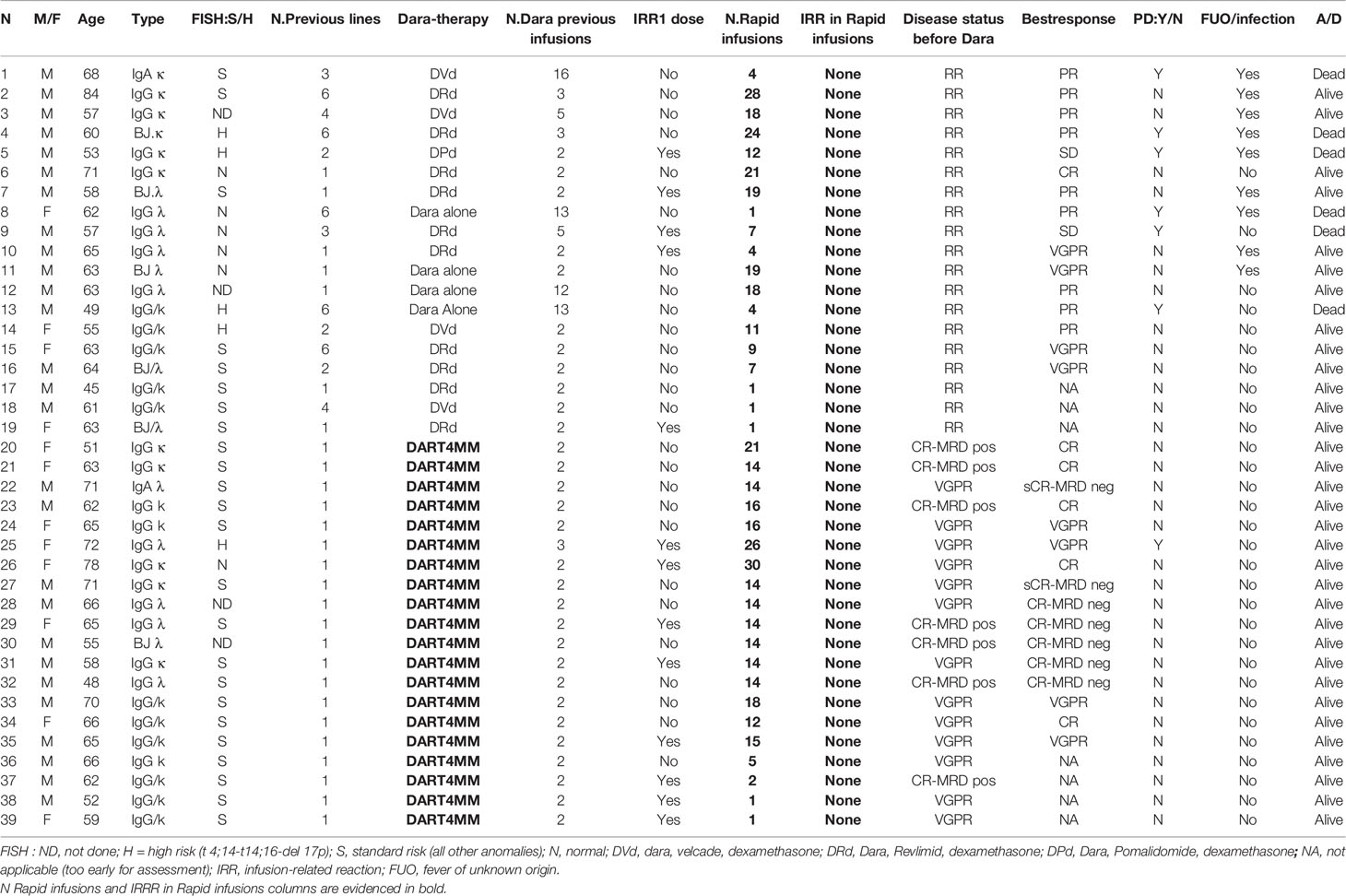
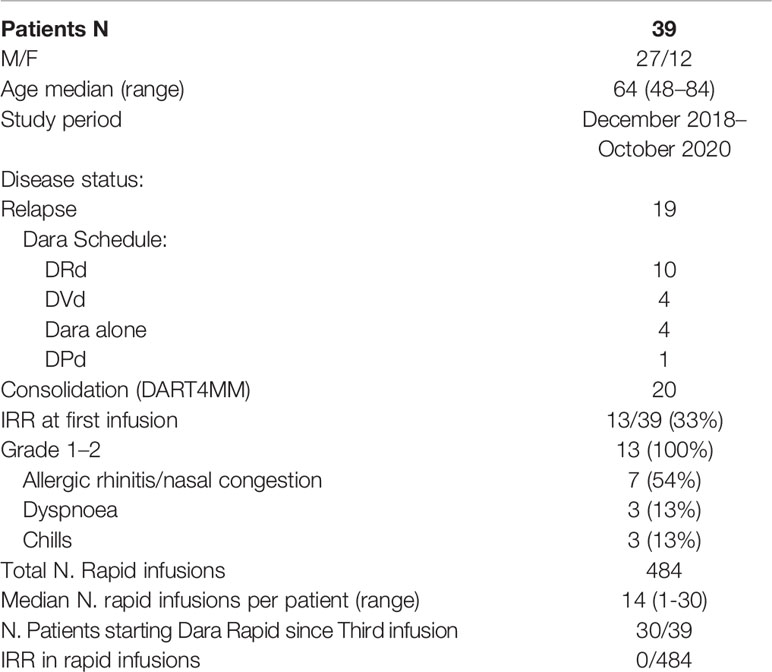
From December 2018 to October 2020, we performed an observational prospective single-arm, single-center study, with the twofold aim of reducing the time of infusion and the stay of the patient in the day hospital. The primary endpoint of the study was the safety of rapid Daratumumab infusions. The secondary endpoint was the safety of the first Daratumumab infusions. Patients receiving Daratumumab as standard clinical practice at relapse and patients enrolled in clinical trials at diagnosis could be enrolled. Patient characteristics are reported in Table 1. Nineteen patients were affected by RRMM and received Daratumumab alone or in combination with other agents (lenalidomide, bortezomib, pomalidomide), and 20 patients received Daratumumab as consolidation therapy in the protocol DART4MM (this trial was registered at ClinicalTrials.gov with the number NCT039922170; EUDARACT N. 2018-000386-36: Daratumumab as consolidation therapy in patients who already achieved >VGPR/MRD positivity during first line therapy). Ethical approval was obtained locally, and DART4MM was also approved by the Italian Dug Regulatory Agency (AIFA, with a specific approval amendment for rapid Daratumumab infusions).
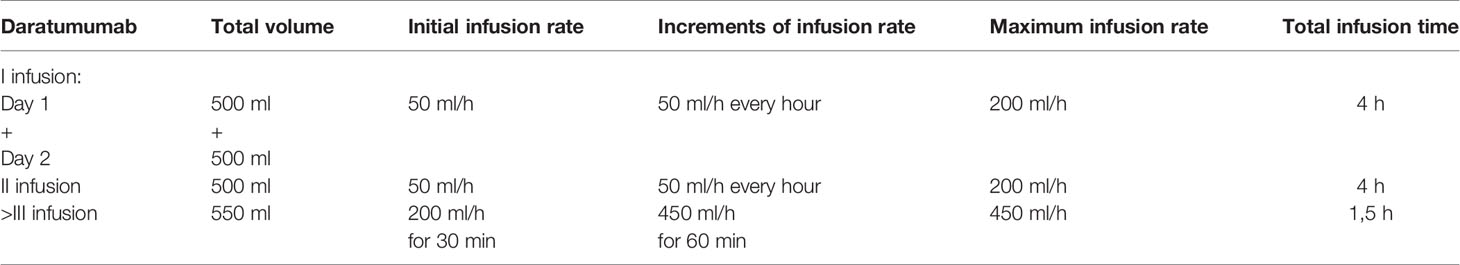
Treatment Schedule
The infusion schedule is reported in Table 2. The first dose of daratumumab was split into day 1 and day 2 with a median infusion duration of 4 h each. Rapid infusion could start from the third dose if no IRR was seen in the previous infusion (second). A rapid infusion rate was calculated to deliver 20% of the dose over 30 min (200 ml/h), and then the rate was increased to deliver the remaining 80% over 60 min (450 ml/h). This resulted in a 90 min estimated infusion time (total volume 550 ml). Premedication drugs, according to the current clinical practice, were corticosteroids (IV dexamethasone 20 mg), antipyretic (oral paracetamol 1.000 mg), and antihistamine (IV chlorphenamine maleate 10 mg); a two-puff inhalation of β-adrenergic bronchodilator (salbutamol) given 20 min before the first infusion was chosen instead of montelukast after a referral with a local pneumologist. All patients received antiviral and antibacterial prophylaxis (Acyclovir 400 mg twice daily, trimethoprim–sulfamethoxazole, 160 + 800 mg twice daily twice/week). All patients treated with lenalidomide or pomalidomide received thromboprophylaxis with low-dose aspirin (18). Safety assessments included any adverse events (AEs), physical examinations, clinical laboratory parameters, vital signs measurement, and Eastern Cooperative Oncology Group performance status. AEs were assessed using the National Cancer Institute Common Terminology Criteria for Adverse Events Version 4.03 (19). Responses were defined according to IMWG criteria (20). Minimal residual disease (MRD) was evaluated by next-generation flow on bone marrow aspirate with a sensitivity of 10-6 (Euroflow criteria) (21).
Results
A total of 39 consecutive patients (27 M/12 F) with a median age of 64 years (range 48–84 years) were referred to our Hematology center and received a rapid infusion of daratumumab, leading to a total of 484 rapid infusions (median number 14, range 1–30) over a 22 month observational period (Table 1). No serious adverse event was recorded in all patients during rapid infusion. Six out of 39 (15%) patients (one with associated renal amyloidosis) had been previously treated with Daratumumab on entry to the study. They had already received a median of 12 infusions (range 5–16), and no IRRs were registered during subsequent rapid infusions (Table 3). Pre-existing chronic obstructive pulmonary disease or asthma were absent in previous patient history in 38 out of 39 patients. One patient reported smoking activity in their past history; they were then referred to the pneumologist, and a therapy with β−adrenergic bronchodilator was administered three days before the first infusion.
Infusion-Related Reactions at First Dose During Daratumumab Long-Infusion Treatment
IRRs at the first Daratumumab split infusion were seen in 13 of 39 patients (33%): five were in RR MM patients, while the other 8 patients were included in the DART4MM study. All IRRs at the first dose happened on day 1; they were mild and of grades 1–2: (seven showed allergic rhinitis, three showed dyspnea, and three exhibited chills), and the drug was temporarily stopped in all cases. Allergic rhinitis was treated with IV hydrocortisone hemisuccinate at 100/200 mg, chlorphenamine maleate, and salbutamol. All bronchospasms were treated with salbutamol aerosol: in one case, IV chlorphenamine maleate at 10 mg was also added, and in two cases, hydrocortisone hemisuccinate at 200 mg was also added. Chills were treated with corticosteroids IV in all cases. The median time to recovery after IRRs was 30 min. All patients who had an IRR during the first split dose did not have other reactions during subsequent infusions, regardless of the infusion time.
Infusion-Related Reactions at Rapid Infusions
Thirty-three of 39 (79%) patients received Daratumumab as a rapid infusion upfront (30 at the third infusion, day 15, cycle 1; and three patients at the fourth infusion, day 22, cycle 1). No subsequent IRRs were seen. Premedication was reduced after dose >10, when Daratumumab was used as a monotherapy or in the DART4MM study, with oral antihistamine (loratadine 10 mg), dexamethasone 10 mg (IV), and paracetamol 500 mg (oral) in all patients. Moreover, in 6 patients, corticosteroids were reduced to 4 mg dexamethasone after dose >14.
Adverse Events That Were Not Infusion Related
Treatment-emergent adverse events (TEAEs) during therapy and that were not infusion-related were similar to other populations of patients treated with daratumumab, all of grades 1–2 (Hematological TEAEs: lymphopenia in 12 patients, 31%; anemia in 9, 23%; thrombocytopenia in 9, 23%; neutropenia in 9, 23%. Non-hematological TEAEs: arthralgia in 8 patients, 20%; fever of unknown origin (FUO) in 8 patients, 20%). Two patients who received Daratumumab in combination with lenalidomide had pneumonia/infection and stopped treatment: one patient had a septic shock requiring emergency care unit admission—at last follow-up, they are alive and in VGPR—the other patient had bacterial pneumonia (staphylococcus aureus), maintaining a stable response. Both patients had grade 3 neutropenia at the time of hospitalization.
Response to Treatment
During Daratumumab therapy, 23 of 32 evaluable patients had a response improvement (72%). In particular, in the DART4MM protocol, 9 of 16 patients showed an improved response, from a VGPR or CR-MRD pos to a CR or CR-MRD neg by next-generation flow, while in the evaluable RRMM patients, 14 of 16 had at least a PR. Six of 39 patients exhibited a halted progression: three patients were treated at line 6, two at line 3 and one patient at line 2 of therapy, respectively. The latter maintained an SD for 6 months with Daratumumab before progressing (who received Daratumumab for 6 months while maintaining a SD).
Discussion
In this study, we describe the largest population of MM patients so far reported to receive rapid infusions of Daratumumab from cycle 1 day 15 (n = 30) with the longest follow-up to evaluate safety. In fact, the long follow-up period reported of 22 months makes the study quite reliable to evaluate both short and long-term safety. The availability of Daratumumab has revolutionized treatment practice for MM, leading to a marked improvement in outcomes for the treatment of MM patients. However, the current administration schedules can negatively impact patient’s compliance and out-patient care system organization. The rapid infusion Daratumumab schedule here reported provides a practical and safe solution that has a positive impact on resource utilization. Another point of interest is that rapid infusion was revealed to be particularly convenient during the Covid-19 emergency, reducing patients’ time spent in hospitals and reducing social contacts for patients and staff. Rapid infusions have been tested with other monoclonal antibodies in the past; for example, rapid 60 min infusions of rituximab (IgG1 chimeric anti CD20 antibody) for B cell lymphoproliferative disorders have been adopted at our institution and many others since 2006 (22, 23). The efficacy of rituximab was maintained and patients were rapidly dismissed from the clinic. Rapid Daratumumab infusion has very recently been reported in another trial (24) in which 53 MM patients received rapid infusions and no difference was seen in terms of IRRs with respect to 47 patients receiving long infusions (1.9% vs 4.3%). The latter study compared rapid infusions vs standard IV infusions: 53 patients received rapid infusions of Daratumumab, but only 18 received the rapid infusion starting from cycle 1 day 15 upfront (as in our study). Importantly, the authors showed a cost saving for rapid infusions: the total costs estimated for a 52 week regimen of Daratumumab infused at standard and rapid rates were $137,200 and $122,200 (P <.001), respectively. However, in comparison to our study, there is no report on the safety of the method in long-term follow-up, nor regarding the efficacy of the drug. Recent studies have also shown the good safety and efficacy of the subcutaneous (SC) infusion with a dose of 1,800 mg with recombinant human hyaluronidase PH20 (rHuPH20)(concentration 30,000 U; in 15 ml) in a single, premixed vial that was administered over 3 to 5 min, and this formulation will be available soon (12, 25). The serum pharmacokinetic (PK) concentrations and efficacy achieved with an 1800 mg SC dose were consistent with what has been observed for Daratumumab 16 mg/kg IV in patients with RRMM. Certainly, SC administration will be more utilized in the near future, but we have to consider that, despite the reduced number of IRRs during SC therapy compared to the IV formulation, almost all reactions happened during the first 6 h after injection. Although PK was not performed in the present study, efficacy was maintained in our study. To our knowledge, no study has so far reported on the efficacy of rapid infusions; however, even considering the small number of patients treated, the treatment efficacy appeared to be quite in line with that expected after the standard infusion length. In conclusion, our study demonstrates that a rapid infusion of Daratumumab after the second dose is safe and well tolerated. As such, while waiting for the SC formulation, this schedule can be adopted by many hematological centers to improve MM patients’ quality of life and allow more sustainable out-patient care infusion planning.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Comitato Etico Regionale-Regione toscana, area vasta sud est; Agenzia Italiana del Farmaco. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
AG designed the study and wrote the manuscript. MD, EZ, AF, and EC were involved in the patient treatment. AS and DR performed the laboratory analysis. FB, VS, and BM collected the data and helped to write the manuscript. MB supervised the study and revised the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The handling Editor declared a past co-authorship with one of the authors AG.
Acknowledgments
We thank patients and staff. We thank the Italian Association against Lymphoma, Myeloma, and Leukemia (Siena section) for patient support. This work has been presented in part as a poster at the International Myeloma Workshop in Boston, 12–15 September 2019.
References
1. Gozzetti A, Candi V, Papini G. Bocchia. Therapeutic advancements in multiple myeloma. Front Oncol (2014) 4:241. doi: 10.3389/fonc.2014.00241
2. Mohty M, Terpos E, Mateos MV, Cavo M, Lejniece S, Beksac M, et al. EMMOS Investigators. Multiple Myeloma Treatment in Real-world Clinical Practice: Results of a Prospective, Multinational, Noninterventional Study. Clin Lymphoma Myeloma Leuk (2018) 18:e401–19. doi: 10.1016/j.clml.2018.06.018
3. Kumar SK, Rajkumar SV, Dispenzieri A, Lacy MQ, Hayman SR, Buadi FK, et al. Improved survival in multiple myeloma and the impact of novel therapies. Blood (2008) 111:2516–20. doi: 10.1182/blood-2007-10-116129
4. Jurczyszyn A, Grzasko N, Gozzetti A, Czepiel J, Cerase A, Hungria V, et al. Central nervous system involvement by multiple myeloma: A multi-institutional retrospective study of 172 patients in daily clinical practice. Am J Hematol (2016) 91:575–80. doi: 10.1002/ajh.24351
5. Ocio EM, Richardson PG, Rajkumar SV, Palumbo A, Mateos MV, Orlowski R, et al. New drugs and novel mechanisms of action in multiple myeloma 2013: a report from the International Myeloma Working group (IMWG). Leukemia (2014) 28:525–42. doi: 10.1038/leu.2013.350
6. Gozzetti A, Cerase A. Novel agents in CNS myeloma treatment. Cent Nerv Syst Agents Med Chem (2014) 14:23–7. doi: 10.2174/1871524914999140818111514
7. Usmani SZ, Weiss BM, Plesner T, Bahlis NJ, Belch A, Lonial S, et al. Clinical efficacy of daratumumab monotherapy in patients with heavily pretreated relapsed or refractory multiple myeloma. Blood (2016) 128:37–44. doi: 10.1182/blood-2016-03-705210
8. Dimopoulos MA, Oriol A, Nahi H, San-Miguel J, Bahlis NJ, Usmani SZ, et al. POLLUX Investigators. Daratumumab, Lenalidomide, and Dexamethasone for Multiple Myeloma. N Engl J Med (2016) 375:1319–31. doi: 10.1056/NEJMoa1607751
9. Palumbo A, Chanan-Khan A, Weisel K, Nooka AK, Masszi T, Beksac M, et al. CASTOR Investigators. Daratumumab, Bortezomib, and Dexamethasone for Multiple Myeloma. N Engl J Med (2016) 375:754–66. doi: 10.1056/NEJMoa1606038
10. Chari A, Suvannasankha A, Fay JW, Arnulf B, Kaufman JL, Ifthikharuddin JJ, et al. Daratumumab plus pomalidomide and dexamethasone in relapsed and/or refractory multiple myeloma. Blood (2017) 130:974–81. doi: 10.1182/blood-2017-05-785246
11. Dimopoulos M, Quach H, Mateos MV, Landgren O, Leleu X, Siegel D, et al. Carfilzomib, dexamethasone, and daratumumab versus carfilzomib and dexamethasone for patients with relapsed or refractory multiple myeloma (CANDOR): results from a randomised, multicentre, open-label, phase 3 study. Lancet (2020) 396:186–97. doi: 10.1016/S0140-6736(20)30734-0
12. Mateos MV, Cavo M, Blade J, Dimopoulos MA, Suzuki K, Jakubowiak A, et al. Overall survival with daratumumab, bortezomib, melphalan, and prednisone in newly diagnosed multiple myeloma (ALCYONE): a randomised, open-label, phase 3 trial. Lancet (2020) 395:132–41. doi: 10.1016/S0140-6736(19)32956-3
13. Facon T, Kumar S, Plesner T, Orlowski RZ, Moreau P, Bahlis N, et al. MAIA Trial Investigators. Daratumumab plus Lenalidomide and Dexamethasone for Untreated Myeloma. N Engl J Med (2019) 380(22):2104–15. doi: 10.1056/NEJMoa1817249
14. Moreau P, Attal M, Hulin C, Arnulf B, Belhadj K, Benboubker L, et al. Bortezomib, thalidomide, and dexamethasone with or without daratumumab before and after autologous stem-cell transplantation for newly diagnosed multiple myeloma (CASSIOPEIA): a randomised, open-label, phase 3 study. Lancet (2019) 394(10192):29–38. doi: 10.1016/S0140-6736(19)31240-1
15. DARZALEX® (daratumumab) injection, for intravenous use. May 2020 (2019). Available at: http://www.janssenlabels.com/package-insert/product-monograph/prescribing-information/DARZALEX-pi.pdf.
16. Barr H, Dempsey J, Waller A, Huang Y, Williams N, Sharma N, et al. Ninety-minute daratumumab infusion is safe in multiple myeloma. Leukemia (2018) 32:2495–518. doi: 10.1038/s41375-018-0120-2
17. Usmani SZ, Nahi H, Mateos MV, van de Donk NWCJ, Chari A, Kaufman JL, et al. Subcutaneous delivery of daratumumab in relapsed or refractory multiple myeloma. Blood (2019) 134:668–77. doi: 10.1182/blood.2019000667
18. Cini M, Zamagni E, Valdré L, Palareti G, Patriarca F, Tacchetti P, et al. Thalidomide-dexamethasone as up-front therapy for patients with newly diagnosed multiple myeloma: thrombophilic alterations, thrombotic complications, and thromboprophylaxis with low-dose warfarin. Eur J Haematol (2010) 84:484–92. doi: 10.1111/j.1600-0609.2010.01434.x
19. Common terminology criteria for adverse events (CTCAE) (2010): Version 4.03 (2020). Available at: https://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03, US Department of Health and Human Services, National Institutes of Health, National Cancer Institute.
20. Kumar S, Paiva B, Anderson KC, Durie B, Landgren O, Moreau P, et al. International Myeloma Working Group consensus criteria for response and minimal residual disease assessment in multiple myeloma. Lancet Oncol (2016) 17:e328–46. doi: 10.1016/S1470-2045(16)30206-6
21. Flores-Montero J, Sanoja-Flores L, Paiva B, Puig N, García-Sánchez O, Böttcher S, et al. Next Generation Flow for highly sensitive and standardized detection of minimal residual disease in multiple myeloma. Leukemia (2017) 31:2094–103. doi: 10.1038/leu.2017.29
22. Sehn LH, Donaldson J, Filewich A, Fitzgerald C, Gill KK, Runzer N, et al. Rapid infusion rituximab in combination with corticosteroid-containing chemotherapy or as maintenance therapy is well tolerated and can safely be delivered in the community setting. Blood (2007) 109:4171–3. doi: 10.1182/blood-2006-11-059469
23. Fabbri A, Gozzetti A, Lazzi S, Lenoci M, D’Amuri A, Leoncini L, et al. Activity of rituximab monotherapy in refractory splenic marginal zone lymphoma complicated with autoimmune hemolytic anemia. Clin Lymphoma Myeloma (2006) 6:496–9. doi: 10.3816/CLM.2006.n.033
24. Hamadeh IS, Reese ES, Arnall JR, Kachur E, Martin AL, Schneider M, et al. Safety and Cost Benefits of the Rapid Daratumumab Infusion Protocol. Clin Lymphoma Myeloma Leuk (2020) 7:S2152–2650(20)30105-1. doi: 10.1016/j.clml.2020.02.014
25. Mateos MV, Nahi H, Legiec W, Grosicki S, Vorobyev V, Spicka I, et al. Subcutaneous versus intravenous daratumumab in patients with relapsed or refractory multiple myeloma (COLUMBA): a multicentre, open-label, non-inferiority, randomised, phase 3 trial. Lancet Haematol (2020) 7:e370–80. doi: 10.1016/S2352-3026(20)30070-3
Keywords: Daratumumab, multiple myeloma, rapid infusion, safety, efficacy
Citation: Gozzetti A, Bacchiarri F, Sammartano V, Defina M, Sicuranza A, Mecacci B, Zappone E, Cencini E, Fabbri A, Raspadori D and Bocchia M (2020) Long-Term Safety of Rapid Daratumumab Infusions in Multiple Myeloma Patients. Front. Oncol. 10:570187. doi: 10.3389/fonc.2020.570187
Received: 06 June 2020; Accepted: 13 November 2020;
Published: 21 December 2020.
Edited by:
María-Victoria Mateos, University Hospital of Salamanca, SpainReviewed by:
Elena Zamagni, University of Bologna, ItalyAlessandra Larocca, University Hospital of the City of Health and Science of Turin, Italy
Copyright © 2020 Gozzetti, Bacchiarri, Sammartano, Defina, Sicuranza, Mecacci, Zappone, Cencini, Fabbri, Raspadori and Bocchia. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alessandro Gozzetti, Z296emV0dGlAdW5pc2kuaXQ=
 Alessandro Gozzetti
Alessandro Gozzetti Francesca Bacchiarri
Francesca Bacchiarri Emanuele Cencini
Emanuele Cencini Alberto Fabbri
Alberto Fabbri Donatella Raspadori
Donatella Raspadori Monica Bocchia
Monica Bocchia