- Department of Nuclear Medicine, Affiliated Cancer Hospital & Institute of Guangzhou Medical University, Guangzhou, China
Background: Solitary lesions in the extremities showing 99mTc-methylene diphosphate (MDP) uptake are often encountered on whole-body bone scan (WBS), and proper interpretation of this diagnostic method is important for patients with known cancer. The purpose of this study was to summarize the characteristics of solitary lesions in the extremities of patients with known cancer and to evaluate the diagnostic accuracy of single-photon emission computed tomography/computed tomography (SPECT/CT) in differentiating bone metastases from benign bone lesions.
Methods: This study was a retrospective review of 86 patients (54 males and 32 females; mean age, 57.88 ± 10.97 years; range, 31–81 years) with known cancer who underwent WBS and showed solitary lesions with 99mTc-MDP uptake in the extremities and then underwent SPECT/CT for further diagnosis. SPECT/CT images were independently interpreted by two experienced nuclear medicine physicians. The diagnostic accuracy of SPECT/CT in differentiating malignant from benign solitary lesions in the extremities was evaluated. Inter-reviewer agreement was assessed by using weighted k statistics. The standard diagnostic criterion was based on biopsy or radiologic follow-up over at least 12 months.
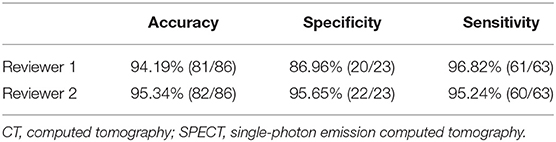
Results: In total, 23 bone metastases and 63 (73.26%) benign lesions were diagnosed. The majority (16/23, 69.57%) of bone metastases were found in the diaphyses. The most common benign bone disease was a benign bone tumor (31.75%, 20/63). The majority (13/20, 65%) of benign bone tumors were enchondromas. In the proximal and distal extremities, the most common disease was degeneration (27.11%, 16/59), followed by benign bone tumors and osteonecrosis of the femoral head (ONFH) (22.03%, 13/59). In the diaphyses of the extremities, bone metastasis was the most common disease, accounting for 64% (16/25) of the findings. For the SPECT/CT analysis, the accuracy was 94.19% (81/86) for reviewer 1 and 95.34% (82/86) for reviewer 2. The weighted kappa score for inter-reviewer agreement was 0.813.
Conclusion: When solitary disease of the extremities is detected by WBS in patients with known cancer, benign lesions may be more common than malignant lesions. SPECT/CT resulted in not only fewer equivocal lesions but also in higher diagnostic accuracy.
Introduction
99mTc-labeled methylene diphosphonate (99mTc-MDP) whole-body bone scan (WBS) is commonly used for detecting bone metastases in patients with known cancer with high sensitivity but low specificity (1). The extremities are not the most common site of bone metastasis, and only 9% of bone metastases initially appear as a single focus on WBS (2). However, some investigators have reported that some benign bone diseases that showed significantly increased 99mTc-MDP uptake in the extremities on WBS may mimic bone metastasis and should be further distinguished, especially in patients with known cancer (3–5). Currently, single-photon emission computed tomography/computed tomography (SPECT/CT) is superior to WBS alone in differentiating benign from malignant lesions (6–8). SPECT/CT not only provides information about the location, matrix changes, and appearance of soft tissues around the bone lesion but also characterizes abnormal radiotracer uptake (7, 9). To our knowledge, many studies have revealed that SPECT/CT increases the diagnostic accuracy for lesions identified on WBS (6, 7, 9, 10). However, the diagnostic accuracy of SPECT/CT in differentiating malignant from benign solitary lesions in the extremities detected by WBS is still unclear (3, 6, 7, 9). The literature on the general characteristics of solitary lesions in the extremities is sparse (3). Accordingly, the aim of our study was to summarize the characteristics of solitary lesions with 99mTc-MDP uptake in the extremities on WBS in patients with known cancer and to evaluate the diagnostic accuracy of SPECT/CT in differentiating bone metastasis from benign bone lesions.
Methods
Patients
Between March 2009 and March 2016, we undertook a single-center retrospective diagnostic study. The criteria for inclusion in the study were as follows: (1) patients with known malignancy, (2) patients who underwent 99mTc- MDP WBS for screening, (3) patients with areas of the extremities with abnormal radiotracer uptake who underwent SPECT/CT for further diagnosis, and (4) patients with more than 12 months of follow-up imaging after undergoing SPECT/CT. In addition, we excluded diseases with a definitive diagnosis of bone metastasis on WBS and without a definitive diagnosis within the follow-up period. Patients with benign bone lesions (such as fracture and degeneration) in the axial skeleton were not excluded. This study was approved by the local ethics committee, and because of the retrospective nature of the study, written informed consent was omitted.
Image Acquisition
All acquisitions were performed using a Philips SPECT/CT scanner (Netherlands). WBS was carried out 2–3 h after the intravenous injection of 99mTc-MDP at a dose of 15–25 mCi. After WBS acquisition, the images were directly interpreted by an experienced nuclear medicine physician. If doubtful lesions were identified on WBS, the addition of SPECT/CT was then immediately performed for anatomical localization and further diagnosis. First, a low-dose CT was performed for anatomic location and attenuation correction. CT data were acquired with exposure of 120 KV, 100 mAs/slice, window width of 15%, pitch of 1.25, and slice thickness of 5.0 mm. After CT acquisition, the SPECT acquisition protocol was started. The acquisition parameters for SPECT were as follows: 15% energy window at 140 keV and 64 × 64 matrix. Processing of the WBS and SPECT/CT images was performed on Jet Steam Workspace (Philips).
Data/Image Analysis
Images were independently interpreted by two experienced nuclear medicine physicians with knowledge of the history of malignancy. On WBS analysis, all 86 lesions were interpreted as equivocal. All bone lesions were classified on a 3-point scale as benign, malignant or equivocal on SPECT/CT. Malignant lesions were suggested by the presence of lytic, sclerotic, or mixed changes and a soft tissue mass. Furthermore, the presence of osteophytes or subchondral sclerosis was regarded as a clear sign of benignity. Lesions were classified as equivocal if they could not be confidently diagnosed as malignant or benign.
We evaluated the following features of the lesion: (1) location and (2) degree of osteoblastic activity. High activity was considered if the lesion showed uptake of 99mTc-MDP higher than that of the sternum on WBS images, moderate activity was considered if the lesion uptake was equal to that of the sternum, and low activity was considered if the lesion uptake was lower than that of the sternum.
Pathology and Follow-Up
The final decision regarding the true status of lesions was based on biopsy or follow-up imaging, which was made after consideration of all the available clinical information, including histological confirmation. This was then used as a criterion standard for this study. Pathologic analysis confirmed the diagnosis in 13 cases. In the remaining 73 cases, the patients had been diagnosed based on radiologic investigations (WBS and/or SPECT/CT, MRI) and follow-up of at least 12 months.
Statistical Analysis
Categorical data are expressed as numbers and frequencies (%). Continuous data are expressed as the means and standard deviations. Intergroup differences in the location and osteoblastic activity were analyzed using chi-square tests. The results were considered significant for a P-value of <0.05.
To evaluate the diagnostic accuracy of SPECT/CT for solitary lesions in the extremities, the sensitivity, specificity, and accuracy were calculated. Inter-reviewer agreement was estimated using a weighted k-statistic. A 95% confidence interval (CI) was chosen to determine the significance between groups, with P-values <0.05 indicating significant differences. The k-statistic was used for inter-reviewer reliability analysis. The k-values were interpreted as indicating poor (k < 0), slight (0 < k < 0.2), fair (0.21 < k < 0.4), moderate (0.41 < k < 0.6), substantial (0.61 < k < 0.8), and almost perfect (0.81 < k < 1.0) inter-observer agreement (11, 12). All statistical tests were performed using SPSS Statistics 17.0 software (SPSS Inc., Chicago, IL, USA).
Results
Patient Population
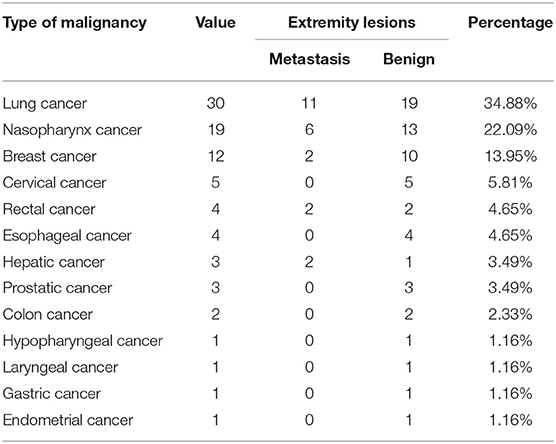
A total of 86 patients with 99mTc-MDP uptake in the extremities on WBS were included. Fifty-four patients were men, and 32 were women, ranging in age from 31 to 81 years (mean age 57.88 ± 10.97 years). The primary malignancies included lung cancer (n = 30), nasopharyngeal cancer (n = 19), breast cancer (n = 12), cervical cancer (n = 5), rectal cancer (n = 4), esophageal cancer (n = 4), hepatic cancer (n = 3), prostatic cancer (n = 3), and colon cancer (n = 2), and one patient each had hypopharyngeal cancer, laryngeal cancer, gastric cancer, endometrial cancer, as summarized in Table 1.
Patient Analysis
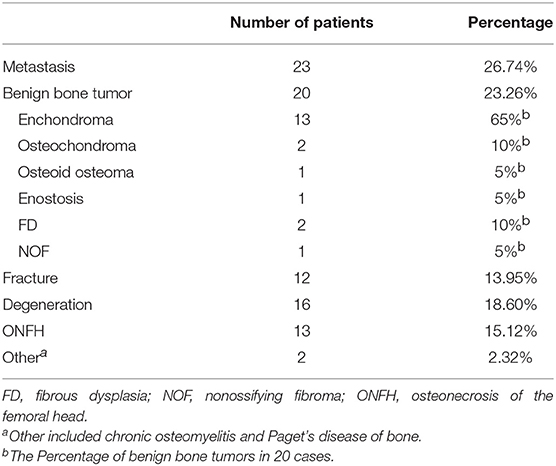
On the basis of the criterion standard, 63 (73.26%) lesions were diagnosed as benign bone disease, whereas 23 (26.74%) were determined to be malignant. All 86 lesions were classified into six types, as detailed in Table 2.
Site and Intensity of 99m Tc-MDP Uptake
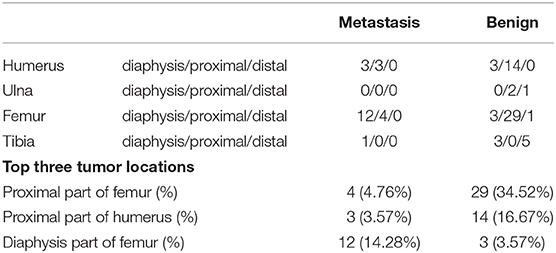
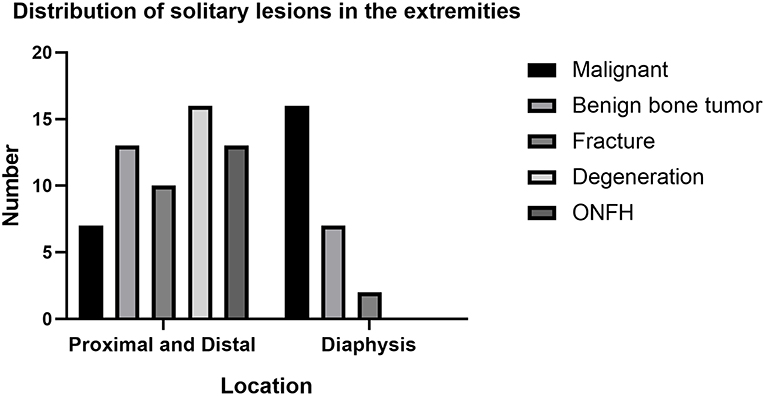
Two lesions (diagnosed as chronic osteomyelitis and Paget's disease of bone) showed diffuse areas of radiotracer uptake in a single bone, while the remaining 84 lesions showed focal radiotracer uptake on WBS. The anatomical location and final diagnosis of these 84 lesions are shown in Table 3. In proximal and distal extremities, benign bone disease was more frequently identified than malignant disease (Figure 1). The most common disease was degeneration (27.11%, 16/59), followed by benign bone tumors and ONFH (22.03%, 13/59). In the diaphyses of the extremities, bone metastasis was the most common disease, accounting for 64% (16/25) of the findings (Figure 2). When excluding disease with a diffuse area of radiotracer uptake on WBS, the difference in location between two groups was significant (χ2 = 24.00, P < 0.01) (Table 4).
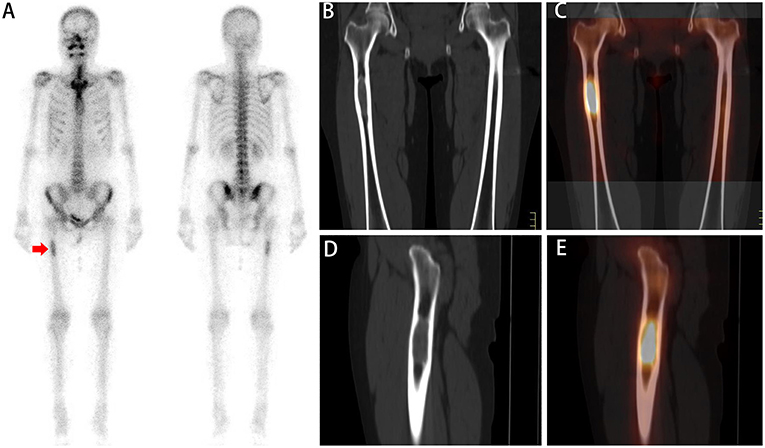
Figure 2. A whole-body scan (A) revealed a focal area of low 99mTc-MDP activity in the right femur (red arrow). No additional areas of abnormal 99mTc-MDP uptake were identified in the remainder of the skeleton. Coronal (B,C) and sagittal (D,E) CT and SPECT/CT imaging showed focally increasing 99mTc-MDP uptake corresponding to lytic changes and soft tissue masses in the diaphysis of the femur. A biopsy was subsequently performed, and pathologic analysis confirmed the diagnosis of bone metastasis.
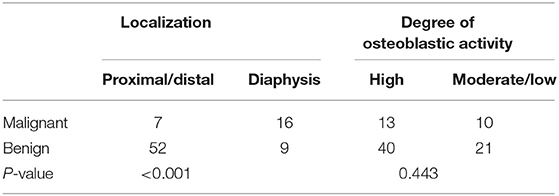
Table 4. The relation between localization/degree of osteoblastic activity and final diagnosis of extremity lesions.
The intensity of 99mTc-MDP uptake in malignant bone disease was considered high in 13 lesions and moderate or low in 10 sites. The intensity of uptake in benign diseases was considered high in 40 sites and moderate or low in 21 sites. The osteoblastic activity was not significantly different between the two groups (χ2 = 0.588, P > 0.05) (Table 4).
SPECT/CT Diagnostic Efficacy
All 86 lesions detected on WBS were interpreted as equivocal. On SPECT/CT analysis, for reviewer 1, 64 lesions with benign findings were interpreted as benign (Figures 3, 4), and 19 lesions with malignant findings were interpreted as bone metastases. Only three lesions were interpreted as equivocal on SPECT/CT. Based on the standard criterion, one of three equivocal lesions were diagnosed as benign (Figure 5), and two lesions were diagnosed as malignant. Reviewer 2 reclassified 61 lesions with benign findings as benign and 20 lesions with malignant findings as bone metastases. Only five lesions were interpreted as equivocal. Based on the standard criterion, three of five lesions were diagnosed as benign (Figure 5), and two lesions were diagnosed as malignant. Considering equivocal lesions as positive, the accuracy, specificity, and sensitivity for reviewer 1 were 94.19% (81/86), 86.96% (20/23), and 96.82% (61/63), respectively. The accuracy, specificity, and sensitivity for reviewer 2 were 95.34% (82/86), 95.65% (22/23), and 95.24% (60/63), respectively (Table 5). The inter-reviewer agreements were almost perfect. The k score for inter-reviewer agreement was 0.813 (P < 0.001, 95% CI 0.661–0.964) for SPECT/CT.
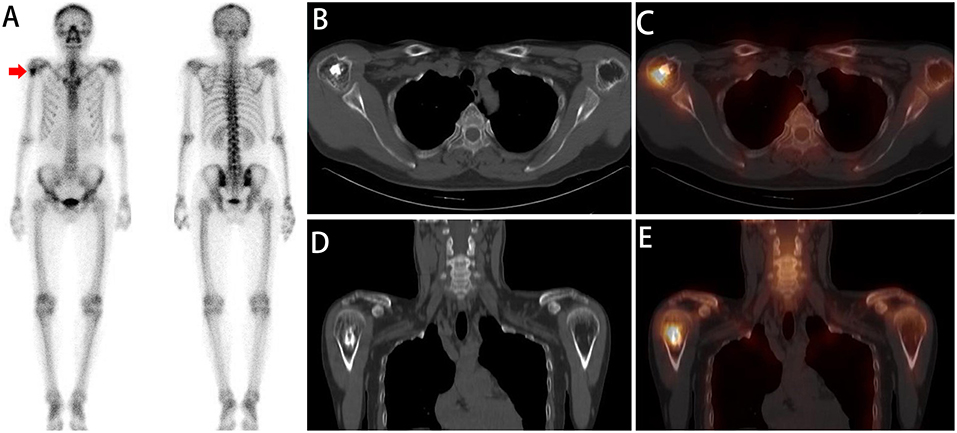
Figure 3. A whole-body scan (A) revealed a focal area of high 99mTc-MDP activity in the right humerus (red arrow). No additional areas of abnormal 99mTc-MDP uptake were identified in the remainder of the skeleton. Axial (B,C) and coronal (D,E) CT and SPECT/CT imaging showed focally increased 99mTc-MDP uptake corresponding to ossification in the proximal part of the humerus. The diagnosis of enchondromas was established by a combined assessment of clinical and radiologic follow-up.
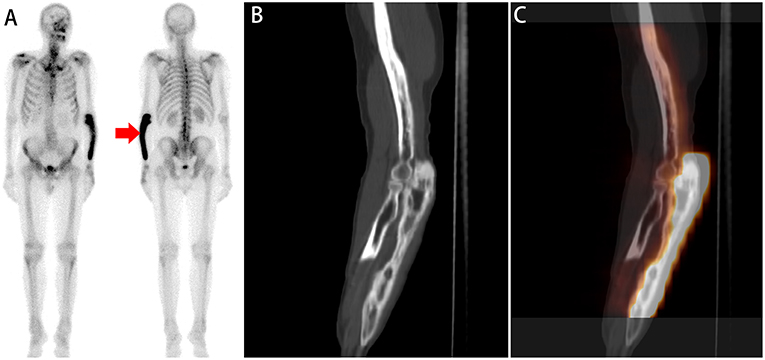
Figure 4. A whole-body scan (A) revealed diffuse high 99mTc-MDP activity in the left forearm (red arrow). No additional areas of abnormal 99mTc-MDP uptake were identified in the remainder of the skeleton. Sagittal (B,C) CT and SPECT/ CT imaging showed diffusely increased 99mTc-MDP uptake corresponding to irregular cortical thickening and porous sclerosis in the ulna. The diagnosis of Paget's disease of bone was established by a combined assessment of clinical and radiologic follow-up.
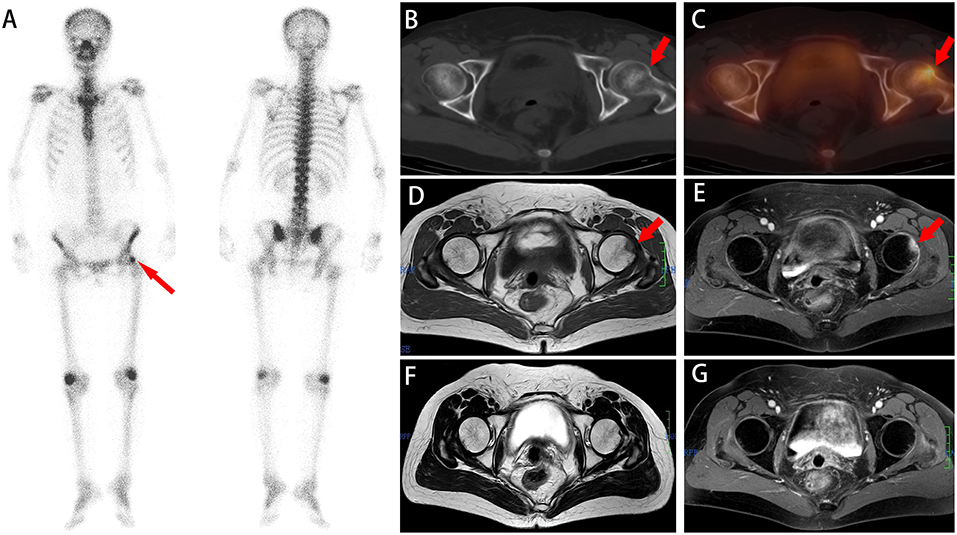
Figure 5. A whole-body scan (A) revealed a focal area of high 99mTc-MDP activity in the left femur (red arrow). No additional areas of abnormal 99mTc-MDP uptake were identified in the remainder of the skeleton. Axial (B,C) CT and SPECT/ CT imaging showed focally increased 99mTc-MDP uptake without density changes in the proximal part of the femur. Axial (D,E) MR images show high signal on T1WI and T2WI that disappeared 5 months later (F,G). The diagnosis of IF was established based on a combined assessment of clinical and radiologic follow-up.
Discussion
Final diagnoses of the 86 solitary lesions detected on WBS showed that 73.26% were benign bone lesions and 26.74% were bone metastases. As a rare disease, the incidence of solitary bone metastases accounts for only 2–3% of all skeletal spread situations (13). Compared to the extremities, vertebrae are the most common sites of bone metastases (13). Furthermore, recent studies have shown that the number of solitary bone metastases is less than the number of benign lesions in the spine (10, 14). Considering that only 10% of bone metastases occur in the limbs, which is a lower rate than that in the spine (15), the incidence of benign disease is obviously higher than that of bone metastases. The study performed by Daisuke Utsunomiya (6), which had similarities to this study, recruited 45 patients with a total of 82 areas of abnormal tracer uptake on WBS and found the majority of metastases located in the axial skeleton (83.33%, 35/42) and only four in the femur. L. C. McLoughlin recruited 54 male prostate cancer patients into the study, and only three of 13 bone metastatic lesions were located in the extremities (8). Therefore, we assumed that benign bone disease could be even more common than bone metastases of solitary lesions in the extremities.
In our study, we found that the most common begin bone disease was benign bone tumors (31.75%, 20/63). To our knowledge, degeneration is a common pathology among the elderly, and approximately half of the lesions in our groups belonged to patients who were older than 60 years. However, the number of benign bone tumors is similar to the number of lesions that were comorbid with degeneration in our groups, which may indicate that not all cases of degeneration show obvious radiotracer uptake on WBS or SPECT/CT. Therefore, we assumed that the actual incidence of degeneration may be higher than that of benign bone tumors. In addition, the majority (13/20.65%) of benign bone tumors were enchondromas, which were frequently found in the proximal femur, accounting for 61.53% (8/13). Although enchondroma occurs mostly in the metaphysis (16, 17), only 2.6% of all benign bone tumors are enchondromas (18–25). On the one hand, the majority of enchondromas are asymptomatic and most often identified incidentally for other reasons (26–28). Hence, we assumed that the incidence of enchondromas may be higher than that reported. On the other hand, with their distinct mineralization, most enchondromas show high tracer uptake on WBS (29). In our trial, all enchondromas showed high activity on WBS, and we assumed that enchondroma is easy to detect on WBS.
The locations of 84 focal lesions in the extremities were documented and evaluated to determine the correlation with diagnosis. In the proximal and distal extremities, the most common disease was degeneration (27.11%, 16/59), followed by benign bone tumors and ONFH (22.03%, 13/59). In the diaphyses of the extremities, bone metastasis was the most common disease, accounting for 61.53% (8/13). This may suggest that degeneration and ONFH are not only common among the elderly but also frequently occur in the proximal or distal extremities near the joints. In addition, many benign bone tumors (such as enchondroma and osteochondroma) occur mostly in the metaphysis (16). The findings of Rikard W. also revealed that metastases located in the humeral diaphysis were the most common, followed by proximal and distal lesions (30). Accordingly, it was important that solitary lesions in the proximal or distal parts of the extremities were usually benign, and diaphyseal lesions were usually malignant. The osteoblastic activity was not significantly different between metastases and benign lesions.
However, provided only limited spatial resolution and anatomical correlation, WBS may often be difficult to differentiate between bone metastasis and a benign lesion (31, 32). SPECT/CT not only precisely matched images of body structure and degree of osteoblastic activity in one imaging session but also enhanced the specificity of characteristics of lesions on CT, which assisted in distinguishing benign from malignant lesions (9, 31). In our study, we found that SPECT/CT exhibited a high sensitivity and specificity in differentiating malignant from benign solitary lesions in the extremities and showed almost perfect inter-reviewer agreement. Previous work in other patient cohorts supports the high specificity of SPECT/CT (7, 33, 34).
Our study had several limitations. First, a histopathological diagnosis was not available for all patients, especially for those with degenerative or fracture lesions. The final diagnosis of 73 lesions was based on radiological investigations (WBS and/or SPECT/CT, MRI), clinical information, and follow-up imaging. Second, some solitary lesions without radiotracer uptake (such as osteolytic bone metastases) could have been missed. Third, the number of patients included in the study was relatively small.
In summary, as for the interpretation of solitary bone disease in the extremities of patients with known cancer detected by WBS, SPECT/CT showed great diagnostic efficiency and was significant in differentiating malignant from benign solitary lesions in the extremities. Benign bone disease (such as benign bone tumors and degeneration) may be even more common than malignancy among solitary lesions in the extremities. Bone metastases were found more frequently in the diaphyses of the extremities rather than in other bone areas. Degeneration was the most frequent disease located in the proximal extremities, followed by benign bone tumors and ONFH.
Data Availability
The datasets generated for this study are available on request to the corresponding author.
Ethics Statement
The current study was approved by the Institutional Ethics Committee of the Affiliated Cancer Hospital & Institute of Guangzhou Medical University (No. 2017003), and the need for signed informed consent was waived.
Author Contributions
HP and LZ participated in the design of the study and drafted the manuscript and TZ collected the patients' data. WeiL and WenL interpreted the WBS and SPECT/CT images and LM processed the figures. RZ conceived the study and supervised the project. All authors read and approved the final version of the manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Abbreviations
99mTc-MDP, 99mTc-labeled methylene diphosphonate; WBS, whole-body bone scans; SPECT/CT, single-photon emission computed tomography/computed tomography.
References
1. Einat ES. Imaging of malignant bone involvement by morphologic, scintigraphic, and hybrid modalities. J Nuclear Med. (2005) 46:1356–67. doi: 10.1002/jmri.20365
2. Tofe AJ, Francis MD, Harvey WJ. Incidence of solitary skull and extremity involvement in whole-body scintigrams. J Nuclear Med. (1976) 17:755–6. doi: 10.1097/00004424-197611000-00020
3. Abikhzer G, Srour S, Keidar Z, Bar-Shalom R, Kagna O, Israel O, et al. Added value of SPECT/CT in the evaluation of benign bone diseases of the appendicular skeleton. Clin Nucl Med. (2016) 41:e195–9. doi: 10.1097/RLU.0000000000001042
4. Zhang L, He Q, Li W, Zhang R. The value of (99m)Tc-methylene diphosphonate single photon emission computed tomography/computed tomography in diagnosis of fibrous dysplasia. BMC Med Imaging. (2017) 17:46. doi: 10.1186/s12880-017-0218-4
5. Tsai SY, Wang SY, Shiau YC, Wu YW. Benign incidental findings of osteopoikilosis on Tc-99m MDP bone SPECT/CT. Medicine. (2016) 95:e3868. doi: 10.1097/MD.0000000000003868
6. Utsunomiya D, Shiraishi S, Imuta M, Tomiguchi S, Kawanaka K, Morishita S, et al. Added value of SPECT/CT fusion in assessing suspected bone metastasis: comparison with scintigraphy alone and nonfused scintigraphy and CT. Radiology. (2006) 238:264–71. doi: 10.1148/radiol.2373041358
7. Helyar V, Mohan HK, Barwick T, Livieratos L, Gnanasegaran G, Clarke SEM, et al. The added value of multislice SPECT/CT in patients with equivocal bony metastasis from carcinoma of the prostate. Eur J Nuclear Med Mol Imaging. (2009) 37:706–13. doi: 10.1007/s00259-009-1334-3
8. McLoughlin L, O'Kelly F, O'Brien C, Sheikh M, Feeney J, Torreggiani W, et al. The improved accuracy of planar bone scintigraphy by adding single photon emission computed tomography (SPECT-CT) to detect skeletal metastases from prostate cancer. Ir J Med Sci. (2016) 185:101–5. doi: 10.1007/s11845-014-1228-7
9. Linke R, Kuwert T, Uder M, Forst R, Wuest W. Skeletal SPECT/CT of the peripheral extremities. AJR Am J Roentgenol. (2010) 194:W329–35. doi: 10.2214/AJR.09.3288
10. Zhang Y, Shi H, Li B, Gu Y. Diagnostic value of 99Tcm-MDP SPECT/spiral CT combined with three-phase bone scintigraphy in assessing suspected bone tumor of patients without malignant history. Nuclear Med Commun. (2015) 36:686–94. doi: 10.1097/MNM.0000000000000299
11. Landis J, Koch GG. The measurement of observer agreement for categorical data. Biometrics. (1977) 33:159–74. doi: 10.2307/2529310
12. Kundel HL, Polansky M. Measurement of observer agreement. Radiology. (2003) 228:303–8. doi: 10.1148/radiol.2282011860
13. Rubin P, Brasacchio R, Katz A. Solitary metastases: illusion versus reality. Semin Radi Oncol. (2006) 16:120–30. doi: 10.1016/j.semradonc.2005.12.007
14. Kim Y, Han I, Lee I, Lee J, Choi B. Imaging findings of solitary spinal bony lesions and the differential diagnosis of benign and malignant lesions. J Korean Neurosurg Soc. (2012) 52:126–32. doi: 10.3340/jkns.2012.52.2.126
15. Cheng D-D, Yang J-L, Hu T, Yang Q-C. Efficacy of limb salvage with primary tumor resection simultaneously for solitary bone metastasis in limbs. World J Surg Oncol. (2016) 14:31. doi: 10.1186/s12957-016-0786-8
16. Motamedi K, Seeger LL. Benign bone tumors. Radiol Clin North Am. (2011) 49:1115–34. doi: 10.1016/j.rcl.2011.07.002
17. Hakim DN, Pelly T, Kulendran M, Caris JA. Benign tumours of the bone: a review. J Bone Oncol. (2015) 4:37–41. doi: 10.1016/j.jbo.2015.02.001
18. Kushner BH, Roberts SS, Friedman DN, Deborah K, Irina O, Shakeel M, et al. Osteochondroma in long-term survivors of high-risk neuroblastoma. Cancer. (2015) 121:2090–6. doi: 10.1002/cncr.29316
19. Solooki S, Vosoughi AR, Masoomi V. Epidemiology of musculoskeletal tumors in Shiraz, south of Iran. Indian J Med Paediatr Oncol. (2011) 32:187–91. doi: 10.4103/0971-5851.95138
20. Baena-Ocampo Ldel C, Ramirez-Perez E, Linares-Gonzalez LM, Delgado-Chavez R. Epidemiology of bone tumors in Mexico City: retrospective clinicopathologic study of 566 patients at a referral institution. Ann Diagn Pathol. (2009) 13:16–21. doi: 10.1016/j.anndiagpath.2008.07.005
21. Young BRD. Tumors of the bones and joints. Am J Clin Pathol. (1994) 102:703. doi: 10.1093/ajcp/102.5.703a
22. Nasr B, Albert B, David CH, Marques da Fonseca P, Badra A, Gouny P. Exostoses and vascular complications in the lower limbs: two case reports and review of the literature. Ann Vasc Surg. (2015) 29:1315.e7-.e14. doi: 10.1016/j.avsg.2015.02.020
23. Herget GW, Kontny U, Saueressig U, Baumhoer D, Hauschild O, Elger T, et al. Osteochondroma and multiple osteochondromas: recommendations on the diagnostics and follow-up with special consideration to the occurrence of secondary chondrosarcoma. Radiologe. (2013) 53:1125–35. doi: 10.1007/s00117-013-2571-9
24. Rao VS, Pai MR, Rao RC, Adhikary MM. Incidence of primary bone tumours and tumour like lesions in and around Dakshina Kannada district of Karnataka. J Indian Med Assoc. (1996)94:103–4.
25. Smith JR. Bone tumors. General aspects and data on 6,221 cases. J Clin Pathol. (1980) 32:742. doi: 10.1136/jcp.32.7.742-b
26. Herget GW, Strohm P, Rottenburger C, Kontny U, Krauß T, Bohm J, et al. Insights into Enchondroma, Enchondromatosis and the risk of secondary Chondrosarcoma. Review of the literature with an emphasis on the clinical behaviour, radiology, malignant transformation and the follow up. Neoplasma. (2014) 61:365–78. doi: 10.4149/neo_2014_046
27. Lang S, Adler CP. Bone diseases: macroscopic, histological and radiological diagnosis of structural changes in skeleton. Eur J Radiol. (2001) 37:139. doi: 10.1016/S0720-048X(00)00246-1
28. Murphey MD, Choi JJ, Kransdorf MJ, Flemming DJ, Gannon FH. Imaging of osteochondroma: variants and complications with radiologic-pathologic correlation. Radiographics. (2015) 20:1407–34. doi: 10.1148/radiographics.20.5.g00se171407
29. Yong-Whee Bahk MD. Combined scintigraphic and radiographic diagnosis of bone and joint diseases. J Nuclear Med. (2013) 54:1168–9. doi: 10.2967/jnumed.113.126557
30. Rikard W, Hansen BH, Minna L, Clement T, Olga Z, Peter B, et al. Complications and survival after surgical treatment of 214 metastatic lesions of the humerus. J Shoulder Elbow Surg. (2012) 21:1049–55. doi: 10.1016/j.jse.2011.06.019
31. Beiderwellen K, Huebner M, Heusch P, Grueneisen J, Ruhlmann V, Nensa F, et al. Whole-body [18F]FDG PET/MRI vs. PET/CT in the assessment of bone lesions in oncological patients: initial results. Eur Radiol. (2014) 24:2023–30. doi: 10.1007/s00330-014-3229-3
32. Gates FG. SPECT bone scanning of the spine. Semin Nucl Med. (1998) 28:78–94. doi: 10.1016/S0001-2998(98)80020-2
33. Römer W, Nömayr A, Uder M, Bautz W, Kuwert T. SPECT-guided CT for evaluating foci of increased bone metabolism classified as indeterminate on SPECT in cancer patients. J Nuclear Med. (2006) 47:1102–6. doi: 10.1016/j.nuclcard.2006.05.010
Keywords: solitary lesion, extremities, 99mTc-MDP, SPECT/CT, whole-body bone scan
Citation: Peng H, Zhang L, Zhou T, Li W, Li W, Ma L and Zhang R (2019) Characterization of Solitary Lesions in the Extremities on Whole-Body Bone Scan in Patients With Known Cancer: Contribution of Single-Photon Emission Computed Tomography/Computed Tomography. Front. Oncol. 9:607. doi: 10.3389/fonc.2019.00607
Received: 08 April 2019; Accepted: 20 June 2019;
Published: 09 July 2019.
Edited by:
Georgios S. Limouris, National and Kapodistrian University of Athens, GreeceReviewed by:
Zhongxiang Ding, Hangzhou First People's Hospital, ChinaAthanasios Zafeirakis, Army Share Fund Hospital (NIMTS), Greece
Ioannis Karfis, Institut Jules Bordet, Belgium
Copyright © 2019 Peng, Zhang, Zhou, Li, Li, Ma and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rusen Zhang, emhhbmdydXNlbkBnemhtdS5lZHUuY24=
†These authors have contributed equally to this work
 Hao Peng
Hao Peng Linqi Zhang
Linqi Zhang Tao Zhou
Tao Zhou Wei Li
Wei Li Wen Li
Wen Li Liwu Ma
Liwu Ma Rusen Zhang
Rusen Zhang