- 1Botswana Harvard AIDS Institute Partnership, Gaborone, Botswana
- 2Division of Global Health Equity, Brigham and Women’s Hospital, Boston, MA, United States
- 3Department of Medicine, Brigham and Women’s Hospital, Boston, MA, United States
- 4Department of Social and Behavioral Sciences, Harvard TH Chan School of Public Health, Center for Community-Based Research, Dana-Farber Cancer Institute, Boston, MA, United States
- 5Princess Marina Hospital, Ministry of Health and Wellness, Gaborone, Botswana
- 6Department of Pathology, Faculty of Medicine, University of Botswana, Gaborone, Botswana
- 7University of Pennsylvania, Philadelphia, PA, United States
- 8Botswana Upenn Partnership, Gaborone, Botswana
- 9Department of Medicine, Beth Israel Deaconess Medical Center, Boston, MA, United States
- 10Center for Global Cancer Medicine, Abramson Cancer Center, University of Pennsylvania, Philadelphia, PA, United States
- 11Harvard TH Chan School of Public Health, Boston, MA, United States
- 12Division of Infectious Diseases, Brigham and Women’s Hospital, Boston, MA, United States
Introduction: Health system delays in diagnosis of cancer contribute to the glaring disparities in cancer mortality between high-income countries and low- and middle-income countries. In Botswana, approximately 70% of cancers are diagnosed at late stage and median time from first health facility visit for cancer-related symptoms to specialty cancer care was 160 days (IQR 59–653). We describe the implementation and early outcomes of training targeting primary care providers, which is a part of a multi-component implementation study in Kweneng-East district aiming to enhance timely diagnosis of cancers.
Methods: Health-care providers from all public facilities within the district were invited to participate in an 8-h intensive short-course program developed by a multidisciplinary team and adapted to the Botswana health system context. Participants’ performance was assessed using a 25-multiple choice question tool, with pre- and post-assessments paired by anonymous identifier. Statistical analysis with Wilcoxon signed-rank test to compare performance at the two time points across eight sub-domains (pathophysiology, epidemiology, social context, symptoms, evaluation, treatment, documentation, follow-up). Linear regression and negative binomial modeling were used to determine change in performance. Participants’ satisfaction with the program was measured on a separate survey using a 5-point Likert scale.
Results: 176 participants attended the training over 5 days in April 2016. Pooled linear regression controlling for test version showed an overall performance increase of 16.8% after participation (95% CI 15.2–18.4). Statistically significant improvement was observed for seven out of eight subdomains on test A and all eight subdomains on test B. Overall, 71 (40.3%) trainees achieved a score greater than 70% on the pretest, and 161 (91.5%) did so on the posttest. Participants reported a high degree of satisfaction with the training program’s content and its relevance to their daily work.
Conclusion: We describe a successfully implemented primary health care provider-focused training component of an innovative intervention aiming to reduce health systems delays in cancer diagnosis in sub-Saharan Africa. The training achieved district-wide participation, and improvement in the knowledge of primary health-care providers in this setting.
Clinical Trial Registration: www.ClinicalTrials.gov, identifier NCT02752061.
Introduction
Cancer is more deadly in resource-rich than resource-limited regions of the world. The mortality-to-incidence ratio of cancers in the United States and the European Union are 0.36 and 0.48, respectively, while they range between 0.66 and 0.70 in World Health Organization’ Western Pacific, Southeast Asia, and Africa regions (1, 2). As an example, overall, 5-year survival for breast cancer ranges from 88% in the US, 64% in South Africa, and 56% in Uganda, and significantly less than this in many parts of Africa (3–6). This glaring disparity in outcomes is due in part to late diagnosis of cancer (2, 4), which corresponds with poorer prognosis.
Patient, provider, and health system factors contribute to late diagnosis of cancer (7). Fears, stigma, limited cancer awareness and fatalistic beliefs (8, 9), male sex (10), spiritual and traditional beliefs (11–14), as well as low socioeconomic position (9, 11, 15) and difficulty navigating the health system are notable patient-related factors affecting delays. Health systems and provider factors include shortage of health-care providers, limited cancer knowledge and skills (12, 14, 16), lack of diagnostic tools and technologies including pathology services (17, 18), diagnostic errors (4), type of cancer (19), geographic distribution of services, and delayed referrals and poor coordination between facilities (8). Although much of the literature describes patient-related delays, evidence suggests that health system delays may play a greater role in late diagnosis (4, 20, 21), and few studies have implemented and evaluated interventions aimed to address health system factors.
In Botswana, a middle-income country of two million people, approximately 70% of cancers are diagnosed at late stage (unpublished, National Non-Communicable Diseases Program data) despite efforts to increase cancer screening and provision of treatment of major cancers to citizens free of charge. We previously found that median time from symptom onset to first presentation at a health facility was 29 days (IQR 0–185), while median time from first health facility visit to specialty cancer care was 160 days (IQR 59–653) (10). Therefore, we sought to implement and evaluate a comprehensive quality improvement project to facilitate earlier cancer detection, particularly targeting health system and provider-related factors.
The Potlako initiative is an implementation study in Kweneng-East district in Botswana that aims to enhance timely diagnosis of cancer through a package of (a) training primary care clinicians to identify, manage, triage, and refer patients with cancer-related symptoms, (b) developing a standardized referral algorithm, (c) introducing a nurse coordinator role to support patients and clinicians across facility levels to navigate the health system, and (d) providing transport assistance for vulnerable patients (22). To the best of our knowledge Potlako, which means “hurry” in Setswana, is the first study in sub-Saharan Africa to evaluate a multi-component intervention package that addresses contributors to both patient and health system delays to improve timely diagnosis of cancer. Here, we describe the implementation and early outcomes of the training component of this intervention. Results from other Potlako components will be assessed and reported after study completion.
Materials and Methods
Study Setting
Botswana has a relatively well-resourced health-care system, with primary health-care services available for free to all citizens and over 95% of residents residing within 8 km of a health facility (23). There are 38 doctors, and 272 nurses/midwives per 100,000 population (24). The country has a network of over 600 of primary health-care facilities (health posts and primary clinics) each staffed by at least one general nurse (with at least 2 years diploma post-secondary training). Government is the leading source of health-care financing covering 65% of total health expenditure (25), and total health expenditure per capita is Int’l $ 87 (26). Treatment of cancer, including chemotherapy, systemic therapy, surgery, and radiotherapy is available for free to all citizens who meet clinical indication at tertiary facilities located in the two largest cities in the country.
Patients with cancer are referred for treatment at Princess Marina Hospital, a 500-bed facility that is one of the two national referral hospitals providing oncology specialty services. Cancer pathology-based diagnosis and treatment (chemotherapy and systemic, surgery) are available at public facilities for free to citizens; radiotherapy at a private hospital is also available for free for patients referred through the public facility system.
Potlako initiative is based in Kweneng-East District, one of Botswana’s 27 health districts located approximately 50 km west of Botswana’s capital city Gaborone. The health district serves 150,131 residents (27) who live in a range of settings including semi-urban to rural remote cattle posts (Figure 1). Potlako is a district-wide initiative involving participation of all 35 primary care clinics (21 health posts, 14 primary clinics) as well as a primary hospital and a general (district) hospital in the district.
Trainees and Process of Invitation
The training component of Potlako targeted health-care providers, particularly nurses, practicing at primary care clinics who typically are the first point of contact for adults with undiagnosed cancer symptoms. Providers from all public facilities in Kweneng-East District were invited to participate, including the HIV/infectious diseases care clinic (IDCC), sexual and reproductive health clinic, and general medical and surgical outpatient clinics (OPD). For the two district hospitals, providers from the inpatient medical, surgical, and gynecologic wards were also invited. Overall 170 health-care providers were invited to the training, with a goal of training at least 40% of those working in primary clinics and at least 25% of those at relevant outpatient clinics and wards in the hospital.
A dedicated process of stakeholder engagement and participation in planning was followed. A series of meetings were held, first involving the head of district management team and facility managers to identify facility-based focal points at each facility. Then focal points worked with managers to identify individuals suitable for training given specified criteria such as working in the relevant units and size of facilities. Training dates were also set according to preferences expressed by facility and district leadership. Letters of invitation were emailed and faxed, and subsequently followed up by phone-call confirmation of names of those who would be attending.
Curriculum Development and Trainers
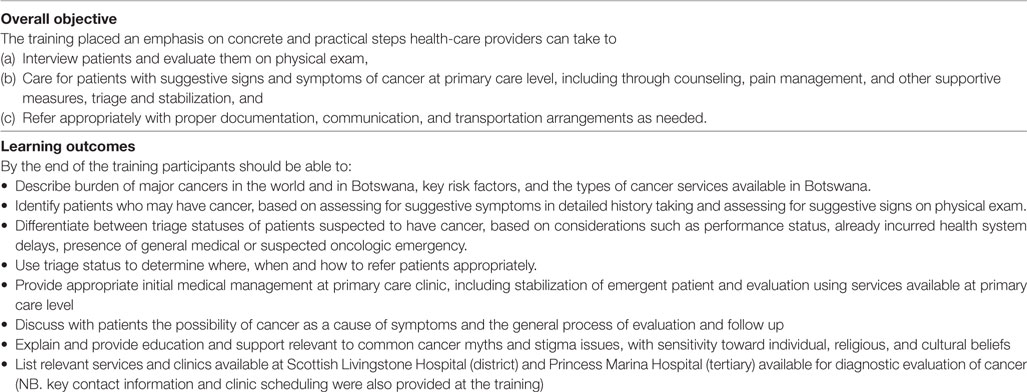
The overall objective was to empower primary health-care providers with increased knowledge on how to identify, provide primary care, and promptly and appropriately refer patients who may have cancer (Boxes 1 and 2). We developed an intensive 8-h short-course program, employing multi-method format including participatory didactic slide-based presentations, role-playing demonstrations, case studies, small group discussions, self- and group-reflection on clinical experiences, and open question and answer sessions.
Box 1. Overview of Potlako health-care provider learning objectives.
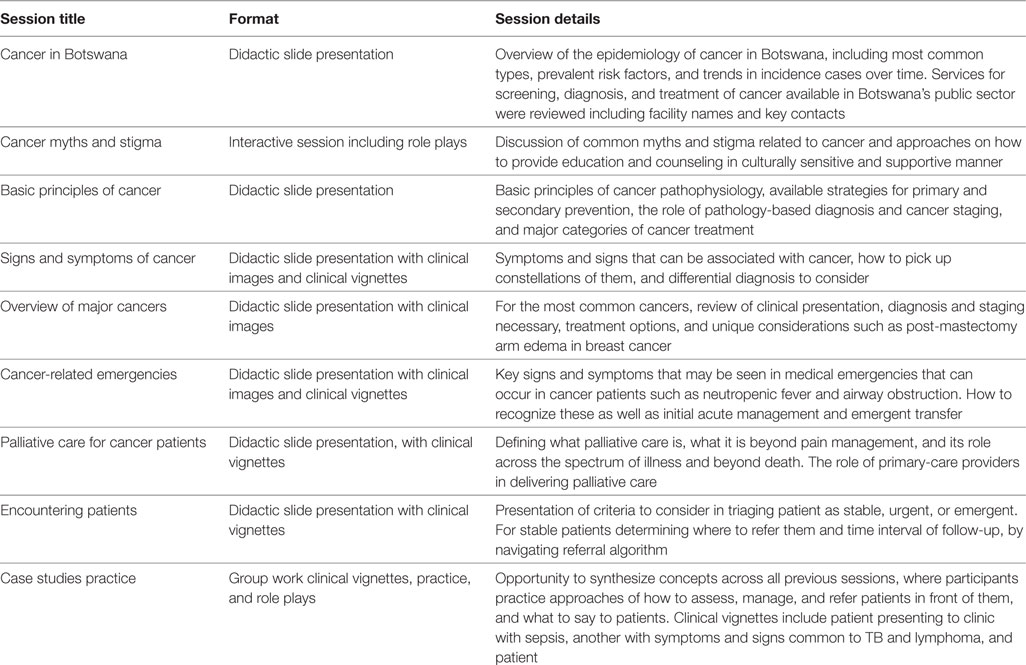
Box 2. Training session topics and format.
The curriculum was developed by a multidisciplinary team with experience working in Botswana (two oncologists, one oncology fellow, one medical officer, one infectious disease specialist, one internal medicine resident, one family medicine resident, one internal medicine specialist, one pathologist, one palliative care specialist, one public health officer, and two nurses). Consultation and inputs from the team of experts were obtained through workshops, individual discussions, and email communication, to reach consensus regarding (a) competencies of health-care providers relevant to cancer early detection within study context and relevant learning outcomes, (b) general teaching and learning strategies, (c) training material being developed, and (d) training evaluation tool (described below). Curriculum content was adapted to the Botswana context using training material that had been used for similar purposes in Rwanda’s national baseline cancer training program jointly developed by Rwanda Ministry of Health, Partners in Health and Dana Farber/Brigham and Women’s Cancer Center (28, 29). Adaptation employed an iterative review process incorporating inputs from the literature and training team expertise and lessons learned in structuring Botswana’s HIV training program (KITSO) for primary-care providers (30).
The curriculum was delivered as a 1-day program and was administered five times in April 2016. Most of the trainers facilitating the lectures and activities (Table 2) also contributed to curriculum development. All participants received printed materials of lecture slides, referral algorithms, and discussion topics.
Training Evaluation
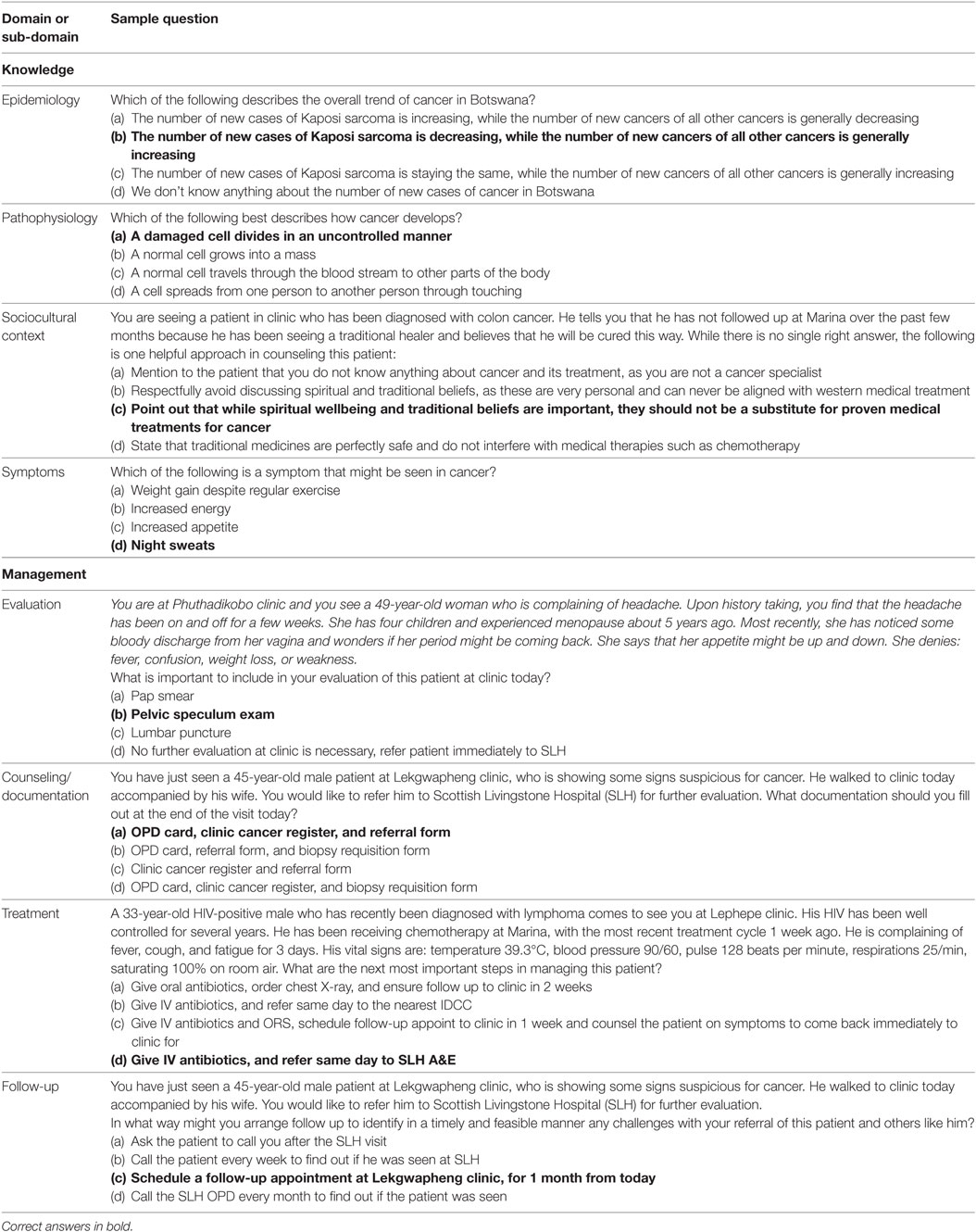
A single answer multiple-choice format pre- and posttest was developed to evaluate knowledge gained and achievement of learning objectives of the training program (Table 1). While we did not employ a formal consensus building technique, development of the training pre/posttest was informed by literature review, previous experience with similar trainings in rural Rwanda, and involved an iterative process of consultation and revisions by a multi-disciplinary panel of experts (the same individuals who had been involved in the broader curriculum development). Inputs from experts were obtained through workshops, individual discussions, and over email. Items selected for inclusion were those that assessed immediate impact of training in accordance with the first two levels of Kirkpatrick’s training evaluation framework (31): (1) reaction and (2) acquisition of knowledge, attitudes, and skills. Selection of questions emphasized diversity across two broad domains of knowledge and management, and corresponding eight sub-domains: pathophysiology, epidemiology, social context, symptoms, evaluation, treatment, documentation, follow-up. Prior to finalization of the pre/posttest, inputs were obtained from the team regarding clarity and specificity of questions, and agreement on the correct answer.
In response to feedback from participants during the first 2 days of training, trainers (who included members of the curriculum development team) identified the need to refine some of the questions to put less emphasis on the epidemiology, and more emphasis on practical information on evaluation, treatment and counseling as well as follow-up. The format of some of the questions was also revised from stand-alone questions to clinical vignettes containing a series of questions. This resulted in change in content of 14 questions. Given this change, analysis for pre/posttest scoring were performed and presented separately as test version A (first and second trainings), and version B (third, fourth, and fifth trainings).
Pre/posttests were administered on paper, with trainees asked to generate an anonymous ID code to allow for matching of answers across pre/posttest time points. The posttest was identical to the pretest administered on any given training day. Following completion of posttest, questions were reviewed with open discussion of correct answers and questions that were particularly challenging. Trainees were also asked to complete an anonymous satisfaction form in order to provide feedback on the quality of execution of the training including relevance to day-to-day work, clarity of content, and general training logistics. On a daily basis, research assistants transcribed the pre- and posttests from paper into excel spreadsheet that had pre-programmed data quality checks and scoring. 10% of tests were audited by NT and MP.
Statistical Analysis
Correct responses were summed and overall scores were calculated as the total percentage of correct responses. Domain and sub-domain scores were also calculated. A score of 70% or greater was considered passing. Descriptive statistics were used to characterize counts of correct responses, overall score percent, and change. We used the Wilcoxon signed-rank test to compare differences between test versions and scores. Because of the changes across test versions and significant differences in scores between versions, data for each version of the exam are presented separately. We used a panel design and ran both linear regression (on overall percent score) and negative binomial (on correct count) models clustered on the individual and controlling for the test version to determine the change in performance. Analyses were performed using Stata (Version 14, College Station, TX, USA).
Ethical Review
Project was reviewed and approved by the institutional review boards of the Botswana Ministry of Health and Wellness and the Harvard T.H. Chan School of Public Health. Additional approvals were obtained from the participating health facilities. Requirement for written informed consent was waived given the minimal risk of the study, and to reduce risk of reputational harm based on test performance.
Results
Participation
At the beginning of the study period, Kweneng-East had 134 nurses and 7 rotating general practitioner doctors staffing the primary clinics; the two hospitals had 26 doctors and 327 nurses on their rosters. We invited 170 providers to the program, with a goal of training at least 40% of those working in primary clinics to ensure availability of trained personnel even with routine staffing turn-over. A total of 176 trainees attended with 100% of all Kweneng-East public facilities represented and 60% of general nurses, midwives, and family nurse practitioners working at the primary clinics attending the training. 111 (63%) of trainees were nurses, 36 (21%) were midwives, 7 (4%) were family nurse practitioners, and 19 (11%) were general practitioner doctors. 87 of the trainees (49.4%) were from primary clinics, while 22 (12%) were from outpatient clinics at the primary and district hospitals, 52 (30%) from the inpatient wards at those hospitals and 12 (7%) were from unspecified units at the hospitals.
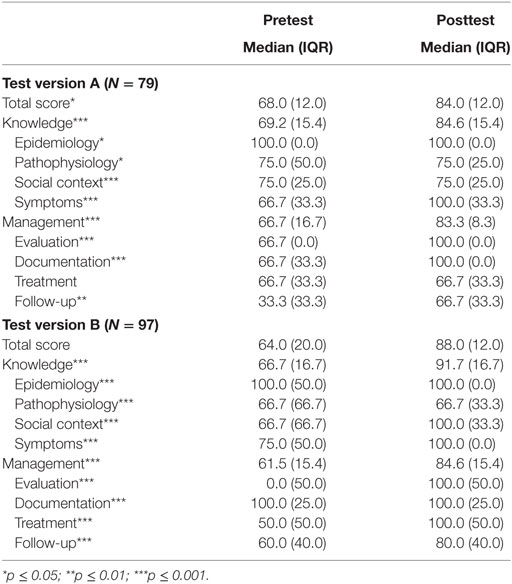
Overall Knowledge Gains
All attendees completed pre/posttests. There were significant differences between the scores on different test versions (Table 2). Among the 79 trainees who completed test version A, the mean change was 12.9 percentage points. Among the 97 who took test version B, the mean change was 20.0 percentage points. The pooled linear regression results for the overall score showed an increase of 16.8 percentage points on the posttest controlling for the test version [95% confidence interval (CI): 15.2–18.4, p < 0.001].
We used an arbitrary cut-off score of 70% as the threshold for passing. Prior to the training, less than half of the trainees passed the assessment test (49% version A, 33% version B). Following the training, nearly all participants passed (89% version A, 94% version B). Overall, about half of the sample improved from below the threshold on the pre-test to above the passing score (92, 52%) after the training. However, 13 (7%) did not improve their scores above passing. All but two participants with passing scores on the pre-test also passed the posttest.
Knowledge Gains Across Sub-Domains
We analyzed improvement within two domains and saw significant improvements in both the knowledge and management domains on both test versions (Table 2). Participants completing test version A demonstrated improvement in the following subdomains: epidemiology (p = 0.04), pathophysiology (p = 0.019), social context (p < 0.0001), symptoms (p < 0.0001), evaluation (p < 0.0001), documentation (p < 0.0001), and follow-up (p = 0.0029). There was no difference in the treatment subdomain. Participants completing test version B demonstrated improvement in all subdomains: epidemiology (p < 0.0001), pathophysiology (p < 0.0001), social context (p < 0.0001), symptoms (p < 0.0001), evaluation (p < 0.0001), documentation (p < 0.0001), treatment (p < 0.0001), and follow-up (p = 0.0003).
Trainee Satisfaction With Training Program
Ninety-six percent (169) participants completed the satisfaction survey. Overall, participants reported a high degree of satisfaction with the training program. On a 5-point scale, participants rated the format in which the training was delivered, including the balance between lectures and interactive sessions with a mean score of 4.5 (range 1–5). They rated the content of the training, including key learning points and topics covered, with a mean score of 4.5 (range 3–5). Participants rated the usefulness of the training to their job, including how they would be able to utilize the lessons from it in their day-to-day work, with a mean score of 4.7 (range 3–5). Of 169 respondents, 166 (98.2%) stated that they would be interested in attending a follow-up training.
Training Material and Tools
A set of training material including didactic power-point slides, case studies/scenarios, trainer’s notes, and pre/posttest has been developed. These have been placed in repository that is accessible for future trainings and adaptation for other related trainings.
Discussion
We successfully implemented the health-care provider training component of an innovative intervention aiming to reduce health systems delays in cancer diagnosis, had high district-wide attendance, and demonstrated gains in knowledge among participants. Knowledge gaps identified and addressed included in the areas (sub-domains) of understanding better a patient’s social context, cancer-associated symptoms, and primary-care based patient evaluation, and follow-up.
Curriculum Development
Development of the curriculum of this training leveraged South–South collaboration and use of material and experience developed in the region including in Rwanda (24, 25) and national structured HIV training program targeting primary care health-care providers that facilitated Botswana’s rapid implementation of the continent’s first national anti-retroviral treatment program (30). Training material is available for future implementation, adaptation, and sharing and there is a need to strengthen avenues for best practices sharing of these and training approaches, such as have been initiated by American Society of Clinical Oncology and the Kenya-based Academic Model Providing Access to Health care consortium (32).
There have been many more studies on training to improve early detection of disease focusing non-communicable diseases (NCDs) other than cancer, and those involving cancer have been specific to a type of cancer such as oral cancer in Asia and cervical cancer in Africa (33–36). The training program presented here is among the few that we are aware of that covers cancers broadly and concepts in signs, symptoms, triage, referral in consideration of a group of major cancers. It is also one that focuses on history and physical exam, available at the primary care level in any setting, rather than reliant on need for additional technology or equipment. While basic, this training is indeed fitting for primary care and low technology setting and employing an integrated approach. The training also serves as a pilot and first building block for a core module on cancer early detection, to which other components such as clinical breast exam practicum can be added in the future.
Training Participation and Stakeholder Engagement
The positive response to training invitations reflects an interest in learning opportunities about cancers and a knowledge gap identified by facility managers. The high rate of participation was likely the result of active stakeholder engagement in the planning process.
Impact of Training on Knowledge
We found a statistically significant improvement in overall and across several sub-domains including in cancer-associated symptoms, appropriate evaluation, referral, and follow-up. These are notable as medical training institutions in Botswana, as with those in many LMICs (32), have traditionally not included significant cancer content in their undergraduate curriculums. Furthermore, Botswana’s experience with high prevalence of HIV, which peaked at 27% in 2001 (37), and the successful scale of up a structured training (30) has resulted in most health-care providers being competent in diagnosis and management of major infectious diseases while seldom considering cancer and NCDs in their differential diagnosis, much less managing appropriately. This knowledge gap is increasingly important to address given the changing landscape of longer life expectancy, unhealthy lifestyle habits, and indeed the excess risk of cancer introduced by HIV. The described training focuses on tackling this gap at patient’s first encounter with the health system, the primary care level.
Limitations
This analysis is not without its limitations. First, given the revision of pre/posttest administered on the last 3 days of the training, we were not able to meaningfully analyze data across all 5 days of the training period. We thus present test scores during the first 2 days of training and the last 3 days of training separately. We were unable to collect information on demographics and other characteristics of trainees and, therefore, could not investigate differences across sub-groups of trainees. We found a statistically significant 16.8% absolute difference between pre- and posttesting scores, this was not as large an improvement as observed in other studies (38, 39). This may indicate that the test questions could have been designed to be more challenging; to the best of our knowledge, there are no relevant validated testing tools that might have been applied. Furthermore, while pre/post testing and setting of an arbitrary passing threshold is informative in understanding knowledge gained during the training, the ultimate assessment is whether the learning is retained and translates into improved care for patients who could have cancer.
While our training intervention was effective with respect to immediate learning outcomes, we recognize that this is not sufficient to translate to improved practices as has been described in many studies (40–42). Other than knowledge and skills, there are other determinants of health-care provider performance as it related to early detection, such as provider’s motivation, attitudes and perceptions regarding responsibilities, and work environment (40). These would need to be evaluated and addressed in further studies. Additionally, there are patient and health system factors to take into account, such as patient awareness and socioeconomic barriers, and health system funding, leadership, policies, and guidelines in place overall absorptive capacity personnel and infrastructure (43, 44). Thus, we present here only a piece of the puzzle, so to speak, to achieve earlier detection of cancer in our context. The broader Potlako initiative seeks to address these other factors as well, including through case management mentorship supports, job aids, coordination of visit scheduling and pathology results, navigation, and transport support for patients. While a comprehensive cancer early detection strategy and program does not currently exist in Botswana, there are various policies and guideline developments that support cancer early detection. Early detection is listed as a component of Botswana’s Essential Health Services Package, a national cervical cancer screening program has been in existence since 2012 (34) and roll out is ongoing, the country’s first national Primary Health-care guidelines, which include protocol for early detection of breast cancer were endorsed in 2016, and development of national treatment guidelines for specific cancers is underway.
Conclusion
This description of the development, implementation, and preliminary knowledge gains from a health-care provider training demonstrate an avenue by which primary care health-care providers can be engaged in efforts to diagnose cancer earlier. This report is particularly timely given increasing global discourse on leveraging the primary care platform in strengthening health systems, and in more efficiently using limited health resources in low- and middle-income countries. Further studies are needed to assess and address the other key determinants of health-care provider performance related to early diagnosis, such as provider’s motivation, attitudes and perceptions regarding responsibilities, and work environment. Our description of approach and findings thus far are a first step in this inquiry, which may inform Botswana’s cancer early detection approaches facilitated by implementation of Primary Health-care guidelines. Findings may also be relevant to other settings seeking to improve cancer early detection and quality of service delivery through training of primary care providers.
Availability of Data and Material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Statement
Project was reviewed and approved by the institutional review boards of the Botswana Ministry of Health and Wellness and the Harvard T.H. Chan School of Public Health. Additional approvals were obtained from the participating health facilities. Requirement for written informed consent was waived given the minimal risk of the study, and to reduce risk of reputational harm based on test performance.
Author Contributions
NT conducted literature review, contributed to study conception and design, supported cleaning, analysis and interpretation, and led writing and critical review of the manuscript. MP conducted literature review, performed data analysis, and contributed to writing and critical review of manuscript. REK supported data analysis and contributed to critical review and editing of manuscript. SD-P and SL contributed to the conception, analysis interpretation, and critical review of the manuscript. KB, KG, and IN contributed to data collection and data cleaning, and critical review of manuscript. IIS, MN, MM, SG, TB, and LS contributed to interpretation of findings, organization and critical review of manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to express gratitude to the following for their support and leadership of Dr. Kitenge Kalenga, Mrs. Moetse, Dr. Sebathu Chiyapo, Dr. Malebogo Kebabonye-Pusoentsi. We would like to thank the health-care providers across Kweneng-East district for their active participation and tireless work in improving patient care.
Funding
The study described in this article is supported by funding from the United States National Institutions of Health (Award No. 3P30CA006516-51S4, K23AI091434, C06CA059267) and the Paul G. Allen Family Foundation (11689). The funding institution had no role in study design, data collection, data analysis, data interpretation, or writing of this manuscript.
References
1. Lopes Gde L Jr, de Souza JA, Barrios C. Access to cancer medications in low- and middle-income countries. Nat Rev Clin Oncol (2013) 10(6):314–22. doi:10.1038/nrclinonc.2013.55
2. de Souza JA, Hunt B, Asirwa FC, Adebamowo C, Lopes G. Global health equity: cancer care outcome disparities in high-, middle-, and low-income countries. J Clin Oncol (2017) 34(1):6–13. doi:10.1200/JCO.2017.35.8_suppl.6
3. Gakwaya A, Kigula-Mugambe JB, Kavuma A, Luwaga A, Fualal J, Jombwe J, et al. Cancer of the breast: 5-year survival in a tertiary hospital in Uganda. Br J Cancer (2008) 99(1):63–7. doi:10.1038/sj.bjc.6604435
4. Unger-Saldana K. Challenges to the early diagnosis and treatment of breast cancer in developing countries. World J Clin Oncol (2014) 5(3):465–77. doi:10.5306/wjco.v5.i3.465
5. Agarwal G, Ramakant P. Breast cancer care in India: the current scenario and the challenges for the future. Breast Care (Basel) (2008) 3(1):21–7. doi:10.1159/000115288
6. El Saghir NS, Khalil MK, Eid T, El Kinge AR, Charafeddine M, Geara F, et al. Trends in epidemiology and management of breast cancer in developing Arab countries: a literature and registry analysis. Int J Surg (2007) 5(4):225–33. doi:10.1016/j.ijsu.2006.06.015
7. Kohler RE, Gopal S, Miller AR, Lee CN, Reeve BB, Weiner BJ, et al. A framework for improving early detection of breast cancer in sub-Saharan Africa: a qualitative study of help-seeking behaviors among Malawian women. Patient Educ Couns (2017) 100(1):167–73. doi:10.1016/j.pec.2016.08.012
8. Almuammar A, Dryden C, Burr JA. Factors associated with late presentation of cancer: a limited literature review. J Radiother Pract (2010) 9(2):117–23. doi:10.1017/S146039690999029X
9. Buckle GC, Collins JP, Sumba PO, Nakalema B, Omenah D, Stiffler K, et al. Factors influencing time to diagnosis and initiation of treatment of endemic Burkitt lymphoma among children in Uganda and western Kenya: a cross-sectional survey. Infect Agent Cancer (2013) 8(1):36. doi:10.1186/1750-9378-8-36
10. Brown CA, Suneja G, Tapela N, Mapes A, Pusoentsi M, Mmalane M, et al. Predictors of timely access of oncology services and advanced-stage cancer in an HIV-endemic setting. Oncologist (2016) 21(6):731–8. doi:10.1634/theoncologist.2015-0387
11. Brinton L, Figueroa J, Adjei E, Ansong D, Biritwum R, Edusei L, et al. Factors contributing to delays in diagnosis of breast cancers in Ghana, West Africa. Breast Cancer Res Treat (2017) 162(1):105–14. doi:10.1007/s10549-016-4088-1
12. Patel JD, Galsky MD, Chagpar AB, Pyle D, Loehrer PJ Sr. Role of American society of clinical oncology in low- and middle-income countries. J Clin Oncol (2011) 29(22):3097–102. doi:10.1200/JCO.2011.35.6378
13. Ezeome ER. Delays in presentation and treatment of breast cancer in Enugu, Nigeria. Nigerian J Clin Pract (2010) 13(3):311–6.
14. Pace LE, Mpunga T, Hategekimana V, Dusengimana JM, Habineza H, Bigirimana JB, et al. Delays in breast cancer presentation and diagnosis at two rural cancer referral centers in Rwanda. Oncologist (2015) 20(7):780–8. doi:10.1634/theoncologist.2014-0493
15. Ibrahim NA, Oludara MA. Socio-demographic factors and reasons associated with delay in breast cancer presentation: a study in Nigerian women. Breast (2012) 21(3):416–8. doi:10.1016/j.breast.2012.02.006
16. Akhigbe AO, Omuemu VO. Knowledge, attitudes and practice of breast cancer screening among female health workers in a Nigerian urban city. BMC Cancer (2009) 9:203. doi:10.1186/1471-2407-9-203
17. Adesina A, Chumba D, Nelson AM, Orem J, Roberts DJ, Wabinga H, et al. Improvement of pathology in sub-Saharan Africa. Lancet Oncol (2013) 14(4):e152–7. doi:10.1016/S1470-2045(12)70598-3
18. Mpunga T, Tapela N, Hedt-Gauthier BL, Milner D, Nshimiyimana I, Muvugabigwi G, et al. Diagnosis of cancer in rural Rwanda: early outcomes of a phased approach to implement anatomic pathology services in resource-limited settings. Am J Clin Pathol (2014) 142(4):541–5. doi:10.1309/AJCPYPDES6Z8ELEY
19. Handayani K, Sitaresmi MN, Supriyadi E, Widjajanto PH, Susilawati D, Njuguna F, et al. Delays in diagnosis and treatment of childhood cancer in Indonesia. Pediatr Blood Cancer (2016) 63(12):2189–96. doi:10.1002/pbc.26174
20. Unger-Saldana K, Infante-Castaneda C. Is breast cancer delay really the patient’s fault. In: Deng M, Raia F, Vacarella M, editors. Relational Concepts in Medicine. Inter-disciplinary press (2012). Available from: https://www.researchgate.net/profile/Karla_Unger-Saldana/publication/265411300_Is_breast_cancer_delay_really_the_patient%27s_fault/links/54e74c8b0cf2cd2e0292ca8a/Is-breast-cancer-delayreally-the-patients-fault.pdf
21. Unger-Saldana K, Infante-Castaneda C. Delay of medical care for symptomatic breast cancer: a literature review. Salud Publica Mex (2009) 51(Suppl 2):s270–85. doi:10.1590/S0036-36342009000800018
22. Tapela Neo M, Kebabonye-Pusoentsi M, Botebele K, Peluso MJ, Nkele I, Efstathiou J, et al. Tackling health system delays for cancer patients in LMICs: an innovative multicomponent programmatic intervention in Botswana. J Global Oncol (2016) 2(3 Suppl):41s–2s. doi:10.1200/JGO.2016.003715
23. Ndlovu K, Littman-Quinn R, Park E, Dikai Z, Kovarik CL. Scaling up a mobile telemedicine solution in Botswana: keys to sustainability. Front Public Health (2014) 2:275. doi:10.3389/fpubh.2014.00275
24. The World Bank Group. Available from: https://data.worldbank.org/indicator/SH.MED.NUMW.P3?locations=BW (Accessed: April 23, 2018).
25. Botswana Health Accounts Report 2013/4. Statistical report. Available from: https://www.hfgproject.org/botswana-health-accounts-2013-2014-statistical-report/ (Accessed: April 23, 2018).
26. World Health Organization. Botswana country profile 2014. Available from: http://www.who.int/countries/bwa/en/ (Accessed: April 23, 2018).
27. Botswana Population Census. 2011. Available from: https://www.statsbots.org.bw/sites/default/files/2011%20Population%20and%20housing%20Census.pdf (Accessed: May 15, 2017).
28. Musabyemariya F, Kirby K, Nshimyiryo A, et al. Laying the foundation for national scale-up of cancer care: feedback on nationally implemented baseline cancer trainings for non-oncology clinicians in Rwanda. Presented at the Fifth Annual East African Health and Scientific Conference & International Health Exhibition and Trade Fair. Kampala, Uganda (2014).
29. Tapela NM, Mpunga T, Hedt-Gauthier B, Moore M, Mpanumusingo E, Xu MJ, et al. Pursuing equity in cancer care: implementation, challenges and preliminary findings of a public cancer referral center in rural Rwanda. BMC Cancer (2016) 16:237. doi:10.1186/s12885-016-2256-7
30. Bussmann C, Rotz P, Ndwapi N, Baxter D, Bussmann H, Wester CW, et al. Strengthening healthcare capacity through a responsive, country-specific, training standard: the KITSO AIDS training program’s support of Botswana’s national antiretroviral therapy rollout. Open AIDS J (2008) 2:10–6. doi:10.2174/1874613600802010010
31. Kirkpatrick DL. Evaluating Training Programs: The Four Levels. 2nd ed. San Francisco, CA: Berrett-Koehler (1998).
32. Asirwa FC, Greist A, Busakhala N, Rosen B, Loehrer PJ. Medical education and training: building in-country capacity at all levels. J Clin Oncol (2017) 34(1):36–42. doi:10.1200/JCO.2015.63.0152
33. Gajalakshmi CK, Krishnamurthi S, Ananth R, Shanta V. Cervical cancer screening in Tamilnadu, India: a feasibility study of training the village health nurse. Cancer Causes Control (1996) 7(5):520–4. doi:10.1007/BF00051884
34. Ramogola-Masire D, de Klerk R, Monare B, Ratshaa B, Friedman HM, Zetola NM. Cervical cancer prevention in HIV-infected women using the “see and treat” approach in Botswana. J Acquir Immune Defic Syndr (2012) 59(3):308–13. doi:10.1097/QAI.0b013e3182426227
35. Sankaranarayanan R, Ramadas K, Thomas G, Muwonge R, Thara S, Mathew B, et al. Trivandrum oral cancer screening study G: effect of screening on oral cancer mortality in Kerala, India: a cluster-randomised controlled trial. Lancet (2005) 365(9475):1927–33. doi:10.1016/S0140-6736(05)66658-5
36. Warnakulasuriya KA, Ekanayake AN, Sivayoham S, Stjernsward J, Pindborg JJ, Sobin LH, et al. Utilization of primary health care workers for early detection of oral cancer and precancer cases in Sri Lanka. Bull World Health Organ (1984) 62(2):243–50.
37. Stover J, Fidzani B, Molomo BC, Moeti T, Musuka G. Estimated HIV trends and program effects in Botswana. PLoS One (2008) 3(11):e3729. doi:10.1371/journal.pone.0003729
38. Kar SS, Thakur JS, Jain S, Kumar R. Cardiovascular disease risk management in a primary health care setting of north India. Indian Heart J (2008) 60(1):19–25.
39. Labhardt ND, Balo JR, Ndam M, Grimm JJ, Manga E. Task shifting to non-physician clinicians for integrated management of hypertension and diabetes in rural Cameroon: a programme assessment at two years. BMC Health Serv Res (2010) 10:339. doi:10.1186/1472-6963-10-339
40. Rowe AK, De Savigny D, Lanata CF, Victora CG. How can we achieve and maintain high-quality performance of health workers in low-resource settings? Lancet (2005) 366(9490):1026–35. doi:10.1016/S0140-6736(05)67028-6
41. Moodley J, Kawonga M, Bradley J, Hoffman M. Challenges in implementing a cervical screening program in South Africa. Cancer Detect Prev (2006) 30(4):361–8. doi:10.1016/j.cdp.2006.07.005
42. Paredes P, Pena M, Flores-Guerra E, Diaz J, Trostle J. Factors influencing physicians’ prescribing behavior in the treatment of childhood diarrhoea: knowledge may not be the clue. Soc Sci Med (1996) 42:1141–53. doi:10.1016/0277-9536(95)00387-8
43. Aarons GA, Hurlburt M, Horwitz SM. Advancing a conceptual model of evidence-based practice implementation in public service sectors. Adm Policy Ment Health (2011) 38:4–23. doi:10.1007/s10488-010-0327-7
Keywords: cancer early diagnosis, health system delays, primary care, primary care providers, Botswana, sub-Saharan Africa, training
Citation: Tapela NM, Peluso MJ, Kohler RE, Setlhako II, Botebele K, Gabegwe K, Nkele I, Narasimhamurthy M, Mmalane M, Grover S, Barak T, Shulman LN, Lockman S and Dryden-Peterson S (2018) A Step Toward Timely Referral and Early Diagnosis of Cancer: Implementation and Impact on Knowledge of a Primary Care-Based Training Program in Botswana. Front. Oncol. 8:187. doi: 10.3389/fonc.2018.00187
Received: 28 February 2018; Accepted: 11 May 2018;
Published: 29 May 2018
Edited by:
Jianguang Ji, Lund University, SwedenReviewed by:
Hao Liu, Southern Medical University, ChinaAlireza Sadjadi, Tehran University of Medical Sciences, Iran
Copyright: © 2018 Tapela, Peluso, Kohler, Setlhako, Botebele, Gabegwe, Nkele, Narasimhamurthy, Mmalane, Grover, Barak, Shulman, Lockman and Dryden-Peterson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Neo M. Tapela, bnRhcGVsYUBnbWFpbC5jb20=
 Neo M. Tapela
Neo M. Tapela Michael J. Peluso
Michael J. Peluso Racquel E. Kohler4
Racquel E. Kohler4 Mompati Mmalane
Mompati Mmalane Surbhi Grover
Surbhi Grover Lawrence N. Shulman
Lawrence N. Shulman Scott Dryden-Peterson
Scott Dryden-Peterson