- Department of Radiation Oncology, Rhode Island Hospital/Brown Alpert Medical School, Providence, RI, USA
The Malcolm Baldrige National Quality Improvement Act was signed into law in 1987 to advance US business competitiveness and economic growth. Administered by the National Institute of Standards and Technology, the Act created the Baldrige National Quality Program, recently renamed the Baldrige Performance Excellence Program. The comprehensive analytical approaches referred to as the Baldrige Healthcare Criteria, are very well-suited for the evaluation and sustainable improvement of radiation oncology management and operations. A multidisciplinary self-assessment approach is used for radiotherapy program evaluation and development in order to generate a fact-based, knowledge-driven system for improving quality of care, increasing patient satisfaction, enhancing leadership effectiveness, building employee engagement, and boosting organizational innovation. This methodology also provides a valuable framework for benchmarking an individual radiation oncology practice’s operations and results against guidelines defined by accreditation and professional organizations and regulatory agencies.
Introduction
Administered by the National Institute of Standards and Technology (NIST), the Malcolm Baldrige National Quality Improvement Act was signed into law in 1987 to advance US business competitiveness and economic growth. The Act created the original Baldrige National Quality Program, recently renamed the Baldrige Performance Excellence Program. At first targeted exclusively to large commercial, for-profit enterprises, categories for health care, education, and non-profits were later added. Today, Baldrige assessment and quality improvement tools are widely and effectively used by organizations of all types and sizes (Latham and Vinyard, 2008).
Analytical techniques presented in the Baldrige 2011–2012 Health Care Criteria for Performance Excellence are well-suited for the evaluation and sustainable improvement of Radiation Oncology management and operations (Sternick, 2010). The Criteria are designed to facilitate organizational performance enhancement within an increasingly complex and competitive health care environment. A fact-based system is used for review of processes and procedures aimed at improving quality of care, increasing patient satisfaction, enhancing leadership effectiveness, building employee engagement, and boosting organizational innovation.
The Baldrige Performance Excellence Framework (Figure 1) consists of an Organizational Profile and seven interdependent Criteria Categories, with a dual focus on both process and results.
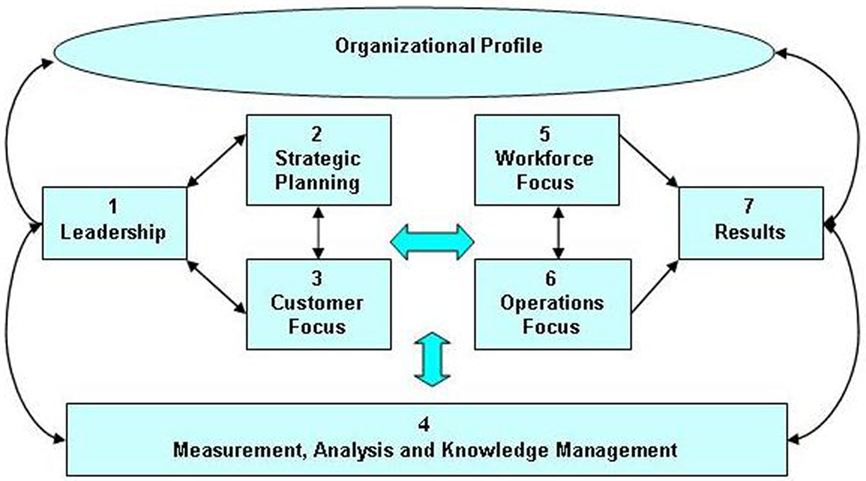
Figure 1. Baldrige health care criteria for performance excellence framework. Source: National Institute of Standards and Technology, Department of Commerce.
Organizational Profile
Organizational Profile preparation serves as an essential preamble to the individual Criteria Categories. Factors are selected for consideration in the Profile that have a demonstrable impact on a Radiation Oncology organization’s operating environment, its strategic situation and key relationships with patients and other stakeholders.
Developing Mission, Vision, and Values Statements
The successful practice of Radiation Oncology requires a staff receptive to collaborative involvement with multiple activities. Individual affirmation of the need for participation in these efforts by each staff member is critical. To this end, Mission, Vision, and Values statements (Pierce and Robinson, 2003) developed by consensus are key to the creation of a clear understanding of and commitment to organizational principles, goals, and strategic initiatives.
The Mission Statement expresses functions that contribute directly to Radiation Oncology strategic imperatives. The Vision Statement defines a preferred future for the organization in order to inspire confident participation by all staff and facilitate positive outcomes. Values are deeply held convictions that provide the ethical foundation on which staff behavior is built in order to successfully fulfill the Mission and Vision of the organization.
The following are examples of Mission, Vision, and Values statements that have been designed for a hospital-based, academic-affiliated Radiation Oncology Department.
Mission: “What are we trying to accomplish?”
We are committed to providing the highest quality patient care, innovative scientific advances, and teaching programs in support of the clinical, research, and educational objectives of the Radiation Oncology Department, the Hospital, and the Medical School.
Vision: “Where are we headed, and how do we want to be viewed?”
The exceptional quality and significance of the clinical, research, and educational programs we offer will generate widespread acknowledgment among our professional peers and the population we serve that we are a center of Radiation Oncology performance excellence.
Values: “What is truly important to us?”
• Excellence – We strive for excellence, delivering the best possible Radiation Oncology services in an environment that attracts and retains outstanding professionals.
• Customer Focus – We work diligently to satisfy our customers including patients and their families, referring physicians, administrators, co-workers, and other stakeholders.
• Innovation – We are constantly looking for ways to improve the quality of our services by supporting innovation, embracing change, and encouraging the development of new ideas and knowledge.
• Teamwork – We endeavor to create a supportive, enjoyable working atmosphere where our collective energy and intelligence enable us to succeed at our highest potential, both individually and as a department.
• Compassion – We earn trust through the courtesy, sensitivity, and respect we demonstrate to our patients and co-workers.
• Integrity – We are truthful, equitable, and open in all our relationships.
Relationship Analysis
Relationship analysis includes an evaluation of the Radiation Oncology management structure to ensure that its design and operational effectiveness are adequate to fulfill the expectations and gain the support of a multidisciplinary workforce as it personalizes and assesses the quality of radiotherapy operations. Throughout their daily routines, Radiation Oncology staff members of necessity develop a range of communication channels both within and outside of their workgroup-associated specialty roles. Because maintaining successful interpersonal relationships is an important component of job satisfaction, appropriate management of these interactions is vital to both individual and organizational success (Fisher et al., 1991).
Monitoring Productivity and Financial Position
Accurate documentation of clinical procedures is mandatory for billing purposes as well as a valuable means of illustrating the range of services and the significant contributions made by a Radiation Oncology practice in support of broader institutional operations and objectives. The method of coding utilized by health care providers to account for these services is the current procedural terminology (CPT) system, which is maintained and updated annually by the American Medical Association (Abraham et al., 2011). Teletherapy and brachytherapy CPT procedure codes documenting initial consultation, treatment planning, medical physics, treatment devices, special services, and treatment management have been authorized for insurance claims submitted to the Center for Medicare and Medicaid Services (CMS) and private insurers. These data can be summarized advantageously for internal use to demonstrate Radiation Oncology productivity.
Criteria Category Assessments
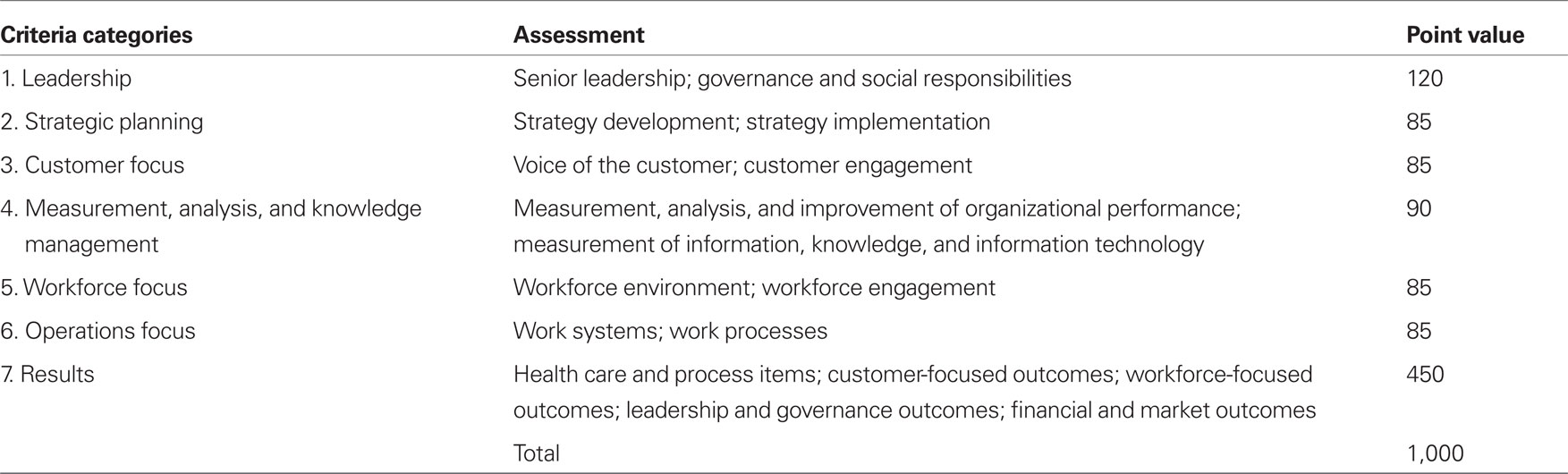
After the Organizational Profile is completed, the subsequent phases of the Performance Excellence agenda move to an in-depth appraisal of seven principal Health Care Criteria Categories (Figure 1; Table 1).
A Point Value is assigned to each of the Categories, facilitating a review of the status of current operations and progress over time so that defined goals can be measured and evaluated objectively. Scoring guidelines are described further in Section “Scoring Guidelines.”
Category 1 – Leadership (120 Points)
The Leadership Category deals with approaches used by the senior management team to deploy the organization’s Mission, Vision, and Values and fulfill legal and ethical responsibilities for patients, accrediting bodies, regulatory agencies, and other stakeholders. Areas to be reviewed for demonstrated evidence of leadership commitment include:
• Planning – Dedication to the concept of creating a sustainable organization by preparing adequately for future internal and external regulatory, financial, market, and operational challenges.
• Environment – Creation of a working environment that endorses a culture of patient safety, quality, and satisfaction.
• Communications – Encouragement of open participative communication techniques involving the full Radiation Oncology multidisciplinary staff to support organizational and personal learning and the development of future leaders.
• Implementation – A focus on action to achieve defined goals and objectives.
Category 2 – Strategic Planning (85 Points)
Successful Strategic Planning requires decisive leadership involvement for generating plans to achieve strategic objectives. In this Category, a number of processes are evaluated for the effectiveness of the techniques used to formulate and implement them:
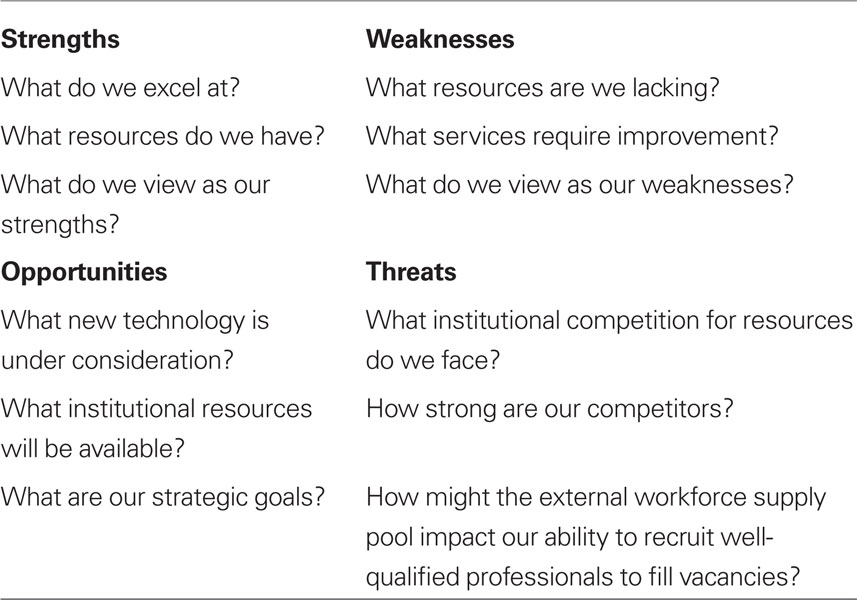
• SWOT Analysis – Strengths, Weaknesses, Opportunities, Threats (SWOT) analysis is an established strategic planning tool used by diverse organizations as a guide for decision-making (Blaney, 2008). The SWOT matrix-based process (Table 2) assists with the initial consideration of internal resources and deficiencies (Strengths and Weaknesses) and environmental impacts (Opportunities and Threats) that influence successful achievement of defined strategic objectives. Strengths are characteristics that make a positive contribution to the achievement of an objective. Weaknesses are characteristics detrimental to the achievement of an objective. Opportunities are factors that can facilitate achievement of an objective and perhaps lead to additional or modified objectives. Threats are factors that might obstruct the achievement of an objective.
• Consideration of Options – Evaluation of alternative strategies using the SWOT analysis as a guide to move the implementation stage forward effectively by utilizing Strengths, confronting Weaknesses, taking advantage of Opportunities, and minimizing Threats.
• Selection of Objectives – Targeting for implementation the most desirable options that are consistent with the Mission, Vision, and Values analysis performed during preparation of the Organizational Profile (see Developing Mission, Vision, and Values Statements).
• Implementation – Specification of action plans for the allocation of required personnel, equipment, and financial resources to achieve defined strategic objectives.
• Evaluation – Development of indicators that assess progress to defined strategic objectives.
Category 3 – Customer Focus (85 Points)
Radiation Oncology “customers” or stakeholders include patients and their families, referring physicians, administrators, potential donors, community groups, and others who might be impacted by the organization’s actions. Building successful stakeholder relationships is vital to the attainment of goals and the identification of new opportunities for innovation. The following elements in the Customer Focus Category are evaluated:
• Categorization – Identification of stakeholders who directly and indirectly influence Radiation Oncology operations.
• Listening – Determination of the differing requirements, needs, and expectations of stakeholders.
• Feedback – Methods used to acquire feedback from patients and other stakeholders regarding satisfaction with the clinical services provided and overall organizational performance.
• Communication – Information transmission and exchange techniques employed to ensure that stakeholders are kept fully informed about Radiation Oncology operations and concerns.
Category 4 – Measurement, Analysis, and Knowledge Management (90 Points)
Evidence-based measurement of organizational performance takes into account the techniques employed for resource utilization and information technology management and how their application demonstrates continuous improvement over time. Indicators to be analyzed in this Category include:
• Equipment Management – Policies and procedures to ensure the accuracy, integrity, and reliability of Radiation Oncology equipment, computer hardware, and software and the data that are acquired and utilized for treatment planning, machine control, and electronic medical record (EMR) systems.
• Patient Data Management – Policies and procedures to maintain the privacy and security of patient information.
• Performance Improvement – Policies and procedures for prioritizing projects and processes to facilitate innovation and the achievement of strategic objectives.
Category 5 – Workforce Focus (85 Points)
During this review, key factors are evaluated that impact the multidisciplinary team of clinical professionals, support staff, service personnel, students, and volunteers who are actively engaged in the organization’s work and contributing to the advancement of its Mission, Vision, and Values. Areas to be assessed include:
• Engagement – Reward system for high performance work, innovation, and initiative.
• Learning – Support for continuing education, maintenance of certification, and development of new knowledge and skills through formal training or on-the-job mentoring.
• Workforce Core Competencies – Approaches for recruiting and retaining key staff to fulfill clinical, research, and teaching responsibilities and address strategic challenges.
• Environment – Provision of adequate personnel, space, and equipment to successfully carry out clinical, teaching, and research responsibilities and undertake new programs.
Category 6 – Operations Focus (85 Points)
The Operations Focus assesses the format and effectiveness of the radiotherapy quality and safety management program and the use of work process improvement tools (Pawlicki et al., 2011) such as Lean Thinking, Six Sigma Methodology, and Plan-Do-Check-Act (PDCA) to support operations and strategic initiatives.
Evaluation includes:
• Implementation and Management – Identification, design, and execution of work processes that provide value to patients and other key stakeholders.
• Documentation – Tracking of Radiation Oncology work processes to demonstrate improvements in provided services and outcomes.
Category 7 – Results (450 Points)
Results factors (LETCI) summarize, review, and evaluate the overall outcomes achieved in Categories 1–6:
• Levels – measured performance achievements.
• Trends – rate and extent of performance improvements.
• Comparisons – performance relative to industry and/or accreditation agency standards.
• Integration – degree to which processes, procedures, and outcomes support defined organizational goals and objectives.
Scoring Guidelines
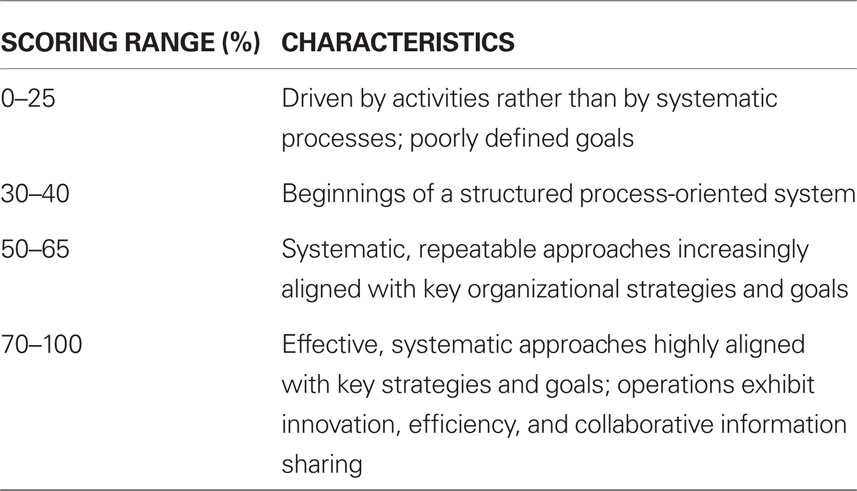
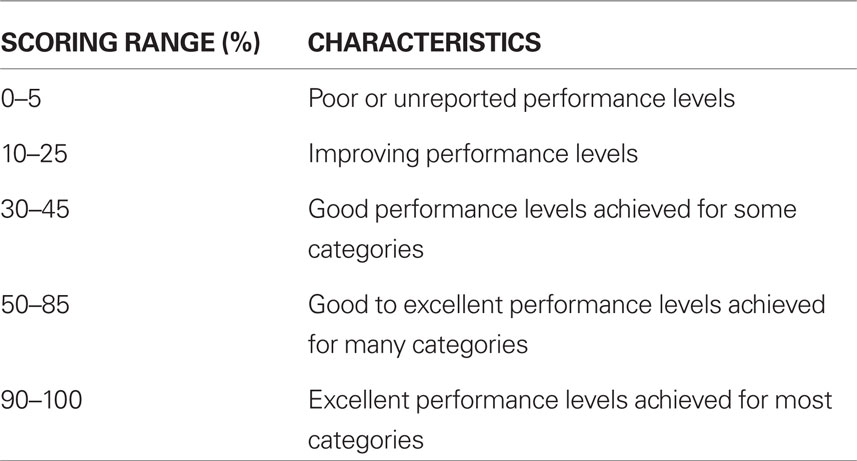
Scoring can be determined using rating scales for two dimensions – processes (Categories 1–6, Table 3) and results (Category 7, Table 4). Approaches and outcomes that meet the general requirements of a particular Category are characterized by a score of 50%. Accomplishments determined to be inferior to or exceeding that ranking are scored accordingly. Final scores are calculated using the product of defined percentiles and the available point value assignments (Table 1).
Conclusion
Based on well-tested approaches that focus on the successful management of complex clinical, educational, and research challenges, the Baldrige Performance Excellence Program offers Radiation Oncology a rich set of tools to achieve measurable advances in the pursuit of quality care, patient satisfaction, and workforce commitment.
Conflict of Interest Statement
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Abraham, M., Ahlman, J. T., Boudreau, A. J., Connelly, J. L., Evans, D. D., and Glenn, R. L. (2011). Current Procedural Terminology – CPT® (2011), Standard Edition. Chicago, IL: American Medical Association.
Fisher, R., Uri, W., and Patton, B. (1991). Getting to Yes – Negotiating Agreement Without Giving In, 2nd Edn. New York: Penguin Books.
Latham, J., and Vinyard, J. (2008). Baldrige User’s Guide – Organization, Diagnosis, Design, and Transformation, 3rd Edn. Hoboken, NJ: John Wiley & Sons.
Pawlicki, T., Dunscombe, P. B., Mundt, A. J., and Scalliet, P. (eds). (2011). Quality and Safety in Radiotherapy, Boca Raton, FL: Taylor & Francis.
Pierce, J. A., and Robinson, R. B. (2003). Strategic Management – Formulation, Implementation and Control. New York: McGraw-Hill Irwin.
Keywords: Baldrige program, health care criteria, radiation oncology performance excellence
Citation: Sternick ES (2011) Using Baldrige performance excellence program approaches in the pursuit of radiation oncology quality care, patient satisfaction, and workforce commitment. Front. Oncol. 1:9. doi: 10.3389/fonc.2011.00009
Received: 13 May 2011; Accepted: 03 June 2011;
Published online: 20 June 2011.
Edited by:
Daniel Grant Petereit, Rapid City Regional Hospital, USAReviewed by:
Daniel Ma, Washington University School of Medicine, USAChristopher Schultz, Medical College of Wisconsin, USA
Copyright: © 2011 Sternick. This is an open-access article subject to a non-exclusive license between the authors and Frontiers Media SA, which permits use, distribution and reproduction in other forums, provided the original authors and source are credited and other Frontiers conditions are complied with.
*Correspondence: Edward S. Sternick, Department of Radiation Oncology, Rhode Island Hospital, 593 Eddy Street, Providence, RI 02903, USA. e-mail: esternick@lifespan.org