- 1Yunnan University of Traditional Chinese Medicine, Kunming, China
- 2Department of Acupuncture and Moxibustion, Yunnan Provincial Hospital of Traditional, Chinese Medicine, The First Affiliated Hospital of Yunnan University of Chinese Medicine, Kunming, China
- 3Yan’an Hospital Affiliated to Kunming Medical University, Kunming, China
- 4Second Clinical Medical College, Heilongjiang University of Chinese Medicine, Harbin, China
Objective: This systematic review and meta-analysis aimed to evaluate the efficacy of combination scalp acupuncture in treating post-stroke cognitive impairment.
Methods: A comprehensive search was conducted across eight databases: PubMed, Web of Science, Cochrane Database, Embase, CBM, CNKI, WanFang, and VIP, targeting randomized controlled trials (RCTs) published from the inception of these databases until October 24, 2024. The inclusion criteria focused on RCTs that compared scalp acupuncture with conventional treatments as therapeutic interventions for patients suffering from post-stroke cognitive impairment (PSCI). The effectiveness of these treatments was evaluated using various outcome measures, including the Mini-Mental State Examination (MMSE), the Montreal Cognitive Assessment (MoCA), the Loewenstein Occupational Therapy Cognitive Assessment (LOTCA), as well as P300 latency and amplitude, which collectively assess cognitive function. Two independent reviewers conducted a risk of bias (ROB2) assessment, and data analysis was performed using Review Manager (RevMan) version 5.4.
Results: This analysis included a total of 28 studies involving 1,995 patients. However, according to the standards of the ROB2 tool, most of these studies exhibited various methodological issues. The comprehensive analysis indicates that the efficacy of combined scalp acupuncture in treating post-stroke cognitive impairment (PSCI) is superior to that of single treatments, as evidenced by improvements across multiple scales, including the Montreal Cognitive Assessment (MoCA), Mini-Mental State Examination (MMSE), Loewenstein Occupational Therapy Cognitive Assessment (LOTCA), P300 latency, and amplitude. Specifically, the overall effective rate was reported as (RR = 1.28, 95% CI: 1.14–1.45, p < 0.0001; I2 = 51%, random effects model). The mean differences for the various scales were as follows: MoCA (MD = 3.55, 95% CI: 2.68–4.41, I2 = 93%, random effects model), MMSE (MD = 3.78, 95% CI: 2.83–4.73, I2 = 94%, random effects model), LOTCA (MD = 9.70, 95% CI: 7.72–11.69, I2 = 57%, random effects model), P300 latency (MD = −21.83, 95% CI: −26.31 to −17.35, I2 = 55%, random effects model), and amplitude (MD = 1.05, 95% CI: 0.76–1.34, I2 = 0%, fixed effects model), demonstrating low, medium, and high levels of heterogeneity, respectively. Notably, one study reported an adverse event related to participant withdrawal during the study.
Conclusion: Combination scalp acupuncture exhibits superior efficacy compared to single-treatment modalities in patients with post-stroke cognitive impairment (PSCI). However, the higher risk of bias (ROB) in the included trials suggests that the quality of evidence about these assessment results may be compromised. Therefore, there is an urgent need for additional high-quality clinical trials to further validate the efficacy and effectiveness of combined scalp acupuncture in treating PSCI, ultimately enhancing the overall level of evidence.
Systematic review registration: https://www.crd.york.ac.uk/prospero/, identifier CRD42024519200.
1 Introduction
Stroke is a predominant cause of mortality and disability globally. A 2019 survey conducted by the World Health Organization (WHO) identifies stroke as the second leading cause of death, responsible for 11% of total fatalities, with a significant proportion of survivors experiencing various functional disabilities (Feigin et al., 2022). Post-stroke cognitive impairment (PSCI) encompasses a broad spectrum of neurological disorders characterized by varying degrees of cognitive dysfunction that may persist for 3 to 6 months following a stroke (Wang and Dong, 2021). The prevalence of post-stroke cognitive impairment (PSCI) ranges from approximately 17 to 66%, with variations influenced by factors such as country, race, and diagnostic criteria (Li M. et al., 2023). PSCI primarily manifests as impairments in higher-level cognitive functions, including learning, memory, executive function, and visuospatial abilities following a stroke. Common symptoms encompass attention deficits, memory impairments, and difficulties in learning (Levine et al., 2015). These cognitive challenges significantly diminish the patient’s quality of life and impose substantial financial and psychological burdens on the patient and their family. Consequently, the pursuit of a safe, effective, affordable, and acceptable treatment has become an urgent priority.
Current effective methods for enhancing cognitive function in stroke patients primarily include pharmacological treatments such as nimodipine, donepezil, and piracetam, as well as cognitive function training (CFT), the use of virtual environments and nursing care (Chang et al., 2011; Rao et al., 2013; Li Y. et al., 2023). Furthermore, research has demonstrated that several other neuroprotective agents can safely and effectively ameliorate cognitive impairment to some degree (Zhang et al., 2014). Nevertheless, long-term treatment presents several challenges that warrant attention, including potential liver and kidney toxicity, gastrointestinal issues, high costs, and concerns regarding patient compliance (Marucci et al., 2021).
Acupuncture has been widely employed in the treatment of stroke patients, addressing cognitive impairment (Liu Y. et al., 2023), dysphagia (Zhu et al., 2023), and motor functions (Bao et al., 2021). Systematic reviews and meta-analyses suggest that acupuncture may enhance post-stroke cognitive impairment (PSCI); however, the considerable heterogeneity among studies raises concerns regarding the reliability of these findings (Wu et al., 2024). Scalp acupuncture (SA), a novel approach distinct from traditional acupuncture, targets specific reflex areas of the brain that correspond to anatomical structures on the surface of the head. This technique stimulates particular regions of the scalp, which can exert direct or indirect effects on the associated brain functional areas, thereby improving cerebral blood circulation and regulating neurotransmitter release, ultimately facilitating neurological recovery. Research has also confirmed its efficacy in ameliorating the condition of patients with PSCI (Du et al., 2018; Chen J. et al., 2020; Xiong et al., 2020). Furthermore, studies suggest that the mechanisms by which acupuncture enhances PSCI involve the inhibition of nuclear factor (NF)-κB and its downstream target gene P53, as well as the modulation of neuronal apoptosis and hippocampal synaptic plasticity (Feng et al., 2013; Yang J. W. et al., 2019; Zhang et al., 2023). Additionally, some research indicates that electroacupuncture can reduce the expression and activity of calmodulin (CaM) while simultaneously increasing calmodulin-dependent protein kinase type IV (CaMKIV) and cyclic adenosine monophosphate response element-binding protein (CREB), along with their related phosphorylation, thereby improving cognitive function (Zhang et al., 2016).
Current research is deficient in data analysis concerning the efficacy of scalp acupuncture treatment for PSCI, which limits the availability of credible evidence. To scientifically assess the effectiveness of scalp acupuncture in treating PSCI, this study conducts a comprehensive analysis of randomized controlled trial data from the establishment of the database up to October 24, 2024. By evaluating multiple outcome indicators, this research aims to provide more robust evidence to support clinical practice.
2 Methods
2.1 Protocol and registration
This study was conducted as a meta-analysis by the Cochrane Handbook for Systematic Reviews of Interventions and has been registered with PROSPERO under registration number CRD 42024519200. Our research strictly adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guidelines (Page et al., 2021). The PRISMA checklist is provided in the Appendix 1.
2.2 Literature search
We conducted a comprehensive search across eight databases, which included four English databases—PubMed, Cochrane Library, Embase, and Web of Science (WoS)—and four Chinese databases—China Biomedicine (CBM), China National Knowledge Infrastructure (CNKI), Chinese Science and Technology Journals (VIP), and WanFang Database. The search covered the period from the establishment of each database up to October 24, 2024, without restrictions on country, language, or publication status. We utilized the MeSH subject headings “scalp acupuncture,” “stroke,” and “cognitive impairment,” with a focus on randomized controlled trials (RCTs) to develop our search strategy. This strategy was specifically tailored to accommodate the unique characteristics of each database. Detailed search terms and strategies for each database are provided in Appendix 2. Additionally, we manually screened the reference lists of all included articles to identify potentially relevant RCTs.
2.3 Inclusion and exclusion criteria
The studies included in this analysis were not restricted by age, gender, race, or ethnicity. The inclusion is as follows: (1) research subjects must meet the diagnostic criteria for stroke patients; (2) the intervention involves scalp acupuncture; (3) the control group consists of sham acupuncture or other treatment methods such as primary treatment or blank control; (4) the study design must be a RCTs; (5) the research must include complete data recording and analysis.
The exclusion criteria are (1) non-randomized controlled trials; (2) exclusion of animal studies; (3) dissertations, conference papers, and case reports; (4) unavailability of original text or full-text data; (5) review articles.
2.4 Study selection and data extraction
Two researchers independently screened the literature included in this study based on established inclusion and exclusion criteria. They selected the titles and abstracts of relevant literature to identify qualified studies for retention. A third researcher assessed any controversial literature. Basic information from the included studies was extracted, including the first author’s name, year of publication, subject status, sample size, intervention measures, and outcome indicators. For articles with incomplete data, the original authors were contacted via email or telephone to obtain any missing or unclear information.
2.5 Risk of bias in individual studies
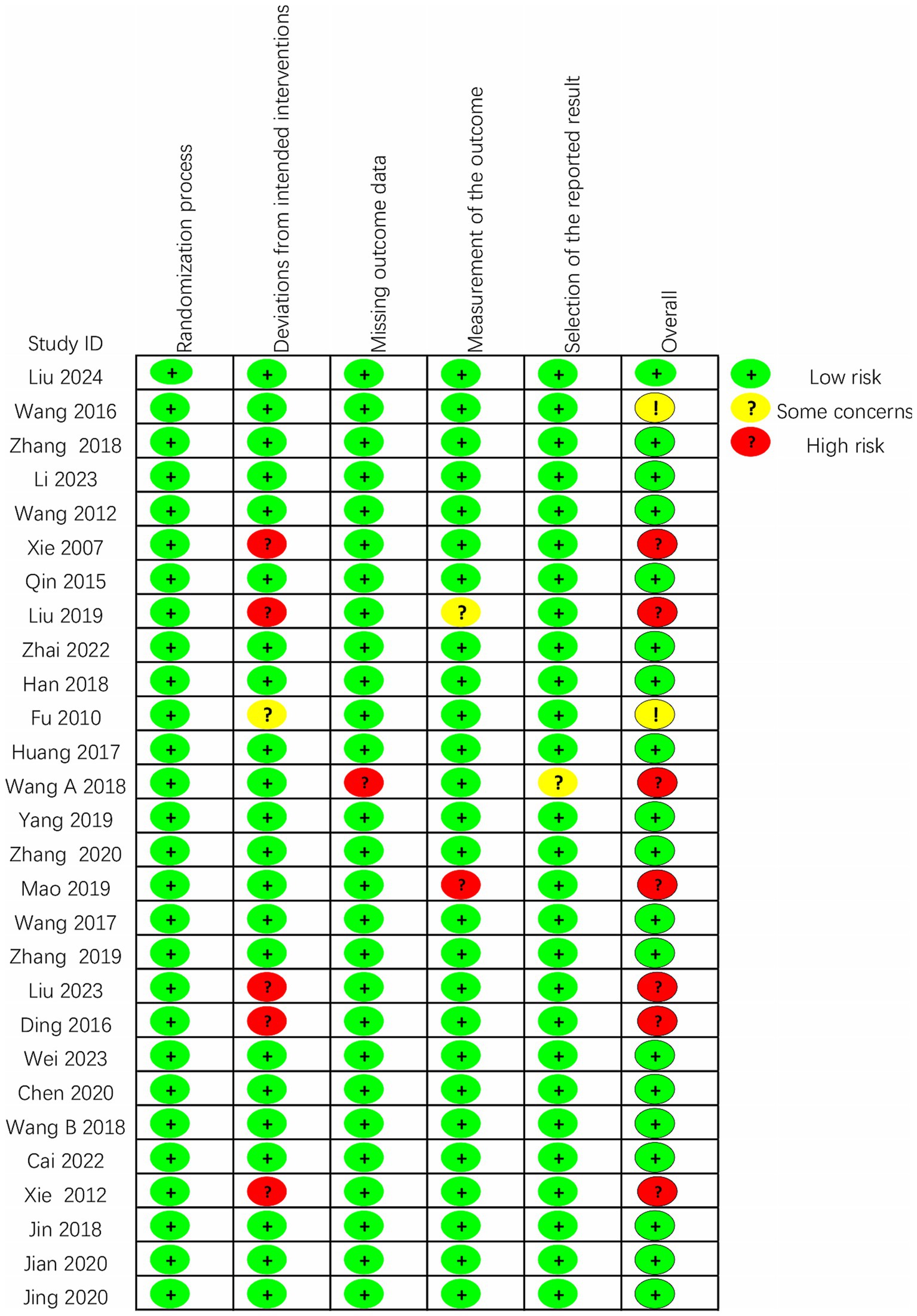
All included studies were RCTs, and the Cochrane Risk of Bias Tool 2.0 (RoB 2) was utilized to assess the risk of bias within these trials. This comprehensive tool evaluates potential biases across five key domains: (1) the randomization process, (2) deviations from the intended intervention, (3) instances of missing outcome data, (4) methods of outcome measurement, and (5) criteria for the selection of reported outcomes. Each domain is classified according to the risk of bias as low risk, high risk, or some concern. To maintain rigorous methodological standards, the risk of bias for each included study was independently assessed by two researchers. A third researcher addressed any discrepancies or inconsistencies identified during the independent assessment to ensure an unbiased evaluation.
2.6 Data analysis
This study utilized RevMan 5.4 software to perform a meta-analysis. The mean difference (MD) is reported as the effect size for continuous outcome measures. In the case of binary variables, the relative risk (RR) and the corresponding 95% confidence interval (CI) represent the effect size. We employed the χ2 test with I2 quantitative analysis to assess inter-study heterogeneity. If p > 0.1 and I2 < 50%, it is deemed that there is no significant heterogeneity among the included studies, and a fixed effects model is applied for the meta-analysis. Conversely, if p < 0.1 and I2 > 50%, it indicates a significant heterogeneity among the studies. Lastly, we conducted subgroup and sensitivity analyses to investigate the sources of heterogeneity and gain a deeper understanding of the intervention’s effects. Publication bias was evaluated using funnel plots and Egger’s bias test.
3 Results
3.1 Study selection
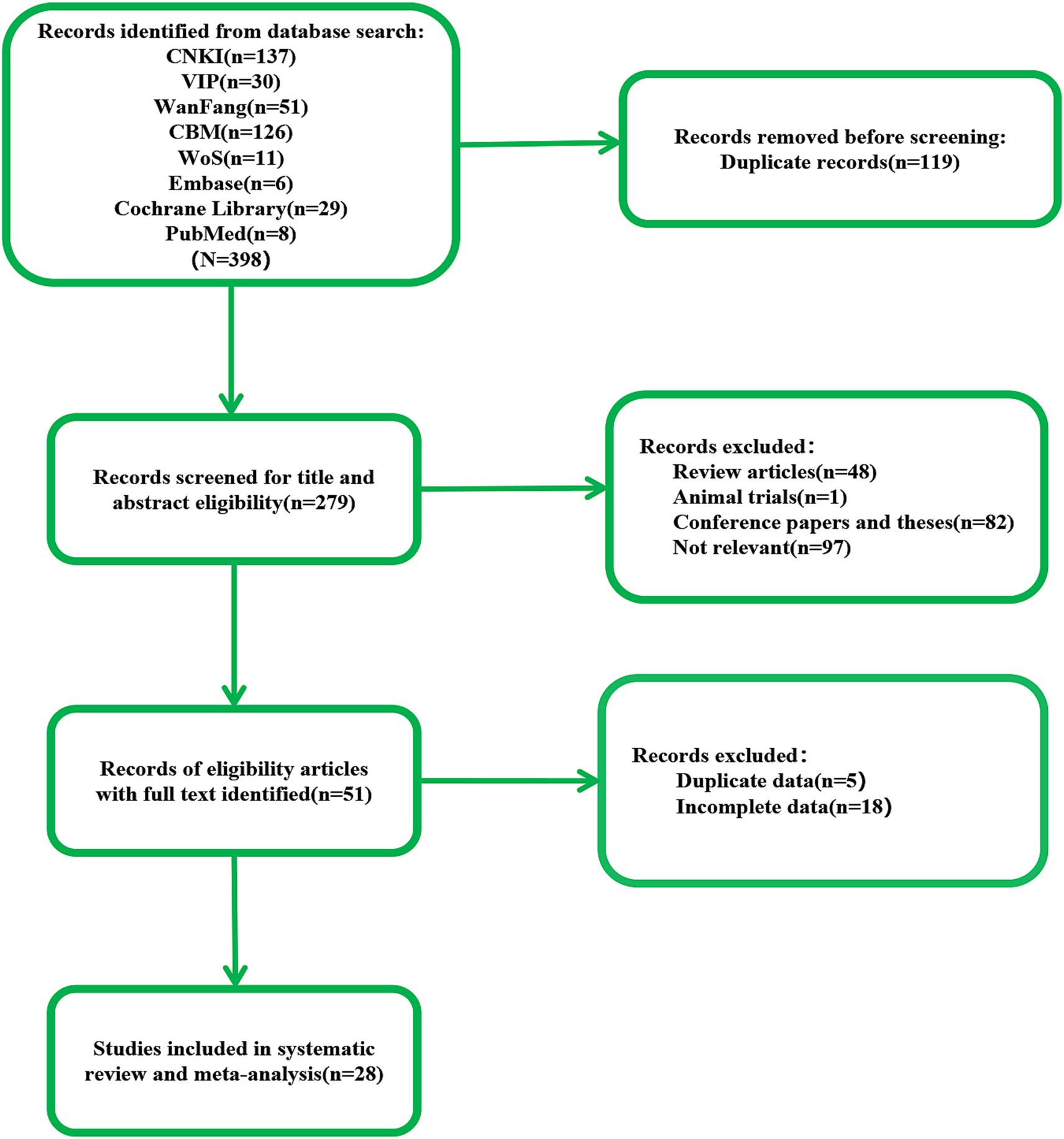
According to the search strategy, we retrieved 398 documents. Our preliminary screening excluded 119 duplicate documents, 82 conference papers and theses, and 49 reviews, systematic reviews, meta-analyses, and animal experiments. Reviewing the titles, abstracts, and keywords, we identified 97 documents that did not align with the research content. Upon examining the complete texts, we discovered that 23 articles contained duplicate or incomplete data. Ultimately, 28 articles were included in this study (Figure 1).
3.2 Study characteristics
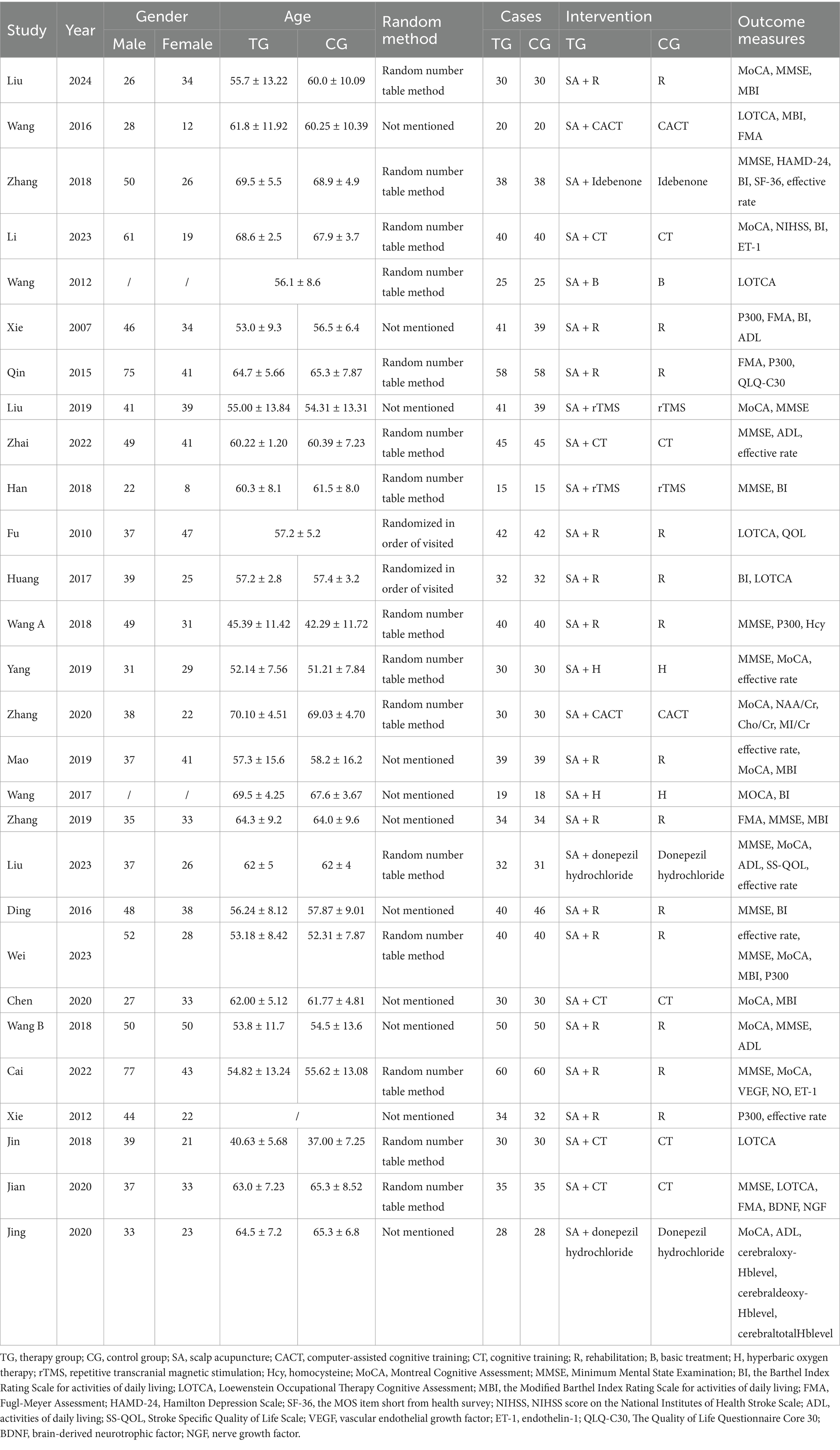
All studies included in this analysis were RCTs. A total of 28 studies involving 1995 participants were examined, with 998 in the treatment group and 997 in the control group. Among the included studies, four were conducted in English (Xie et al., 2012; Du et al., 2018; Chen J. et al., 2020; Xiong et al., 2020), while the remaining 24 were conducted in Chinese (Xie et al., 2007; Fu et al., 2010; Wang et al., 2012; Qin, 2015; Ding and Zhang, 2016; Wang, 2016; Huang et al., 2017; Wang et al., 2017; Han et al., 2018; Wang W. et al., 2018; Wang Y. X. et al., 2018; Zhang and An, 2018; Yang L. et al., 2019; Liu et al., 2019; Mao and Cheng, 2019; Zhang et al., 2019; Chen A. Z. et al., 2020; Zhang et al., 2020; Cai et al., 2022; Zhai et al., 2022; Li and Pan, 2023; Wei et al., 2023; Liu Y. F. et al., 2023; Liu et al., 2024), all within China. There was no statistically significant difference in the baseline characteristics of the treatment and control groups regarding age, disease duration, education level, outcome indicators, and other basic information before enrollment. The intervention methods varied across studies. One study exclusively utilized scalp acupuncture combined with basic treatment (B) (Wang et al., 2012), while the other 27 studies incorporated additional intervention methods, including rehabilitation therapy (R) (Xie et al., 2007; Fu et al., 2010; Xie et al., 2012; Qin, 2015; Ding and Zhang, 2016; Huang et al., 2017; Wang W. et al., 2018; Wang Y. X. et al., 2018; Mao and Cheng, 2019; Zhang et al., 2019; Cai et al., 2022; Wei et al., 2023; Liu et al., 2024), computer-assisted cognitive training (CACT) (Wang, 2016; Zhang et al., 2020) hyperbaric oxygen therapy (H) (Wang et al., 2017; Yang L. et al., 2019), repetitive transcranial magnetic stimulation (rTMS) (Han et al., 2018; Liu et al., 2019), cognitive training (CT) (Du et al., 2018; Chen A. Z. et al., 2020; Xiong et al., 2020; Zhai et al., 2022; Li and Pan, 2023), the donepezil hydrochloride (Chen J. et al., 2020; Liu Y. et al., 2023) and the drug idebenone (Zhang and An, 2018). The control group interventions included nimodipine, CT, donepezil hydrochloride, R, CACT, H, rTMS, idebenone, and conventional symptomatic treatment.
The 28 studies included in this analysis employed four evaluation tools—MoCA, MMSE, LOTCA, and P300—as outcome indicators for scalp acupuncture treatment of post-stroke cognitive impairment (PSCI). Among these, 13 studies (Wang et al., 2017; Wang W. et al., 2018; Yang L. et al., 2019; Liu et al., 2019; Mao and Cheng, 2019; Chen A. Z. et al., 2020; Chen J. et al., 2020; Zhang et al., 2020; Cai et al., 2022; Li and Pan, 2023; Wei et al., 2023; Liu Y. F. et al., 2023; Liu et al., 2024) utilized the MoCA scale as their primary outcome measure. In contrast, 14 studies (Ding and Zhang, 2016; Han et al., 2018; Wang W. et al., 2018; Wang Y. X. et al., 2018; Zhang and An, 2018; Yang L. et al., 2019; Liu et al., 2019; Zhang et al., 2019; Xiong et al., 2020; Cai et al., 2022; Zhai et al., 2022; Wei et al., 2023; Liu Y. et al., 2023; Liu et al., 2024) selected the MMSE scale as their outcome measure, while seven studies (Wang W. et al., 2018; Yang L. et al., 2019; Liu et al., 2019; Cai et al., 2022; Wei et al., 2023; Liu Y. F. et al., 2023; Liu et al., 2024) employed both the MoCA and MMSE scales as outcome measures. Additionally, six studies (Fu et al., 2010; Wang et al., 2012; Wang, 2016; Huang et al., 2017; Du et al., 2018; Xiong et al., 2020) utilized the LOTCA score as an outcome measure. Among the 28 studies, seven studies (Xie et al., 2012; Zhang and An, 2018; Yang L. et al., 2019; Mao and Cheng, 2019; Zhai et al., 2022; Wei et al., 2023; Liu Y. F. et al., 2023) indicated total effectiveness as an outcome indicator. Furthermore, five studies (Xie et al., 2007; Xie et al., 2012; Qin, 2015; Wang Y. X. et al., 2018; Wei et al., 2023) assessed P300’s latency and amplitude as evaluation tools. The included studies primarily employed the Barthel index (BI) and modified Barthel index (MBI) scores to evaluate daily activities. Notably, one study reported an adverse event involving participant withdrawal during the investigation. The characteristics of all 28 studies are summarized in Table 1.
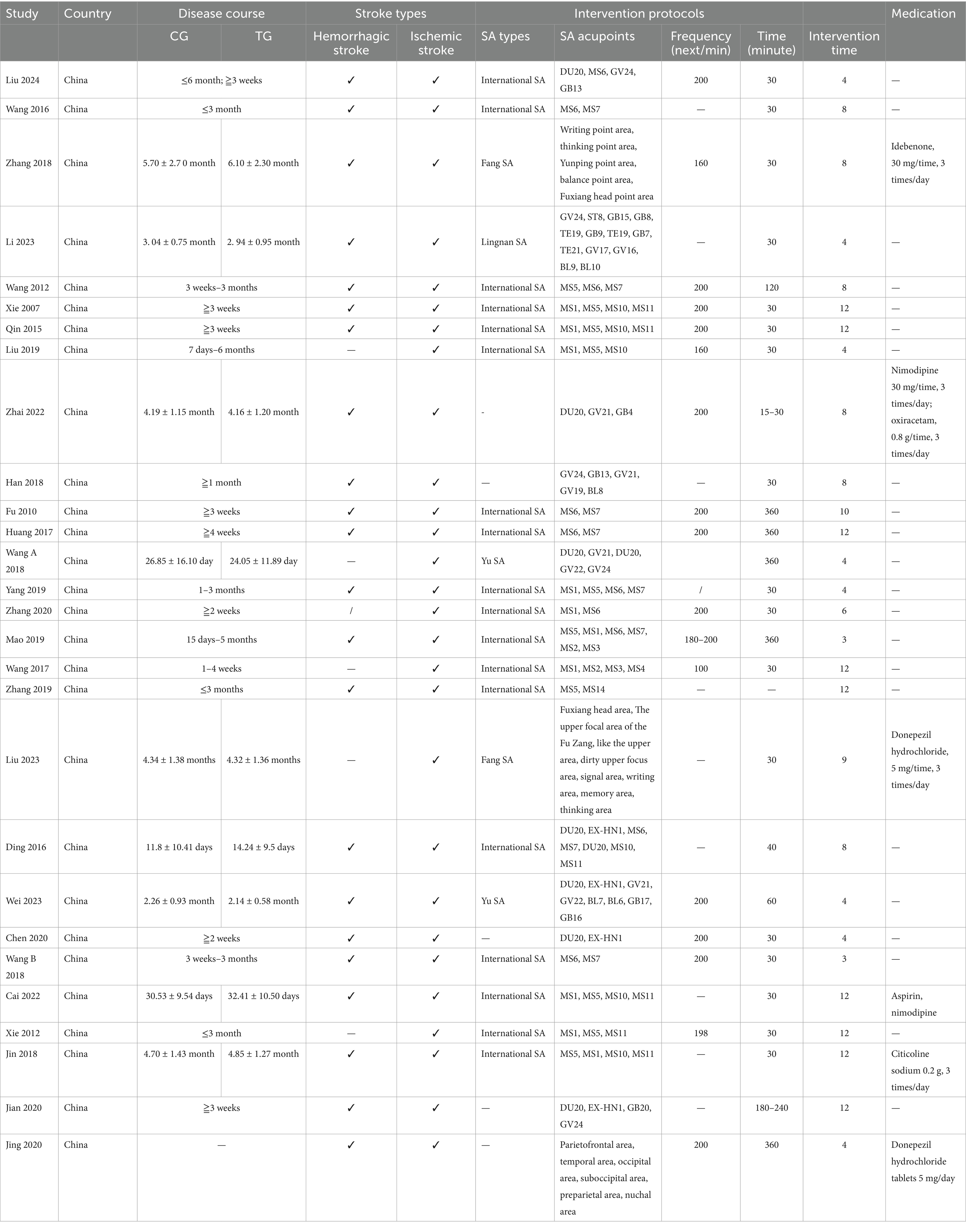
The characteristics of SA parameters vary across the 28 studies examined. Regarding SA type, 19 studies employed International SA (Xie et al., 2007; Fu et al., 2010; Wang et al., 2012; Xie et al., 2012; Qin, 2015; Ding and Zhang, 2016; Wang, 2016; Huang et al., 2017; Wang et al., 2017; Du et al., 2018; Wang W. et al., 2018; Yang L. et al., 2019; Liu et al., 2019; Mao and Cheng, 2019; Zhang et al., 2019; Zhang et al., 2020; Cai et al., 2022; Liu et al., 2024), while two studies utilized Fang SA (Zhang and An, 2018; Liu Y. F. et al., 2023), and another two studies employed Yu SA (Wang Y. X. et al., 2018; Wei et al., 2023). Additionally, 1 study focused on Lingnan SA (Li and Pan, 2023). In terms of treatment duration, 17 studies administered sessions lasting 30 min each (Xie et al., 2007; Wang et al., 2012; Qin, 2015; Wang, 2016; Wang et al., 2017; Du et al., 2018; Han et al., 2018; Wang W. et al., 2018; Zhang and An, 2018; Yang L. et al., 2019; Liu et al., 2019; Chen A. Z. et al., 2020; Zhang et al., 2020; Cai et al., 2022; Li and Pan, 2023; Liu Y. F. et al., 2023; Liu et al., 2024), whereas 1 study lasted 40 min (Ding and Zhang, 2016), another lasted 60 min (Wei et al., 2023), and 1 study had a duration of 120 min (Wang et al., 2012), furthermore, five studies reported sessions lasting 360 min each (Fu et al., 2010; Huang et al., 2017; Wang Y. X. et al., 2018; Mao and Cheng, 2019; Chen J. et al., 2020), while 1 study varied between 15 to 30 min (Zhai et al., 2022), and another ranged from 180 to 240 min (Xiong et al., 2020). The SA parameter characteristics are detailed in Table 2.
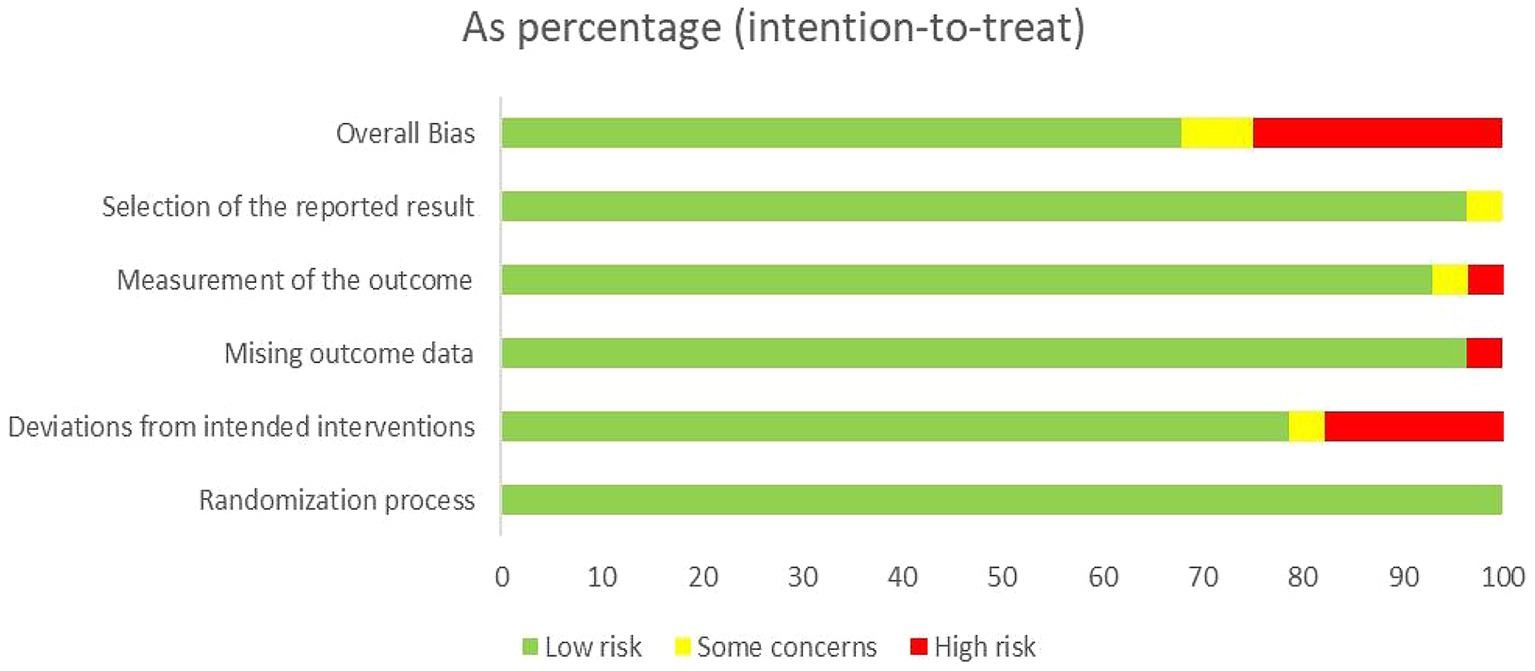
3.3 Study design and risk of bias
The quality of the 28 included randomized controlled trials was generally classified as “low to moderate.” It is important to note that due to the unique nature of scalp acupuncture, all studies were unable to blind operators and participants. Two studies were assessed as having a risk of “some concern” (Fu et al., 2010; Wang, 2016), while 19 studies were categorized as having a low risk (Wang et al., 2012; Qin, 2015; Huang et al., 2017; Wang et al., 2017; Du et al., 2018; Han et al., 2018; Wang W. et al., 2018; Zhang and An, 2018; Yang L. et al., 2019; Zhang et al., 2019; Chen A. Z. et al., 2020; Chen J. et al., 2020; Xiong et al., 2020; Zhang et al., 2020; Cai et al., 2022; Zhai et al., 2022; Li and Pan, 2023; Wei et al., 2023; Liu et al., 2024), and seven studies were identified as having a high risk of bias (Xie et al., 2007; Xie et al., 2012; Ding and Zhang, 2016; Wang Y. X. et al., 2018; Liu et al., 2019; Mao and Cheng, 2019; Liu Y. F. et al., 2023). Regarding the randomization process, most studies were deemed to have a low risk, as the randomization methods were reported in detail, with the random number table method being the most commonly employed technique. Additionally, there was a possibility of selective reporting of results in one study (Wang W. et al., 2018). Detailed quality assessments are presented in Figures 2, 3.
3.4 Meta-analysis
3.4.1 The total effective rate
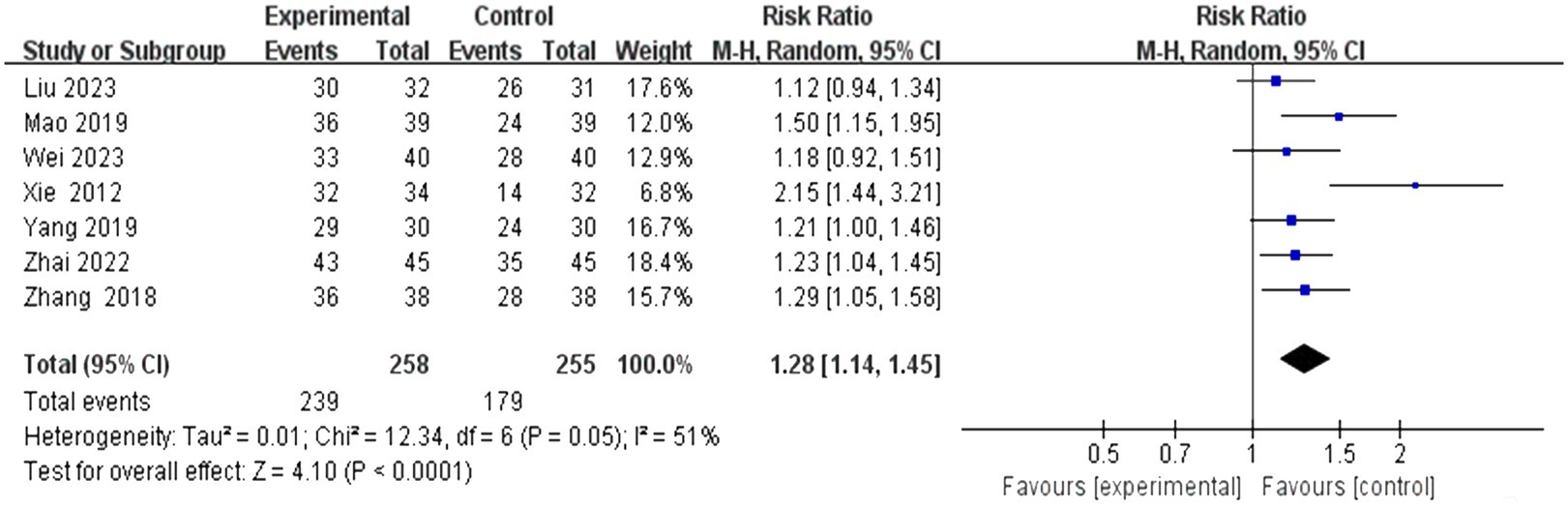
This study encompassed 28 individual studies, of which seven reported on this specific outcome. A subsequent meta-analysis employing a random effects model revealed that the efficacy of the combined scalp acupuncture treatment group was significantly superior to that of the control group (RR = 1.28, 95% CI: 1.14 to 1.45, I2 = 51%, 7 studies, 513 participants). Additionally, the results of the heterogeneity analysis suggest that these findings are robust (Figure 4).
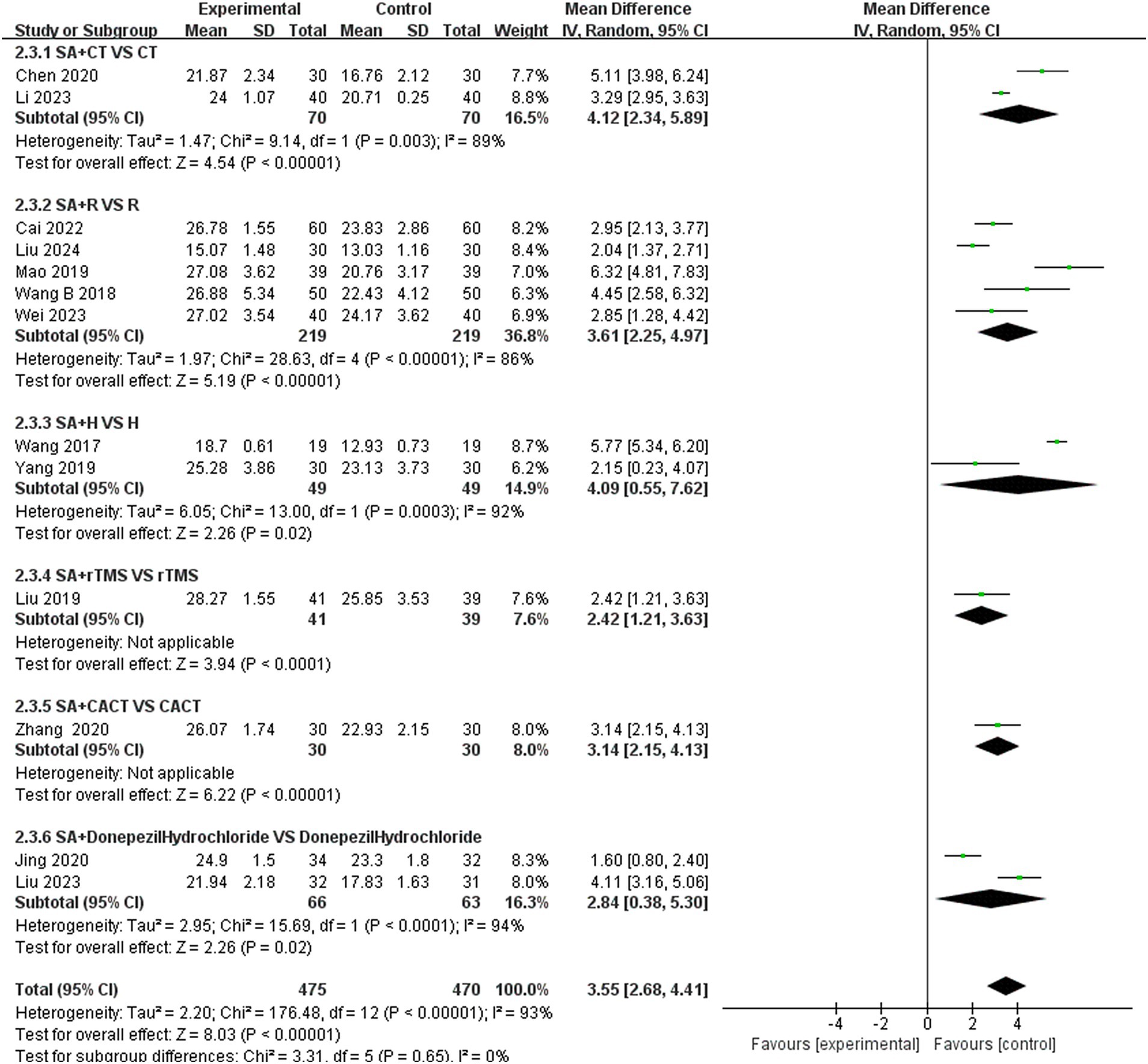
3.4.2 The MoCA scores
In this study, 13 investigations reported MoCA scores. A meta-analysis of the included studies was conducted using a random effects model. The results indicated that the combination of the combined scalp acupuncture treatment was more effective than the control group in enhancing the MoCA scores of PSCI patients (MD = 3.55, 95% CI: 2.68–4.41, I2 = 93%, 13 studies, 944 participants) (Figure 5A). However, there was a high level of heterogeneity across the studies.
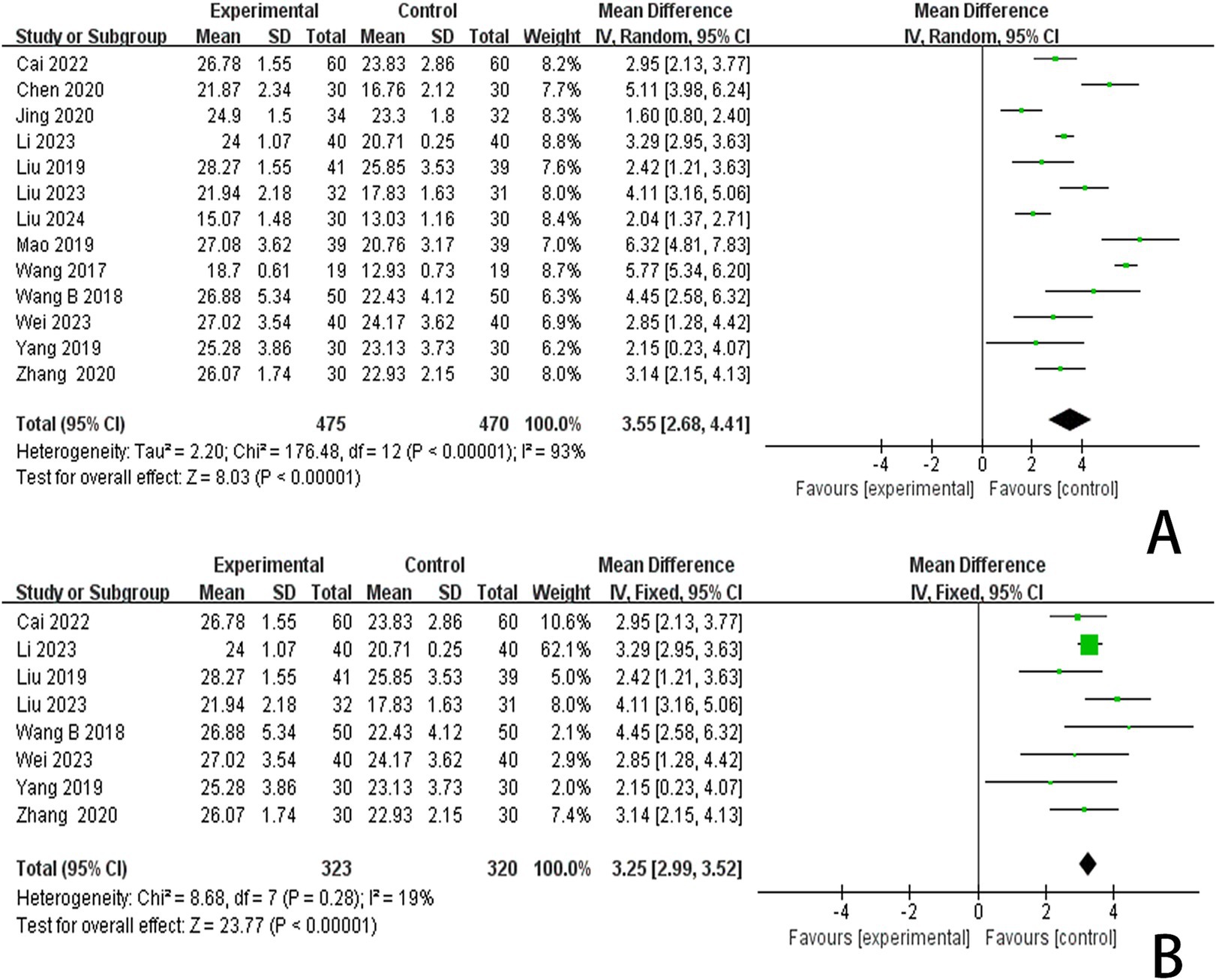
Figure 5. (A) Forest plots of the MoCA scores. (B) Forest plots of the MoCA scores after removing four studies.
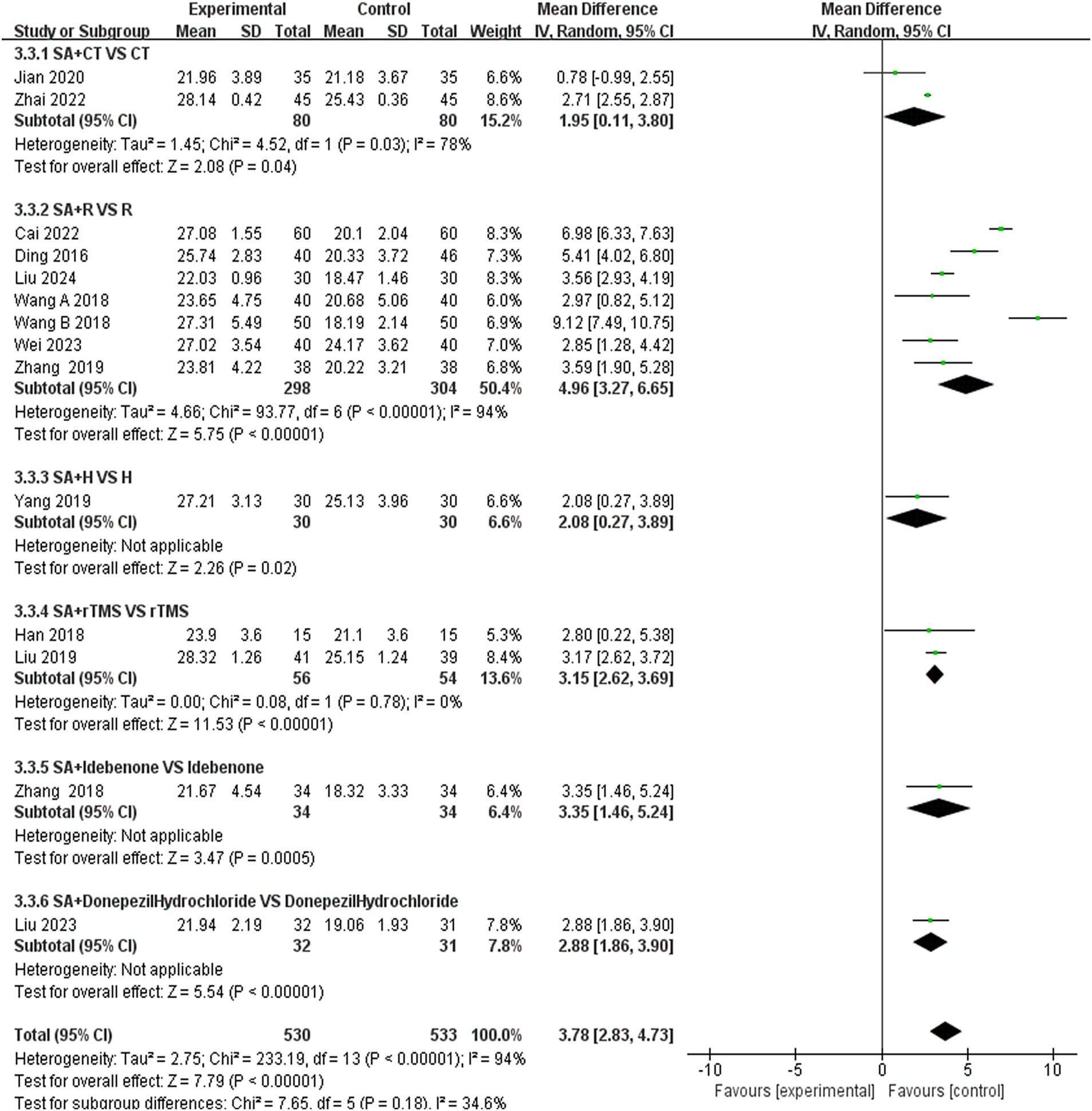
3.4.3 The MMSE scores
In this study, 13 investigations reported MoCA scores. A meta-analysis of the included studies was conducted using a random effects model. The results indicated that the combination of scalp acupuncture treatment was more effective than the control group in enhancing the MoCA scores of PSCI patients (MD = 3.78, 95% CI: 2.83–4.73, I2 = 94%, 14 studies, 1,063 participants) (Figure 6A). However, there was a high level of heterogeneity across the studies.
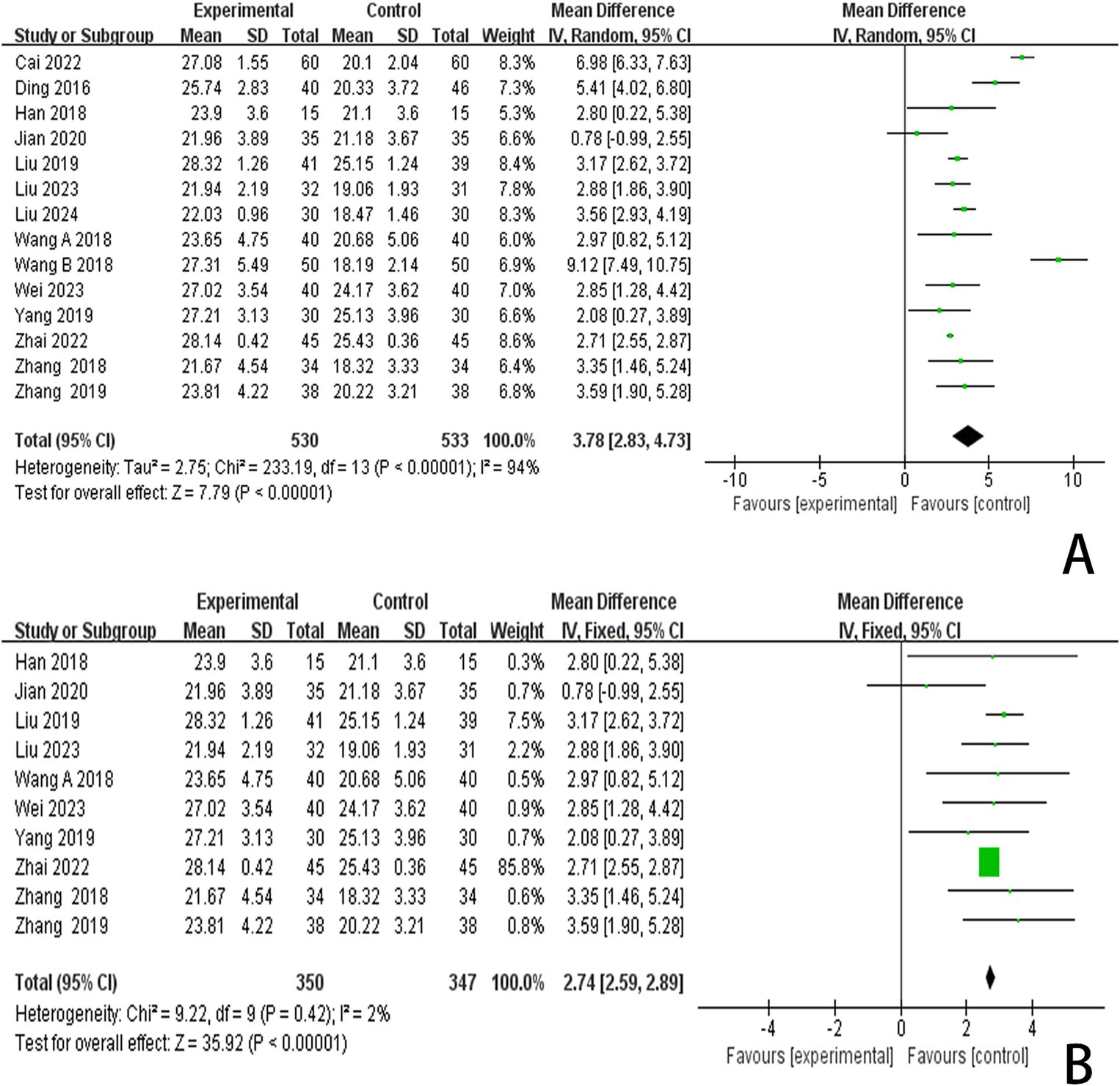
Figure 6. (A) Forest plots of the MMSE scores. (B) Forest plots of the MMSE scores after removing four studies.
3.4.4 The LOTCA scores
Six studies reported LOTCA scores and a random effects model was employed to conduct a meta-analysis of the data from each study. The results indicated that combined scalp acupuncture treatment significantly improves the LOTCA scores of PSCI patients compared to the control group (MD = 9.70, 95% CI: 7.72–11.69, I2 = 57%, 6 studies, 368 participants) (Figure 7A), with moderate heterogeneity observed between the studies.
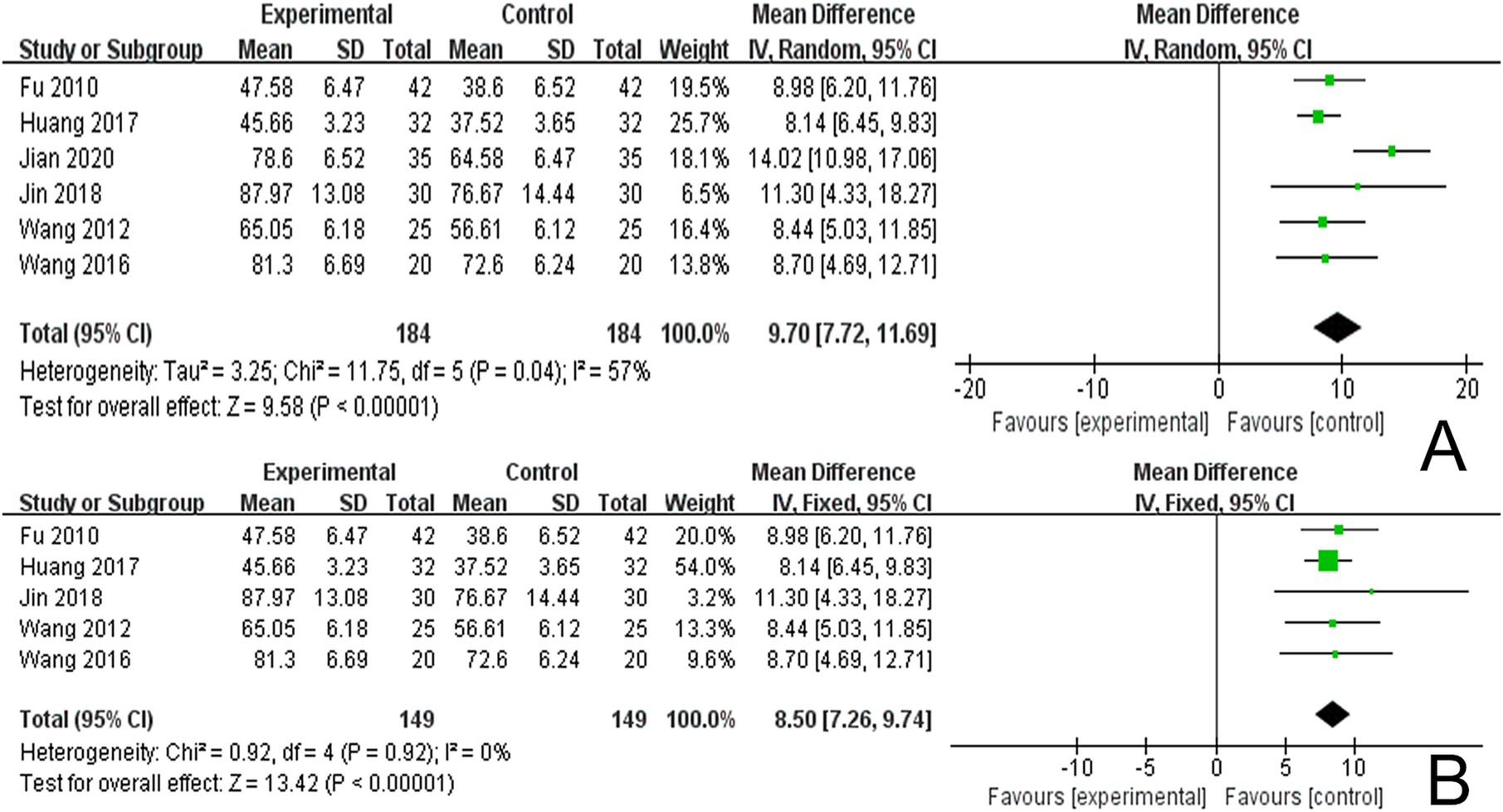
Figure 7. (A) Forest plots of the LOTCA scores. (B) Forest plots of the LOTCA scores after removing one study.
3.4.5 The P300 scores
In reviewing the 28 studies included in this analysis, 5 reported P300 latency, while 4 studies reported P300 amplitude. We employed a random effects model to meta-analyze the latency results and found that scalp acupuncture combined with treatment significantly reduced P300 latency in patients with PSCI compared to the control group (MD = −21.83, 95% CI: −26.31 to −17.35, I2 = 55%, 5 studies, 422 participants) (Figure 8A). Additionally, a meta-analysis of the 4 studies reporting P300 amplitude, utilizing a fixed effects model, indicated that scalp acupuncture combined with treatment could enhance P300 amplitude in PSCI patients relative to the control group (MD = 1.05, 95% CI: 0.76–1.34, I2 = 0%, 4 studies, 342 participants) (Figure 8B).
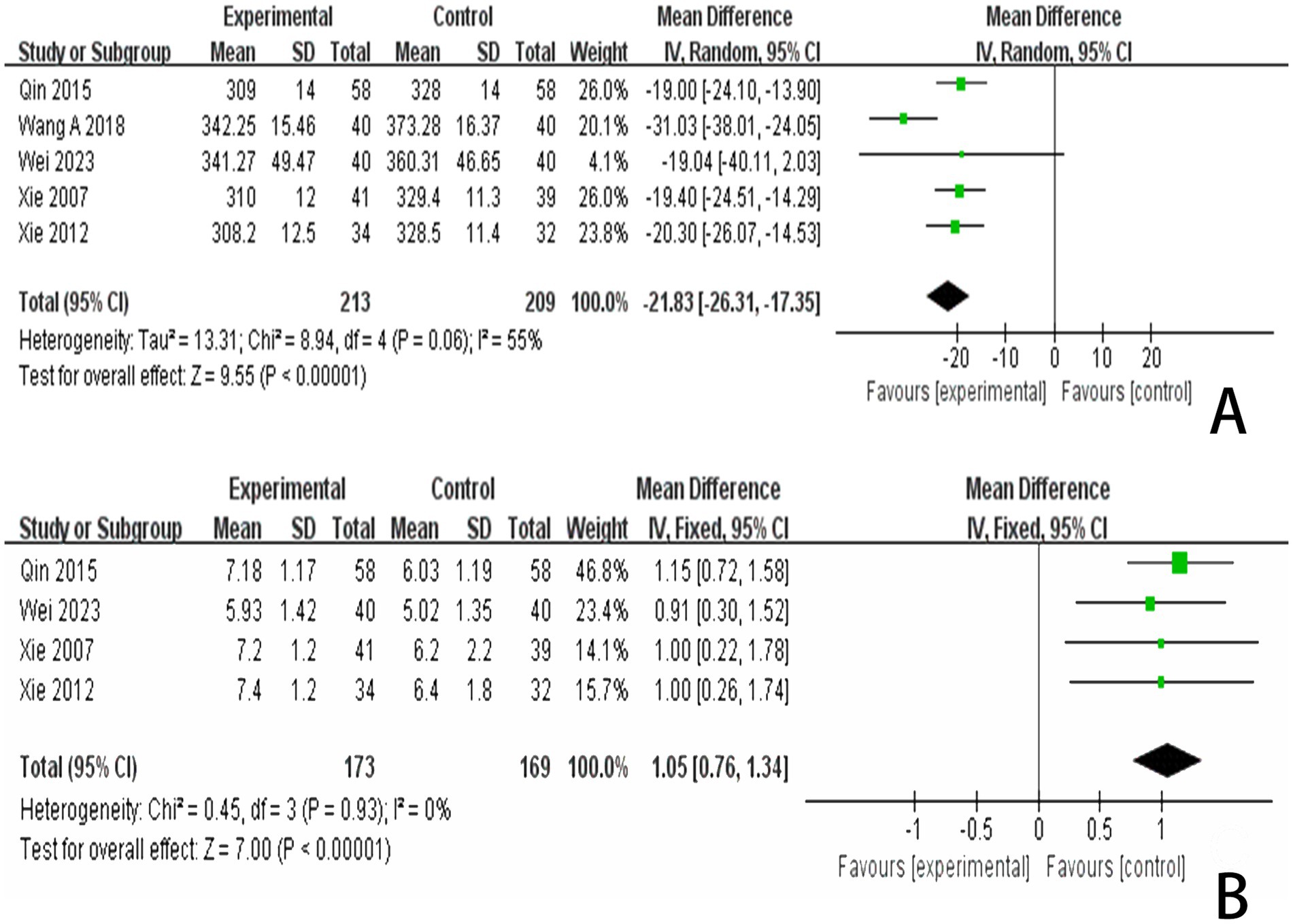
Figure 8. (A) Forest plots of the P300 latency. (B) Forest plots of the P300 latency after removing one study. (C) Forest plots of the P300 amplitude.
3.5 Subgroup analysis
3.5.1 Subgroup analysis of MoCA scores
We conducted a subgroup analysis of studies that recorded MoCA scores based on the type of treatment administered in the control group (Figure 9). The results indicated that the SA + CT vs. CT subgroup was significantly effective (MD = 4.12, 95% CI: 2.34–5.89, I2 = 89%, 2 studies, 140 participants). Similarly, the SA + R vs. R subgroup also demonstrated significant effectiveness (MD = 3.61, 95% CI: 2.25–4.97, I2 = 86%, 5 studies, 438 participants). The SA + H vs. H subgroup showed significant effectiveness as well (MD = 4.09, 95% CI: 0.55–7.62, I2 = 92%, 2 studies, 97 participants). In the comparison of SA + donepezil hydrochloride vs. donepezil hydrochloride, the results were significant (MD = 2.84, 95% CI: 0.38–5.30, I2 = 94%, 2 studies, 129 participants). Heterogeneity was considered high, as I2 > 75% in four subgroups, indicating that the results were less reliable. Additionally, the subgroup SA + rTMS vs. rTMS showed significant results (MD = 2.42, 95% CI: 1.21–3.63, Z = 3.94, p < 0.0001), and SA + CACT vs. CACT also yielded significant findings (MD = 3.14, 95% CI: 2.15–4.13, Z = 6.22, p < 0.00001), although there is only one study among the three subgroup analyses, the p < 0.05 for each study indicates that the efficacy is evident.
3.5.2 Subgroup analysis of MMSE scores
We further conducted a subgroup analysis of the 14 studies that recorded MMSE scores based on the type of treatment (Figure 10). The results indicated that the SA + CT vs. CT subgroup was significantly effective (MD = 1.95, 95% CI: 0.11–3.80, I2 = 78%, 2 studies, 160 participants). Similarly, the SA + R vs. R subgroup demonstrated significant effectiveness (MD = 4.96, 95% CI: 3.27–6.65, I2 = 94%, 7 studies, 602 participants). The SA + rTMS vs. rTMS subgroup also showed significant effectiveness (MD = 3.15, 95% CI: 2.62–3.69, I2 = 0%, 2 studies, 110 participants). Notably, the I2 was >75% in the SA + CT vs. CT and SA + R vs. R subgroups, suggesting high heterogeneity, which may compromise the reliability of these results. In contrast, the SA + rTMS vs. rTMS subgroup analysis, with an I2 = 0% (less than 50%), indicates low heterogeneity, suggesting that scalp acupuncture combined with rTMS treatment is more effective than rTMS alone in treating PSCI, rendering these results highly reliable. Furthermore, in the comparison of SA + donepezil hydrochloride vs. donepezil hydrochloride (MD = 2.88, 95% CI: 1.86–3.90, Z = 5.54, p < 0.00001), SA + H vs. H (MD = 2.08, 95% CI: 0.27–3.89, Z = 2.26, p < 0.02), SA + idebenone vs. idebenone (MD = 3.59, 95% CI: 1.90–5.28, Z = 4.17, p < 0.0001), there is only one study for each of the three subgroup analyses. Nonetheless, the p-values of each study were less than 0.05, indicating that the efficacy was evident.
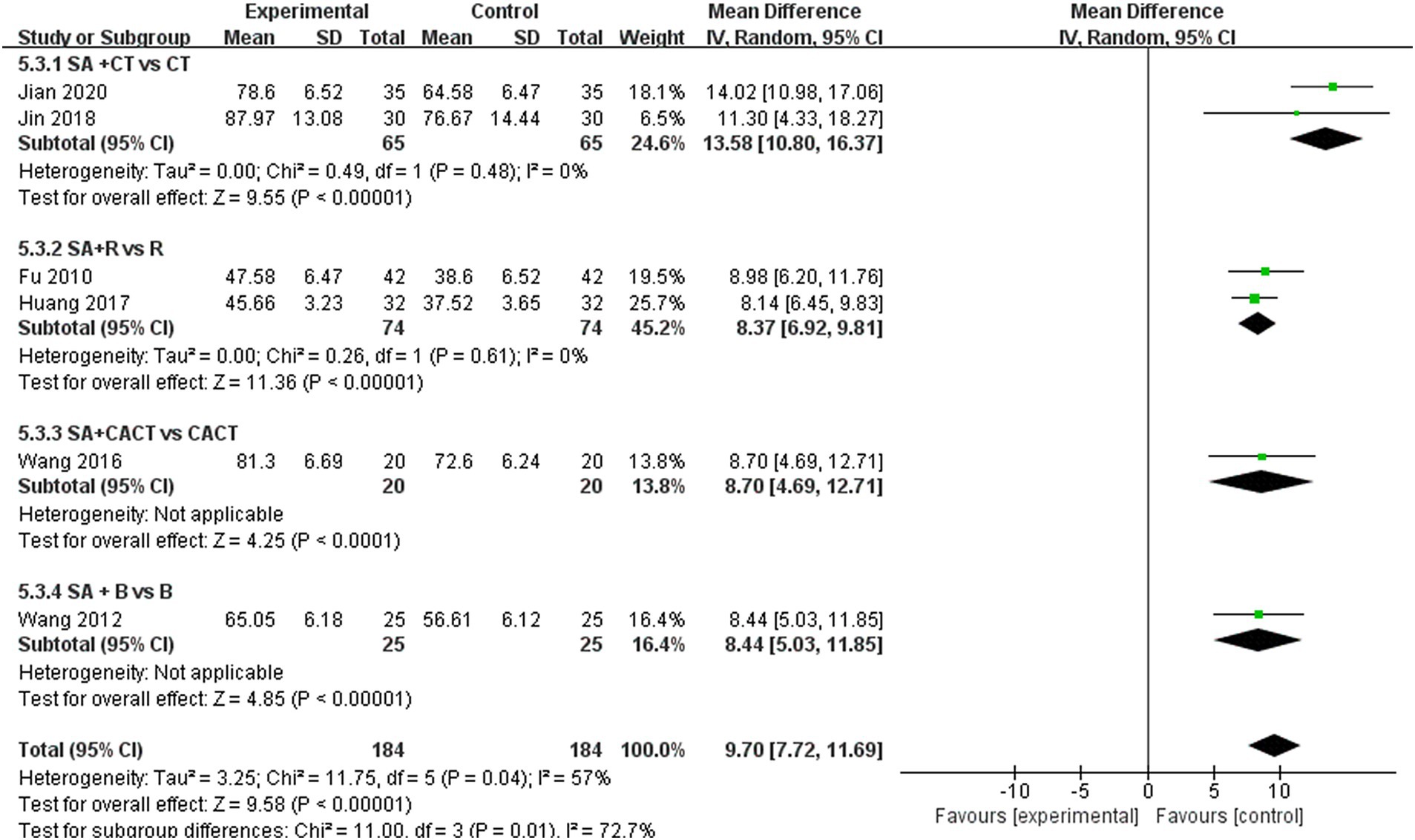
3.5.3 Subgroup analysis of LOTCA scores
We further conducted a subgroup analysis on the six studies that recorded LOTCA scores based on the type of treatment administered in the control group (Figure 11). The results indicated that the subgroup comparison of SA + CT vs. CT was significantly effective (MD = 13.58, 95% CI: 10.08–16.37, I2 = 0%, 2 studies, 130 participants). Similarly, the subgroup comparison of SA + R vs. R demonstrated significant effectiveness (MD = 8.37, 95% CI: 6.92–9.81, I2 = 0%, 2 studies, 148 participants). Since I2 = 0 < 50%, heterogeneity is considered low, suggesting that the results are reliable. Additionally, the comparison of SA + CACT vs. CACT (MD = 8.70, 95% CI: 4.69–12.71, Z = 4.25, p < 0.0001), SA + B vs. B (MD = 8.44, 95% CI: 5.03–11.85, Z = 4.85, p < 0.00001) Although each of the two subgroup analyses includes only one study, the p < 0.05 for each indicate that the efficacy is evident.
3.6 Publication bias and sensitive estimate
An analysis of 13 studies documenting MoCA scores revealed that the funnel plot exhibited asymmetry, with 5 studies falling outside the 95% CI (Figure 12A). After excluding these 5 studies (Wang et al., 2017; Mao and Cheng, 2019; Chen A. Z. et al., 2020; Chen J. et al., 2020; Liu et al., 2024), we observed that I2 = 19 < 50%, indicating that the reliability of scalp acupuncture in improving cognitive dysfunction post-stroke is supported (MD = 3.25, 95% CI: 2.99–3.52, I2 = 19%, 8 studies, 643 participants) (Figure 5B). Nonetheless, the funnel plot still displayed slight asymmetry (Figure 12B). In the analysis of 14 studies that recorded MMSE scores, the funnel plot also showed asymmetry, with 4 studies falling outside the 95% CI (Figure 12C). Upon excluding these 4 studies (Ding and Zhang, 2016; Wang W. et al., 2018; Cai et al., 2022; Liu et al., 2024) (MD = 2.74, 95% CI: 2.59–2.89, I2 = 2%, 10 studies, 697 participants), we found that I2 = 2% < 50% (Figure 6B). At the same time, the funnel plot exhibited slight asymmetry (Figure 12D). Additionally, the analysis of 6 studies that recorded LOTCA scores indicated that the funnel plot was asymmetric, with 1 study falling outside the 95% CI (Figure 12E). After excluding this 1 study (Xiong et al., 2020) (MD = 8.50, 95% CI: 7.26–9.74, I2 = 0%, 5 studies, 298 participants), we determined that I2 = 0% < 50 (Figure 7B) and the funnel plot showed slight asymmetry (Figure 12F). A consistent conclusion was reached through the analysis of studies recording both MMSE and LOTCA scores.
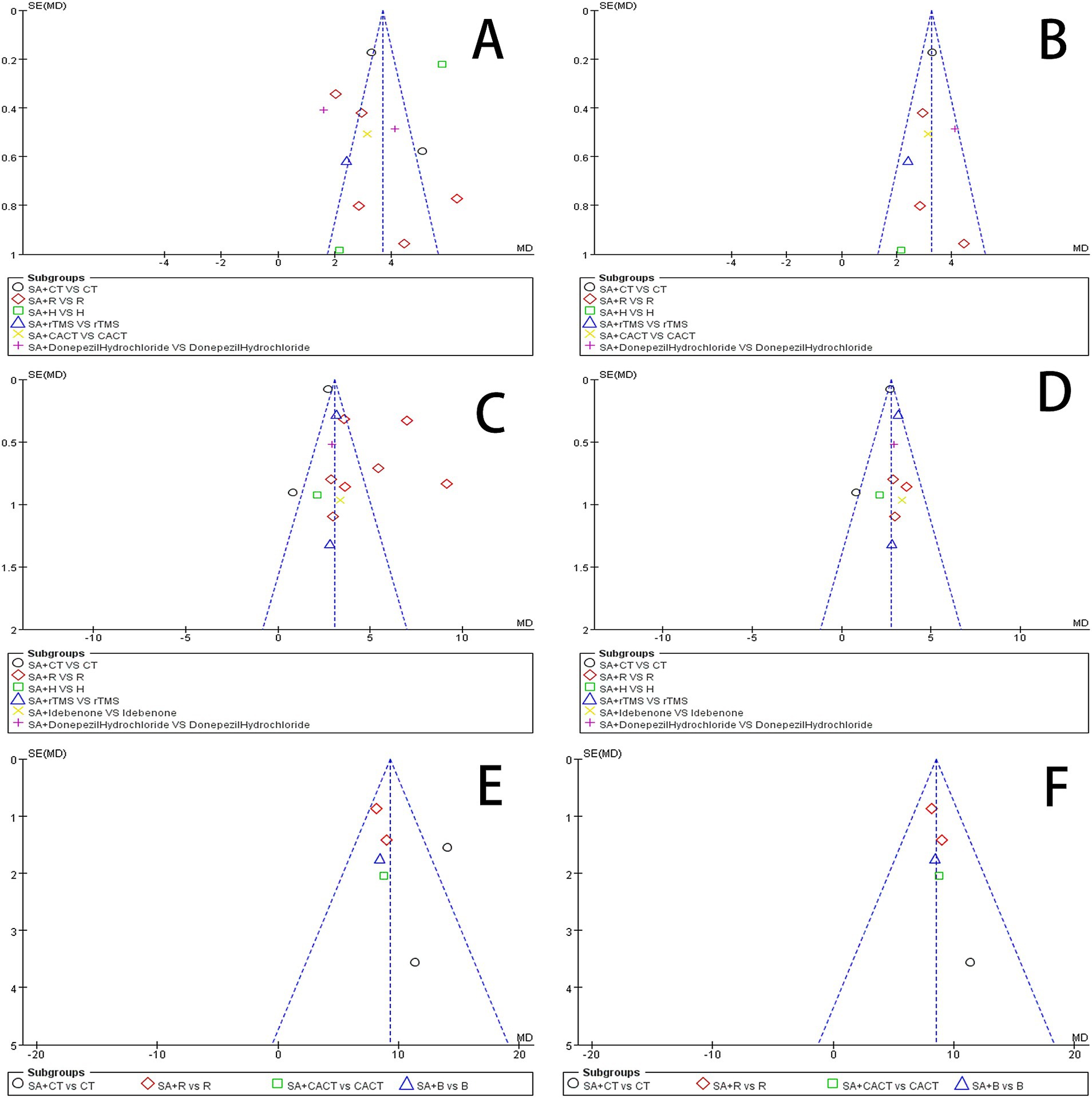
Figure 12. (A) Funnel plot of the MoCA scores. (B) Funnel plot of the MoCA scores after removing four studies. (C) Funnel plot of the MMSE scores. (D) Funnel plot of the MoCA scores after removing one from four studies. (E) Funnel plot of the LOTCA scores. (F) Funnel plot of the MoCA scores after removing one study.
Begg’s test and Egger’s test can detect the symmetry of the funnel plot to determine whether there is publication bias (Jin et al., 2015). The results of the Begg and Egger bias tests are presented in Table 3. The Egger bias tests for the prevalence of MoCA (p = 0.6590), MMSE (p = 0.1790), LOTCA (p = 0.4350), P300 latency (p = 0.7300), and P300 amplitude (p = 0.2590) indicated the absence of publication bias. However, the Egger bias test regarding the incidence rate of effective rate (p = 0.0100 < 0.05) revealed the presence of publication bias.

Table 3. Beeg test and Egger test for publication bias of outcome indicators reported in this study.
3.7 Adverse events
One study (Liu Y. F. et al., 2023) observed that some patients did not adhere to the prescribed treatment and subsequently dropped out. The remaining 27 studies (Xie et al., 2007; Fu et al., 2010; Wang et al., 2012; Xie et al., 2012; Qin, 2015; Ding and Zhang, 2016; Wang, 2016; Huang et al., 2017; Wang et al., 2017; Du et al., 2018; Han et al., 2018; Wang W. et al., 2018; Wang Y. X. et al., 2018; Zhang and An, 2018; Yang L. et al., 2019; Liu et al., 2019; Mao and Cheng, 2019; Zhang et al., 2019; Chen A. Z. et al., 2020; Chen J. et al., 2020; Xiong et al., 2020; Zhang et al., 2020; Cai et al., 2022; Zhai et al., 2022; Li and Pan, 2023; Wei et al., 2023; Liu et al., 2024) did not report any adverse events. Consequently, we were unable to assess the safety of scalp acupuncture in the treatment of PSCI, which raises concerns about a potential risk of reporting bias.
4 Discussion
4.1 Main findings
The study encompassed 28 randomized controlled trials involving a total of 1,995 participants. It evaluated the efficacy of combined scalp acupuncture in treating PSCI by examining multiple outcome indicators, including the MoCA, MMSE, and LOTCA scale scores, as well as P300 latency and amplitude. The findings indicate that the combination of scalp acupuncture with CT, CACT, R, H, and rTMS is more effective than any single treatment modality. Notably, the evidence supporting the effectiveness of scalp acupuncture combined with R in improving P300 latency and amplitude in PSCI patients is considered reliable. Furthermore, there is moderate to high heterogeneity among the studies regarding MoCA, MMSE, and LOTCA scores, along with a moderate to high risk of bias. All included studies focused on the application of scalp acupuncture for patients in the acute stroke phase. Thus, this study concludes that combined scalp acupuncture is more effective in addressing cognitive impairment following acute stroke compared to individual therapies such as CT, CACT, R, H, and rTMS.
Subgroup analyses of studies examining the MoCA and MMSE scores across various intervention approaches revealed a consistent association with moderate to high risk. In contrast, studies focusing on LOTCA scores exhibited lower risks, suggesting that the findings from the subgroup analyses comparing SA + CT versus CT, SA + R versus R, SA + CACT, and SA + donepezil hydrochloride were reliable.
In the context of the scalp acupuncture treatment regimens examined in the studies included in this analysis, the majority utilized the International SA method, with the additional incorporation of Yu SA and Fang SA. The most frequently employed acupoints are the mid-frontal line (MS1), mid-parietal line (MS5), anterior parietotemporal oblique line (MS6), posterior parietotemporal oblique line (MS7), anterior temporal line (MS10), and posterior temporal line (MS11). Other notable acupoints include the Baihui point (DU20), Sishencong point (EX-HN1), Qianding (GV21), and Shenting (GV24). This suggests that SA treatment primarily targets the frontal, temporal, and parietal regions, which correspond to the frontal lobes, temporal lobes, and parietal lobes—areas closely associated with the brain’s learning, memory, executive functions, and visuospatial/structural abilities. However, the underlying mechanisms of action remain to be elucidated in future studies. The most common treatment duration is 30 min per session, with a typical operational frequency of 200 sessions per minute. This clinical treatment protocol may serve as a guide for future clinical applications.
Resting-state functional magnetic resonance imaging (resting-state fMRI) is a technology employed to investigate the treatment mechanisms of PSCI, observing changes in brain function by analyzing changes in resting blood oxygen level signals. This technology primarily evaluates three indicators: amplitude of low-frequency fluctuations (ALFF), regional homogeneity (ReHo), and functional connectivity (Zhang et al., 2021). Studies have confirmed that scalp acupuncture treatment can enhance ALFF values in various regions of the brain, including the hippocampus, cingulate gyrus, splenium cortex, right inferior temporal gyrus, left middle occipital gyrus, left superior occipital gyrus, right superior parietal gyrus, prelimbic cortex, and sensory cortex (Wen et al., 2018; Han et al., 2024). The effectiveness of this treatment is associated with an increase in spontaneous neuronal activity in these areas (Han et al., 2024), which may facilitate the recovery of overall cognitive function, executive abilities, attention, and speech expression. ReHo is a technique utilized for processing local brain functional activity data, with its values closely linked to cognitive functions (Veselinovic et al., 2022). Following PSCI, alterations in functional brain activity are observed. Research indicates that scalp acupuncture can positively influence ReHo values in the brain regions of PSCI patients, particularly in the superior parietal gyrus, right inferior frontal gyrus, right inferior temporal gyrus, precuneus, lentiform nucleus, ventrolateral nucleus of the thalamus, and middle temporal gyrus. Conversely, negative activation was noted in the lentiform nucleus, ventrolateral thalamic nucleus, middle temporal gyrus, and parahippocampal gyrus (Han et al., 2024). These findings indicate that scalp acupuncture treatment may enhance the regeneration and repair of synapses in nerve cells, thereby facilitating the recovery of brain regions associated with cognitive functions in patients with PSCI. Furthermore, PSCI can lead to abnormal functional connections within the brain’s cognitive-related networks, resulting in alterations to the brain’s information integration processes (Xiong et al., 2022). Studies have confirmed that scalp acupuncture can influence the topological properties of brain functional network nodes in patients with PSCI (Wang, 2021), modulating brain networks by increasing functional connectivity between brain regions related to cognitive activities (Tan et al., 2017) and thereby improving the cognitive function of patients to a certain extent.
Diffusion tensor imaging (DTI) is a non-invasive technique that visualizes brain white matter fiber tracts and detects changes in brain white matter microstructure in vivo (Zhu et al., 2019; Li X. T. et al., 2022). Following PSCI, abnormal alterations in white matter fiber tracts occur, with fractional anisotropy (FA) values in the frontal lobe, hippocampus, and corpus callosum typically decreasing. This reduction suggests that the white matter fibers in these regions may have sustained damage or degeneration, thereby impacting the brain’s information integration processes (Yin et al., 2019). Research has demonstrated that scalp acupuncture can enhance the blood supply to white matter tracts in the brain and facilitate the repair of white matter fiber damage, consequently improving cognitive function in PSCI patients (Sun and Zhang, 2020). Additionally, scalp acupuncture may stimulate the release of neurotransmitters and neuropeptides by enhancing cerebral blood circulation, which can slow neuronal apoptosis, activate neural pathways, and further enhance cognitive function (Zhou et al., 2020). Furthermore, scalp acupuncture can improve the metabolic levels of brain functional tissues (Zhang et al., 2020), increase blood circulation, and promote the release of neurotransmitters and neuropeptides, thereby contributing to the reduction of neuronal cell apoptosis, activation of brain neural pathways, and enhancement of cognitive function.
In terms of basic research, a substantial number of studies have demonstrated that scalp acupuncture can influence the expression of tumor necrosis factor-α (TNF-α), interleukin-1β (IL-1β), and other cytokines associated with the inflammatory response in rats with middle cerebral artery occlusion (MCAO) (Li et al., 2020). This effect is specifically characterized by the down-regulation of these cytokines’ expression levels. Concurrently, scalp acupuncture treatment has been shown to increase the expression of brain-derived neurotrophic factor (BDNF) (Zheng et al., 2020) and plasticity-related proteins such as postsynaptic density protein 95 (PSD-95) in the hippocampus (Li et al., 2020). Additionally, scalp acupuncture can enhance mitophagy and reduce apoptosis levels (Liu et al., 2021). Through these mechanisms, scalp acupuncture treatment contributes to mitigating the cascade effects following a stroke, improving neuronal deficits, and fostering the repair of motor, cognitive, speech, and other neuronal functions. Despite this, there is still a lack of more specific research on SA treatment of PICS that is different from other sequelae after stroke and cognitive function in the elderly.
In summary, the potential mechanisms by which scalp acupuncture may treat PSCI can be categorized into several key aspects: (1) it may increase spontaneous neuronal activity in brain regions associated with cognitive functions and enhance functional connectivity between these areas; (2) it may promote the regeneration of synapses and repair of nerve cells; (3) it could enhance blood supply to white matter tracts in the brain, improve overall blood circulation, stimulate the release of neurotransmitters and neuropeptides, while also slowing neuronal apoptosis and elevating the metabolic levels of functional brain tissues; (4) it may down-regulate levels of inflammation-related factors and promote the expression of BDNF and proteins associated with neuroplasticity in the hippocampus; and (5) it may downregulate apoptosis levels and increase mitophagy.
4.2 Characteristics of outcome indicators
Appropriate assistive tools are critical for the study of cognitive impairment following a stroke. Currently, commonly used cognitive function evaluation tools include MMSE, MoCA, Hasegawa Dementia Scale (HDS-R), the Oxford Cognitive Screening (OCS), and LOTCA (Wang and Dong et al., 2021; Li L. et al., 2022). This study utilized the most widely adopted assessment tools, specifically the MMSE and MoCA scores, as outcome measures. The MMSE is particularly sensitive to cognitive domains such as memory and language, especially in the context of left hemisphere stroke, and demonstrates high sensitivity and specificity for diagnosing dementia. However, its sensitivity to mild cognitive impairment is relatively low (Mancuso et al., 2018; Milosevich et al., 2024). In contrast, the MoCA compensates for this limitation, exhibiting higher sensitivity and specificity in identifying mild cognitive impairment. Both assessments are suitable for less educated individuals but may not be appropriate for patients with post-stroke aphasia or neglect (Mancuso et al., 2018; Milosevich et al., 2024). Conversely, the LOTCA is frequently employed in clinical settings to assess non-verbal cognitive dysfunction in patients with aphasia (Almomani et al., 2018). These considerations underscore the importance of addressing the limitations associated with the MMSE and MoCA scales.
Event-related potentials (ERPs) are specific types of electrical signals in the brain (Kayser and Tenke, 2015). Research has demonstrated a significant correlation between components of event-related potentials that peak at approximately 300 ms and cognitive function, making them a valuable tool for assessing cognitive performance in the brain (Tyson-Carr et al., 2018). P300 can reflect the brain’s memory, attention, and mental processing speed through variations in amplitudes and latencies (Morrison et al., 2019). Consequently, the P300 component offers a quantitative, objective, and non-invasive electrophysiological testing method for future research on cognitive impairment following a stroke.
4.3 Quality of the evidence
The randomized controlled trials analyzed in this study indicate that most items in the ROB2 assessment are categorized as low risk. However, several studies demonstrate unclear risks related to “participant and personnel blinding bias,” “allocation concealment procedures,” and “outcome assessment blinding bias,” which could potentially skew study results toward a positive outcome. Therefore, the principle of allocation concealment should be strictly adhered to in future trial design and implementation. Given the specific nature of scalp acupuncture treatment, it is not feasible to blind participants and operators, which diminishes the overall quality of the study. Furthermore, sensitivity analyses conducted during the meta-analysis revealed that 11 studies (Xie et al., 2012; Ding and Zhang, 2016; Wang et al., 2017; Wang W. et al., 2018; Wang Y. X. et al., 2018; Mao and Cheng, 2019; Chen A. Z. et al., 2020; Chen J. et al., 2020; Xiong et al., 2020; Cai et al., 2022; Liu et al., 2024) exhibited high heterogeneity. This heterogeneity may arise from imbalances between the control and experimental groups, unclear randomization methods, selective reporting, small sample sizes, and a lack of control over participants, possibly influenced by variations in cultural backgrounds. To address these issues, future studies should aim to increase sample sizes and the number of research centers, as well as assess the educational levels of subjects to enhance research quality. Consequently, the included studies were rated as being at high risk of implementation bias.
5 Limitation
This study has several limitations that merit discussion. First, due to the inherent nature of scalp acupuncture, neither the operator nor the subjects can be blinded. In many studies, the research design must delineate the randomization method; consequently, the quality of the included studies could have been enhanced. Second, during the meta-analysis, various factors contributed to high heterogeneity in specific outcomes. These factors include individual differences, varying treatment options (such as operator skill, the subject’s disease course, observation duration, and acupuncture point selection), stroke type (ischemic versus hemorrhagic), as well as the subject’s education level and degree of cognitive function impairment. Third, the general acceptance of scalp acupuncture treatment varies among individuals, and all studies included in this analysis were conducted in China, with limited engagement from scholars in other countries. This geographical limitation significantly undermines the reliability of the meta-analysis results. Finally, meta-analyses typically involve the aggregation of results from multiple trials, which increases the likelihood of random errors. Such errors can profoundly influence the outcomes of meta-analyses (Wetterslev et al., 2017). Therefore, future research should focus on strategies to mitigate the impact of random errors on the results of meta-analyses.
6 Conclusion
Although the sample size and methodological quality of the 28 randomized controlled trials included in this study were not entirely satisfactory, we observed changes in outcome indicators—specifically, the total effective rate, MMSE score, MoCA score, P300 latency and amplitude, and LOTCA score—before and after treatment, suggesting that scalp acupuncture can improve PSCI. Furthermore, due to the high risk of bias (ROB) in the included trials and the very low quality of the evidence for assessing outcomes, the results of this study should be interpreted with caution. Future clinical research should employ high-quality randomized double-blind controlled trial designs, utilize multi-center studies with large sample sizes, conduct long-term efficacy evaluations, and apply scientifically sound methods. Additionally, the procedures for scalp acupuncture should be standardized and unified.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
SL: Writing – original draft, Writing – review & editing, Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization. AD: Writing – original draft, Writing – review & editing, Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization. YZ: Writing – original draft, Writing – review & editing, Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization. XC: Writing – original draft, Writing – review & editing, Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Supervision. YC: Investigation, Methodology, Software, Supervision, Writing – original draft, Writing – review & editing, Conceptualization, Data curation, Formal analysis. LZ: Writing – original draft, Writing – review & editing, Conceptualization, Data curation, Investigation, Methodology, Project administration, Software, Validation, Visualization. XY: Writing – original draft, Writing – review & editing, Conceptualization, Data curation, Investigation, Methodology, Project administration, Resources, Software, Validation. MY: Writing – original draft, Writing – review & editing, Conceptualization, Data curation, Formal analysis, Investigation, Project administration, Software, Validation. JS: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. YQ: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study received funding from National Natural Science Foundation of China, No. 81760893, JS; Fundamental Research Key Project of Yunnan Science and Technology Department, 202101AZ070001-165, JS. The Special Project for Famous Doctors of “Xingdian Talent Support Program” in Yunnan Province, JS.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer CW declared a shared affiliation with the author YZ to the handling editor at the time of review.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnins.2024.1468331/full#supplementary-material
Abbreviations
WHO, World Health Organization; PSCI, Post-stroke cognitive impairment; MoCA, Montreal Cognitive Assessment; MMSE, Mini-Mental State Examination Scale; LOTCA, Loewenstein Occupational Therapy Cognitive Assessment; CFT, Cognitive function training; CaMKIV, Calmodulin-dependent protein kinase type IV; CREB, Cyclic adenosine monophosphate response element binding protein; HDS-R, Hasegama’s Dementia Scale; OCS, Oxford Cognitive Screen; ERP, Event-related potentials; RCT, Randomized controlled trials; R, Rehabilitation therapy; CACT, Computer-assisted cognitive training; H, Hyperbaric oxygen therapy; rTMS, Repetitive transcranial magnetic stimulation; CT, Cognitive training; Resting-state fMRI, Resting-state functional magnetic resonance imaging; ALFF, Amplitude of low-frequency fluctuation; ReHo, Regional homogeneity; DTI, Diffusion tensor imaging; IL-1β, Interleukin-1β.
References
Almomani, F., Avi-Itzhak, T., Demeter, N., Josman, N., and Al-Momani, M. O. (2018). Construct validity and internal consistency reliability of the Loewenstein Occupational Therapy Cognitive Assessment (LOTCA). BMC Psychiatry 18:184. doi: 10.1186/s12888-018-1776-x
Bao, X., Li, L., Liu, H., Shi, H. F., Xu, S., Wang, M. H., et al. (2021). Effect of acupuncture combined with rehabilitation on cognitive and motor functions in poststroke patients. Anat. Rec. 304, 2531–2537. doi: 10.1002/ar.24700
Cai, C., Sun, Q. F., and Ge, J. H. (2022). The application effect of occupational therapy combined with scalp acupuncture in the rehabilitation of patients with cognitive impairment after stroke. Chronic Pathematol. J. 23, 579–582. doi: 10.16440/J.CNKI.1674-8166.2022.04.25
Chang, W. H., Park, Y. H., Ohn, S. H., Park, C. H., Lee, P. K., and Kim, Y. H. (2011). Neural correlates of donepezil-induced cognitive improvement in patients with right hemisphere stroke: a pilot study. Neuropsychol. Rehabil. 21, 502–514. doi: 10.1080/09602011.2011.582708
Chen, J., Li, H., Zeng, C., Li, J., and Zhao, B. (2020). Evaluation of the recovery outcome of poststroke cognitive impairment after cluster needling of scalp acupuncture therapy based on functional near-infrared spectroscopy. Brain Behav. 10:e01731. doi: 10.1002/brb3.1731
Chen, A. Z., Lin, Z. C., and Lan, L. (2020). Effects of long-term scalp acupuncture combined with cognitive rehabilitation training platform on cognitive function after stroke. Chin. Manipul. Rehabil. Med. 11, 22–23. doi: 10.19787/j.issn.1008-1879.2020.06.009
Ding, X., and Zhang, H. (2016). Effect of scalp acupuncture combined with motor relearning on cognitive impairment in post-stroke patients. Hebei J. Tradit. Chin. Med. 38, 586–588. doi: 10.3969/j.issn.1002-2619.2016.04.033
Du, J., Yin, J., Liu, L., Chen, J., and He, M. (2018). Clinical observation of 60 cases of treating cognitive disorder after cerebral injury in combination with scalp acupuncture and cognitive training. Medicine 97:e12420. doi: 10.1097/MD.0000000000012420
Feigin, V. L., Brainin, M., Norrving, B., Martins, S., Sacco, R. L., Hacke, W., et al. (2022). World Stroke Organization (WSO): global stroke fact sheet 2022. Int. J. Stroke 17, 18–29. doi: 10.1177/17474930211065917
Feng, X., Yang, S., Liu, J., Huang, J., Peng, J., Lin, J., et al. (2013). Electroacupuncture ameliorates cognitive impairment through inhibition of NF-kappaB-mediated neuronal cell apoptosis in cerebral ischemia-reperfusion injured rats. Mol. Med. Rep. 7, 1516–1522. doi: 10.3892/mmr.2013.1392
Fu, J. M., Gu, X. D., Yao, Y. H., Wang, J., Li, L., Gu, M., et al. (2010). Effects of scalp acupuncture and long-term needle retention combined with rehabilitation training on the quality of life of patients with cognitive impairment after stroke. Chin. Arch. Tradit. Chin. Med. 28, 796–798. doi: 10.13193/j.archtcm.2010.04.126.fujm.071
Han, S. W., Cao, D. N., Li, X. L., Wang, Y., Zhang, Q. H., Yue, J. H., et al. (2024). Progress in multimodal fMRI research on scalp acupuncture for treating post-stroke cognitive impairment. Chin. Imaging J. Integr. Tradit. West. Med. 22, 41–44. doi: 10.3969/j.issn.1672-0512.2024.01.009
Han, C. Y., Wen, W. S., and Ye, X. M. (2018). Observation on the efficacy of scalp acupuncture combined with repetitive transcranial magnetic stimulation in the treatment of post-stroke cognitive dysfunction. Mod. Chin. Doct. 56, 88–92.
Huang, J. H., Fu, J. M., Ye, J. R., and Zhang, L. J. (2017). Observation on the efficacy of scalp acupuncture for long-term needle retention in the treatment of cognitive impairment and ADL defects in community-based stroke patients. J. Emerg. Tradit. Chin. Med. 8, 15–17.
Jin, Z. C., Zhou, X. H., and He, J. (2015). Statistical methods for dealing with publication bias in meta-analysis. Stat. Med. 34, 343–360. doi: 10.1002/sim.6342
Kayser, J., and Tenke, C. E. (2015). Issues and considerations for using the scalp surface Laplacian in EEG/ERP research: a tutorial review. Int. J. Psychophysiol. 97, 189–209. doi: 10.1016/j.ijpsycho.2015.04.012
Levine, D. A., Galecki, A. T., Langa, K. M., Unverzagt, F. W., Kabeto, M. U., Giordani, B., et al. (2015). Trajectory of cognitive decline after incident stroke. JAMA 314, 41–51. doi: 10.1001/jama.2015.6968
Li, Y., Cui, R., Liu, S., Qin, Z., Sun, W., Cheng, Y., et al. (2023). The efficacy and safety of post-stroke cognitive impairment therapies: an umbrella review. Front. Pharmacol. 14:1207075. doi: 10.3389/fphar.2023.1207075
Li, Z., Meng, X., Ren, M., and Shao, M. (2020). Combination of scalp acupuncture with exercise therapy effectively counteracts ischemic brain injury in rats. J. Stroke Cerebrovasc. Dis. 29:105286. doi: 10.1016/j.jstrokecerebrovasdis.2020.105286
Li, L. D., and Pan, J. (2023). Clinical effect of Lingnan scalp acupuncture combined with cognitive training in the treatment of mild cognitive impairment after stroke. Chin. J. Gerontol. 43, 2073–2076. doi: 10.3969/j.issn.1005-9202.2023.09.008
Li, X. T., Wang, K., and Ai, L. (2022). A preliminary study on the diagnosis and differential diagnosis of MCI using diffusion tensor imaging and 18F-AV1451 PET tau protein brain imaging. Chin. J. Magn. Reson. Imaging 13, 5–14. doi: 10.12015/issn.1674-8034.2022.04.002
Li, L., Yang, L., Luo, B., Deng, L., Zhong, Y., Gan, D., et al. (2022). Acupuncture for post-stroke cognitive impairment: an overview of systematic reviews. Int. J. Gen. Med. 15, 7249–7264. doi: 10.2147/IJGM.S376759
Li, M., Yao, L., Lu, Z., Yang, L., and Fan, H. (2023). Preliminary MRS study of critical values of relevant brain metabolites in elderly Chinese patients with post-stroke cognitive impairment. IBRO Neurosci. Rep. 15, 287–292. doi: 10.1016/j.ibneur.2023.10.002
Liu, P., Lu, X. Y., Wang, H., Lu, W., and Hu, C. (2024). Robot-assisted virtual scenario training combined with scalp acupuncture can relieve cognitive impairment among stroke survivors. Chin. J. Phys. Med. Rehabil. 46, 242–246. doi: 10.3760/cma.j.issn.0254-1424.2024.03.010
Liu, Y. F., Mao, H. L., Liu, Y. Y., Wang, Z. M., and An, J. M. (2023). Observation on the efficacy of scalp acupuncture combined with drugs in the treatment of cognitive dysfunction after ischemic stroke. Shanghai J. Acupunct. Moxibustion 42, 331–335. doi: 10.13460/j.issn.1005-0957.2023.04.0331
Liu, L., Xia, W. G., and Xu, T. (2019). Clinical observation on scalp acupuncture combined with repetitive transcranial magnetic stimulation in the treatment of cognitive dysfunction after cerebral infarction. Chin. J. Rehabil. 34, 123–126. doi: 10.3870/zgkf.2019.03.003
Liu, P., Yu, X., Dai, X., Zou, W., Yu, X., Niu, M., et al. (2021). Scalp acupuncture attenuates brain damage after intracerebral hemorrhage through enhanced mitophagy and reduced apoptosis in rats. Front. Aging Neurosci. 13:718631. doi: 10.3389/fnagi.2021.718631
Liu, Y., Zhao, L., Chen, F., Li, X., Han, J., Sun, X., et al. (2023). Comparative efficacy and safety of multiple acupuncture therapies for post stroke cognitive impairment: a network meta-analysis of randomized controlled trials. Front. Neurol. 14:1218095. doi: 10.3389/fneur.2023.1218095
Mancuso, M., Demeyere, N., Abbruzzese, L., Damora, A., Varalta, V., Pirrotta, F., et al. (2018). Using the Oxford cognitive screen to detect cognitive impairment in stroke patients: a comparison with the mini-mental state examination. Front. Neurol. 9:101. doi: 10.3389/fneur.2018.00101
Mao, C. X., and Cheng, F. N. (2019). Scalp acupuncture combined with modern rehabilitation training to treat 39 cases of post-stroke cognitive impairment. Tradit. Chin. Med. Res. 32, 47–49. doi: 10.3969/j.issn.1001-6910.2019.10.21
Marucci, G., Buccioni, M., Ben, D. D., Lambertucci, C., Volpini, R., and Amenta, F. (2021). Efficacy of acetylcholinesterase inhibitors in Alzheimer’s disease. Neuropharmacology 190:108352. doi: 10.1016/j.neuropharm.2020.108352
Milosevich, E. T., Moore, M. J., Pendlebury, S. T., and Demeyere, N. (2024). Domain-specific cognitive impairment 6 months after stroke: the value of early cognitive screening. Int. J. Stroke 19, 331–341. doi: 10.1177/17474930231205787
Morrison, C., Rabipour, S., Taler, V., Sheppard, C., and Knoefel, F. (2019). Visual event-related potentials in mild cognitive impairment and Alzheimer’s disease: a literature review. Curr. Alzheimer Res. 16, 67–89. doi: 10.2174/1567205015666181022101036
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., et al. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. doi: 10.1136/bmj.n71
Qin, D. (2015). Effects of scalp on motor function and cognitive function in patients recovering from stroke. Chin. J. Gerontol. 35, 5161–5163. doi: 10.3969/j.issn.1005-9202.2015.18.054
Rao, M. G., Holla, B., Varambally, S., Raveendranathan, D., Venkatasubramanian, G., and Gangadhar, B. N. (2013). Piracetam treatment in patients with cognitive impairment. Gen. Hosp. Psychiatry 35, 451.e5–451.e6. doi: 10.1016/j.genhosppsych.2012.05.009
Sun, G. C., and Zhang, W. Z. (2020). Predictive value of DTI brain network analysis for early post-stroke cognitive impairment. J. Int. Psychiatry 47, 972–975. doi: 10.13479/j.cnki.jip.2020.05.033
Tan, T. T., Wang, D., Huang, J. K., Zhou, X. M., Yuan, X., Liang, J. P., et al. (2017). Modulatory effects of acupuncture on brain networks in mild cognitive impairment patients. Neural Regen. Res. 12, 250–258. doi: 10.4103/1673-5374.200808
Tyson-Carr, J., Kokmotou, K., Soto, V., Cook, S., Fallon, N., Giesbrecht, T., et al. (2018). Neural correlates of economic value and valuation context: an event-related potential study. J. Neurophysiol. 119, 1924–1933. doi: 10.1152/jn.00524.2017
Veselinovic, T., Rajkumar, R., Amort, L., Junger, J., Shah, N. J., Fimm, B., et al. (2022). Connectivity patterns in the core resting-state networks and their influence on cognition. Brain Connect. 12, 334–347. doi: 10.1089/brain.2020.0943
Wang, J. (2016). Effects of scalp acupuncture combined with computer-assisted cognitive training with background music on cognitive impairment in stroke. Chin. J. Rehabil. 31, 128–130. doi: 10.3870/zgkf.2016.02.015
Wang, R. (2021). Study on the brain functional network of patients with post-stroke cognitive dysfunction treated with acupuncture. Kawakita Medical College. doi: 10.27755/d.cnki.gcbyx.2021.000035
Wang, K., and Dong, Q. (2021). Expert consensus on the management of cognitive impairment after stroke 2021. Chin. J. Stroke 16, 376–389. doi: 10.3969/j.issn.1673-5765.2021.04.011
Wang, W., Fu, J. M., Gu, X. D., Li, Y., Chen, Y. C., and Jin, M. M. (2012). Observation on the efficacy of scalp acupuncture extraction method combined with cognitive training on the cognitive function of stroke patients during recovery period. Chin. Arch. Tradit. Chin. Med. 30, 2578–2580. doi: 10.13193/j.archtcm.2012.11.212.wangw.008
Wang, L. T., Jang, Y. M., Cong, Y., Wang, J., Shen, X. Y., and Yang, Y. C. (2017). Effects of scalp acupuncture combined with hyperbaric oxygen chamber therapy on cognitive function in patients recovering from cerebral infarction. Mod. J. Integr. Tradit. Chi. West. Med. 26, 3829–3831. doi: 10.3969/j.issn.1008-8849.2017.34.021
Wang, W., Lu, X. Y., Zhu, L. S., Zhang, P., Wei, D. Q., and Zhou, G. (2018). Effects of early scalp acupuncture and long-term needle retention combined with rehabilitation training on cognitive dysfunction in stroke patients. J. New Chin. Med. 50, 164–167. doi: 10.13457/j.cnki.jncm.2018.03.044
Wang, Y. X., Miao, W., Zhang, H. S., Wang, L. C., Liu, J., Ma, X., et al. (2018). Effect of head acupuncture combined with cognitive rehabilitation on cognitive impairment after cerebral infarction. Guiding J. Tradit. Chin. Med. Pharm. 24, 84–86.
Wei, B. X., Liu, G. C., and Zeng, J. Y. (2023). Clinical observation on scalp acupuncture combined with cognitive function training in the treatment of post-stroke cognitive impairment. J. Guangzhou Univ. Tradit. Chin. Med. 40, 368–374. doi: 10.13359/j.cnki.gzxbtcm.2023.02.016
Wen, T., Zhang, X., Liang, S., Li, Z., Xing, X., Liu, W., et al. (2018). Electroacupuncture ameliorates cognitive impairment and spontaneous low-frequency brain activity in rats with ischemic stroke. J. Stroke Cerebrovasc. Dis. 27, 2596–2605. doi: 10.1016/j.jstrokecerebrovasdis.2018.05.021
Wetterslev, J., Jakobsen, J. C., and Gluud, C. (2017). Trial sequential analysis in systematic reviews with meta-analysis. BMC Med. Res. Methodol. 17:39. doi: 10.1186/s12874-017-0315-7
Wu, W., Song, C., Yang, Y., Hu, Y., and Lin, H. (2024). Acupuncture for cognitive impairment after stroke: a systematic review and meta-analysis. Heliyon 10:e30522. doi: 10.1016/j.heliyon.2024.e30522
Xie, D. L., Zhu, L. F., Liu, H. Y., Chen, J. B., Zeng, C. Y., Wang, S. X., et al. (2007). Observation on the therapeutic effect of scalp therapy on cognitive and motor dysfunction in patients recovering from stroke. Chin. J. Rehabi. Theory Pract. 6, 542–543.
Xie, D. L., Zhu, L. F., Liu, H. Y., and Zeng, C. Y. (2012). Application of P300 in scalp acupuncture for cognitive disorder due to cerebral infarction. J. Acupunct. Tuina Sci. 10, 26–28. doi: 10.1007/s11726-012-0564-2
Xiong, Z. L., Li, D. X., Wang, R. P., Xiang, H., Yao, Y. R., and Xia, K. (2022). An fMRI study of functional connectivity changes in the default mode brain network during the progression of Alzheimer’s disease. Chin. Imaging J. Integr. Tradit. West. Med. 20, 107–111. doi: 10.3969/j.issn.1672-0512.2022.02.002
Xiong, J., Zhang, Z., Ma, Y., Li, Z., Zhou, F., Qiao, N., et al. (2020). The effect of combined scalp acupuncture and cognitive training in patients with stroke on cognitive and motor functions. NeuroRehabilitation 46, 75–82. doi: 10.3233/NRE-192942
Yang, L., Tan, J., and Chen, L. Z. (2019). Clinical observation on scalp acupuncture combined with hyperbaric oxygen in treating cognitive impairment after stroke. Guiding J. Tradit. Chin. Med. Pharm. 25, 36–38. doi: 10.13862/j.cnki.cn43-1446/r.2019.24.012
Yang, J. W., Wang, X. R., Ma, S. M., Yang, N. N., Li, Q. Q., and Liu, C. Z. (2019). Acupuncture attenuates cognitive impairment, oxidative stress and NF-kappaB activation in cerebral multi-infarct rats. Acupunct. Med. 37, 283–291. doi: 10.1136/acupmed-2017-011491
Yin, B., Li, D. D., Huang, H., Gu, C. H., Bai, G. H., Hu, L. X., et al. (2019). Longitudinal changes in diffusion tensor imaging following mild traumatic brain injury and correlation with outcome. Front. Neural Circuits 13:28. doi: 10.3389/fncir.2019.00028
Zhai, D., Duan, L. Z., and Wang, L. Q. (2022). Effect of scalp acupuncture combined with cognitive rehabilitation training on patients with mild cognitive impairment after stroke. Med. J. Chin. People’s Health 34, 75–77. doi: 10.3969/j.issn.1672-0369.2022.19.023
Zhang, X. Y., and An, J. M. (2018). Clinical efficacy of Fang’s scalp acupuncture combined with idebenone in the treatment of post-stroke cognitive impairment. Pract. J Card. Cereb. Pneumal Vasc. Dis. 26, 146–148. doi: 10.3969/j.issn.1008-5971.2018.04.040
Zhang, H. L., Che, W. S., and Chu, N. N. (2019). Effect of scalp acupuncture combined with virtual scenario interactive training on functional rehabilitation of stroke patients. Chin. J. Gerontol. 39, 4902–4906. doi: 10.3969/j.issn.1005-9202.2019.20.008
Zhang, J., Gui, Y., Leng, C., Li, Y., Zhou, R., Liu, W., et al. (2023). Electroacupuncture at “Baihui, Yintang and Shuigou” acupoints improves post-stroke cognitive impairment in mice. Stud. Health Technol. Inform. 308, 723–732. doi: 10.3233/SHTI230905
Zhang, Y., Lin, R., Tao, J., Wu, Y., Chen, B., Yu, K., et al. (2016). Electroacupuncture improves cognitive ability following cerebral ischemia reperfusion injury via CaM-CaMKIV-CREB signaling in the rat hippocampus. Exp. Ther. Med. 12, 777–782. doi: 10.3892/etm.2016.3428
Zhang, T., Wang, H., Li, Q., Huang, J., and Sun, X. (2014). Modulating autophagy affects neuroamyloidogenesis in an in vitro ischemic stroke model. Neuroscience 263, 130–137. doi: 10.1016/j.neuroscience.2014.01.012
Zhang, J. B., Wei, R. P., Yang, H., Shen, Y. X., and Zheng, J. (2020). Scalp acupuncture combined with computer-assisted training in the treatment of cognitive impairment after cerebral infarction in the elderly magnetic resonance spectroscopy imaging. Chin. J. Gerontol. 40, 4067–4070. doi: 10.3969/j.issn.1005-9202.2020.19.011
Zhang, X., Xue, C., Cao, X., Yuan, Q., Qi, W., Xu, W., et al. (2021). Altered patterns of amplitude of low-frequency fluctuations and fractional amplitude of low-frequency fluctuations between amnestic and vascular mild cognitive impairment: an ALE-based comparative meta-analysis. Front. Aging Neurosci. 13:711023. doi: 10.3389/fnagi.2021.711023
Zheng, Y., Qin, Z., Tsoi, B., Shen, J., and Zhang, Z. J. (2020). Electroacupuncture on trigeminal nerve-innervated acupoints ameliorates poststroke cognitive impairment in rats with middle cerebral artery occlusion: involvement of neuroprotection and synaptic plasticity. Neural Plast. 2020, 8818328–8818313. doi: 10.1155/2020/8818328
Zhou, X. L., Lou, M. W., Wu, W. L., Yuan, H. T., and Huang, J. H. (2020). Study on fMRI-based brain network node flexibility in patients with vascular cognitive impairment. Chin. J. Med. Imaging 30, 349–353.
Zhu, H., Deng, X., Luan, G., Zhang, Y., and Wu, Y. (2023). Comparison of efficacy of non-pharmacological intervention for post-stroke dysphagia: a systematic review and Bayesian network meta-analysis. BMC Neurosci. 24:53. doi: 10.1186/s12868-023-00825-0
Keywords: scalp acupuncture, stroke, cognitive impairment, meta-analysis, randomized controlled trials
Citation: Li S, Dai A, Zhou Y, Chen X, Chen Y, Zhou L, Yang X, Yue M, Shi J and Qiu Y (2024) Efficacy of combination scalp acupuncture for post-stroke cognitive impairment: a systematic review and meta-analysis. Front. Neurosci. 18:1468331. doi: 10.3389/fnins.2024.1468331
Edited by:
Cancheng Li, Beihang University, ChinaReviewed by:
Chaojie Wang, Heilongjiang University of Chinese Medicine, ChinaShaobo Lv, North China University of Science and Technology, China
Tao Liu, University of Oxford, United Kingdom
Copyright © 2024 Li, Dai, Zhou, Chen, Chen, Zhou, Yang, Yue, Shi and Qiu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jing Shi, MjY2MjgzMTI5MUBxcS5jb20=; Yong Qiu, MjIyNTg1MTY3NEBxcS5jb20=
†These authors have contributed equally to this work and share first authorship
 Song Li
Song Li Anhong Dai3†
Anhong Dai3† Yihao Zhou
Yihao Zhou Yizhou Chen
Yizhou Chen