- 1Department of Neurology, Sichuan Taikang Hospital, Chengdu, China
- 2Department of Rehabilitation, Sichuan Taikang Hospital, Chengdu, China
- 3Department of Nephrology, Sichuan Taikang Hospital, Chengdu, China
Background: Many systematic reviews (SRs) have reported the efficacy of acupuncture in improving Parkinson’s disease (PD), but the quality of evidence is unknown. Therefore, it is necessary to comprehensively summarize and objectively evaluate the evidence of acupuncture for PD.
Methods: Seven databases were searched to retrieve SRs on the acupuncture for PD. Two reviewers independently completed literature retrieval, screening, and data extraction. The methodological quality, risk of bias (RoB), evidence quality of the included SRs were assessed by the Assessing the Methodological Quality of Systematic Reviews 2 (AMSTAR 2), the Risk of Bias in Systematic Reviews (ROBIS), the Grading of Recommendations Assessment, Development and Evaluation (GRADE) tool.
Results: A total of 24 SRs were included. According to AMSTAR 2, 6 (25%) were rated as high quality, 6 (25%) were rated as moderate quality, and 12 (50%) were rated as very low quality. The application of the ROBIS tool showed that 12 (25%) SRs were at low risk of bias. The results of GRADE showed that 8 (7.62%) outcomes provided high quality evidence, 23 (21.9%) outcomes provided moderate quality evidence, 42 (40%) outcomes provided low quality evidence, and 32 (30.48%) outcomes provided very low quality evidence.
Conclusion: The overview indicates that acupuncture shows promise as a treatment for PD, although the evidence is limited and inconclusive due to methodological flaws and the heterogeneity of existing studies. Future research should focus on fully reporting methodological details and following review guidelines to produce more reliable and consistent evidence on the effectiveness of acupuncture for PD.
Systematic review registration: https://inplasy.com, identifier INPLASY202480049.
1 Introduction
Parkinson’ s disease (PD) is the second most common neurodegenerative disease globally, with its prevalence steadily rising as the population ages (Simon et al., 2020). In 2019, approximately 8.51 million individuals worldwide were affected by PD, a number projected to double to over 12 million by 2040 due to global aging trends (Huang et al., 2023; Dorsey et al., 2018). Motor symptoms like resting tremor, abnormal posture and gait, myotonia, and bradykinesia are prevalent in PD patients. Additionally, non-motor symptoms such as cognitive impairment, affective disorders, sleep disturbances, pain, and autonomic nervous system dysfunction are also common (Armstrong and Okun, 2020). PD not only impacts patients’ self-care abilities but also imposes a significant financial burden on families and society. Pathologically, PD is characterized by the progressive degeneration of dopaminergic neurons in the substantia nigra and the formation of Lewy bodies. Biochemically, there is a decrease in dopamine (DA) transmission in the striatum and an imbalance between DA and acetylcholine (ACh) transmitters (Simon et al., 2020). Presently, drug therapy is the primary clinical approach for treating PD, with commonly used medications including compound levodopa, dopamine receptor agonists, and monoamine oxidase inhibitors (Angelopoulou et al., 2023). Although these drugs are effective in delaying the development of PD, most patients require long-term or even lifelong treatment. However, long-term use drugs can cause many adverse reactions, such as gastrointestinal discomfort, dyskinesia, mental disorders, etc., affecting clinical efficacy and reduce patients’ quality of life. Consequently, there is a growing interest in non-pharmacological interventions for PD (Olanow et al., 2009).
Acupuncture, a traditional Chinese treatment known for its simplicity and acceptance, has been utilized in the treatment of neurodegenerative diseases such as Alzheimer’s disease and Parkinson’s disease. According to the World Health Organization survey on complementary and alternative therapies, acupuncture is practiced in 113 out of 133 countries (Deuel and Seeberger, 2020; World Health Organization, 2019). A multicenter randomized controlled trial (RCT) demonstrated that combining acupuncture with conventional PD drug treatment can significantly enhance the motor function of PD patients (Li et al., 2023). Animal studies have further validated the therapeutic potential of acupuncture for PD, indicating that acupuncture at GB34 and LR3 acupoints can stimulate motor function recovery and activate dopaminergic neurons in specific brain regions via the Akt-BDNF pathway and autophagy, ultimately reducing dopaminergic neuron degeneration (Hsu et al., 2020). These findings suggest that acupuncture may have a promising role in managing the motor symptoms of PD by modulating neuronal activity in targeted brain regions. In addition, non-motor symptoms of PD patients, such as sleep disorders, constipation and fatigue have attracted increasing attention (Armstrong and Okun, 2020). These non-motor symptoms seriously affect the quality of life of patients. Constipation is the highest incidence of non-motor symptoms in PD patients, and more than 80% of PD patients have constipation symptoms. Studies have shown that acupuncture of specific brain regions and spinal cord segments can balance the activities of the sympathetic and parasympathetic nervous systems, thereby regulating the function of the brain-gut axis and improving gastrointestinal motility (Deuel and Seeberger, 2020; Zhang et al., 2023). Furthermore, between 60 and 90% of PD patients may experience sleep disorders. A recent RCT demonstrated that acupuncture can improve Parkinson’s Disease Sleep Scale (PDSS) scores, thereby enhancing sleep quality in PD patients (Yan et al., 2024). These findings suggest that acupuncture may also alleviate non-motor symptoms associated with PD.
In recent years, numerous systematic reviews (SRs) have demonstrated that acupuncture can effectively improve both motor and non-motor symptoms in patients with PD. Systematic reviews are considered to provide high-quality and reliable information in evidence-based medicine. However, the quality of evidence in SRs is influenced by the included studies and the researchers’ grasp of methodology, leading to varying reliability of conclusions. The diverse types of acupuncture therapies and outcome indicators in the literature result in inconsistent conclusions across studies, hindering direct clinical recommendations. This review employs the Assessment Tool for Systematic Reviews 2 (AMSTAR 2), Risk of Bias for Systematic Reviews (ROBIS), and Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) to comprehensively evaluate SRs on acupuncture for PD treatment (Shea et al., 2017; Whiting et al., 2016; Schünemann et al., 2008). The aim is to rigorously assess the quality of relevant SRs and objectively assess the effectiveness and safety of acupuncture for PD.
2 Methods
2.1 Search strategy
We searched the PubMed, Embase, Web of Science, The Cochrane Library, China National Knowledge Infrastructure (CNKI), Wanfang Database, and Chongqing VIP database from their inception until March 1, 2024. We used a combination of subject words and free words, including “Parkinson Disease,” “Parkinson’s Disease,” “primary parkinsonism,” “Parkinsonism,” “Meta-Analysis,” “meta analysis,” “systematic review,” “acupuncture,” “electroacupuncture,” “scalp acupuncture.” In addition, we manually searched the list of references in the included SRs. Gray literature was excluded due to resource limitations. The detailed retrieval strategy is shown in Supplementary Table S1.
2.2 Inclusion criteria
We included SRs based on RCT of acupuncture for patients who were diagnosed with PD according to any internationally recognized clinical guidelines, regardless of symptoms or stage of PD. The experimental group interventions included manual acupuncture, electroacupuncture, scalp acupuncture, ear acupuncture, or acupuncture combined with PD conventional treatment (e.g., Madopar, levodopa, medication, repetitive transcranial magnetic stimulation). The control group interventions was treated with any other methods except acupuncture, such as sham acupuncture, placebo, PD conventional treatment, traditional Chinese medicine, and repetitive transcranial magnetic stimulation (rTMS). Assess motor and non-motor symptoms of PD as primary outcome measures in SRs: such as efficacy rate, Unified Parkinson’s disease rating scale (UPDRS), Parkinson’ s disease sleep scale (PDSS), Pittsburgh sleep quality indexs (PSQI), Hamilton Depression Scale (HAMD), Hamilton Anxiety Scale (HAMA), Standardized Swallowing Assessment (SSA), Parkinson’ s disease questionnaire (PDQ-39), et al.
2.3 Exclusion criteria
We excluded SRs if they met any of the following criteria: (a) The intervention was non-acupuncture based or the control group received the same acupuncture treatment as the experimental group; (b) SRs were analyzed using network meta-analysis or indirect comparison; (c)) duplicate publications; (d) unavailable full text or incomplete data; (e) other types of research, such as animal experiments, experimental protocols, conference papers.
2.4 Study selection and data extraction
Two reviewers (HX and YX-L) searched the databases according to a pre-established standardized search strategy. All retrieved literature was imported into the Literature Manager. Two reviewers independently screened candidate literature by reading titles and abstracts according to inclusion and exclusion criteria. The full text was then downloaded for further screening. At the same time, references were also reviewed to identify potential references. After identifying eligible studies, two reviewers independently extracted relevant data such as authors, year of publication, number of studies, sample size, interventions, outcomes, adverse effects, and conclusions. The two reviewers cross-checked the extracts and if there were discrepancies, a third reviewer (HX-H) was consulted to resolve the discrepancies.
2.5 Quality assessment
The evaluation for inclusion of SRs was conducted independently by two reviewers. Prior to the evaluation, each topic of the evaluation tool was discussed in depth to reach a consensus. At the end of the evaluation, the results were cross-checked by 2 reviewers. Disagreements were resolved by team discussion or by independent decision of the 3rd reviewer.
We used the Assessing the Methodological Quality of Systematic Reviews 2 (AMSTAR 2) to evaluate the methodological quality of the inclusion of SRs (Shea et al., 2017). The AMSTAR 2 scale consists of 16 items, each of which can be described as “Yes” and “No” and some of which can be described as “Partial yes”. Items 2, 4, 7, 9, 11, 13, and 15 are critical items and are used to critically assess the validity of an SRs. If there are no items deficiencies or only one non-critical items deficiency, the methodology is of high quality and the conclusions of the SRs are accurate and comprehensive; if there are non-critical items deficiencies but no critical items deficiencies, the methodology is of moderate quality and the conclusions of the SRs are accurate; if there is one critical items deficiency, with or without non-critical items deficiencies, the methodology is of low quality and the conclusions of the SRs are low; if there are more than one critical items deficiencies with or without non-critical items deficiencies, the methodology is of very low quality. The conclusion of SRs is inaccurate and incomplete.
We used the Risk of Bias in Systematic reviews (ROBIS) tool to assess the risk of bias (RoB) for SRs (Whiting et al., 2016). The assessment process was divided into three phases: (a) assessing relevance; (b) determining the degree of RoB in the SR process; and (c) judging RoB. The four key areas in phase 2 included study eligibility criteria, identification and selection of studies, data collection and study evaluation, and review and conclusions. Stage 3 judges the overall RoB based on the results of Stage 2, and finally categorizes the risk level as “Low risk,” “High risk,” and “Unclear risk”.
The GRADE (Grading of Recommendation, Assessment, Development, and Evaluation) tool was used to assess the quality of evidence (Schünemann et al., 2008). The quality of evidence was rated as high, moderate, low, or very low in four categories based on the presence of study limitations, inconsistency, imprecision, indirectness, or publication bias.
3 Results
3.1 Search results
According to the search strategy, 116 papers were retrieved, including 23 Meta-analyses and one qualitative analysis. 24 duplicates were excluded by filtration, 58 papers were screened by titles and abstracts. The remaining 34 papers were considered to be of interest. After full-text read, four papers were excluded due to not being SRs, two papers were not rigorous, four papers were network Meta-analyses. Thus, 24 papers met the inclusion criteria and were included in the final analysis (Fu and Shi, 2022; Hsu et al., 2023; Lee et al., 2008, 2013; Lee and Lim, 2017; Lei et al., 2023; Li et al., 2020, 2022; Lin et al., 2024; Liu et al., 2017, 2019; Liu and Jin, 2023; Noh et al., 2017; Ou and Xu, 2017; Sun and Zhang, 2013; Sun et al., 2023; Tan et al., 2023; Wen et al., 2021; Wu et al., 2023; Yan et al., 2024; Yang et al., 2010; Yin et al., 2016; Zhang et al., 2024; Zhou et al., 2020). The literature screening process is shown in Figure 1.
3.2 Characteristics of the included SRs
Table 1 presents the characteristics of the included studies. A total of 24 systematic reviews (SRs) were included that were published between 2008 and 2024, with 20 published after 2015. The number of original studies included ranged from 4 to 61, and nine SRs did not report sample sizes. Interventions in the treatment group were mainly acupuncture or acupuncture plus PD conventional treatment, rTMS, and traditional Chinese medicine, and interventions in the control group were mainly medication, rTMS, and sham acupuncture. 19 of the 24 SRs performed subgroup analyses, and eight performed sensitivity analyses. 20 SRs assessed risk of bias (RoB) using the Cochrane risk of bias tool, two used the Jadad scale, and two reviews did not mention risk of bias. In terms of conclusion, most SRs concluded that acupuncture has some advantages in treating PD, but the results still need to be validated by more and higher quality studies.
3.3 Methodological assessment
The methodological quality of the 24 SRs was evaluated using the AMSTAR 2 scale. Table 2 provides an overview of the methodological quality of the included SRs. Out of the 24 SRs, 6 (25%) were rated as high quality (Hsu et al., 2023; Lei et al., 2023; Li et al., 2022; Noh et al., 2017; Wen et al., 2021; Zhang et al., 2024), 6 (25%) as moderate quality (Lee and Lim, 2017; Lin et al., 2024; Tan et al., 2023; Wu et al., 2023; Yan et al., 2024; Zhou et al., 2020), and 12 (50%) as very low quality (Fu and Shi, 2022; Lee et al., 2008, 2013; Li et al., 2020; Liu et al., 2017, 2019; Liu and Jin, 2023; Ou and Xu, 2017; Sun and Zhang, 2013; Sun et al., 2023; Yang et al., 2010; Yin et al., 2016). The compliance rate for items 1, 3, 8, 10, and 16 was 100%. Regarding critical item 2, only 10 (41.67%) SRs clearly stated the review method before conducting the review. For critical item 4, 16 (66.67%) SRs provided detailed search strategies. In terms of critical item 7, 14 (58.34%) SRs provided reasons and lists for excluded literature. The compliance rate for key items 9 and 11 was 91.67%. For critical items 13 and 15, the compliance rate was 75%, with six SRs not meeting the requirements. Among non-critical items, items 1, 3, 8, 10, and 16 have a compliance rate of 100%. When assessing non-critical items 5 and 6, study selection and data extraction were repeated for 75% of SRs. When assessing non-critical item 12, 10 (41.67%) SRs assessed the potential impact of RoB in individual studies on the results of meta-analyses or other evidence reviews. 66.67% of SRs provided satisfactory explanations and discussions of the heterogeneity observed in the review results (Table 2).
3.4 Results of ROBIS evaluation
The Risk of Bias in Systematic reviews (ROBIS) tool was used to assess risk of bias (RoB). All SRs included in phase 1 were rated as having a low risk of bias in terms of relevance to the research topic. In domain 1, which evaluated study eligibility criteria, 6 SRs that lacked a detailed search strategy were rated as having a high risk of bias (Li et al., 2020; Liu et al., 2017; Liu and Jin, 2023; Ou and Xu, 2017; Yang et al., 2010; Yin et al., 2016). Domain 2, which focused on the identification and selecting of studies, found 9 SRs to have a high risk of bias (Fu and Shi, 2022; Li et al., 2020; Liu et al., 2017; Liu and Jin, 2023; Ou and Xu, 2017; Sun and Zhang, 2013; Sun et al., 2023; Yang et al., 2010; Yin et al., 2016). Moving on to domain 3, which assessed the collection and appraisal of studies, 14 SRs were deemed to have a low risk of bias (Fu and Shi, 2022; Hsu et al., 2023; Lee and Lim, 2017; Lei et al., 2023; Li et al., 2022; Lin et al., 2024; Liu et al., 2017; Liu and Jin, 2023; Sun and Zhang, 2013; Sun et al., 2023; Tan et al., 2023; Zhang et al., 2024; Zhou et al., 2020). In domain 4, which examined the synthesis and findings, 14 out of the 24 SRs were rated as having a low risk of bias (Hsu et al., 2023; Lee and Lim, 2017; Lei et al., 2023; Li et al., 2022; Lin et al., 2024; Noh et al., 2017; Ou and Xu, 2017; Tan et al., 2023; Wen et al., 2021; Wu et al., 2023; Yan et al., 2024; Yang et al., 2010; Zhang et al., 2024; Zhou et al., 2020). Phase 3 evaluated the overall risk of bias of the reviews, with 12 SRs being classified as having a low risk of bias (Hsu et al., 2023; Lee and Lim, 2017; Lei et al., 2023; Li et al., 2022; Lin et al., 2024; Liu et al., 2017; Noh et al., 2017; Tan et al., 2023; Wen et al., 2021; Wu et al., 2023; Yan et al., 2024; Zhang et al., 2024; Zhou et al., 2020). For more detailed information, please refer to Table 3.
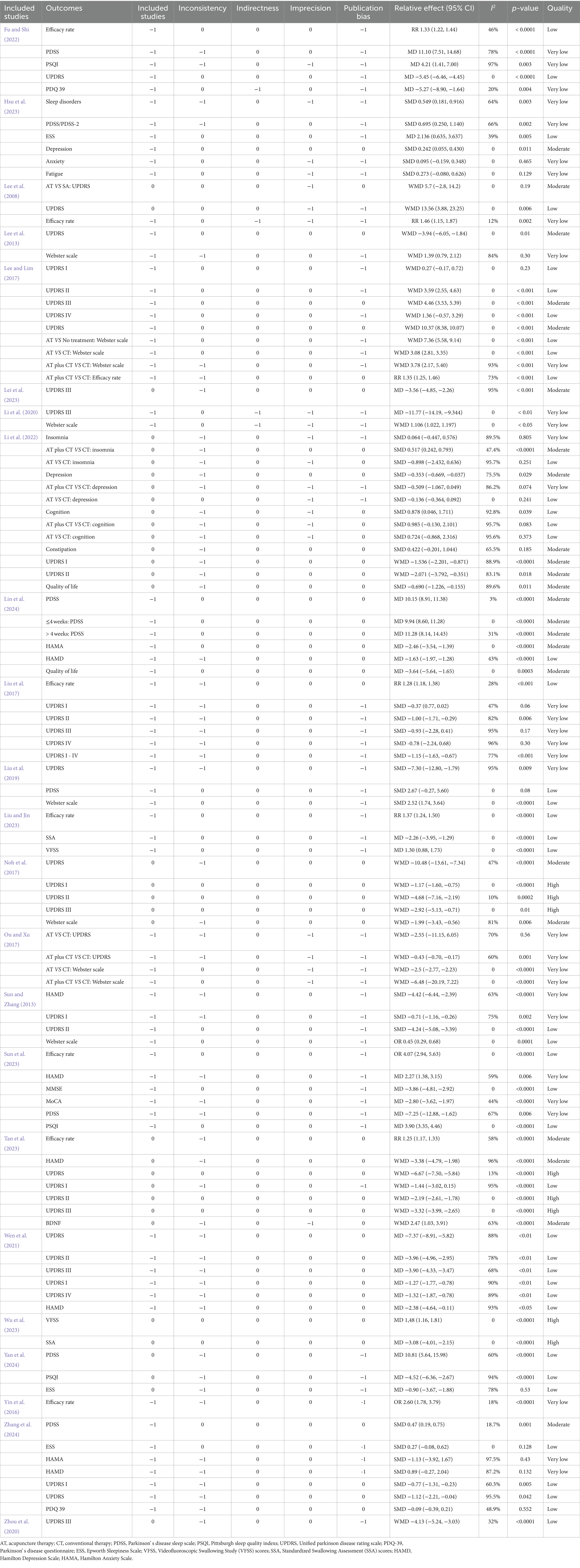
3.5 Quality of evidence
The 24 SRs consisted of 105 outcomes related to the effectiveness of acupuncture in the treatment of PD with respect to effectiveness rate, UPDRS, UPDRS I, UPDRS II, UPDRS III, UPDRS IV, PDSS, PSQI, PDQ-39, ESS, Webster scale, Quality of life, HAMA, HAMD, etc. The GRADE assessment showed that 8 (7.62%) outcomes provided high quality evidence, 23 (21.9%) outcomes provided moderate quality evidence, 42 (40%) outcomes provided low quality evidence, and 32 (30.48%) outcomes provided very low quality evidence. The evidence was downgraded due to the following limitations: (1) Randomization, blinding, and allocation concealment bias in clinical studies reduce the validity of the GRADE method. (2) We downgraded the quality of the evidence based on publication bias due to incomplete literature search and the number of research clinical trials. (3) We downgrade the quality of the evidence to imprecise if the confidence interval is wide or the number of participants is small. (4) Heterogeneity was high, and we downgraded the quality of the evidence on the grounds of inconsistency. Additional details are provided in Table 4.
3.6 Outcome indicators and related conclusions
Ten SRs assessed the UPDRS, and eight of these SRs came to the unanimous conclusion that acupuncture in combination with conventional treatments or acupuncture treatment alone was more advantageous in improving the UPDRS than the control group (Fu and Shi, 2022; Lee et al., 2008, 2013; Lee and Lim, 2017; Liu et al., 2019; Noh et al., 2017; Ou and Xu, 2017; Tan et al., 2023; Wen et al., 2021; Zhang et al., 2024). Lee et al. (2008) SRs comparing acupuncture with placebo acupuncture resulted in acupuncture failing to be more advantageous in UPDRS (WMD = 5.7, 95% CI 22.8 to 14.2, p = 0.19). In addition, acupuncture combined with medication was superior to medication alone for UPDRS (WMD = 13.56, 95% CI 3.88 to 23.25, p = 0.006) (Lee et al., 2008). Meta-analysis by Ou et al. showed that acupuncture alone did not provide an advantage over conventional treatment for PD in terms of improvement in UPDRS between the two groups (WMD = −2.77, 95% CI −11.15 to 6.05, p = 0.56), and acupuncture combined with PD conventional treatment was more advantageous than conventional treatment alone (WMD = −0.43, 95% CI -0.7 to −0.17, p = 0.001) (Ou and Xu, 2017). Eight SRs focused on UPDRS I scores, with two SRs concluding that UPDRS I scores did not significantly improve after acupuncture treatment (Lee and Lim, 2017; Liu et al., 2017), and six SRs concluding that acupuncture therapy in combination with medications or acupuncture alone significantly improved UPDRS I scores compared with medications alone (Li et al., 2022; Noh et al., 2017; Sun and Zhang, 2013; Tan et al., 2023; Wen et al., 2021; Zhang et al., 2024). UPDRS II was the activity of daily living score, and 7 SRs focused on UPDRS II score (Lee and Lim, 2017; Li et al., 2022; Liu et al., 2017; Noh et al., 2017; Sun and Zhang, 2013; Tan et al., 2023; Wen et al., 2021). The results showed that acupuncture combined with drugs was superior to the control group in reducing UPDRS II score (Lee and Lim, 2017; Li et al., 2022; Liu et al., 2017; Noh et al., 2017; Sun and Zhang, 2013; Tan et al., 2023; Wen et al., 2021). Eight SRs focused on UPDRS III scores, with the results of one SR concluding that acupuncture therapy did not demonstrate a significant advantage over conventional treatment, and the results of seven SRs showing that acupuncture therapy was superior to controls in reducing UPDRS III scores (Lee and Lim, 2017; Lei et al., 2023; Li et al., 2020; Liu et al., 2017; Noh et al., 2017; Tan et al., 2023; Wen et al., 2021; Zhou et al., 2020). Three SRs focused on the UPDRS IV, of which two SRs considered that acupuncture combined with drug therapy had an advantage over conventional treatment in reducing the UPDRS IV score, and 1 SR considered that acupuncture combined with conventional therapy did not show a significant advantage over conventional therapy (Lee and Lim, 2017; Liu et al., 2017; Wen et al., 2021).
Seven SRs assessed the efficacy rate and showed that the acupuncture group had a higher efficacy rate than the control group (Fu and Shi, 2022; Lee et al., 2008; Lee and Lim, 2017; Liu et al., 2017; Sun et al., 2023; Tan et al., 2023; Yin et al., 2016). 7 SRs used the Webster score to evaluate the overall symptoms (Lee et al., 2013; Lee and Lim, 2017; Li et al., 2020; Liu et al., 2019; Noh et al., 2017; Ou and Xu, 2017; Sun and Zhang, 2013). 6 of them concluded that the Webster score after acupuncture treatment was lower than that after conventional treatment, and that acupuncture treatment was better than conventional treatment (Lee and Lim, 2017; Li et al., 2020; Liu et al., 2019; Noh et al., 2017; Ou and Xu, 2017; Sun and Zhang, 2013). One SR concluded that there was no significant difference in Webster scores after acupuncture treatment and conventional treatment (Lee et al., 2013). Eight SRs evaluated the efficacy of acupuncture in the treatment of sleep disorders in PD patients. The outcome indicators mainly included PDSS, PSQI, ESS (Fu and Shi, 2022; Hsu et al., 2023; Li et al., 2022; Lin et al., 2024; Liu et al., 2019; Sun et al., 2023; Yan et al., 2024; Zhang et al., 2024), of which 2 SRs considered that acupuncture had no significant effect in improving sleep disorders (Li et al., 2022; Liu et al., 2019), of which 2 SRs considered that acupuncture did not improve the ESS score (Yan et al., 2024; Zhang et al., 2024). 8 SRs focused on the mental disorder of PD patients, and outcome indicators included HAMA, HAMD, anxiety symptoms, depressive symptoms, fatigue, etc. (Hsu et al., 2023; Li et al., 2022; Lin et al., 2024; Sun and Zhang, 2013; Sun et al., 2023; Tan et al., 2023; Wen et al., 2021; Zhang et al., 2024). The results of 3 of the SRs showed that acupuncture treatment could not improve anxiety, depression, and fatigue (Hsu et al., 2023; Li et al., 2022; Zhang et al., 2024). Four articles focused on the daily living abilities of PD patients (Fu and Shi, 2022; Li et al., 2022; Lin et al., 2024; Zhang et al., 2024), and the outcome indicators included PDQ 39. One of the SR believed that acupuncture treatment did not improve the daily living abilities of PD patients (Zhang et al., 2024). Two SRs evaluated the swallowing ability of patients with PD treated with acupuncture, and the outcome indicators included SSA and VFSS (Liu and Jin, 2023; Wu et al., 2023). 2SRs demonstrated that acupuncture could improve dysphagia. Only 1 SR focused on constipation, and the results showed that acupuncture cannot improve constipation in PD patients (Li et al., 2022). Two SRs focused on the cognitive function of PD patients, and the outcome indicators included MMSE and MoCA (Li et al., 2022; Sun et al., 2023). They concluded that acupuncture can improve the cognitive function of PD.
4 Discussion
4.1 Summary of the main results
This overview provides a comprehensive descriptive analysis of 24 SRs of acupuncture for patients with PD, involving 425 clinical studies. We used AMSTAR 2, ROBIS, and GRADE to comprehensively assess the methodological quality, quality of evidence, and RoB of the published SRs. According to AMSTAR 2, 6 (25%) were rated as high quality, 6 (25%) were rated as moderate quality, and 12 (50%) were rated as very low quality. The application of the ROBIS tool showed that 12 (25%) SRs were at low risk of bias. The results of GRADE showed that 8 (7.62%) outcomes provided high quality evidence, 23 (21.9%) outcomes provided moderate quality evidence, 42 (40%) outcomes provided low quality evidence, and 32 (30.48%) outcomes provided very low quality evidence.
4.2 Results-based discussion
According to AMSTAR 2, 50% of systematic reviews (SRs) were deemed to have very low methodological quality, indicating a significant issue with the overall quality of SRs. Specifically, 58.33% (14/24) of SRs lacked a comprehensive plan prior to commencing the review process, raising concerns about the adherence to a structured research plan during the review. This lack of clarity in the research process can potentially introduce bias. Additionally, 8 out of 24 SRs had deficiencies in their literature search strategies due to the absence of detailed search strategies, keywords, and Mesh terms. Furthermore, 10 out of 24 SRs did not provide explanations for excluding specific literature, while 6 out of 24 SRs failed to adequately address bias in individual studies and explore publication bias. In terms of non-critical items, some SRs did not implement duplicate study screening and data extraction.
The GRADE assessment revealed that 8 (7.62%) outcomes presented high quality evidence, 23 (21.9%) outcomes presented moderate quality evidence, 42 (40%) outcomes presented low quality evidence, and 32 (30.48%) outcomes presented very low quality evidence. Study limitations, publication bias, inconsistency, and inaccuracy in systematic reviews reduce the overall quality of evidence. The majority of evidence in the original studies included in the literature was deemed to have a high risk of bias due to insufficient reporting of randomization, blinding, allocation concealment, and other factors, as well as issues such as loss of visits, withdrawals, and publication bias. To enhance the reliability of results, researchers conducting systematic reviews should thoroughly evaluate and report on these key aspects of the original literature. Some studies had small sample sizes but showed large differences in effect sizes and minimal overlap in confidence intervals, resulting in imprecise results. Furthermore, there was significant heterogeneity among the raw data, which was not adequately addressed during the analysis, thereby diminishing the quality of the evidence. Possible sources of this heterogeneity include: 1) Variations in acupuncture techniques across studies, which may involve different acupuncture points, frequencies, or treatment duration; 2) Differences in outcome measures, as studies may utilize varying scales or assess the effects of acupuncture differently; and 3) Variability in the characteristics of study participants, such as age, disease severity, and medication use. These findings highlight the importance of a thorough description of included RCTs in systematic reviews to help identify sources of heterogeneity and facilitate a more objective and comprehensive analysis of the results.
4.3 Mechanism of acupuncture for PD
This overview suggests that acupuncture has potential in the treatment of PD, and most of the conclusions indicate that it can alleviate the motor and non-motor symptoms of PD. The main characteristic of PD is the degeneration and loss of dopamine (DA) neurons. Dopamine neurons are located in the substantia nigra and plays an important role in regulating movement and coordinating muscle activity (Simon et al., 2020). Apoptosis may participate in the degenerative process of neurons through multiple pathways in PD, and is also one of the main pathways leading to PD (Lev et al., 2003). Increased P53 expression plays an important role in the pathogenesis of PD (Luo et al., 2022). Electroacupuncture can inhibit cell apoptosis and improve PD behavioral disorders by down regulating the P53 pathway in the striatum, providing a theoretical basis for the prevention and treatment of PD (Park et al., 2015). Acupuncture can inhibit the activation of the MAP4K3/MKK4/JNK pathway, thereby alleviating cell death and pathological changes in the hippocampal tissue of PD rats, while also improving their cognitive and behavioral functions (Park et al., 2015). Research indicates a close relationship between oxidative stress and Parkinson’s disease (PD) (Zhao et al., 2022). Acupuncture treatment has been shown to regulate oxidative stress indicators in patients by reducing malondialdehyde levels and increasing superoxide dismutase, glutathione peroxidase, and catalase levels (Zhao et al., 2022). Additionally, acupuncture has been found to regulate oxidative stress by activating the Nrf2/ARE pathway and Nrf2/ARE-related pathways, demonstrating antioxidant effects that help protect dopaminergic neurons from degeneration (Huang and Hsieh, 2021). Glutamic acid (Glu) is the predominant excitatory amino acid in the central nervous system, widely utilized. While Glu is not inherently toxic, it can modulate dopamine activity and release by activating specific Glu receptors in dopaminergic neurons, leading to potential toxicity. Research indicates that electroacupuncture can effectively modulate glutamate receptors, thereby decreasing glutamate levels in the striatum and cortex of mice (Jia et al., 2017). Damage to the substantia nigra area in PD is closely associated with an inflammatory response. Research indicates that the impact of acupuncture on improving motor function and preserving dopaminergic neurons may be linked to its ability to regulate intestinal microbial dysbiosis, consequently reducing neuroinflammation in PD mice (Jang et al., 2020). Based on current research conclusions, acupuncture can improve PD by regulating oxidative stress, immune inflammation, neurotransmitters, and mitochondrial function.
4.4 Implications for further study
Based on the results of the evaluations, we made several recommendations for improvement in response to the shortcoming. For example, to further clarify the conclusions on the effectiveness and safety of acupuncture for improving PD, reviewers should pre-register or publish the study protocols to avoid any risk of bias and to ensure the rigor of the SR process. During literature screening, a detailed and comprehensive search strategy should be provided with a list and explanation of excluded literature to avoid publication bias. When analyzing the data, subgroup analyses should be performed based on interventions, demographic information, etc. In terms of quality of evidence, future RCTs should address methodological issues through rigorous trial design, rational assessment, and critical analysis, and researchers should follow basic guidelines for clinical trial reporting, such as Comprehensive Standards for Trial Reporting (CONSORT) and Standards for Reporting of Interventions in Clinical Trials of Acupuncture (STRICTA2010).
5 Strengths and limitations
SRs based on high quality randomized controlled trials (RCTs) are essential for clinical decision-making in evidence-based medicine. However, the proliferation of SRs in recent years has raised concerns about their overall quality. Numerous studies have been published recently demonstrating the positive effects of acupuncture on PD. We systematically assessed the methodological quality, RoB and quality of evidence of relevant SRs using AMSTAR 2, ROBIS and GRADE tools, respectively. Limitations of our overview: First, we can only provide a comprehensive description of all SRs. Differences in study design and acupuncture intervention details may have resulted in a higher RoB for SR, thereby reducing the quality of the evidence and methods. Second, it must be acknowledged that quality assessment remains a subjective process and individual reviewers may judge each factor differently, leading to possible differences in results. Although evaluated and reviewed by two independent reviewers, the results of our study may differ from those of the other reviewers. Third, due to resource limitations, although seven databases were searched, they only included studies published in English or Chinese. This may create language bias and may exclude relevant SRs published in other languages.
5 Conclusion
The overview indicates that acupuncture is promising as an adjuvant therapy in improving movement disorder, depression, and sleep disorders in PD. Due to methodological flaws and the heterogeneity of available studies, current evidence is limited and inconclusive. High-quality, rigorously designed RCT studies should be conducted in the future to verify the effectiveness and safety of acupuncture in treating PD, which is crucial to advancing clinical decision-making and the development of treatment guidelines.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
HX: Conceptualization, Methodology, Writing – original draft, Writing – review & editing. H-xH: Formal analysis, Software, Writing – review & editing. DW: Methodology, Software, Writing – review & editing. W-hF: Data curation, Formal analysis, Funding acquisition, Methodology, Writing – review & editing. Y-xL: Conceptualization, Methodology, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnins.2024.1415008/full#supplementary-material
References
Angelopoulou, E., Stanitsa, E., Karpodini, C. C., Bougea, A., Kontaxopoulou, D., Fragkiadaki, S., et al. (2023). Pharmacological and non-pharmacological treatments for depression in Parkinson's disease: an updated review. Medicina (Kaunas) 59:1454. doi: 10.3390/medicina59081454
Armstrong, M. J., and Okun, M. S. (2020). Diagnosis and treatment of Parkinson disease: a review. JAMA 323, 548–560. doi: 10.1001/jama.2019.22360
Deuel, L. M., and Seeberger, L. C. (2020). Complementary therapies in Parkinson disease: a review of acupuncture, tai chi, Qi Gong, yoga, and cannabis. Neurotherapeutics 17, 1434–1455. doi: 10.1007/s13311-020-00900-y
Dorsey, E. R., Sherer, T., Okun, M. S., and Bloem, B. R. (2018). The emerging evidence of the Parkinson pandemic. J. Parkinsons Dis. 8, S3–s8. doi: 10.3233/jpd-181474
Fu, J., and Shi, J. (2022). Treatment of Parkinson disease with sleep wake disorders by acupuncture: a meta-analysis. J. Xinjiang Med. Univ. 45, 1348–1361. doi: 10.3969/j.issn.1009-5551.2022.11.021
Hsu, W. T., Chen, Y. H., Yang, H. B., Lin, J. G., and Hung, S. Y. (2020). Electroacupuncture improves motor symptoms of Parkinson's disease and promotes neuronal autophagy activity in mouse brain. Am. J. Chin. Med. 48, 1651–1669. doi: 10.1142/s0192415x20500822
Hsu, W. T., Hsu, C. M., Hung, S. C., and Hung, S. Y. (2023). Acupuncture improves sleep disorders and depression among patients with Parkinson's disease: a meta-analysis. Healthcare (Basel) 11:2042. doi: 10.3390/healthcare11142042
Huang, T. I., and Hsieh, C. L. (2021). Effects of acupuncture on oxidative stress amelioration via Nrf2/ARE-related pathways in Alzheimer and Parkinson diseases. Evid. Based Complement. Alternat. Med. 2021:6624976. doi: 10.1155/2021/6624976
Huang, Y., Li, Y., Pan, H., and Han, L. (2023). Global, regional, and National Burden of neurological disorders in 204 countries and territories worldwide. J. Glob. Health 13:04160. doi: 10.7189/jogh.13.04160
Jang, J. H., Yeom, M. J., Ahn, S., Oh, J. Y., Ji, S., Kim, T. H., et al. (2020). Acupuncture inhibits Neuroinflammation and gut microbial Dysbiosis in a mouse model of Parkinson's disease. Brain Behav. Immun. 89, 641–655. doi: 10.1016/j.bbi.2020.08.015
Jia, Y. J., Deng, J. H., Zhang, W. Z., Sun, Z. L., Yang, J., Yu, Y., et al. (2017). The role of group ii metabotropic glutamate receptors in the striatum in Electroacupuncture treatment of parkinsonian rats. CNS Neurosci. Ther. 23, 23–32. doi: 10.1111/cns.12587
Lee, S. H., and Lim, S. (2017). Clinical effectiveness of acupuncture on Parkinson disease: a Prisma-compliant systematic review and meta-analysis. Medicine (Baltimore) 96:e5836. doi: 10.1097/md.0000000000005836
Lee, H. S., Park, H. L., Lee, S. J., Shin, B. C., Choi, J. Y., and Lee, M. S. (2013). Scalp acupuncture for Parkinson's disease: a systematic review of randomized controlled trials. Chin. J. Integr. Med. 19, 297–306. doi: 10.1007/s11655-013-1431-9
Lee, M. S., Shin, B. C., Kong, J. C., and Ernst, E. (2008). Effectiveness of acupuncture for Parkinson's disease: a systematic review. Mov. Disord. 23, 1505–1515. doi: 10.1002/mds.21993
Lei, S., Fan, J., Liu, X., Xv, X., Zhang, J., Zhou, Z., et al. (2023). Qualitative and quantitative meta-analysis of acupuncture effects on the motor function of Parkinson's disease patients. Front. Neurosci. 17:1125626. doi: 10.3389/fnins.2023.1125626
Lev, N., Melamed, E., and Offen, D. (2003). Apoptosis and Parkinson's disease. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 27, 245–250. doi: 10.1016/s0278-5846(03)00019-8
Li, X. Y., Dong, Q. J., Ma, T. Y., Li, J. F., and Tang, M. Q. (2020). Systematic review of randomized controlled trials of acupuncture for Parkinson's disease. Heilongjiang Chin. Med. 3.
Li, Q., Wu, C., Wang, X., Li, Z., Hao, X., Zhao, L., et al. (2022). Effect of acupuncture for non-motor symptoms in patients with Parkinson's disease: a systematic review and meta-analysis. Front. Aging Neurosci. 14:995850. doi: 10.3389/fnagi.2022.995850
Li, K., Xu, S., Wang, R., Zou, X., Liu, H., Fan, C., et al. (2023). Electroacupuncture for motor dysfunction and constipation in patients with Parkinson's disease: a randomised controlled multi-Centre trial. EClinicalMedicine 56:101814. doi: 10.1016/j.eclinm.2022.101814
Lin, J., Kong, Y., Chen, H., Ding, X., and Zhou, W. (2024). Effects of acupuncture on sleep quality in patients with Parkinson's disease: a systematic review and meta-analysis. Clin. Rehabil. 38, 478–496. doi: 10.1177/02692155231218535
Liu, H., Chen, L., Zhang, Z., Geng, G., Chen, W., Dong, H., et al. (2017). Effectiveness and safety of acupuncture combined with Madopar for Parkinson's disease: a systematic review with meta-analysis. Acupunct. Med. 35, 404–412. doi: 10.1136/acupmed-2016-011342
Liu, Y. W., and Jin, H. P. (2023). Meta-analysis of the efficacy and safety of acupuncture in the treatment of Parkinson’s disease combined with dysphagia. Chin. Med. Sci. 13, 95–98. doi: 10.20116/j.issn2095-0616.2023.19.21
Liu, M. H., Wang, S. J., and Yuan, L. (2019). Meta-analysis of scalp acupuncture in the treatment of Parkinson's disease. Lishizhen Med. Materia Med. Res. 30.
Luo, Q., Sun, W., Wang, Y. F., Li, J., and Li, D. W. (2022). Association of P53 with neurodegeneration in Parkinson's disease. Parkinsons Dis. 2022:6600944. doi: 10.1155/2022/6600944
Noh, H., Kwon, S., Cho, S. Y., Jung, W. S., Moon, S. K., Park, J. M., et al. (2017). Effectiveness and safety of acupuncture in the treatment of Parkinson's disease: a systematic review and meta-analysis of randomized controlled trials. Complement. Ther. Med. 34, 86–103. doi: 10.1016/j.ctim.2017.08.005
Olanow, C. W., Stern, M. B., and Sethi, K. (2009). The scientific and clinical basis for the treatment of Parkinson disease. Neurology 72, S1–S136. doi: 10.1212/WNL.0b013e3181a1d44c
Ou, Y. S., and Xu, W. (2017). Systematic evaluation of the efficacy comparison between acupuncture and Western medicine in the treatment of Parkinson 'S disease. J. Tradit. Chin. Med. 16, 34–38. doi: 10.14046/j.cnki.zyytb2002.2017.01.014
Park, J. Y., Choi, H., Baek, S., Jang, J., Lee, A., Jeon, S., et al. (2015). P53 signalling mediates acupuncture-induced neuroprotection in Parkinson's disease. Biochem. Biophys. Res. Commun. 460, 772–779. doi: 10.1016/j.bbrc.2015.03.105
Schünemann, H. J., Oxman, A. D., Brozek, J., Glasziou, P., Jaeschke, R., Vist, G. E., et al. (2008). Grading quality of evidence and strength of recommendations for diagnostic tests and strategies. BMJ 336, 1106–1110. doi: 10.1136/bmj.39500.677199.AE
Shea, B. J., Reeves, B. C., Wells, G., Thuku, M., Hamel, C., Moran, J., et al. (2017). Amstar 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 358:j4008. doi: 10.1136/bmj.j4008
Simon, D. K., Tanner, C. M., and Brundin, P. (2020). Parkinson disease epidemiology, pathology, genetics, and pathophysiology. Clin. Geriatr. Med. 36, 1–12. doi: 10.1016/j.cger.2019.08.002
Sun, Y., Pan, J. H., Zhang, F. Y., and Fu, W. B. (2023). Accupuncture and Moxibustion for the treatment of non-motor symptoms in Parkinson’s disease: a meta-analysis. J. Guangzhou Univ. Trad. Chin. Med. 40, 516–525. doi: 10.13359/j.cnki.gzxbtcm.2023.02.039
Sun, M. X., and Zhang, X. (2013). Meta-analysis of the efficacy of acupuncture in the treatment of non-motor symptoms of Parkinson 'S disease. J. Shanghai Univ. Trad. Chin. Med. 27, 41–44. doi: 10.16306/j.1008-861x.2013.05.018
Tan, W. Q., Li, M. C., Chen, Y. Y., Wang, N. B., and Zhuang, L. X. (2023). Meta-analysis of acupuncture therapy for Parkinson's disease depression. World J. Tradit. Chin. Med. 18, 2457–2465. doi: 10.3969/j.issn.1673-7202.2023.17.009
Wen, X., Li, K., Wen, H., Wang, Q., Wu, Z., Yao, X., et al. (2021). Acupuncture-related therapies for Parkinson's disease: a meta-analysis and qualitative review. Front. Aging Neurosci. 13:676827. doi: 10.3389/fnagi.2021.676827
Whiting, P., Savović, J., Higgins, J. P., Caldwell, D. M., Reeves, B. C., Shea, B., et al. (2016). Robis: a new tool to assess risk of bias in systematic reviews was developed. J. Clin. Epidemiol. 69, 225–234. doi: 10.1016/j.jclinepi.2015.06.005
World Health Organization (2019). WHO global report on traditional and complementary medicine. Available at: https://apps.who.int/iris/handle/10665/312342
Wu, J., Wang, Y., Wang, X., Xie, Y., and Li, W. (2023). A systematic review and meta-analysis of acupuncture in Parkinson's disease with dysphagia. Front. Neurol. 14:1099012. doi: 10.3389/fneur.2023.1099012
Yan, F., Chen, C., Feng, Q., Huang, Z., Chen, Y., and Chen, H. (2024). Acupuncture and sleep disorders in Parkinson's disease: a systematic evaluation with meta-analysis. Medicine (Baltimore) 103:e36286. doi: 10.1097/md.0000000000036286
Yan, M., Fan, J., Liu, X., Li, Y., Wang, Y., Tan, W., et al. (2024). Acupuncture and sleep quality among patients with Parkinson disease: a randomized clinical trial. JAMA Netw. Open 7:e2417862. doi: 10.1001/jamanetworkopen.2024.17862
Yang, L. H., Du, Y. H., Xiong, J., Liu, J. L., Wang, Y. N., and Li, Y. (2010). Acupuncture treatment for Parkinson disease: a systematic review. Chin. J. Evid. Based Med.
Yin, H. N., Han, C., Sun, Z. R., Han, B., and Chang, Y. (2016). Randomized controlled trials of acupuncture for Parkinson's disease: a systematic review and meta-analysis. Clin. J. Acupunct. 32, 67–70. doi: 10.19917/j.cnki.1005-0779.2016.08.022
Zhang, J., Ge, X., Zhang, K., Qi, Y., Ren, S., and Zhai, X. (2023). Acupuncture for Parkinson's disease-related constipation: current evidence and perspectives. Front. Neurol. 14:1253874. doi: 10.3389/fneur.2023.1253874
Zhang, A., Song, Z., Di, A., Zhou, Z., Zheng, L., and Zhuang, L. (2024). Acupuncture for the treatment of neuropsychiatric symptoms in Parkinson's disease: a systematic review and meta-analysis. Complement. Ther. Med. 80:103020. doi: 10.1016/j.ctim.2024.103020
Zhao, Y., Zhou, B., Zhang, G., Xu, S., Yang, J., Deng, S., et al. (2022). The effect of acupuncture on oxidative stress: a systematic review and meta-analysis of animal models. PLoS One 17:e0271098. doi: 10.1371/journal.pone.0271098
Keywords: acupuncture, systematic review, GRADE, Parkinson’s disease, AMSTAR 2
Citation: Xue H, He H-x, Wu D, Fan W-h and Li Y-x (2024) An overview of systematic reviews of acupuncture for Parkinson’s disease. Front. Neurosci. 18:1415008. doi: 10.3389/fnins.2024.1415008
Edited by:
Muthuraju Sangu, Universiti Sains Malaysia Health Campus, MalaysiaReviewed by:
Xu Zhai, China Academy of Chinese Medical Sciences, ChinaBharatkumar Asokar, Tamil Nadu Dr. M.G.R. Medical University, India
Copyright © 2024 Xue, He, Wu, Fan and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wen-hui Fan, ZmFud2VuaHVpNTEyOEAxMjYuY29t; Ya-xin Li, bGl5eDE0NEAxNjMuY29t
 Hua Xue
Hua Xue Hong-xian He
Hong-xian He Dan Wu3
Dan Wu3 Wen-hui Fan
Wen-hui Fan