
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Neurosci. , 26 September 2023
Sec. Translational Neuroscience
Volume 17 - 2023 | https://doi.org/10.3389/fnins.2023.1275452
Background and objective: Post-stroke constipation (PSC) is a common complication of strokes that seriously affects the recovery and quality of life of patients, and effective treatments are needed. Acupuncture is a viable treatment option, but current evidence is insufficient to support its efficacy and safety. This study aims to evaluate the efficacy and safety of acupuncture in the treatment of PSC.
Methods: A systematic search of eight databases was conducted to identify PSC-related randomized clinical trials from the inception of each database through May 2023. Methodological quality assessment was conducted by RoB 2.0, meta-analysis was conducted by RevMan 5.3 and Stata 15.1, and evidence quality was evaluated by GRADE. Moreover, reporting quality of acupuncture interventions was assessed using the Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA).
Results: Thirty RCTs involving 2,220 patients were identified. We found that acupuncture was superior to conventional treatment (CT) in improving total responder rate [risk ratio (RR): 1.16, 95% confidence interval (CI): 1.09 to 1.25, p < 0.0001], decreasing constipation symptom scores [standardized mean difference (SMD): -0.65, 95% CI: −0.83 to −0.46, p < 0.00001], increasing serum P substance (SP) levels (SMD: 1.92, 95% CI: 0.47 to 3.36, p = 0.009), reducing the time to first bowel movement (BM) (SMD: -1.19, 95% CI: −2.13 to −0.25, p = 0.01), and lowing serum vasoactive intestinal peptide (VIP) levels (SMD: –2.11, 95% CI: −3.83 to −0.38, p = 0.02). Furthermore, acupuncture plus CT was superior regarding total responder rate (RR: 1.26, 95% CI: 1.17 to 1.35, p < 0.00001), serum SP levels (SMD: 2.00, 95% CI: 1.65–2.35, p < 0.00001), time to first BM (SMD: –2.08, 95% CI: −2.44 to −1.71, p < 0.00001), and serum VIP levels (SMD: –1.71, 95% CI: −2.24 to −1.18, p < 0.00001). However, regarding Bristol Stool Scale (BSS) score, acupuncture plus CT was superior to CT (SMD: -2.48, 95% CI: −3.22 to −1.73, p < 0.00001), while there was no statistically significant difference between acupuncture and CT (SMD: 0.28, 95% CI: −0.02 to 0.58, p = 0.07). Acupuncture causes fewer AEs than CT (RR: 0.13, 95% CI: 0.06 to 0.26, p < 0.00001), though there was no statistically significant difference between acupuncture plus CT vs. CT (RR: 1.30, 95% CI: 0.60 to 2.84, p = 0.51).
Conclusion: Acupuncture may be an effective and safe therapy for PSC. However, given the inferior quality of clinical data, additional well-designed RCTs are required to confirm these findings.
Stroke is one of the top three global disease burdens (GBD 2019 Stroke Collaborators, 2021), and post-stroke constipation (PSC) is a common complication with a prevalence of 50–70% in stroke patients (Su et al., 2009; Liu Q. et al., 2018; Liu Z. et al., 2018). PSC seriously affects the treatment and rehabilitation of stroke (Harris and Chang, 2022), leading to decreased quality of life, prolonged hospitalization, and increased healthcare costs. PSC also induces or aggravates other complications like post-stroke depression and may lead to recurrent stroke and death (Sumida et al., 2019), placing a substantial burden on the national healthcare system.
The exact mechanism of PSC is unclear. Studies suggest a close relationship with autonomic dysfunction (Liu Q. et al., 2018; Liu Z. et al., 2018), multidrug usage (Su et al., 2009), dietary changes, and reduced activity (Lim et al., 2015). Recently, the brain-gut axis has received much attention as a bi-directional channel between the gastrointestinal tract and the autonomic nerves of the central nervous system that uses a variety of neurotransmitters, brain-gut peptides, and gut microbes (Carabotti et al., 2015; Camilleri, 2021; Xu et al., 2021), which are considered relevant to the development of PSC. Because of the lack of clinical and basic research related to PSC, current treatment strategies are mostly based on clinical practice guidelines for functional constipation (Chang et al., 2022, 2023), such as the use of laxatives, 5-hydroxytryptamine type 4 agonists, and enemas. However, relief is usually temporary, and side effects such as bloating, diarrhea, colon damage, melanosis coli, and cardiovascular adverse events cannot be ignored (Gilsenan et al., 2019; Chang et al., 2022, 2023). Safer and more effective alternative treatments are urgently needed.
Acupuncture is a complementary and alternative medicine of Chinese origin, of which the most common forms include manual acupuncture (MA), electroacupuncture (EA), moxibustion, and warm acupuncture (WA). Studies demonstrate that acupuncture is a relatively safe alternative to laxatives that effectively alleviates gastrointestinal and neurological symptoms in patients (Wang et al., 2015; Liu et al., 2016; Pei et al., 2020; Lu et al., 2022; Zheng et al., 2022). Moreover, electrophysiology studies have shown that acupuncture regulates autonomic nerves and gastrointestinal hormones by transmitting signals from somatic stimulation to the central nervous system via the upper spinal cord, thereby affecting gastrointestinal tract function (Takahashi, 2013).
Clearly, acupuncture may be an effective and safe complementary and alternative therapy to improve PSC. Previous meta-analyses (Yang et al., 2014; Tang et al., 2020) have investigated the therapeutic effects of acupuncture on PSC, but their conclusions require further validation because of deficiencies in outcome indicators, included literature, and controls for confounding factors. Therefore, to further confirm the efficacy and safety of the treatment, we conducted a comprehensive evaluation of the available clinical evidence on the latest randomized clinical trial (RCT) data of acupuncture for PSC.
The protocol for this systematic review and meta-analysis was registered in PROSPERO (No. CRD42023425087; https://www.crd.york.ac.uk/PROSPERO/), and followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Page et al., 2021).
Two researchers (STY and WKY) independently searched PubMed, EMBASE, Cochrane Library, Web of Science, Chinese National Knowledge Infrastructure (CNKI), SinoMed, Chinese Science and Technique Journals Database (VIP), Wanfang Database, and two clinical trial registries (ClinicalTrials.gov and the Chinese Clinical Trial Registry) from study inception to May 9, 2023. The language restriction was English and Chinese. The search terms were “Constipation” “Dyschezia” “Colonic Inertia” “Astriction” “Stroke” “Cerebral Infarction” “Cerebral Hemorrhage” “Cerebrovascular Disorders” “Post stroke constipation” “Acupuncture” “Electroacupuncture” “Dry Needling” “Moxibustion” “Integrated Chinese and western medicine” “Complementary Therapies” and related terms. We also consulted citations from relevant systematic reviews. Details of the search strategies were shown in Supplementary File S1.
Prospective parallel RCTs of acupuncture for the treatment of PSC.
Participants diagnosed with PSC, without gender or age restrictions. Stroke was diagnosed by Magnetic Resonance Imaging or Computed Tomography scan, and constipation was diagnosed by Rome II, Rome III, Rome IVcriteria, diagnostic and curative effect standard of Chinese medicine disease and syndrome, or the guiding principles for clinical research of new Chinese medicine (The State Administration of Traditional Chinese Medicine, 1994; Drossman, 1999, 2006, 2016; Zheng, 2002).
The experimental group received acupuncture as monotherapy or as an adjunct to conventional treatment (CT), including manual acupuncture (MA), electroacupuncture (EA), warm-acupuncture (WA), moxibustion, dry needling, auricular acupuncture, and laser acupuncture, etc.
Participants in the control group were treated with CT or sham acupuncture. Conventional treatment was limited to fiber, osmotic laxatives (e.g., polyethylene glycol, lactulose, magnesium oxide), stimulant laxatives (e.g., senna, sodium picosulfate, bisacodyl), gastrointestinal prokinetic drugs (e.g., prucalopride, cisapride, mosapride), and secretagogues (e.g., lubiprostone, linaclotide, plecanatide). There were no restrictions on dosage, route of administration, or treatment duration.
The included studies reported at least one primary outcome of total responder rate and constipation symptom score. The secondary outcomes included time to first bowel movement (BM), serum vasoactive intestinal peptide (VIP) levels, serum P substance (SP) levels, Bristol Stool Scale (BSS) score, and adverse events (AEs).
The total responder rate was defined as the proportion of patients whose symptoms improved, and we accepted the definitions reported in each study. The constipation symptom score referred to the Constipation Symptoms Scale designed by Anorectal Surgery Group of the Chinese Medical Association’s Surgery Branch (2005); the scale considers criteria of difficulty in defecation, duration of defecation, BSS score, incomplete defecation, frequency of defecation, and bloating.
We excluded the following studies: (1) studies with other Chinese medicine treatments, such as Chinese herbs, massage, acupoint injection, auricular acupressure, scraping, cupping, and catgut embedding therapy, and trials that compared different acupuncture types; (2) studies with incomplete or incorrect data; (3) studies involving patients with disorders of consciousness, cognitive impairment, or serious diseases of the heart, liver, and kidney hematopoietic system; (4) studies without full-text availability.
Two researchers (WKY and LLL) independently screened the titles, abstracts, and full texts of the retrieved studies for eligibility and independently extracted the data of the final included literature. Disagreements were resolved by mutual negotiation or by consultation with a third researcher (STY). The following information was extracted: authors, publication year, general information, participants’ characteristics, details of interventions (type of acupuncture, acupoints, frequency, duration of treatment, retention time of acupuncture), and outcomes.
Two researchers (ZL and ZM) independently assessed the methodological quality of the included studies using the Cochrane Risk of Bias Tool 2.0 (RoB 2.0) (Sterne et al., 2019), which contains six aspects: randomization, deviations from the intended interventions, missing outcome data, measurement of the outcome, selective outcome reporting, and overall bias. Each aspect was evaluated as “low risk of bias,” “some concerns,” or “high risk of bias.” Disagreements were resolved by mutual negotiation or by consultation with a third researcher (YSY).
Two researchers (YMY and WJ) independently evaluated the reporting quality of interventions in each study with the Revised Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA) (MacPherson et al., 2010). The revised STRICTA consists of six items: acupuncture rationale, details of needling, treatment regimen, other components of treatment, practitioner background, and control intervention. Disagreements were resolved by mutual negotiation or by consultation with a third researcher (STY).
All statistical analyses were conducted using Review Manager 5.4 and Stata 15.1 software. Dichotomous outcomes were expressed as the risk ratio (RR) with 95% confidence interval (CI), while continuous outcomes were expressed as standardized mean difference (SMD) with 95% CI (Murad et al., 2019). Heterogeneity was assessed by the χ2 test and the I2 statistic (Higgins et al., 2019). The fixed-effect model was used in cases with low heterogeneity (p > 0.1, I2 < 50%), and the random-effect model was applied in cases with substantial heterogeneity (p ≤ 0.1, I2 ≥ 50%) (Higgins et al., 2019; Murad et al., 2019).
Sensitivity analysis was conducted by excluding individual studies to investigate the stability of the results. Subgroup analysis was conducted to investigate the potential causes of heterogeneity with four prespecified aspects: (1) treatment duration (<2 weeks, ≥2 weeks); (2) acupuncture frequency (<1 time/day, ≥1 time/day); (3) needle retention time (<30 min, ≥30 min); (4) types of control interventions (osmotic laxatives, stimulant laxatives, gastrointestinal prokinetic drugs, secretagogues). In addition, a funnel plot and Egger’s test were applied to evaluate publication bias when the number of included studies was more than 10, and the trim-and-fill method was used to explore whether publication bias impacted the results. Descriptive analysis was performed if the data were not suitable for meta-analysis.
The GRADE (Grading of Recommendations Assessment, Development and Evaluatio) system (Liu, 2022) was used to rank the quality of evidence in five downgrading domains: risk of bias, inconsistency, indirectness, imprecision, and publication bias. The quality of evidence was classified into four grades: high, moderate, low, or very low.
A total of 2,966 publications were retrieved from the eight databases and two clinical trial registries, and 1,413 duplicate publications were eliminated. After a review of the titles and abstracts, 1,409 publications were excluded, leaving 144 publications for secondary assessment. After reading the full text, 114 studies were eliminated (reasons for exclusion are shown in Supplementary Table S1), leaving 30 studies for inclusion (Zhou and Wang, 2001; Li and Song, 2005; Liu et al., 2008; Wang et al., 2008, 2019, 2021; Zhang et al., 2008, 2015; Cao and Sun, 2009; Shi, 2009; Zhu and Chen, 2010; Tian and Wang, 2012; Man, 2014; Yuan et al., 2014, 2021; Ma and Li, 2015; Song and Liu, 2015; Xie et al., 2016; Zhang, 2016; Gao et al., 2017; Li et al., 2018; Liu Q. et al., 2018; Liu Z. et al., 2018; Yang, 2018; Guan, 2019; Luo, 2019; Lu et al., 2020; Wu et al., 2020; Liu and Wang, 2022; Tian, 2022; Zhong et al., 2022; Figure 1).
Thirty RCTs were included in the systematic review and meta-analysis. The 30 RCTs enrolled a total of 2,220 participants (n = 1,125 and n = 1,095 from the intervention and control groups, respectively), with sample sizes ranging from 40 to 110. All trials were single-center RCTs conducted in China and published in Chinese from 2001 to 2022. Twenty-seven studies (Zhou and Wang, 2001; Li and Song, 2005; Liu et al., 2008; Wang et al., 2008, 2019, 2021; Zhang et al., 2008, 2015; Cao and Sun, 2009; Shi, 2009; Tian and Wang, 2012; Man, 2014; Yuan et al., 2014; Ma and Li, 2015; Song and Liu, 2015; Xie et al., 2016; Zhang, 2016; Gao et al., 2017; Li et al., 2018; Liu Q. et al., 2018; Liu Z. et al., 2018; Yang, 2018; Guan, 2019; Luo, 2019; Wu et al., 2020; Liu and Wang, 2022; Tian, 2022; Zhong et al., 2022) were two-armed, while three studies (Zhu and Chen, 2010; Lu et al., 2020; Yuan et al., 2021) were three-armed. Of the three-arm studies, two (Zhu and Chen, 2010; Yuan et al., 2021) compared low stimulus vs. high stimulus vs. CT, and one (Lu et al., 2020) compared Tianshu (ST25) vs. Zhigou (SJ6) vs. CT.
Eleven studies compared MA with CT, six trials compared EA with CT, three trials compared WA with CT, one trial compared moxibustion vs. CT, seven trials compared MA plus CT vs. CT, and two trials compared moxibustion plus CT vs. CT. Control interventions included osmotic laxatives (polyethylene glycol, lactulose), stimulant laxatives (senna, bisacodyl, phenolphthalein), and gastrointestinal prokinetic drugs (cisapride). Table 1 displays the characteristics of the 30 studies.
Eighteen studies (Zhang et al., 2008, 2015; Cao and Sun, 2009; Shi, 2009; Man, 2014; Yuan et al., 2014, 2021; Xie et al., 2016; Gao et al., 2017; Li et al., 2018; Liu Q. et al., 2018; Liu Z. et al., 2018; Yang, 2018; Guan, 2019; Lu et al., 2020; Wang et al., 2021; Liu and Wang, 2022; Tian, 2022; Zhong et al., 2022) used MA, six studies (Zhou and Wang, 2001; Liu et al., 2008; Wang et al., 2008, 2019; Tian and Wang, 2012; Luo, 2019) used EA, three studies (Li and Song, 2005; Song and Liu, 2015; Zhang, 2016) used WA, and three studies (Zhu and Chen, 2010; Ma and Li, 2015; Wu et al., 2020) used moxibustion. The frequency of treatment ranged from 5 to 7 sessions per week for a 1–7 week duration of treatment. Retention times ranged from 15 to 120 min. Twenty-five studies (Zhou and Wang, 2001; Li and Song, 2005; Liu et al., 2008; Wang et al., 2008, 2019; Zhang et al., 2008, 2015; Cao and Sun, 2009; Shi, 2009; Zhu and Chen, 2010; Tian and Wang, 2012; Yuan et al., 2014, 2021; Ma and Li, 2015; Xie et al., 2016; Zhang, 2016; Gao et al., 2017; Li et al., 2018; Liu Q. et al., 2018; Liu Z. et al., 2018; Yang, 2018; Luo, 2019; Lu et al., 2020; Wu et al., 2020; Liu and Wang, 2022; Zhong et al., 2022) applied fixed treatment protocols, three studies (Man, 2014; Song and Liu, 2015; Wang et al., 2021) applied individualized treatment protocols (fixed acupoints combined with acupoints based on symptoms and syndrome differentiation of Chinese medicine), and two (Guan, 2019; Tian, 2022) reported only representative acupoints. The most common acupoints were Tianshu (ST25), Zusanli (ST36), Qihai (RN6), Zhigou (SJ6), Zhongwan (RN12), Taichong (LR3), Shangjuxu (ST37), Neiguan (PC6), Danzhong (RN17), and Guanyuan (RN4). Frequency ranking of acupoints is shown in Supplementary Table S2.
The reporting quality of trial treatment protocols was evaluated by STRICTA with 17 items. As shown in Supplementary Figure S1, nearly all trials reported item 1a (acupuncture rationale), item 1b (reasoning for acupuncture treatment), item 3a (number of treatment sessions), item 3b (frequency and duration of treatment sessions), and item 6b (precise description of the control group). No studies mentioned item 4b (setting and context of treatment) and item 5 (acupuncturist’s background). The STRICTA checklist is provided in Supplementary Table S3.
Regarding randomization, 16 studies (Wang et al., 2008, 2019, 2021; Zhang et al., 2008, 2015; Shi, 2009; Tian and Wang, 2012; Man, 2014; Yuan et al., 2014, 2021; Ma and Li, 2015; Gao et al., 2017; Luo, 2019; Lu et al., 2020; Tian, 2022; Zhong et al., 2022) provided a sufficient randomized sequence generation process. In addition, one study (Ma and Li, 2015) used consecutively numbered, opaque, sealed envelopes for allocation concealment and was evaluated as low risk. The remaining studies did not provide specific details of allocation concealment, and therefore we evaluated the risk of bias as unclear. Regarding deviations from the intended interventions, due to the specificity of acupuncture therapy, one study (Gao et al., 2017) implemented blinding of therapists, and the remaining 29 studies did not report the implementation of blinding. With respect to missing outcome data, one study (Ma and Li, 2015) reported missing visits but did not perform an intention-to-treat approach, which may affect the true outcome. The remaining 29 studies had no missing data, so we evaluated the risk of bias as low. Regarding outcome measurement, one study (Gao et al., 2017) implemented blinding of outcome assessors, and the remaining 29 studies did not mention the implementation of blinding. Regarding selective outcome reporting, the expected outcomes of all studies are fully reported. The risk of bias for all trials is shown in Figure 2.
Nineteen studies compared the total responder rates for acupuncture and CT, and the random-effects model was used for the meta-analysis because of the high heterogeneity among studies (p < 0.0001, I2 = 64%). We found that acupuncture was superior to CT in total responder rate (RR 1.16, 95% CI: 1.09–1.25, p < 0.0001), and sensitivity analysis revealed that results were robust against the exclusion of any one study (Supplementary Figure S2A). Furthermore, we conducted a subgroup meta-analysis to determine if treatment duration influences the efficacy of acupuncture treatment; we found that acupuncture treatment durations of <2 weeks did not offer a benefit, while treatment durations ≥2 weeks were more effective. Notably, the difference in interaction effect between these two subgroups was highly significant. These results indicate an optimal treatment duration of ≥2 weeks (Figure 3).
We also conducted subgroup analyses of the effects of acupuncture frequency (< 1 time/day, ≥ 1 time/day), needle retention time (time < 30 min, time ≥ 30 min, not reported), and the types of control interventions (OL, SL, GP) on the efficacy of acupuncture. We found that most subgroups were consistent with the overall findings, suggesting that the acupuncture frequency and types of medication did not significantly influence the positive effect of acupuncture in treating PSC. However, within the subgroup analysis in which needle retention time was not mentioned, acupuncture was not superior to CT (RR: 1.17, 95% CI: 0.87–1.58, p = 0.31) (Figure 4).
Nine studies compared the total responder rate for acupuncture plus CT vs. CT, and the fixed-effects model was used because there was no heterogeneity among the studies (p = 0.58, I2 = 0%). We found that acupuncture plus CT was superior to CT regarding total responder rate (RR: 1.26, 95% CI: 1.17 to 1.35, p < 0.00001) (Figure 5), and sensitivity analysis revealed that results were robust against the exclusion of any one study (Supplementary Figure S2B).
In addition, we conducted subgroup analyses based on acupuncture frequency (<1 time/day, ≥1 time/day), treatment duration (<2 weeks, ≥2 weeks), needle retention time (time < 30 min, time ≥ 30 min, not reported), and the types of control interventions (OL, SL) to determine the influence of these characteristics on the efficacy of acupuncture. We found that all subgroups were consistent with the overall findings, suggesting that these characteristics did not significantly affect the positive effect of acupuncture in treating PSC (Figure 6).
Seven studies compared constipation symptom scores for acupuncture vs. CT, and the fixed-effects model was used because of the low heterogeneity among the studies (p = 0.11, I2 = 42%). As shown in Figure 7, acupuncture reduced constipation symptom scores to a greater extent than did CT (SMD: -0.65, 95% CI: −0.83 to −0.46, p < 0.00001), and sensitivity analysis revealed that results were robust against the exclusion of any one study (Supplementary Figure S2C).
Three studies compared the time to first BM for acupuncture vs. CT, and the random-effects model was used because of the high heterogeneity among the studies (p < 0.0001, I2 = 90%). As shown in Figure 8A, acupuncture resulted in a greater reduction in the time to first BM than did CT (SMD: –1.19, 95% CI: −2.13 to −0.25, p = 0.01). Sensitivity analysis revealed that heterogeneity decreased significantly (p = 0.42, I2 = 0%) after removing the study by Guan (2019), which did not describe detailed methods for generating random sequences, thus leading to methodological heterogeneity.
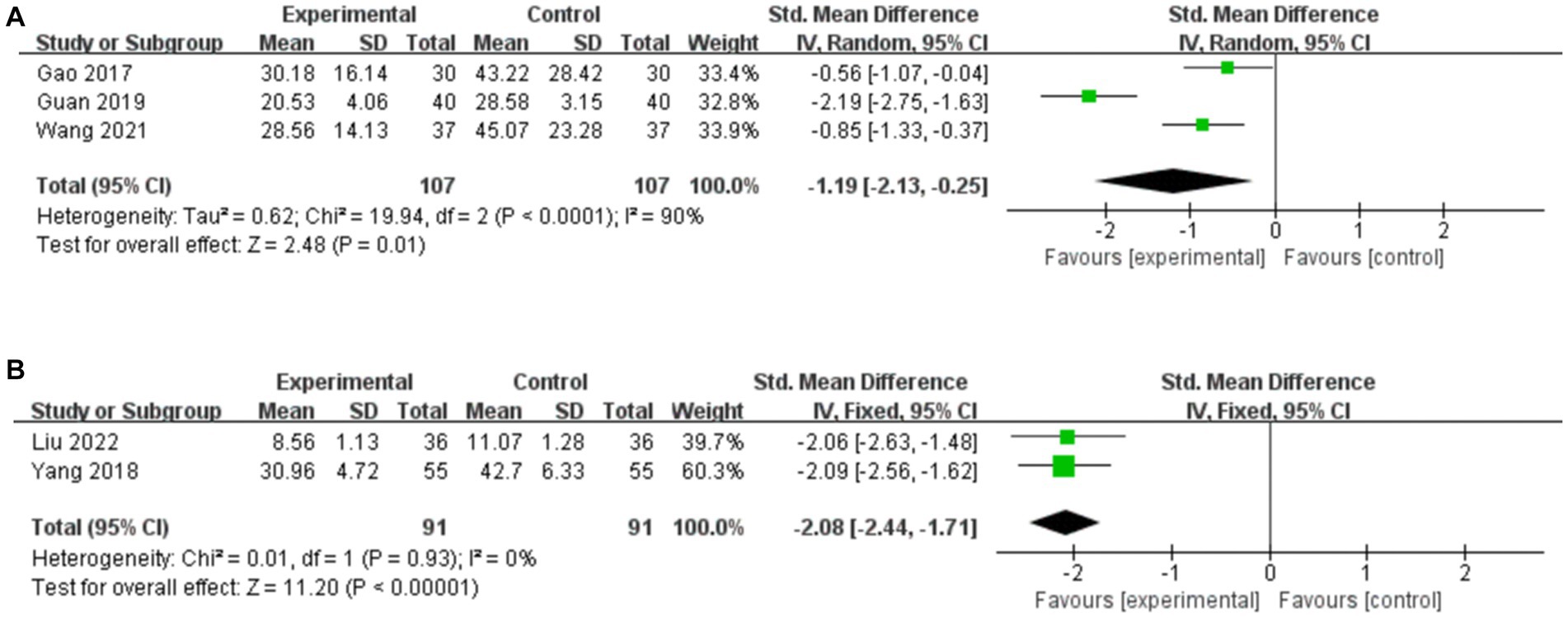
Figure 8. Forest plot of the time to first BM. (A) Acupuncture vs. CT. (B) Acupuncture plus CT vs. CT.
Two studies compared the time to first BM for acupuncture plus CT vs. CT, and the fixed-effects model was used because there was no heterogeneity among the studies (p = 0.93, I2 = 0%). As shown in Figure 8B, acupuncture plus CT resulted in a greater reduction in the time to first BM than did CT (SMD: –2.08, 95% CI: −2.44 to −1.71, p < 0.00001).
Three studies compared serum VIP levels for acupuncture vs. CT, and the random-effects model was used because of the high heterogeneity among the studies (p < 0.00001, I2 = 95%). As shown in Figure 9A, acupuncture resulted in a greater reduction in serum VIP levels than did CT (SMD: –2.11, 95% CI: −3.83 to −0.38, p = 0.02). Sensitivity analysis revealed that heterogeneity decreased significantly (p = 0.28, I2 = 15%) after removing the study by Lu et al. (2020), which did not include the Tianshu acupoint, thus leading to clinical heterogeneity.
Three studies compared serum VIP levels for acupuncture plus CT vs. CT, and the random-effects model was used because of the high heterogeneity among the studies (p = 0.04, I2 = 68%). As shown in Figure 9B, acupuncture plus CT resulted in a greater reduction in the serum level of VIP compared to CT (SMD: -1.71, 95% CI: −2.24 to −1.18, p < 0.00001). Sensitivity analysis demonstrated that the heterogeneity was significantly decreased (p = 0.45, I2 = 0%) after removing the studies by Li et al. (2018).
Three studies compared serum SP levels for acupuncture vs. CT, and the random-effects model was used because of the high heterogeneity among the studies (p < 0.00001, I2 = 94%). As shown in Figure 10A, we found that acupuncture was superior to CT in increasing serum levels of SP (SMD: 1.92, 95% CI: 0.47–3.36, p = 0.009). However, the sensitivity analysis demonstrated that the result for serum SP level was no longer significant (SMD: 2.13, 95% CI: −0.60 to 4.86, p = 0.13) after removing the study by Lu et al. (2020), suggesting that the conclusion is not stable.
Two studies compared serum SP levels for acupuncture plus CT vs. CT, and the random-effects model was used because there was no heterogeneity among the studies (p = 0.59, I2 = 0%). As shown in Figure 10B, we found that acupuncture plus CT was superior to CT in increasing serum SP levels (SMD: 2.00, 95% CI: 1.65–2.35, p < 0.00001).
Three studies compared the BSS score for acupuncture vs. CT, and the fixed-effects model was used because of the low heterogeneity among the studies (p = 0.15, I2 = 48%). As shown in Figure 11A, acupuncture did not result in a greater reduction in the BSS score compared to CT (SMD: 0.28, 95% CI: −0.02 to 0.58, p = 0.07). Sensitivity analysis revealed that heterogeneity decreased significantly (p = 0.81, I2 = 0%) after removing the study by Yuan et al. (2021), which used the diagnostic criteria of Rome III, leading to clinical heterogeneity.
Two studies compared the BSS score for acupuncture plus CT vs. CT, and the random-effects model was used because of the high heterogeneity among the studies (p = 0.06, I2 = 72%). As shown in Figure 11B, acupuncture plus CT resulted in a greater reduction in the BSS score than did CT (SMD: –2.48, 95% CI: −3.22 to −1.73, p < 0.00001).
Thirteen studies reported AEs, of which four (Zhang et al., 2015; Gao et al., 2017; Liu Q. et al., 2018; Liu Z. et al., 2018; Liu and Wang, 2022) reported no AEs in either the experimental or control group. The primary AEs in the medication group were abdominal pain, diarrhea, nausea, vomiting, and abdominal bloating, while the primary AEs in the acupuncture treatment group were fainting during acupuncture.
Eight studies compared AEs for acupuncture vs. CT, and the fixed-effects model was used because there was no heterogeneity among the studies (p = 0.97, I2 = 0%). As shown in Figure 12A, acupuncture resulted in a greater reduction in the incidence of AEs compared to CT (RR: 0.13, 95% CI: 0.06–0.26, p < 0.00001), and sensitivity analysis revealed the robustness of the conclusions (Supplementary Figure S2D).
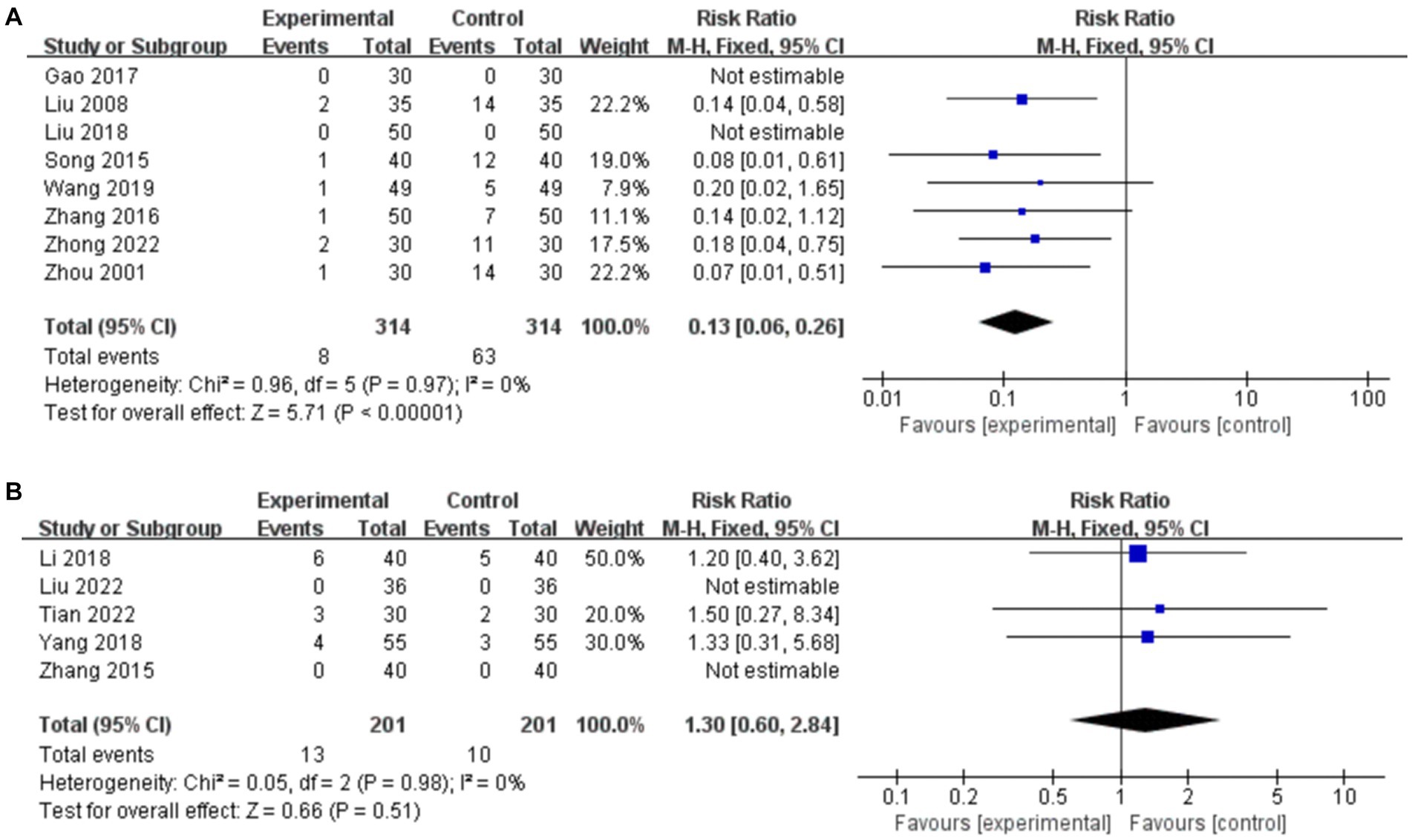
Figure 12. Forest plot of the incidence of AEs. (A) Acupuncture vs. CT. (B) Acupuncture plus CT vs. CT.
Five studies compared AEs for acupuncture plus CT vs. CT, and the fixed-effects model was used because there was no heterogeneity among the studies (p = 0.98, I2 = 0%). As shown in Figure 12B, acupuncture plus CT did not result in a greater reduction in the incidence of AEs than did CT (RR: 1.30, 95% CI: 0.60–2.84, p = 0.51), and sensitivity analysis revealed the robustness of the conclusions (Supplementary Figure S2E).
The plot of acupuncture vs. CT on total responder rate was visibly asymmetric (Figure 13A), and Egger’s test revealed potential publication bias (Egger’s test p = 0.001) (Figure 13B). We conducted trim-and-fill test analysis to assess the effect of publication bias on the interpretation of the results, and we found that this publication bias did not affect the estimates, although several RCTs showing negative findings remained unpublished (Supplementary Table S4).
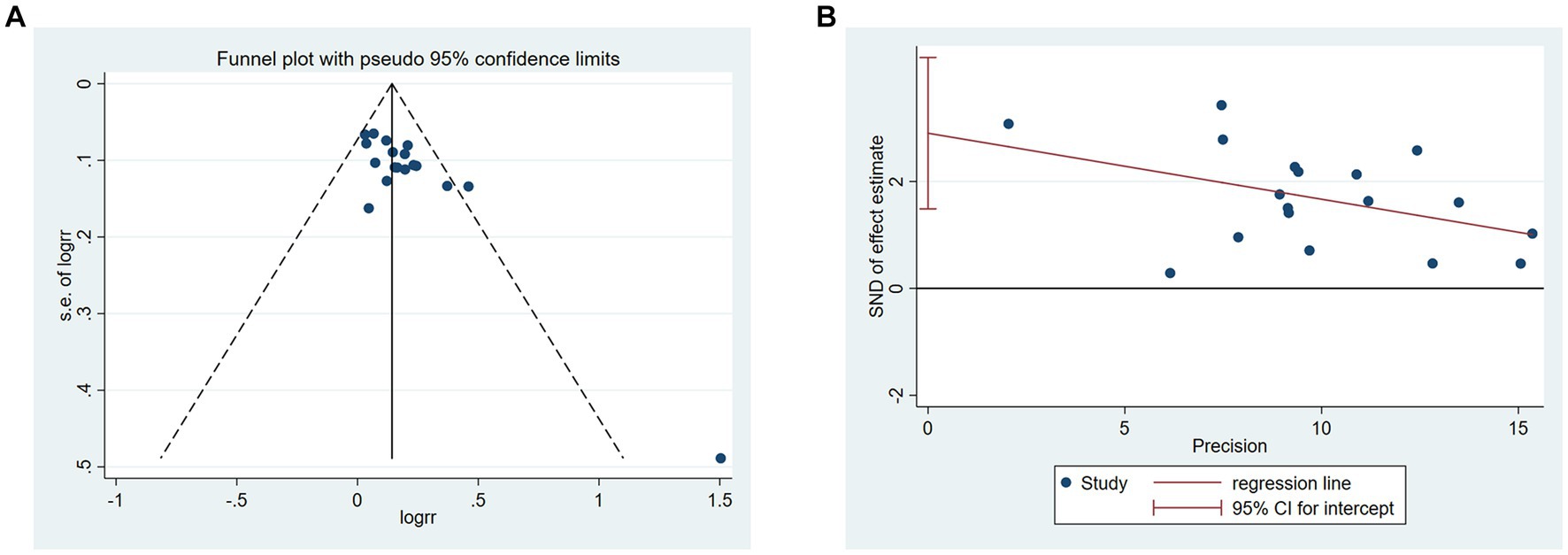
Figure 13. Publication bias of acupuncture vs. CT in the total responder rate. (A) Funnel plots. (B) Egger’s test.
The certainty of evidence for the meta-analysis was evaluated by GRADE. The quality of evidence ranged from very low to high (Table 2). The primary reasons for downgrading were inconsistency (high heterogeneity) and imprecision (small sample size).
In this study, a total of 30 RCTs involving 2,220 (1,125/1,095) patients were included to systematically evaluate the efficacy and safety of acupuncture treatments for PSC. We found that both acupuncture and acupuncture plus CT offer significant benefits over CT on metrics of total responder rate, serum SP levels, time to first BM, and serum VIP levels. Acupuncture was also superior to CT in reducing constipation symptom scores, but the level of evidence was very low to high because of potential publication bias and heterogeneity. Acupuncture operates by multiple mechanisms.
Acupuncture operates by multiple mechanisms. Clinical studies (Xiong et al., 2014; Chen et al., 2022) demonstrate that acupuncture regulates autonomic function by increasing vagal activity and inhibiting sympathetic activity, thereby affecting the central nervous system and reflex pathways involved in defecation. The treatment rebalances inhibitory and excitatory gastrointestinal hormone levels to promote colonic motility, shorten colonic transit time, and improve constipation symptoms. Xu et al. (2020) observed that in patients with functional constipation, compared with mosapride & sham EA group and mosapride control group, EA significantly increased the weekly spontaneous bowel movements, improved stool consistency, and reduced the intensity of defecating difficulty. Meanwhile, it also ameliorated the quality-of-life scores, and there were no serious adverse events during the course of the study. The potential mechanisms of acupuncture stimulation in promoting gastrointestinal function were studied more deeply in animal experiments. Studies have confirmed that acupuncture not only regulates the level of hormones related to intestinal motility (Zhu et al., 2016; Jang et al., 2017), but also improves the morphologic structure of colonic smooth muscle (He et al., 2023), and rebalances the gut microbiota (Xu et al., 2023). Wang et al. (2023) found that acupuncture could improve enteric glial cells autophagy by inhibiting PI3K/AKT/mTOR signaling. Moreover, acupuncture could restore gastrointestinal basic electrical rhythm by increasing the number of interstitial cells of Cajal (He et al., 2023).
Notably, the two interventions differed in the degree of improvements in BSS scores and AEs. Regarding BSS scores, acupuncture offered no significant advantage over CT, while acupuncture plus CT was superior to CT, which is consistent with previous findings (Zheng et al., 2018; Wang et al., 2020; Liu et al., 2021) and may result from direct action on the intestines that changes stool consistency to facilitate defecation (Chang et al., 2022, 2023). In contrast, acupuncture operates through a series of neurological and endocrine mechanisms to improve gastrointestinal tract function, and we found that acupuncture synergizes well with CT to effectively improve stool consistency, even though short-term treatment with acupuncture alone does not offer relief. Regarding safety, acupuncture alone was superior to CT, but there was no significant difference when comparing acupuncture plus CT vs. CT. It is clear that acupuncture does not cause serious AEs as a monotherapy or an adjunctive therapy.
We evaluated the effects of treatment duration, acupuncture frequency, types of control interventions, and needle retention time on total responder rates, which are relevant to clinical practice. We found that acupuncture significantly improves total responder rate with all studied treatment frequencies, control interventions, and defined needle retention times, and is effective as a monotherapy or an adjunctive therapy. Notably, though, acupuncture therapy was not found effective with uncertain needle retention time. Moreover, subgroup meta-analysis revealed that treatment durations of >2 weeks may be more effective than shorter treatment regiments at improving total responder rate. Furthermore, we evaluated acupuncture treatment regimens using STRICTA and summarized commonly used acupoints, providing scientific guidance for clinical practice and for the design and implementation of clinical studies. A total of 51 acupoints with frequencies ranging from 1 to 23 were used; the most commonly used acupoints for PSC were Tianshu (ST25), Zusanli (ST36), Qihai (RN6), and Zhigou (SJ6).
Because of the high heterogeneity of meta-analysis results, we performed sensitivity analysis and subgroup analysis to explore and eliminate sources of heterogeneity. We found that heterogeneity in total responder rates resulted from the inconsistency of treatment duration, while the heterogeneity in serum VIP levels resulted from differences in therapeutic acupoints. The source of heterogeneity in the time to first BM resulted from the higher risk of overall bias in the included studies, and the source of heterogeneity in the BSS score resulted from differences in diagnostic criteria. Some outcome indicators were still highly heterogeneous after our corrections, meaning that additional studies are needed to determine if acupuncture plus CT can improve serum VIP levels and if acupuncture can increase serum SP levels.
Compared to previous studies, our study has several strengths. First, we found that treatment duration may influence efficacy, thus providing a reference for clinical practice and clinical research. Second, we have adopted updated and objective constipation-related indicators such as time to first BM and serum gastrointestinal peptide levels to evaluate the effects of acupuncture, further supporting the use of acupuncture in treating PSC. Third, we enhanced the credibility of our results by using sensitivity analyses and subgroup analyses to explore the sources of heterogeneity, the robustness of the results, and the effects of some characteristics on the efficacy of acupuncture. Fourth, the STRICTA checklist and GRADE were used to assess clinical trial reporting quality and evidence quality, respectively. Finally, to minimize heterogeneity in the included studies, we limited the types of control interventions used and we excluded co-treatment with herbal formulas, Chinese patent medicines, and acupressure.
Some limitations in this work should be noted. First, there are no standardized diagnostic criteria for PSC, and the different Rome diagnostic criteria (e.g., Rome II vs. Rome IV) may affect the assessment of acupuncture efficacy. Second, all included studies were conducted in China, and the conclusions of our study must be verified in patients of other races. Third, the strength of our conclusions may be limited by small sample sizes, poor methodological quality (e.g., some of the included studies did not describe the randomization methodology and allocation concealment in detail), and the potential risk of bias. Fourth, most of the included studies do not report complete acupuncture details according to the STRICTA checklist, which may lead to bias in the interpretation of results. Fifth, Differences in gender and age of patients in RCTs, as well as in interventions in the control group, may lead to a risk of bias that reduces the credibility of the findings, so we should be cautious about the conclusions. Finally, we were unable to compare acupuncture vs. sham acupuncture, and the long-term effects of acupuncture, because of the limited number of studies and follow-up data.
Our meta-analysis suggests that acupuncture has great potential for the treatment of PSC and deserves further exploration. First, we found that 2 weeks may be the minimum effective treatment duration for acupuncture efficacy, though more research is needed to verify the robustness and scientific validity of this conclusion, as high-quality evidence is limited. Second, there are still few PSC trials that use sham acupuncture as a control treatment to eliminate the non-specific effects of acupuncture; future clinical studies should use sham acupuncture as a control. Third, the quality of future studies would be improved by standardizing study protocols, unifying diagnostic criteria, and improving the implementation of randomization, allocation concealment, and blinding. In addition, more scientific and objective outcome indicators such as complete spontaneous BMs and recurrence rates should be selected, and follow-up times should be extended. Finally, clinical studies should strictly follow the CONSORT 2010 statement (Schulz et al., 2010) and STRICTA (MacPherson et al., 2010) to improve reporting quality, especially regarding details of acupuncture treatments that are critical for the accuracy of results. More reliable guidance for clinical practice would be provided by large, high-quality, multicenter, double-blinded RCTs that comprehensively assess the efficacy and safety of acupuncture and identify efficient and rational treatment protocols.
Acupuncture alone or as an adjunctive treatment for PSC is superior to CT in terms of efficacy and safety, indicating that acupuncture is a potential alternative therapy for PSC. However, because the evidence quality in this study is unstable, more well-designed long-term follow-up RCTs are needed to evaluate acupuncture efficacy and safety.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
TS: Conceptualization, Data curation, Formal analysis, Investigation, Project administration, Resources, Validation, Visualization, Writing – original draft. KW: Data curation, Formal analysis, Investigation, Resources, Validation, Visualization, Writing – original draft. LL: Data curation, Investigation, Resources, Writing – original draft. MY: Data curation, Investigation, Writing – original draft. LZ: Data curation, Investigation, Writing – original draft. MZ: Data curation, Investigation, Writing – original draft. SY: Data curation, Investigation, Writing – original draft. JW: Data curation, Investigation, Writing – original draft. JL: Conceptualization, Funding acquisition, Project administration, Supervision, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by the Fundamental Research Funds for the Central Universities (2020-JYB-ZDGG-131) and Beijing-Tianjin-Hebei Chinese Medicine Collaborative Development Program (GZY-GCS-2017-0).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnins.2023.1275452/full#supplementary-material
Anorectal Surgery Group of the Chinese Medical Association’s Surgery Branch (2005). Evaluation of constipation symptoms and efficacy. Chin. J. Gastrointes. Surg. 4:355.
Camilleri, M. (2021). Gastrointestinal motility disorders in neurologic disease. J. Clin. Invest. 131:e143771. doi: 10.1172/JCI143771
Cao, T., and Sun, Y. (2009). Acupuncture treatment of post-stroke constipation in 30 cases. Shaanxi J Trad Chin Med 30, 199–200.
Carabotti, M., Scirocco, A., Maselli, M. A., and Severi, C. (2015). The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Ann. Gastroenterol. 28, 203–209.
Chang, L., Chey, W. D., Imdad, A., Almario, C. V., Bharucha, A. E., Diem, S., et al. (2023). American Gastroenterological Association-American College of Gastroenterology clinical practice guideline: pharmacological management of chronic idiopathic constipation. Gastroenterology 164, 1086–1106. doi: 10.1053/j.gastro.2023.03.214
Chang, L., Sultan, S., Lembo, A., Verne, G. N., Smalley, W., and Heidelbaugh, J. J. (2022). AGA clinical practice guideline on the pharmacological Management of Irritable Bowel Syndrome with Constipation. Gastroenterology 163, 118–136. doi: 10.1053/j.gastro.2022.04.016
Chen, B. L., Zhong, C. L., Li, Y., and Zhang, B. P. (2022). Application of acupuncture in inhibiting intestinal peristalsis in colonoscopy. Zhongguo Zhen Jiu 42, 799–802. doi: 10.13703/j.0255-2930.20210620-k0002
Drossman, D. A. (1999). The functional gastrointestinal disorders and the Rome II process. Gut 45, ii1–ii5. doi: 10.1136/gut.45.2008.ii1
Drossman, D. A. (2006). The functional gastrointestinal disorders and the Rome III process. Gastroenterology 130, 1377–1390. doi: 10.1053/j.gastro.2006.03.008
Drossman, D. A. (2016). Functional gastrointestinal disorders: history, pathophysiology, clinical features and Rome IV. Gastroenterology. S0016-5085(16)00223-7 doi: 10.1053/j.gastro.2016.02.032
Gao, Y., Li, J., Su, M., and Li, Y. (2017). Acupuncture with smoothing liver and regulating qi for post-stroke slow transit constipation and its gastrointestinal hormone level. Chin Acupuncture Moxibust 37, 125–129. doi: 10.13703/j.0255-2930.2017.02.005
GBD 2019 Stroke Collaborators (2021). Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet Neurol. 20, 795–820. doi: 10.1016/S1474-4422(21)00252-0
Gilsenan, A., Fortuny, J., Cainzos-Achirica, M., Cantero, O. F., Flynn, R. W. V., Garcia-Rodriguez, L., et al. (2019). Cardiovascular safety of prucalopride in patients with chronic constipation: a multinational population-based cohort study. Drug Saf. 42, 1179–1190. doi: 10.1007/s40264-019-00835-0
Guan, P. (2019). Effectiveness of Shugan-Tiaoqi acupoint acupuncture in the treatment of slow transit constipation after stroke. Guide China Med 17:161. doi: 10.15912/j.cnki.gocm.2019.31.125
Harris, L. A., and Chang, C. H. (2022). Burden of constipation: looking beyond bowel movements. Am. J. Gastroenterol. 117, S2–S5. doi: 10.14309/ajg.0000000000001708
He, Y. Q., Liu, J. F., and Liu, H. X. (2023). Research progress on the mechanism of action of acupuncture in the treatment of slow-transmission constipation. Acupunct Res. 48, 411–414. doi: 10.13702/j.1000-0607.20211387
Higgins, J.P.T., Chandler, J., Cumpston, M., Li, T., Page, M.J., and Welch, V.A. (Eds) (2019). Cochrane handbook for systematic reviews of interventions. 2nd ed. Chichester, UK: John Wiley & Sons.
Jang, J. H., Lee, D. J., Bae, C. H., Ha, K. T., Kwon, S., Park, H. J., et al. (2017). Changes in small intestinal motility and related hormones by acupuncture stimulation at Zusanli (ST 36) in mice. Chin. J. Integr. Med. 23, 215–220. doi: 10.1007/s11655-016-2609-8
Li, H., Fu, C., Yan, L., and Li, H. (2018). Efficacy of Shugan-Tiaoqi acupoint acupuncture in the treatment of post-stroke slow-transmission constipation and its effect on oxidative stress indicators and gastrointestinal hormone levels. Modern J. Integr. Trad. Chin. Western Med. 27, 2120–2123.
Li, S., and Song, M. (2005). Observation on the efficacy of warm acupuncture in the treatment of post-stroke constipation. China Sci Technol Inform 9:139.
Lim, S. F., Ong, S. Y., Tan, Y. L., Ng, Y. S., Chan, Y. H., and Childs, C. (2015). Incidence and predictors of new-onset constipation during acute hospitalisation after stroke. Int. J. Clin. Pract. 69, 422–428. doi: 10.1111/ijcp.12528
Liu, J. P. (2022). GRADE methods in traditional medicine. Integr. Med. Res. 11:100836. doi: 10.1016/j.imr.2022.100836
Liu, Z., Ge, Y., Xu, F., Xu, Y., Liu, Y., Xia, F., et al. (2018). Preventive effects of transcutaneous electrical acustimulation on ischemic stroke-induced constipation mediated via the autonomic pathway. Am. J. Physiol. Gastrointest. Liver Physiol. 315, G293–G301. doi: 10.1152/ajpgi.00049.2018
Liu, Q., Huang, P., and Su, W. (2018). Comparison of effect of Shugan-Tiaoqi acupoint acupuncture and lactulose on chronic transmission constipation after stroke. Clin. J. Chin. Med. 10, 97–98.
Liu, B., and Wang, P. (2022). Efficacy of acupuncture assisted Western medicine in the treatment of patients with constipation of Yang deficiency type after stroke and its influence on quality of life. Reflexol. Rehabil. Med. 3, 57–61.
Liu, W., Wu, Q., Li, X., Tan, T., Shi, X., and Li, L. (2008). Observation on the therapeutic effect of electroacupuncture in the treatment of post-stroke constipation. J. Clin. Acupunct. Moxibust. 9, 17–18.
Liu, B., Wu, J., Yan, S., Zhou, K., He, L., Fang, J., et al. (2021). Electroacupuncture vs prucalopride for severe chronic constipation: a multicenter, randomized, controlled, noninferiority trial. Am. J. Gastroenterol. 116, 1024–1035. doi: 10.14309/ajg.0000000000001050
Liu, Z., Yan, S., Wu, J., He, L., Li, N., Dong, G., et al. (2016). Acupuncture for chronic severe functional constipation: a randomized trial. Ann. Intern. Med. 165, 761–769. doi: 10.7326/M15-3118
Lu, C., Zhang, H., Chen, S., and Zhang, L. (2020). The regulation mechanism and clinical observation of acupuncting Tianshu point deeply on the serum SP, VIP of constipation after apoplexy. World Sci. Technol. Modern. Trad. Chin. Med. 22, 2000–2005.
Lu, L., Zhang, Y., Tang, X., Ge, S., Wen, H., Zeng, J., et al. (2022). Evidence on acupuncture therapies is underused in clinical practice and health policy. BMJ 376:e067475. doi: 10.1136/bmj-2021-067475
Luo, Q. (2019). Analysis of the therapeutic effect of acupuncture on scalp point and foot transport sensory area on constipation after cerebrovascular disease. Yiyao Qianyan 9, 195–196.
Ma, Y., and Li, C. (2015). Clinical observalion to thunder-fire moxibustion therapy for stroke sequels period constipation type of qi deficiency. Chin. Med. Modern Distance Educ. China 13, 73–75.
MacPherson, H., Altman, D. G., Hammerschlag, R., Youping, L., Taixiang, W., White, A., et al. (2010). Revised STandards for reporting interventions in clinical trials of acupuncture (STRICTA): extending the CONSORT statement. PLoS Med. 7:e1000261. doi: 10.1371/journal.pmed.1000261
Man, B. (2014). Clinical efficacy of acupuncture in the treatment of post-stroke constipation in 49 cases. J. Med. Inform. 363–364. doi: 10.3969/j.issn.1006-1959.2014.17.407
Murad, M. H., Wang, Z., Chu, H., and Lin, L. (2019). When continuous outcomes are measured using different scales: guide for meta-analysis and interpretation. BMJ 364:k4817. doi: 10.1136/bmj.k4817
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., et al. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. doi: 10.1136/bmj.n71
Pei, L., Geng, H., Guo, J., Yang, G., Wang, L., Shen, R., et al. (2020). Effect of acupuncture in patients with irritable bowel syndrome: a randomized controlled trial. Mayo Clin. Proc. 95, 1671–1683. doi: 10.1016/j.mayocp.2020.01.042
Schulz, K. F., Altman, D. G., and Moher, D., Group, C (2010). CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMC Med. 8:18. doi: 10.1186/1741-7015-8-18
Shi, J. (2009). Clinical observations on the treatment of postapoplectic constipation by Back-Shu-front-mu- source point combination. Shanghai J. Acupunct. Moxibust. 28, 709–710.
Song, C., and Liu, L. (2015). Observation on the efficacy of warm acupuncture in the treatment of post-stroke constipation. All Health 9:40.
Sterne, J. A. C., Savovic, J., Page, M. J., Elbers, R. G., Blencowe, N. S., Boutron, I., et al. (2019). RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:l4898. doi: 10.1136/bmj.l4898
Su, Y., Zhang, X., Zeng, J., Pei, Z., Cheung, R. T., Zhou, Q. P., et al. (2009). New-onset constipation at acute stage after first stroke: incidence, risk factors, and impact on the stroke outcome. Stroke 40, 1304–1309. doi: 10.1161/STROKEAHA.108.534776
Sumida, K., Molnar, M. Z., Potukuchi, P. K., Thomas, F., Lu, J. L., Yamagata, K., et al. (2019). Constipation and risk of death and cardiovascular events. Atherosclerosis 281, 114–120. doi: 10.1016/j.atherosclerosis.2018.12.021
Takahashi, T. (2013). Effect and mechanism of acupuncture on gastrointestinal diseases. Int. Rev. Neurobiol. 111, 273–294. doi: 10.1016/B978-0-12-411545-3.00014-6
Tang, O. F., Huang, S. M., Ye, X. X., Liu, Q. X., Chen, T. T., and Zhan, C. J. (2020). Effect of acupuncture and moxibustion on post-stroke constipation: a network Meta-analysis. Zhongguo Zhen Jiu 40, 1011–1016. doi: 10.13703/j.0255-2930.20190717-k0008
The State Administration of Traditional Chinese Medicine. (1994). Efficacy criteria for diagnosis of TCM syndrome. Nanjing: Nanjing University Press.
Tian, T. (2022). Observation on the effect of Xiefei-Qingchang acupuncture in the treatment of excess constipation after stroke. Capital Med 29, 121–123. doi: 10.3969/j.issn.1005-8257.2022.05.050
Tian, X., and Wang, Q. (2012). Combination of scalp acupuncture and body acupuncture for the treatment of constipation after ischemic stroke in 30 cases. Guangxi J. Trad. Chin. Med. 35, 22–23.
Wang, L., Chen, Y., Xu, M. M., Cao, W., Zheng, Q. H., Zhou, S. Y., et al. (2023). Electroacupuncture alleviates functional constipation in mice by activating enteric glial cell autophagy via PI3K/AKT/mTOR Signaling. Chin. J. Integr. Med. 29, 459–469. doi: 10.1007/s11655-023-3594-3
Wang, Z., Liu, Z., Yang, M., and Liu, R. (2021). Treatment of post-stroke constipation with acupuncture at extra points combined with point selection based on syndrome differentiation. Jilin J. Chin. Med. 41, 119–122. doi: 10.13463/j.cnki.jlzyy.2021.01.032
Wang, X., Sun, Y., and Pan, C. (2019). Observations on the efficacy of He-Sea-front-mu point combination acupuncture for post-stroke constipation. Shanghai J Acupunct Moxibust 38, 714–717. doi: 10.13460/j.issn.1005-0957.2019.07.0714
Wang, D., Wang, S., Kong, L., Wang, W., and Cui, X. (2008). Clinical observation on abdominal electroacupuncture for treatment of poststroke constipation. Chin. Acupunct. Moxibust. 1, 7–9.
Wang, C. L. M., Wen, Q., and Li, N. (2015). Clinical observation of preventing and treating constipation by electroacupuncture intervention in ischemic stroke patients at acute stage. Chin Acupunct Moxibust 35, 430–434.
Wang, L., Xu, M., Zheng, Q., Zhang, W., and Li, Y. (2020). The effectiveness of acupuncture in Management of Functional Constipation: a systematic review and Meta-analysis. Evid. Based Complement. Alternat. Med. 2020:6137450. doi: 10.1155/2020/6137450
Wu, R., Shui, L., and Na, M. (2020). Clinical observation on the treatment of constipation in stroke by moxibustion of navel with Mongolian medicine. J. Med. Pharmacy Chin. Minorities 26, 26–27. doi: 10.16041/j.cnki.cn15-1175.2020.01.017
Xie, H., Xiong, Y., Li, Y., Cao, L., Yang, H., Jiang, S., et al. (2016). Therapeutic effect of abdominal acupuncture combined with body acupuncture of Zhuang medicine in the treatment of post-stroke constipation observed. J. Guangxi Univ. Chin. Med. 19, 22–23.
Xiong, F., Wang, Y., Li, S. Q., Tian, M., Zheng, C. H., and Huang, G. Y. (2014). Clinical study of electro-acupuncture treatment with different intensities for functional constipation patients. J. Huazhong Univ. Sci. Technolog. Med. Sci. 34, 775–781. doi: 10.1007/s11596-014-1351-8
Xu, K., Gao, X., Xia, G., Chen, M., Zeng, N., Wang, S., et al. (2021). Rapid gut dysbiosis induced by stroke exacerbates brain infarction in turn. Gut, gutjnl-2020-323263. doi: 10.1136/gutjnl-2020-323263
Xu, M. M., Guo, Y., Chen, Y., Zhang, W., Wang, L., and Li, Y. (2023). Electro-acupuncture promotes gut motility and alleviates functional constipation by regulating gut microbiota and increasing butyric acid generation in mice. J. Integr. Med. 21, 397–406. doi: 10.1016/j.joim.2023.05.003
Xu, X. H., Zhang, M. M., Wu, X., Xu, S. B., Wang, W., Zheng, C. H., et al. (2020). Efficacy of electro-acupuncture in treatment of functional constipation: a randomized controlled trial. Curr. Med. Sci. 40, 363–371. doi: 10.1007/s11596-020-2188-y
Yang, N. (2018). Efficacy of Shugan-Tiaoqi acupoint acupuncture in the treatment of post-stroke slow transmit constipation and its effect on gastrointestinal hormone levels. Modern J. Integr. Trad. Chin. Western Med. 27, 3488–3491.
Yang, J.P.L., J. Y.; Gu, H. Y., Lv, W. L., Zhao, H., and Li, G. P. (2014). Randomized controlled trials of acupuncture and moxibustion for post-stroke constipation: a meta analysis. Chin. Acupunct. Moxibust. 34, 833–836.
Yuan, H., Lin, L., Liu, K., and Yang, Z. (2021). Clinical observation on treatment of post-stroke constipation by acupuncture at Tianshu point with different stimulation acupuncture based on mild reinforcing-attenuating acupuncture. Yunnan J. Trad. Chin. Med. Materia Medica 42, 46–50. doi: 10.16254/j.cnki.53-1120/r.2021.02.015
Yuan, X., Wang, B., and Zhang, Y. (2014). Therapeutic observation of cluster needling at the middle line of vertex (MS 5) for post-stroke constipation. Shanghai J. Acupunct. Moxibust. 33, 988–989. doi: 10.13460/j.issn.1005-0957.2014.11.0988
Zhang, J. (2016). Evaluation on clinical effect of warming needle moxibustion for treating deficient constipation after apoplexy. Continuing Med. Educ. 30, 160–161.
Zhang, Y., Yuan, P., and Dong, G. (2008). Treatment of post-stroke constipation by scalp acupuncture of the foot motor sensory area in conjunction with the five-zang shu-points. J. Clin. Acupunct. Moxibust. 1, 20–21.
Zhang, H., Zhang, B., and Liu, R. (2015). Acupuncture combined polyethylene glycol in the treatment of hemorrhage stroke minimally invasive postoperative constipation random parallel control study. J. Pract. Trad. Chin. Internal Med. 29, 93–95. doi: 10.13729/j.issn.1671-7813.2015.05.46
Zheng, X. (2002). Guiding principles for clinical research of new TCM drugs (trial implementation) Beijing: China Medical Science and Technology Press.
Zheng, H., Gao, T., Zheng, Q. H., Lu, L. Y., Hou, T. H., Zhang, S. S., et al. (2022). Acupuncture for patients with chronic tension-type headache: a randomized controlled trial. Neurology. doi: 10.1212/WNL.0000000000200670
Zheng, H., Liu, Z. S., Zhang, W., Chen, M., Zhong, F., Jing, X. H., et al. (2018). Acupuncture for patients with chronic functional constipation: a randomized controlled trial. Neurogastroenterol. Motil. 30:e13307. doi: 10.1111/nmo.13316
Zhong, Y., Jia, X., and Wu, Y. (2022). Clinical observation of mind-regulating acupuncture in the treatment of post-stroke constipation. J. Guangzhou Univ. Trad. Chin. Med. 39, 1824–1829. doi: 10.13359/j.cnki.gzxbtcm.2022.08.020
Zhou, W., and Wang, L. (2001). Observation on therapeutic effect of scalp acupuncture on constipation after cerebrovascular disorders. Chinese Acupunct. Moxibust. 6, 21–22.
Zhu, X., and Chen, X. (2010). Comparison of the clinical efficacy of "heavy moxibustion" and "light moxibustion" on post-stroke constipation. World Health Digest 7, 337–339. doi: 10.3969/j.issn.1672-5085.2010.26.343
Keywords: acupuncture, post-stroke constipation, efficacy, safety, meta-analysis, systematic review, randomized clinical trials
Citation: Sun T, Wang K, Li L, Yan M, Zou L, Zhang M, Yang S, Wu J and Liu J (2023) Efficacy and safety of acupuncture in post-stroke constipation: a systematic review and meta-analysis. Front. Neurosci. 17:1275452. doi: 10.3389/fnins.2023.1275452
Received: 10 August 2023; Accepted: 07 September 2023;
Published: 26 September 2023.
Edited by:
Guanhu Yang, Ohio University, United StatesReviewed by:
Jieying Zhang, First Teaching Hospital of Tianjin University of Traditional Chinese Medicine, ChinaCopyright © 2023 Sun, Wang, Li, Yan, Zou, Zhang, Yang, Wu and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jinmin Liu, am12aXBAdmlwLjE2My5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.