- 1Department of Rehabilitation, Xinhua Hospital, School of Medicine, Shanghai Jiaotong University, Shanghai, China
- 2Xinhua Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 3Chongming Hospital, Shanghai University of Medicine and Health Sciences, Shanghai, China
Objective: Fibromyalgia is a chronic musculoskeletal disorder characterized by generalized pain, which is also known as “muscular rheumatism” in Chinese medicine. We undertook this systematic review to evaluate the effectiveness of non-pharmacological traditional Chinese medicine (TCM) combined with conventional therapy on pain, health status, depression, and the quality of life of fibromyalgia patients.
Methods: Studies were retrieved from five electronic databases (PubMed, the Cumulative Index to Nursing and Allied Health, Cochrane Library, Embase, and Web of Science) with publication date up to August 2022. We included randomized controlled trials examining the effects of a combination of non-pharmacological TCM and conventional therapy on pain intensity, health status, depression, and quality of life.
Results: Four randomized controlled trials with 384 fibromyalgia patients met the inclusion criteria. Results of the meta-analysis showed that non-pharmacological TCM combined with conventional therapy exerted significant positive effects on alleviating pain at the post-intervention time point than conventional therapy only (visual analog scale WMD1 = −1.410, P < 0.01; pressure pain threshold WMD2 = 0.830, P < 0.001, respectively). Significant differences in pain assessment were also observed between the two groups after a long-term follow-up (12 months) (WMD1 = −1.040 and WMD2= 0.380, all P < 0.05). The combination therapy group also showed a greater reduction in fibromyalgia impact questionnaire than the control group after a long-term follow-up (WMD = −6.690, P < 0.05). Depression and pain-related quality of life showed no difference between groups (all P > 0.05).
Conclusion: Non-pharmacological TCM combined with conventional therapy may be more effective in alleviating pain and improving health status than conventional therapy only. However, it remains some concerns over the safety and clinic application.
Systematic review registration: Identifier: CRD42022352991.
1. Introduction
Fibromyalgia is a chronic musculoskeletal disorder characterized by diffuse pain, fatigue, and sleep disturbances (Clauw, 2014; Arnold et al., 2019). It has been the second most common rheumatologic disorder after osteoarthritis, affecting at least 2 to 4% of the population worldwide (Häuser et al., 2015). The core symptom of fibromyalgia is variable and multifocal pain, which occurs at different intensities and multiple sites during the disease. Individuals with fibromyalgia are more vulnerable to hyperalgesia or allodynia (Chinn et al., 2016), thus leading to cognitive impairment, emotional disorders (depression or anxiety), and somatic symptoms (headaches) (Bair and Krebs, 2020).
Conventional therapy, which is a multidisciplinary and non-invasive treatment, is the preferred choice for fibromyalgia patients according to the guidelines in different countries (Fitzcharles et al., 2013; Macfarlane et al., 2017; Ariani et al., 2021). Conventional therapy includes exercise, education, cognitive behavioral therapy (CBT) and drug therapy. As European League Against Rheumatism (EULAR) revised recommendations suggested (Macfarlane et al., 2017), patient education can be used as a basic treatment, and exercise is a “strong for” recommendation for improving pain and physical function. Psychological therapies, especially CBT, may help to ease pain-related negative emotions, such as depression and anxiety. Besides, as one of the recommended treatments, pharmacotherapy may also be a beneficial supplement for pain and depression relief, which includes gabapentinoids, tricyclic antidepressants (TCAs), and serotonin-norepinephrine reuptake inhibitors (SNRI). These conventional therapies mentioned above recommended by the EULAR revised recommendations are widely recognized and used in clinical practice for fibromyalgia.
Non-pharmacological TCM (traditional Chinese medicine, such as Qigong and acupuncture) is also considered as an effective alternative therapy in managing fibromyalgia recommended by the latest two practice guidelines (Ariani et al., 2021; Qian, 2021). It has been well-accepted among patients with fibromyalgia due to high safety, simple operation, fewer adverse reactions, and no addiction (Deare et al., 2013; Sarzi-Puttini et al., 2020). TCM has obvious superiority in the treatment of chronic pain and concomitant mental disorders as it is based on the concept of wholism and harmony of body and mind (Bushnell et al., 2013; Patel et al., 2020). From the TCM point of view, fibromyalgia is generally classified as “muscular rheumatism”. The pathogenesis includes the internal factor (deficiency of vital Qi) and the external factor (invasion of pathogenic Qi). It leads to the stagnation of blood vessels and loss of muscle nourishment (Yun, 2022a). The negative mood state is a main clinical manifestation of fibromyalgia, and the liver dominates emotions. In order to relieve patients' psychiatric and somatic symptoms, the treatment for fibromyalgia should focus on how to dredge the liver meridian and manage emotions (Yang, 2022; Yun, 2022b).
Although non-pharmacological TCM (such as Qigong and acupuncture) proved to be effective (Sarzi-Puttini et al., 2020), it remains unclear whether a combination of non-pharmacological TCM and conventional therapy is more effective than conventional therapy only in treating fibromyalgia in clinical settings. This systematic review aims to figure out the analgesic effect of integrated TCM and conventional therapy on the health status, depression, and pain-related quality of life of patients with fibromyalgia.
2. Methods
The protocol of this systematic review was registered in PROSPERO (No. CRD42022352991) and the work adheres to PRISMA guidelines (Moher et al., 2009).
2.1. Search strategy
Systematic searches were conducted in the databases PubMed, the Cumulative Index to Nursing and Allied Health, Cochrane Library, Embase, and Web of Science. We used search terms such as “traditional Chinese medicine”, “TCM”, and “fibromyalgia” to find relevant studies published until August 2022, and the full search strategy was listed in the Supplementary Table 1.
2.2. Eligibility criteria
Studies published in English were eligible if they met the following inclusion criteria: (1) Participants: patients over 17 years of age with a diagnosis of fibromyalgia according to the American College of Rheumatology (ACR) criteria or the ACTTION-American Pain Society Pain Taxonomy (AAPT) criteria. (2) Interventions: non-pharmacological TCM combined with conventional therapy. (3) Comparisons: conventional therapy in treating fibromyalgia (such as exercise, psychological therapies, patient education, pharmacotherapy). (4) Outcome measures: Primary outcome measures: Pain intensity: visual analog scale (VAS), and pressure pain threshold (PPT) (Fischer, 1987). Secondary outcome measures: Health status: total Fibromyalgia Impact Questionnaire (FIQ) score (Williams and Arnold, 2011). Depression: Hamilton test score (HAM) and Beck Depression Inventory (BDI) (Beck et al., 1961; Ramos-Brieva and Cordero-Villafafila, 1988). Pain-related quality of life: the bodily pain score of the short form-36 (SF-36). Adverse events: specific adverse events reported during the treatment and follow-up (Bair and Krebs, 2020). Study design: Randomized Controlled Trial (RCT).
Studies were excluded if they were: (1) Self-reported diagnosis without clinical confirmation. (2) Participants in the combination therapy group were treated concomitantly with herbal medicine. (3) Participants in the control group received TCM treatment.
2.3. Data extraction
Two reviewers (ZC and LC) independently screened the enrolled articles through title and abstract screening and full-text reading. Extracted data included: source, setting and language, study type, demographics, symptom duration and severity of fibromyalgia, interventions, outcome measures, adverse events, time points, and overall dropout rate. Disagreements were resolved through discussion with a third reviewer (QD).
2.4. Risk of bias assessment
The methodological quality of the included studies was evaluated using the Cochrane Risk of Bias Tool 2.0 (Rob 2.0). Grading of Recommendation Assessment, Development, and Evaluation (GRADE) was used to assess the quality of the evidence. JL, YS, and HY performed the quality assessment.
2.5. Statistical analysis
Data analysis was performed using Review Manager (RevMan, Version 5.4. Copenhagen: The Nordic Cochrane Center, The Cochrane Collaboration, 2020). A fixed-effects model was used for the quantitative analysis if I2 ≤ 50%, which represented low to moderate heterogeneity, while a random-effects model was used when I2 > 50%, to reduce the impact of substantial heterogeneity. The results would be presented as weighted mean difference (WMD) or standardized mean difference (SMD) and 95% confidence interval (CI) with a significance value set as 0.05.
3. Results
3.1. Identification of studies
The flow diagram of the study selection was provided in Figure 1. Our search retrieved 1617 relevant articles from the five databases. Following the removal of duplicates, the remaining 940 articles were evaluated based on their relevance and publication type. In total, 907 articles with obvious irrelevant topics or non-RCTs were excluded. After the full-text reading, 28 studies only using TCM in the intervention group and 1 study using TCM in the control group were excluded. Four RCTs (Astin et al., 2003; Mannerkorpi and Arndorw, 2004; Targino et al., 2008; Vas et al., 2016) finally met the eligibility criteria.
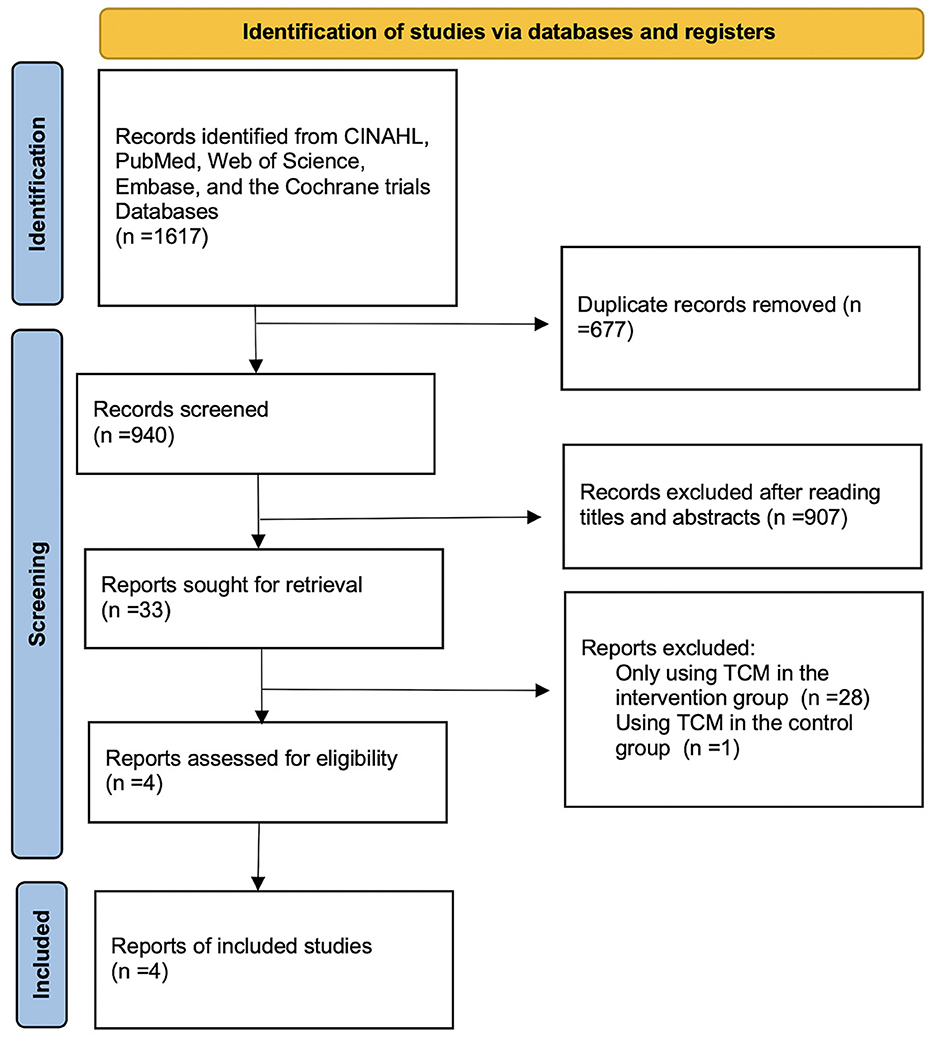
Figure 1. Flowchart of the process of literature search and extraction of studies meeting the inclusion criteria.
3.2. Studies' characteristics
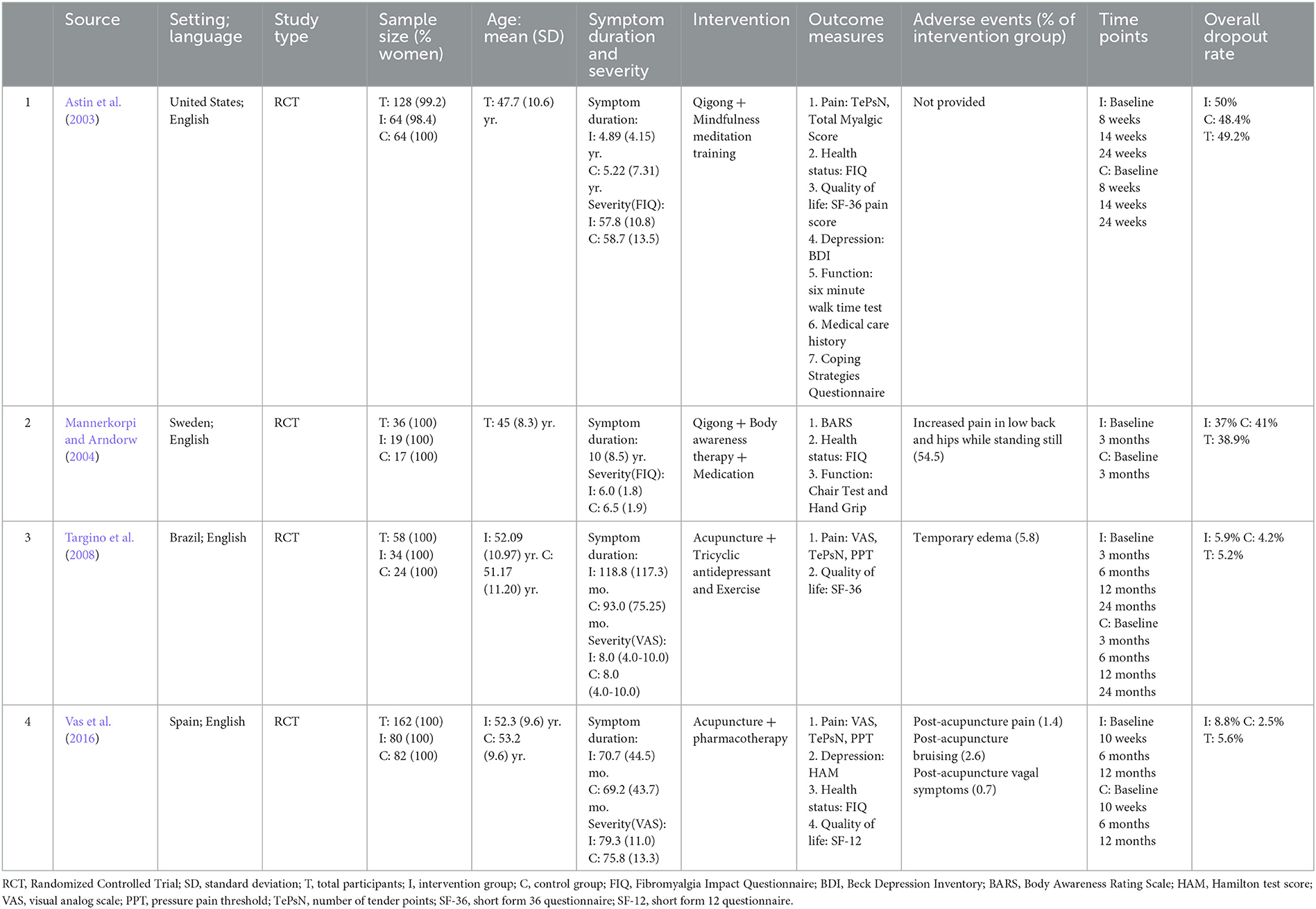
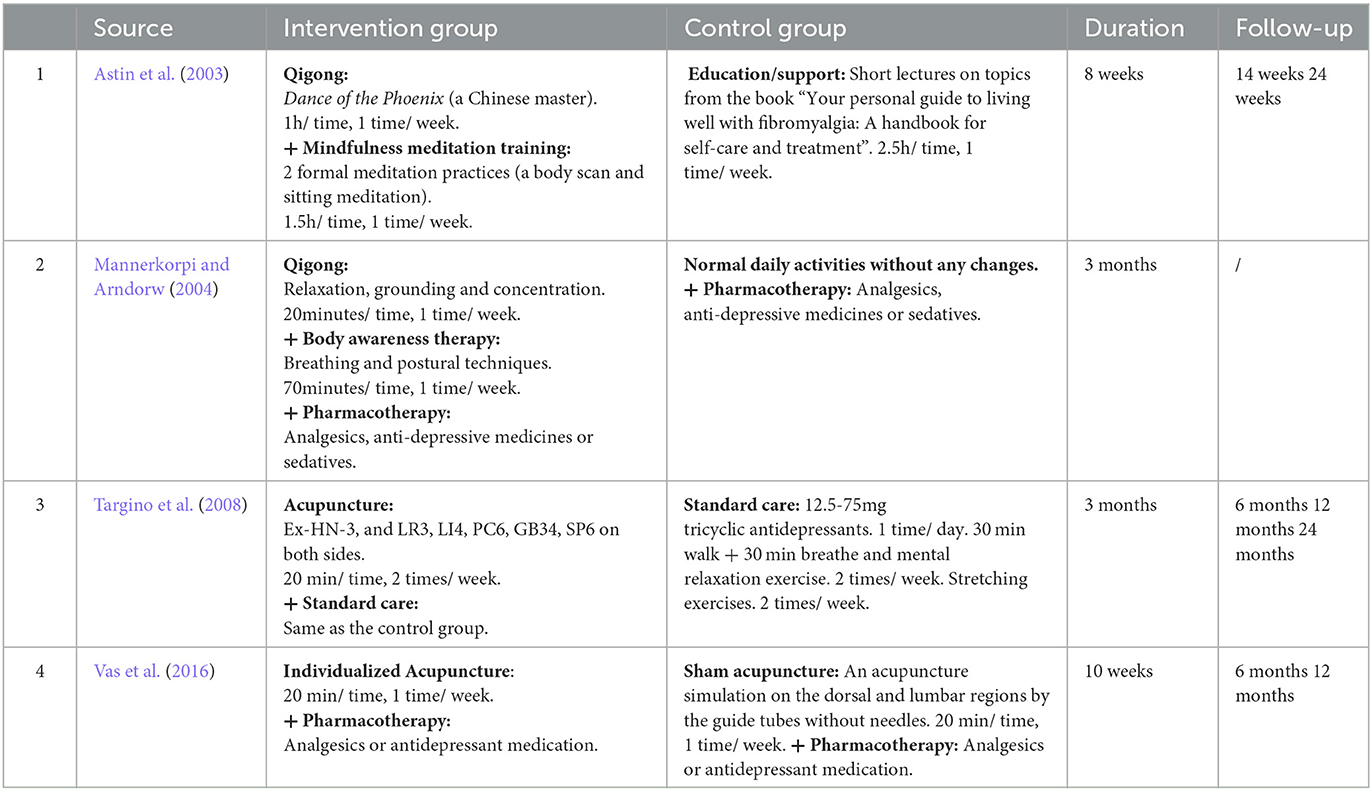
The baseline characteristics of enrolled patients, a summary of outcome measures, and adverse events in included studies were shown in Table 1. The intervention method, treatment frequency, treatment duration, and follow-up of the combination therapy group or control group were shown in Table 2.
This review included 4 articles published from 2003 to 2016, and data from 4 studies were included in the meta-analysis. All included studies were RCTs in English. In total, 197 patients were allocated to the combination therapy group and 187 patients received control intervention.
The duration of intervention for fibromyalgia patients ranged from 8 weeks to 3 months, and the frequency of treatment ranged from once to twice a week. Patients in the combination therapy group were treated with non-pharmacological TCM in addition to conventional therapy. Non-pharmacological TCM treatment included Qigong (Astin et al., 2003; Mannerkorpi and Arndorw, 2004) and acupuncture (Targino et al., 2008; Vas et al., 2016). Conventional therapy included mindfulness meditation training (Astin et al., 2003), body awareness therapy plus pharmacotherapy (Mannerkorpi and Arndorw, 2004), tricyclic antidepressants plus exercise (Targino et al., 2008), and conventional pharmacotherapy (Vas et al., 2016).
3.3. Primary outcomes
3.3.1. Pain intensity
Two trials assessed pain intensity using VAS and PPT (Targino et al., 2008; Vas et al., 2016). Targino et al. (2008) reported a significant decrease in VAS score and increase in PPT after 3-month and 12-month acupuncture treatment combined with antidepressants and exercise. The same conclusion could be drawn from another article (Vas et al., 2016). The pain intensity reduction was also greater in the acupuncture plus medication group than in the sham acupuncture group after 10-week and 12-month follow-up.
The pooled data showed that the combination therapy group exhibited a more significant decrease in VAS score than the control group after intervention (WMD −1.410; 95% CI −2.31 to −0.50, P < 0.01, I2 = 36.0%) (Figure 2A) and after a long-term follow-up (WMD −1.040; 95%CI −1.77 to −0.31, P < 0.01, I2 = 0.0%) (Figure 2B).
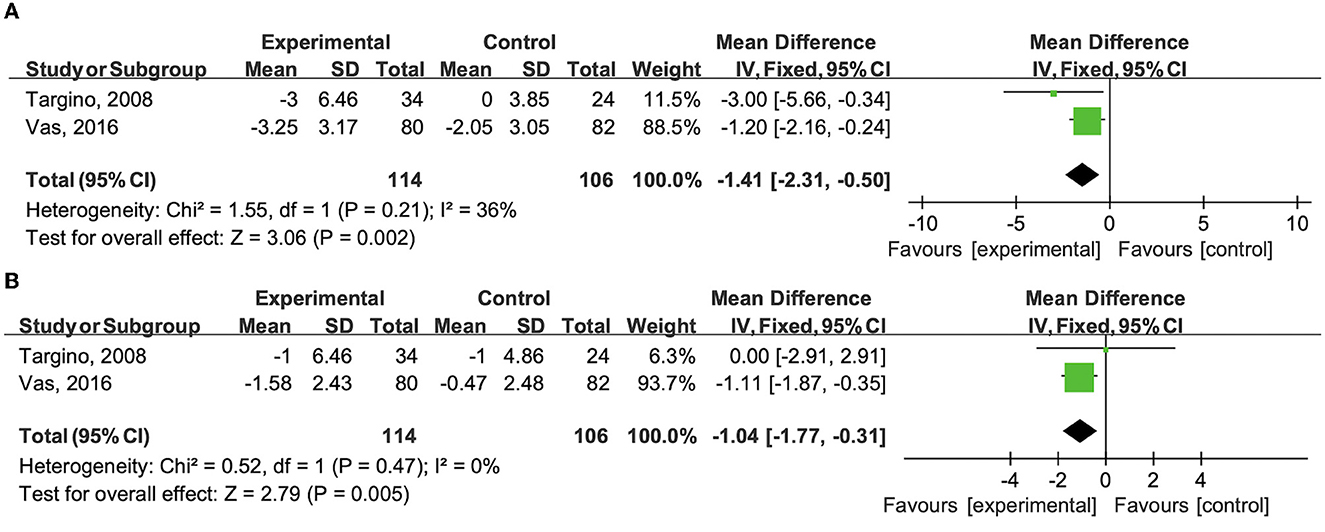
Figure 2. (A) Effects of the combination therapy on VAS score in fibromyalgia after the treatment. (B) Effects of the combination therapy on VAS score in fibromyalgia after a long-term follow-up.
PPT was assessed in two studies (Targino et al., 2008; Vas et al., 2016). As shown in Figures 3A, B, patients in the combination therapy group demonstrated a substantially better improvement in PPT than those in the control group after intervention (WMD 0.830; 95% CI 0.54 to 1.11, P < 0.001, I2 = 0.0%) and after a long-term follow-up (WMD 0.380; 95% CI 0.16 to 0.61, P < 0.001, I2 = 0.0%).
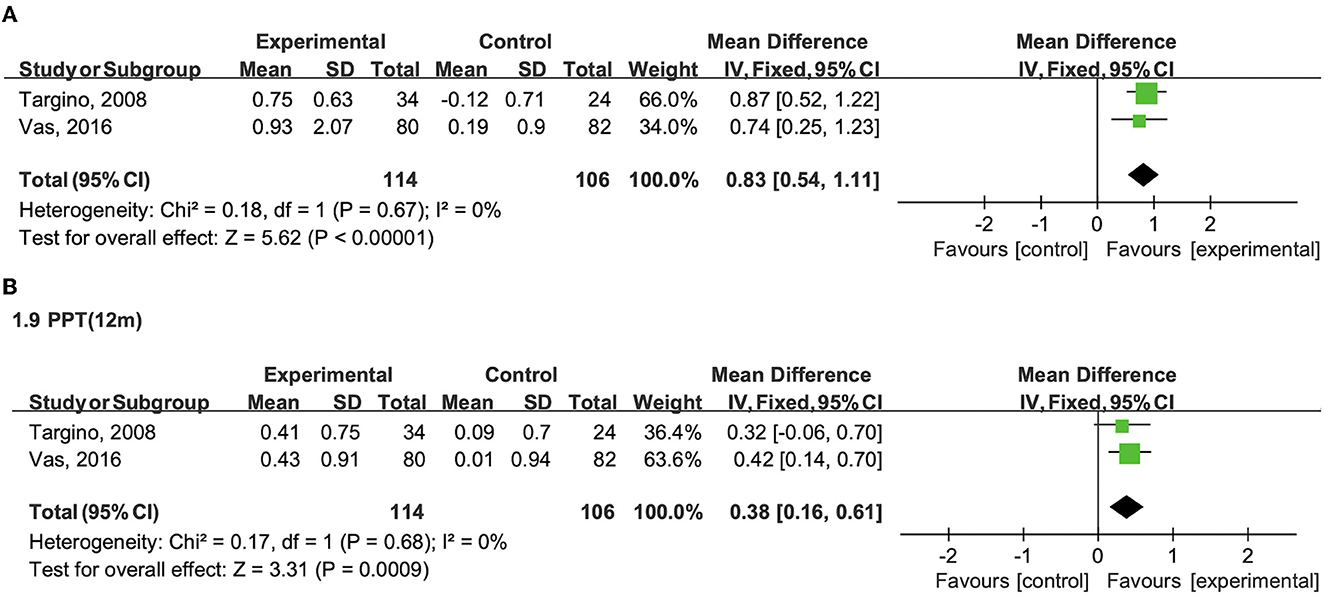
Figure 3. (A) Effects of the combination therapy on PPT in fibromyalgia after the treatment. (B) Effects of the combination therapy on PPT in fibromyalgia after a long-term follow-up.
3.4. Secondary outcomes
3.4.1. Health status
Health status was investigated in 3 studies by using the total FIQ score (Astin et al., 2003; Mannerkorpi and Arndorw, 2004; Vas et al., 2016). FIQ is a 10-item questionnaire to measure the health status of patients with fibromyalgia, with higher scores indicating worse function and symptoms (Burckhardt et al., 1991).
Astin et al. (2003) reported that both Qigong plus mindfulness meditation training group and the control group registered statistically significant improvements after 8-week and 24-week follow-up, but no statistically significant between-group difference for FIQ score was detected. Mannerkorpi and Arndorw (2004) also pointed out that no differences were found between groups after a 3-month follow-up. However, Vas et al. (2016) obtained a result that the FIQ score of the patients in the acupuncture plus medication group was significantly better than in the sham acupuncture group after 10-week and 12-month follow-up.
When the results were pooled, no significant differences were shown between the combination therapy group and control group after intervention (WMD −2.090; 95%CI −7.55 to 3.37, P = 0.450, I2 = 69.0%) (Figure 4A). However, the pooled results showed a greater reduction in total FIQ score than the control group after a long-term follow-up (WMD −6.690; 95%CI −12.18 to −1.21, P < 0.05, I2 = 42.0%) (Figure 4B).
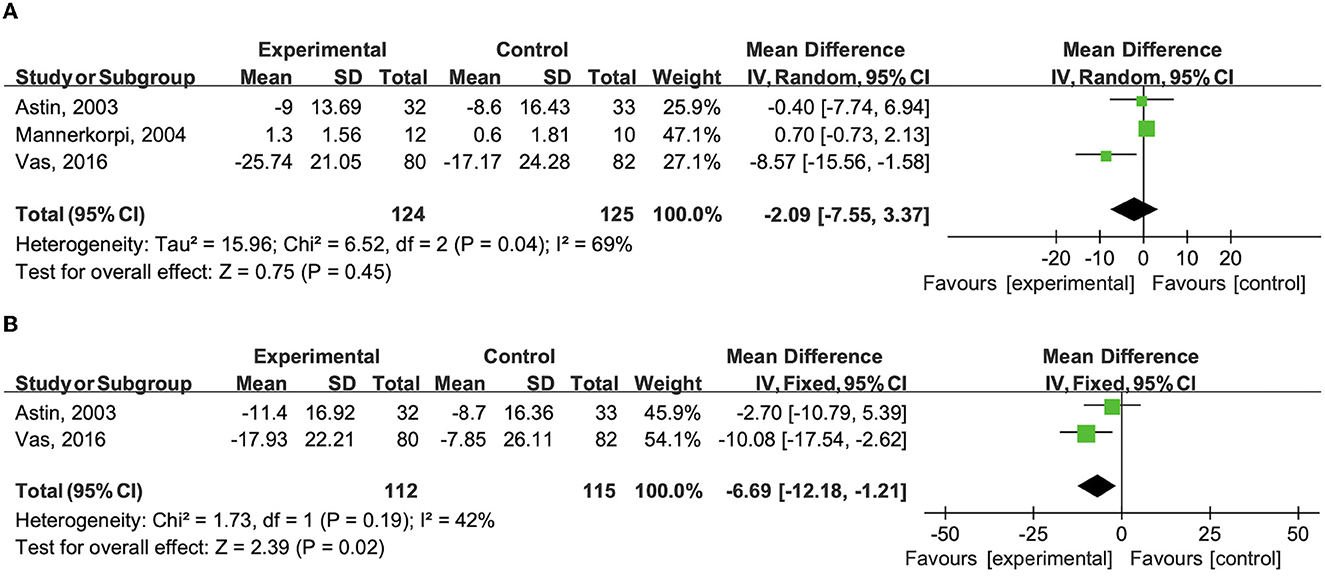
Figure 4. (A) Effects of the combination therapy on total FIQ score in fibromyalgia after the treatment. (B) Effects of the combination therapy on total FIQ score in fibromyalgia after a long-term follow-up.
After removing the study from Vas et al. (2016) based on sensitivity analysis, there was no significant statistical heterogeneity and no significant results were found after intervention (WMD 0.66; 95% CI −0.74 to 2.06, P = 0.36, I2 = 0%).
3.4.2. Depression
Regarding the assessment of depression, Astin et al. (2003) used BDI while Vas et al. (2016) measured HAM. Patients with higher scores of BDI and HAM may have more severe depression.
The study from Vas et al. (2016) showed that HAM scores decreased in the acupuncture plus medication group and control group after the 10-week and 6-month treatments, but the difference was not statistically and clinically significant. Astin et al. (2003) also yielded no positive results between Qigong + mindfulness meditation training group and the control group after 8-week and 24-week follow-up.
Compared to the control group, no significant improvement in the combination therapy group was observed in the level of depression after intervention (SMD −0.090; 95% CI −0.35 to 0.17, P = 0.500, I2 = 0.0%) (Supplementary Figure 1A). The results led to a similar conclusion after a long-term follow-up (SMD −0.150; 95%CI −0.41 to 0.11, P = 0.260, I2 = 0.0%) (Supplementary Figure 1B).
3.4.3. Pain-related quality of life
Two studies reported pain-related quality of life using the bodily pain score of the SF-36 (Astin et al., 2003; Targino et al., 2008).
Compared to the control group, the pooled data showed no more improvement in the bodily pain score of the SF-36 in the combination therapy group after intervention (WMD −0.050; 95%CI −7.84 to 7.74, P = 0.990, I2 = 39.0%) and after a long-term follow-up (WMD −0.890; 95%CI −9.84 to 8.06, P = 0.850, I2 = 0.0%). The results are presented in Supplementary Figures 2A, B.
3.4.4. Adverse events
Three studies mentioned adverse events (Mannerkorpi and Arndorw, 2004; Targino et al., 2008; Vas et al., 2016). Over half of the patients with fibromyalgia in the Qigong group reported increased pain in low back and hips while standing still (Mannerkorpi and Arndorw, 2004). With regard to the adverse events of acupuncture in 2 trials (Targino et al., 2008; Vas et al., 2016), 5.8% of patients with fibromyalgia in the combination therapy group reported temporary oedema, 1.4% reported post-acupuncture pain, 2.6% reported post-acupuncture bruising, and 0.7% reported post-acupuncture vagal symptoms.
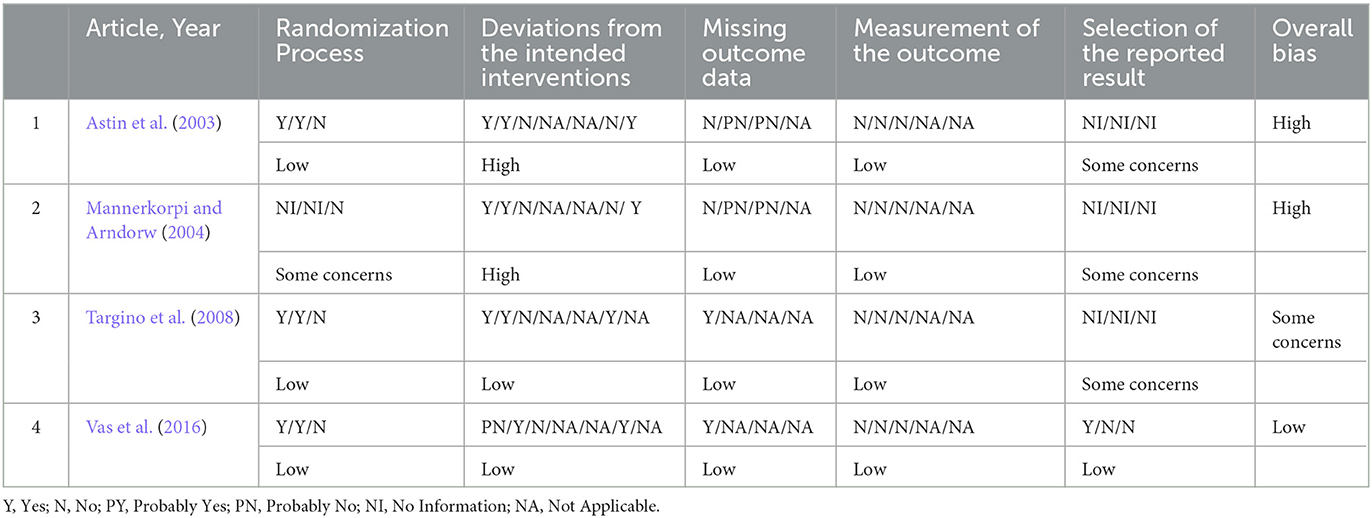
3.5. Quality appraisal
The risk of bias assessment is provided in the Supplementary material (Supplementary Figure 3). Two studies had a high risk of bias due to no blinding of participants or personnel and a high dropout rate (Astin et al., 2003; Mannerkorpi and Arndorw, 2004). The other two studies were respectively classified as moderate and low risk of bias (Table 3) (Targino et al., 2008; Vas et al., 2016). The quality of the evidence for each outcome measure was rated from moderate to very low. Outcomes including VAS and PPT showed moderate quality, while the remaining six outcome measures showed very low quality (Supplementary Table 2).
4. Discussion
This meta-analysis evaluated the effect of a combination of non-pharmacological TCM and conventional therapy in treating fibromyalgia compared to conventional therapy only. The present meta-analysis of data from 4 RCTs revealed that non-pharmacological TCM combined with conventional therapy was superior to the control intervention in the improvement of pain and health status.
Fibromyalgia is characterized by poor circulation of Qi and blood that could not nourish muscles in the perspective of TCM. The moody state is a prominent external manifestation of this disease, associated with physical dysfunction such as pain and sleep quality. Therefore, focusing on the movement of Qi, mainly in the liver meridian, may be the key to improving the moody state and somatic dysfunctions (Yang, 2022; Yun, 2022b). Blood stasis leads to inadequate blood flow to the liver and stagnation of liver Qi, which hinders the liver meridian from timely regulation of other organs. It may result in various somatic dysfunctions, especially pain. In TCM intervention, the key to alleviating pain is to disperse stagnated liver Qi and eliminate Qi stagnation.
Central sensitization marked by the dysfunction of neuro-circuits is one of the main pathogenesis of fibromyalgia (Siracusa et al., 2021). Central sensitization refers to the enhanced transmission of nociceptive signals in the dorsal horn of the spinal cord. Animal studies showed that acupuncture may activate bioactive chemicals (such as opioids) and inhibit the activation of spinal microglia to modulate the local inflammatory environment to inhibit central sensitization (Lai et al., 2019). In addition, the pathogenesis of fibromyalgia may also link to inflammatory factors (Littlejohn and Guymer, 2018). Moderate-intensity exercise has been proven to decrease fibromyalgia patients' blood levels of cytokines (Bote et al., 2013). Qigong is a moderate-intensity exercise incorporating Qi regulation and supporting the righteous Qi (Jiao et al., 2019), as well regulating breath control and mental adjustment. It may also ameliorate symptoms (especially pain) caused by liver Qi stagnation through physical and emotional regulation in the process of training (Yeung et al., 2018). Meanwhile, clinical practice and the animal experiment proved that stimulating Yintang (Ex-HN-3) may be related to inflammatory pathways, and it is considered effective in improving negative emotions (Armour et al., 2019). Taichong (LR3) and Yanglingquan (GB34) are also classical acupoints employed (WHO, 1991; Qiao et al., 2020).
Our results showed that a significantly more decrease in pain was found in the combination therapy group than that in the control group. However, it seems difficult to define a minimal clinical important difference (MCID) in pain improvement in patients with fibromyalgia. A consensus statement indicated that a 1.0 cm reduction in the 10 cm VAS may represent a “minimal” or “little” change in chronic pain, while a 2.0 to 2.7 cm reduction may be more clinically meaningful (Dworkin et al., 2008). The decrease of VAS scores (WMD = −1.410) in this meta-analysis suggests a “little” difference in pain between the combination therapy group and the control group. Since MCID values varied widely depending on the type of chronic pain and baseline pain intensity (Muñoz-Leyva and Chan, 2020), future studies should focus on the calculation of MCID in pain measurements (e.g., VAS and PPT) in patients with fibromyalgia.
There were no significant differences in depression and pain-related quality of life between the combination therapy group and the control group. A likely explanation is that TCM emphasizes individualized treatment, however, none of the included studies mentioned TCM diagnosis (Mist et al., 2011). Acupuncture points and the frequency or intensity of interventions may focus only on core symptoms such as pain, while the individual needs such as quality of life and improving depression are possibly ignored. Another underlying reason is that though Qigong is effective in regulating body and mind, the exercise requires continuous participation, long-term adherence, and high-level cognitive ability for the patients (Jones and Liptan, 2009; Sawynok and Lynch, 2017). No results showed an improvement in depression and quality of life due to the high dropout rate (37–50%). Moreover, patients with comorbid depression can benefit from specific treatment such as psychopharmacological treatment or cognitive behavioral therapies recommended by the guidelines, but only one article mentioned tricyclic antidepressants were used and no articles included in our systematic review employed CBT as conventional therapy.
Three studies mentioned the adverse events in the combination therapy group, including temporary edema (acupuncture), post-acupuncture pain, post-acupuncture bruising, post-acupuncture vagal symptoms, and increased pain in low back and hips in Qigong exercise (Mannerkorpi and Arndorw, 2004; Targino et al., 2008; Vas et al., 2016). Acupuncture is an invasive treatment, but bleeding and swelling after acupuncture can be relieved by a cold compress. It is necessary to inform patients of the underlying risks before administering needles and apply acupuncture more gently to minimize side effects. It is worth noting that up to 54.5% of patients who took part in Qigong plus body awareness therapy reported increased pain in low back and hips while standing still (Mannerkorpi and Arndorw, 2004). The possible explanation may be that Qigong is a moderate-intensity exercise that may increase the pain and discomfort of patients with fibromyalgia due to exercise-induced fatigue (Lima et al., 2017). Hence, we need to pay more attention to patients and require timely feedback on any discomfort during Qigong intervention. Additionally, to reduce the rate of side effects and increase patient compliance, we should appropriately increase the frequency of rest between training sessions, and guide patients on how to perform relaxation and stretching after training (Garber et al., 2011).
5. Limitations
Some limitations need to be addressed when interpreting the results. First, it may be difficult to draw any sound conclusion because only four eligible RCTs were included in the meta-analysis. Different types of interventions (Qigong, acupuncture, exercise, etc.) and acupoints (standardized or individualized acupuncture) were employed in these studies. The high methodological heterogeneity may restrict the possibility of inferences from the present results and subgroup analysis could not be conducted due to the limited number of studies. A standardized intervention protocol should be developed in the future. Second, two of the included studies showed a high risk of bias due to a high overall dropout rate. Improving the acceptance and comfort of TCM intervention may be a feasible plan to reduce the dropout rate. Future studies should focus on stretching and relaxation after exercise to reduce pain. Online guidance or supervision may be a key way to enhance the adherence of fibromyalgia patients to TCM. Third, although there was a more significant decrease in pain intensity in the combination therapy group than in the control group, it remained unclear whether the effect size reached MCID. Hence the effect of combination therapy on relieving pain should be interpreted with caution and the calculation of MCID in pain measurements warrants further research.
6. Conclusion
Non-pharmacological TCM combined with conventional therapy may be more effective than conventional therapy only in alleviating pain and improving the health status of patients with fibromyalgia. A long-term effect of non-pharmacological TCM combined with conventional therapy was also found in the treatment of pain and health status. However, our results should be applied to the clinic with caution due to the limited number of included studies, methodological heterogeneity, and potential adverse events. To increase the safety and adherence to non-pharmacological TCM, future studies should add stretching and relaxation after exercise and provide online supervision to fibromyalgia patients during the intervention.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
LC and ZC conceived the idea and contributed to the writing of the manuscript and screened the enrolled articles and completed the data extraction. LC, JZ, and QW performed the literature search. JL, YS, and HY assessed the risk of bias and the quality of the evidence. LC, ZC, and JL conducted the statistical analyses and interpreted the results. QD and XZ revised the manuscript and gave guidance throughout the process of this study. All authors read and approved the summited and final version of the manuscript to be published.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnins.2023.1097475/full#supplementary-material
References
Ariani, A., Bazzichi, L., Sarzi-Puttini, P., Salaffi, F., Manara, M., Prevete, I., et al. (2021). The italian society for rheumatology clinical practice guidelines for the diagnosis and management of fibromyalgia best practices based on current scientific evidence. Reumatismo. 73, 89–105. doi: 10.4081/reumatismo.2021.1362
Armour, M., Smith, C. A., Wang, L. Q., Naidoo, D., Yang, G. Y., MacPherson, H., et al. (2019). Acupuncture for depression: a systematic review and meta-analysis. J. Clin. Med. 8, 1140. doi: 10.3390/jcm8081140
Arnold, L. M., Bennett, R. M., Crofford, L. J., Dean, L. E., Clauw, D. J., Goldenberg, D. L., et al. (2019). AAPT diagnostic criteria for fibromyalgia. J. Pain. 20, 611–628. doi: 10.1016/j.jpain.2018.10.008
Astin, J. A., Berman, B. M., Bausell, B., Lee, W. L., Hochberg, M., Forys, K. L., et al. (2003). The efficacy of mindfulness meditation plus Qigong movement therapy in the treatment of fibromyalgia: a randomized controlled trial. J. Rheumatol. 30, 2257–2262.
Bair, M. J., and Krebs, E. E. (2020). Fibromyalgia. Ann. Intern Med. 172, ITC33–ITC48. doi: 10.7326/AITC202003030
Beck, A. T., Ward, C. H., Mendelson, M., Mock, J., and Erbaugh, J. (1961). An inventory for measuring depression. Arch. Gen. Psychiatry. 4, 561–571. doi: 10.1001/archpsyc.1961.01710120031004
Bote, M. E., Garcia, J. J., Hinchado, M. D., and Ortega, E. (2013). Fibromyalgia: anti-inflammatory and stress responses after acute moderate exercise. PLoS ONE. 8, e74524. doi: 10.1371/journal.pone.0074524
Burckhardt, C. S., Clark, S. R., and Bennett, R. M. (1991). The fibromyalgia impact questionnaire: development and validation. J. Rheumatol. 18, 728–733.
Bushnell, M. C., Ceko, M., and Low, L. A. (2013). Cognitive and emotional control of pain and its disruption in chronic pain. Nat. Rev. Neurosci. 14, 502–511. doi: 10.1038/nrn3516
Chinn, S., Caldwell, W., and Gritsenko, K. (2016). Fibromyalgia pathogenesis and treatment options update. Curr. Pain Headache Rep. 20, 25. doi: 10.1007/s11916-016-0556-x
Clauw, D. J. (2014). Fibromyalgia: a clinical review. JAMA. 311, 1547–1555. doi: 10.1001/jama.2014.3266
Deare, J. C., Zheng, Z., Xue, C. C., Liu, J. P., Shang, J., Scott, S. W., et al. (2013). Acupuncture for treating fibromyalgia. Cochrane Database Syst. Rev. 2013, Cd007070. doi: 10.1002/14651858.CD007070.pub2
Dworkin, R. H., Turk, D. C., Wyrwich, K. W., Beaton, D., Cleeland, C. S., Farrar, J. T., et al. (2008). Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J. Pain. 9, 105–121. doi: 10.1016/j.jpain.2007.09.005
Fischer, A. A. (1987). Pressure algometry over normal muscles. Standard values, validity and reproducibility of pressure threshold. Pain. 30, 115–126. doi: 10.1016/0304-3959(87)90089-3
Fitzcharles, M. A., Ste-Marie, P. A., Goldenberg, D. L., Pereira, J. X., Abbey, S., Choinière, M., et al. (2013). 2012 Canadian guidelines for the diagnosis and management of fibromyalgia syndrome: executive summary. Pain Res. Manag. 18, 119–126. doi: 10.1155/2013/918216
Garber, C. E., Blissmer, B., Deschenes, M. R., Franklin, B. A., Lamonte, M. J., Lee, I. M., et al. (2011). American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med. Sci. Sports Exerc. 43, 1334–1359. doi: 10.1249/MSS.0b013e318213fefb
Häuser, W., Ablin, J., Fitzcharles, M. A., Littlejohn, G., Luciano, J. V., Usui, C., et al. (2015). Fibromyalgia. Nat. Rev. Dis. Primers. 1, 15022. doi: 10.1038/nrdp.2015.22
Jiao, J., Russell, I. J., Wang, W., Wang, J., Zhao, Y. Y., Jiang, Q., et al. (2019). Ba-Duan-Jin alleviates pain and fibromyalgia-related symptoms in patients with fibromyalgia: results of a randomised controlled trial. Clin. Exp. Rheumatol. 37, 953–962.
Jones, K. D., and Liptan, G. L. (2009). Exercise interventions in fibromyalgia: clinical applications from the evidence. Rheum. Dis. Clin. North Am. 35, 373–391. doi: 10.1016/j.rdc.2009.05.004
Lai, H. C., Lin, Y. W., and Hsieh, C. L. (2019). Acupuncture-analgesia-mediated alleviation of central sensitization. Evid Compl. Alt. Med. 2019, 6173412. doi: 10.1155/2019/6173412
Lima, L. V., Abner, T. S. S., and Sluka, K. A. (2017). Does exercise increase or decrease pain? Central mechanisms underlying these two phenomena. J. Physiol. 595, 4141–4450. doi: 10.1113/JP273355
Littlejohn, G., and Guymer, E. (2018). Neurogenic inflammation in fibromyalgia. Semin Immunopathol. 40, 291–300. doi: 10.1007/s00281-018-0672-2
Macfarlane, G. J., Kronisch, C., Dean, L. E., Atzeni, F., Häuser, W., Fluß, E., et al. (2017). EULAR revised recommendations for the management of fibromyalgia. Ann. Rheum. Dis. 76, 318–328. doi: 10.1136/annrheumdis-2016-209724
Mannerkorpi, K., and Arndorw, M. (2004). Efficacy and feasibility of a combination of body awareness therapy and qigong in patients with fibromyalgia: a pilot study. J. Rehabil. Med. 36, 279–281. doi: 10.1080/16501970410031912
Mist, S. D., Wright, C. L., Jones, K. D., and Carson, J. W. (2011). Traditional Chinese medicine diagnoses in a sample of women with fibromyalgia. Acupunct. Med. 29, 266–269. doi: 10.1136/acupmed-2011-010052
Moher, D., Liberati, A., Tetzlaff, J., and Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J. Clin. Epidemiol. 62, 1006–1012. doi: 10.1016/j.jclinepi.2009.06.005
Muñoz-Leyva, F. E. B. K., and Chan, V. (2020). Is the minimal clinically important difference (MCID) in acute pain a good measure of analgesic efficacy in regional anesthesia? Reg. Anesth. Pain Med. 45, 1000–1005. doi: 10.1136/rapm-2020-101670
Patel, M., Urits, I., Kaye, A. D., and Viswanath, O. (2020). The role of acupuncture in the treatment of chronic pain. Best. Pract Res. Clin Anaesthesiol. 34, 603–616. doi: 10.1016/j.bpa.2020.08.005
Qian, Z. (2021). Chinese expert consensus on the diagnosis and treatment of fibromyalgia. Chin. J. Pain Med. 27, 721–727. doi: 10.3969/j.issn.1006-9852.2021.10.001
Qiao, L., Guo, M., Qian, J., Xu, B., Gu, C., Yang, Y., et al. (2020). Research advances on acupuncture analgesia. Am. J. Chin. Med. 48, 245–258. doi: 10.1142/S0192415X20500135
Ramos-Brieva, J. A., and Cordero-Villafafila, A. A. (1988). New validation of the hamilton rating scale for depression. J. Psychiatr. Res. 22, 21–28. doi: 10.1016/0022-3956(88)90024-6
Sarzi-Puttini, P., Giorgi, V., Marotto, D., and Atzeni, F. (2020). Fibromyalgia: an update on clinical characteristics, aetiopathogenesis and treatment. Nat. Rev. Rheumatol. 16, 645–660. doi: 10.1038/s41584-020-00506-w
Sawynok, J., and Lynch, M. E. (2017). Qigong and fibromyalgia circa 2017. Medicines. 4, 37. doi: 10.3390/medicines4020037
Siracusa, R., Paola, R. D., Cuzzocrea, S., and Impellizzeri, D. (2021). Fibromyalgia: pathogenesis, mechanisms, diagnosis and treatment options update. Int. J. Mol. Sci. 22, 891. doi: 10.3390/ijms22083891
Targino, R. A., Imamura, M., Kaziyama, H. H., Souza, L. P., Hsing, W. T., Furlan, A. D., et al. (2008). A randomized controlled trial of acupuncture added to usual treatment for fibromyalgia. J. Rehabil. Med. 40, 582–588. doi: 10.2340/16501977-0216
Vas, J., Santos-Rey, K., Navarro-Pablo, R., Modesto, M., Aguilar, I., Campos, M., et al. (2016). Acupuncture for fibromyalgia in primary care: a randomised controlled trial. Acupunct. Med. 34, 257–266. doi: 10.1136/acupmed-2015-010950
WHO (1991). Proposed Standard International Acupuncture Nomenclature: Report of a WHO Scientific Group. Geneva: WHO.
Williams, D. A., and Arnold, L. M. (2011). Measures of fibromyalgia: fibromyalgia impact questionnaire (FIQ), brief pain inventory (BPI), multidimensional fatigue inventory (MFI-20), medical outcomes study (MOS) sleep scale, and multiple ability self-report questionnaire (MASQ). Arthritis Care Res. 63, S86–97. doi: 10.1002/acr.20531
Yang, L. (2022). Distribution and characteristics of traditional Chinese medicine patterns in 165 patients with fibromyalgia. J. Beijing Univ. Trad. Chin. Med. 45, 630–636. doi: 10.3969/j.issn.1006-2157.2022.06.013
Yeung, A., Chan, J. S. M., Cheung, J. C., and Zou, L. (2018). Qigong and Tai-Chi for mood regulation. Focus. 16, 40–47. doi: 10.1176/appi.focus.20170042
Yun, D. (2022a). Treating fibromyalgia syndrome thinking based on the theory of “as for the yang qi, if it is firm, it nourishes spirit; if it is soft, it nourishes sinew”. China J. Trad. Chin. Med. Pharmacy. 37, 3312–335.
Keywords: fibromyalgia, traditional Chinese medicine, pain, depression, quality of life, systematic review
Citation: Cai L, Chen Z, Liang J, Song Y, Yu H, Zhu J, Wu Q, Zhou X and Du Q (2023) Effectiveness of non-pharmacological traditional Chinese medicine combined with conventional therapy in treating fibromyalgia: a systematic review and meta-analysis. Front. Neurosci. 17:1097475. doi: 10.3389/fnins.2023.1097475
Received: 13 November 2022; Accepted: 09 May 2023;
Published: 01 June 2023.
Edited by:
Min Fang, Shanghai University of Traditional Chinese Medicine, ChinaReviewed by:
Yazhuo Kong, Chinese Academy of Sciences (CAS), ChinaBo Yu, Shanghai General Hospital, China
Copyright © 2023 Cai, Chen, Liang, Song, Yu, Zhu, Wu, Zhou and Du. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qing Du, ZHVxaW5nQHhpbmh1YW1lZC5jb20uY24=; Xuan Zhou, emhvdXh1YW5AeGluaHVhbWVkLmNvbS5jbg==
†These authors have contributed equally to this work and share first authorship
 Lili Cai1,2†
Lili Cai1,2† Xuan Zhou
Xuan Zhou Qing Du
Qing Du