
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Neurosci., 06 October 2022
Sec. Sleep and Circadian Rhythms
Volume 16 - 2022 | https://doi.org/10.3389/fnins.2022.975576
Although bright light therapy (BLT) has been widely used in the clinical treatment of depression, the antidepressant effect of BLT is not well understood. Considering the connection between depression and disrupted circadian rhythm, we assumed the model of human circadian phototransduction could be more accurate in evaluating the efficacy of BLT for depression compared to light level and spectrum. A systematic review and meta-analysis were conducted and the CS (circadian stimulus) model was used to quantify the efficacy of lighting in BLT. Articles published up to June 2022 were searched in COCHRANE, EMBASE, MEDLINE, and Web of Science. Randomized clinical trials included articles using high circadian stimulus (H-CS, CS > 0.1) as lighting therapy for people with depressive disorder vs. a control group (CS < 0.1). The treatment effect was estimated by calculating the mean difference (MD) with 95% confidence intervals (CIs). Seven trials involving 258 participants met the inclusion criteria. In this sample size, H-CS lighting was associated with a significant reduction in depressive symptoms (MD = −5.56, 95% CI = −9.22 to −1.90, P = 0.003, I2 = 64%). According to the meta-analysis, CS can be employed for the clinical evaluation of BLT for patients with depressive disorder and exposure to H-CS lighting significantly reduced depressive symptoms among adults. A range of CS > 0.57 was obtained, during which different lighting parameter combinations (e.g., light levels, spectra, duration, and light distribution) could achieve better treatment for depression.
Systematic review registration: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021253648.
BLT has been proven to be an effective and comparatively safe form of depression therapy. It is widely used in clinical practice, and is included in therapeutic guidelines for both seasonal affective disorder (SAD) and non-seasonal depression (NSD) (Lam and Levitt, 1999; Al-Karawi and Jubair, 2016). Electric lighting for 0.5–6 h/day (Lewy et al., 1986; Partonen, 1994) for a week or more has been shown to alleviate depressive symptoms for patients with depression diagnosed by standard clinical methods (Al-Karawi and Jubair, 2016). With advancements in basic science and electric lighting technology, it is now possible to quantify the dosing of lighting therapy. White light is currently used as the standard treatment spectrum for SAD and NSD (Al-Karawi and Jubair, 2016; Ravindran et al., 2016). In some studies, blue and green lights (Benedetti et al., 2003; Anderson et al., 2009) have also been shown to induce a positive therapeutic effect. The illumination is another mode of quantification, and cool-white sources with light level of 10,000 lx have been widely recommended in guidelines on treating depression (Golden et al., 2005). However, the Cochrane review of BLT for NSD concluded that there was no difference between the effects of bright light (>2500 lx) and the control groups (2500 lx maximum) (Kripke, 1998).
To explore the mechanism of light on human physiology, the non-visual effects should be distinguished from the visual effect. Visual effects come from the visual pathway, which extends from retinal photoreceptor cells to the visual cortex area (Kolb et al., 1995). The human eye perceives light in the visible spectrum with various photoreceptor cells, and different wavelengths contribute differently to the perception of vision. The visual perception is quantified by the photopic luminous efficiency function V(λ), which is the basic of photometric values such as illuminance (lux) (CIE, 2020). However, with the discovery of intrinsically photosensitive retinal ganglion cells (ipRGCs) and their non-visual effects such as mood changes (Berson et al., 2002; Lucas et al., 2003; Munch and Wirz-Justice, 2018), there is reason to believe that the light parameters used for characterizing vision may be inappropriate for evaluating the effects of non-vision neural pathways from the retina. Thus, although the parameters (e.g., lux, correlated color temperature) of the visual pathway are most commonly used to evaluate lighting, they may not be suitable to quantify the dose of lighting therapy.
Clinical studies have shown an association between circadian disruption and depression. Circadian rhythm disturbances are present in both SAD and NSD (Germain and Kupfer, 2008; McClung, 2011). Compared with normal people, patients with depression experience a delayed secretion of melatonin before bedtime (Bunney and Potkin, 2008). Melatonin is a pineal hormone regulated by the circadian clock, which is a reliable marker of the circadian rhythm (Peschke and Mühlbauer, 2010). It is worth noting that melatonin can be mediated by light exposure through the non-visual pathway (Berson et al., 2002). Therefore, the regulation of melatonin levels by lighting intervention may be a possible mechanism of BLT for both SAD and NSD.
In order to further validate the relationship between circadian regulation and BLT, the model of human circadian phototransduction is needed to quantify light as a stimulus for the circadian system. According to the non-visual physiological effects in humans, retinal photoreceptor cells respond to light, which then send the signals to the biological clock in the hypothalamic suprachiasmatic nucleus (SCN) (Wright and Lack, 2001). CIE 026 recommended using spectral sensitivity curves for five retinal opsin proteins (melanopsin, rhodopsin, S-, M-, and L-cone opsin), obtaining the equivalent illuminance corresponding to each opsin protein (CIE, 2018; Brown et al., 2022). Though ipRGCs are central to the non-visual pathway, ipRGCs also receive signals originating from rods and cones (Do, 2019). They are all involved in the circadian system phototransduction. Therefore, the equivalent illuminance corresponding to individual opsin proteins cannot completely represent the circadian response to light.
Another possible model is the circadian stimulus (CS), developed by Rea et al., which is based on the principles of retinal neurophysiology and psychophysics experiments (Rea and Figueiro, 2018; Rea et al., 2021a,b). CS takes into account the spectral sensitivity of the three photoreceptors (cones, rods, and ipRGCs) and can be used to characterize both the spectral sensitivity and the response magnitude characteristic of the circadian phototransduction circuit (Rea et al., 2021a). The latest model of CS is quantified in terms of spectrum, light levels, exposure time (duration of the circadian stimulus), and lighting distribution across the retina (Rea et al., 2021a). Melatonin suppression by the pineal gland at night was used as the outcome measure. Compared with single photoreceptor, the CS model can more accurately quantify circadian phototransduction. In the present study, CS was adopted as a new indicator to evaluate the therapeutic efficacy of lighting.
Here, we present a systematic review and meta-analysis of the CS model, uniting the multiple elements of lighting mentioned in the reviewed BLT studies. The Mean Difference (MD) of the depression scale was calculated to assess the efficacy of BLT. Using the reported light levels, spectral data, and the lighting distribution over time and space, the findings of the existing trials were screened based on the CS values. A systematic literature review and meta-analysis were conducted to verify the correlation between CS value and therapeutic effect, thus providing scientific metrics for lighting dose quantification of lighting therapy in clinical applications.
This systematic review was registered with PROSPERO under code number CRD42021253648 and was conducted in accordance with the PRISMA guidelines (Moher et al., 2009). Articles published before 2021 were searched in the Cochrane Library, EMBASE, MEDLINE, and Web of Science. Various synonyms from MeSH (“depressive disorder,” “phototherapy,” and “randomized controlled trial”) were entered in these electronic databases to improve the sensitivity of the search. Supplementary searches of relevant systematic reviews and references within the included articles were performed manually.
As mentioned previously, CS refers to the spectral sensitivity and the response magnitude characteristic of the circadian phototransduction circuit, and melatonin suppression is used as the outcome measure. The specific calculation process for CS was based on the studies of Rea et al. (2021a, 2022). The calculation formula is as follows (Eq. 1):
where t represents the exposure durations of circadian light exposure, f represents the spatial distribution of circadian light exposure (Rea et al., 2021a), CLA represents circadian light illumination determined by the physiological properties of human eyes and stimulus light source (spectrum and level) (Rea et al., 2022). The calculation of CS requires the spectral power distribution. However, some of the previous related studies did not report detailed spectral information. Therefore, the CIE standard light source closest to the description of the light conditions given in these studies was used as a substitute source of spectral information for the CS calculation. The specific substituted spectral information is shown in Table 1.
Advantageously, CS = 0.1 is established as a clear and quantifiable cutoff level that has demonstrated no effect on the circadian rhythm (Alzahrani et al., 2022). Therefore, CS = 0.1 was set as the demarcation criteria for the intervention group and the control group of the light therapy, CS < 0.1 was defined as the low CS group (the control group), and CS > 0.1 as the high CS group (the intervention group).
Studies that met the following criteria were included: (A) clinical trials with randomized allocation; (B) patients diagnosed with SAD or NSD by standard clinical methods; (C) patients not in a specific physiological state (such as the period before and after pregnancy) and having no other physiological diseases; (D) patient consented to light therapy as the only independent intervention, with no antidepressant medication or other treatment modalities; (E) the CS of the control/placebo groups (e.g., treated with dim lighting or negative air ions) was relatively low (< 0.1) while the CS of the intervention group was relatively high (>0.1); (F) the outcome variable and effect size were reported in terms of standardized depression scales. The inclusion and exclusion protocols are summarized as a PRISMA flow chart in Figure 1.
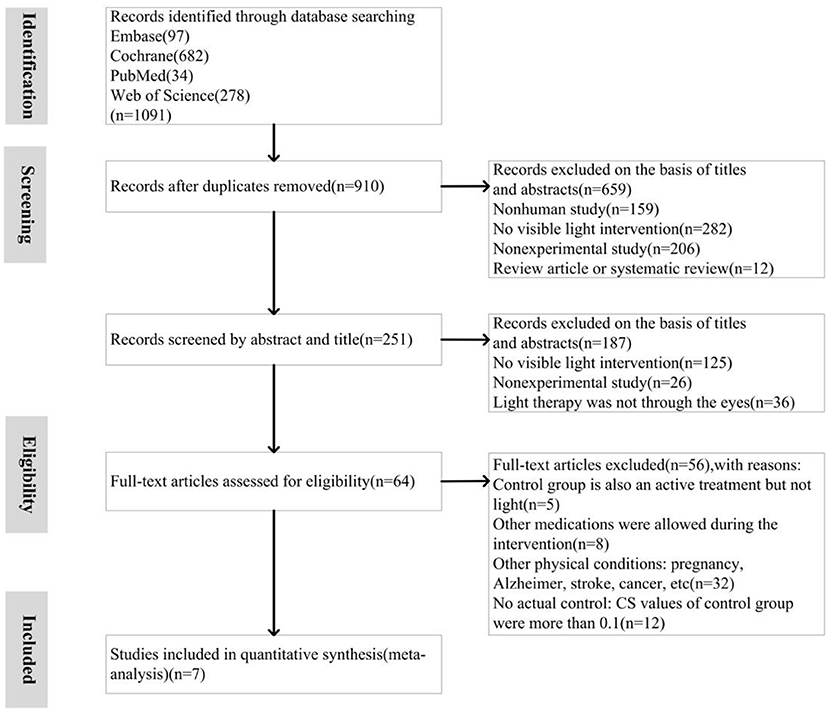
Figure 1. Meta-analysis of high circadian stimulus (H-CS) lighting therapy for depression: Trial selection process.
The following data were extracted from the identified trials: participant characteristics, sample size, assessment modalities, types of depression, sex, diagnostic criteria for depression, illumination parameters, duration of lighting intervention, the definition of the control group, and basic conclusion. The parameters of the interventional lighting used to calculate CS included illuminance, spectra, duration of exposure, and light distribution (illumination configuration).
Two reviewers independently assessed trial quality using the “Risk of Bias Table” from the Cochrane Handbook. This table was amended to include selection bias, performance bias, detection bias, attrition bias, and reporting bias, and was used to evaluate the randomization and blinding methods, outcome measures, and loss to follow-up of the included trials. The final score for each study was quantified as “Low risk,” “Unclear risk,” or “High risk.”
Although the identified trials included cases of seasonal and non-seasonal depression, they used the same continuous outcome variable, namely SIGH-SAD scores. The mean difference (MD) and weighted mean difference with 95% CI were chosen as the effect size. The meta-analysis factored in the mean, standard deviation (SD), sample size, and weight of each original study. In this study, the weight was the inverse of the variance calculated by Review Manager Software (version 5.3.0). The heterogeneity was assessed by evaluating the P and I2 values, and different effect models were selected according to the results of the heterogeneity analysis. In addition, sensitivity analysis was performed to test the stability of the model, which involved examining the heterogeneity and effect size before and after a specific study was deleted.
Of 1,091 studies identified in the database, 7 were included in the meta-analysis. Figure 1 depicts the selection process. Notably, all identified studies had been included in previously published reviews. However, based on the inclusion criteria, we studied both seasonal and non-seasonal depression and intervention/control conditions after parameter conversion (CS value of the intervention group > 0.1; CS value of the control group < 0.1). The lighting parameters were extracted from the 7 clinical trials and analyzed. The results for a total of 258 participants were evaluated, of which 130 patients received H-CS lighting therapy (CS > 0.1) and 128 patients received a placebo control H-CS lighting therapy (CS < 0.1). All patients were diagnosed with standardized screening measures: seven datasets were based on clinical diagnosis using DSM-IV, and one used the Geriatric Depression Scale for elderly participants. All the included trials quantified improvements in depression using standardized scales.
The eligible studies were all randomized controlled trials and the quality of evidence was evaluated with the Revised Cochrane Risk of Bias Tool (Evans et al., 2015), as displayed in Figure 2. Among these 7 studies, two studies adopted a random number table (Goel et al., 2005; Lieverse et al., 2011) and one study used a computer-generated randomization sequence (Rastad et al., 2008) to generate the groups. Since the four remaining studies did not specify any random sequence generation methods, they were categorized as a moderate risk of selection bias. Two studies reported allocation concealment using opaque envelopes (Lieverse et al., 2011) and specific examiners (Koorengevel et al., 2001). The five remaining studies were at high risk of bias in terms of allocation concealment because methods of allocation concealment were not mentioned. Two studies were at high risk of attrition bias as participants withdrew from the experiment (Glickman et al., 2006; Desan et al., 2007).
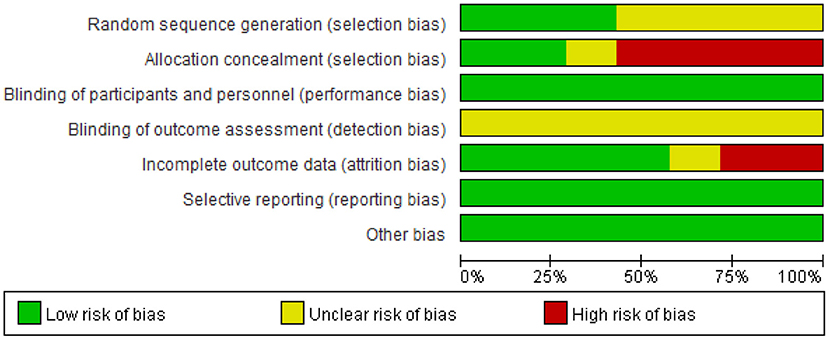
Figure 2. Risk-of-bias graph: Shown are the judgments about each risk-of-bias item, presented as percentages of all included studies.
Notably, lighting interventions are distinct from pharmaceutical interventions as lighting properties are intuitively recognized by the human eye. Thus, while the participants may not recognize experimental drugs and vitamins, they can easily distinguish different colors and light levels. Participants were told that the importance of color and different wavelengths remained uncertain (Strong et al., 2009). Thus, the blinding of outcomes and personnel was unclear.
Table 1 presents a synopsis of the included studies, briefly describing the study design, sample, interventions, circadian stimulus values, outcomes, and results. The studies included a variety of measures, methods, samples, and analytical approaches. The meta-analysis included all 7 eligible estimates addressing SAD, NSD (Goel et al., 2005) and geriatric depression (Lieverse et al., 2011). The meta-analysis revealed that H-CS lighting therapy was associated with a significant reduction in depressive symptoms (MD = −5.56, 95% CI = −9.22 to −1.90, P = 0.003, I2 = 64%) (Figure 3). This finding implies that the H-CS lighting intervention showed a significant reduction of depressive symptoms compared to the corresponding control group (CS < 0.1).
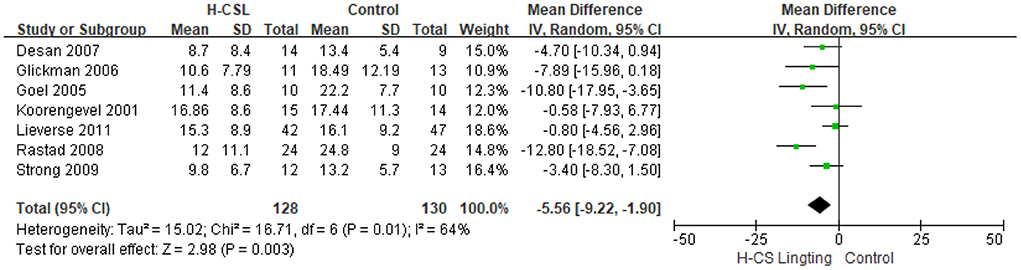
Figure 3. Forest plot comparison: High circadian stimulus lighting (H-CS) group vs. the control group. Outcome: Mean difference.
Sensitivity analysis was conducted to assess the stability of the results and the influence of each study on the total estimate, by omitting one study at a time (Figure 4). When any single finding is excluded, sensitivity analyses reveal that the overall result does not change. Since only one paper evaluated geriatric depression (i.e., depression in participants over 60 y of age), subgroup analysis was performed to assess the influence of age on the association between light therapy and depression. As displayed in Table 2, the results for the older adults subgroup (Lieverse et al., 2011) were not significant (MD = −0.8, 95% CI = −4.56 to 2.96). Several other studies (Rastad et al., 2008; Strong et al., 2009) included older adults and non-elderly participants. The studies that provided an accurate age range of the non-elderly participants (Koorengevel et al., 2001; Goel et al., 2005; Glickman et al., 2006; Desan et al., 2007) were included in the non-elderly subgroup (MD = −5.85, 95% CI = −9.97 to −1.73, P = 0.005, I2 = 29%). Data were also subgrouped based on the length of treatment. The result showed that the short-term exposure to H-CS lighting therapy (MD = −4.90, 95% CI = −9.57 to −0.23, P = 0.04, I2 = 71%) was not significantly different compared to exposure to long-term exposure (MD = −7.34, 95% CI = −13.26 to −1.41, P = 0.02, I2 = 42%).
CS can be used as a new metric quantification method of lighting, which might more accurately represent the dose of light therapy in depression than vision parameters. In this review, H-CS lighting was associated with a significant reduction in depressive symptoms across 7 studies regardless of participant characteristics (e.g., sex, SAD vs. NSD) or individual lighting features (e.g., light levels, spectra, duration, and light distribution).
The funnel plot does not reliably represent the risk of publication bias due to the small number of trials included in this study. Moreover, the presence of low sample size trials can indirectly contribute to publication bias (Sterne et al., 2000). However, eligible articles were screened to meet the requirements of the experimental and control groups based on the range of CS values reducing publication bias. The relationship between CS and therapeutic outcomes could not be obtained from the original articles because the CS measure was introduced only in the present study.
Some previous studies have already proposed that illuminance measurement in lux (lx) may be inadequate for evaluating the dose in BLT studies. For example, the therapeutic effect of blue-appearing light with an illumination of 98 lx was similar to that of white-appearing light with an illumination of 700 lx (Anderson et al., 2009). Notably, the CS values of both groups were equal (0.6) in the research. Several studies (Sumaya et al., 2001; Anderson et al., 2009; Meesters et al., 2018) were not included in our analysis due to the CS values being similar between groups. All of these studies reported decreased depression ratings in both the intervention and control groups, with no statistically significant differences.
Furthermore, another experiment by Anderson et al. showed that both the blue light-free group (CS = 0.30 ± 0.03) and the blue light group (CS = 0.68 ± 0.06) had a significant treatment effect and there was no significantly different between the two groups (Anderson et al., 2016). The results of Anderson's study suggested that depression can be effectively treated when CS > 0.3, however, as the CS values of both groups in this study were greater than 0.1, this research was not included in the present study. According to the meta-analysis result, a certain range of CS values (0.57–0.7) exerts a positive effect on depression but is not restricted in high illumination or specific wavelengths.
In the subgroup analysis based on age, non-elderly patients showed a statistically significant effect in response to H-CS lighting therapy. Only one article specifically investigated the elderly population and showed no significant effect when treated with H-CS lighting. Similarly, a reduction in responsiveness to photic stimuli in the circadian timing system in older adults was reported (Kim et al., 2014). This difference may be attributed to the physiology of the elderly eye. With age, the retina, cornea, lens, and other structures in the visual organs undergo substantial changes, including a reduction of lens transparency and changes in the crystalline lens color, which can result in variations in the refractive index of the lens. These age-related lens changes increase short wavelength light absorption, impairing the ability to absorb short wavelengths light (Mellerio, 1987). Another possible contributing factor is that, as described in previous studies, melanopsin is a short-wavelength-sensitive opsin located in ipRGCs that plays a key role in the non-vision pathways (Berson et al., 2002). Hence, elderly patients receive markedly weaker circadian stimulation than non-elderly patients, prompting caution in the evaluation and quantification of CS in elderly patients. Another study also observed the positive effects of lighting with CS = 0.3 on depression therapy in older persons at risk for Alzheimer's disease (Figueiro and Kales, 2021). Therefore, more clinical research focusing on elderly patients is required due to the limited number of studies.
Further subgroup analysis was performed based on the duration of the intervention. Analyses of two subgroups showed consistent results, with the long-term group (≥4 weeks) showing no significant advantage over the short-term group (1–3 weeks). Thus, the non-visual impact of light may have a cumulative efficacy over a limited period and reaches saturation after a specific duration.
Nevertheless, this study has several limitations. Only seven studies (N = 258) were included in the meta-analysis, which restricts the quality of the evidence. Notably, according to the inclusion criterion (E) for the intervention group, when the CS value was larger than 0.1, the research can be incorporated into the meta-analysis. However, the article screening results yielded only CS values above 0.57 in the intervention group, and intermediate CS values were missing. Therefore, the treatment effect of CS in depression could only be determined for two extreme cases. In conclusion, a significant treatment effect of H-CS photomedicine was achieved with CS higher than 0.57; the present analysis did not establish a therapeutic effect for CS in the range of 0.1–0.57.
Another issue that requires attention is the heterogeneity of the populations in this study. The included sample consisted of SAD and NSD, and also cover patients of different ages and depression severity. Due to the physiological peculiarities of depressed patients, H-CS lighting therapy requires further validation. In the future, more targeted phototherapy studies are necessary to help discovering the specificity of phototherapy for different natures of depression (type, gender, age, degree of illness, etc.). Future trials should also include additional intermediate CS values to establish a model based on treatment outcomes and non-visual light parameters. Moreover, in comparison with visual parameters, non-visual optical parameters have been poorly researched to date. Future studies may identify new parameters that are more appropriate for the accurate evaluation of the therapeutic effect of lighting.
By controlling the spectrum and level of the light for depression disorder therapy, H-CS light mode may be achieved with a preferred color or a gentle light level, improving comfort for the patients, and increasing the effects of light therapy.
Data from this review support the use of CS as a new quantitative measure for the evaluation of bright light therapy in depression. Compared with visual parameters, CS accounts for spectra, illumination, duration, and spatial distribution and how the circadian system responds to them. Based on this sample size, a relatively better therapeutic effect was achieved when the CS value was above 0.57 (H-CS lighting therapy).
Furthermore, additional clinical research should be conducted by using the same CS values to validate this model. Meanwhile, the therapeutic effect of light therapy with CS in the 0.1–0.57 range remains unknown, and future studies should investigate the effect of these intermediate CS values.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
YL supervised the research and built the article framework. All authors contributed to the literature search. Data collection and analysis were performed by LZ and DH. Study quality and risk-of-bias assessments were performed by LZ, YW, and SZ. The first draft of the manuscript was written by LZ and all authors commented on previous versions of the manuscript. All authors have read and approved the final manuscript.
This study was funded by the Shanghai Municipal Science and Technology Major Project (Grant No. 2017SHZDZX01).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Al-Karawi, D., and Jubair, L. (2016). Bright light therapy for nonseasonal depression: meta-analysis of clinical trials. J. Affect. Disord. 198, 64–71. doi: 10.1016/j.jad.2016.03.016
Alzahrani, H. S., Khuu, S. K., and Roy, M. (2022). Modelling the effect of light through commercially available blue-blocking lenses on the human circadian system. Clin. Exp. Optom. 105, 275–280. doi: 10.1080/08164622.2021.1898276
Anderson, J. L., Glod, C. A., Dai, J., Cao, Y., and Lockley, S. W. (2009). Lux vs. wavelength in light treatment of Seasonal Affective Disorder. Acta. Psychiatr. Scand. 120, 203–212. doi: 10.1111/j.1600-0447.2009.01345.x
Anderson, J. L., St Hilaire, M. A., Auger, R. R., Glod, C. A., Crow, S. J., Rivera, A. N., et al. (2016). Are short (blue) wavelengths necessary for light treatment of seasonal affective disorder? Chronobiol. Int. 33, 1267–1279. doi: 10.1080/07420528.2016.1207660
Benedetti, F., Colombo, C., Pontiggia, A., Bernasconi, A., Florita, M., and Smeraldi, E. (2003). Morning light treatment hastens the antidepressant effect of citalopram: a placebo-controlled trial. J. Clin. Psychiatry 64, 648–653. doi: 10.4088/JCP.v64n0605
Berson, D. M., Dunn, F. A., and Takao, M. (2002). Phototransduction by retinal ganglion cells that set the circadian clock. Science 295, 1070–1073. doi: 10.1126/science.1067262
Brown, T. M., Brainard, G. C., Cajochen, C., Czeisler, C. A., Hanifin, J. P., Lockley, S. W., et al. (2022). Recommendations for daytime, evening, and nighttime indoor light exposure to best support physiology, sleep, and wakefulness in healthy adults. PLoS Biol. 20, e3001571. doi: 10.1371/journal.pbio.3001571
Bunney, J. N., and Potkin, S. G. (2008). Circadian abnormalities, molecular clock genes and chronobiological treatments in depression. Br. Med. B 86, 23–32. doi: 10.1093/bmb/ldn019
CIE (2018). CIE System for Metrology of Optical Radiation for ipRGC-Influenced Responses to Light. Standard CIES 026/E:2018. Vienna: Commission Internationale de l'Éclairage. doi: 10.25039/S026.2018
CIE (2020). ILV: International Lighting Vocabulary 2nd Edn. Standard CIES 017/E:2020. Vienna: Commission Internationale de l'Éclairage. doi: 10.25039/S017.2020
Desan, P. H., Weinstein, A. J., Michalak, E. E., Tam, E. M., Meesters, Y., Ruiter, M. J., et al. (2007). A controlled trial of the Litebook light-emitting diode (LED) light therapy device for treatment of Seasonal Affective Disorder (SAD). BMC Psychiatry 7, 38. doi: 10.1186/1471-244X-7-38
Do, M. T. H. (2019). Melanopsin and the intrinsically photosensitive retinal ganglion cells: biophysics to behavior. Neuron 104, 205–226. doi: 10.1016/j.neuron.2019.07.016
Evans, N., Lasen, M., and Tsey, K. (2015).Appendix A: Effective Public Health Practice Project (Ephpp) Quality Assessment Tool for Quantitative Studies. A Systematic Review of Rural Development Research: Characteristics, Design Quality And Engagement With Sustainability. USA: Springer 45–63. doi: 10.1007/978-3-319-17284-2
Figueiro, M. G., and Kales, H. C. (2021). Lighting and Alzheimer's disease and related dementias: spotlight on sleep and depression. Ltg. Res. Tech. 53, 405–422. doi: 10.1177/14771535211005835
Germain, A., and Kupfer, D. J. (2008). Circadian rhythm disturbances in depression. Hum. Psychopharmacol. 23, 571–585. doi: 10.1002/hup.964
Glickman, G., Byrne, B., Pineda, C., Hauck, W. W., and Brainard, G. C. (2006). Light therapy for seasonal affective disorder with blue narrow-band light-emitting diodes (LEDs). Biol. Psychiatry 59, 502–507. doi: 10.1016/j.biopsych.2005.07.006
Goel, N., Terman, M., Su Terman, J., Macchi, M. M., and Stewart, J. W. (2005). Controlled trial of bright light and negative air ions for chronic depression. Psychol. Med. 35, 945–955. doi: 10.1017/S0033291705005027
Golden, R. N., Gaynes, B. N., Ekstrom, R. D., Hamer, R. M., Jacobsen, F. M., Suppes, T., et al. (2005). The efficacy of light therapy in the treatment of mood disorders: a review and meta-analysis of the evidence. Am. J. Psychiatry 162, 656–662. doi: 10.1176/appi.ajp.162.4.656
Kim, S. J., Benloucif, S., Reid, K. J., Weintraub, S., Kennedy, N., Wolfe, L. F., et al. (2014). Phase-shifting response to light in older adults. J. Physiol. 592, 189–202. doi: 10.1113/jphysiol.2013.262899
Kolb, H., Fernandez, E., and Nelson, R. (1995). Webvision: The Organization of the Retina and Visual System. Salt Lake City (UT): University of Utah Health Sciences Center.
Koorengevel, K. M., Gordijn, M. C. M., Beersma, D. G. M., Meesters, Y., den Boer, J. A., van den Hoofdakker, R. H., et al. (2001). Extraocular light therapy in winter depression: a double-blind placebo-controlled study. Biol. Psychiatry 50, 691–698. doi: 10.1016/S0006-3223(01)01182-9
Kripke, D. F. (1998). Light treatment for nonseasonal depression: speed, efficacy, and combined treatment. J. Affect. Disord. 49, 109–117. doi: 10.1016/S0165-0327(98)00005-6
Lam, R., and Levitt, A. (1999). Canadian Consensus Guidelines for the Treatment of Seasonal Affective Disorder. The Canadian Journal of Diagnosis Supplement, October.
Lewy, A. J., Sack, R. L., Miller, L. S., Hoban, T. M., Singer, C. M., Samples, J. R., et al. (1986). The use of plasma melatonin levels and light in the assessment and treatment of chronobiologic sleep and mood disorders. J. Neural Transm. Suppl. 21, 311–322.
Lieverse, R., Van Someren, E. J. W., Nielen, M. M. A., Uitdehaag, B. M. J., Smit, J. H., and Hoogendijk, W. J. G. (2011). Bright light treatment in elderly patients with nonseasonal major depressive disorder: a randomized placebo-controlled trial. Arch. Gen. Psychiatry 68, 61–70. doi: 10.1001/archgenpsychiatry.2010.183
Lucas, R. J., Hattar, S., Takao, M., Berson, D. M., Foster, R. G., and Yau, K. W. (2003). Diminished pupillary light reflex at high irradiances in melanopsin-knockout mice. Science 299, 245–247. doi: 10.1126/science.1077293
McClung, C. A. (2011). Circadian rhythms and mood regulation: insights from pre-clinical models. Eur. Neuropsychopharmacol. 21(Suppl. 4), S683–S693. doi: 10.1016/j.euroneuro.2011.07.008
Meesters, Y., Duijzer, W. B., and Hommes, V. (2018). The effects of low-intensity narrow-band blue-light treatment compared to bright white-light treatment in seasonal affective disorder. J. Affect. Disord. 232, 48–51. doi: 10.1016/j.jad.2018.01.024
Mellerio, J. (1987). Yellowing of the human lens: nuclear and cortical contributions. Vision Res. 27, 1581–1587. doi: 10.1016/0042-6989(87)90166-0
Moher, D., Liberati, A., Tetzlaff, J., and Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J. Clin. Epidemiol. 62, 1006–1012. doi: 10.1016/j.jclinepi.2009.06.005
Munch, M., and Wirz-Justice, A. (2018). Chronobiology: Society for light treatment and biological rhythms, 30th annual meeting, Groningen (The Netherlands), June 21–24, 2018. Neuropsychobiology. 76, 1–46. Available online at: https://www.karger.com/Article/Pdf/489584
Partonen, T. (1994). Effects of morning light treatment on subjective sleepiness and mood in winter depression. J. Affect. Disord. 30, 47–56. doi: 10.1016/0165-0327(94)90150-3
Peschke, E., and Mühlbauer, E. (2010). New evidence for a role of melatonin in glucose regulation. Best Pract. Res. Clin. Endocrinol. Metab. 24, 829–841. doi: 10.1016/j.beem.2010.09.001
Rastad, C., Ulfberg, J., and Lindberg, P. (2008). Light room therapy effective in mild forms of seasonal affective disorder-a randomised controlled study. J. Affect. Disord. 108, 291–296. doi: 10.1016/j.jad.2007.10.009
Ravindran, A. V., Balneaves, L. G., Faulkner, G., Ortiz, A., McIntosh, D., Morehouse, R. L., et al. (2016). Canadian network for mood and anxiety treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: section 5. Complementary and alternative medicine treatments. Can. J. Psychiatry 61, 576–587. doi: 10.1177/0706743716660290
Rea, M. S., and Figueiro, M. G. (2018). Light as a circadian stimulus for architectural lighting. Ltg. Res. Tech. 50, 497–510. doi: 10.1177/1477153516682368
Rea, M. S., Nagare, R., and Figueiro, M. G. (2021a). Modeling circadian phototransduction: quantitative predictions of psychophysical data. Front. Neurosci. 15, 615322. doi: 10.3389/fnins.2021.615322
Rea, M. S., Nagare, R., and Figueiro, M. G. (2021b). Modeling circadian phototransduction: retinal neurophysiology and neuroanatomy. Front. Neurosci. 14, 615305. doi: 10.3389/fnins.2020.615305
Rea, M. S., Nagare, R., and Figueiro, M. G. (2022). Corrigendum: modeling circadian phototransduction: quantitative predictions of psychophysical data. Front. Neurosci. 16, 849800. doi: 10.3389/fnins.2022.849800
Sterne, J. A. C., Gavaghan, D., and Egger, M. (2000). Publication and related bias in meta-analysis: Power of statistical tests and prevalence in the literature. J. Clin. Epidemiol. 53, 1119–1129. doi: 10.1016/S0895-4356(00)00242-0
Strong, R. E., Marchant, B. K., Reimherr, F. W., Williams, E., Soni, P., and Mestas, R. (2009). Narrow-band blue-light treatment of seasonal affective disorder in adults and the influence of additional nonseasonal symptoms. Depress. Anxiety 26, 273–278. doi: 10.1002/da.20538
Sumaya, I. C., Rienzi, B. M., Deegan, J. F. II., and Moss, D. E. (2001). Bright light treatment decreases depression in institutionalized older adults: a placebo-controlled crossover study. J. Geront. A 56, M356–M360. doi: 10.1093/gerona/56.6.M356
Keywords: lighting therapy, circadian stimulus, depression, meta-analysis, non-visual effects
Citation: Zhou L, Hou D, Wang Y, Zhou S and Lin Y (2022) High circadian stimulus lighting therapy for depression: Meta-analysis of clinical trials. Front. Neurosci. 16:975576. doi: 10.3389/fnins.2022.975576
Received: 22 June 2022; Accepted: 20 September 2022;
Published: 06 October 2022.
Edited by:
Melissa A. St. Hilaire, Brigham and Women's Hospital and Harvard Medical School, United StatesReviewed by:
Mariana Figueiro, Icahn School of Medicine at Mount Sinai, United StatesCopyright © 2022 Zhou, Hou, Wang, Zhou and Lin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yandan Lin, eWRsaW5AZnVkYW4uZWR1LmNu
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.