
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurosci., 05 August 2022
Sec. Neurodegeneration
Volume 16 - 2022 | https://doi.org/10.3389/fnins.2022.934149
 Song Hwangbo1,2
Song Hwangbo1,2 Young Ju Kim1,2
Young Ju Kim1,2 Yu Hyun Park1,3
Yu Hyun Park1,3 Hee Jin Kim1,2
Hee Jin Kim1,2 Duk L. Na1,2,3,4
Duk L. Na1,2,3,4 Hyemin Jang1,2,5*†
Hyemin Jang1,2,5*† Sang Won Seo1,2,3,5,6*†
Sang Won Seo1,2,3,5,6*†Purpose: Many epidemiological studies suggest that lower education levels and vascular risk factors increase the likelihood of developing Alzheimer's disease dementia (ADD) and subcortical vascular dementia (SVaD). However, whether the brain-battering hypothesis can explain the relationship between education levels and the clinical diagnosis of dementia remains controversial. The objective of this study was to investigate whether vascular risk factors mediate the association between education level and the diagnosis of amyloid-beta positive (Aβ+) ADD and amyloid-beta negative (Aβ-) SVaD.
Methods: We analyzed 376 participants with Aβ normal cognition (Aβ- NC), 481 with Aβ+ ADD, and 102 with Aβ- SVaD. To investigate the association of education level and vascular risk factors with these diagnoses, multivariable logistic regression analysis was used, with age, sex, and APOE ε4 carrier status used as covariates. Path analysis was performed to investigate the mediation effects of hypertension on the diagnosis of Aβ- SVaD.
Results: The Aβ- SVaD group (7.9 ± 5.1 years) had lower education levels than did the Aβ- NC (11.8 ± 4.8 years) and Aβ+ ADD (11.2 ± 4.9 years) groups. The frequencies of hypertension and diabetes mellitus were higher in the Aβ- SVaD group (78.4 and 32.4%, respectively) than in the Aβ- NC (44.4 and 20.8%) and Aβ+ ADD (41.8 and 15.8%, respectively) groups. Increased education level was associated with a lower risk of Aβ- SVaD [odds ratio (OR) 0.866, 95% confidence interval (CI), 0.824–0.911], but not Aβ+ ADD (OR 0.971, 95% CI 0.940–1.003). The frequency of hypertension was associated with a higher risk of developing Aβ- SVaD (OR 3.373, 95% CI, 1.908–5.961), but not Aβ+ ADD (OR 0.884, 95% CI, 0.653–1.196). In the path analysis, the presence of hypertension partially mediated the association between education level and the diagnosis of Aβ- SVaD.
Conclusion: Our findings revealed that education level might influence the development of Aβ- SVaD through the brain-battering hypothesis. Furthermore, our findings suggest that suitable strategies, such as educational attainment and prevention of hypertension, are needed for the prevention of Aβ- SVaD.
Alzheimer's disease dementia (ADD), characterized by amyloid-beta (Aβ), and subcortical vascular dementia (SVaD), indicated by extensive white matter hyperintensities (WMH), are the two most common causes of dementia. Low educational attainment has been regarded as a risk factor for these two types of dementia (Katzman, 1993; Caamaño-Isorna et al., 2006; Sharp and Gatz, 2011). As one of the supporting hypotheses, the brain-battering hypothesis was suggested (Del Ser et al., 1999). This theory postulates that individuals with lower education are likely to have lower socioeconomic status (SES) that is subsequently related to lower health consciousness, bad habits, exposure to various toxins, and uncontrolled vascular risk factors than those with higher education and associated higher SES. Thus, individuals with lower education and more vascular risk factors are likely to develop brain pathologic burdens, which result in the development of dementia (Del Ser et al., 1999; Meng and D'Arcy, 2012). This brain-battering hypothesis is in comparison with the cognitive reserve (CR) theory which explains that lower educated individuals cannot cope with pathological changes in the brain and consequently are more likely to develop dementia. Thus, we consider that the CR theory explains the difference in clinical manifestation according to education when pathologic burdens are equal, while the brain-battering hypothesis may explain the difference in the probability of pathologic burden development according to education levels. Compared to the CR theory, the brain-battering hypothesis has been scarcely studied, especially in terms of its relation to two major pathologies of dementia.
To understand how a brain-battering hypothesis works in each phenotype, it is necessary to entangle the association between education, related risk factors, and each type of dementia. In fact, a previous study investigated this relationship, demonstrating that the association between education and risk of dementia was independent of SES, vascular or lifestyle characteristics (Ngandu et al., 2007). However, this study did not discriminate against dementia subtypes, which limits a separate interpretation in ADD and SVaD.
Considering that the brain-battering hypothesis is closely related to vascular risk factors, in this study, we aimed to examine the brain-battering hypothesis in two dementia subtypes by investigating whether two well-known vascular risk factors—hypertension and diabetes mellitus (DM)—mediate the association between education levels and the development of ADD and SVaD. Here, we used Aβ positron emission tomography (PET) imaging to discriminate a pure form of ADD (Aβ+ ADD) and SVaD (Aβ- SVaD) from patients with mixed or other possible pathologies. Many studies have suggested that vascular risk factors increase the development of dementia, especially SVaD (Launer et al., 2000; Kivipelto et al., 2005; Duron and Hanon, 2008; Rönnemaa et al., 2011; Caruso et al., 2019; Moretti and Caruso, 2020; Malik et al., 2021). However, it is controversial that vascular risk factors are directly associated with AD pathology (Chui et al., 2011). Therefore, we hypothesized that the brain-battering hypothesis would explain the relationship between education levels and the development of dementia in patients with Aβ- SVaD, rather than in patients with Aβ+ ADD (Scarmeas et al., 2003).
We consecutively recruited 2,274 participants from the memory clinic in the Department of Neurology at the Samsung Medical Center (SMC) in Seoul, Korea, between 2008 and 2020. All participants underwent brain magnetic resonance imaging (MRI) and Aβ PET, including 11C-PiB PET, 18F-florbetaben PET, and 18F-flutemetamol PET. Among them, 464 were normal cognition [NC], 589 were ADD, and 177 were SVaD. Participants with ADD met the National Institute on Aging-Alzheimer's Association diagnostic criteria (McKhann et al., 2011). Participants with SVaD met the criteria described in the Diagnostic and Statistical Manual of Mental Disorders–Fourth Edition (Bell, 1994) and had severe WMHs on fluid-attenuated inversion recovery (FLAIR) images (Kalaria and Erkinjuntti, 2006), which satisfied the following criteria: (1) WMH ≥10 mm in the periventricular white matter (caps or rim); and (2) WMH ≥25 mm (maximum diameter) in the deep white matter, consistent with extensive white matter lesions or diffusely confluent lesions. We excluded participants who met any of the following conditions: (1) WMH due to etiologies other than vascular pathology, such as radiation injury, multiple sclerosis, leukodystrophy, or metabolic/toxic disorders; and (2) the presence of cerebral infarction, including large territory infarction and small cortical infarction, brain tumor, or vascular malformation on MRI. Participants with NC comprised healthy controls who visited the memory clinic for early prevention of dementia, healthy volunteers for comprehensive dementia evaluation, and participants with subjective cognitive complaints. All participants with NC met the following criteria: (1) no medical history that is likely to affect cognitive function based on Christensen's health screening criteria (Christensen et al., 1991), (2) no objective cognitive impairment from a comprehensive neuropsychological test battery on any cognitive domains (at least –1.0 SD above age-adjusted norms on any cognitive tests); (3) independence in activities of daily living; and (4) no structural lesions or severe WMH on brain MRI.
All participants were assessed through clinical interviews and neurological examinations, and clinical diagnoses were established by consensus among a multidisciplinary team. Blood tests included complete blood count, blood chemistry, vitamin B12/folate measurement, syphilis serology, thyroid function test, and APOE genotyping. Participants were excluded if they had territorial infarctions, cortical strokes, brain tumors, or vascular malformations on MRI.
Written informed consent was obtained from all participants. This study was approved by the Institutional Review Board of the SMC. All procedures were performed in accordance with the approved guidelines.
All participants underwent Aβ PET: 11C-PiB PET scans were conducted in 117 participants, 18F-florbetaben PET scans in 521 participants, and 18F-flutemetamol PET scans in 592 participants at the SMC using a Discovery STE PET/computed tomography scanner (GE Medical Systems, Milwaukee, WI, United States). For 11C-PiB PET, a 30-min static emission PET scan was performed 60 min after a bolus injection of a mean dose of 420 MBq. For 18F-florbetaben PET and 18F-flutemetamol PET, a 20-min emission PET scan in dynamic mode (consisting of 4 × 5 min frames) was performed 90 min after an injection of a mean dose of 311.5 MBq and 197.7 MBq for 18F-florbetaben and 18F-flutemetamol, respectively.
11C-PiB PET was regarded as positive if the global PiB uptake value was >1.5 (Lee et al., 2011). Florbetaben PET was classified as positive if the amyloid-plaque load on the florbetaben PET scan was visually rated as 2 or 3 on the brain amyloid-plaque load scoring system, and flutemetamol PET was classified as positive when one of the five brain regions (frontal, parietal, posterior cingulate/precuneus, striatum, and lateral temporal lobes) systematically reviewed for flutemetamol PET was positive in either hemisphere (Kim et al., 2018). To include participants with relatively pure pathology, we excluded 108 (18.3%) participants with Aβ- ADD, 75 (42.4%) participants with Aβ+ SVaD, and 88 (19.0%) participants with Aβ+ NC.
T2, T1, FLAIR, and T2*-weighted GRE MRI images were acquired from all participants at the SMC using the same 3.0-Tesla MRI scanner (Philips, Best, the Netherlands). An Achieva 3.0-Tesla MRI scanner (Philips) was used to acquire three-dimensional T1 turbo field echo MRI data from all study participants, with the following imaging parameters: sagittal slice thickness, 1.0 mm with 50% overlap; no gap; repetition time, 9.9 ms; echo time, 4.6 ms; flip angle, 8°; and matrix size, 240 × 240 pixels reconstructed to 480 × 480 over a field view of 240 mm.
All participants underwent neuropsychological testing using the Seoul Neuropsychological Screening Battery 2nd edition for diagnostic purposes (Kang, and Na, 2012; Kang et al., 2019). The battery comprised tests for attention, language, calculation, praxis, visuospatial/constructive function, verbal/visual memory, and frontal executive function, as previously described (Seo et al., 2007).
Medical assessments were conducted by medically trained health professionals based on standard protocols. To evaluate the level of education, we inquired about participants' formal education in detail, including whether they had completed each educational level and the total duration of educational attainment. We identified the cardiometabolic risk factors as follows: hypertension (defined as the past medical history of hypertension or the participant taking any antihypertensive drugs at present), and diabetes mellitus (DM), defined as a previous history of DM or the participant currently taking insulin or oral anti-diabetic medications].
The demographic and clinical differences between Aβ- NC and Aβ+ ADD, or between Aβ- NC and Aβ- SVaD, were analyzed using the Student's t-test and chi-square test. To investigate the relationship between the measurement variables and dementia status, we performed multivariable logistic regression analysis including age, sex, hypertension status, DM status, APOE ε4 carrier status, and education level as covariates.
Path analysis was performed using the Mplus software (version 8.0) to investigate whether vascular risk factors mediate the effect of education on the development of dementia. Since our model had binary dependent variables and mediators, we used the weighted least squares method, which is widely used in the analysis of categorical variables (Muthén and Muthén, 1998; MacKinnon et al., 2007). Indirect, direct, and total effects were calculated to examine the effect of vascular risk factors on the relationship between education level and the development of dementia. First, we fitted a saturated model with all associations. Subsequently, we considered years of education as the predictor, vascular risk factors as the mediators, and dementia as the binary outcome variable, after controlling for age and sex.
The flowchart for the selection of study participants is shown in Figure 1. A total of 376 Aβ- NC, 481 Aβ+ ADD, and 102 Aβ- SVaD patients were finally included in the study. The clinical characteristics of the study participants are shown in Table 1. Aβ- SVaD (75.5 ± 7.1 years) was significantly older than Aβ- NC (70.1 ± 7.1 years) and Aβ+ ADD (70.0 ± 8.8 years) (p < 0.05). Aβ- SVaD had lower education (7.9 ± 5.1 years) than did Aβ- NC (11.8 ± 4.8 years) and Aβ+ ADD (11.2 ± 4.9 years) (p < 0.05). The prevalence of APOE4 carriers was higher in the Aβ+ ADD group (54.9%) than in the Aβ- SVaD (21.6%) and Aβ- NC (19.1%) groups. The frequencies of hypertension and DM were higher in the Aβ- SVaD group (78.4 and 32.4%, respectively) than in the Aβ+ ADD (41.8 and 15.8%, respectively) and Aβ- NC (44.4 and 20.8%, respectively) groups.
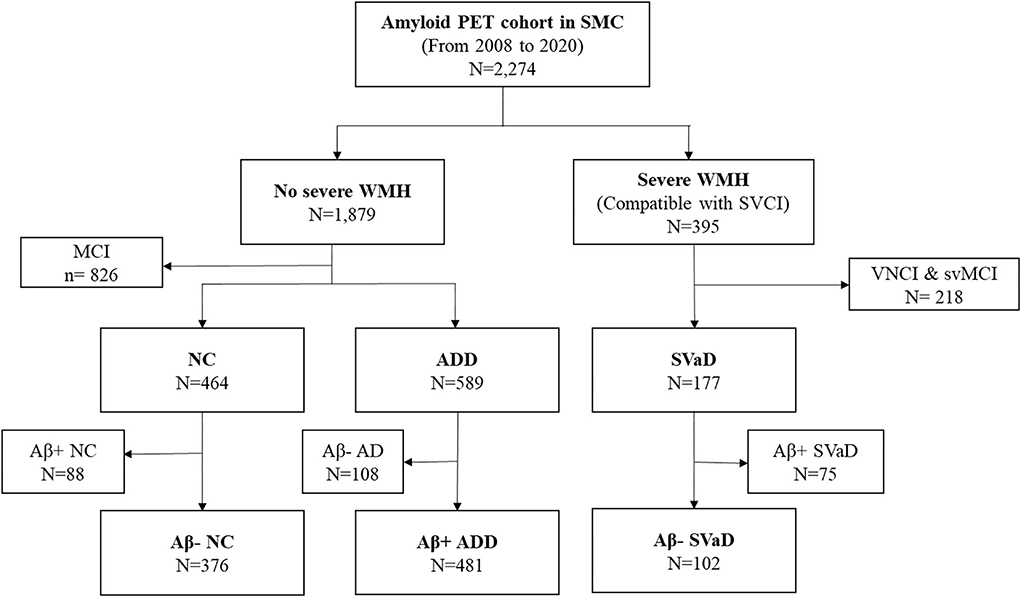
Figure 1. Flowchart for subjects selection. PET, positron emission tomography; SMC, Samsung medical center; WMH, white matter hyperintensities; MCI, mild cognitive impairment; VNCI, vascular no cognitive impairment; svMCI, subcortical vascular MCI; NC, normal cognition; ADD, Alzheimer's disease dementia; SVaD, subcortical vascular dementia.
Table 2 shows the results of multivariable logistic regression analysis for the clinical predictors of the Aβ+ ADD and Aβ- SVaD groups. An increased age independently predicted Aβ- SVaD [odds ratio (OR) 1.100, 95% confidence interval (CI), 1.059–1.143], but not Aβ+ ADD (OR 0.997, 95% CI, 0.979–1.015). An increase in the number of years of education was independently associated with Aβ- SVaD (OR: 0.866, 95% CI: 0.824–0.911) but not with Aβ+ ADD (OR 0.971, 95% CI 0.940–1.003). The presence of APOE4 carriers predicted Aβ+ ADD (OR 5.158, 95% CI, 3.760–7.075), but not Aβ- SVaD (OR 1.046, 95% CI, 0.556–1.967). The frequency of hypertension was independently associated with Aβ- SVaD (OR 3.373, 95% CI, 1.908–5.961), but not with Aβ+ ADD (OR 0.884, 95% CI, 0.653–1.196).
To verify whether hypertension and DM act as mediators in the relationship between educational level and Aβ- SVaD, the dementia type which low education was only associated with, we analyzed a mediated model, as shown in Figure 1. In the relationship between education and Aβ- SVaD, lower education was associated with a higher risk of Aβ- SVaD [total effect, β = 0.090, standard error (SE)= 0.016, p < 0.001]. In a mediation analysis between education, hypertension, and Aβ- SVaD, lower education was associated with a higher risk of hypertension (p = 0.004), which was further associated with a higher risk of SVaD (p = 0.001) [indirect effect, β = −0.015; SE = 0.007; p = 0.037; Bootstrap 95% confidence interval (CI) −0.033, −0.004]. In addition, lower education was directly associated with a higher risk of SVaD, even without the mediation of hypertension (direct effect, β = −0.084; SE = 0.016; p < 0.001). In terms of the relationship between education, DM, and Aβ- SVaD, education was not associated with DM (p = 0.556), and DM was not associated with a risk of Aβ- SVaD (p = 0.480), which supported that DM did not mediate the relationship between education and Aβ- SVaD (indirect effect, β = −0.001; SE = 0.002; p = 0.759; Bootstrap 95% CI −0.007, 0.003). The chi-square test of model fit for the baseline model showed a value of 173.230 with p-value < 0.001 (Figure 2; Table 3).
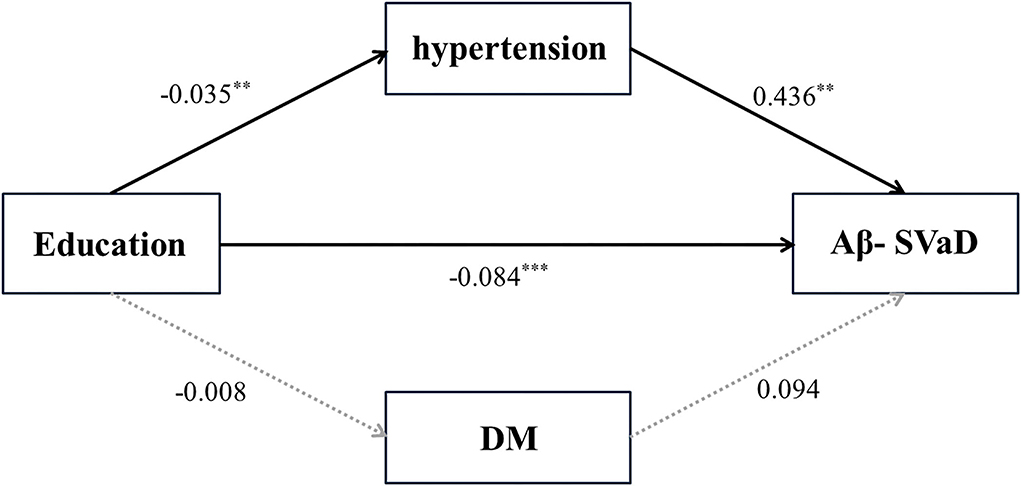
Figure 2. Path analysis of education levels and vascular risk factors for dementia. DM, diabetes mellitus, SVaD, subcortical vascular dementia; β, unstandardized beta; SE, standard error. **p-value < 0.005, ***p-value < 0.001.
In this study, we investigated the effects of vascular risk factors on the association between educational level and the risk of developing Aβ+ ADD or Aβ- SVaD. The major findings of our study are as follows. First, lower education levels were associated with a higher risk of Aβ- SVaD. Second, the presence of vascular risk factors, particularly hypertension, was also related to a higher risk of Aβ- SVaD, but not Aβ+ ADD. Finally, path analysis showed that the presence of hypertension, but not DM, partially mediated the relationship between education level and diagnosis of Aβ- SVaD. Considered together, our findings suggest that education level might influence the development of Aβ- SVaD through the brain-battering hypothesis, which particularly involves deleterious effects of hypertension. Furthermore, our findings suggest that suitable strategies, such as education and the prevention of hypertension, are needed to prevent Aβ- SVaD.
Our first major finding was that lower education level was associated with Aβ- SVaD, which is consistent with the results of previous studies. One previous study revealed that cerebral small vessel disease (CSVD), such as subcortical lacunar infarcts, white matter lesions, and macroscopic infarcts, was more frequent in individuals with lower education levels (64% incidence in individuals with a below high school education level vs. 37% incidence in individuals who had graduated high school) (Del Ser et al., 1999). These results suggest that lower education levels were correlated with increased risk for SVaD, as SVaD is characterized by extensive CSVD (Erkinjuntti et al., 2000). Another Aβ PET-based study also found that participants with Aβ- SVaD (8.1 years) have lower levels of education than did the participants with Aβ+ ADD (10.5 years) or Aβ- NC (13.9 years) (Yoon et al., 2013). Although lower educational attainment has been generally regarded as a risk factor for the clinical diagnosis of ADD, in this study, there was no significant correlation between lower levels of education and the diagnosis of Aβ+ ADD (Katzman, 1993; Munoz et al., 2000; Caamaño-Isorna et al., 2006; Sharp and Gatz, 2011). This contradicting result might be related to the different study populations, such as the inclusion of Aβ+ ADD in this study in comparison to a clinical diagnosis of ADD in previous studies (Alexander et al., 1997; Scarmeas et al., 2003; Kemppainen et al., 2008; Meng and D'Arcy, 2012). Our findings were also supported by previous studies revealing no significant association between lower education levels and amyloid pathology (Jansen et al., 2015; Gottesman et al., 2016; Insel et al., 2016; Landau et al., 2016). Therefore, we consider that high education is not a protective factor for AD pathology, alternatively, it might be due to selection bias which excludes low-educated individuals with AD pathology who do not visit a clinic.
In this study, as expected, we observed a positive association between hypertension and Aβ- SVaD. The mechanism and effects of hypertension on the risk of development of SVD and subsequent SVaD have been well-elaborated in previous studies (Caruso et al., 2019; Moretti and Caruso, 2020). One of the main pathomechanisms underlying SVD is arteriolosclerosis caused by hypertension and subsequent hypoperfusion. However, in terms of dementia progression in individuals with SVD, it is also argued that hypotension rather than hypertension is more important (Moretti et al., 2008; Caruso et al., 2019; Moretti and Caruso, 2020). In this study, we simply used the presence of hypertension as a predictor, instead of many hypertension-related risk factors such as pulse pressure, hypotension, or interaction with age, which should be investigated further to help in the interpretation of underlying mechanisms leading to SVaD. In terms of the relationship between hypertension and ADD, we did not find any relationship between hypertension and Aβ+ ADD, although previous studies have shown that hypertension increases the risk of the development of ADD (Kivipelto et al., 2002; Qiu et al., 2003; Skoog and Gustafson, 2006; Purnell et al., 2009). This inconsistency may have come from a lack of biomarker information in the previous ADD population. In fact, our findings were supported by previous studies that indicated that there was no significant association between hypertension and amyloid pathology (Gottesman et al., 2017). Unexpectedly, DM was not associated with the risk of Aβ- SVaD (Abner et al., 2015); rather, DM was negatively associated with Aβ+ ADD. Our findings might be related to previous studies showing a negative association between amyloid pathology and DM (Beeri et al., 2005; Nelson et al., 2009; Sonnen et al., 2009; Ahtiluoto et al., 2010; Kang et al., 2021). Therefore, it is possible that DM affects cognitive decline through non-amyloid pathology.
Our final major finding was that the presence of hypertension (but not DM) partially mediated the association between lower educational levels and the diagnosis of Aβ- SVaD. Our findings are consistent with the brain-battering hypothesis. That is, a lower level of education might be related to a lower socioeconomic status (SES), which might be related to higher exposure to toxins, and less healthy lifestyles, such as irregular or unhealthy diet, smoking and alcohol consumption, and poor access to medical care (Del Ser et al., 1999; Yoon et al., 2013). Furthermore, the development of hypertension and poorly-controlled hypertension induced by lower SES might eventually result in the development of Aβ- SVaD. Interestingly, another pathway was observed between lower levels of education and Aβ- SVaD, without the mediation of hypertension. This pathway might be related to the effects of lower educational attainment on the development of Aβ- SVaD through other unmeasured risk factors or imaging markers for detecting changes in brain structure and function, which we did not investigate. Additionally, the above mediation effects did not correspond to the relation between education, DM, and Aβ- SVaD. This might suggest that the presence of DM itself is not mainly affected by low education or related low SES, and it is not associated with Aβ- SVaD. We should look into the relation between DM and dementia more closely, by investigating whether unmeasured DM-related risk factors such as glycemic variability or hypoglycemia have a role in the development of different types of dementia.
The strength of our study lies in its well-characterized and large cohort of patients who underwent Aβ PET and structural MRI according to standardized protocols. However, our study had several limitations that should be addressed. First, because of the cross-sectional study design, the causal relationship between education level, vascular risk factors, and the development of ADD or SVaD remains unclear. Therefore, future longitudinal studies are required to determine temporal relationships. Second, because we intentionally excluded subjects with mixed dementia (Aβ+ SVaD) to clarify and separately investigate the relation between education, vascular risk factors, and either of two major pathologies, this study cannot be generalizable to mixed dementia cases which are common in old age. In contrast, we used Aβ PET and MRI for severe WMH to diagnose pure ADD and pure SVaD—the possibility of other mixed pathologies could not be ruled out, owing to the lack of histopathological confirmation. Third, we could not directly measure and consider SES in the model, which might partially explain the association between education and the risk of developing SVaD. Finally, we could not consider other newly-acknowledged vascular risk factors (such as homocysteine, folate, or vitamin deficiency) or the downstream imaging markers of brain pathological changes (such as the volume of WMH, number of lacunes, and cortical thickness), but instead used hypertension or DM as an independent variable and each specific dementia subtype (ADD and SVaD) as the dependent variable. Therefore, further research on path analysis, including these various variables as mediators, is needed to understand the association between education, vascular risk factors, and each pathological marker. However, our study is noteworthy because we included biomarker-guided diagnoses of ADD and SVaD and used a simple study design to demonstrate the association between education level, hypertension, and SVaD.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by Samsung Medical Center. The patients/participants provided their written informed consent to participate in this study.
Conceptualization: SH, HJ, HK, DN, and SS. Methodology: SH, HJ, and SS. Formal analysis and investigation: SH, YK, YP, and HK. Writing—original draft preparation: SH and HJ. Writing—review and editing: SH, YK, HJ, and SS. Funding acquisition: SS. Supervision: HJ, DN, and SS. All authors contributed to manuscript revision, read, and approved the submitted version.
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health and Welfare and Ministry of Science and ICT, Republic of Korea (grant number: HU20C0111), the Ministry of Health Welfare, Republic of Korea (grant number: HR21C0885), and the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (NRF-2020R1A2C1009778). This study was also supported by Future Medicine 2030 Project of the Samsung Medical Center (#SMX1210771), a grant of the Korean Health Technology R&D Project, Ministry of Health and Welfare, Republic of Korea (HI19C1132), and the National Institute of Health Research Project (2021-ER1006-01).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abner, E. L., Nelson, P. T., Kryscio, R. J., Schmitt, F. A., Fardo, D. W., Woltjer, R. L., et al. (2015). (2016). Diabetes is associated with cerebrovascular but not Alzheimer's disease neuropathology. Alzheimers Dement. 12, 882–889. doi: 10.1016/j.jalz.2015.12.006
Ahtiluoto, S., Polvikoski, T., Peltonen, M., Solomon, A., Tuomilehto, J., Winblad, B., et al. (2010). Diabetes, Alzheimer disease, and vascular dementia: a population-based neuropathologic study. Neurology 75, 1195–1202. doi: 10.1212/WNL.0b013e3181f4d7f8
Alexander, G. E., Furey, M. L., Grady, C. L., Pietrini, P., Brady, D. R., Mentis, M. J., et al. (1997). Association of premorbid intellectual function with cerebral metabolism in Alzheimer's disease: implications for the cognitive reserve hypothesis. Am. J. Psychiatry 154, 165–1672. doi: 10.1176/ajp.154.2.165
Beeri, M. S., Silverman, J. M., Davis, K. L., Marin, D., Grossman, H. Z., Schmeidler, J., et al. (2005). Type 2 diabetes is negatively associated with Alzheimer's disease neuropathology. J. Gerontol. A Biol. Sci. Med. Sci. 60, 471–475. doi: 10.1093/gerona/60.4.471
Bell, C. C.. (1994). DSM-IV: diagnostic and statistical manual of mental disorders. JAMA 272, 828–829. doi: 10.1001/jama.1994.03520100096046
Caamaño-Isorna, F., Corral, M., Montes-Martínez, A., and Takkouche, B. (2006). Education and dementia: a meta-analytic study. Neuroepidemiology 26, 226–232. doi: 10.1159/000093378
Caruso, P., Signori, R., and Moretti, R. (2019). Small vessel disease to subcortical dementia: a dynamic model, which interfaces aging, cholinergic dysregulation and the neurovascular unit. Vasc. Health Risk Manag. 15, 259–281. doi: 10.2147/VHRM.S190470
Christensen, K. J., Multhaup, K. S., Nordstrom, S., and Voss, K. (1991). A cognitive battery for dementia: development and measurement characteristics. Psychol. Assess. J. Consult. Clin. Psychol. 3, 168. doi: 10.1037/1040-3590.3.2.168
Chui, H. C., Zheng, L., Reed, B. R., Vinters, H. V., and Mack, W. J. (2011). Vascular risk factors and Alzheimer's disease: are these risk factors for plaques and tangles or for concomitant vascular pathology that increases the likelihood of dementia? An evidence-based review. Alzheimers Res. Ther. 3, 1–13. doi: 10.1186/alzrt98
Del Ser, T., Hachinski, V., Merskey, H., and Munoz, D. G. (1999). An autopsy-verified study of the effect of education on degenerative dementia. Brain 122, 2309–2319. doi: 10.1093/brain/122.12.2309
Duron, E., and Hanon, O. (2008). Vascular risk factors, cognitve decline, and dementia. Vasc. Health Risk Manag. 4, 363. doi: 10.2147/VHRM.S1839
Erkinjuntti, T., Inzitari, D., Pantoni, L., Wallin, A., Scheltens, P., Rockwood, K., et al. (2000). Research criteria for subcortical vascular dementia in clinical trials. J. Neural Transm. Suppl. 59, 23–30. doi: 10.1007/978-3-7091-6781-6_4
Gottesman, R. F., Schneider, A. L., Zhou, Y., Chen, X., Green, E., Gupta, N., et al. (2016). The ARIC-PET amyloid imaging study: brain amyloid differences by age, race, sex, and APOE. Neurology 87, 473–480. doi: 10.1212/WNL.0000000000002914
Gottesman, R. F., Schneider, A. L., Zhou, Y., Coresh, J., Green, E., Gupta, N., et al. (2017). Association between midlife vascular risk factors and estimated brain amyloid deposition. JAMA 317, 1443–1450. doi: 10.1001/jama.2017.3090
Insel, P. S., Palmqvist, S., Mackin, R. S., Nosheny, R. L., Hansson, O., Weiner, M. W., et al. (2016). Assessing risk for preclinical β-amyloid pathology with APOE, cognitive, and demographic information. Alzheimers Dement. 4, 76–84. doi: 10.1016/j.dadm.2016.07.002
Jansen, W. J., Ossenkoppele, R., Knol, D. L., Tijms, B. M., Scheltens, P., Verhey, F. R., et al. (2015). Prevalence of cerebral amyloid pathology in persons without dementia: a meta-analysis. JAMA. 313, 1924–1938. doi: 10.1001/jama.2015.4668
Kalaria, R. N., and Erkinjuntti, T. (2006). Small vessel disease and subcortical vascular dementia. J. Clin. Neurol. 2, 1–11. doi: 10.3988/jcn.2, 1.1
Kang, S. H., Kim, M. E., Jang, H., Kwon, H., Lee, H., Kim, H. J., et al. (2021). Amyloid positivity in Alzheimer/subcortical-vascular spectrum. Neurology 96, e2201–e2211. doi: 10.1212/WNL.0000000000011833
Kang, S. H., Park, Y. H., Lee, D., Kim, J. P., Chin, J., Ahn, Y., et al. (2019). The Cortical Neuroanatomy related to specific neuropsychological deficits in Alzheimer's continuum. Dement. Neurocogn. Disord. 18, 77–95. doi: 10.12779/dnd.2019.18.3.77
Kang, Y.J. S, and Na, D. L. (2012). Seoul Neuropsychological Screening Battery, 2nd Edn. Seoul: Human Brain Research and Consulting Co.
Katzman, R.. (1993). Education and the prevalence of dementia and Alzheimer's disease. Neurology. 43, 13–20. doi: 10.1212/WNL.43.1_Part_1.13
Kemppainen, N. M., Aalto, S., Karrasch, M., Någren, K., Savisto, N., Oikonen, V., et al. (2008). Cognitive reserve hypothesis: Pittsburgh Compound B and fluorodeoxyglucose positron emission tomography in relation to education in mild Alzheimer's disease. Ann. Neurol. 63, 112–118. doi: 10.1002/ana.21212
Kim, S. E., Woo, S., Kim, S. W., Chin, J., Kim, H. J., Lee, B. I., et al. (2018). A nomogram for predicting amyloid PET positivity in amnestic mild cognitive impairment. J. Alzheimers. Dis. 66, 681–691. doi: 10.3233/JAD-180048
Kivipelto, M., Helkala, E-. L., Laakso, M. P., Hänninen, T., Hallikainen, M., Alhainen, K., et al. (2002). Apolipoprotein E ε4 allele, elevated midlife total cholesterol level, and high midlife systolic blood pressure are independent risk factors for late-life Alzheimer disease. Ann. Intern. Med. 137, 149–155. doi: 10.7326/0003-4819-137-3-200208060-00006
Kivipelto, M., Ngandu, T., Fratiglioni, L., Viitanen, M., Kåreholt, I., Winblad, B., et al. (2005). Obesity and vascular risk factors at midlife and the risk of dementia and Alzheimer disease. Arch. Neurol. 62, 1556–1560. doi: 10.1001/archneur.62.10.1556
Landau, S. M., Horng, A., Fero, A., and Jagust, W. J. (2016). Amyloid negativity in patients with clinically diagnosed Alzheimer disease and MCI. Neurology 86, 1377–1385. doi: 10.1212/WNL.0000000000002576
Launer, L. J., Ross, G. W., Petrovitch, H., Masaki, K., Foley, D., White, L. R., et al. (2000). Midlife blood pressure and dementia: the Honolulu-Asia aging study. Neurobiol. Aging 21, 49–55. doi: 10.1016/S0197-4580(00)00096-8
Lee, J. H., Kim, S. H., Kim, G. H., Seo, S. W., Park, H. K., Oh, S. J., et al. (2011). Identification of pure subcortical vascular dementia using 11C-Pittsburgh compound B. Neurology 77, 18–25. doi: 10.1212/WNL.0b013e318221acee
MacKinnon, D. P., Lockwood, C. M., Brown, C. H., Wang, W., and Hoffman, J. M. (2007). The intermediate endpoint effect in logistic and probit regression. Clin. Trials 4, 499–513. doi: 10.1177/1740774507083434
Malik, R., Georgakis, M. K., Neitzel, J., Rannikmäe, K., Ewers, M., Seshadri, S., et al. (2021). Midlife vascular risk factors and risk of incident dementia: longitudinal cohort and Mendelian randomization analyses in the UK Biobank. Alzheimers. Dement. 17, 1422–1431. doi: 10.1002/alz.12320
McKhann, G. M., Knopman, D. S., Chertkow, H., Hyman, B. T., Jack, C. R. Jr., Kawas, C. H., et al. (2011). The diagnosis of dementia due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement. 7, 263–269. doi: 10.1016/j.jalz.2011.03.005
Meng, X., and D'Arcy, C. (2012). Education and dementia in the context of the cognitive reserve hypothesis: a systematic review with meta-analyses and qualitative analyses. PLoS ONE. 7, e38268. doi: 10.1371/journal.pone.0038268
Moretti, R., and Caruso, P. (2020). Small vessel disease-related dementia: an invalid neurovascular coupling? Int. J. Mol. Sci. 21, 1095. doi: 10.3390/ijms21031095
Moretti, R., Torre, P., Antonello, R. M., Manganaro, D., Vilotti, C., Pizzolato, G., et al. (2008). Risk factors for vascular dementia: hypotension as a key point. Vasc. Health Risk Manag. 4, 395–402. doi: 10.2147/VHRM.S2434
Munoz, D. G., Ganapathy, G. R., Eliasziw, M., and Hachinski, V. (2000). Educational attainment and socioeconomic status of patients with autopsy-confirmed Alzheimer disease. Arch. Neurol. 57, 85–89. doi: 10.1001/archneur.57.1.85
Muthén, L., and Muthén, B. (1998). Mplus user's guide Eighth edition. Los Angeles, CA: Muthén and Muthén.
Nelson, P. T., Smith, C. D., Abner, E. A., Schmitt, F. A., Scheff, S. W., Davis, G. J., et al. (2009). Human cerebral neuropathology of Type 2 diabetes mellitus. Biochim. Biophys. Acta. 1792, 454–469. doi: 10.1016/j.bbadis.2008.08.005
Ngandu, T., von Strauss, E., Helkala, E.-L., Winblad, B., Nissinen, A., Tuomilehto, J., et al. (2007). Education and dementia: what lies behind the association? Neurology 69, 1442–1450. doi: 10.1212/01.wnl.0000277456.29440.16
Purnell, C., Gao, S., Callahan, C. M., and Hendrie, H. C. (2009). Cardiovascular risk factors and incident Alzheimer disease: a systematic review of the literature. Alzheimer Dis. Assoc. Disord. 23, 1. doi: 10.1097/WAD.0b013e318187541c
Qiu, C., Winblad, B., Fastbom, J., and Fratiglioni, L. J. N. (2003). Combined effects of APOE genotype, blood pressure, and antihypertensive drug use on incident AD. Neurology 61, 655–660. doi: 10.1212/WNL.61.5.655
Rönnemaa, E., Zethelius, B., Lannfelt, L., and Kilander, L. (2011). Vascular risk factors and dementia: 40-year follow-up of a population-based cohort. Dement. Geriatr. Cogn. Disord. 31, 460–466. doi: 10.1159/000330020
Scarmeas, N., Zarahn, E., Anderson, K. E., Habeck, C. G., Hilton, J., Flynn, J., et al. (2003). Association of life activities with cerebral blood flow in Alzheimer disease: implications for the cognitive reserve hypothesis. Arch. Neurol. 60, 359–365. doi: 10.1001/archneur.60.3.359
Seo, S. W., Im, K., Lee, J. M., Kim, Y. H., Kim, S. T., Kim, S. Y., et al. (2007). Cortical thickness in single- versus multiple-domain amnestic mild cognitive impairment. Neuroimage 36, 289–297. doi: 10.1016/j.neuroimage.2007.02.042
Sharp, E. S., and Gatz, M. (2011). elationship between education and dementia: an updated systematic review. Alzheimer Dis. Assoc. Disord. 25, 289–304. doi: 10.1097/WAD.0b013e318211c83c
Skoog, I., and Gustafson, D. (2006). Update on hypertension and Alzheimer's disease. Neurol. Res. 28, 605–611. doi: 10.1179/016164106X130506
Sonnen, J. A., Larson, E. B., Brickell, K., Crane, P. K., Woltjer, R., Montine, T. J., et al. (2009). Different patterns of cerebral injury in dementia with or without diabetes. Arch. Neurol. 66, 315–322. doi: 10.1001/archneurol.2008.579
Keywords: Alzheimer's disease, vascular dementia, education, hypertension, vascular risk factor
Citation: Hwangbo S, Kim YJ, Park YH, Kim HJ, Na DL, Jang H and Seo SW (2022) Relationships between educational attainment, hypertension, and amyloid negative subcortical vascular dementia: The brain-battering hypothesis. Front. Neurosci. 16:934149. doi: 10.3389/fnins.2022.934149
Received: 09 June 2022; Accepted: 08 July 2022;
Published: 05 August 2022.
Edited by:
Fabricio Ferreira de Oliveira, Elysian Clinic, BrazilReviewed by:
Renata Kochhann, Hospital Moinhos de Vento, BrazilCopyright © 2022 Hwangbo, Kim, Park, Kim, Na, Jang and Seo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hyemin Jang, aG1qYW5nNTdAZ21haWwuY29t; Sang Won Seo, c2FuZ3dvbnNlb0BlbXBhbC5jb20=; c3c3Mi5zZW9Ac2Ftc3VuZy5jb20=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.