- 1Graduate College, Beijing University of Chinese Medicine, Beijing, China
- 2Department of Geriatrics, Xiyuan Hospital, China Academy of Chinese Medical Sciences, Beijing, China
- 3Wangjing Hospital, China Academy of Chinese Medical Sciences, Beijing, China
- 4First Clinical College, Shandong University of Traditional Chinese Medicine, Jinan, China
Introduction: The second most prevalent cause of dementia is vascular dementia (VaD). Furthermore, acupuncture is a relatively safe and effective traditional therapy for individuals with VaD. We performed a network meta-analysis to assess the effectiveness and safety of various acupuncture therapies for VaD based on existing research.
Methods: We searched six electronic databases to screen for randomized controlled trials (RCTs) comparing different acupuncture treatments in VaD patients. The Cochrne tool (Review Manager 5.3) was used to evaluate the risk of bias of the included RCTs. Based on the Grading of Recommendations Assessment, Development and Evaluation framework, we assessed the confidence in the evidence using the Confidence In the results from Network Meta-Analysis approach. We used the frequency approach to perform the network meta-analysis. Data were analyzed using R 4.1.1.
Results: In total, we included 46 eligible studies. The results of the network analysis showed that the combined interventions of moxibustion (MB) with body acupuncture (BA) (MB + BA) and electroacupuncture (EA) with scalp acupuncture (SA) with BA (EA + SA + BA) were more effective in improving cognitive functions and activities of daily living compared with SA or BA alone. However, in the subgroup analysis, EA + SA + BA showed better efficacy in short- and mid-term acupuncture compared with other acupuncture therapies.
Conclusion: Combined acupuncture therapy may be a safe and effective intervention for individuals with VaD, and MB + BA and EA + SA + BA appear to be the most effective interventions. However, because the analysis of this study was based on low-to-moderate evidence, there remains no strong supporting evidence. Thus, high-quality, large-scale, and long-term studies should be conducted in the future to assess the effectiveness and safety of acupuncture in VaD.
Systematic review registration: https://www.crd.york.ac.uk/prospero/, identifier: CRD42022354573.
Introduction
Vascular dementia (VaD) is the second most prevalent cause of dementia (Yang et al., 2022), accounting for roughly 15% to 20% of dementia cases in North America and Europe, and about 30% of dementia cases in Asia (Wolters and Ikram, 2019). The risk of VaD doubles every 5.3 years, with the incidence rate increasing with age. Age-related dementia has become one of the major health problems worldwide (Iadecola et al., 2019). According to the World Health Organization, 35.6 million individuals worldwide suffer from dementia, and this figure is anticipated to quadruple by 2050 (World Health, 2012), which would place a huge burden on families, primary caregivers, and the economic cost to society. In the United States, such costs have exceeded those of cancer and heart disease (Hurd et al., 2013). Although the average cognitive impairment rates of VaD and Alzheimer's disease are similar, the mortality rate is higher in VaD than that in Alzheimer's disease (Kua et al., 2014). Therefore, there is an urgent need to identify suitable treatments for VaD.
VaD is characterized by progressive deterioration of memory and other cognitive functions due to cerebrovascular disease. The major cause of VaD is chronic cerebral hypoperfusion (Wang et al., 2020) and tissue hypoxia (Iadecola et al., 2019) after cerebral ischemia, which enhances the permeability of the blood-brain barrier permeability and plasma protein extravasation into the brain, resulting in a severe inflammatory response and oxidative stress, further leading to white matter damage (Rouhl et al., 2012). Although several advancements have been made in understanding the relationship between cerebrovascular disease and dementia, the underlying pathogenesis of VaD remains poorly understood. Currently, beneficial therapies include cholinesterase inhibitors and memantine, which are licensed drugs for Alzheimer's disease (O'Brien and Thomas, 2015). Several large studies have shown that cholinesterase inhibitors and memantine are effective in the treatment of VaD; however, the magnitude of their effectiveness is limited. Therefore, the regulators and guideline panels of these trials have recommended that memantine and cholinesterase inhibitors are inappropriate for the treatment of patients with VaD (Joshua et al., 2018). The same phenomenon is observed with N-methyl-D-aspartate antagonists (Orgogozo et al., 2002; Wilcock et al., 2002). For these reasons, alternative approaches, including acupuncture, have been adopted for VaD.
Acupuncture, which is a traditional Chinese medical therapy, is one of the most commonly employed non-pharmacological therapies, and has been used in many countries for the treatment of neurological disorders (Wu et al., 2010; Wan et al., 2016). Accumulated evidence has also shown that acupuncture can improve the symptoms of VaD through its antioxidant, anti-inflammatory, and anti-apoptotic effects (Ye et al., 2017; Yang et al., 2018; Zhu et al., 2018). The network meta-analysis (NMA) method is effective for comparing and ranking various therapies; therefore, this study aimed to assess the efficacy and safety of different acupuncture techniques for the treatment of patients with VaD, and to determine the most suitable method for the acupuncture treatment of VaD.
Methods
This review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses for Network Meta-Analyses (Moher et al., 2009; Page et al., 2021). In addition, our study protocol has been registered with the International Prospective Register of Systematic Reviews (PROSPERO) (registration number: CRD42022354573).
Search strategy for identification of studies
We conducted a systematic search of six databases, including PubMed, Cochrane Library, Embase, Web of Science, MEDLINE, and China National Knowledge Infrastructure, from their establishment on July 31, 2022. The following keywords were used during the search: (acupuncture therapy, acupuncture, acupuncture treatment, electro-acupuncture, needling, scalp acupuncture, electrostimulation, body acupuncture, electroacupuncture, moxibustion) and (dementia, vascular dementia, infarct dementia, post-stroke dementia, and vascular cognitive impairment). We adjusted and specified the retrieval strategies according to the different databases. The specifics of the search strategies are listed in the Supplementary Appendix 1.
Study selection
Two reviewers (JYW and SRC) independently evaluated the included studies. Any discrepancies were reviewed by a third reviewer (ZZ) and resolved by discussion among all the reviewers. Included studies fulfilled the following criteria: (i) randomized controlled trials (RCTs); (ii) included patients who matched the established diagnostic criteria for VaD, including the Diagnostic and Statistical Manual of Mental Disorders, the National Institute of Neurological Disorders and Stroke, and the Association Internationale pour la Recherche et l'Enseignement en Neurosciences criteria, Hachinski Ischemic Score ≥ 7, and the outcomes of computed tomography or magnetic resonance imaging; (iii) types of acupuncture included were electroacupuncture (EA), scalp acupuncture (SA) (including traditional SA and modern SA) (Jian-Li et al., 2019), body acupuncture (BA), and moxibustion (MB); and (iv) the control group received sham acupuncture, blank control, wait-list control and anti-dementia medications (for whom the observation group used acupuncture combined with anti-dementia medications). Studies that met the following criteria were excluded: (i) comprised of patients with Alzheimer's disease or dementia caused by other factors; (ii) included patients with Hachinski Ischemic Score < 7; (iii) included patients with a score > 8 on the Cornell Scale for Depression in Dementia and who were diagnosed according to the Diagnostic and Statistical Manual of Mental Disorders criteria as having evident mental depression, or patients with other mental diseases or disorders; and (iv) included patients with severe neurological deficits or serious medical conditions, such as dysopia, aphasia and dysacusis, and malignancy.
Data abstraction
Two reviewers (JYW and QYH) independently extracted data from the included RCTs. The extracted data included study characteristics such as first author, title of study, participants (sex, age, month of diagnoses, sample sizes), study design (randomization, blinding), interventions, controlled interventions, outcome measures, results and adverse events, we recorded these characteristics in advance. The four categories of acupuncture treatments were EA, SA, BA, and MB. The control groups included patients receiving anti-dementia medications, for whom the observation group used acupuncture combined with anti-dementia medications; sham acupuncture; blank control; wait-list control. Any discrepancies were evaluated by a third reviewer (JXY) and resolved by discussion among all the reviewers.
Outcomes
The Mini-Mental State Examination (MMSE) and Hasegawa Dementia Scale (HDS) were defined as the primary efficiency outcome measures. When more than one measure of cognitive function was used in a study, we preferentially used the MMSE in all cases for inclusion in our meta-analysis. However, due to the high similarity in scoring criteria, total score and content between MMSE and HDS (Kim et al., 2005; Senda et al., 2020), we included a very small number of HDS scores to analyze together. The Barthel Index of ADLs and activities of daily living (ADLs) were identified as the secondary efficacy outcome indicators.
Quality assessment
Two independent reviewers (SRC and WW) evaluated the identified trials. The revised Cochrane risk-of-bias tool for randomized trials (Review Manager 5.3) was used to assess the bias risk of the included RCTs. Any disagreements were reviewed by a third reviewer (QYH) and resolved by discussion among all the reviewers.
Data synthesis and analysis
A pairwise meta-analysis was performed in this study using the random-effects model in Stata 14 (StataCorp LLC, College Station, Texas 77845, USA). Then, the “netmeta” version 0.9–2 of the R-4.1.1 software was used to conduct a frequentist NMA (Rücker, 2012; Krahn et al., 2013) in this study. To display and describe the geometric features of different acupuncture treatments, we used the “networkPlot” function of Stata 14 (College Station, Texas 77,845 USA) to draw and generate network graphs. Different nodes represented different treatments, and edges represented head-to-head comparisons between different treatments. We used the “decomp.design” function to evaluate the consistency of entire network, homogeneity within designs, and homogeneity/consistency between designs. We used a node-splitting method (Rücker and Schwarzer, 2015) to evaluate the inconsistency between direct and indirect comparisons. The different interventions were ranked in accordance with the P-score, which were based only on the standard errors of the network and point estimations. These scores, which gauge the degree of certainty between comparisons of different interventions, are averaged across all competing treatments (Brehm et al., 2009).
We calculated pooled estimates and 95% confidence intervals (95% CIs) by performing a random-effects NMA. Generally speaking, when studies use the same evaluation method to assess our results of interest, the mean difference in the change scores between the final and baseline scores on the scale was regarded as a treatment effect to evaluate the outcomes. Since lower scores represented more severe cognitive impairment, the final minus the baseline scores served as the change scores definition. One treatment was considered more effective than the other if the corresponding estimate of the mean difference in the change score was positive and the 95% CI did not include zero.
Moreover, to investigate the probable sources of heterogeneity more thoroughly in this study, we performed subgroup analyses according to different acupuncture treatment durations. Based on the duration of treatment, all results from the included studies were divided into three groups i.e., short-term (1 ≤ × ≤ 30 days), mid-term (30 < × ≤ 60 days), and long-term (× > 60 days).
Assessing confidence of the evidence
Confidence in the results from Network Meta-Analysis (CINeMA) was used to assess the confidence of the evidence in all the trials, and ratings were assigned using the CINeMA application (Nikolakopoulou et al., 2020).
CINeMA evaluates six domains as follows: within-study bias, reporting bias, indirectness, imprecision, heterogeneity, and incoherence. With the exception of reporting bias, which is classified as suspect or undetected, they are graded as no concerns, some concerns, or major concerns. The conclusions are then presented for each treatment comparison across these six dimensions as high, moderate, low, or very low confidence (Papakonstantinou et al., 2020).
All or most comparisons from industry-funded trials were considered to be at a risk of reporting bias. For comparisons with poor network connections, indirection is downgraded. For imprecision, the threshold was set to a mean difference of 0 for continuous comparisons.
Results
Study identification
For the present study, a total of 1,814 studies were identified. After reviewing the titles and abstracts, 102 studies were chosen for further review. Of these, 50 were excluded: 14 did not report the related data, 13 did not include the relevant target populations, 11 were not RCTs, and 12 did not investigate the target interventions. After qualitative synthesis, 8 studies were excluded. In total, 46 RCTs met the inclusion criteria and were included in this meta-analysis study (Huang et al., 1992, 2007, 2012; Liu et al., 1997, 1998, 2016; Lai et al., 1998; Li et al., 1999, 2014; Lun et al., 2003; Lai and Huang, 2005; Wu, 2006; Xu, 2006; Zhang et al., 2006, 2008; Ling et al., 2007; Chu et al., 2008; Han, 2009; Peng, 2009; Wang, 2009, 2014; Zhao et al., 2009; Teng, 2011; Yin et al., 2011; Teng and Lai, 2012; Zhou and Zhou, 2012; Dai et al., 2013a,b; Gao et al., 2013; Sheng et al., 2013; He and Guo, 2014; Shi et al., 2014; Jin, 2015; Li, 2015; Luo et al., 2015; Xie and Junming, 2016; Chen, 2017; Sheng and Cai, 2017; Wang and Wang, 2018; Wang et al., 2018; Feng, 2020; Guo, 2020; Ouyang, 2020; Yao, 2020; Zhu, 2020; Han et al., 2021). The detailed selection process is illustrated in Figure 1.
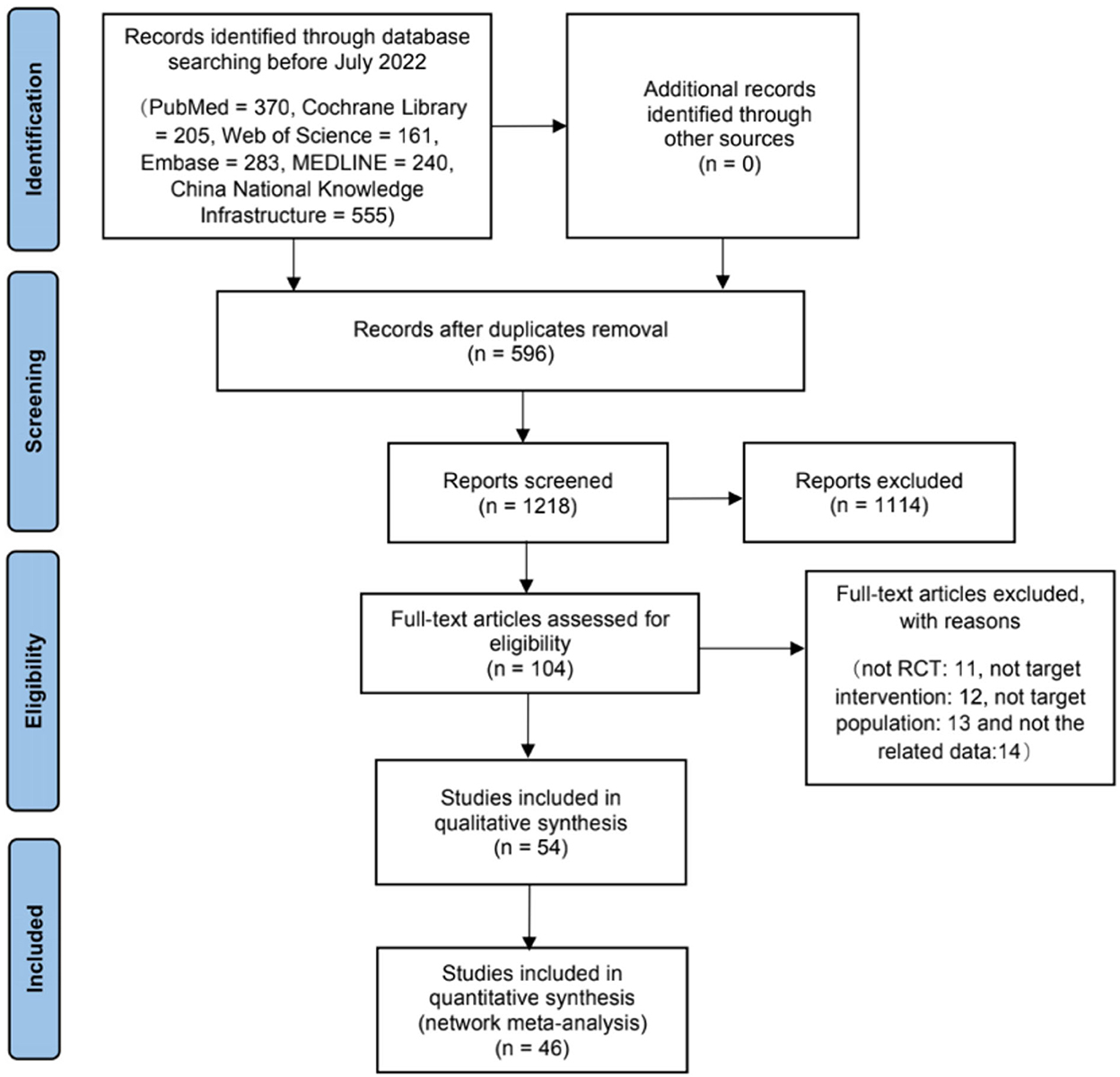
Figure 1. Flowchart of literature selection on systematic reviews on acupuncture for treating vascular dementia.
Characteristics of the included studies
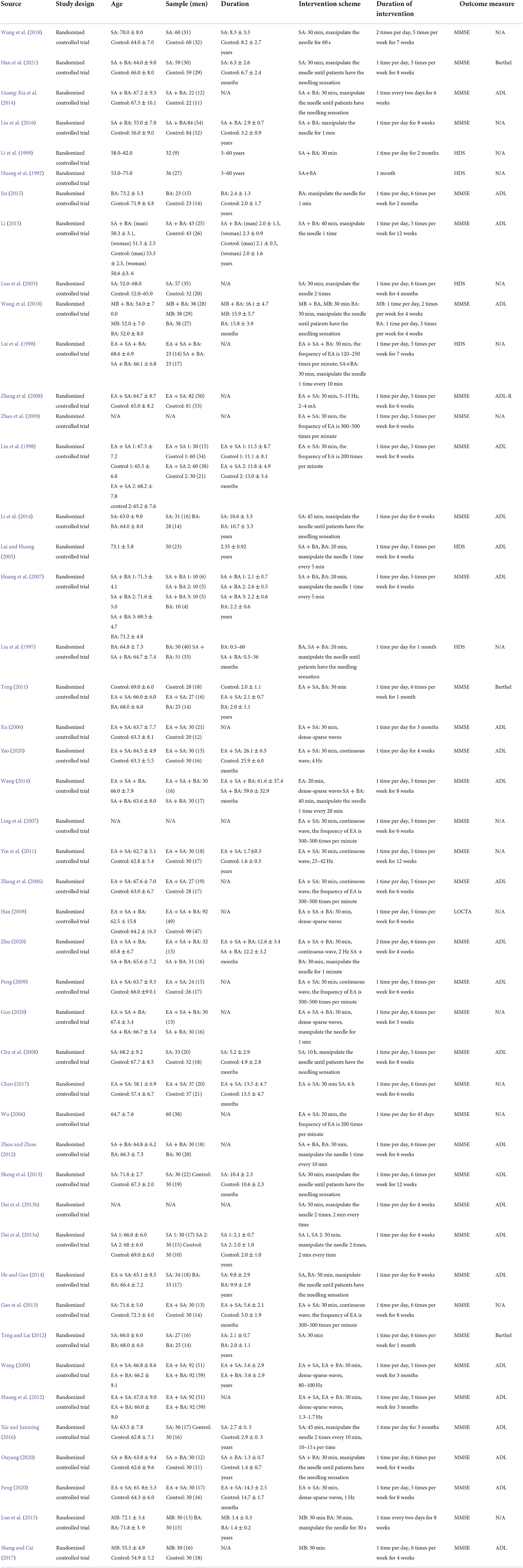
The aggregated characteristics of the included RCTs are shown in Table 1.
The included studies were released between 1992 and 2022. Forty-six of the RCTs originated in China. Thirty-seven studies were published in Chinese, whereas nine studies were published in English. Thirty RCTs were two-arm trials, 13 were three-arm trials, and three were multi-arm trials. Courses of acupuncture and other therapies ranged from 4 to 12 weeks in the included studies.
Quality of evidence
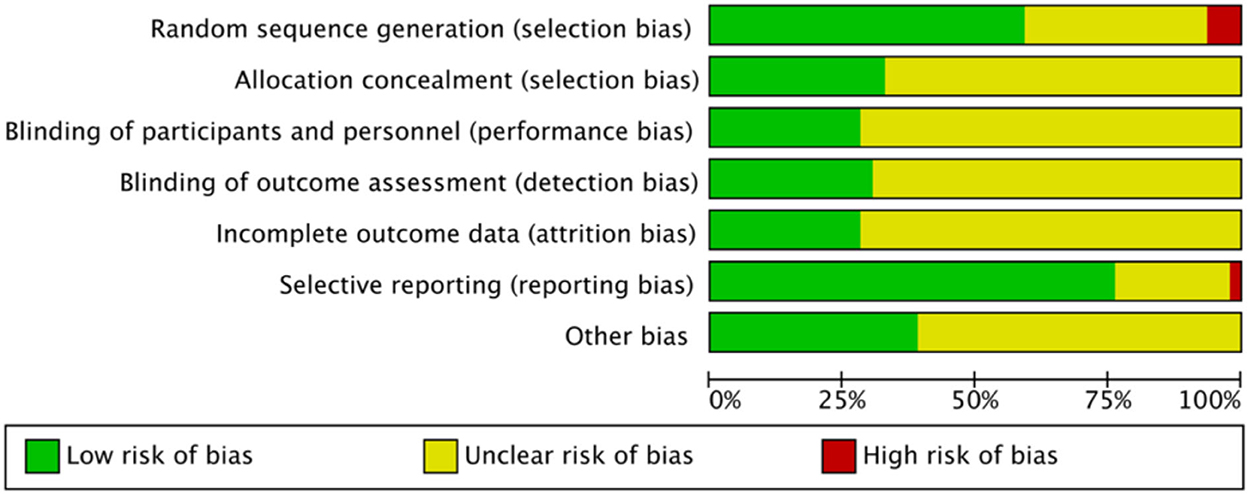
Figure 2 presents the evaluation results of the risk of bias (Supplementary Appendix 2). All 46 included studies were RCTs. Methods for generating random sequences were clearly stated in 30 studies, of which 3 studies (Liu et al., 1997; Sheng and Cai, 2017; Wang et al., 2018) were classified as high risk of bias due to the use of hospital or clinical record numbers as sequence numbers. The remaining 16 studies demonstrated an unclear risk of bias, as the random sequence generation method was not specified. Fifteen studies demonstrated a low risk of bias and the remaining 31 studies showed an unclear risk of bias in allocation concealment.
Due to the specificity of the interventions evaluated in this review, blinding between patients and clinicians was difficult to implement. Thirteen studies showed a low risk of bias and 33 studies showed an unclear risk of bias in the blinding of the participants and personnel. Fourteen studies showed a low risk of bias and 32 studies showed an unclear risk of bias in the blinding of outcome assessment.
Thirteen studies showed a low risk of bias in incomplete outcome data, whilst 33 studies showed an unclear risk of bias for incomplete outcome data. Regarding selective outcome reporting, one study (Guang-Xia et al., 2014) demonstrated a high risk of bias because it did not report pre-determined outcomes, 35 studies showed a low risk of bias, and the remaining 10 studies showed an unclear risk of bias. Twenty-eight studies showed an unclear risk of bias due to other bias.
Outcome analysis of cognitive function
Pairwise meta-analysis
We performed a pairwise meta-analysis of cognitive function and the results are shown in Supplementary Appendix 3. The results of the pairwise meta-analysis showed that although each acupuncture therapy had certain advantages compared with the control group (among which the advantages of MB + BA and EA + SA were larger), there was no significant difference in any of the comparisons.
Network meta-analysis
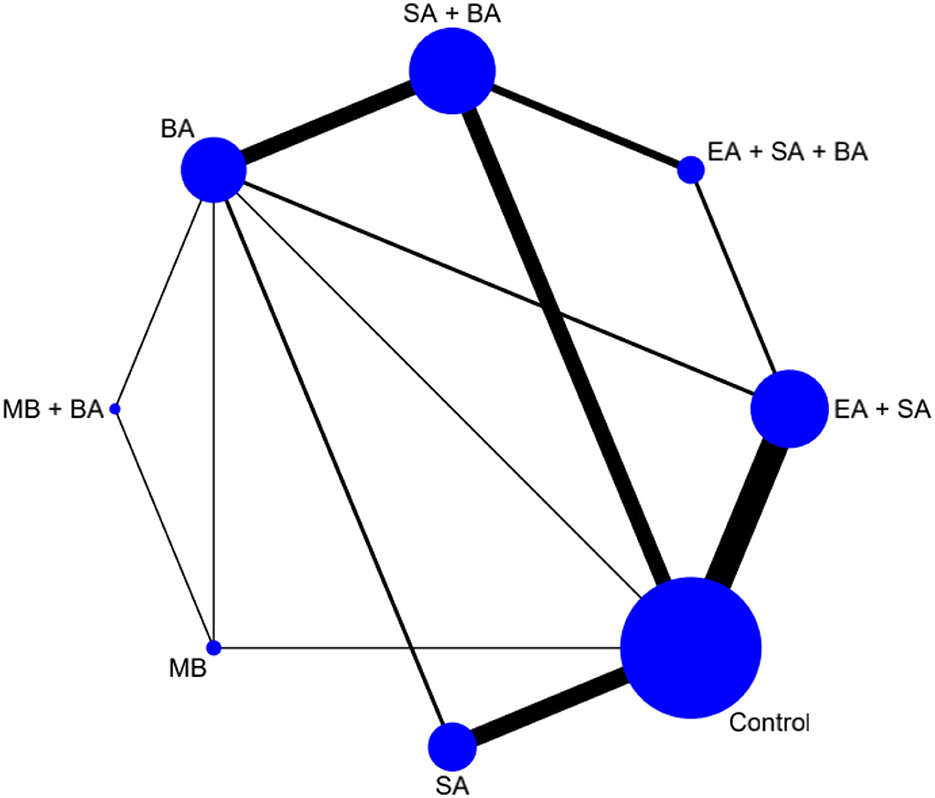
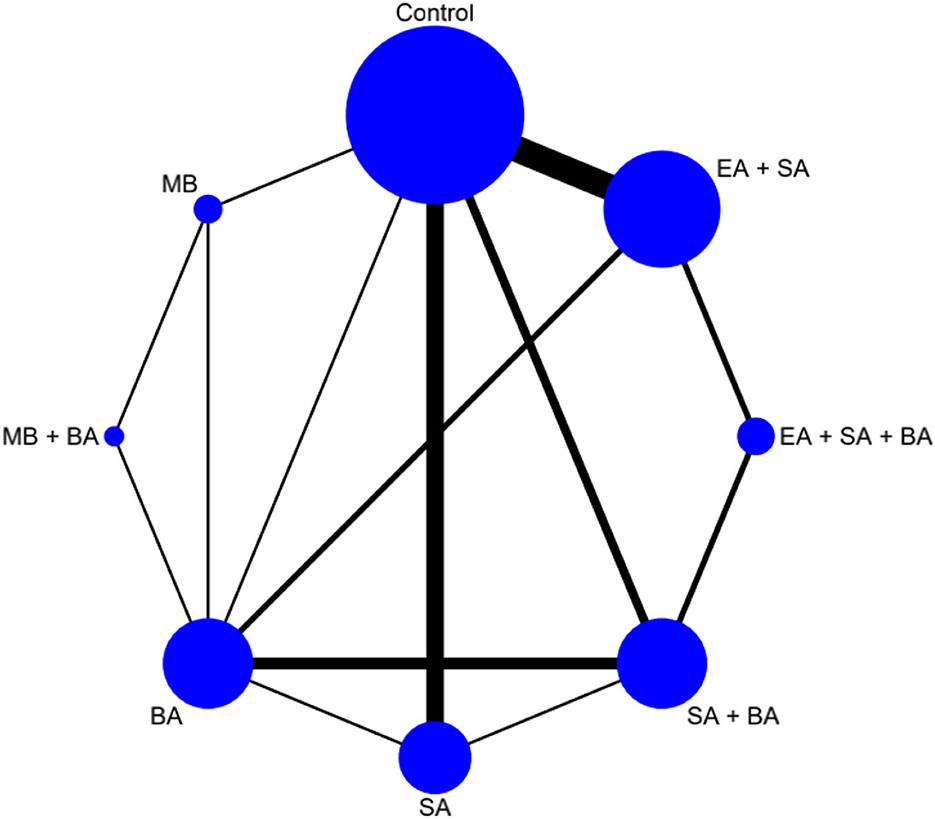
The network plot is shown in Figure 3. Eight interventions were involved i.e., EA + SA + BA, SA + BA, EA + SA, SA, BA, MB + BA, MB, and control.
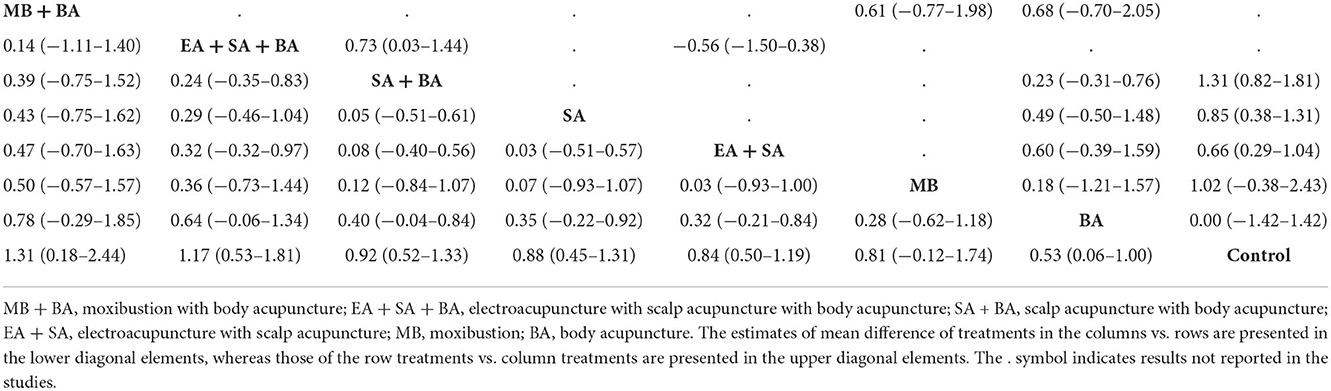
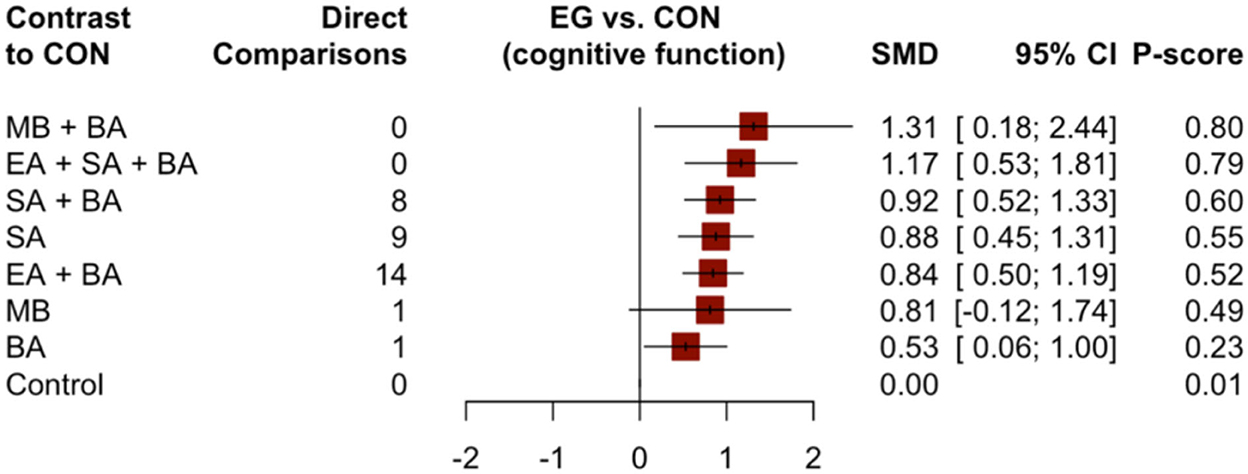
Forty-six studies, which contributed 3,731 patients in the main NMA, reported changes in cognitive function scores using the MMSE and HDS. The results of the NMA of different interventions are shown in Table 2. Compared to the control group, MB + BA (1.31, 95% CI: 0.18–2.44), EA + SA + BA (1.17, 95% CI: 0.53–1.81), SA + BA (0.92, 95% CI: 0.52–1.33), SA (0.88, 95% CI: 0.45–1.31), EA + SA (0.84, 95% CI: 0.50–1.19), and BA (0.53, 95% CI: 0.06–1.00) showed better improvement in cognitive function.
Compared to simple SA and BA, the combined interventions EA + SA + BA (0.29, 95% CI: −0.46–1.04 and 0.64, 95% CI: −0.06–1.34, respectively) and SA + BA (0.05, 95% CI: −0.51–0.61 and 0.40, 95% CI: −0.04–0.84, respectively) showed better improvement in cognitive function. Compared to simple MB, the combined intervention MB + BA (0.50, 95% CI: −0.57–1.57) showed better improvement in cognitive function. SA may be more effective in relieving dementia symptoms than BA (0.35, 95% CI: −0.22–0.92). However, there were no appreciable differences between these acupuncture therapies in terms of improving cognitive function. However, acupuncture combined with EA or MB was better than SA or BA alone. Moreover, MB + BA showed the greatest possibility of becoming the most effective intervention for improving cognitive function (P-score = 0.80, Figure 4).
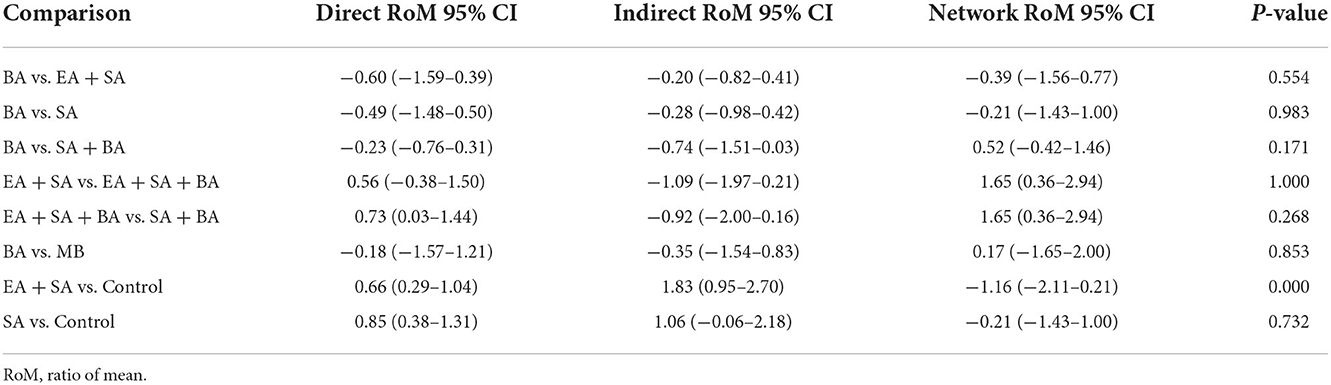
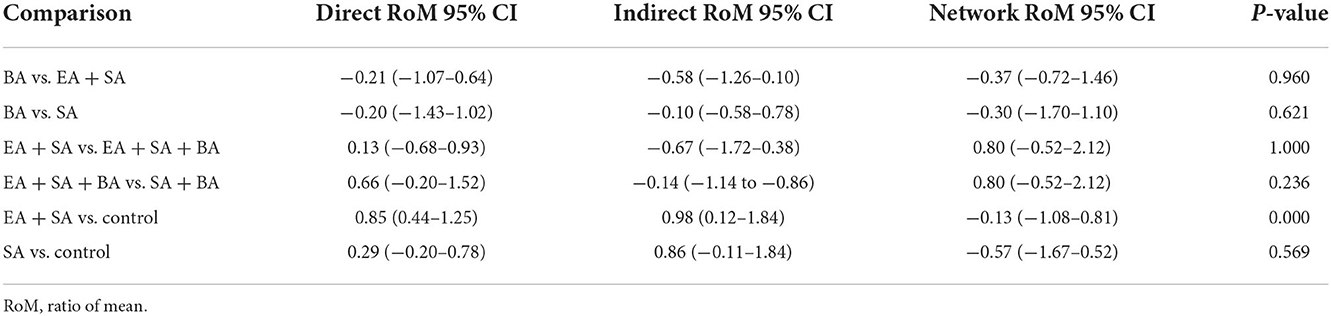
Inconsistency between direct and indirect comparisons of cognitive function scores
Inconsistency between direct and indirect comparisons was assessed using a node-splitting model, showing no inconsistencies among the studies (P > 0.05). Details of the results are presented in Table 3.
Subgroup analysis
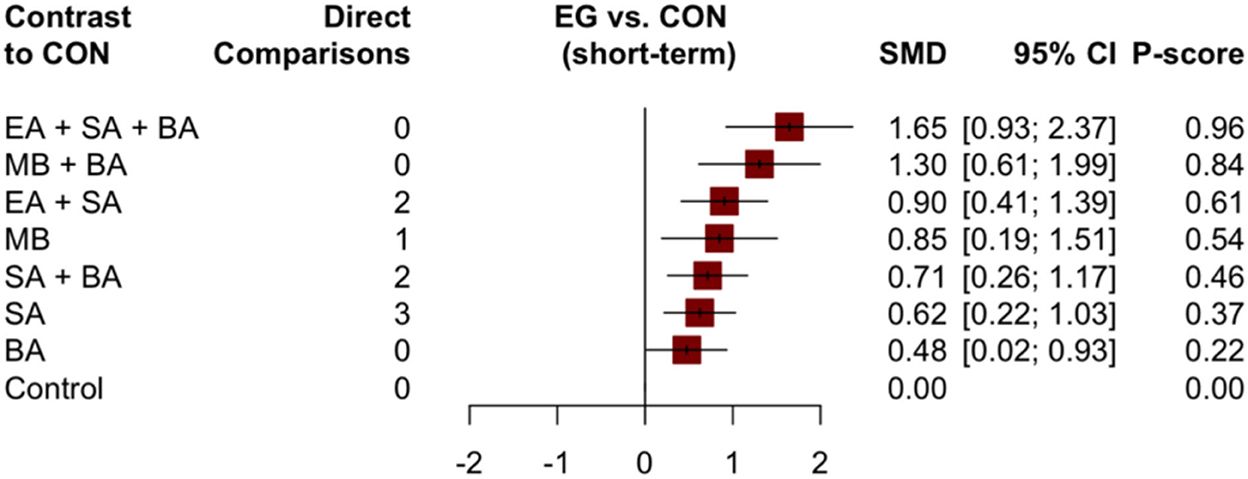
An improvement in cognition scores in the short-term (1 ≤ × ≤ 30 days) was reported in 16 trials; 22 trials reported an improvement in cognition scores in the mid-term (30 < × ≤ 60 days), and eight trials reported an improvement in cognition scores in the long-term (× > 60 days). Data from different treatments were evaluated separately in accordance with different treatment durations in each subgroup. There were eight different interventions in the short-term. Paired meta-analysis showed that EA + SA + BA vs. BA (1.13, 95% CI: 0.43–1.84), SA + BA vs. EA + SA + BA (−0.93, 95% CI: −1.52– −0.35), control vs. EA + SA + BA (−1.53, 95% CI: −2.78– −0.27), and control vs. EA + SA (−0.88, 95% CI: −1.48– −0.28) were all statistically significantly different (Supplementary Appendix 7). In the NMA, the EA + SA + BA treatment showed the best improvement in cognitive function (0.96), followed by MB + BA (0.84), EA + SA (0.61), MB (0.54), SA + BA (0.46), SA (0.37), and BA (0.22). The details are illustrated in Figure 5. There were significant differences in the curative effects between EA + SA + BA and SA + BA (0.93, 95% CI: 0.37–1.49), SA (1.02, 95% CI: 0.24–1.80), and BA (1.17, 95% CI: 0.52–1.82, Supplementary Appendix 7).
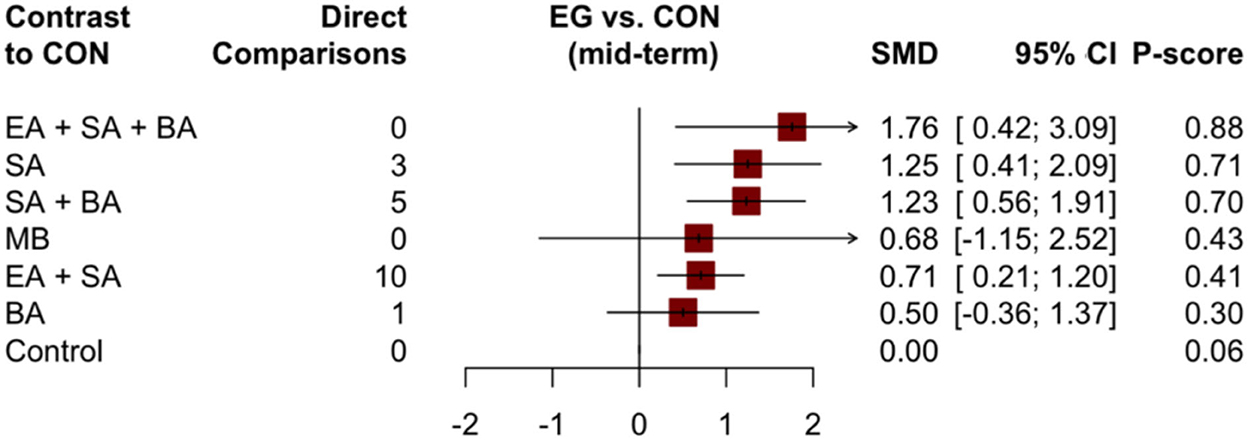
For the mid-term, there were no statistically significant differences between the groups in the paired meta-analysis (Supplementary Appendix 7). In the NMA, the highest probability of enhancing cognitive function was observed for EA + SA + BA, with a probability of 0.88, followed by SA and SA + BA with probabilities of 0.71 and 0.70, respectively (Figure 6, Supplementary Appendix 7). For the long-term, eight studies with five treatments (SA + BA, SA, EA + SA, control, and EA + SA + BA) were included. However, we failed to perform the corresponding network analysis because of the long-term network was disconnected.
Nine studies (Lai et al., 1998; Ling et al., 2007; Huang et al., 2012; Luo et al., 2015; Liu et al., 2016; Xie and Junming, 2016; Sheng and Cai, 2017; Feng, 2020; Ouyang, 2020) reported change scores using syndrome differentiation score of vascular dementia; however, failed to perform the corresponding network analysis due to the limited number of studies included.
Outcome analysis of living ability
Pairwise meta-analysis
We performed a pairwise meta-analysis of living ability and the results are shown in Supplementary Appendix 3. The results of the pairwise meta-analysis showed that although each acupuncture therapy had slight advantages compared with the control group, there was no significant difference in any of the comparisons.
Network meta-analysis
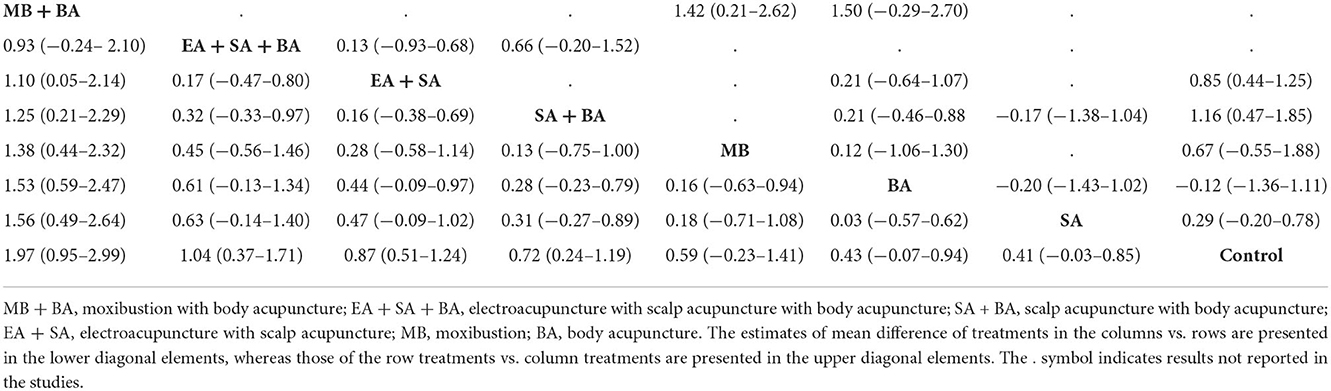
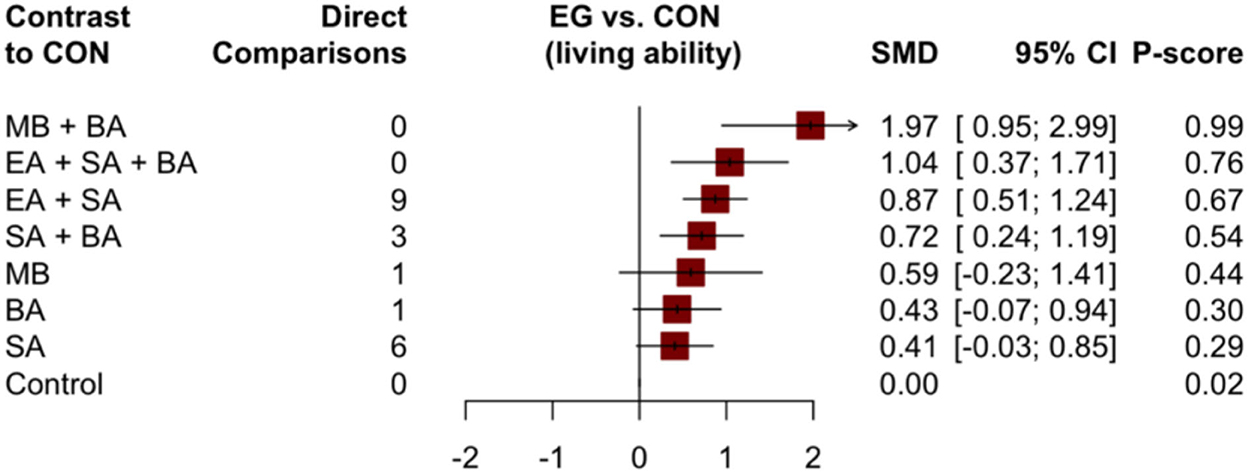
The network plot is shown in Figure 7. Eight interventions were involved: EA + SA + BA, SA + BA, EA + SA, SA, BA, MB + BA, MB, and control.
Thirty studies with 2,486 patients in the main NMA reported changes in ADL scores using the ADLs and Barthel index. The results of the NMA of different treatments are shown in Table 4. Compared to the control group, MB + BA (1.97, 95% CI: 0.95–2.99), EA + SA + BA (1.04, 95% CI: 0.37–1.71), EA + SA (0.87, 95% CI: 0.51–1.24), and SA + BA (0.72, 95% CI: 0.24–1.19) showed better improvement in ADLs. However, other acupuncture treatments showed no significant difference compared to the control group. MA + BA may be more suitable for improving the activity of daily living compared to MB (1.38, 95% CI: 0.44–2.32) and BA (1.53, 95% CI: 0.59–2.47). Furthermore, combined acupuncture MB + BA (P-score = 0.99) and EA + SA + BA (P-score = 0.76, Figure 8) are likely to be the best intervention to improve the ADLs of patients with VaD.
Inconsistency between direct and indirect comparisons of life function scores
Inconsistency between direct and indirect comparisons was assessed using a node-splitting model, showing no inconsistencies among the studies (P > 0.05). Details of the results are presented in Table 5.
Adverse events
Forty participants from eight studies (Zhang et al., 2008; Huang et al., 2012; Shi et al., 2014; Wang, 2014; Wang et al., 2018; Feng, 2020; Ouyang, 2020; Yao, 2020) reported the presence of adverse events. The main adverse effects reported in the acupuncture group were “discomfort at the acupuncture site” (16 patients), “skin bruising at acupoints” (15 patients), “fainting during acupuncture treatment” (seven patients), and “bleeding at acupuncture points” (two patients). These symptoms are mild and persist for a short period of time.
Confidence in evidence
The confidence ratings for these comparisons with CINeMA (Supplementary material) were mostly low to moderate confidence. This was mainly because of within-study bias, lack of precision, and/ or heterogeneity. Poor reporting of the randomization and blinding procedures explained the concerns of within-study bias. The relatively small number of studies with direct evidence included in all the comparisons explains the imprecision. The observed heterogeneity is likely because of the small number of trials in some comparisons, whereas some of the RCTs focused on different subgroups of VaD.
Discussion
To the best of our knowledge, this study is the first NMA to explore the efficacy of different acupuncture treatments for VaD. The MMSE scale (Cui et al., 2019) is currently the most widely used neuropsychological scale for clinical cognitive function screening, which can comprehensively reflect the cognitive state and cognitive characteristics of patients. Cognitive impairment is a core symptom of VaD; therefore, we chose to assess changes in cognitive impairment as the primary efficiency outcome of this review. In addition, the decline in the ability to perform ADLs is also one of the main symptoms of VaD; thus, we choose the ADLs as secondary efficacy outcome indicators. We used direct and indirect evidence to evaluate the relative effects of different acupuncture therapies on cognitive function and the ability to perform ADLs in patients with VaD. Based on the currently available data, our NMA suggests that combined acupuncture interventions (EA + SA + BA and MB + BA) show better efficacy in improving cognitive function and the ability to perform ADLs compared with MB, SA, and BA alone. SA was more effective than BA in improving cognitive function. Using a subgroup analysis of cognitive function, we found that EA + SA + BA achieved the best effect among the therapies analyzed for both the short- and mid-terms. However, for the short-term, EA + SA was more effective than SA + BA, whereas the opposite was true for the mid-term. This may be why there is a certain degree of heterogeneity in our review. Furthermore, the efficacy of EA in improving the ADLs was better than that of non-EA treatments.
Based on the analysis of adverse reactions from all included studies, all included acupuncture treatments were relatively safe for patients with VaD. Although some cases of adverse reactions have been reported, these adverse reactions are mild, and there is no direct association between adverse reactions and interventions. Therefore, these cases were justified.
Numerous studies have reported that VaD may be caused by hypoperfusion (Ruitenberg et al., 2005) and hypoxia (Fernando et al., 2006) after cerebral ischemia, resulting in alterations in blood–brain barrier permeability (Candelario-Jalil et al., 2011; Wardlaw et al., 2013), oxidative stress, and inflammation (Gallacher et al., 2010; Rouhl et al., 2012), which in turn can lead to white matter damage (Iadecola et al., 2019). The exact mechanism by which EA + SA + BA and MB + BA show better therapeutic efficiency in patients with VaD is still not fully understood. However, studies have shown that EA can enhance the secretion of brain-derived neurotrophic factors to exert neuroprotective effects after cerebral ischemia (Tao et al., 2016). EA can reduce oxidative stress and anti-apoptotic cell death by increasing superoxide dismutase activity in the brain (Wang et al., 2011). MB can inhibit apoptosis and oxidative stress and improve vascular endothelial growth factor inflammation (Lai et al., 2022). MB may improve cognitive function in VaD patients by inhibiting hippocampal neuronal apoptosis (Yang et al., 2021). SA can improve blood supply to the brain and enhance neuronal metabolism (Chen et al., 2020). EA + SA can improve the learning and memory ability of VaD rats by down-regulating inflammatory factors, reducing neuronal apoptosis, and improving synaptic plasticity (Ma et al., 2022). SA + BA can improve cognitive function by inhibiting brain oxidative stress and inflammation, alleviating neuronal death in VaD rats (Du et al., 2018). Therefore, we speculate that the reason why EA + SA + BA and MB + BA are superior to other acupuncture treatments may be that the combination therapy brings together the advantages of individual acupuncture treatments. However, to determine whether these findings are attributed to simple additive effects or due to the interaction of multiple signaling pathways in vivo requires further research.
Limitations
This study had the following limitations: (i) the included RCTs were mainly conducted in China, (ii) Reliability of results may be affected by incomplete reporting of test details, (iii) testing indexes other than the scale could not be included because of the limited number of studies, and (iv) due to the limited number of studies retrieved, we could not extend our review more beneficially, such as whether the analysis results varied by patient sex (male vs. female), or whether effect size corresponds to the atherosclerotic cardiovascular disease (ASCVD) burden.
The lack of long-term follow-up studies makes it hard to conclude substantial implications of the study. The disease cycle in patients with VaD usually has longer chronic progression. More evidence is required to confirm whether acupuncture has long-term efficacy in addition to short-term improvement in cognitive function.
Conclusion
Combined acupuncture therapy may be an effective and safe intervention for patients with VaD, and MB + BA and EA + SA + BA emerged as the most effective interventions in this study. EA + SA + BA shows the best efficacy when the course of acupuncture is short or moderate. However, because the analysis in this study was based on low-to-moderate evidence, there is no strong supporting evidence in this regard. High-quality, large-scale, long-term studies should be performed in the future to investigate the efficacy and safety of acupuncture in VaD.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary material.
Author contributions
JW: research design and writing. YC, HP, and HL: guidance of the relevant methodology. JW, SC, and ZZ: study selection. JW, QH, and JY: data abstraction. WW, SC, and QH: quality assessment. JW and SC: data statistics and analysis. All authors examined the results of this study and approved the final submission.
Funding
This study was supported by the Scientific and Technological Innovation Project of China Academy of Chinese Medical Sciences (CI2021A01401 and CI2021A01403).
Acknowledgments
The authors thank the Editage (http://www.editage.cn) for the English language editing of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The handling editor declared a shared affiliation with the authors JW, YC, QH, ZZ, and HP at the time of review.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnins.2022.1053283/full#supplementary-material
Abbreviations
RCTs, Randomized controlled trials; MB, moxibustion; BA, body acupuncture; EA, electroacupuncture; SA, scalp acupuncture; VaD, Vascular dementia; NMA, Network meta-analysis; MMSE, Mini-Mental State Examination; ADLs, Activities of daily living; CINeMA, Confidence In the results from Network Meta-Analysis; CI, Confidence interval.
References
Brehm, B. J., Lattin, B. L., Summer, S. S., Boback, J. A., Gilchrist, G. M., Jandacek, R. J., et al. (2009). One-year comparison of a high-monounsaturated fat diet with a high-carbohydrate diet in type 2 diabetes. Diabetes Care 32, 215–220. doi: 10.2337/dc08-0687
Candelario-Jalil, E., Thompson, J., Taheri, S., Grossetete, M., Adair, J. C., Edmonds, E., et al. (2011). Matrix metalloproteinases are associated with increased blood-brain barrier opening in vascular cognitive impairment. Stroke 42, 1345–1350. doi: 10.1161/STROKEAHA.110.600825
Chen, J. (2017). Effects of scalp acupuncture on cognitive function and limb motor function in patients with vascular dementia. J. Pract. Tradit. Chin. Med. 33, 711. doi: 10.3696/j.issn.1004-2814.2017.06.086
Chen, J., Li, H., Zeng, C., Li, J., and Zhao, B. (2020). Evaluation of the recovery outcome of poststroke cognitive impairment after cluster needling of scalp acupuncture therapy based on functional near-infrared spectroscopy. Brain Behav. 10, e01731. doi: 10.1002/brb3.1731
Chu, J.-M., Bao, Y.-H., and Zou, C. (2008). Effect of long-time retention of scalp needle on the abilities of cognition, daily living activity and P300 in vascular dementia patients. Acupunct. Res. 33, 334–338. doi: 10.3969/j.issn.1000-0607.2008.05.010
Cui, S., Chen, N., Yang, M., Guo, J., Zhou, M., Zhu, C., et al. (2019). Cerebrolysin for vascular dementia. Cochrane Database Syst. Rev. 2019, CD008900. doi: 10.1002/14651858.CD008900.pub3
Dai, X. H., Guo, Y., Zhang, H., and Zou, W. (2013a). Clinical observation of 35 cases of mild vascular dementia treated mainly by scalp acupuncture with rapid needling manipulations. J. Clin. Acupunct. Moxibustion 29, 10–11. doi: 10.3969/j.issn.1005-0779.2013.08.005
Dai, X. H., Guo, Y. H., Zhang, H. W., and Wei, Z. (2013b). Therapeutic observation on the treatment of vascular dementia majorly with scalp acupuncture with rapid needling manipulations. Shanghai J. Acupunct. Moxibustion 32, 709–710. doi: 10.3969/j.issn.1005-0957.2013.09.709
Du, S.-Q., Wang, X.-R., Zhu, W., Ye, Y., Yang, J.-W., Ma, S.-M., et al. (2018). Acupuncture inhibits TXNIP-associated oxidative stress and inflammation to attenuate cognitive impairment in vascular dementia rats. CNS Neurosci. Ther. 24, 39–46. doi: 10.1111/cns.12773
Feng, L. (2020). Clinical observation on the treatment of mild vascular dementia after stroke with zhiqi acupuncture (Master thesis). Guangzhou University of Chinese Medicine, Guangzhou, China. doi: 10.27465/d.cnki.gzzyc.2020.000004
Fernando, M. S., Simpson, J. E., Matthews, F., Brayne, C., Lewis, C. E., Barber, R., et al. (2006). White matter lesions in an unselected cohort of the elderly: molecular pathology suggests origin from chronic hypoperfusion injury. Stroke 37, 1391–1398. doi: 10.1161/01.STR.0000221308.94473.14
Gallacher, J., Bayer, A., Lowe, G., Fish, M., Pickering, J., Pedro, S., et al. (2010). Is sticky blood bad for the brain?: hemostatic and inflammatory systems and dementia in the caerphilly prospective study. Arterioscler. Thromb. Vasc. Biol. 30, 599–604. doi: 10.1161/ATVBAHA.109.197368
Gao, Q., Su, C., and Huang, Y. (2013). Effect of scalp acupuncture therapy on post-stroke mild vascular dementia. J. Pract. Trad. Chin. Med. 29, 891. doi: 10.3969/j.issn.1004-2814.2013.11.001
Guang-Xia, S., Cun-Zhi, L., Wei, G., Zhan-Kui, W., Lei, W., Chuan, X., et al. (2014). Effects of acupuncture on Chinese medicine syndromes of vascular dementia. Chin. J. Integr. Med. 20, 661–666. doi: 10.1007/s11655-013-1323-4
Guo, P. (2020). The clinical study on treatment of cognitive function of subcortical adterioscleroyic encephalopathy by scalp electroacupuncture (Master thesis). Heilongjiang University of Chinese Medicine, Harbin, China. doi: 10.27127/d.cnki.ghlzu.2020.000263
Han, B. (2009). Electric acupuncture treating 92 vascular dementia patients. Shanxi J. Trad. Chin. Med. 30, 1523–1524. doi: 10.3969/j.issn.1000-7369.2009.11.066
Han, H., Li, X., Jiang, H.-N., Xu, K., and Wang, Y. (2021). Effect of early acupuncture on cognitive function in patients with vascular dementia after cerebral infarction. Zhongguo Zhen Jiu 41, 979–983. doi: 10.13703/j.0255-2930.20210117-k0008
He, J., and Guo, S. (2014). Effects of scalp acupuncture combined with auricular point sticking on clinical symptoms and cognitive behavior ability in eldly patients with vascular dementia. Chin. J. Gerontol. 34, 5576–5577. doi: 10.3969/j.issn.1005-9202.2014.19.123
Huang, L. N., An, J. M., Su, T. S., Pu, W., Dong, L., Zhang, R. P., et al. (2012). Therapeutic efficacy observation on scalp acupuncture for vascular dementia. J. Acupunct. Tuina Sci. 10, 38–43. doi: 10.1007/s11726-012-0567-z
Huang, W. C., Xu, J., and Wang, X. (1992). Study on the acupuncture in treating multiple infarctional dementia. Zhongguo Zhen Jiu 12, 113–115.
Huang, Y., Lai, X., and Tang, A. (2007). Comparative study of the specificities of needling acupoints DU20, DU26 and HT7 in intervening vascular dementia in different areas in the brain on the basis of scale assessment and cerebral functional imaging. Chin. J. Integr. Med. 13, 103–108. doi: 10.1007/s11655-007-0103-z
Hurd, M. D., Martorell, P., Delavande, A., Mullen, K. J., and Langa, K. M. (2013). Monetary costs of dementia in the United States. N. Engl. J. Med. 368, 1326–1334. doi: 10.1056/NEJMsa1204629
Iadecola, C., Duering, M., Hachinski, V., Joutel, A., Pendlebury, S. T., Schneider, J. A., et al. (2019). Vascular cognitive impairment and dementia: JACC scientific expert panel. J. Am. Coll. Cardiol. 73, 3326–3344. doi: 10.1016/j.jacc.2019.04.034
Jian-Li, W. U., Xin, H. N., Wang, D. L., Zhu, Z. W., and Sun, Z. R. (2019). Origin and development situation of scalp acupuncture therapy. J. Guangzhou Univ. Trad. Chin. Med. 36, 1783–1787. doi: 10.13359/j.cnki.gzxbtcm.2019.11.022
Jin, Z. (2015). Efficacy of acupuncture combined with nimodipine in the treatment of vascular dementia. China Foreign Med. Treat. 35, 3–4. doi: 10.1662/j.cnki.1674-0742.2015.14.074
Joshua, P., John, O., Louise, R., and Damien, L. (2018). Dementia: assessment, management and support: summary of updated NICE guidance. BMJ Clin. Res. 361, k2438. doi: 10.1136/bmj.k2438
Kim, K. W., Lee, D. Y., Jhoo, J. H., Youn, J. C., Suh, Y. J., Jun, Y. H., et al. (2005). Diagnostic accuracy of mini-mental status examination and revised hasegawa dementia scale for Alzheimer's disease. Dement. Geriatr. Cogn. Disord. 19, 324–330. doi: 10.1159/000084558
Krahn, U., Binder, H., and König, J. (2013). A graphical tool for locating inconsistency in network meta-analyses. BMC Med. Res. Methodol. 13, 35. doi: 10.1186/1471-2288-13-35
Kua, E. H., Ho, E., Tan, H. H., Tsoi, C., Thng, C., and Mahendran, R. (2014). The natural history of dementia. Psychogeriatrics 14, 196–201. doi: 10.1111/psyg.12053
Lai, X., and Huang, Y. (2005). A comparative study on the acupoints of specialty of Baihui, Shuigou and Shenmen in treating vascular dementia. Chin. J. Integr. Med. 11, 161–166. doi: 10.1007/BF02836497
Lai, X., Mo, F., and Jiang, G. (1998). Observation of clinical effect of acupuncture on vascular dementia and its influence on superoxide dismutase, lipid peroxide and nitric oxide. Chin. J. Int. Trad. Western Med. 18, 648–651.
Lai, Z., Zhang, Q., Liang, L., Wei, Y., Duan, G., Mai, W., et al. (2022). Efficacy and mechanism of moxibustion treatment on mild cognitive impairment patients: an fMRI study using ALFF. Front. Mol. Neurosci. 15, 852882. doi: 10.3389/fnmol.2022.852882
Li, B. (2015). Governor vessel acupuncture method in the treatment of vascular dementia for 43 cases. Chin. Med. Mod. Dist. Educ. China 13, 70–72. doi: 10.3969./j.issn.1672-2779.2015.15.036
Li, S.-K., Ding, D.-M., Zhang, Z.-L., Ma, L., Huang, H.-Y., and Wu, X.-H. (2014). Effects of scalp acupuncture combined with auricular point sticking on cognitive behavior ability in patients with vascular dementia. Zhongguo Zhen Jiu 34, 417–420. doi: 10.13703/j.0255-2930.2014.05.012
Li, Y., Zhuang, L., Zheng, L., and Yang, W. (1999). Study on treatment of vascular dementia with acupuncture and moxibustion principally. World J. Acupunct. Moxibustion. 9, 6–11.
Ling, Z., Hong, Z., and Zhong, Z. (2007). The clinical research on scalp electric acupuncture improving the cognition function of 90 vascular dementia patients. J. Sichuan Trad. Chin. Med. 25, 105–108. doi: 10.3969/j.issn.1000-3649.2007.09.066
Liu, H., Hou, D., Diao, Z., and Yun, W. (1997). Observation on the clinical curative effects of turbit-clearing and intelligence-improving acupuncture therapy on vascular dementia and the study on its mechanisms. Chin. Acuponct. Moxibustion 9, 521–525.
Liu, J., Peng, X., and Lin, D. (1998). Clinical study on treatment of vascular dementia by electroacupuncture of scalp- acupoints. Chin. Acupunct. Moxibustion 4, 197–200.
Liu, Q., Wang, X.-J., Zhang, Z.-C., Xue, R., Li, P., and Li, B. (2016). Neuroprotection against vascular dementia after acupuncture combined with donepezil hydrochloride: P300 event related potential. Neural Rege. Res. 11, 460–464. doi: 10.4103/1673-5374.179059
Lun, X., Rong, L., and Yang, W. (2003). Observation on efficacy of CT positioning scalp circum-needling combined with Chinese herbal medicine in treating poly-infarctional vascular dementia. Chin. J. Int. Trad. Western Med. 23, 423–425. doi: 10.3221/j.issn:1003-5370.2003.06.008
Luo, B. H., Jian-Chun, Y. U., Yue-Qiang, H. U., Xue, L. F., Liang, Y. J., and Qin, B. N. (2015). Clinical observation about treatment of 30 cases of mild and moderate vascular dementia with “Yi Qi, Tiao Xue, Fu Ben, Pei Yuan” Moxibustion of Zhuang medicated thread. Lishizhen Med. Materia Medica Res. 26, 649–651. doi: 10.3969/j.issn.1008-0805.2015.03.053
Ma, C., Zhou, Y., Yi, W., Zhou, X., Guo, W., Xu, X., et al. (2022). Electroacupuncture of the Baihui and Shenting acupoints for vascular dementia in rats through the miR-81/IL-16/PSD-95 pathway. Ann. Transl. Med. 10, 540. doi: 10.21037/atm-22-2068
Moher, D., Liberati, A., Tetzlaff, J., and Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339, b2535. doi: 10.1136/bmj.b2535
Nikolakopoulou, A., Higgins, J. P. T., Papakonstantinou, T., Chaimani, A., Del Giovane, C., Egger, M., et al. (2020). CINeMA: an approach for assessing confidence in the results of a network meta-analysis. PLoS Med. 17, e1003082. doi: 10.1371/journal.pmed.1003082
O'Brien, J. T., and Thomas, A. (2015). Vascular dementia. Lancet 386, 1698–1706. doi: 10.1016/S0140-6736(15)00463-8
Orgogozo, J.-M., Rigaud, A.-S., Stöffler, A., Möbius, H.-J., and Forette, F. (2002). Efficacy and safety of memantine in patients with mild to moderate vascular dementia: a randomized, placebo-controlled trial (MMM 300). Stroke 33, 1834–1839. doi: 10.1161/01.STR.0000020094.08790.49
Ouyang, C. (2020). Clinical study on acupuncture treatment of mild to moderate vascular dementia (Master thesis). Guangzhou University of Chinese Medicine, Guangzhou, China. doi: 10.27044/d.cnki.ggzzu.2020.000791
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., et al. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372, n71. doi: 10.1136/bmj.n71
Papakonstantinou, T., Nikolakopoulou, A., Higgins, J. P. T., Egger, M., and Salanti, G. (2020). CINeMA: software for semiautomated assessment of the confidence in the results of network meta-analysis. Campbell Syst. Rev. doi: 10.1002/cl2.1080
Peng, X. (2009). Research on scalp electric acupuncture in improving the cognition function of vascular dementia patients. J. Sich. Trad. Chin. Med. 27, 113–115.
Rouhl, R., Damoiseaux, J., Lodder, J., Theunissen, R., Knottnerus, I., Staals, J., et al. (2012). Vascular inflammation in cerebral small vessel disease. Neurobiol. Aging 33, 1800–1806. doi: 10.1016/j.neurobiolaging.2011.04.008
Rücker, G. (2012). Network meta-analysis, electrical networks and graph theory. Res. Synth. Method. 3, 312–324. doi: 10.1002/jrsm.1058
Rücker, G., and Schwarzer, G. (2015). Ranking treatments in frequentist network meta-analysis works without resampling methods. BMC Med. Res. Methodol. 15, 58. doi: 10.1186/s12874-015-0060-8
Ruitenberg, A., den Heijer, T., Bakker, S. L. M., van Swieten, J. C., Koudstaal, P. J., Hofman, A., et al. (2005). Cerebral hypoperfusion and clinical onset of dementia: the rotterdam study. Ann. Neurol. 57, 789–794. doi: 10.1002/ana.20493
Senda, M., Terada, S., Takenoshita, S., Hayashi, S., Yabe, M., Imai, N., et al. (2020). Diagnostic utility of the addenbrooke's cognitive examination - III (ACE-III), mini-ACE, mini-mental state examination, montreal cognitive assessment, and hasegawa dementia scale-revised for detecting mild cognitive impairment and dementia. Psychogeriatrics 20, 156–162. doi: 10.1111/psyg.12480
Sheng, D., and Cai, S. (2017). Observation of the efficacy of wenyang bushen moxibustion treatment vascular dementia. J. Pract. Trad. Chin. Med. 33, 58–59. doi: 10.3969/j.issn.1004-2814.2017.01.049
Sheng, G., Zhao, Q., Guo, J., and Huang, L. (2013). Clinical observation on the treatment of post-stroke dementia with scalp acupuncture combined with Tianzhi gradules. Acta Chin. Med. Pharmacol. 41, 83–84. doi: 10.19664/j.cnki.1002-2392.2013.02.033
Shi, G., Liu, C., Guan, W., Wang, Z., Wang, L., Xiao, C., et al. (2014). Effects of acupuncture on Chinese medicine syndromes of vascular dementia. Chin. J. Integr. Med. 20, 661–666.
Tao, J., Zheng, Y., Liu, W., Yang, S., Huang, J., Xue, X., et al. (2016). Electro-acupuncture at LI11 and ST36 acupoints exerts neuroprotective effects via reactive astrocyte proliferation after ischemia and reperfusion injury in rats. Brain Res. Bull. 120, 14–24. doi: 10.1016/j.brainresbull.2015.10.011
Teng, X. (2011). Clinical study on vascular dementia treated by electroacupuncture at neck points plus scalp acupuncture. Shanghai J. Acupunct. Moxibustion 30, 84–86. doi: 10.3969/j/issn.1005-0957.2011.02.084
Teng, X. Y., and Lai, Z. J. (2012). Clinical efficacy observation of scalp-acupuncture-based therapy for vascular dementia. J. Acupunct. Tuina Sci. 10, 34–37. doi: 10.1007/s11726-012-0566-0
Wan, F., Niu, X., Song, Y.-L., and Si, Y.-C. (2016). The role of Chinese herbs and acupuncture on the inflammation reaction after cerebral ischemia. Curr. Pharm. Des. 22, 709–719. doi: 10.2174/1381612822666151204001348
Wang, F., and Wang, M. (2018). Acupuncture at five mind points combined with modified kidney decoction for vascular dementia of kidney essence deficiency. Zhongguo Zhen Jiu 38, 127–134. doi: 10.13703/j.0255-2930.2018.02.004
Wang, H., Pan, Y., Xue, B., Wang, X., Zhao, F., Jia, J., et al. (2011). The antioxidative effect of electro-acupuncture in a mouse model of Parkinson's disease. PLoS ONE 6, e19790. doi: 10.1371/journal.pone.0019790
Wang, J. (2014). The clinical study of electro-acupuncture cephalic and nuchal points of du meridian with acupuncture back shu points in treatment of vascular dementia (Master thesis). Heilongjiang University of Chinese Medicine, Harbin, China.
Wang, L., Yang, J.-W., Lin, L.-T., Huang, J., Wang, X.-R., Su, X.-T., et al. (2020). Acupuncture attenuates inflammation in microglia of vascular dementia rats by inhibiting miR-93-mediated TLR4/MyD88/NF-B signaling pathway. Oxid. Med. Cell. Longev. 2020, 8253904. doi: 10.1155/2020/8253904
Wang, P. (2009). Clinical Study on Vascular Dementia with Liver-Kidney Deficiency and Phlegm Stasis Syndromes Treated by Scalp Acupuncture. Master, Shaanxi University of Chinese Medicine.
Wang, S., Ye, G., Xu, C., Jia, A., Ru, Y., Guan, S., et al. (2018). Flipping moxibustion of medicine at acupoints in governor vessel combined with acupuncture for vascular dementia. Zhongguo Zhen Jiu 38, 919–924.
Wardlaw, J. M., Smith, C., and Dichgans, M. (2013). Mechanisms of sporadic cerebral small vessel disease: insights from neuroimaging. Lancet Neurol. 12, 483–497. doi: 10.1016/S1474-4422(13)70060-7
Wilcock, G., Möbius, H. J., and Stöffler, A. (2002). A double-blind, placebo-controlled multicentre study of memantine in mild to moderate vascular dementia (MMM500). Int. Clin. Psychopharmacol. 17, 297–305. doi: 10.1097/00004850-200211000-00005
Wolters, F. J., and Ikram, M. A. (2019). Epidemiology of vascular dementia. Arterioscler. Thromb. Vasc. Biol. 39, 1542–1549. doi: 10.1161/ATVBAHA.119.311908
Wu, H. (2006). Effects of scalp acupuncture plus electrical stimulation on cognitive and limb motor functions in patients with vascular dementia. J. Clin. Exp. Med. 5, 1160. doi: 10.3969/j.issn.1671-4695.2006.08.069
Wu, P., Mills, E., Moher, D., and Seely, D. (2010). Acupuncture in poststroke rehabilitation: a systematic review and meta-analysis of randomized trials. Stroke 41, e171–e179. doi: 10.1161/STROKEAHA.109.573576
Xie, X., and Junming, A. N. (2016). Clinical randomized controlled study of applying scalp acupuncture in treating vascular dementia. J. Sichuan Trad. Chin. Med. 34, 182.
Xu, L. (2006). Clinical study on the treatment of vascular dementia with EX-HN1 (Master thesis). Guangzhou University of Chinese Medicine, Guangzhou, China.
Yang, J.-W., Wang, X.-R., Zhang, M., Xiao, L.-Y., Zhu, W., Ji, C.-S., et al. (2018). Acupuncture as a multifunctional neuroprotective therapy ameliorates cognitive impairment in a rat model of vascular dementia: a quantitative iTRAQ proteomics study. CNS Neurosci. Ther. 24, 1264–1274. doi: 10.1111/cns.13063
Yang, K., Song, X.-G., Ruan, J.-R., Cai, S.-C., Zhu, C.-F., Qin, X.-F., et al. (2021). Effect of moxibustion on cognitive function and proteins related with apoptosis of hippocampal neurons in rats with vascular dementia. Zhongguo Zhen Jiu 41, 1371–1378. doi: 10.13703/j.0255-2930.20210124-k0006
Yang, Y., Zhao, X., Zhu, Z., and Zhang, L. (2022). Vascular dementia: a microglia's perspective. Ageing Res. Rev. 81, 101734. doi: 10.1016/j.arr.2022.101734
Yao, J. (2020). Clinical effect of electroacupuncture at sishencong point combined with donepezil on subcortical arteriosclerotic encephalopathy (Master thesis). Heilongjiang University of Chinese Medicine, Harbin, China. doi: 10.27127/d.cnki.ghlzu.2020.000201
Ye, Y., Li, H., Yang, J.-W., Wang, X.-R., Shi, G.-X., Yan, C.-Q., et al. (2017). Acupuncture attenuated vascular dementia-induced hippocampal long-term potentiation impairments via activation of D1/D5 receptors. Stroke 48, 1044–1051. doi: 10.1161/STROKEAHA.116.014696
Yin, J. Q., Li-Hong, L. I., and Feng, A. C. (2011). Clinical observation to improve symptoms in patients with vascular dementia treated with electric needle on scalp acupuncture. Chin. Arch. Tradit. Chin. Med. 29, 415–416. doi: 10.3109/9781841848433
Zhang, H., Zhao, L., He, C.-Q., Hu, K.-M., and Liu, J. (2008). Clinically multi-central randomized controlled study on scalp electroacupuncture for treatment of vascular dementia. Zhongguo Zhen Jiu 28, 783–787.
Zhang, H., Zhao, L., Zhu, M. J., and Fang, Y. J. (2006). Clinical research on cognition level and living quality of vascular dementia by scalp electric acupuncture. J. Chengdu Univ. Tradit. Chin. Med. 29, 6–15.
Zhao, L., Zhang, H., Zheng, Z., and Huang, J. (2009). Electroacupuncture on the head points for improving gnosia in patients with vascular dementia. J. Tradit. Chin. Med. 29, 29–34. doi: 10.1016/S0254-6272(09)60027-3
Zhou, W., and Zhou, Z. Y. (2012). Vascular dementia treated by scalp acupuncture plus body acupuncture therapy. J. Clin. Acupunct. Moxibustion 28, 11–14. doi: 10.3969/j.issn.1005-0779.2012.06.004
Zhu, H. (2020). Clinical observation of cross-electric acupuncture in the treatment of vascular dementia (Master thesis). Heilongjiang University of Chinese Medicine, Harbin, China. doi: 10.27127/d.cnki.ghlzu.2020.000252
Keywords: vascular dementia, electroacupuncture, scalp acupuncture, body acupuncture, moxibustion, cognitive function, ability of daily life, frequentist network meta-analysis
Citation: Wen J, Cao Y, Chang S, Huang Q, Zhang Z, Wei W, Yao J, Pei H and Li H (2022) A network meta-analysis on the improvement of cognition in patients with vascular dementia by different acupuncture therapies. Front. Neurosci. 16:1053283. doi: 10.3389/fnins.2022.1053283
Received: 25 September 2022; Accepted: 28 November 2022;
Published: 14 December 2022.
Edited by:
Jianxun Liu, Xiyuan Hospital, China Academy of Chinese Medical Sciences, ChinaReviewed by:
Mukaila Raji, University of Texas Medical Branch at Galveston, United StatesChao-Qun Yan, Dongzhimen Hospital, Beijing University of Chinese Medicine, China
Copyright © 2022 Wen, Cao, Chang, Huang, Zhang, Wei, Yao, Pei and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hui Pei, cGh4eWRvY3RvckAxMjYuY29t; Hao Li, eHlocGxpaGFvMTk2NUAxMjYuY29t
 Jiayu Wen
Jiayu Wen Yu Cao
Yu Cao Surui Chang
Surui Chang Qiaoyi Huang1,2
Qiaoyi Huang1,2 Zhen Zhang
Zhen Zhang Wei Wei
Wei Wei Jiuxiu Yao
Jiuxiu Yao Hui Pei
Hui Pei Hao Li
Hao Li