- 1Department of Clinical and Experimental Medicine, Psychiatry Unit, University of Catania, Catania, Italy
- 2Psychopharmacology, Drug Misuse and Novel Psychoactive Substances Research Unit, School of Life and Medical Sciences, University of Hertfordshire, Hatfield, United Kingdom
- 3East London Foundation Trust (ELFT), Homerton University Hospital, London, United Kingdom
- 4Department of Health Sciences, University of Milan, Milan, Italy
- 5Gabalfa Clinic, Cardiff and Vale NHS Health Board, Cardiff, United Kingdom
- 6Swansea University Medical School, Institute of Life Sciences, Swansea University, Singleton Park, Swansea, United Kingdom
- 7Addictions’ Observatory (ODDPSS), Rome, Italy
- 8School of Psychology, G. Marconi, Telematic University, Rome, Italy
- 9Department of Mental Health, Rome, Italy
Background: A wide range of novel psychoactive substances (NPSs) are regularly searched and discussed online by e-psychonauts. Among NPSs, the range of prescription/non-prescription opioids (fentanyl and non-fentanyl analogs) and herbal derivatives currently represents a challenge for governments and clinicians.
Methods: Using a web crawler (i.e., NPS.Finder®), the present study aimed at assessing psychonaut fora/platforms to better understand the online situation regarding opioids.
Results: The open-web crawling/navigating software identified some 426 opioids, including 234 fentanyl analogs. Of these, 176 substances (162 were very potent fentanyls, including two ohmefentanyl and seven carfentanyl analogs) were not listed in either international or European NPS databases.
Conclusion: A web crawling approach helped in identifying a large number, indeed higher than that listed by European/international agencies, of unknown opioids likely to possess a significant misuse potential. Most of these novel/emerging substances are still relatively unknown. This is a reason of concern; each of these analogs potentially presents with different toxicodynamic profiles, and there is a lack of docking, preclinical, and clinical observations. Strengthening multidisciplinary collaboration between clinicians and bioinformatics may prove useful in better assessing public health risks associated with opioids.
Introduction
Novel psychoactive substances (NPSs) are substances that are not controlled by the United Nations (UN) 1961 Single Convention on Narcotic Drugs or by Psychotropic Substances Conventions (United Nations Office on Drugs and Crime [UNODC], 2019a). By definition, “novel” does not necessarily imply that a drug has been recently developed (Hassan et al., 2017); it may also refer to substances that have lately become popular and/or more widely available, constituting a reason of current or potential public health concern (Schifano et al., 2015). NPSs are mainly of synthetic origin and comprise different drug classes (Schifano et al., 2019b). Among them, over the recent years, there has been an increase in the appearance of novel synthetic opioids (NSOs) on the recreational drug market (Zawilska, 2017). NSOs are frequently used with other illegal or prescribed drugs (Pichini et al., 2018; Pérez-Mañá et al., 2018). Owing to a range of reasons, the non-medical use of opioids such as fentanyl analogs and a range of remaining prescription/non-prescription substances is spreading worldwide (Prekupec et al., 2017; Lovrecic et al., 2019) and is affecting the entire life span, from youngsters to the elderly (Huhn et al., 2018; Kelley-Quon et al., 2019). Opioids are among the most powerful analgesic drugs, but they are burdened by unwanted adverse effects, in particular the abuse liability and the respiratory depression, with the last being the primary cause of death from overdose (Valentino and Volkow, 2018; Algera et al., 2019; Varga et al., 2020). Further, the evidence suggests that opioids’ consumption impacts the in utero neuronal development and induces in humans long-lasting transgenerational changes in subsequent generations owing to epigenetic alterations (Gilardi et al., 2018). For these reasons, worldwide intensive endeavors are directed from academics, clinicians, and industries toward expanding, intensifying, and coordinating fundamental, translational, and clinical research with respect to opioid abuse. To this respect, there is strong focus at present on the study and development of abuse-deterrent opioid formulations (Pergolizzi et al., 2018). Despite the efforts of law enforcement and other agencies (European Monitoring Centre for Drugs and Drug Addiction [EMCDDA], 2019; United Nations Office on Drugs and Crime [UNODC], 2019c), an unknown number of substances are continuously manufactured, (illicitly) offered for sale, and inappropriately consumed (Davey et al., 2012; Orsolini et al., 2017). Some concerns are related as well to the lack of regulation relating to so-called home-brew opiates (Galanie et al., 2015; Oye et al., 2015).
Number of Opioids Identified
By April 2019, the EMCDDA European Database on New Drugs (European Database on New Drugs [EDND], 2019) contained 751 entries, with 51 of them being classified as opioids. By February 2019, the UNODC listed a total of 892 substances in their NPS database (Unodc Early Warning Advisory on New Psychoactive Substances [UNODC EWA NPS], 2019), with 61 being NSOs. It could, however, be argued that the NPS scenario is much larger than that outlined by those substances that have been seized and formally identified by the European Union (EU) and the UN databases. Because the online NPS scenario typically predicts the real-life NPS market availability (Corazza et al., 2013; Schifano et al., 2015), identifying what is being discussed online by web-based NPS enthusiasts (e.g., the “e-psychonauts”) may well be of interest (Orsolini et al., 2015; Corkery et al., 2017).
Although data about the clinical, pharmacological, and toxicological characteristics of a number of opioid drugs have already been made available (Suzuki and El-Haddad, 2017; Armenian et al., 2018; Baumann et al., 2018; Beardsley and Zhang, 2018; Tabarra et al., 2019), there is a clear lack of knowledge relating to the number of novel substances offered to online/real-life customers (Kacinko and Papsun, 2019), also owing to the difficulties in detecting them in both interdiction and clinical settings (Abdulrahim and Bowden-Jones, 2018).
Aims
The aim of the current research was to (a) identify and categorize the number of opioids collected by the NPS.Finder® web crawler from a range of psychonaut, NPS-related, online sources; and (b) compare the NPS.Finder® opioid list with related findings from the UNODC and the EMCDDA.
Materials and Methods
Identification of Substances
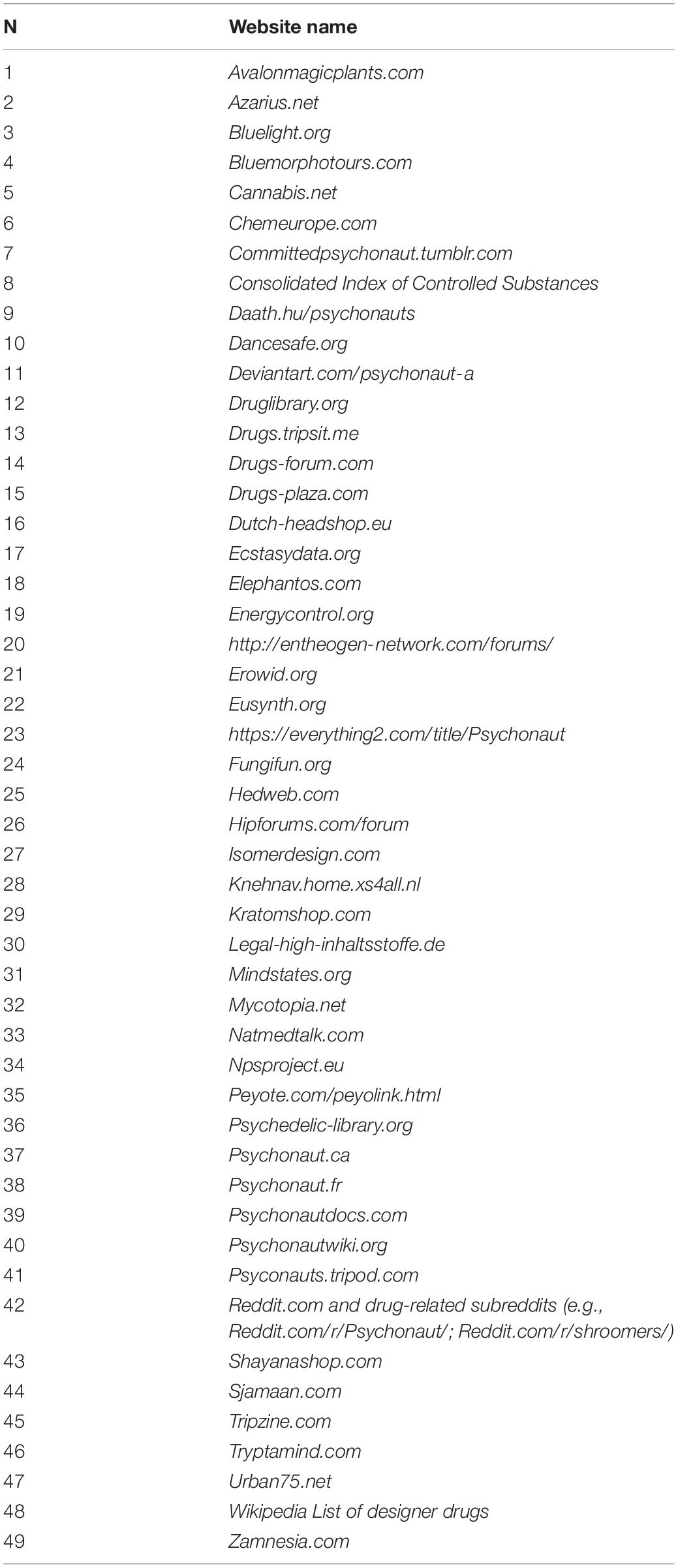
To facilitate the process of early recognition of the increasing dissemination of new substances online and the variability of information sources, a crawling/navigating software (i.e., “NPS.Finder®”) was designed to automatically scan the open/surface web for new/novel/emerging NPSs (for a thorough description of web crawling and data cleaning activities, see Schifano et al., 2019b). This software was designed to map on a 24/7 basis the large variety of psychoactive substances mentioned/discussed within a range of popular online psychonauts websites/fora. NPS.Finder® was designed de novo (e.g., it was not designed by the authors; neither was it adapted from another program) by Damicom, an IT enterprise based in Rome (Italy), to extract a range of information regarding NPSs, including chemical and street names; chemical formula; three-dimensional images; and anecdotally reported clinical/psychoactive effects. These data were then automatically stored in an online, restricted-access/password-controlled database located within firewall protected, highly secure, and consistently performing servers. First, a number of proper piloting searches were carried out (see also Schifano et al., 2019b), and any new website of interest was added to the list, whose final version is attached as Table 1. Although the language most typically used in these websites was English, further languages analyzed by NPS.Finder® included the following: Dutch, French, Turkish, Swedish, Spanish, German, Russian, and Italian. Afterward, a range of specific web scraper/crawler activities, to extract all accessible posts/entries from November 26, 2017 to May 31, 2019, were carried out. With the help an ad hoc check control panel, all data were manually and carefully analyzed by four medically/psychiatrically trained professionals (e.g., FN, DA, CZ, and LG). In this way, a full assessment and editing of each NPS.Finder® data entry were carried out, and the range of unique opioids here commented was identified. Finally, using chemical structure identification and published related data, researchers assigned each molecule to its NPS drug class (Schifano et al., 2019b).
Classification of Opioid Drugs
The web crawler-identified substances’ denominations were first searched in Medline/PubMed (PubMed, 2019) and in Google®/Google® Scholar (Google, 2019; Google Scholar, 2019). The used terms were “opiates/opioids,” “opioids,” “novel synthetic opioids,” “fentanyl analogs,” “opioid receptors,” “mu-opioid receptor,” “delta-opioid receptor,” “kappa-opioid receptor,” “receptor binding affinity,” and “herbal compounds.” An initial screening was performed to classify the substances according to their main description (e.g., fentanyl vs. non-fentanyl analogs). For this purpose, both the PuCchem (PubChem, 2019) and ChEMBL (Davies et al., 2015; Gaulton et al., 2017; EMBL-EBI, 2019) were searched; and whenever possible, the International Union of Pure and Applied Chemistry (IUPAC) name was also used. For fentanyl analogs, to make sure that the index molecule was indeed a fentanyl, the IUPAC name proposed by “isomer design” (PiHKAL, 2019) was here considered. For a handful of substances, when there were errors in published IUPAC names, the ChemDraw approach, able to generate chemical names from structures and/or vice versa, was used (ChemDraw, 2019).
A further screening was performed to compare the NPS.Finder® results with those reported by both the EMCDDA and the UNODC. More precisely, the search was performed on the following UN databases: International Narcotics Control Board (INCB) “Yellow List” (International Narcotics Control Board [INCB], 2019a); the Unodc Early Warning Advisory on New Psychoactive Substances [UNODC EWA NPS] (2019); and the fentanyl-related substances INCB report (International Narcotics Control Board [INCB], 2019a). For European data, the European Database on New Drugs [EDND] (2019) was accessed. To understand if an index opioid was currently being used as a prescribed medication, further screenings were carried out in the United Kingdom and United States lists of controlled substances (GOV.UK, 2017; DEA, 2019), and in the Anatomical Therapeutic Chemical/defined daily dose (ATC/DDD) list (Chen et al., 2012; WHO Collaborating Centre [WHOCC], 2016; WHO Collaborating Centre [WHOCC], 2019). The ATC substances were listed according to the ATC classification by WHO and manually searched in the ATC/DDD Index (WHO Collaborating Centre [WHOCC], 2019). In the ATC/DDD Index, most opioids are grouped with the code N02A (WHO Collaborating Centre [WHOCC], 2016).
Results
Identification and Classification of Opioid Drugs
After about 18 months of operation, the number of substances identified by the web crawler activities was 5,922. By the time of writing, some 4,204 unique NPSs were included in the database, and 1,718/5,922 (29.01%) remaining substances were found to be false positives or duplicates. The most common NPS mentioned in psychonaut fora included the following: psychedelic phenethylamines (30.1%; CI 95%: 28.7–31.5%); synthetic cannabimimetics (29.8%; CI 95%: 28.4–31.2%); and opioids (10.1%; CI 95%: 9.2–11.0%).
The opioids (n = 426) were then divided into two groups: fentanyl analogs (n = 234; 54.9%; CI 95%: 50.1–59.5%; Supplementary Table S1) and miscellaneous opioids (n = 192; 45.0%; CI 95%: 40.0–49.8%; Supplementary Tables S2A–C). The miscellaneous opioids group included the following: (a) all the prescribing opioids classified in the ATC/DDD Index (n = 48; 11.2% of 426; CI 95%: 8.6–14.6%); (b) the non-fentanyl analog opioids (n = 136; 31.9%; CI 95%: 27.6–36.5%); and (c) the herbal derivatives (n = 8; 1.8%; CI 95%: 0.9–3.6%) (Supplementary Tables S2A–C).
Comparison With Novel Psychoactive Substance-/Opioid-Focused European and United Nations Databases
Current NPS.Finder® results were compared with those pertaining to opioids listed in the EMCDDA and UN databases (Supplementary Tables 1, 2A–C). Overall, the NPS.Finder® detected a larger number of opioids than was in the remaining databases. The opioids identified by NPS.Finder® only were 176 chemically different substances. In particular, out of the 234 fentanyl analogs, 162 (69.2% of 234) were listed only in the NPS.Finder®; 7 (2.99%; e.g., 4-fluoroisobutyrfentanyl, acetylfentanyl, acrylfentanyl, butyrylfentanyl, furanylfentanyl, ocfentanil, and tetrahydrofuranylfentanyl) were listed in all databases, and the remaining 65 (27.78%) substances were reported in one or more of the EU or UN databases (i.e., INCB Yellow List; INCB “Fentanyl-related substances with no known legitimate use list”; UNODC EWA NPS; and EDND). Out of the 136 substances in the non-fentanyl analog opioid list, 14 (10.29%) were listed only in NPS.Finder®, and not in any of the following: INCB Yellow list (updated March 2019), EDND (April 2019), and UNODC EWA NPS (July 2019). The remaining 122 substances were reported both in the NPS.Finder® and in at least one of the following: INCB Yellow list (updated March 2019), EDND (April 2019), or UNODC EWA NPS (July 2019).
Discussion
To the best of our knowledge, an unprecedented list of opioid drugs with a possible recreational/misuse potential was generated by these open web-only crawling software activities, which were focusing on a range of psychonaut forum entries. For all these fentanyl/non-fentanyl/miscellaneous drugs, only limited levels of preclinical/clinical data are typically available (Deluca et al., 2012; Armenian et al., 2018; Frisoni et al., 2018; Gerace et al., 2018a; Ventura et al., 2018; European Database on New Drugs [EDND], 2019; Tabarra et al., 2019; United Nations Office on Drugs and Crime [UNODC], 2019b). Apart from the vast range of previously undescribed fentanyl analogs, NPS.Finder® identified a further number of “novel” and potent/very potent, chemically diverse miscellaneous substances. This may suggest that psychonauts are attracted to a variety of drugs, which range from research chemicals and their derivatives to more “traditional” substances, including failed pharmaceuticals or old patents that have been “rediscovered” and marketed for their potential use as “recreational” substances (Corkery et al., 2018). At present, we cannot establish with certainty whether the opioids here identified are all, or in part, currently circulating in the community and are available for consumption. Indeed, the current paper focused on the e-psychonauts’ discussions only; these web-based drug enthusiasts, however, have been suggested to somehow represent the drug scenarios’ “trend setters” (Schifano et al., 2015, 2019b). Hence, a focus on web-based drug discussion may well be of interest to better assess, and possibly predict (Corazza et al., 2013), the international drug misuse concerns. Ongoing studies from our group will hopefully better identify the following: a) which of the e-psychonauts’ substances, including opioids, will make an entry into the future markets; and b) which is the time gap, for an index drug, between the start of the e-psychonauts’ interest and their actual identification on the international drug scenarios.
Different from both the UNODC and the EMCDDA, which report in their NPS databases only those substances that have been both seized from the community and chemically analyzed, it was unclear from here if the mentioned opioids have already been synthesized or not. For each mentioned opioid, however, the unique IUPAC name was here identified and reported, and those further sources here are considered (e.g., PubChem, ChEMBL, ChemDraw, and Isomer Design) confirmed that the substance was properly chemically characterized. Hence, one could argue that the rogue producers’ synthesis of any of the opioids here commented is indeed a real and distinct possibility (Kata et al., 2018; Financial Crimes Enforcement Network [FinCHEN], 2019; Pardo et al., 2019; Whitehouse, 2019).
Present results, highlighting a strong interest by psychonauts toward opioid drugs, are consistent with previous studies, which have analyzed the opioids’ debate both in social media settings (Kalyanam et al., 2017; Kim et al., 2017; Pandrekar et al., 2018; Li et al., 2019) and on the darknet (Mackey et al., 2018; Tzanetakis, 2018; Cunliffe et al., 2019).
Fentanyl Analogs
Most (e.g., 55%) opioids identified here were fentanyl analogs. Although present findings do not necessarily confirm in any possible way these substances’ levels of use, they can still reflect the attention given by psychonauts to these drugs and help in explaining aspects of the current “opioid epidemic” (Kakko et al., 2019; Zhao, 2019). A few fentanyl analogs have been mentioned in the literature (Suzuki and El-Haddad, 2017; Zawilska, 2017; Misailidi et al., 2018; Lipiński et al., 2019), especially in terms of the acute clinical toxicity issues relating to their intake (Abdulrahim and Bowden-Jones, 2018). Vulnerable subjects can access online a large number of these substances (Suzuki and El-Haddad, 2017), without even being aware of what they are taking exactly (Ciccarone et al., 2017; Bardwell et al., 2019; McLean et al., 2019; Stein et al., 2019). Indeed, levels of related clinical toxicological information are sometimes available only postmortem (Giorgetti et al., 2017; Concheiro et al., 2018; D’Errico, 2018; Kraemer et al., 2019).
Apart from a range of some well-known fentanyl-related substances, two ohmefentanyl and seven carfentanyl analogs were here identified. It is of interest that the analgesic activity of ohmefentanyl in mice is 6,300 times more potent than that of morphine (Xu et al., 1985) and that carfentanyl has been reported in association with a number of fatalities (Wilcoxon et al., 2018). Given the wide range of common and street names available for each molecule, even small modifications occurring in the fentanyl family structure can lead to misidentification of the index drug (Akhondi et al., 2015) and potentially provoke clinically unexpected effects. It is also possible that some substances here commented by psychonauts included fentanyl precursors or metabolites (Wilde et al., 2019). Hence, it is particularly relevant, for the vast range of fentanyl analogs, to use unique codes such as those of IUPAC (Gaulton et al., 2017; Hähnke et al., 2018; PiHKAL, 2019).
Miscellaneous: Non-fentanyl Compounds, Prescribing Opioids, Herbals, and Derivatives
The 136 non-fentanyl analog opioids identified in the NPS.Finder® database belong to a range of pharmacological classes, and some 10.2% were not reported by the EU and UN databases. Several of these substances have been used in the past for research purposes and/or were never marketed. The present findings are consistent with the current “top” and “rising” posts on social networks like Reddit (Reddit, 2019d). Some of these substances, for example, BDPC/bromadol have already been described as being some 500 times more potent than morphine (Reddit, 2019a; Sharma et al., 2019; TripSit Factsheets, 2019a), whereas others, for example, embutramide, have been associated with suicidal intent (Lajtai et al., 2016). A range of remaining substances identified here have received little/no attention in the literature and include acetoxyketobemidone (e.g., an alternative to ketobemidone, a prescription analgesic that is scheduled in different countries; United Nations Office on Drugs and Crime [UNODC], 1954; Drugs-forum, 2007; Bluelight, 2019a; Reddit, 2019c); 6-methylenedihydrodesoxymorphine/6-MDDM (e.g., a semi-synthetic derivative of hydromorphone about 80 times more potent than morphine and associated with euphoriant effects; Bluelight, 2019b; TripSit Factsheets, 2019b; Reddit, 2019e); isopropyl-U-47700 (identified for the first time in 2018 and belonging to N-substituted benzamides and acetamide opioid analgesics, colloquially known as “U-compounds” or “U-drugs;” Krotulski and Logan, 2018; Sharma et al., 2019; Yin, 2019); and piperidylthiambutene (developed in the 1950s and equipotent to morphine; Adamson and Green, 1950).
NPS.Finder® identified here virtually all the prescription opioids listed in the ATC/DDD Index. The psychonauts’ interest in commenting about these substances may be a reason of concern, because prescription opioid misuse is a challenging issue worldwide, especially so in both North America and Europe (van Amsterdam and van den Brink, 2015; Helmerhorst et al., 2017).
NPS.Finder® identified as well a range of well-known opioid herbal compounds, including Papaver somniferum and some crude opiate extracts (e.g., granulate, tincture, and poppy seed tea); Mitragyna speciosa/kratom (but not mitragynine and 7-hydroxymitragynine; Fluyau and Revadigar, 2017; Graziano et al., 2017; Coe et al., 2019; Corkery et al., 2019); and Salvia divinorum. Although herkinorin (Ventura et al., 2018) was not identified in the current database, salvinorin B ethoxymethyl ether/“Symmetry” (e.g., an unusually potent synthetic salvinorin compound, potently binding to kappa opioid receptors; Peet and Baker, 2011; Erowid, 2015; Reddit, 2019b), salvinorin B methoxymethyl (a potent semi-synthetic derivative of salvinorin A; Baker et al., 2009; Peet and Baker, 2011; Reddit, 2019f; Zjawiony et al., 2019), and salvinorin A received here the attention of psychonauts. This may be a cause for concern, because salvinorin products’ psychoactive effects include perceptual disturbances, psychosis, irritability, and anxiety (Ventura et al., 2018).
Finally, it is interesting to note that a range of both endogenous (e.g., amphibian opioid peptides such as dermorphins and deltorphins) and food-derived (e.g., derivatives from milk and soya such as soymorphines and β-casomorphins) opioid peptides, possessing low levels of potency (Teschemacher et al., 1997; Negri et al., 2000; Ohinata et al., 2007; Liu and Udenigwe, 2018), were not mentioned in psychonaut fora.
Comparison With European Union and United Nations Novel Psychoactive Substance-Related Databases
A total of 426 opioids (e.g., 234 fentanyl analogs and 192 non-fentanyl analogs) were identified. The number of NPS.Finder® opioids is indeed higher than that listed by international agencies like the UNODC and the EMCDDA. By May 2019, the INCB identified 115 opioids (International Narcotics Control Board [INCB], 2019a); up to 2019, the UNODC EWA NPS listed 61 different opioids; by June 2018, the INCB listed 93 fentanyl-related substances with no known legitimate use (International Narcotics Control Board [INCB], 2019b); and by April 2019, the EMCDDA reported 51 opioids out a total of 749 EDND substances (European Database on New Drugs [EDND], 2019). There might be different reasons behind these inconsistencies. First, both the UN and EU agencies collect in their databases only those substances that are detected/seized and properly analyzed and most importantly reported, respectively, worldwide or in the European region. Furthermore, the NPS.Finder® carried out a range of open web crawling identification activities focusing on a large range of psychonaut-based, specialized, multilingual, sources with a specific focus on new/old psychoactive substances of likely recreational interest. From this point of view, one could also argue that discussing a molecule on the web is not, per se, an indication that the index molecule is being/will be ingested by interested individuals. This can explain why the opioids common to all lists (e.g., the fentanyl analogs 4-fluoroisobutyrfentanyl, acetylfentanyl, acrylfentanyl, butyrylfentanyl, furanylfentanyl, ocfentanil, tetrahydrofuranylfentanyl, and the non-fentanyl analogs AH-7921 and U-47700) are only a small proportion of the total.
Pharmacological and Clinical Considerations
Fentanyl, fentanyl analogs, and the remaining opioids here commented present as partial/full agonists, and with different affinity levels, at the mu, delta, and kappa opioid receptors. This may well suggest the existence of a possible vast range of ill-health consequences associated with these substances (Stein, 2016). However, a clear understanding of the clinical toxicity of each compound is at present problematic. In fact, although the in vitro pKi values/binding affinities, potency, and efficacy levels for a number of opioids are already available (World Health Organization [WHO], 2016; Baumann et al., 2018; World Health Organization [WHO], 2018), these may not provide enough information about the relative in vivo potency (Baumann et al., 2018). In fact, there might be variable effects on G-protein-coupled receptors, which could potentially give rise to a great diversity of intracellular consequences following the administration of different analogs with apparently similar pharmacodynamics (Smith et al., 2018). Furthermore, as highlighted using a molecular docking model, some substances are too structurally similar for the scoring function to distinguish between different analogs (Ellis et al., 2018, 2019). For some opioids, larger dosages of naloxone may be required to reverse the opioid toxidrome than needed in case of a typical heroin overdose (Armenian et al., 2018; Lovrecic et al., 2019). The greatest levels of concerns remain related to fentanyl analogs, because of their harmful potential (Schifano et al., 2019a), the continuous high incidence of emerging analogs on the markets over the last years (Schueler, 2017), and the difficulties in identifying them with analytical chemistry techniques (Gerace et al., 2018b; Morrow et al., 2019). Conversely, those substances here identified possessing a full/partial kappa opioid receptor agonist activities (including salvinorin A and its derivatives; tifluadom; and pethidine) are likely to be particularly attractive for opioid and other research chemical consumers prone to a recreational experimentation associated with complex psychoactive effects (Coffeen and Pellicer, 2019).
Limitations
NPS.Finder® crawled only on the open web during the present phase of its development. Future studies by our group will be focused on expanding drug searches on less accessible areas of the web such as the deep web and the darknet (Orsolini et al., 2017). A qualitative/netnographic approach (Loi et al., 2017; Wang, 2019) will be needed as well to better assess the levels of online information relating to the possible psychonauts’ preference between analogs and their motivation for use, that is, recreational or self-medication purposes. As previous studies have highlighted their importance in NPS-based studies (Deluca et al., 2012), next NPS.Finder®-based projects will need to focus as well on further languages, for example, Chinese, Japanese, and Arabic. Some consideration needs to be given as well to some opioids not having been reported by NPS.Finder®. The present findings, however, relate only to the psychonauts’ interest, who are typically debating/discussing/mentioning only those substances that are considered as “trendy.” Furthermore, it is possible that owing to fentanyl/non-fentanyl nomenclature issues, there may be discrepancies between the denomination of substances resulting from international/EU interdiction data and those mentioned by psychonauts.
Conclusion
The web crawler activities may well possess the potential to identify a wide range of novel/previously undescribed NPSs, including opioids. The literature base regarding these substances is limited in terms of acute and long-term effects, adverse effects, abuse potential, and manufacturing/distribution in both the virtual and real markets. It is difficult for health professionals to keep up to date with the growing number of opioids being made available. Clinicians are not always aware of the risks relating to novel psychoactives’ intake, and, at the same time, they are not typically able to identify a potential NPS user (Simonato et al., 2013). This may be a reason for concern, especially for emergency professionals confronting acute, and at times dramatic, clinical situations that are suspected of being drug related but in which the standard urine specimen turns out to be negative (Guirguis et al., 2017). Hence, clinicians should be informed about the range of opioids, their idiosyncratic drug–drug combinations, and their medical risks (Orsolini et al., 2015). The availability of new digital technologies, and the current systematic web crawling activities, provided here better levels of knowledge about the emerging number of opioid derivatives. This may help in designing and developing a range of efficient opioid on−site screening and detection techniques (Guirguis et al., 2017) and in drafting potent opioids’ specific treatment and management guidelines.
Raising awareness and education among users, the general public, and frontline staff and the development of harm reduction techniques are of paramount importance to tackle the flood of opioids. The epidemic of opioid overdose is a complex problem that can only be addressed by concerted and multidisciplinary efforts. Indeed, in silico, in vitro, and in vivo studies could provide important findings; furthermore, it is deemed here essential to monitor the real-life scenarios through drug checking in interdiction, drug outpatient clinics, and critical care settings. The provided lists can be useful in prospective and forward-looking terms. More studies should aim at providing better levels of misusing drugs’ clinical pharmacological-related knowledge, so that properly tailored prevention strategies can be drawn up and made available.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.
Author Contributions
FS and AV have conceived the idea of the manuscript and have coordinated the whole project. FN, CZ, DA, and LG have actually carried out the process of both data collection and systematization. DA performed the literature searches and the analysis of data and drafted the manuscript. FS and JC supervised the writing of the manuscript and contributed to the final version of the manuscript. FS and EA approved the final content of the manuscript. JC provided data from the EMCDDA and UNODC databases for the purposes of this research. FS, JC, and AG have provided relevant epidemiological data and have contributed as well to the drafting of the manuscript itself.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors are grateful to Damicom srl, a small enterprise from Rome (Italy), whose professionals have developed the NPS.Finder® web crawler and so generously have allowed here the testing of its potential.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnins.2020.00149/full#supplementary-material
References
Abdulrahim, D., and Bowden-Jones, O. (2018). The Misuse of Synthetic Opioids: Harms and Clinical Management of Fentanyl, Fentanyl Analogues and Other Novel Synthetic Opioids Information for Clinicians. Available online at: http://www.neptune-clinical-guidance.co.uk (accessed August 8, 2019).
Adamson, D. W., and Green, A. F. (1950). A new series of analgesics. Nature 165:122. doi: 10.1038/165122a0
Akhondi, S. A., Muresan, S., Williams, A. J., and Kors, J. A. (2015). Ambiguity of non-systematic chemical identifiers within and between small-molecule databases. J. Cheminform. 7:54. doi: 10.1186/s13321-015-0102-6
Algera, M. H., Kamp, J., van der Schrier, R., van Velzen, M., Niesters, M., Aarts, L., et al. (2019). Opioid-induced respiratory depression in humans: a review of pharmacokinetic-pharmacodynamic modelling of reversal. Br. J. Anaesth. 122, e168–e179. doi: 10.1016/j.bja.2018.12.023
Armenian, P., Vo, K. T., Barr-Walker, J., and Lynch, K. L. (2018). Fentanyl, fentanyl analogs and novel synthetic opioids: a comprehensive review. Neuropharmacology 134, 121–132. doi: 10.1016/j.neuropharm.2017.10.016
Baker, L. E., Panos, J. J., Killinger, B. A., Peet, M. M., Bell, L. M., Haliw, L. A., et al. (2009). Comparison of the discriminative stimulus effects of salvinorin A and its derivatives to U69,593 and U50,488 in rats. Psychopharmacology 203, 203–211. doi: 10.1007/s00213-008-1458-3
Bardwell, G., Boyd, J., Arredondo, J., McNeil, R., and Kerr, T. (2019). Trusting the source: the potential role of drug dealers in reducing drug-related harms via drug checking. Drug Alcohol. Depend. 198, 1–6. doi: 10.1016/j.drugalcdep.2019.01.035
Baumann, M. H., Majumdar, S., Le Rouzic, V., Hunkele, A., Uprety, R., Huang, X. P., et al. (2018). Pharmacological characterization of novel synthetic opioids (NSO) found in the recreational drug marketplace. Neuropharmacology 134, 101–107. doi: 10.1016/j.neuropharm.2017.08.016
Beardsley, P. M., and Zhang, Y. (2018). Synthetic opioids. Handb. Exp. Pharmacol. 252, 353–381. doi: 10.1007/164_2018_149
Bluelight, (2019a). Opioids - Big & Dandy Ketobemidone (Ketogan) Thread. Available online at: https://www.bluelight.org/xf/threads/big-dandy-ketobemidone-ketogan-thread.69412/ (accessed August 28, 2019).
Bluelight, (2019b). 6-Mddm. Available online at: https://www.bluelight.org/xf/threads/6-mddm.863982/ (accessed October 9, 2019).
ChemDraw, (2019). Chemical Drawing Software. Available online at: https://www.perkinelmer.com/it/category/chemdraw (accessed October 9, 2019).
Chen, L., Zeng, W. M., Cai, Y. D., Feng, K. Y., and Chou, K. C. (2012). Predicting Anatomical therapeutic chemical (ATC) classification of drugs by integrating chemical-chemical interactions and similarities. PLoS One 7:e35254. doi: 10.1371/journal.pone.0035254
Ciccarone, D., Ondocsin, J., and Mars, S. G. (2017). Heroin uncertainties: exploring users’ perceptions of fentanyl-adulterated and -substituted ‘heroin’. Int. J. Drug Policy 46, 146–155. doi: 10.1016/j.drugpo.2017.06.004
Coe, M. A., Pillitteri, J. L., Sembower, M. A., Gerlach, K. K., and Henningfield, J. E. (2019). Kratom as a substitute for opioids: results from an online survey. Drug Alcohol. Depend. 202, 24–32. doi: 10.1016/j.drugalcdep.2019.05.005
Coffeen, U., and Pellicer, F. (2019). Salvia divinorum: from recreational hallucinogenic use to analgesic and anti-inflammatory action. J. Pain Res. 12, 1069–1076. doi: 10.2147/JPR.S188619
Concheiro, M., Chesser, R., Pardi, J., and Cooper, G. (2018). Postmortem toxicology of new synthetic opioids. Front. Pharmacol. 9:1210. doi: 10.3389/fphar.2018.01210
Corazza, O., Assi, S., Simonato, P., Corkery, J., Bersani, F. S., Demetrovics, Z., et al. (2013). Promoting innovation and excellence to face the rapid diffusion of novel psychoactive substances in the EU: the outcomes of the ReDNet project. Hum. Psychopharmacol. 28, 317–323. doi: 10.1002/hup.2299
Corkery, J. M., Orsolini, L., Papanti, D., and Schifano, F. (2017). From concept(ion) to life after death/the grave: the ‘natural’ history and life cycle(s) of novel psychoactive substances (NPS). Hum. Psychopharmacol. 32:3. doi: 10.1002/hup.2566
Corkery, J. M., Orsolini, L., Papanti, D., and Schifano, F. (2018). Novel Psychoactive Substances (NPS) and Recent Scenarios: Epidemiological, Anthropological and Clinical Pharmacological Issues. Available online at: https://doi.org/10.1039/9781788010344-00207 (accessed September 30, 2019).
Corkery, J. M., Streete, P., Claridge, H., Goodair, C., Papanti, D., Orsolini, L., et al. (2019). Characteristics of deaths associated with kratom use. J. Psychopharmacol. [Epub ahead of print].
Cunliffe, J., Décary-Hêtu, D., and Pollak, T. A. (2019). Nonmedical prescription psychiatric drug use and the darknet: a cryptomarket analysis. Int. J. Drug Policy [Epub ahead of print].
Davey, Z., Schifano, F., Corazza, O., Deluca, P., Schifano, F., Deluca, P., et al. (2012). e-Psychonauts: conducting research in online drug forum communities. J. Ment. Health 21, 386–394. doi: 10.3109/09638237.2012.682265
Davies, M., Nowotka, M., Papadatos, G., Dedman, N., Gaulton, A., Atkinson, F., et al. (2015). ChEMBL web services: streamlining access to drug discovery data and utilities. Nucleic Acids Res. 43, W612–W620. doi: 10.1093/nar/gkv352
DEA, (2019). Controlled Substances - Alphabetical Order. Available online at: https://www.deadiversion.usdoj.gov/schedules/orangebook/c_cs_alpha.pdf (accessed August 22, 2019).
Deluca, P., Davey, Z., Corazza, O., Di Furia, L., Farre, M., Flesland, L. H., et al. (2012). Identifying emerging trends in recreational drug use; outcomes from the Psychonaut Web Mapping Project. Prog. Neuropsychopharmacol. Biol. Psychiatry 39, 221–226. doi: 10.1016/j.pnpbp.2012.07.011
D’Errico, S. (2018). Commentary. Fentanyl-related death and the underreporting risk. J. Foren. Leg. Med. 60, 35–37. doi: 10.1016/j.jflm.2018.09.007
Drugs-forum (2007). Experiences - Ketobemidone Experiences. Available online at: https://drugs-forum.com/threads/ketobemidone-experiences.128285/ (accessed August 28, 2019).
Ellis, C. R., Kruhlak, N. L., Kim, M. T., Hawkins, E. G., and Stavitskaya, L. (2018). Predicting opioid receptor binding affinity of pharmacologically unclassified designer substances using molecular docking. PLoS One 13:e0197734. doi: 10.1371/journal.pone.0197734
Ellis, C. R., Racz, R., Kruhlak, N. L., Kim, M. T., Hawkins, E. G., Strauss, D. G., et al. (2019). Assessing the structural and pharmacological similarity of newly identified drugs of abuse to controlled substances using public health assessment via structural evaluation. Clin. Pharmacol. Ther. 106, 116–122. doi: 10.1002/cpt.1418
EMBL-EBI (2019). CHEMBL Database Release 25. Available online at: https://chembl.gitbook.io/chembl-interface-documentation/downloads (accessed March 6, 2020).
Erowid (2015). Salvinorin B Ethoxymethyl Ether. Available online at: https://erowid.org/chemicals/salvinorin_b_ethoxymethyl_ether/salvinorin_b_ethoxymethyl_ether.shtml (accessed August 13, 2019).
European Database on New Drugs [EDND], (2019). EDND - Login Page. Available online at: https://ednd2.emcdda.europa.eu/ednd/login (accessed August 28, 2019).
European Monitoring Centre for Drugs and Drug Addiction [EMCDDA], (2019). European Drug Report 2019. Available online at: http://www.emcdda.europa.eu/edr2019 (accessed August 9, 2019).
Financial Crimes Enforcement Network [FinCHEN], (2019). Advisory to Financial Institutions on Illicit Financial Schemes and Methods Related to the Trafficking of Fentanyl and Other Synthetic Opioids. Available online at: https://www.fincen.gov/sites/default/files/advisory/2019-08-21/Fentanyl%20Advisory%20FINAL%20508.pdf (accessed January 3, 2019).
Fluyau, D., and Revadigar, N. (2017). Biochemical benefits, diagnosis, and clinical risks evaluation of kratom. Front. Psychiatry 8:62. doi: 10.3389/fpsyt.2017.00062
Frisoni, P., Bacchio, E., Bilel, S., Talarico, A., Gaudio, R. M., Barbieri, M., et al. (2018). Novel synthetic opioids: the pathologist’s point of view. Brain Sci. 8:E170. doi: 10.3390/brainsci8090170
Galanie, S., Thodey, K., Trenchard, I. J., Filsinger Interrante, M., and Smolke, C. D. (2015). Complete biosynthesis of opioids in yeast. Science 349, 1095–1100. doi: 10.1126/science.aac9373
Gaulton, A., Hersey, A., Nowotka, M., Bento, A. P., Chambers, J., Mendez, D., et al. (2017). The ChEMBL database in 2017. Nucleic Acids Res. 45, D945–D954. doi: 10.1093/nar/gkw1074
Gerace, E., Salomone, A., Luciano, C., Di Corcia, D., and Vincenti, M. (2018a). First Case in Italy of fatal intoxication involving the new opioid U-47700. Front. Pharmacol. 9:747. doi: 10.3389/fphar.2018.00747
Gerace, E., Salomone, A., and Vincenti, M. (2018b). Analytical approaches in fatal intoxication cases involving new synthetic opioids. Curr. Pharm. Biotechnol. 19, 113–123. doi: 10.2174/1389201019666180405162734
Gilardi, F., Augsburger, M., and Thomas, A. (2018). Will widespread synthetic opioid consumption induce epigenetic consequences in future generations? Front. Pharmacol. 9:702. doi: 10.3389/fphar.2018.00702
Giorgetti, A., Centola, C., and Giorgetti, R. (2017). Fentanyl novel derivative-related deaths. Hum. Psychopharmacol. 32:3. doi: 10.1002/hup.2605
Google, (2019). Available online at: https://www.google.com/ (accessed September 30, 2019).
Google Scholar, (2019). Available online at: https://scholar.google.com/ (accessed September 30, 2019).
GOV.UK, (2017). Controlled Drugs List. Available online at: https://www.gov.uk/government/publications/controlled-drugs-list–2 (accessed August 22, 2019).
Graziano, S., Orsolini, L., Rotolo, M. C., Tittarelli, R., Schifano, F., and Pichini, S. (2017). Herbal highs: review on psychoactive effects and neuropharmacology. Curr. Neuropharmacol. 15, 750–761. doi: 10.2174/1570159X14666161031144427
Guirguis, A., Corkery, J., Stair, J., Kirton, S., Zloh, M., and Schifano, F. (2017). Intended and unintended use of cathinone mixtures. Hum. Psychopharmacol. Clin. Exp. 32:e2598. doi: 10.1002/hup.2598
Hähnke, V. D., Kim, S., and Bolton, E. E. (2018). PubChem chemical structure standardization. J. Cheminform. 10:36. doi: 10.1186/s13321-018-0293-8
Hassan, Z., Bosch, O. G., Singh, D., Narayanan, S., Kasinather, B. V., Seifritz, E., et al. (2017). Novel psychoactive substances-recent progress on neuropharmacological mechanisms of action for selected drugs. Front. Psychiatry 8:152. doi: 10.3389/fpsyt.2017.00152
Helmerhorst, G. T., Teunis, T., Janssen, S. J., and Ring, D. (2017). An epidemic of the use, misuse and overdose of opioids and deaths due to overdose, in the United States and Canada: is Europe next. Bone Joint J. 99, 856–864. doi: 10.1302/0301-620X.99B7.BJJ-2016-1350.R1
Huhn, A. S., Strain, E. C., Tompkins, D. A., and Dunn, K. E. (2018). A hidden aspect of the U.S. opioid crisis: rise in first-time treatment admissions for older adults with opioid use disorder. Drug Alcohol. Depend. 193, 142–147. doi: 10.1016/j.drugalcdep.2018.10.002
International Narcotics Control Board [INCB], (2019a). INCB Fentanyl-Related Substances With No Known Legitimate Uses. Available online at: https://www.incb.org/incb/en/news/news_2019/experts-and-industry-strategize-next-steps-in-implementing-incbs-list-of-fentanyl-related-substances-with-no-legitimate-uses.html (accessed September 30, 2019).
International Narcotics Control Board [INCB], (2019b). INCB Yellow List. 2019. Available online at: https://www.incb.org/incb/en/narcotic-drugs/Yellowlist_Forms/yellow-list.html (accessed August 8, 2019).
Kacinko, S. L., and Papsun, D. M. (2019). The evolving landscape of designer drugs methods. Mol. Biol. 1872, 129–135. doi: 10.1007/978-1-4939-8823-5_13
Kakko, J., Alho, H., Baldacchino, A., Molina, R., Nava, F. A., and Shaya, G. (2019). Craving in opioid use disorder: from neurobiology to clinical practice. Front. Psychiatry 10:592. doi: 10.3389/fpsyt.2019.00592
Kalyanam, J., Katsuki, T., Lanckriet, G., and Mackey, T. K. (2017). Exploring trends of nonmedical use of prescription drugs and polydrug abuse in the Twittersphere using unsupervised machine learning. Addict. Behav. 65, 289–295. doi: 10.1016/j.addbeh.2016.08.019
Kata, V., Novitch, M. B., Jones, M. R., Anyama, B. O., Helander, E. M., and Kaye, A. D. (2018). Opioid addiction, diversion, and abuse in chronic and cancer pain. Curr. Opin. Support. Palliat. Care 12, 124–130. doi: 10.1097/SPC.0000000000000333
Kelley-Quon, L. I., Cho, J., Strong, D. R., Miech, R. A., Barrington-Trimis, J. L., Kechter, A., et al. (2019). Association of nonmedical prescription opioid use with subsequent heroin use initiation in adolescents. JAMA Pediatr. [Epub ahead of print].
Kim, S. J., Marsch, L. A., Hancock, J. T., and Das, A. K. (2017). Scaling up research on drug abuse and addiction through social media big data. J. Med. Internet Res. 19:e353. doi: 10.2196/jmir.6426
Kraemer, M., Boehmer, A., Madea, B., and Maas, A. (2019). Death cases involving certain new psychoactive substances: a review of the literature. Foren. Sci. Int. 298, 186–267. doi: 10.1016/j.forsciint.2019.02.021
Krotulski, A. J., and Logan, B. K. (2018). Isopropyl-U-47700 Sample Type: Biological Fluid. Available online at: https://www.forensicscienceeducation.org/wp-content/uploads/2018/05/Isopropyl-U-47700_051818_ToxicologyAnalyticalReport.pdf (accessed August 13, 2019).
Lajtai, A., Mayer, M., Lakatos, A., Porpáczy, Z., and Miseta, A. (2016). Embutramide, a component of tanax(®) (T-61) as a new drug of abuse. J. Foren. Sci. 61, 573–575. doi: 10.1111/1556-4029.13010
Li, J., Xu, Q., Shah, N., and Mackey, T. K. (2019). A machine learning approach for the detection and characterization of illicit drug dealers on instagram: model evaluation study. J. Med. Internet Res. 21:e13803. doi: 10.2196/13803
Lipiński, P. F. J., Kosson, P., Matalińska, J., Roszkowski, P., Czarnocki, Z., Jarończyk, M., et al. (2019). Fentanyl family at the mu-opioid receptor: uniform assessment of binding and computational analysis. Molecules 24:E740. doi: 10.3390/substances24040740
Liu, Z., and Udenigwe, C. C. (2018). Role of food-derived opioid peptides in the central nervous and gastrointestinal systems. J. Food Biochem. 43:e12629. doi: 10.1111/jfbc.12629
Loi, B., Zloh, M., De Luca, M. A., Pintori, N., Corkery, J., and Schifano, F. (2017). 4,4′-Dimethylaminorex (‘4,4′-DMAR’; Serotoni’) misuse: a web-based study. Hum. Psychopharmacol. Clin. Exp. 32:E2575. doi: 10.1002/hup.2575
Lovrecic, B., Lovrecic, M., Gabrovec, B., Carli, M., Pacini, M., Maremmani, A. G. I., et al. (2019). Non-medical use of novel synthetic opioids: a new challenge to public health. Int. J. Environ. Res. Public Health 16:E177. doi: 10.3390/ijerph16020177
Mackey, T., Kalyanam, J., Klugman, J., Kuzmenko, E., and Gupta, R. (2018). Solution to detect, classify, and report illicit online marketing and sales of controlled substances via twitter: using machine learning and web forensics to combat digital opioid access. J. Med. Internet Res. 20:e10029. doi: 10.2196/10029
McLean, K., Monnat, S. M., Rigg, K., Sterner, G. E., and Verdery, A. (2019). You never know what you’re getting: opioid users’ perceptions of fentanyl in southwest pennsylvania. Subst. Use Misuse 54, 955–966. doi: 10.1080/10826084.2018.1552303
Misailidi, N., Papoutsis, I., Nikolaou, P., Dona, A., Spiliopoulou, C., and Athanaselis, S. (2018). Fentanyls continue to replace heroin in the drug arena: the cases of ocfentanil and carfentanil. Foren. Toxicol. 36, 12–32. doi: 10.1007/s11419-017-0379-4
Morrow, J. B., Ropero-Miller, J. D., Catlin, M. L., Winokur, A. D., Cadwallader, A. B., Staymates, J. L., et al. (2019). The opioid epidemic: moving toward an integrated, holistic analytical response. J. Anal. Toxicol. 43, 1–9. doi: 10.1093/jat/bky049
Negri, L., Melchiorri, P., and Lattanzi, R. (2000). Pharmacology of amphibian opiate peptides. Peptides 21, 1639–1647. doi: 10.1016/s0196-9781(00)00295-3
Ohinata, K., Agui, S., and Yoshikawa, M. (2007). Soymorphins, novel mu opioid peptides derived from soy beta-conglycinin beta-subunit, have anxiolytic activities. Biosci. Biotechnol. Biochem. 71, 2618–2621. doi: 10.1271/bbb.70516
Orsolini, L., Papanti, D., Corkery, J., and Schifano, F. (2017). An insight into the deep web; why it matters for addiction psychiatry. Hum. Psychopharmacol. 32, e2573. doi: 10.1002/hup.2573
Orsolini, L., Papanti, G. D., Francesconi, G., and Schifano, F. (2015). Mind navigators of chemicals’ experimenters? A web-based description of e-psychonauts. Cyberpsychol. Behav. Soc. Netw. 18, 296–300. doi: 10.1089/cyber.2014.0486
Oye, K. A., Lawson, J. C., and Bubela, T. (2015). Drugs: regulate ‘home-brew’ opiates. Nature 521, 281–283. doi: 10.1038/521281
Pandrekar, S., Chen, X., Gopalkrishna, G., Srivastava, A., Saltz, M., Saltz, J., et al. (2018). Social media based analysis of opioid epidemic using reddit AMIA. Annu. Symp. Proc. 2018, 867–876.
Pardo, B., Taylor, J., Caulkins, J. P., Kilmer, B., Reuter, P., and Stein, B. D. (2019). The Future of Fentanyl and Other Synthetic Opioids. Available online at: https://www.rand.org/content/dam/rand/pubs/research_reports/RR3100/RR3117/RAND_RR3117.pdf (accessed January 3, 2019).
Peet, M. M., and Baker, L. E. (2011). Salvinorin B derivatives, EOM-Sal B and MOM-Sal B, produce stimulus generalization in male sprague-dawley rats trained to discriminate salvinorin A. Behav. Pharmacol. 22, 450–457. doi: 10.1097/FBP.0b013e328349fc1b
Pérez-Mañá, C., Papaseit, E., Fonseca, F., Farré, A., Torrens, M., and Farré, M. (2018). Drug interactions with new synthetic opioids. Front. Pharmacol. 9:1145. doi: 10.3389/fphar.2018.01145
Pergolizzi, J. V. Jr., Raffa, R. B., Taylor, R. Jr., and Vacalis, S. (2018). Abuse-deterrent opioids: an update on current approaches and considerations. Curr. Med. Res. Opin. 34, 711–723. doi: 10.1080/03007995.2017
Pichini, S., Solimini, R., Berretta, P., Pacifici, R., and Busardò, F. P. (2018). Acute intoxications and fatalities from illicit fentanyl and analogues: an update. Ther. Drug Monit. 40, 38–51. doi: 10.1097/FTD.0000000000000465
PiHKAL, (2019). Fentanyl Landscape Info. Available online at: https://isomerdesign.com/PiHKAL/tableLandscape.php?domain=pk&property=fentanyl&sort=name (accessed August 8, 2019).
Prekupec, M. P., Mansky, P. A., and Baumann, M. H. (2017). Misuse of novel synthetic opioids: a deadly new trend. J. Addict. Med. 11, 256–265. doi: 10.1097/ADM.0000000000000324
PubChem, (2019). Available online at: https://pubchem.ncbi.nlm.nih.gov/ (accessed August 8, 2019).
PubMed, (2019). Home - PubMed - NCBI. Available online at: https://www.ncbi.nlm.nih.gov/pubmed/ (accessed September 30, 2019).
Reddit, (2019a). Bromadol BDPC?: Researchchemicals. Available online at: https://www.reddit.com/r/researchchemicals/comments/an9mos/bromadol_bdpc/ (accessed August 13, 2019).
Reddit, (2019b). Human Bioassay of Salvinorin B Ethoxymethyl Ether (Symmetry) a Novel and Unusually Potent and Longer Lasting Salvinorin Analogue: Salvia. Available online at: https://www.reddit.com/r/Salvia/comments/42j4ew/human_bioassay_of_salvinorin_b_ethoxymethyl_ether/ (accessed August 13, 2019).
Reddit, (2019c). Ketobemidone Derivates - Considered One of the Holy Grail of Opiates, since They Are Not Even Scheduled, Why They Don’t Hit the RCs Scene Markets?: Opioid_RCs. Available online at: https://www.reddit.com/r/Opioid_RCs/comments/bbdwlv/ketobemidone_derivates_considered_one_of_the_holy/ (accessed August 28, 2019).
Reddit, (2019d). Opiates. Available online at: https://www.reddit.com/r/opiates/ (accessed August 28, 2019).
Reddit, (2019e). Other than Fent, What Are Other Cutting Chems?: Opiates. Available online at: https://www.reddit.com/r/opiates/comments/bq2k4s/other_than_fent_what_are_other_cutting_chems/ (accessed August 13, 2019).
Reddit, (2019f). Salvinorin B Methoxymethyl Ether: A Drug For Brave Psychonauts?: Researchchemicals. Available online at: https://www.reddit.com/r/researchchemicals/comments/8fm9p4/salvinorin_b_methoxymethyl_ether_a_drug_for_brave/ (accessed August 28, 2019).
Schifano, F., Chiappini, S., Corkery, J. M., and Guirguis, A. (2019a). Assessing the 2004-2018 fentanyl misusing issues reported to an international range of adverse reporting systems. Front. Pharmacol. 10:46. doi: 10.3389/fphar.2019.00046
Schifano, F., Napoletano, F., Chiappini, S., Guirguis, A., Corkery, J. M., Bonaccorso, S., et al. (2019b). New/emerging psychoactive substances and associated psychopathological consequences. Psychol. Med. [Epub ahead of print].
Schifano, F., Orsolini, L., Duccio Papanti, G., and Corkery, J. M. (2015). Novel psychoactive substances of interest for psychiatry. World Psychiatry 14, 15–26. doi: 10.1002/wps.20174
Schueler, H. E. (2017). Emerging synthetic fentanyl analogs. Acad. Foren. Pathol. 7, 36–40. doi: 10.23907/2017.004
Sharma, K. K., Hales, T. G., Rao, V. J., NicDaeid, N., and McKenzie, C. (2019). The search for the “next” euphoric non-fentanil novel synthetic opioids on the illicit drugs market: current status and horizon scanning. Foren. Toxicol. 37, 1–16. doi: 10.1007/s11419-018-0454-5
Simonato, P., Corazza, O., Santonastaso, P., Corkery, J., Deluca, P., Davey, Z., et al. (2013). Novel psychoactive substances as a novel challenge for health professionals: results from an Italian survey. Hum. Psychopharmacol. 28, 324–331. doi: 10.1002/hup.2300
Smith, J. S., Lefkowitz, R. J., and Rajagopal, S. (2018). Biased signalling: from simple switches to allosteric microprocessors. Nat. Rev. Drug Discov. 17, 243–260. doi: 10.1038/nrd.2017.229
Stein, C. (2016). Opioid receptors. Annu. Rev. Med. 67, 433–451. doi: 10.1146/annurev-med-062613-093100
Stein, M. D., Kenney, S. R., Anderson, B. J., and Bailey, G. L. (2019). Perceptions about fentanyl-adulterated heroin and overdose risk reduction behaviors among persons seeking treatment for heroin use. J. Subst. Abuse Treat. 104, 144–147. doi: 10.1016/j.jsat.2019.07.006
Suzuki, J., and El-Haddad, S. (2017). A review: fentanyl and non-pharmaceutical fentanyls. Drug Alcohol. Depend. 171, 107–116. doi: 10.1016/j.drugalcdep.2016.11.033
Tabarra, I., Soares, S., Rosado, T., Gonçalves, J., Luís, A., Malaca, S., et al. (2019). Novel synthetic opioids - toxicological aspects and analysis. Foren. Sci. Res. 4, 111–140. doi: 10.1080/20961790.2019.1588933
Teschemacher, H., Koch, G., and Brantl, V. (1997). Milk protein-derived opioid receptor ligands. Biopolymers 43, 99–117. doi: 10.1002/(sici)1097-0282(1997)43:2¡99::aid-bip3¿3.0.co;2-v
TripSit Factsheets, (2019a). Bromadol. Available online at: http://drugs.tripsit.me/bromadol (accessed August 13, 2019).
TripSit Factsheets, (2019b). 6-MDDM. Available online at: http://drugs.tripsit.me/6-mddm (accessed August 13, 2019).
Tzanetakis, M. (2018). Comparing cryptomarkets for drugs. A characterisation of sellers and buyers over time. Int. J. Drug Policy 56, 176–186. doi: 10.1016/j.drugpo.2018.01.022
United Nations Office on Drugs and Crime [UNODC], (1954). UNODC - Bulletin on Narcotics - 1954 Issue 3 - 005. Available online at: https://www.unodc.org/unodc/en/data-and-analysis/bulletin/bulletin_1954-01-01_3_page006.html (accessed August 28, 2019).
United Nations Office on Drugs and Crime [UNODC], (2019a). Conventions. Available online at: https://www.unodc.org/unodc/en/commissions/CND/conventions.html (accessed August 12, 2019).
United Nations Office on Drugs and Crime [UNODC], (2019b). UNODC Early Warning Advisory (EWA) on New Psychoactive Substances (NPS). Available online at: https://www.unodc.org/LSS/Home/NPS (accessed August 8, 2019).
United Nations Office on Drugs and Crime [UNODC], (2019c). World Drug Report 2019: 35 Million People Worldwide Suffer from Drug Use Disorders While Only 1 in 7 People Receive Treatment. Available online at: https://www.unodc.org/unodc/en/frontpage/2019/June/world-drug-report-2019_-35-million-people-worldwide-suffer-from-drug-use-disorders-while-only-1-in-7-people-receive-treatment.html (accessed August 9, 2019).
Unodc Early Warning Advisory on New Psychoactive Substances [UNODC EWA NPS], (2019). News: February 2019 – UNODC-SMART: Almost 900 NPS Reported to UNODC from 119 Countries and Territories. Available online at: https://www.unodc.org/LSS/Announcement/Details/eff8dc38-7ab0-42b0-8cd9-753b89953fcc (accessed September 30, 2019).
Valentino, R. J., and Volkow, N. (2018). Untangling the complexity of opioid receptor function. Neuropsychopharmacology 43, 2514–2520. doi: 10.1038/s41386-018-0225-3
van Amsterdam, J., and van den Brink, W. (2015). The misuse of prescription opioids: a threat for europe. Curr. Drug Abuse Rev. 8, 3–14. doi: 10.2174/187447370801150611184218
Varga, A. G., Reid, B. T., Kieffer, B. L., and Levitt, E. S. (2020). Differential impact of two critical respiratory centres in opioid-induced respiratory depression in awake mice. J. Physiol. 598, 189–205. doi: 10.1113/JP278612
Ventura, L., Carvalho, F., and Dinis-Oliveira, R. J. (2018). Opioids in the frame of new psychoactive substances network: a complex pharmacological and toxicological issue. Curr. Mol. Pharmacol. 11, 97–108. doi: 10.2174/1874467210666170704110146
Wang, Y. S. (2019). Exploring the “like” in the psychological interaction of users on fan community: a netnography analysis. J. Commun. Psychol. 47, 1380–1398. doi: 10.1002/jcop.22192
Whitehouse, (2019). 21st Century Drug Trafficking: “Manufacturing Advisory” on Fentanyl and Other Synthetic Opioids (Tab A). Available online at: https://www.whitehouse.gov/wp-content/uploads/2019/08/Fentanyl-Advisory-Manufacturing-Tab-A.pdf (accessed January 3, 2020).
WHO Collaborating Centre [WHOCC], (2016). WHOCC - ATC Classification of Combinations of Opioids and Other Analgesics. Available online at: https://www.whocc.no/news/atc_classification_of_combinations_of_opioids_and_other_anal (accessed July 18, 2019).
WHO Collaborating Centre [WHOCC], (2019). WHOCC - ATC/DDD Index. Available online at: https://www.whocc.no/atc_ddd_index/ (accessed August 9, 2019).
Wilcoxon, R. M., Middleton, O. L., Meyers, S. E., Kloss, J., and Love, S. A. (2018). The elephant in the room: outbreak of carfentanil deaths in minnesota and the importance of multiagency collaboration. Acad. Foren. Pathol. 8, 729–737. doi: 10.1177/1925362118797746
Wilde, M., Pichini, S., Pacifici, R., Tagliabracci, A., Busardò, F. P., Auwärter, V., et al. (2019). Metabolic pathways and potencies of new fentanyl analogs. Front. Pharmacol. 10:238. doi: 10.3389/fphar.2019.00238
World Health Organization [WHO], (2016). U-47700 Critical Review Report Agenda Item 4.1 Expert Committee on Drug Dependence Thirty-Eighth Meeting. Available online at: https://www.who.int/medicines/access/controlled-substances/4.1_U-47700_CritReview.pdf (accessed August 12, 2019).
World Health Organization [WHO], (2018). WHO Expert Committee on Drug Dependence Forty-First Report. Available online at: https://www.who.int/medicines/access/controlled-substances/ecdd_41_meeting/en/ (accessed August 12, 2019).
Xu, H., Chen, J., and Chi, Z. Q. (1985). Ohmefentanyl–a new agonist for mu-opiate receptor. Chem. Biol. Agric. Med. Earth Sci. 28, 504–511.
Yin, S. (2019). Adolescents and drug abuse: 21st century synthetic substances. Clin. Pediatr. Emerg. Med. 20, 17–24. doi: 10.1016/J.CPEM.2019.03.003
Zawilska, J. B. (2017). An expanding world of novel psychoactive substances: opioids. Front. Psychiatr. 8:110. doi: 10.3389/fpsyt.2017.00110
Zhao, M. (2019). The illicit supply of new psychoactive substances within and from china: a descriptive analysis. Int. J. Offend. Ther. Comp. Crim. [Epub ahead of print].
Keywords: psychonauts, novel psychoactive substance, novel synthetic opioids, fentanyl analogs, web crawling, drug misuse, prescribed drug misuse
Citation: Arillotta D, Schifano F, Napoletano F, Zangani C, Gilgar L, Guirguis A, Corkery JM, Aguglia E and Vento A (2020) Novel Opioids: Systematic Web Crawling Within the e-Psychonauts’ Scenario. Front. Neurosci. 14:149. doi: 10.3389/fnins.2020.00149
Received: 13 October 2019; Accepted: 07 February 2020;
Published: 18 March 2020.
Edited by:
Liana Fattore, Italian National Research Council, ItalyReviewed by:
Mariana Spetea, University of Innsbruck, AustriaSelena Bartlett, The University of Queensland, Australia
Copyright © 2020 Arillotta, Schifano, Napoletano, Zangani, Gilgar, Guirguis, Corkery, Aguglia and Vento. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Davide Arillotta, ZGF2aWRlLmFyaWxsb3R0YUB5YWhvby5pdA==; Fabrizio Schifano, Zi5zY2hpZmFub0BoZXJ0cy5hYy51aw==
 Davide Arillotta
Davide Arillotta Fabrizio Schifano
Fabrizio Schifano Flavia Napoletano
Flavia Napoletano Caroline Zangani2,4
Caroline Zangani2,4 John Martin Corkery
John Martin Corkery