
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
MINI REVIEW article
Front. Neurosci., 19 December 2017
Sec. Social and Evolutionary Neuroscience
Volume 11 - 2017 | https://doi.org/10.3389/fnins.2017.00708
This article is part of the Research TopicLanguage at the Interface Between the Skull and the BrainView all 5 articles
Deformational plagiocephaly and craniosynostosis are two of the most common neonatal cranial head shape anomalies. Traditionally, both entities were thought to cause aesthetic concerns solely. Recently, many groups have demonstrated that both conditions are strongly associated with developmental delays. The relationship between the abnormal neonatal cranial shape and early developmental delays manifested in both conditions remains poorly understood.
Neonatal cranial head shape anomalies are common and have been attributed to a multitude of factors. Interestingly, despite recent advances in global health care, the incidence of some cranial anomalies has been increasing, making awareness and access to care ever more important. Typically, cranial head shape anomalies are identified in the 1st months of life by primary care providers, who refer these infants to a multi-disciplinary team that specializes in craniofacial disorders. While craniofacial clinics have always been well-suited to manage the aesthetics concerns of cranial head shape anomalies, only recently have concomitant neurodevelopmental delays begun to be addressed in these specialty clinics.
Deformational plagiocephaly (DP), also termed positional plagiocephaly, and craniosynostosis (CS) are two of the most common cranial anomalies encountered in craniofacial clinics. Both conditions can significantly distort the closed cranial vault anatomy in which the developing brain presides. Coincidentally, both conditions are associated with neonatal developmental delays yet it remains indeterminate whether the relationship is causative or correlative. This question has focused recent research efforts to study the impact that the cranial vault shape has on normal brain function and development.
DP is the most common neonatal head shape anomaly affecting 13–48% infants less than 1 year of age (Peitsch et al., 2002). This condition is thought to be exacerbated by prolonged supine positioning. As a result, the skull develops an oblique, parallelogram shape that varies in the severity of the calvarial vault asymmetry (Figure 1). The recent increase in incidence is attributed to the “Back to Sleep Program” introduced by the American Academy of Pediatrics, aimed at combatting the rising numbers of Sudden Infant Death Syndrome (SIDS) (Branch et al., 2015). Interestingly, despite the program's near-universal acceptance by primary care providers, only a minority of infants develop DP, suggesting that this condition is multi-factorial (Habal et al., 2003, 2004). Fortunately, this condition is non-surgical and is managed effectively over several weeks to months with either cranial repositioning interventions or helmet orthosis, though the latter lacks supportive data (Weissler et al., 2016).
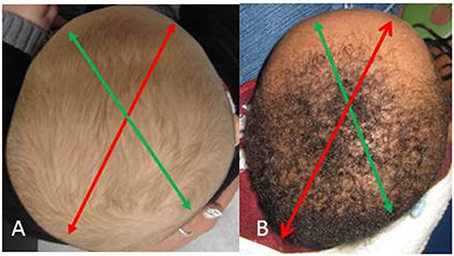
Figure 1. Deformational plagiocephaly. (A) Mild right-sided occipital flattening with minimal frontal changes (B) Severe right-sided occipital flattening with significant contra-lateral frontal deformity. Red arrow indicates long axis and green arrow indicates short axis of cranial vault asymmetry.
Many studies have demonstrated that both motor and cognitive delays are associated with DP (Miller and Clarren, 2000; Panchal et al., 2001; Kordestani et al., 2006; Speltz et al., 2010; Collett et al., 2011, 2013; Fontana et al., 2016). The timing of when developmental delays begin remains unknown and most likely delays are manifested as a result of events early in the 1st year of life. More concerning is the recent finds that demonstrate infants with DP are unlikely to developmentally “catch up” to their normocephalic peers when compared at adolescences (Miller and Clarren, 2000). This observation suggests that normal brain development might be both spatially and temporally affected by cranial vault shape during infancy. Although the current medical literature contains many studies showing correlation between DP and developmental delays, no study proves causation. This is an important knowledge gap to consider as DP is a mult-factoral condition (Habal et al., 2003, 2004). Further work is needed to expand on our current knowledge and how best to manage infants with DP.
CS is a much less common disorder (incidence of 1 in 1,800 to 3,000) and results from early fusion of fibrous cranial sutures which serve as growth centers separating immature, growing cranial bones. Premature ossification and union of individual cranial bones, according to Virchow's rule, results in abnormal cranial growth parallel to the fused suture(s). CS requires surgical correction and often cranial vault expansion/remodeling to restore the “normal” infant head shape and aesthetics. Both the timing and the specific operative technique to restore normal cranial anatomy are surgeon-dependent, creating a confounding factor that permeates the literature on this topic.
It is well established that syndromic variants of CS are often associated with neurologic delay. In addition, non-syndromic CS has also been associated with developmental delay but much less commonly. In 2000, Renier et al. first demonstrated that neurodevelopment was delayed in non-syndromic infants with single suture CS (Renier et al., 2000). Prior to this publication most considered CS to be solely an aesthetic problem, yet others quickly confirmed similar observations (Becker et al., 2005; Patel et al., 2014). Interestingly, isolated metopic synostosis has been repeatedly associated with cognitive, behavioral, and language delays (Sidoti et al., 1996; Mendonca et al., 2009). The association between metopic CS and developmental delays poses the question of whether bifrontotemporoparietal brain development is spatially constricted, limiting development in these infants (Figure 2). Another equally plausible scenario is that the lateral frontal lobes are hypoplastic in infants with metopic CS. As a result, poor lateral brain growth results in trigonocephaly. Interestingly, delays are less frequently observed in unilateral and bilateral coronal CS, yet this condition constricts a similar anatomic area but in a different conformation.
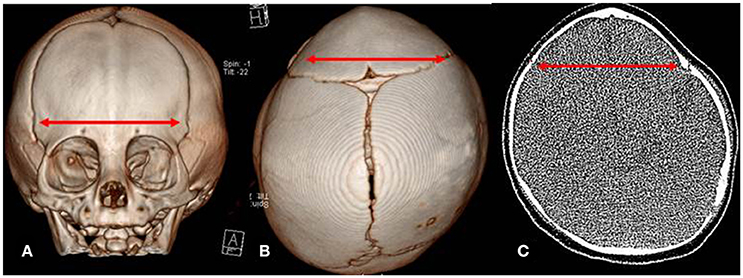
Figure 2. Computed Tomography (CT) images of metopic craniosynostois. (A) Anterior view of metopic deformity (B) Vertex view of metopic deformity with mild occipital deformational plagiocephaly (C) Axial view of metopic deformity. Red arrow indicates bifrontotemporoparietal narrowing in each view.
Further complicating the literature is a lack of uniformity in developmental assessment tools. Methods of assessment range from subjective questionnaires completed solely by the parents or guardians (Denver II Developmental Milestones, Ages and Stages questionnaire, and/or MacArthur-Bates Assessment) to objective measures requiring infant participation, such as the Bayley Scales of Infant and Toddler Development III. A common problem with all these measures is that they are limited to certain age ranges and correlation with adolescent and/or adult development is modest at best. One plausible solution is to utilize to utilize a battery of other developmental tests as an initial screening and longitudinal assessment tool (Hashim et al., 2014). Such assessments include the Wechsler Abbreviated Scale of Intelligence, Wechler Fundamentals, Beery-Buktencia Developmental Test of Visual Motor Integration, Behavioral Rating Inventory of Executive Function, and the Behavioral Assessment System for Children. Unfortunately, providers skilled in their implementation are scarce, thus limiting their use and acceptance. As such, no tool has been universally accepted to screen and assess developmental outcomes in craniofacial clinics (Andrews and Fontana, 2016; Fontana et al., 2016).
For several years our craniofacial team has been investigating neurodevelopmental problems associated with both DP and CS. We have conducted prospective studies involving both conditions. Our team has demonstrated that surprisingly, the severity of DP cannot be used to predict either the presence or degree of infant developmental delays (Fontana et al., 2016). Therefore, we recommend that all infants with DP be assessed for delays and, when appropriate, additional supportive services be provided. Furthermore, our studies involving infants with delayed presentation CS (after 1 year of age) demonstrated developmental problems in all infants with cognitive being the most common delay (Fontana et al., 2018). This same study showed that these delays are reversible or improve with cranial vault expansion surgery indicating that the developing brain is capable of repair when abnormal cranial anatomy is corrected. Recently, we have performed serial developmental testing on infants with moderate metopic CS. The majority of these infants demonstrated either a cognitive, language or motor delay at presentation that persisted with observation-only. An age-matched cohort who chose to undergo late cranial vault expansion (greater than 12 months of age) demonstrated improvement in their respective area of developmental delay within 1 year of their surgery (submitted for publication).
There are several problems and criticisms of the medical literature concerning the relationship of developmental delay with DP and CS. First, most studies are retrospective and/or observational in design. This limits the conclusions that can be drawn from their results and at best the relationship remains correlative not causative. Second, as stated earlier, there is no uniformly accepted developmental screening tool to utilize and assess outcomes among differing institutions. Since centers use different developmental assessments it is difficult to compare results amongst institutions. Finally, all current DP and CS studies are from single institutions only with no multi-center studies or meta-analyses available to interpret. To obtain more useful information a large multi-center study or database is required. These knowledge gaps create a large hole in the medical literature. Further work is needed to better understand the relationship between cranial bone growth patterns and infant neurodevelopment. Many groups, including our own, have demonstrated that abnormal skull growth associated with both DP and CS significantly increases the likelihood of developmental delays. While the cause of these delays occur is yet poorly understood, there does seem to be a trend toward normalization in infants with CS who have surgical correction.
Both BA and SF were involved in the data collection, review of literature and the writing of this paper.
Research for this project was done in conjunction with funding support from the National Institute of Dental and Craniofacial Research (1R03DE025906-01A1).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Andrews, B. T., and Fontana, S. C. (2016). Plagiocephaly and developmental delay: the expanding role of the craniofacial surgeon. J. Craniofac. Surg. 27, 1381–1382. doi: 10.1097/SCS.0000000000002872
Becker, D. B., Petersen, J. D., Kane, A. A., Cradock, M. M., Pilgram, T. K., and Marsh, J. L. (2005). Speech, cognitive, and behavioral outcomes in nonsyndromic craniosynostosis. Plast. Reconstr. Surg. 116, 400–407. doi: 10.1097/01.prs.0000172763.71043.b8
Branch, L. G., Kesty, K., Krebs, E., Wright, L., Leger, S., and David, L. R. (2015). Deformational plagiocephaly and craniosynostosis: trends in diagnosis and treatment after the “back to sleep” campaign. J. Craniofac. Surg. 26, 147–150. doi: 10.1097/SCS.0000000000001401
Collett, B. R., Gray, K. E., Starr, J. R., Heike, C. L., Cunningham, M. L., and Speltz, M. L. (2013). Development at age 36 months in children with deformational plagiocephaly. Pediatrics 131, e109–e115. doi: 10.1542/peds.2012-1779
Collett, B. R., Starr, J. R., Kartin, D., Heike, C. L., Berg, J., Cunningham, M. L., et al. (2011). Development in toddlers with and without deformational plagiocephaly. Arch. Pediatr. Adolesc. Med. 165, 653–658. doi: 10.1001/archpediatrics.2011.92
Fontana, C. S., Belinger, S., Daniels, D., Tuttle, M., Camarata, P. J., and Andrews, B. T. (2018). Longitudinal assessment of developmental outcomes in infants undergoing late craniosynostosis repair. J. Craniofac. Surg. (Accepted in press).
Fontana, S. C., Daniels, D., Greaves, T., Nazir, N., Searl, J., and Andrews, B. T. (2016). Assessment of deformational plagiocephaly severity and neonatal developmental delay. J. Craniofac. Surg. 27, 1934–1936. doi: 10.1097/SCS.0000000000003014
Habal, M. B., Castelano, C., Hemkes, N., Scheuerle, J., and Guilford, A. M. (2004). In search of causative factors of deformational plagiocephaly. J. Craniofac. Surg. 15, 835–841. doi: 10.1097/00001665-200409000-00025
Habal, M. B., Leimkuehler, T., Chambers, C., Scheuerle, J., and Guilford, A. M. (2003). Avoiding the sequela associated with deformational plagiocephaly. J. Craniofac. Surg. 14, 430–437. doi: 10.1097/00001665-200307000-00004
Hashim, P. W., Patel, A., Yang, J. F., Travieso, R., Terner, J., Losee, J. E., et al. (2014). The effects of whole-vault cranioplasty vs. strip craniectomy on long-term neuropsychological outcomes in sagittal craniosynostosis. Plast. Reconstr. Surg. 134, 491–501. doi: 10.1097/PRS.0000000000000420
Kordestani, R. K., Patel, S., Bard, D. E., Gurwitch, R., and Panchal, J. (2006). Neurodevelopmental delays in children with deformational plagiocephaly. Plast. Reconstr. Surg. 117, 207–218; discussion: 219–220. doi: 10.1097/01.prs.0000185604.15606.e5
Mendonca, D. A., White, N., West, E., Dover, S., Solanki, G., and Nishikawa, H. (2009). Is there a relationship between the severity of metopic synostosis and speech and language impairments? J. Craniofac. Surg. 20, 85–88; discussion: 89. doi: 10.1097/SCS.0b013e3181955244
Miller, R. I., and Clarren, S. K. (2000). Long-term developmental outcomes in patients with deformational plagiocephaly. Pediatrics 105:E26. doi: 10.1542/peds.105.2.e26
Panchal, J., Amirsheybani, H., Gurwitch, R., Cook, V., Francel, P., Neas, B., et al. (2001). Neurodevelopment in children with single-suture craniosynostosis and plagiocephaly without synostosis. Plast. Reconstr. Surg. 108, 1492–1498; discussion: 1499–1500. doi: 10.1097/00006534-200111000-00007
Patel, A., Yang, J. F., Hashim, P. W., Travieso, R., Terner, J., Mayes, L. C., et al. (2014). The impact of age at surgery on long-term neuropsychological outcomes in sagittal craniosynostosis. Plast. Reconstr. Surg. 134, 608e–617e. doi: 10.1097/PRS.0000000000000511
Peitsch, W. K., Keefer, C. H., LaBrie, R. A., and Mulliken, J. B. (2002). Incidence of cranial asymmetry in healthy newborns. Pediatrics 110:e72. doi: 10.1542/peds.110.6.e72
Renier, D., Lajeunie, E., Arnaud, E., and Marchac, D. (2000). Management of craniosynostoses. Child's Nerv. Syst. 16, 645–658. doi: 10.1007/s003810000320
Sidoti, E. J. Jr., Marsh, J. L., Marty-Grames, L., and Noetzel, M. J. (1996). Long-term studies of metopic synostosis: frequency of cognitive impairment and behavioral disturbances. Plast. Reconstr. Surg. 97, 276–281. doi: 10.1097/00006534-199602000-00002
Speltz, M. L., Collett, B. R., Stott-Miller, M., Starr, J. R., Heike, C., Wolfram-Aduan, A. M., et al. (2010). Case-control study of neurodevelopment in deformational plagiocephaly. Pediatrics 125, e537–e542. doi: 10.1542/peds.2009-0052
Keywords: early developmental delay, craniosynostosis, deformational plagiocephaly
Citation: Andrews BT and Fontana SC (2017) Correlative vs. Causative Relationship between Neonatal Cranial Head Shape Anomalies and Early Developmental Delays. Front. Neurosci. 11:708. doi: 10.3389/fnins.2017.00708
Received: 05 September 2017; Accepted: 01 December 2017;
Published: 19 December 2017.
Edited by:
Antonio Benítez-Burraco, Universidad de Sevilla, SpainReviewed by:
Mark Harold Moore, Australian Craniofacial Unit, AustraliaCopyright © 2017 Andrews and Fontana. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Brian T. Andrews, YmFuZHJld3NAa3VtYy5lZHU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.