
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol., 21 March 2025
Sec. Headache and Neurogenic Pain
Volume 16 - 2025 | https://doi.org/10.3389/fneur.2025.1547893
 Linda Al-Hassany1
Linda Al-Hassany1 Antoinette MaassenVanDenBrink1*†
Antoinette MaassenVanDenBrink1*† Tobias Kurth2† On behalf of the Lifelines Corona Research Initiative
Tobias Kurth2† On behalf of the Lifelines Corona Research InitiativeBackground: Coronavirus disease 2019 (COVID-19), caused by the SARS-CoV-2 virus, placed unprecedented pressure on public health systems due to its mortality and global panic—and later due to long COVID challenges. One of these long COVID symptoms, headache, often resembles migraine-like features. Migraine shares similarities with COVID-19 and long COVID, yet the influence of sex is understudied. Our primary objective was to study the interrelationship between COVID-19 and migraine prevalence, while considering sex differences. The secondary objective was to examine how long COVID symptoms (headache, anosmia, memory, and concentration problems) affect males and females with and without COVID-19 and migraine.
Methods: All analyses were conducted using Lifelines, a prospective cohort study in the northern Netherlands. Baseline characteristics (2006–2014), self-reported migraine diagnoses (until 2021), and questionnaires on COVID-19 and long COVID symptoms (2020–2022) were collected. Logistic regression analyses were conducted to study the association between lifetime migraine and current SARS-CoV-2 infections while adjusting for age, sex, diet, educational attainment, activity, and smoking. Descriptive and sex-stratified analyses were conducted on long COVID symptoms.
Results: A total of 150,507 individuals were included, of which 29,680 (19.7%) reported migraine and 120,827 (80.3%) not. A total of 1,867 individuals with migraine [6.3% of individuals with migraine, 44.0 years (IQR 36.1–50.3)] and 6,797 individuals without migraine [5.6% of individuals without migraine, 44.4 years (IQR 35.3–52.2)] reported to be SARS-CoV-2 infected. The majority of individuals with migraine consisted of females (77.0% of those with migraine vs. 54.0% of those without migraine). The adjusted odds of having SARS-CoV-2 infections was 6.3% higher among those with (a history of) migraine compared with individuals without migraine in the logistic regression model (OR = 1.06, 95% CI 1.01–1.12). A slightly higher OR was observed in females (OR = 1.08, 95% CI 1.02–1.15), and the association was not apparent in males (OR = 1.00, 95% CI 0.88–1.12). Secondary analyses revealed that individuals with both migraine and COVID-19, and females in particular, were the most frequently bothered by long COVID symptoms headache, anosmia, concentration, and memory problems. Individuals with none of these diseases were the least bothered.
Conclusions: Individuals with migraine, especially females, are slightly more likely to report and/or contract COVID-19. Those with both conditions report long COVID symptoms more frequently, suggesting a shared vulnerability or pathophysiology. This may indicate the need for clinical surveillance of migraine patients recovering from COVID-19.
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has put unprecedented pressure on public health systems and led to over 775 million cumulative cases and 7.1 million deaths globally (1). Great advances have been made in the diagnostics of COVID-19 (2) and the development of life-saving vaccines (3)—leading to a transition of the pandemic disease to a more manageable disease. Whereas, acute respiratory symptoms and lung failure have dominated the clinical manifestations of COVID-19 in the acute phase (4), a substantial number of individuals continue to suffer from heterogeneous prolonged symptoms or so-called “long COVID.” These symptoms range from neurological symptoms and cardiac abnormalities to chronic fatigue (5). One of these most prevalent neurological symptoms is headache, which could manifest as either a new headache or aggravation (in frequency or severity) of preexisting primary headache, including migraine (6). Interestingly, migraine-like features of especially persisting long COVID headaches have been reported in several studies (7–9). Further similarities include the incidence of long COVID headaches and the prevalence of migraine, which both are increased in females (10, 11), and a peak in diagnoses of both diseases until the age of fifty (12). In contrast to the gain in function in the trigeminal system, i.e., headache, another neurologic manifestation of long COVID is a loss of function in the olfactory system, i.e., anosmia (13), which also seems to differ between sexes and age categories (14) and to be increased in migraine patients (15). Further, neuropsychiatric symptoms, including (objectively measured) cognitive impairment and “brain fog,” have been associated with chronic post-COVID-19, especially among females (16–18). Similar symptoms have been described for migraine, even in the interictal phase (19). Notably, these similarities between long COVID (as a symptom of COVID-19) and migraine are not observed in the clinical manifestations of acute SARS-CoV-2 infections. Indeed, retrospective observations indicate that males are rather more likely to exhibit enhanced COVID-19 severity and mortality than females—probably also due to sex differences in the immune response (20, 21).
The interrelationships of migraine, COVID-19, and the long COVID symptoms of headache, anosmia, and memory or concentration problems while accounting for sex differences are understudied. Indeed, the importance of sex and gender, including hormonal influences, in migraine is increasingly being recognized, especially with regard to the prevalence and pathophysiology (22, 23). Yet, there has been a lack in the application of sex-specific methodologies in COVID-19 research, contributing to knowledge gaps on the diagnosis, including the recognition of individuals who are at risk and treatment of long-term symptoms, which have a substantial influence on the quality of life (24, 25). The overlapping clinical symptoms and the enormous socioeconomic burden of migraine, COVID-19, and long COVID-19 probed us to study the influence of sex in their association in a large prospective population-based setting. Thus, our primary objective was to study the interrelationship of COVID-19 and migraine prevalence, accounting for sex differences. Our secondary objective was to study the extent to which individuals, both male and female, with and without COVID-19 and migraine, had long COVID symptoms, i.e., headache, anosmia, and memory and concentration problems.
All analyses were performed within Lifelines, a multidisciplinary prospective population-based cohort study consisting of a total number of 167,729 persons, representing ~10% of the total population in the three northern provinces of the Netherlands. The Lifelines cohort was established in 2006 and designed to enhance our understanding of the complex interactions between genetics, lifestyle, and environment in relation to health (including aging) and (chronic) disease. No specific inclusion criteria were applied, and the risk of selection bias has been demonstrated to be low (26). Individuals were excluded from participation in case they (i) had a terminal illness (life expectancy of < 5 years), (ii) were incapacitated, e.g., due to a severe mental illness, (iii) were unable to visit their general practitioner, (iv) were unable to complete the questionnaires, or (v) had insufficient knowledge of the Dutch language. The collection of baseline characteristics took place between 2006 and 2014. Follow-up procedures included the completion of (digital) questionnaires sent approximately every 1.5–2.5 years.
The current study is based on an add-on to the ongoing observational cohort, i.e., the Lifelines COVID-19 cohort study (27). Questionnaires containing questions on COVID-19 diagnoses, symptoms, comorbidities, and mental aspects, among others, were sent to all Lifelines participants aged ≥18 years with a known email address. These questionnaires were initially sent out weekly, but they were sent out every 2 weeks from June 2020 and every month from August 2020.
The Lifelines Cohort Study, including the COVID-19 add-on study, is conducted according to the principles of the Declaration of Helsinki and approved by the Medical Ethics Committee of the University Medical Center Groningen, the Netherlands (reference numbers METc 2007/152 and METc 2019/571; approval number NL17981.042.07). The overall design and rationale of the cohort have been described in detail elsewhere (28, 29).
All individuals aged ≥18 years who signed informed consent prior to participation during the first visit were included in the current analyses. Age during inclusion was calculated and used for all analyses. Self-reported data on COVID-19 were derived from 27 consecutive measurements collected in the Lifelines COVID-19 cohort study in the form of surveys between March 2020 and March 2022. A positive COVID-19 diagnosis was based on the answers to the questions on whether participants reported that they have or had SARS-CoV-2 infections and whether the doctor had told them they have (or had) a SARS-CoV-2 infection. Vaccination status was also based on self-reporting. The long COVID symptoms of headache, anosmia, memory, and concentration problems were assessed using an ordinal five-point Likert scale to identify to what extent participants were bothered by these symptoms (1 = not at all, 2 = a little bit, 3 = somewhat, 4 = quite a lot, 5 = very much) in the past seven days. The timeframe of 7 days was changed to the past 14 days when questionnaires were administered every 2 weeks and monthly. Data on headache and anosmia symptoms were obtained from 26 questionnaires in total, while data on concentration and memory problems were obtained from the last five questionnaires only.
Migraine diagnoses were self-reported based on questionnaires sent during baseline and four follow-up questionnaires until 2021. Individuals who reported suffering from migraine during at least one questionnaire were categorized as migraine patients. Migraine diagnoses that occurred after COVID-19 were not included in the analysis. The migraine status was solely based on participants' responses in the questionnaire and was not further verified by medical professionals.
The body mass index (BMI) was calculated using the standard formula of [weight (kg)/length2 (m)]. Weight and height were measured using a stadiometer and standard weighing scale, respectively. Both weight and height were measured without shoes, and weight was measured wearing light clothing with empty pockets.
Ever use of hormones is a composite variable for women only and based on the self-reported answers to questions on whether hormonal contraception was ever used and whether they ever received hormone therapy for perimenopausal complaints. Smoking status (current, ever, or never) was also based on self-reported answers.
Total activity scores of the validated Short QUestionnaire to ASsess Health-enhancing physical activity (SQUASH) questionnaire were used to provide an indication of weekly habitual physical activity (30, 31). The activity score (total score per week) was calculated by multiplying minutes per week by a factor for intensity. The Lifelines Diet Score, a relative measure of overall diet quality, is derived from a 110-item food frequency questionnaire and is based on the intake of food groups with positive and negative health effects (32). The intake of these food groups was expressed in grams/1,000 kilocalories, with a higher score indicating a higher diet quality. Alcohol intake was self-reported and expressed as grams per day. For these lifestyle proxies, only single scores per patient were taken into account, obtained prior to their SARS-CoV-2 infection.
Ethnicity was self-reported and reported as categories (White/East and West European, White/Mediterranean or Arabic, Black/Negroid, Asian or other—mainly including participants with a multiethnic background) based on answers to the question of which of these populations participants consider themselves belonging to. No education, primary education, lower or preparatory secondary vocational education, and junior general secondary education are categorized as “low;” secondary vocational education or work-based learning pathway and senior general/pre-university secondary education are categorized as “middle;” higher vocational education and university education are categorized as “high.”
We only included participants whose data on sex, age during baseline, and migraine status were complete. No additional exclusion criteria were applied.
Baseline characteristics are displayed as means (standard deviation) for normally distributed data or medians [interquartile range, Q3–Q1] for non-normally distributed data, or as numbers (percentage) to express frequencies. The Anderson-Darling normality test was used to assess normality. Missing data on ethnicity, educational attainment, smoking status, BMI, alcohol intake, SQUASH activity score, and Lifelines diet score were imputed with 5 imputations and 10 iterations using the “mice” package in R. The missing data pattern was assumed to be missing at random.
Logistic regression analyses were conducted to study the association between lifetime migraine diagnoses and SARS-CoV-2 infections. These models were run on the combined imputed datasets. We report unadjusted and adjusted odds ratios (OR) with accompanying 95% Confidence Intervals (CI). We adjusted for age, sex, Lifelines diet score, educational attainment (as an indication of socioeconomic status), SQUASH activity score, and smoking status (ever smoking), as we considered the factors as potential confounding factors. Indeed, age, sex, and socioeconomic status have been shown to have a profound influence on the burden and prevalence of both migraine (33–35) as well as self-reported acute and persistent COVID symptoms or health outcomes (36, 37). In addition, modifiable lifestyle factors—including smoking, diet, and physical activity—have been reported to be associated with COVID susceptibility and severity (38), and with migraine attack onset (39, 40).
Exploratory analyses were conducted on long COVID symptoms (i.e., headache, anosmia, memory, and concentration problems), and descriptive statistics (relative frequencies) were applied. For each group (SARS-CoV-2 infected yes/no and migraine diagnosis yes/no), relative frequencies of the extent to which participants had these symptoms were calculated and reported. Relative frequencies were calculated by dividing the frequency of each individual score on the Likert scale by the total number of individuals per stratified group (who completed this questionnaire).
Both logistic regression analyses and exploratory analyses on long COVID symptoms were also performed after stratifying for sex (male/female).
All statistical analyses were performed using the R (version 4.2.0, Vienna, Austria), RStudio (2022.2.0.443, Boston, MA, USA), and SPSS 28.0.1.1 (SPSS Inc., Chicago, IL, USA). The graph was created using GraphPad Prism version 8.0.1 (GraphPad Software, Boston, MA, USA).
A total of 150,507 individuals were included, consisting of 29,680 (19.7%) individuals with migraine and 120,827 (80.3%) individuals without migraine. A total of 8,664 individuals reported to have been infected with COVID-19 at least once during follow-up, consisting of 1,867 individuals with migraine (6.3% of individuals with migraine and 6,797 individuals without migraine (5.6% of individuals without migraine). The majority of individuals with migraine consisted of females (77.0% of those with migraine vs. 54.0% of those without migraine). Further, individuals with migraine were more likely to use hormonal contraception and/or hormone therapy, while individuals without migraine were more likely to be ever or current smokers and consumed more alcohol (Table 1). Notably, a total of 38,379 individuals reported to have been at least once vaccinated for COVID-19, consisting of 7,813 (20.4%) individuals with migraine and 30,566 (79.6%) individuals without migraine. While migraine patients appeared to have been tested more frequently than those without migraine, differences between these two groups were limited (Figure 1).
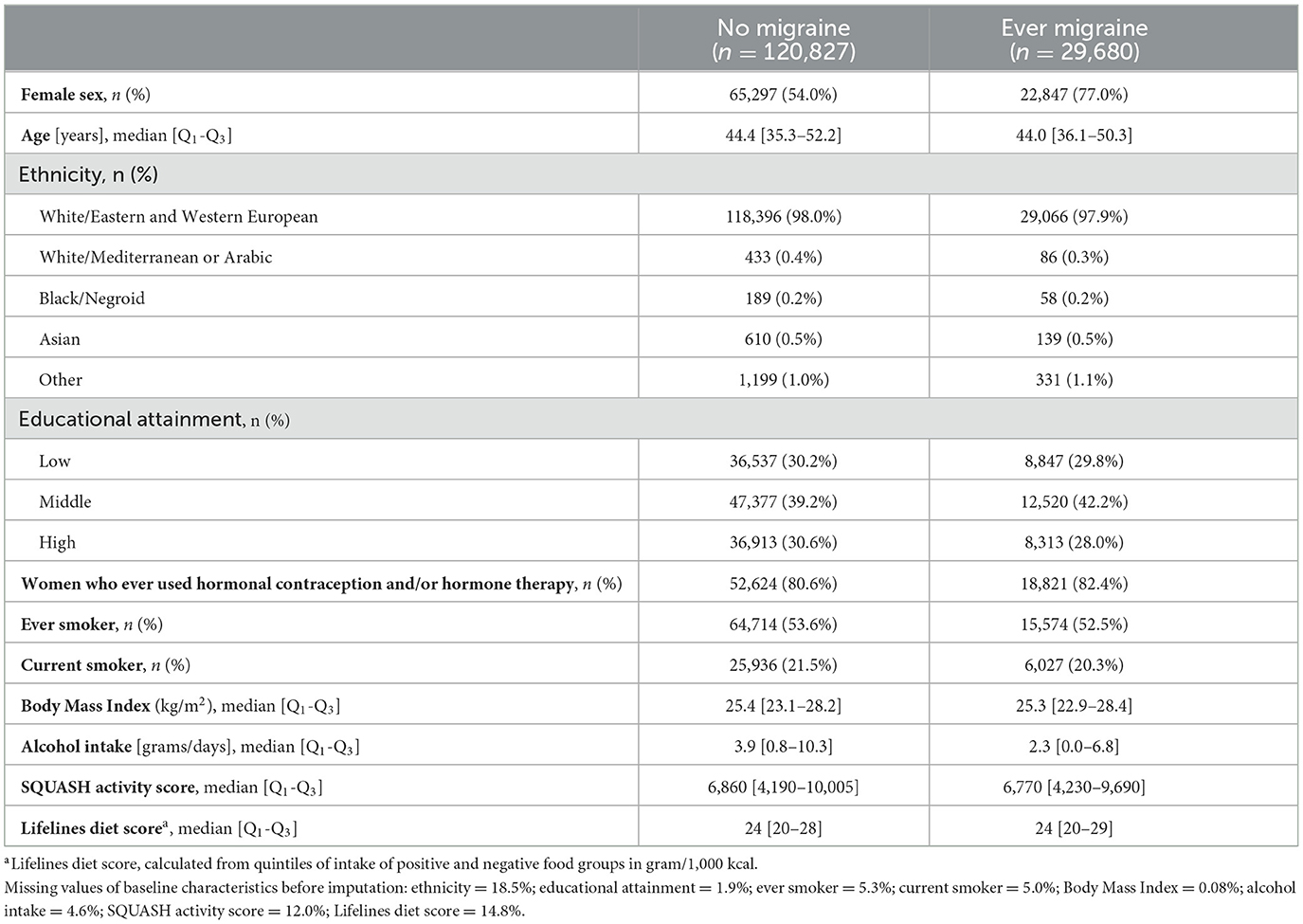
Table 1. Baseline characteristics of Lifelines participants according to self-reported lifetime migraine prevalence.
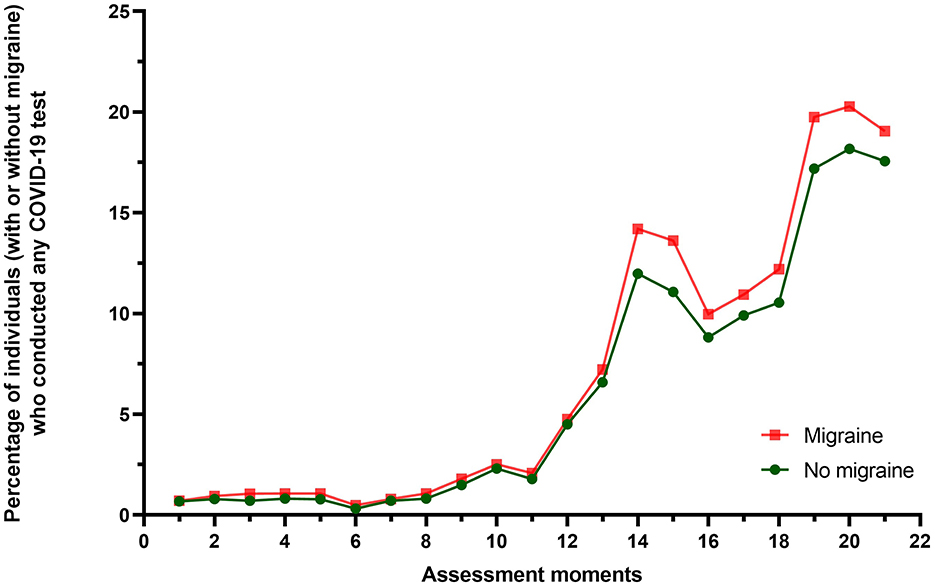
Figure 1. Graph illustrating the percentage of individuals with and without migraine who conducted a COVID-19 test, including both rapid tests and PCR tests, during the Lifelines longitudinal collection moments of COVID-19-related data. As the total number of individuals who did not conduct a COVID-19 test was unknown during the last six assessment moments, the percentages of these moments are not displayed.
The adjusted odds of the probability of having SARS-CoV-2 infections were 6.3% higher among those with (a history of) migraine compared with individuals without migraine in the logistic regression model (OR = 1.06, 95% CI 1.01–1.12; Table 2). Stratification by sex showed similar results in females (OR = 1.08, 95% 1.02–1.15) but not in males (OR = 1.00, 95% CI 0.88–1.12; Table 3).
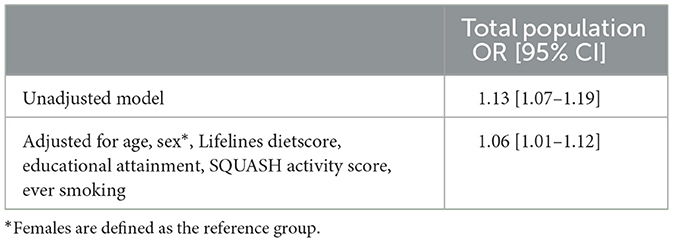
Table 2. The crude and adjusted association between ever having migraine and COVID-19 infections in the total study population.
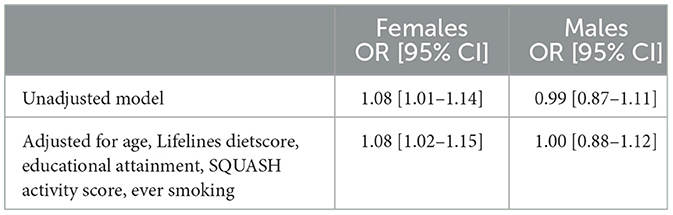
Table 3. The crude and adjusted association between ever having migraine and COVID-19 infections, stratified by sex.
Secondary analyses revealed that, in the total population, individuals with both migraine and COVID-19 were the most frequently bothered by headaches in the last 7–14 days, followed by those with only COVID-19 and no migraine (Table 4). Individuals without either migraine or COVID-19 experienced headaches the least frequently. While a similar pattern of reporting was observed in both sexes, females reported overall to be more bothered by headache than males (Supplementary material, Supplementary Tables 1a, 1b).
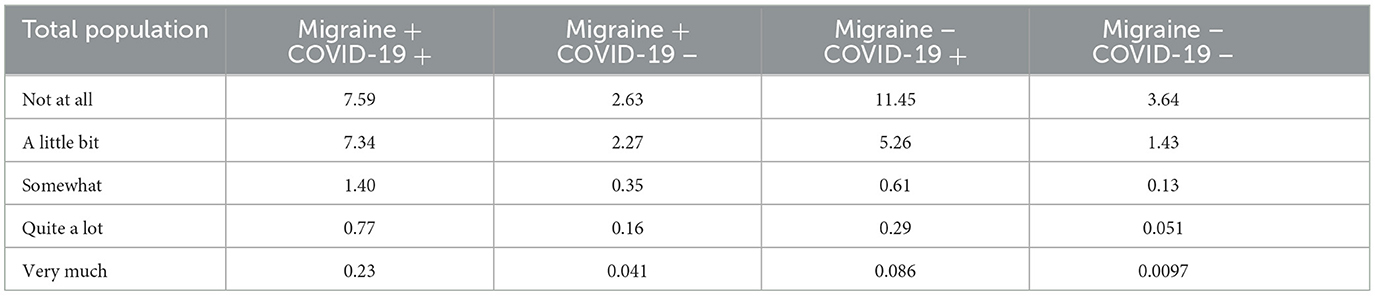
Table 4. The relative frequencies of the total population reporting headache in the last 7–14 days, stratified by migraine and COVID-19 status.
Similar results were noted for the symptom anosmia. Individuals with both migraine and COVID-19 reported the highest burden due to anosmia. They were followed by those with COVID-19 but no migraine, those with migraine but no COVID-19, and finally, those without either condition (Table 5). Yet, for anosmia, there was no discernible difference in frequency between the sexes, although females were slightly more affected by this symptom (Supplementary material, Supplementary Tables 2a, 2b).
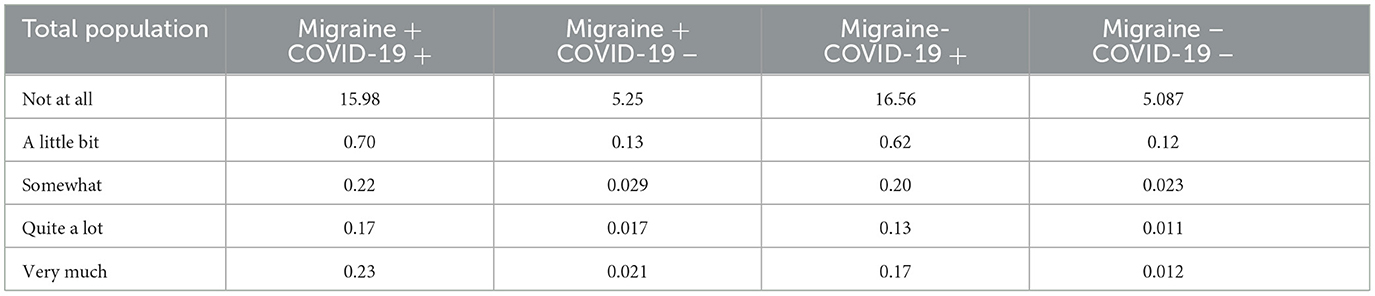
Table 5. The relative frequencies of the total population reporting anosmia (loss of sense of smell or taste) in the last 7–14 days, stratified by migraine and COVID-19 status.
The abovementioned results for memory and concentration problems were also observed across the four groups. However, being bothered by concentration problems seemed to be reported more frequently than memory problems (Tables 6, 7). Both symptoms were also reported more frequently by females across all groups (Supplementary material, Supplementary Tables 3a, 3b and Supplementary material, Supplementary Tables 4a, 4b).
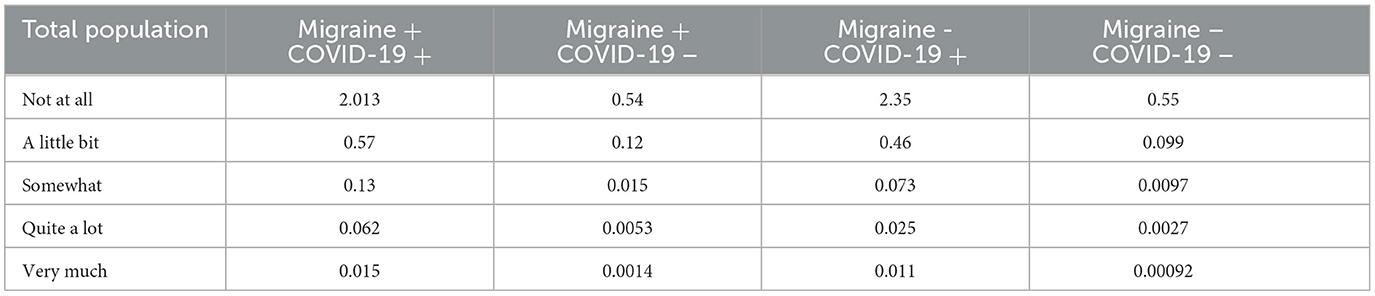
Table 6. The relative frequencies of the total population reporting memory problems in the last 14 days, stratified by migraine and COVID-19 status.
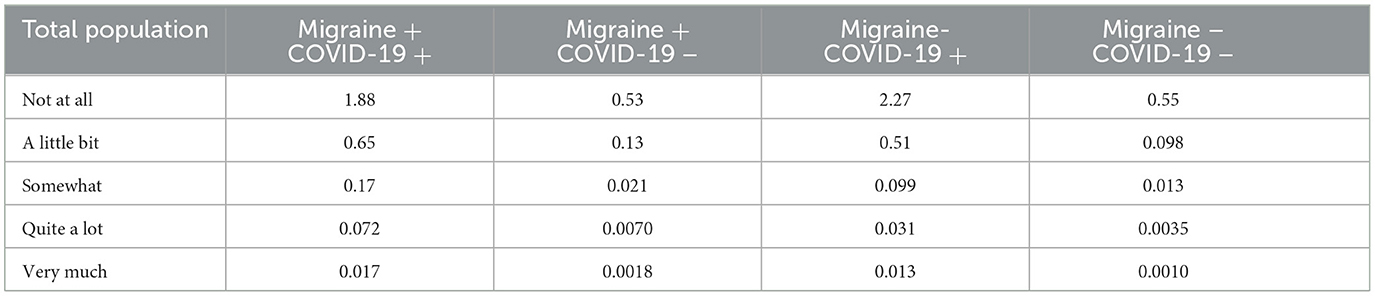
Table 7. The relative frequencies of the total population reporting concentration problems in the last 14 days, stratified by migraine and COVID-19 status.
In the population-based Dutch Lifelines cohort, we studied the interrelation between migraine and COVID-19, as well as long COVID symptoms. We observed a slightly higher prevalence of SARS-CoV-2 infections among individuals with migraine, particularly among females. Furthermore, individuals with migraine who had been infected with SARS-CoV-2—also females in particular—more frequently reported being bothered by long COVID symptoms, including headache, anosmia, and memory and concentration problems.
There are several possible explanations for the relationship between migraine patients, SARS-CoV-2 infections, and—in particular—long COVID symptoms. First, it seems likely that infections in people with migraine are more often symptomatic. This could explain why they are slightly more likely to have a positive test result, considering that they may seek testing earlier due to the more pronounced symptoms. Second, healthcare-seeking behaviors and self-report bias might have led to the increased prevalence of SARS-CoV-2 infections among migraine patients. Indeed, women with migraine, individuals with higher healthcare utilization, and those severely affected by migraine or COVID-19 are more likely to respond to surveys. Third, migraine patients might be more susceptible to coronavirus infections. Previous research suggests that increased social interactions are unlikely to be the reason for higher SARS-CoV-2 infection rates among migraine patients, as migraine patients seem to have reported higher levels of social loneliness during the lockdown (41).
Alternatively, several underlying biological mechanisms might be involved in the overlap between COVID-19 and migraine, although definitive pathophysiological mechanisms cannot be concluded from these results. One mechanism is linked to hyperresponses of mast cells and the activation of cytokine storm, including interleukin-6 and other pro-(neuro-)inflammatory markers, leading to neuroinflammatory processes, microglial activation, and peripheral sensitization (42–46). Another mechanism is linked to the overexpression of the angiotensin-converting enzyme 2, being an important target for SARS-CoV-2 entry (47–49). The trigeminal nerve has also been proposed as a site for entry for the virus into the central nervous system, potentially leading to headache symptoms and anosmia (7, 50). Recently, persistent headaches among those with both COVID-19 and migraine have been hypothesized to be due to changes in retinal nerve fiber layer thickness (51). Endothelial abnormality, being a vascular marker, has been hypothesized to underlie the pathophysiology of long COVID and is involved in migraine as well (52, 53). Furthermore, COVID-19 has been linked to hypoperfusion and changes across multiple brain networks (54)—including regions associated with cognition [e.g., dysfunction of the cingulate cortex; (55)]—while migraine itself has also been associated with cognitive impairment (56). In addition, both COVID and migraine have been associated with a decrease in serotonin levels, serving as another possible explanation for the higher frequency of reported memory and concentration problems in particular (57, 58). Furthermore, patients with pre-existing primary headaches (i.e., migraine) might be more prone to developing other secondary headaches [i.e., post-COVID headaches; (59)]. It should be noted, however, that these mechanisms become relevant only after a person has already been infected with COVID-19. Thus, they do not necessarily account for any increased susceptibility to the virus in migraine patients.
Current literature on the association between migraine and COVID-19 (symptoms) remains conflicting. Previous results from the Women's Health Study demonstrated no association between COVID-19 and migraine among older women with a history of migraine (60). However, some authors observed an association with long COVID symptoms, including a chronic headache transformation among migraine patients (15) and headaches with migraine-like features (7). We also observed that individuals with both migraine and COVID-19 were the most frequently bothered by headaches, which might be explained by the induction of certain proinflammatory cytokines and interleukins of the innate immune system (61), the aforementioned activation of the trigeminovascular system as well as structural and functional brain changes (6). However, others showed that individuals with a history of migraine who recovered from COVID-19 are more likely to experience fatigue rather than headaches as a post-COVID symptom (48). Uncertainties regarding the temporality of the onset of migraine in relation to COVID-19 and long COVID symptoms, as well as the descriptive nature of most studies, including ours, might explain these discrepancies (60). Further, the lack of an intersectional approach in some studies, disregarding differences in COVID-19 outcomes across various demographic groups and different identities, might have previously led to an underestimation of the impact of these diseases (62). Nevertheless, the clinical relevance of the observed slightly higher prevalence of SARS-CoV-2 infections among female individuals with migraine could be debated.
Despite the slightly lower number of vaccinated individuals with migraine and the marginal differences in COVID-19 testing rates, which were higher among migraine patients, we cannot exclude the possibility of a higher nocebo effect in individuals with migraine (63). Although vaccinations have been described to prevent long COVID symptoms (64), this nocebo effect might explain the increase in bothersome long COVID symptoms, including the presence of headaches (63). While the nocebo effect has, in general, been described to be larger among females (65), and might even be exaggerated by the controversy surrounding vaccination debates, we cannot exclude the possibility that this also explains the observed sex differences in long COVID symptoms.
Several limitations must be considered when interpreting our findings. First, we cannot exclude that the presence of sex differences is due to a lower migraine prevalence and power, but also less pronounced migraine symptomatology [including symptoms accompanying migraine headaches; (66)], among males. In addition, whether the observed sex differences can be attributed to biological factors or to behavioral attributes (i.e., gender) remains to be demonstrated (22). Second, migraine was based on self-reported questionnaires and not based on the International Classification of Headache Disorders, nor were diagnoses verified by medical professionals (67). This could have led to migraine misdiagnoses at baseline, while new daily persistent headache could have also been confused with long COVID headache due to their similar clinical characteristics (6). Further, migraine exacerbations during COVID-19 infections could be confused with secondary headaches associated with viral infection. Third, we did not differentiate between COVID-19 subtypes or mutated viruses, which could have different influences on the occurrence, severity, and duration of long COVID symptoms. Fourth, the definition of long COVID might also not have been rigorously met, as we did not clearly distinguish between “ongoing symptomatic COVID-19” (4 to 12 weeks post-infection) and “post-COVID-19 syndrome” (symptoms persisting beyond 12 weeks; 5). These phases exhibit different patterns concerning age, sex, and phenotype, which could also influence long COVID symptoms, including headache characteristics. Fifth, given that our results rely on questionnaire responses, the possibility of selection bias cannot be excluded. Asymptomatic COVID-19-infected individuals, but also more severely ill patients and those admitted to the hospital, are likely to be underrepresented in our study. We hypothesize that mainly symptomatic individuals conducted a test, although it is not unlikely that asymptomatic individuals also did—for example, if they were warned or contacted by a COVID-19-positive individual. As it is likely that the latter group is larger, we cannot rule out the possibility of information bias herein. Moreover, the correct conduct of testing procedures and accuracy of positive COVID-19 test results could not be verified due to this form of data collection. Lastly, vaccines against SARS-CoV-2 have been associated with a 2-fold increased risk of developing headaches within a week of injection, potentially due to a secondary systemic immunological reaction. However, we did not distinguish between vaccinated and non-vaccinated individuals, nor did we consider vaccination-related changes in the migraine course (68).
Notwithstanding these limitations, the large cohort size and follow-up questionnaires provided comprehensive data on migraine and several COVID-19-related outcomes while considering lifestyle factors. A key strength is our focus on sex differences, which addresses a significant gap in the existing literature and contributes to a better understanding of how sex may influence the interrelation between migraine and COVID-19-related symptoms. Indeed, both migraine and long COVID symptoms pose a major physical and mental burden on patients and healthcare services (11, 69). Future research is warranted to understand underlying mechanisms while acknowledging the potential vulnerability of migraine patients in developing such long COVID symptoms, especially when considering social and environmental factors as well as comorbidities, such as psychiatric diseases, including anxiety, post-traumatic stress disorder, and depression (70, 71). In addition, further research on SARS-CoV-2 infections is warranted in migraine patients with other chronic pain disorders and (systemic) autoimmune disorders, especially considering (i) the potential risk of SARS-CoV-2 infections to develop (incident) autoimmune diseases (72), (ii) the impact of SARS-CoV-2 infections in individuals with pre-existing or newly developed chronic pain (73) and (iii) the association between migraine, autoimmune diseases (74) and other chronic pain conditions (71). It is essential that such studies address the diagnostic challenges encountered in this study—particularly those related to self-reported migraine and COVID-19 diagnoses. Considering the fact that the Lifelines cohort consists of a relatively healthy and young population, future studies are also pivotal to extrapolate our findings to other settings.
Individuals with migraine, females in particular, are slightly more likely to be infected by COVID-19. Additionally, individuals with both migraine and COVID-19 report being bothered by long COVID symptoms, including headache, anosmia, and memory and concentration problems more frequently, compared to individuals with one or none of these disease(s). Our results might suggest a shared vulnerability, susceptibility, or pathophysiology between COVID-19 and migraine, indicating the potential need for clinical surveillance of migraine patients upon recovery from SARS-CoV-2 infection. Further sex- and gender-specific research in other populations is highly recommended.
The data analyzed in this study was obtained from Lifelines. Researchers can apply to use the Lifelines data used in this study. More information about how to request Lifelines data and the conditions of use can be found on their website https://www.lifelines-biobank.com/.
The Lifelines Cohort Study, including the COVID-19 add-on study, is conducted according to the principles of the Declaration of Helsinki and approved by the Medical Ethics Committee of the University Medical Center Groningen, the Netherlands (reference numbers METc 2007/152 and METc 2019/571; approval number NL17981.042.07). Written informed consent to participate in this study was provided by the participants.
LA-H: Conceptualization, Formal analysis, Funding acquisition, Methodology, Visualization, Writing – original draft, Writing – review & editing, Investigation. AMvdB: Conceptualization, Funding acquisition, Project administration, Resources, Supervision, Writing – review & editing. TK: Conceptualization, Investigation, Methodology, Supervision, Writing – review & editing.
H. Marike Boezen1, Jochen O. Mierau2,3,4, H. Lude Franke5, Jackie Dekens5,6, Patrick Deelen5, Pauline Lanting5, Judith M. Vonk1, Ilja Nolte1, Anil P.S. Ori5,7, Annique Claringbould5, Floranne Boulogne5, Marjolein X.L. Dijkema5, Henry H. Wiersma5, Robert Warmerdam5, Soesma A. Jankipersadsing5, Irene van Blokland5,8, Geertruida H. de Bock1, Judith GM Rosmalen7,9 and Cisca Wijmenga5
1Department of Epidemiology, University of Groningen, University Medical Center Groningen, Groningen, Netherlands
2Department of Economics, Econometrics and Finance, Faculty of Economics and Business, University of Groningen, Groningen, Netherlands
3Lifelines Cohort Study and Biobank, Groningen, Netherlands
4Team Strategy and External Relations, University of Groningen, University Medical Center Groningen, Netherlands
5Department of Genetics, University of Groningen, University Medical Center Groningen, Groningen, Netherlands
6Center of Development and Innovation, University of Groningen, University Medical Center Groningen, Groningen, Netherlands
7Department of Psychiatry, University of Groningen, University Medical Center Groningen, Groningen, Netherlands
8Department of Cardiology, University of Groningen, University Medical Center Groningen, Groningen, Netherlands
9Department of Internal Medicine, University of Groningen, University Medical Center Groningen, Groningen, Netherlands
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the Dutch Research Council (ZonMw/NWO, Vici Grant (09150181910040) and the SERIOUS-study (555003018)), as well as the Academy Van Leersum grant of the Academy Medical Sciences Fund, Royal Netherlands Academy of Arts and Sciences and a Research Grant from the International Headache Society. The Lifelines initiative has been made possible by a subsidy from the Dutch Ministry of Health, Welfare and Sport, the Dutch Ministry of Economic Affairs, the University Medical Center Groningen (UMCG), Groningen University, and the Provinces in the North of the Netherlands (Drenthe, Friesland, Groningen).
AMvdB received research grants and/or consultation fees from AbbVie, Amgen/Novartis, Eli Lilly, Lundbeck, Manistee, Pfizer, Satsuma, Teva, and Tonix. TK reports receiving research grants from the Gemeinsamer Bundesausschuss (G-BA Federal Joint Committee, Germany). He has also received personal compensation from Eli Lilly and Company, Novartis, the BMJ, and Frontiers.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declare that no Gen AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2025.1547893/full#supplementary-material
BMI, Body Mass Index; CI, Confidence Interval; COVID-19, Coronavirus disease 2019; OR, Odds Ratio; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; SQUASH, Short QUestionnaire to ASsess Health-enhancing physical activity.
1. WHO COVID-19 Dashboard. Geneva: World Health Organization (2020). Available online at: https://covid19.who.int/ (accessed July 1, 2024).
2. Peeling RW, Heymann DL, Teo YY, Garcia PJ. Diagnostics for COVID-19: moving from pandemic response to control. Lancet. (2022) 399:757. doi: 10.1016/S0140-6736(21)02346-1
3. Zhang Z, Shen Q, Chang H. Vaccines for COVID-19: a systematic review of immunogenicity, current development, and future prospects. Front Immunol. (2022) 13:843928. doi: 10.3389/fimmu.2022.843928
4. Aslan A, Aslan C, Zolbanin NM, Jafari R. Acute respiratory distress syndrome in COVID-19: possible mechanisms and therapeutic management. Pneumonia. (2021) 13:14. doi: 10.1186/s41479-021-00092-9
5. Castanares-Zapatero D, Chalon P, Kohn L, Dauvrin M, Detollenaere J, Maertens de Noordhout C, et al. Pathophysiology and mechanism of long COVID: a comprehensive review. Ann Med. (2022) 54:1473–473. doi: 10.1080/07853890.2022.2076901
6. Tana C, Bentivegna E, Cho SJ, Harriott AM, García-Azorín D, Labastida-Ramirez A, et al. Long COVID headache. J Headache Pain. (2022) 23:93. doi: 10.1186/s10194-022-01450-8
7. Caronna E, Ballvé A, Llauradó A, Gallardo VJ, Ariton DM, Lallana S, et al. Headache: a striking prodromal and persistent symptom, predictive of COVID-19 clinical evolution. Cephalalgia. (2020) 40:1410–410. doi: 10.1177/0333102420965157
8. Caronna E, Alpuente A, Torres-Ferrus M, Pozo-Rosich P. Toward a better understanding of persistent headache after mild COVID-19: three migraine-like yet distinct scenarios. Headache. (2021) 61:1277–277. doi: 10.1111/head.14197
9. Garcia-Azorin D, Layos-Romero A, Porta-Etessam J, Membrilla JA, Caronna E, Gonzalez-Martinez A, et al. Post-COVID-19 persistent headache: a multicentric 9-months follow-up study of 905 patients. Cephalalgia. (2022) 42:804. doi: 10.1177/03331024211068074
10. Sudre CH, Murray B, Varsavsky T, Graham MS, Penfold RS, Bowyer RC, et al. Attributes and predictors of long COVID. Nat Med. (2021) 27:626. doi: 10.1038/s41591-021-01292-y
11. Stovner LJ, Nichols E, Steiner TJ, Abd-Allah F, Abdelalim A, Al-Raddadi RM, et al. Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol. (2018) 17:954. doi: 10.1016/S1474-4422(18)30322-3
12. FAIR Health. Patients Diagnosed with Post-COVID Conditions: An Analysis of Private Healthcare Claims Using the Official ICD-10 Diagnostic Code. New York, NY: FAIR Health (2022).
13. Messlinger K, Neuhuber W, May A. Activation of the trigeminal system as a likely target of SARS-CoV-2 may contribute to anosmia in COVID-19. Cephalalgia. (2022) 42:176. doi: 10.1177/03331024211036665
14. Najafloo R, Majidi J, Asghari A, Aleemardani M, Kamrava SK, Simorgh S, et al. Mechanism of anosmia caused by symptoms of COVID-19 and emerging treatments. ACS Chem Neurosci. (2021) 12:3795–795. doi: 10.1021/acschemneuro.1c00477
15. Magdy R, Elmazny A, Soliman SH, Elsebaie EH, Ali SH, Abdel Fattah AM, et al. Post-COVID-19 neuropsychiatric manifestations among COVID-19 survivors suffering from migraine: a cases among tah AMh J Headache Pain. (2022) 23:1. doi: 10.1186/s10194-022-01468-y
16. Asadi-Pooya AA, Akbari A, Emami A, Lotfi M, Rostamihosseinkhani M, Nemati H, et al. Long COVID syndrome-associated brain fog. J Med Virol. (2022) 94:979. doi: 10.1002/jmv.27404
17. Kubota T, Kuroda N, Sone D. Neuropsychiatric aspects of long COVID: a comprehensive review. Psychiatry Clin Neurosci. (2023) 77:84. doi: 10.1111/pcn.13508
18. Hampshire A, Azor A, Atchison C, Trender W, Hellyer PJ, Giunchiglia V, et al. Cognition and memory after COVID-19 in a large community sample. N Engl J Med. (2024) 390:806. doi: 10.1056/NEJMoa2311330
19. Vuralli D, Ayata C, Bolay H. Cognitive dysfunction and migraine. J Headache Pain. (2018) 19:109. doi: 10.1186/s10194-018-0933-4
20. Qi S, Ngwa C, Morales Scheihing DA, Al Mamun A, Ahnstedt HW, Finger CE, et al. Sex differences in the immune response to acute COVID-19 respiratory tract infection. Biol Sex Differ. (2021) 12:66. doi: 10.1186/s13293-021-00410-2
21. Montaño Mendoza VM, Mendez Cortina YA, Rodronse tPerea AL, Fernandez GJ, Rugeles MT, Velilla Hernandez PA, et al. Biological sex and age-related differences shape the antiviral response to SARS-CoV-2 infection. Heliyon. (2023) 9:e13045. doi: 10.1016/j.heliyon.2023.e13045
22. Al-Hassany L, Haas J, Piccininni M, Kurth T, Maassen Van Den Brink A, Rohmann JL. Giving researchers a headache—sex and gender differences in migraine. Front Neurol. (2020) 11:549038. doi: 10.3389/fneur.2020.549038
23. Al-Hassany L, Verdonk P, VanDenBrink AM. Studying sex and gender in neurological disease. Lancet Neurol. (2023) 22:32. doi: 10.1016/S1474-4422(22)00493-8
24. Brady E, Nielsen MW, Andersen JP, Oertelt-Prigione S. Lack of consideration of sex and gender in COVID-19 clinical studies. Nat Commun. (2021) 12:4015. doi: 10.1038/s41467-021-24265-8
25. Stewart S, Newson L, Briggs TA, Grammatopoulos D, Young L, Gill P. Long COVID risk—a signal to address sex hormones and women's health. Lancet Reg Health Eur. (2021) 11:100242. doi: 10.1016/j.lanepe.2021.100242
26. Klijs B, Scholtens S, Mandemakers JJ, Snieder H, Stolk RP, Smidt N. Representativeness of the lifelines cohort study. PLoS ONE. (2015) 10:e0137203. doi: 10.1371/journal.pone.0137203
27. Mc Intyre K, Lanting P, Deelen P, Wiersma HH, Vonk JM, Ori APS, et al. Lifelines COVID-19 cohort: investigating COVID-19 infection and its health and societal impacts in a Dutch population-based cohort. BMJ Open. (2021) 11:e044474. doi: 10.1136/bmjopen-2020-044474
28. Scholtens S, Smidt N, Swertz MA, Bakker SJL, Dotinga A, Vonk JM, et al. Cohort profile: LifeLines, a three-generation cohort study and biobank. Int J Epidemiol. (2015) 44:1172–172. doi: 10.1093/ije/dyu229
29. Sijtsma A, Rienks J, van der Harst P, Navis G, Rosmalen JGM, Dotinga A. Cohort profile update: lifelines, a three-generation cohort study and biobank. Int J Epidemiol. (2022) 51:e29551:2. doi: 10.1093/ije/dyab257
30. Wendel-Vos GCW, Schuit AJ, Saris WHM, Kromhout D. Reproducibility and relative validity of the short questionnaire to assess health-enhancing physical activity. J Clin Epidemiol. (2003) 56:1163–163. doi: 10.1016/S0895-4356(03)00220-8
31. Byambasukh O. Physical Activity and Cardiometabolic Health: Focus on Domain-Specific Associations of Physical Activity Over the Life Course. University of Groningen Press (2020). Available online at: https://research.rug.nl/en/publications/physical-activity-and-cardiometabolic-health-focus-on-domain-spec (accessed January 14, 2023).
32. Vinke PC, Corpeleijn E, Dekker LH, Jacobs DR Jr, Navis G, Kromhout D. Development of the food-based lifelines diet score (LLDS) and its application in 129,369 lifelines participants. Eur J Clin Nutr. (2018) 72:1111–111. doi: 10.1038/s41430-018-0205-z
33. Vetvik KG, MacGregor EA. Sex differences in the epidemiology, clinical features, and pathophysiology of migraine. Lancet Neurol. (2017) 16:1234. doi: 10.1016/S1474-4422(16)30293-9
34. Fila M, Pawlowska E, Szczepanska J, Blasiak J. Different aspects of aging in migraine. Aging Dis. (2023) 14:2028–50. doi: 10.14336/AD.2023.0313
35. Stewart WF, Roy J, Lipton RB. Migraine prevalence, socioeconomic status, and social causation. Neurology. (2013) 81:948. doi: 10.1212/WNL.0b013e3182a43b32
36. Vasilevskaya A, Mushtaque A, Tsang MY, Alwazan B, Herridge M, Cheung AM, et al. Sex and age affect acute and persisting COVID-19 illness. Sci Rep. (2023) 13:6029. doi: 10.1038/s41598-023-33150-x
37. Shabnam S, Razieh C, Dambha-Miller H, Yates T, Gillies C, Chudasama YV, et al. Socioeconomic inequalities of Long COVID: a retrospective population-based cohort study in the United Kingdom. J R Soc Med. (2023) 116:263. doi: 10.1177/01410768231168377
38. Wang Y, Su B, Alcalde-Herraiz M, Barclay NL, Tian Y, Li C, et al. Modifiable lifestyle factors and the risk of post-COVID-19 multisystem sequelae, hospitalization, and death. Nat Commun. (2024) 15:6363. doi: 10.1038/s41467-024-50495-7
39. Seng EK, Martin PR, Houle TT. Lifestyle factors and migraine. Lancet Neurol. (2022) 21:911. doi: 10.1016/S1474-4422(22)00211-3
40. Weinberger AH, Seng EK. The relationship of tobacco use and migraine: a narrative review. Curr Pain Headache Rep. (2023) 27:39. doi: 10.1007/s11916-023-01103-8
41. Cerami C, Crespi C, Bottiroli S, Santi GC, Sances G, Allena M, et al. High perceived isolation and reduced social support affect headache impact levels in migraine after the COVID-19 outbreak: a cross sectional survey on chronic and episodic patients. Cephalalgia. (2021) 41:1437–437. doi: 10.1177/03331024211027568
42. Ruhnau J, Blücher M, Bahlmann S, Zieme A, Vogelgesang A, Steinmetz A, et al. Occurrence of new or more severe headaches following COVID-19 is associated with markers of microglial activation and peripheral sensitization: results from a prospective cohort study. J Headache Pain. (2024) 25:101. doi: 10.1186/s10194-024-01810-6
43. Wang X, Tang G, Liu Y, Zhang L, Chen B, Han Y, et al. The role of IL-6 in coronavirus, especially in COVID-19. Front Pharmacol. (2022) 13:1033674. doi: 10.3389/fphar.2022.1033674
44. Sarchielli P, Alberti A, Baldi A, Coppola F, Rossi C, Pierguidi L, et al. Proinflammatory cytokines, adhesion molecules, and lymphocyte integrin expression in the internal jugular blood of migraine patients without aura assessed ictally. Headache. (2006) 46:200. doi: 10.1111/j.1526-4610.2006.00337.x
45. Conti P, D'Ovidio C, Conti C, Gallenga CE, Lauritano D, Caraffa A, et al. Progression in migraine: role of mast cells and pro-inflammatory and anti-inflammatory cytokines. Eur J Pharmacol. (2019) 844:87–94. doi: 10.1016/j.ejphar.2018.12.004
46. Bolay H, Karadas Ö, Oztürk B, Sonkaya R, Tasdelen B, Bulut TDS, et al. HMGB1, NLRP3, IL-6 and ACE2 levels are elevated in COVID-19 with headache: a window to the infection-related headache mechanism. J Headache Pain. (2021) 22:94. doi: 10.1186/s10194-021-01306-7
47. Baig AM, Khaleeq A, Ali U, Syeda H. Evidence of the COVID-19 Virus targeting the CNS: tissue distribution, host–virus interaction, and proposed neurotropic mechanisms. ACS Chem Neurosci. (2020) 11:995–8. doi: 10.1021/acschemneuro.0c00122
48. Fernández-de-Las-Peñas C, Gómez-Mayordomo V, García-Azorín D, Palacios-Ceña D, Florencio LL, Guerrero AL, et al. Previous history of migraine is associated with fatigue, but not headache, as long-term post-COVID symptom after severe acute respiratory SARS-CoV-2 infection: a case-control study. Front Hum Neurosci. (2021) 15:678472. doi: 10.3389/fnhum.2021.678472
49. Kara I, Ozkok E, Aydin M, Orhan N, Cetinkaya Y, Gencer M, et al. Combined effects of ACE and MMP-3 polymorphisms on migraine development. Cephalalgia. (2007) 27:235. doi: 10.1111/j.1468-2982.2006.01269.x
50. Bolay H, Özge A, Uludüz D, Baykan B. Are migraine patients at increased risk for symptomatic coronavirus disease 2019 due to shared comorbidities? Headache. (2020) 60:2508–508. doi: 10.1111/head.13998
51. Gel MS, Kanat A, Seker D, Koc H, Daltaban IS, Findik H, et al. Changes in retinal nerve fiber layer thickness may be the cause of post-COVID-19 headaches. Neurol Res. (2024) 46:634. doi: 10.1080/01616412.2024.2340875
52. Paolucci M, Altamura C, Vernieri F. The role of endothelial dysfunction in the pathophysiology and cerebrovascular effects of migraine: a narrative review. J Clin Neurol. (2021) 17:164. doi: 10.3988/jcn.2021.17.2.164
53. Davis HE, McCorkell L, Vogel JM, Topol EJ. Long COVID: major findings, mechanisms and recommendations. Nat Rev Microbiol. (2023) 21:133. doi: 10.1038/s41579-022-00846-2
54. Ajčević M, Iscra K, Furlanis G, Michelutti M, Miladinović A, Buoite Stella A, et al. Cerebral hypoperfusion in post-COVID-19 cognitively impaired subjects revealed by arterial spin labeling MRI. Sci Rep. (2023) 13:5808. doi: 10.1038/s41598-023-32275-3
55. Hugon J, Msika EF, Queneau M, Farid K, Paquet C. Long COVID: cognitive complaints (brain fog) and dysfunction of the cingulate cortex. J Neurol. (2022) 269:44. doi: 10.1007/s00415-021-10655-x
56. Gu L, Wang Y, Shu H. Association between migraine and cognitive impairment. J Headache Pain. (2022) 23:88. doi: 10.1186/s10194-022-01462-4
57. Aggarwal M, Puri V, Puri S. Serotonin and CGRP in migraine. Ann Neurosci. (2012) 19:88. doi: 10.5214/ans.0972.7531.12190210
58. Wong AC, Devason AS, Umana IC, Cox TO, Dohnalová L, Litichevskiy L, et al. Serotonin reduction in post-acute sequelae of viral infection. Cell. (2023) 186:4851–67.e20.
59. Schankin CJ, Straube A. Secondary headaches: secondary or still primary? J Headache Pain. (2012) 13:263. doi: 10.1007/s10194-012-0443-8
60. Rist PM, Buring JE, Manson JE, Sesso HD, Kurth T. History of migraine and risk of COVID-19: a cohort study. Am J Med. (2023) 136:1094–094. doi: 10.1016/j.amjmed.2023.07.021
61. Straburzyński M, Kuca-Warnawin E, Waliszewska-Prosół M. COVID-19-related headache and innate immune response—a narrative review. Neurol Neurochir Pol. (2023) 57:43. doi: 10.5603/PJNNS.a2022.0049
62. Cohen J, van der Meulen Rodgers Y. An intersectional analysis of long COVID prevalence. Int J Equity Health. (2023) 22:261. doi: 10.1186/s12939-023-02072-5
63. Melgarejo L, Caronna E, Rosell-Mirmi J, Elosua-Bay-B I, Alpuente A, Torres-Ferrus M, et al. Migraine worsening after COVID-19 and COVID-19 vaccination: are we facing a nocebo effect? Eur J Neurol. (2023) 30:3877–877. doi: 10.1111/ene.16058
64. Trinh NT, Jödicke AM, Català M, Mercadé-Besora N, Hayati S, Lupattelli A, et al. Effectiveness of COVID-19 vaccines to prevent long COVID: data from Norway. Lancet Respir Med. (2024) 12:e33312. doi: 10.1016/S2213-2600(24)00082-1
65. Vambheim SM, Flaten MA. A systematic review of sex differences in the placebo and the nocebo effect. J Pain Res. (2017) 10:1831–831doi: 10.2147/JPR.S134745
66. Allais G, Chiarle G, Sinigaglia S, Airola G, Schiapparelli P, Benedetto C. Gender-related differences in migraine. Neurol Sci. (2020) 41:429. doi: 10.1007/s10072-020-04643-8
67. Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd edition. Cephalalgia. (2018) 38:1–211. doi: 10.1177/0333102417738202
68. Castaldo M, Waliszewska-Prosół M, Koutsokera M, Robotti M, Straburzyński M, Apostolakopoulou L, et al. Headache onset after vaccination against SARS-CoV-2: a systematic literature review and meta-analysis. J Headache Pain. (2022) 23:41. doi: 10.1186/s10194-022-01400-4
69. Carlile O, Briggs A, Henderson AD, Butler-Cole BFC, Tazare J, Tomlinson LA, et al. Impact of long COVID on health-related quality-of-life: an OpenSAFELY population cohort study using patient-reported outcome measures (OpenPROMPT). Lancet Reg Health Eur. (2024) 40:100908. doi: 10.1101/2023.12.06.23299601
70. Mazurek J, Cieślik B, Szary P, Rutkowski S, Szczegielniak J, Szczepańska-Gieracha J, et al. Association of acute headache of COVID-19 and anxiety/depression symptoms in adults undergoing post-COVID-19 rehabilitation. J Clin Med Res. (2022) 11:5002. doi: 10.3390/jcm11175002
71. Henningsen P, Hausteiner-Wiehle C, Häuser W. Migraine in the context of chronic primary pain, chronic overlapping pain disorders, and functional somatic disorders: A narrative review. Headache. (2022) 62:1272–80. doi: 10.1111/head.14419
72. Peng K, Li X, Yang D, Chan SCW, Zhou J, Wan EYF, et al. Risk of autoimmune diseases following COVID-19 and the potential protective effect from vaccination: a population-based cohort study. EClinicalMedicine. (2023) 63:102154. doi: 10.1016/j.eclinm.2023.102154
73. Lavin A, LeBlanc F, El Helou A. The impact of COVID-19 on chronic pain. Front Pain Res. (2023) 4:1234099. doi: 10.3389/fpain.2023.1234099
Keywords: migraine, COVID-19, long COVID, headache, anosmia, memory, concentration, sex differences
Citation: Al-Hassany L, MaassenVanDenBrink A and Kurth T (2025) Sex-related differences in the association between migraine, COVID-19, and long COVID: a population-based cohort. Front. Neurol. 16:1547893. doi: 10.3389/fneur.2025.1547893
Received: 18 December 2024; Accepted: 07 February 2025;
Published: 21 March 2025.
Edited by:
Vincenzo Guidetti, Sapienza University of Rome, ItalyReviewed by:
Marta Waliszewska-Prosół, Wroclaw Medical University, PolandCopyright © 2025 Al-Hassany, MaassenVanDenBrink and Kurth. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Antoinette MaassenVanDenBrink, YS52YW5oYXJlbi1tYWFzc2VudmFuZGVuYnJpbmtAZXJhc211c21jLm5s
†These authors have contributed equally to this work and share senior authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.