- First People’s Hospital of Changshu City, Changshu, Jiangsu, China
Background: Moyamoya disease increases the risk of strokes by impairing cerebral circulation, significantly affecting patients’ quality of life. Despite the profound implications of this condition, there is a limited body of research exploring the factors that contribute to strokes in patients with Moyamoya disease. This study aims to evaluate the predictive value of the triglyceride-glucose index (TyG index) in forecasting stroke events among individuals diagnosed with moyamoya disease.
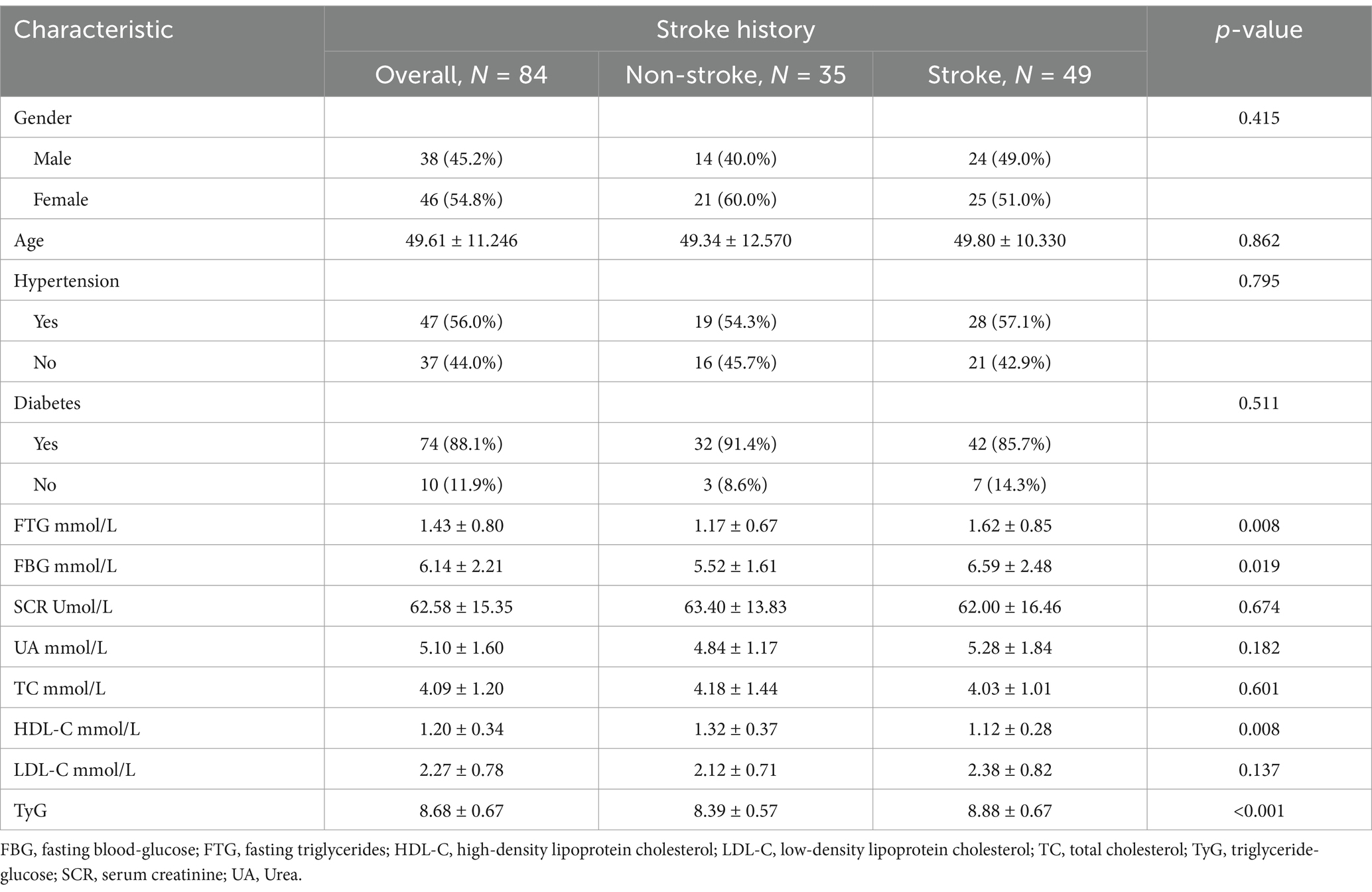
Methods: A total of 84 patients diagnosed with Moyamoya disease were treated at Changshu First People’s Hospital from 01 January 2019 to 31 October 2024 were included in this study. We systematically collected and analyzed their clinical histories, laboratory test results, and baseline data. The patients were classified into two groups based on their history of cerebral stroke. Subsequently, we conducted a comparison and analysis of the TyG index between these two groups.
Results: The TyG index observed in patients with moyamoya disease who have a history of cerebral stroke was significantly elevated compared to that of patients without such a history. This difference was found to be statistically significant (p < 0.05). Furthermore, regression cubic splines analysis indicated a noteworthy linear relationship between the TyG index and the occurrence of cerebral stroke events.
Conclusion: In individuals diagnosed with Moyamoya disease, the TyG index has been shown to have a significant correlation with the risk of cerebral stroke. Furthermore, it has the potential to serve as an effective predictor for the occurrence of stroke.
Introduction
Moyamoya disease (MMD), also known as spontaneous basilar ring occlusive disease or abnormal basal vascular network disorder, is a rare and chronic cerebrovascular condition. It is characterized by the progressive stenosis of the major intracranial arteries, resulting in the formation of a network of small, abnormal blood vessels. Notably, these vessels exhibit a distinct smoke-like appearance during angiographic imaging (1). The etiology of Moyamoya disease is not yet fully understood; however, it is associated with significant neurological complications stemming from compromised cerebral circulation. These complications can manifest as both ischemic and hemorrhagic strokes (2). The occurrence and progression of strokes have a significant impact on the daily lives of patients with Moyamoya disease. It is essential to investigate the factors that contribute to stroke in these patients and to implement targeted interventions aimed at reducing stroke incidence. Such efforts can improve clinical outcomes and overall prognosis for individuals affected by this condition. However, it is important to note that research in this area is currently limited (3, 4).
Insulin resistance (IR) is recognized as an independent risk factor for mortality and significant disability following a stroke (5). Historically, the hyperinsulinemic-euglycemic clamp (HEC) method has been considered the gold standard for diagnosing IR. However, the clinical implementation of this procedure has become increasingly challenging due to its significant cost, complex operational requirements, and the extensive time commitment involved (6). In recent years, the triglyceride-glucose index (TyG index) has emerged as a promising compound metabolic index. Research indicates that it is a straightforward and reliable alternative for evaluating insulin resistance (IR). Furthermore, the TyG index has demonstrated significant associations with the risk of cardiovascular and cerebrovascular events, along with various arterial diseases (7, 8).
This study aims to evaluate the potential of the TyG index as a predictive tool for stroke in patients diagnosed with Moyamoya disease. We collected clinical and laboratory data from 84 patients with Moyamoya disease, including 35 asymptomatic individuals and 49 patients with a history of stroke. The TyG index was calculated using fasting triglyceride and glucose levels, and its association with stroke risk was analyzed using logistic regression models, ROC curve analysis, and restricted cubic splines. Our results revealed that the TyG index was significantly higher in patients with a history of stroke compared to asymptomatic patients, demonstrating a strong linear association with stroke risk and suggesting its potential as a predictive biomarker in Moyamoya disease.
Methods
Study population
This retrospective study collected medical history and clinical examination data from patients with Moyamoya disease admitted to the Department of Neurosurgery at Changshu First People’s Hospital between01 January 2019 and 31 October 2024. A total of 84 patients with Moyamoya disease participated in this study, which included 35 asymptomatic patients and 49 patients who had experienced previous strokes. The inclusion criteria were based on the diagnostic standards outlined in the “Moyamoya disease: diagnosis and interventions” (9). Exclusion criteria: (1) Cerebrovascular changes resembling smog caused by hyperthyroidism, autoimmune diseases, brain radiotherapy, head trauma, and other conditions; (2) Patients who have previously undergone cerebrovascular reconstructive surgery.
In this study, the definition of stroke (10) encompasses both hemorrhagic and ischemic types. Hemorrhagic stroke was defined as a sudden neurological deficit caused by the rupture of a cerebral blood vessel, resulting in bleeding into the brain parenchyma (intracerebral hemorrhage, ICH) or the subarachnoid space (subarachnoid hemorrhage, SAH). Diagnosis was confirmed using non-contrast computed tomography (CT) or magnetic resonance imaging (MRI), which revealed hyperdense areas indicative of hemorrhage. Ischemic stroke was defined as a sudden neurological deficit caused by the interruption of blood flow to a part of the brain, resulting in tissue ischemia and infarction. Ischemic stroke subtypes were classified as thrombotic, embolic, or lacunar based on the underlying mechanism of arterial occlusion. Diagnosis was confirmed using non-contrast computed tomography (CT) or magnetic resonance imaging (MRI), with diffusion-weighted imaging (DWI) used to identify early ischemic changes.
Asymptomatic patients (11) were defined as those without a history of stroke, transient ischemic attack (TIA), or any other neurological symptoms attributable to moyamoya disease at the time of diagnosis. These patients were identified during routine health check-ups or evaluations for unrelated conditions.
Data collection and definition
Clinical medical records were systematically collected from patients, encompassing key demographic information such as age and gender, as well as relevant medical histories, including diabetes and hypertension. In addition, early morning fasting venous blood samples were obtained, with laboratory analyses conducted within 12 h of patient admission. TyG index = ln [fasting triglyceride (mg/dl) × fasting glucose (mg/dl)/2] (12).
Statistical analysis
Quantitative variables were reported as mean ± standard deviation. Differences between groups were assessed using either ANOVA or the Kruskal-Wallis test based on data distribution. Categorical variables are reported in terms of counts and percentages, and their analysis is conducted using chi-square tests.
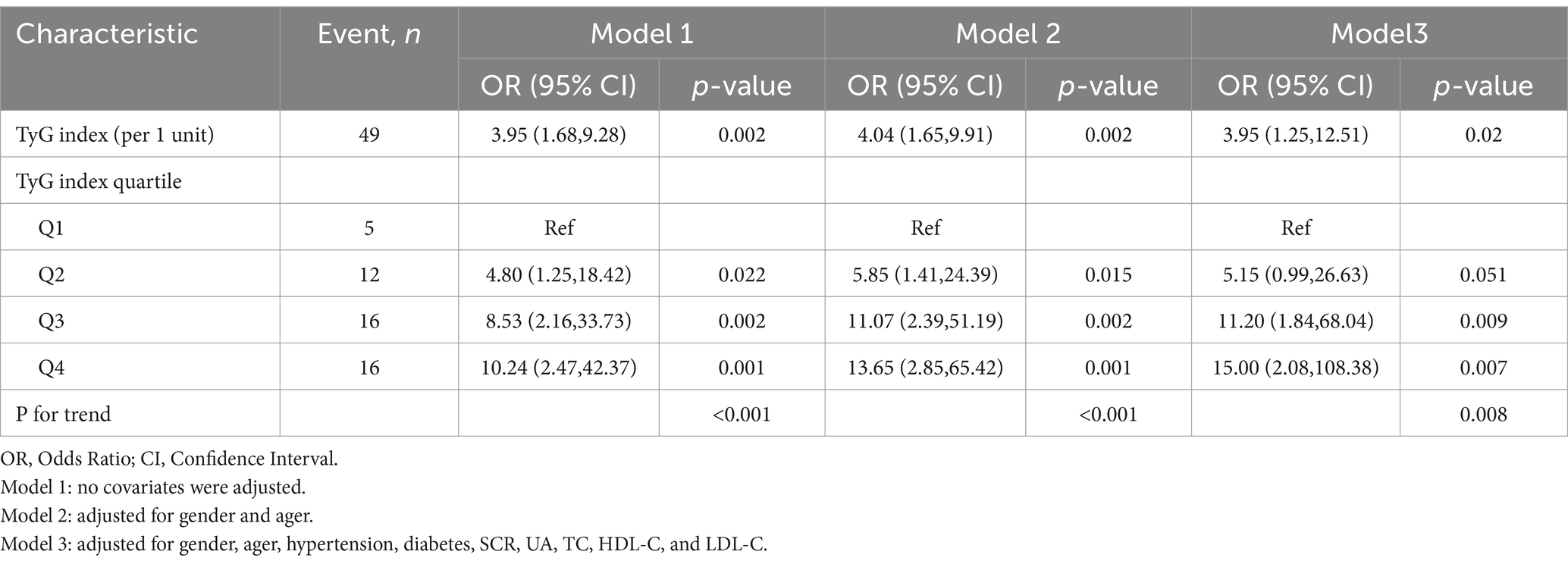
To assess the relationship between the TyG index and the risk of stroke, a logistic proportional hazards regression model was employed to calculate odds ratios (ORs) and 95% confidence intervals (95% CIs). Three statistical models were developed by varying the adjustment for covariates. Model 1 includes no adjustments. Model 2 incorporates adjustments for gender and age. Model 3 provides additional adjustments for hypertension, diabetes, serum creatinine (SCR), uric acid (UA), total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), and low-density lipoprotein cholesterol (LDL-C). The Receiver Operating Characteristic (ROC) curve was utilized to evaluate the predictive performance of the TyG index regarding stroke risk. Additionally, a fully adjusted restricted cubic spline (RCS) analysis was conducted to explore the dose–response relationship between the TyG index and stroke risk in patients diagnosed with Moyamoya disease.
Additionally, subgroup analyses were conducted to determine if the association between the TyG index and stroke risk varied across different demographics, including gender, age, hypertension, and diabetes. Interaction analyses were conducted to investigate potential variations in stroke risk across the identified subgroups. To ensure the robustness of our findings, a sensitivity analysis was performed, calculating an E-value based on Model 3. This analysis aimed to determine the minimum strength of association between unmeasured confounders and the TyG index that could potentially explain the observed association with stroke risk. All statistical analyses were performed utilizing R version 4.2.2. For the purposes of this study, p values below 0.05 were deemed statistically significant.
Results
Baseline characteristics
The baseline characteristics of the participants are summarized in Table 1. In the subgroup with a history of stroke (N = 49), the following measurements were found to be significantly elevated compared to those in the subgroup without a history of stroke (N = 35): fasting triglycerides (1.62 ± 0.85 mmol/L, p = 0.008), fasting blood glucose (6.59 ± 2.48 mmol/L, p = 0.019), TyG index (8.88 ± 0.67, p < 0.001), and high-density lipoprotein (1.12 ± 0.28 mmol/L, p = 0.008). Both groups exhibited no statistically significant differences in the levels of creatinine, urea, total cholesterol, and low-density lipoprotein. The analysis revealed that there were no significant differences in the distribution of sex, hypertension, and diabetes among the groups.
Relationship between stroke risk and TyG index
A total of 49 patients had a documented history of stroke. Logistic regression analysis demonstrated that each one-unit increase in the triglyceride glucose index (TyG), analyzed as a continuous variable, was significantly associated with an increased risk of stroke across all three models. In the unadjusted Model 1, the odds ratio (OR) was calculated at 3.95 (95% CI: 1.68, 9.28; p = 0.002), suggesting a significant association. This strong association persisted in Model 2, which adjusted for sex and age, yielding an OR of 4.04 (95% CI: 1.65, 9.91; p = 0.002). Furthermore, in Model 3, which accounted for additional covariates, the OR was recorded at 3.95 (95% CI: 1.25, 12.51; p = 0.020). These findings highlight the robustness of the association across multiple analytical models. In the analysis of the quartile test utilizing the TyG as a categorical variable with Q1 as the reference group, the odds ratio for Q2 in model 3 is 5.15 (95% confidence interval: 0.99, 26.63; p = 0.051). For Q3, the odds ratio is 11.20 (95% CI: 1.84, 68.04; p = 0.009), and for Q4, it stands at 15.00 (95% CI: 2.08, 108.38; p = 0.007). These findings indicate that, compared to the baseline of Q1, the risk of stroke is elevated by a factor of 5.15 for Q2, 11.2 for Q3, and 15 for Q4. The trend of p-values across all models was found to be statistically significant (p < 0.001). This suggests that the observed relationship continues to be significant even after making the necessary adjustments for covariates (Table 2).
Subgroup and sensitivity analysis
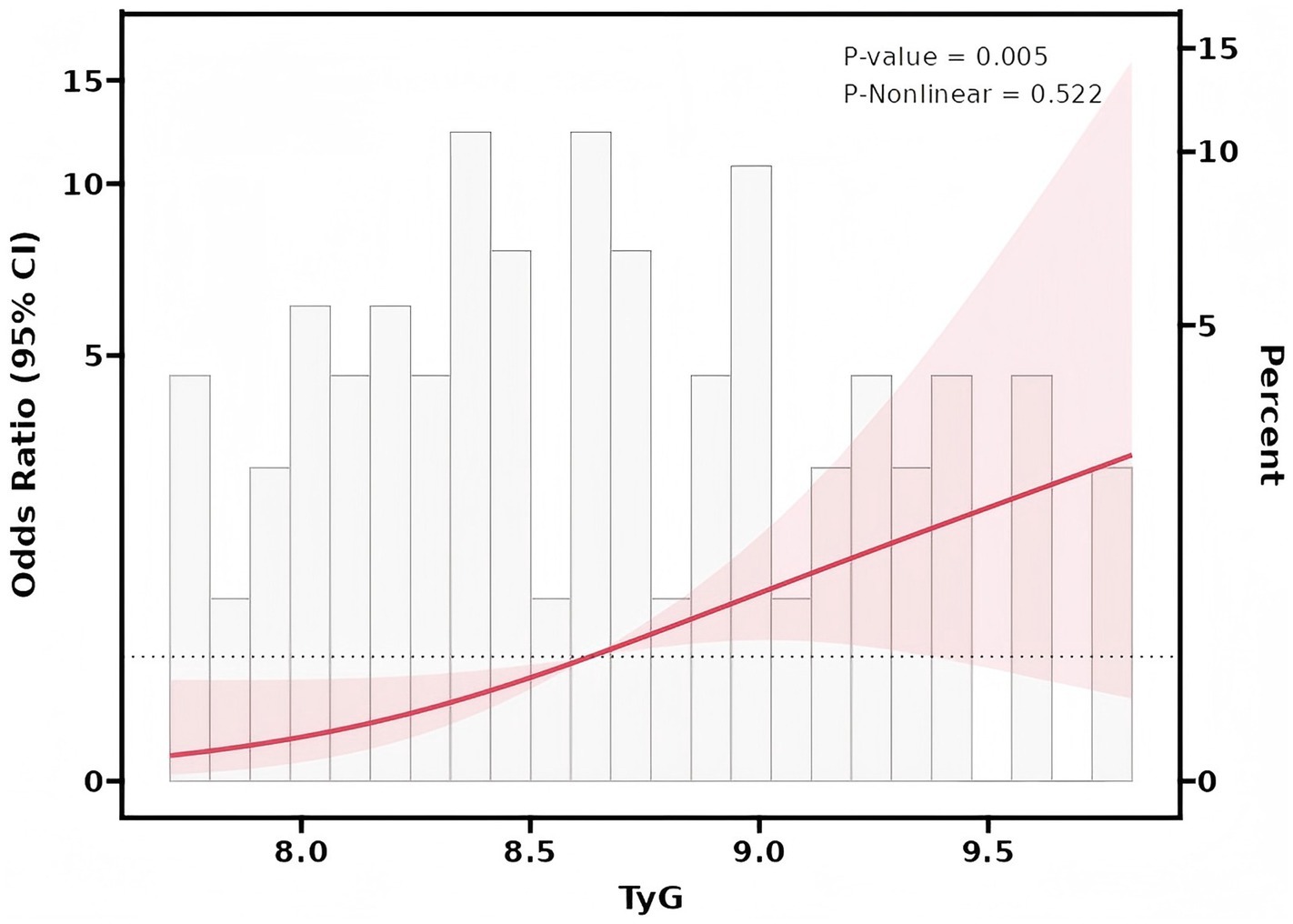
The value of the TyG index in predicting stroke among patients with moyamoya disease has been assessed using the ROC curve analysis. The results indicate an area under the curve (AUC) value of 0.718, signifying a strong predictive capability for this index in this patient population (Figure 1). Further analysis utilizing Restricted Cubic Splines (RCS) revealed a significant linear association between the TyG index and the occurrence of stroke events across all participants (p = 0.005, P for non-linear = 0.522) (Figure 2).
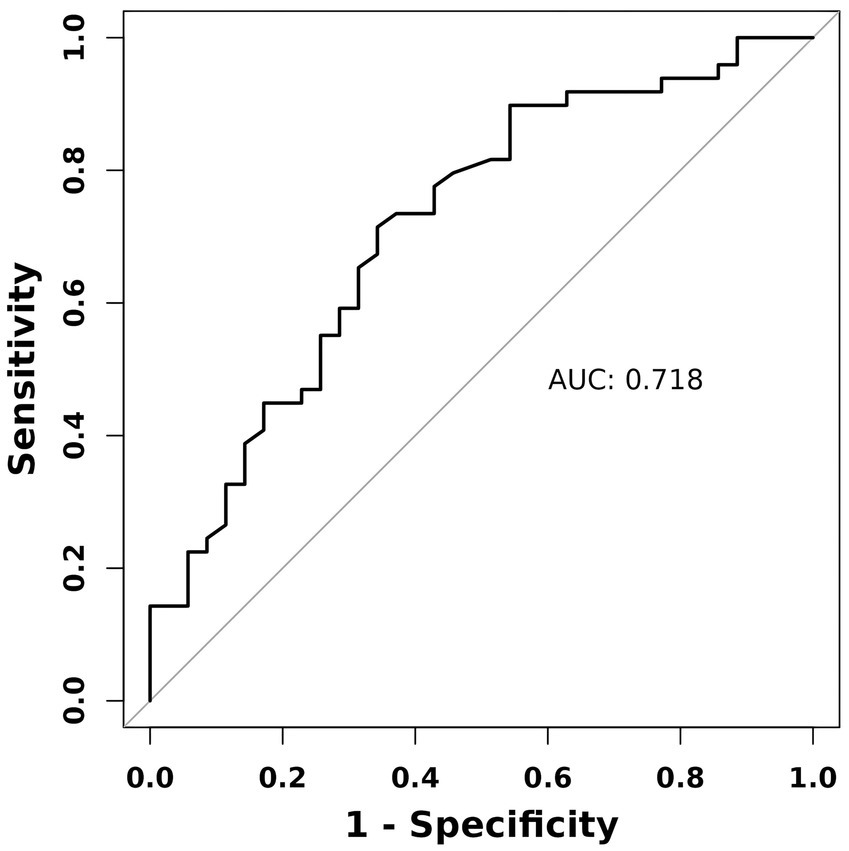
Figure 1. Receiver operating characteristic (ROC) curve analysis of the TyG index for predicting stroke in patients with Moyamoya disease.
Sensitivity analysis
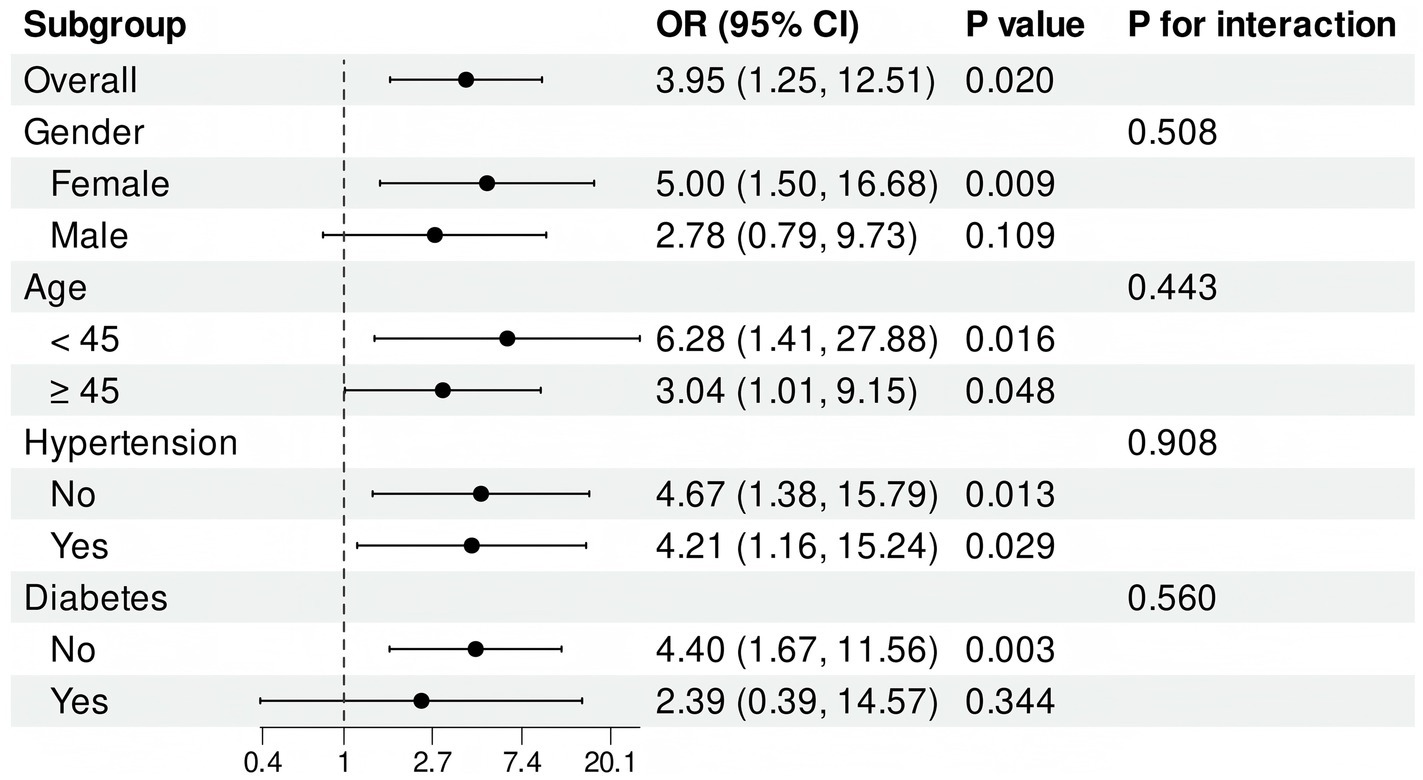
The calculation of an E value of 7.36 for TyG, based on model 3, indicates that only significant unmeasured confounders may account for the observed association. To enhance our understanding of the relationship between the TyG index and stroke incidence in patients diagnosed with Moyamoya disease, we conducted an analysis of the TyG index as a continuous variable. This analysis was performed within subgroups categorized by gender, age, hypertension, and diabetes. The findings demonstrate that elevated levels of the TyG index were consistently observed in female, non-diabetic subgroups, irrespective of age and the presence of co-hypertension. An interaction analysis was conducted to assess potential interactions between these subgroups and the TyG index. The results indicate that no significant interactions were found among the subgroups (Figure 3).
Discussion
Moyamoya disease, first recognized by Japanese scholars in the 1850s, derives its name from the appearance of the abnormal network of blood vessels located at the base of the brain (13, 14). Presently, the etiology of Moyamoya disease is not fully understood. The condition is characterized by progressive stenosis and obstruction of the ends of the bilateral internal carotid arteries, as well as the anterior and middle cerebral arteries. Additionally, compensatory collateral vessels are formed that facilitate blood circulation (15). Moyamoya disease presents with a variety of initial forms, the most prevalent of which is stroke. This can manifest as both ischemic and hemorrhagic strokes (16, 17). Stroke represents one of the primary causes of significant disability in adults. Its impact extends beyond the affected individuals, profoundly influencing their long-term quality of life and imposing considerable challenges on their families and society as a whole (18). At this time, the understanding of the factors that affect stroke onset and prognosis in moyamoya disease is still quite limited. Further research is necessary to enhance our knowledge in this area.
Insulin resistance (IR) is a widely recognized concern within clinical practice and is a critical factor in the development and progression of cardiovascular and cerebrovascular diseases. In recent years, the triglyceride glucose index (TyG index) has emerged as a prominent research focus due to its status as a simple and reliable surrogate marker of IR (19). The TyG index serves as an effective indicator of the body’s metabolic state by integrating fasting triglyceride and blood glucose levels (20). It is closely associated with the risk of atherosclerosis as well as cardiovascular and cerebrovascular events (21).
Recent studies indicate that the TyG index plays a significant role in enhancing the instability of atherosclerotic plaques (22). This occurs through the activation of innate immune responses and the elevation of systemic inflammatory markers (23). The accumulation of advanced glycosylation end products (AGEs) is associated with the development of arteriosclerosis (24). A high TyG index has dual implications for cerebral health. On one hand, it is associated with a reduction in telangiectasia and the development of cerebral vasoconstriction, which can exacerbate cerebral ischemia through inflammatory processes (25). On the other hand, an elevated TyG index enhances the permeability of the blood–brain barrier, leading to brain edema, damage to vascular endothelial cells, and an increased risk of cerebral hemorrhage (26, 27). Furthermore, a high TyG index may be significantly associated with both the severity and number of intracranial artery stenosis, which may subsequently increase the risk of stroke (28). Extensive research has demonstrated a correlation between elevated TyG index levels and the progression of atherosclerosis (29, 30). This condition is a critical contributor to ischemic stroke, which subsequently impacts the course of stroke development (31). Limited research exists regarding the association between the TyG index and the incidence and progression of stroke in patients diagnosed with Moyamoya disease. This study represents the first investigation into the predictive value of the TyG index for stroke occurrence in patients with moyamoya disease. The findings reveal a significant correlation between the TyG index and the incidence of stroke in these patients, underscoring its considerable clinical relevance.
This study retrospectively examined a cohort of 84 patients diagnosed with Moyamoya disease, classifying them based on their history of stroke. The analysis indicated that the triglyceride-glucose (TyG) index was significantly elevated in patients with a prior stroke compared to those without. Additionally, when controlling for various covariates, including gender, age, total cholesterol, high-density lipoprotein (HDL), low-density lipoprotein (LDL), creatinine, and urea levels, the association between the TyG index and stroke remained statistically significant. The results of this study suggest that the TyG index may be an independent risk factor for stroke in patients diagnosed with Moyamoya disease. Additionally, the ROC curve analysis indicates that the TyG index is highly effective in predicting stroke, with an area under the curve (AUC) of 0.718. These findings further substantiate the clinical application potential of the TyG index.
The findings of this study present valuable new perspectives on the prevention and management of stroke in individuals diagnosed with Moyamoya disease. In patients exhibiting a high TyG index, early intervention and proactive treatment strategies may significantly mitigate the risk of stroke. Enhancing insulin sensitivity along with the regulation of lipid and glucose levels may effectively reduce the incidence of cerebrovascular events. Furthermore, early cerebral revascularization surgery has the potential to serve as an effective preventive measure for patients identified as high-risk.
It is important to note that this study has some inherent limitations, including individual variability in laboratory measurements, which may impact the outcomes. Additionally, the long-term predictive impact of continuous changes in the TyG index on the prognosis of Moyamoya patients was not evaluated. Future research should focus on larger sample sizes and extended follow-up periods to further substantiate these findings.
Conclusion
In conclusion, this study presents, for the first time, a significant correlation between the TyG index and the occurrence of strokes in patients with moyamoya disease. This finding suggests that the TyG index may serve as a valuable predictor of stroke risk in this patient population. Consequently, it provides a novel perspective for the clinical management of moyamoya disease. Further research is warranted to confirm its clinical applicability and to investigate the underlying pathophysiological mechanisms.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Medical Ethics Committee of the First People's Hospital of Changshu. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
CZ: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. KG: Data curation, Formal analysis, Investigation, Methodology, Supervision, Writing – original draft. HX: Conceptualization, Formal analysis, Project administration, Validation, Writing – review & editing. GK: Funding acquisition, Resources, Visualization, Writing – review & editing. CL: Software, Supervision, Validation, Writing – review & editing, Data curation, Formal analysis, Investigation, Methodology.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Rifino, N, Hervè, D, Acerbi, F, Kuroda, S, Lanzino, G, Vajkoczy, P, et al. Diagnosis and management of adult Moyamoya angiopathy: an overview of guideline recommendations and identification of future research directions. Int J Stroke. (2024):17474930241297031. doi: 10.1177/17474930241297031
2. Zeferino, D Jr, Thiago, C, and Sandrieli, A. Moyamoya Angiopathy and 15q11.2 gene deletion syndrome. World Neurosurg. (2023) 172:1–2. doi: 10.1016/j.wneu.2023.01.005
3. Futier, E, Lefrant, JY, Guinot, PG, Godet, T, Lorne, E, Cuvillon, P, et al. Effect of individualized vs standard blood pressure management strategies on postoperative organ dysfunction among high-risk patients undergoing major surgery: a randomized clinical trial. JAMA. (2017) 318:1346–57. doi: 10.1001/jama.2017.14172
4. Archana, H. Posterior reversible encephalopathy syndrome: clinical features and outcome. Front Neurol. (2020) 11:71. doi: 10.3389/fneur.2020.00071
5. Ago, T, Matsuo, R, Hata, J, Wakisaka, Y, Kuroda, J, Kitazono, T, et al. Insulin resistance and clinical outcomes after acute ischemic stroke. Neurology. (2018) 90:e1470–7. doi: 10.1212/WNL.0000000000005358
6. Se Eun, P, Cheol-Young, P, and Gary, S. Biomarkers of insulin sensitivity and insulin resistance: past, present and future. Crit Rev Clin Lab Sci. (2015) 52:180–90. doi: 10.3109/10408363.2015.1023429
7. Ramdas Nayak, VK, Satheesh, P, Shenoy, MT, and Kalra, S. Triglyceride glucose (TyG) index: a surrogate biomarker of insulin resistance. J Pak Med Assoc. (2022) 72:986–8. doi: 10.47391/JPMA.22-63
8. Miao, M, Zhou, G, Bao, A, Sun, Y, Du, H, Song, L, et al. Triglyceride-glucose index and common carotid artery intima-media thickness in patients with ischemic stroke. Cardiovasc Diabetol. (2022) 21:43. doi: 10.1186/s12933-022-01472-1
9. Ihara, M, Yamamoto, Y, Hattori, Y, Liu, W, Kobayashi, H, Ishiyama, H, et al. Moyamoya disease: diagnosis and interventions. Lancet Neurol. (2022) 21:747–58. doi: 10.1016/S1474-4422(22)00165-X
10. Sacco, RL, Kasner, SE, Broderick, JP, Caplan, LR, Connors, JJ, Culebras, A, et al. An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. (2013) 44:2064–89. doi: 10.1161/STR.0b013e318296aeca
11. Satoshi, K. Asymptomatic moyamoya disease: literature review and ongoing AMORE study. Neurol Med Chir (Tokyo). (2015) 55:194–8. doi: 10.2176/nmc.ra.2014-0305
12. Rangan, A, Balaji, D, Chand, U, Raghunathan, E, Deepthi, N, and Karthik, P. Triglyceride-glucose index, remnant cholesterol and common carotid artery intima-media thickness as an atherosclerotic marker in ischemic stroke patients. Georgian Med News. (2024):59–65.
13. Gonzalez, NR, Amin-Hanjani, S, Bang, OY, Coffey, C, Du, R, Fierstra, J, et al. Adult Moyamoya disease and syndrome: current perspectives and future directions: a scientific statement from the American Heart Association/American Stroke Association. Stroke. (2023) 54:e465–79. doi: 10.1161/STR.0000000000000443
14. Berry, JA, Cortez, V, Toor, H, Saini, H, and Siddiqi, J. Moyamoya: an update and review. Cureus. (2020) 12:e10994. doi: 10.7759/cureus.10994
15. Zhang, X, Xiao, W, Zhang, Q, Xia, D, Gao, P, Su, J, et al. Progression in Moyamoya disease: clinical features, neuroimaging evaluation, and treatment. Curr Neuropharmacol. (2021) 20:292–308. doi: 10.2174/1570159X19666210716114016
16. Brandicourt, P, Blanc, C, Bonnet, L, Bejot, Y, Ricolfi, F, Drouet, C, et al. Adult moyamoya angiopathy in Bourgogne-Franche-Comté: epidemiology, diagnosis and management. Rev Neurol (Paris). (2018) 175:247–51. doi: 10.1016/j.neurol.2018.05.004
17. Hui, Z, Lijian, Z, and Lei, F. Epidemiology, diagnosis and treatment of moyamoya disease. Exp Ther Med. (2019) 17:1977–84. doi: 10.3892/etm.2019.7198
18. Nguyen, VN, Motiwala, M, Elarjani, T, Moore, KA, Miller, LE, Barats, M, et al. Direct, indirect, and combined Extracranial-to-intracranial bypass for adult Moyamoya disease: an updated systematic review and Meta-analysis. Stroke. (2022) 53:3572–82. doi: 10.1161/STROKEAHA.122.039584
19. Zhang, N, Xiang, Y, Zhao, Y, Ji, X, Sang, S, Shao, S, et al. Association of triglyceride-glucose index and high-sensitivity C-reactive protein with asymptomatic intracranial arterial stenosis: a cross-sectional study. Nutr Metab Cardiovasc Dis. (2021) 31:3103–10. doi: 10.1016/j.numecd.2021.07.009
20. Wang, L, Li, Z, Qiu, R, Luo, L, and Yan, X. Triglyceride glucose index-body mass index as a predictor of coronary artery disease severity in patients with H-type hypertension across different glucose metabolic states. Diabetol Metab Syndr. (2025) 17:15. doi: 10.1186/s13098-024-01568-6
21. Devesa, A, Fuster, V, Vazirani, R, García-Lunar, I, Oliva, B, España, S, et al. Cardiac insulin resistance in subjects with metabolic syndrome traits and early subclinical atherosclerosis. Diabetes Care. (2023) 46:2050–7. doi: 10.2337/dc23-0871
22. Zhang, J, Hu, M, Jia, Y, Zhao, S, Lv, P, Fan, M, et al. The triglyceride glucose index is associated with the cerebral small vessel disease in a memory clinic population. J Clin Neurosci. (2022) 104:126–33. doi: 10.1016/j.jocn.2022.08.019
23. Dang, K, Wang, X, Hu, J, Zhang, Y, Cheng, L, Qi, X, et al. The association between triglyceride-glucose index and its combination with obesity indicators and cardiovascular disease: NHANES 2003-2018. Cardiovasc Diabetol. (2024) 23. doi: 10.1186/s12933-023-02115-9
24. Cui, C, Liu, L, Zhang, T, Fang, L, Mo, Z, Qi, Y, et al. Triglyceride-glucose index, renal function and cardiovascular disease: a national cohort study. Cardiovasc Diabetol. (2023) 22:325. doi: 10.1186/s12933-023-02055-4
25. Nam, K, Kwon, H, and Lee, Y. Triglyceride-related parameters and symptomatic atherosclerotic lesions in patients with ischemic stroke. J Lipid Atheroscler. (2024) 13:155–65. doi: 10.12997/jla.2024.13.2.155
26. Huo, RR, Liao, Q, Zhai, L, You, XM, and Zuo, YL. Interacting and joint effects of triglyceride-glucose index (TyG) and body mass index on stroke risk and the mediating role of TyG in middle-aged and older Chinese adults: a nationwide prospective cohort study. Cardiovasc Diabetol. (2024) 23. doi: 10.1186/s12933-024-02122-4
27. Yang, Y, Huang, X, Wang, Y, Leng, L, Xu, J, Feng, L, et al. The impact of triglyceride-glucose index on ischemic stroke: a systematic review and meta-analysis. Cardiovasc Diabetol. (2023) 22:2. doi: 10.1186/s12933-022-01732-0
28. Tao, LC, Xu, JN, Wang, TT, Hua, F, and Li, JJ. Triglyceride-glucose index as a marker in cardiovascular diseases: landscape and limitations. Cardiovasc Diabetol. (2022) 21:68. doi: 10.1186/s12933-022-01511-x
29. Wu, L, Zhu, J, Li, C, Zhu, J, Dai, Z, and Jiang, Y. Association of triglyceride-glucose index with ischemic stroke recurrence in nondiabetic patients with small vessel occlusion: a multicenter hospital-based prospective cohort study. Cardiovasc Diabetol. (2022) 21:250. doi: 10.1186/s12933-022-01693-4
30. Nam, KW, Kwon, HM, Jeong, HY, Park, JH, Kwon, H, and Jeong, SM. High triglyceride-glucose index is associated with subclinical cerebral small vessel disease in a healthy population: a cross-sectional study. Cardiovasc Diabetol. (2020) 19:1–8. doi: 10.1186/s12933-020-01031-6
Keywords: triglyceride-glucose index, Moyamoya disease, stroke, insulin resistance, atherosclerosis of the arteries
Citation: Zhang C, Guo K, Xu H, Kong G and Liu C (2025) Association between triglyceride-glucose index and the risk of stroke among moyamoya patients: a single-center retrospective study. Front. Neurol. 16:1547627. doi: 10.3389/fneur.2025.1547627
Edited by:
Shihao He, Peking Union Medical College Hospital (CAMS), ChinaReviewed by:
Xiaofan Yu, Capital Medical University, ChinaZhenyu Zhou, Capital Medical University, China
Copyright © 2025 Zhang, Guo, Xu, Kong and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chuanghong Liu, bnNjaC5oLmxpdUBmb3htYWlsLmNvbQ==
†These authors have contributed equally to this work
 Chi Zhang
Chi Zhang Kai Guo†
Kai Guo†