
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol. , 31 January 2025
Sec. Headache and Neurogenic Pain
Volume 16 - 2025 | https://doi.org/10.3389/fneur.2025.1529213
 Nura A. Almansour1,2†
Nura A. Almansour1,2† Seham S. Alsalamah1,2†
Seham S. Alsalamah1,2† Razan S. Alsubaie1,2*†
Razan S. Alsubaie1,2*† Nada N. Alshathri1,2†
Nada N. Alshathri1,2† Yasmeen A. Alhedyan1,2†
Yasmeen A. Alhedyan1,2† Faisal Y. Althekair’s1,2,3†
Faisal Y. Althekair’s1,2,3†Background: Migraine is a primary headache disorder that affects more than 1 billion individuals globally and imposes a significant disability burden on society. Although migraine patients commonly experience poor sleep quality, the relationship between migraine and sleep is not yet fully understood. This study therefore aimed to determine the association between sleep quality and migraine severity.
Methods: A comparative cross-sectional study was conducted with 1,399 participants across all regions of Saudi Arabia from August to October 2023 using standardized questionnaires. Participants were categorized into patients with migraine and non-migraine patients, according to the International Headache Society (IHS) criteria. This study utilized The Migraine Disability Assessment Scale (MIDAS) and Pittsburgh Sleep Quality Index (PSQI) to evaluate migraine severity and sleep quality, respectively.
Results: The prevalence of migraine was 25%, while poor sleep quality was evident in 42.4% of the patients. No significant difference in PSQI scores was observed between patients with migraine and non-migraine patients (p = 0.821). Migraine patients with poor sleep quality showed significantly higher MIDAS scores than those with good sleep quality (10.37 vs. 6.58; p = 0.002), while patients with migraine with higher levels of disability had higher PSQI scores than those with lower levels of disability, although the difference was not statistically significance (7.61 vs. 6.81, p = 0.053). A significant positive correlation was found between the PSQI and MIDAS scores (r = 0.179, p < 0.001). MIDAS was also significantly positively correlated with the following PSQI components: subjective sleep quality (p = 0.047), sleep latency (p < 0.001), sleep disturbance (p < 0.001), and daytime dysfunction (p < 0.001).
Conclusion: These findings suggest a notable correlation between poor sleep quality and increased migraine severity, emphasizing the importance of addressing sleep disturbance as a potential strategy to mitigate migraine severity and improve patient outcomes.
Migraine is a recurrent, burdensome neurovascular disorder characterized by bouts of disabling, throbbing, and often unilateral headaches, accompanied by various concomitant symptoms such as nausea, vomiting, and light and sound sensitivity (1). Of all headache disorders, migraine is one of the most prevalent and most disabling (2). Globally, migraine ranked as the 19th most common cause of disability according to the Global Burden of Disease Report (GBD) in 2000 (3). However, on the GBD 2015, migraine was ranked as the third most disabling disorder in individuals below 50 years of age (4). Along the same lines, the GBD Report 2016 shows that tension-type headaches and migraine are ranked third and sixth in terms of prevalence, respectively (2). Although the underlying pathophysiology has not yet been fully elucidated, migraine are known to be triggered by numerous environmental factors, including lifestyle, hormones, and sleep disturbances (5). Sleep is a physiological aspect of human life that is essential for preserving health and welfare. It is a natural and reversible condition primarily regulated by neurobiological processes (6, 7). Sleep quality is a multifaceted construct that considers several factors, including waking following sleep start, frequency and number of night awakenings, sleep latency, and subjective assessments of rested and awakened (8). A “good night’s sleep” is generally classified as a night with adequate rest (often 78 h) to allow for the homeostatic restorative process, and it is distinguished by an overall high quality of the entire sleep period (9). One-third of the general population experienced sleep problems. Sleep quality is generally considered as a significant indicator of quality of life, given the high prevalence of sleep disorders and the close connection between sleep and quality of life (10).
Poor sleep quality is more common in patients with migraine than in the general population and affects migraine patients in many ways (11). In one study investigating 103 university students with migraine, 85 (82.5%) had poor sleep quality, whereas 18 (17.5%) had normal sleep quality (12). In another study, one-third of 50 patients with migraine and tension-type headaches reported sleep problems as the cause of their headaches. Of these, 68.7% were awakened by headaches, 30% of whom reported that their headaches were caused by sleep deprivation, excessive sleep, or both (13). Migraine chronicity is significantly affected by poor sleep quality (9, 14). It is also possible that migraine episodes were preceded by poor sleep (15). Headache severity and frequency are commonly affected both directly and indirectly by sleep quality in migraine (16). Similarly, because migraine has frequently been observed as a triggering factor, they can also be a triggering factor for other types of illnesses. Migraine patients have an increased risk of ischemic stroke, sleep disruption, and depression (17–19). Further, sleep quality and how migraine exerts its effects have been emphasized owing to their relevance. A high incidence of 61.61% of patients with migraine complain about their sleep quality (20). Furthermore, the relationship between migraine and sleep has been validated by the prevalent complaints regarding difficulty in initiating and maintaining a healthy sleep rhythm (21). Moreover, sleep interruption is a common problem among patients with migraine, and multiple studies have shown a higher prevalence of poor sleep quality compared with normal individuals (22–25). Although Fox and Davis concluded that headache attacks are not associated with disturbed sleep (26), while indistinguishable sleep parameters were reported in migraine patients and controls, migraine subjects exhibited a longer sleep onset latency (27). Boosting sleep quality has also shown to be more achievable if the recurrence of headache attacks diminishes (28). These findings indicate that a complex relationship exists between migraine and sleep quality.
Migraine patients have further been found to have reduced subjective sleep quality and altered sleep architecture compared to non-migraine patients (29). However, data on the association between migraine and sleep quality are lacking. The present study is one of the first to thoroughly examine the relationship between migraine and sleep quality from a population-based perspective to learn more about the specific relationship between migraine and sleep quality.
This study investigated the association between migraine severity and sleep quality in all regions of Saudi Arabia from August to October 2023. This study is a comparative cross-sectional study enrolling 1,399 participants from all regions of Saudi Arabia. The required sample size was calculated using the Epitools website1 using g-power, with an effect size of 0.1 and one degree of freedom. The inclusion criterion was anyone above the age of 18 years of either sex. The exclusion criteria included primary headaches other than migraine, evaluation using the IHS criteria, and surgery within the last 6 months. The participants were further divided into migraine patients (cases) and non-migraine patients (controls), based on the application of the IHS criteria.
Data were obtained using an online, structured, self-administered questionnaire in Arabic created using Google Forms. The first part of the questionnaire explored the sociodemographic characteristics of the study participants. Age, sex, height, weight, and BMI of the participants were all obtained. Other participant characteristics, such as smoking status, presence of comorbidities, and family history of headaches, were also recorded. Finally, a screening question regarding the history of headaches in one’s life was posed to all participants. If the participant answered yes, they were moved to the IHS criteria page and the Migraine Disability Assessment Scale (MIDAS). If not, they would move on to the Pittsburgh Sleep Quality Index (PSQI) page.
The International Headache Society (IHS) criteria were included in the questionnaire to diagnose and differentiate patients with migraine from non-migraine patients (control group). The IHS classification is a 4-digit hierarchical method used to diagnose headaches with variable specificities, with the first digit being specific for diagnostic categories, the second digit for subtypes, and the third and fourth digits for more specifications. The criteria were as follows: untreated or unsuccessfully treated headache attacks that last 4–72 h occurring more than 15 times per month not attributed to any other disease; a headache that had at least two features (unilateral, pulsatile, moderate, and severe pain, aggravated by physical activity); and at least one of the following associated symptoms (nausea and/or vomiting, photophobia, or phonophobia) must occur alongside the headache (30).
An Arabic-validated form of the MIDAS questionnaire was used to measure disability levels linked to migraine (31). Comprising five questions, this questionnaire assesses the number of workdays lost due to migraine over 3 months. The MIDAS focuses on migraine-induced disability affecting work/study, household duties, and leisure activities on migraine days (32). The questions measure either complete inactivity days or days with productivity reduced by 50% or more. The cumulative total of these days was subsequently categorized into four disability severity levels, as follows: Grade I (0–5 points), indicating little to no disability; Grade II (6–10 points), mild disability; Grade III (11–20 points), moderate disability; and Grade IV (21 points or more), severe disability. The MIDAS questionnaire has two components: MIDAS A, which tracks the frequency of headaches, and MIDAS B, which rates the intensity of pain on a scale of 0 (no pain) to 10 (extremely severe pain) over a three-month period.
The PSQI is a questionnaire that assesses total sleep time, self-reported sleep quality, and disorders present over the past month. The questionnaire contains 19 questions distributed across seven domains. Subjective sleep quality, sleep latency, sleep length, sleep activity, sleep medication usage, sleep disorders, and daytime functional performance are the seven primary elements of this scale. The sum of all component scores yields the total PSQI score, for which a decline in sleep quality is indicated by a PSQI score of >5. The Arabic version of the questionnaire was based on a previously published paper (33) and incorporated into Google Forms. Respondents were either asked to write a short text answer or select one out of four options, as per the PSQI questionnaire.
Statistical Analysis was conducted using the Statistical Package for the Social Sciences (SPSS) version 29.0, released in 2022 by SPSS Inc., Chicago, IL, United States. Data are presented as the mean ± standard deviation (SD), or frequency counts and corresponding percentages. Chi-square and independent t-tests were applied to compare variables. Pearson’s correlation analysis was further used to assess the correlations between the scales. A multivariate linear regression analysis was conducted to evaluate the effect of sleep quality on migraine severity under different adjustment conditions and subgroups. Likewise, multivariate linear regression analysis was conducted to evaluate the effect of migraine severity on sleep quality. Three multivariate linear regression models were used, and all variables that were significant in the univariate regression analysis were included in the multivariate regression models. Statistical significance was set at p < 0.05.
A total of 1,567 individuals completed the questionnaire, of whom 35 were excluded for being under 18 years of age, 116 for having undergone a surgical procedure within the last 6 months, and 17 for disagreeing to participate in the study. Finally, the enrolled cohort comprised 1,399 individuals with a mean (SD) age of 27.9 ± 11.6 and BMI of 24.4 ± 6.1, most of whom were from the central region of Saudi Arabia (376 [26.9%]), were married (977 [69.8%]), and were university students or graduates (1,056 [75.5%]). A small proportion of participants were current or previous smokers (n = 129 [9.1%]). Moreover, almost two-thirds of the study participants had a family member complaining of headaches (898 [71.7%]).
Of the 1,399 participants included in the study, 349 had migraine according to the IHS diagnostic criteria, representing 24.95% of the total study population. Table 1 presents the sociodemographic data of the migraine patients and 1,050 controls. Notable findings included a significant sex difference, with females predominating in the migraine group [311 (89.1) vs. 758 (72.2); p < 0.001]. A higher proportion of individuals in the migraine group were unemployed or retired than in the control group [103 (29.5) vs. 208 (19.8); p < 0.001]. The average height of the migraine group was notably lower than that of the control group [160.14 (7.9) vs. 162.6 (9.2); p < 0.001].
As shown in Table 2, of the 349 participants with migraine, 83% did not miss work or school because of headaches over a period of 3 months. However, more than half of the participants did not perform household work for one or more days because of headaches. The mean total MIDAS score was 8.19 days, and was shown to be negatively affected by headaches for a duration of 3 months, while the mean MIDAS B score was 7.05. Regarding the overall MIDAS grade, more than half of the participants belonged to the little or no disability group. Moreover, only approximately 10% of migraine patients were categorized in the severe disability group.
As shown in Table 3, there was no significant difference in PSQI scores between the migraine and control groups. The overall cohort had a score of 6.9 (3.4), with 7.02 (3.4) for the migraine group and 6.97 (3.4) for the control group. The subjective sleep quality scores were 1.15 (0.8) in the migraine group and 1.09 (0.830) in the control group. The daily disturbance factor scores were similar between the migraine and control groups, with scores of 1.32 (0.64) and 1.36 (0.7), respectively. Overall, the PSQI score showed that most of the 813 participants had mild sleeping difficulty (56.4% migraine patients and 58.7% controls), and approximately 539 participants had moderate sleeping difficulty (40.1% migraine patients and 38% controls).
The association between MIDAS grade and various characteristics in the 349 migraine patients is presented in Table 4, of whom 259 had a little/mild MIDAS grade, and the remaining 90 migraine patients had moderate/severe disability levels. A family history of headache was significantly more common in both the little/mild (69.9%) and moderate/severe (76.7%) migraine severity groups. Another statistically significant parameter, shown in Table 4, was waking up from sleep due to headaches. More than half of those with a little/mild severity level (61.4%) did not have headache-related awakenings, whereas (35.5%) of those with the same severity grade reported sleep interruption due to headache. Conversely, approximately 50 percent of moderate/severe migraine patients (62.2%) reported waking from sleep, compared to 33.3 and 4.4% of the remaining patients who never wake up and always wake up because of headaches by (33.3%) and (4.4%), respectively. Among the medications taken for headache, ibuprofen was the only significant drug taken for headaches among both little/mild migraine patients (7.3%) and moderate/severe migraine patients (17.8%), as opposed to Panadol, Solpadeine, or other medications. Regarding whether headache improved with medications, both the little/mild (44.8%) and moderate/severe (65.6%) MIDAS groups reported that their headache sometimes improved with medications. Of the reported PSQI scores, the PSQI sleep latency score (C2; p = 0.02), PSQI sleep disturbance score (C5; p < 0.001), and PSQI daytime dysfunction score (C7; p = 0.022) all showed significant associations, as shown in Table 4. Finally, there was no statistically significant difference in PSQI scores across patients with different MIDAS severities.
Table 5 presents the association between the PSQI and migraine characteristics in 349 patients with migraine. Accordingly, 201 patients with migraine had no/mild PSQI grades and 148 had moderate/severe levels of sleep difficulty. Statistical analysis of the sociodemographic variables revealed no statistical differences in PSQI grade. High blood pressure was the only statistically significant comorbidity among patients with migraine. Statistically significant differences were further observed between those with no or mild sleeping difficulties, and those with moderate or severe sleeping difficulties taking medications for the comorbidities listed in Table 5. Among migraine patients in both PSQI groups, Table 5 shows the factors that trigger/worsen headaches. Overall, a lack of or excessive sleep was the most common migraine trigger for people with no/mild sleeping difficulties (61.7%) and moderate/severe sleeping difficulties (81.8%). This was followed by fatigue, stress, and certain smells with comparative frequencies in both the no/mild and moderate/severe PSQI groups, as shown in Table 5. Both PSQI groups reported significant results, indicating that both suffered from sleep disturbances as a result of headaches, albeit with differences in frequency. The no/mild sleeping difficulty group reported almost never waking up from sleep because of headaches. However, the moderate/severe group occasionally awoke from sleep. On the PSQI, 33.8% of those with no or mild sleeping difficulties reported occasional disturbances during sleep, compared with 54.1% of those with moderate or severe sleeping difficulties. In the no/mild sleep difficulty group, 3% reported always experiencing disturbed sleep due to headaches, whereas the moderate/severe sleep difficulty group reported a PSQI score of 4.1%. Medications improving headaches have been shown to be statistically significant in both PSQI groups, with the moderate to severe group reporting that using medications sometimes improved the headache (60.8%) With respect to the means to avoid headaches, taking medications demonstrated a statistical significance in both the no/mild sleeping difficulty (36.8%) and the moderate/ severe sleeping difficulty (50%) groups, making it the only statistically significant prophylactic strategy employed compared to the other practices. In this study, PSQI severity exhibited a significant p-value of <0.001. MIDAS scores and grades had p-values of 0.002 and 0.003, respectively, indicating that MIDAS grades and sleep quality were related.
A positive correlation was found between the PSQI and MIDAS scores in migraine patients, which was statistically significant (r = 0.18, p < 0.001) as shown in Table 6. The MIDAS was significantly correlated positively with the following PSQI components: subjective sleep quality (r = 0.11, p = 0.047), sleep latency (r = 0.19, p < 0.001), sleep disturbance (r = 0.23, p < 0.001), and daytime dysfunction (r = 0.2, p < 0.001). The Pearson correlation test did not reveal any association between the PSQI and its components with MIDAS B (Figure 1).
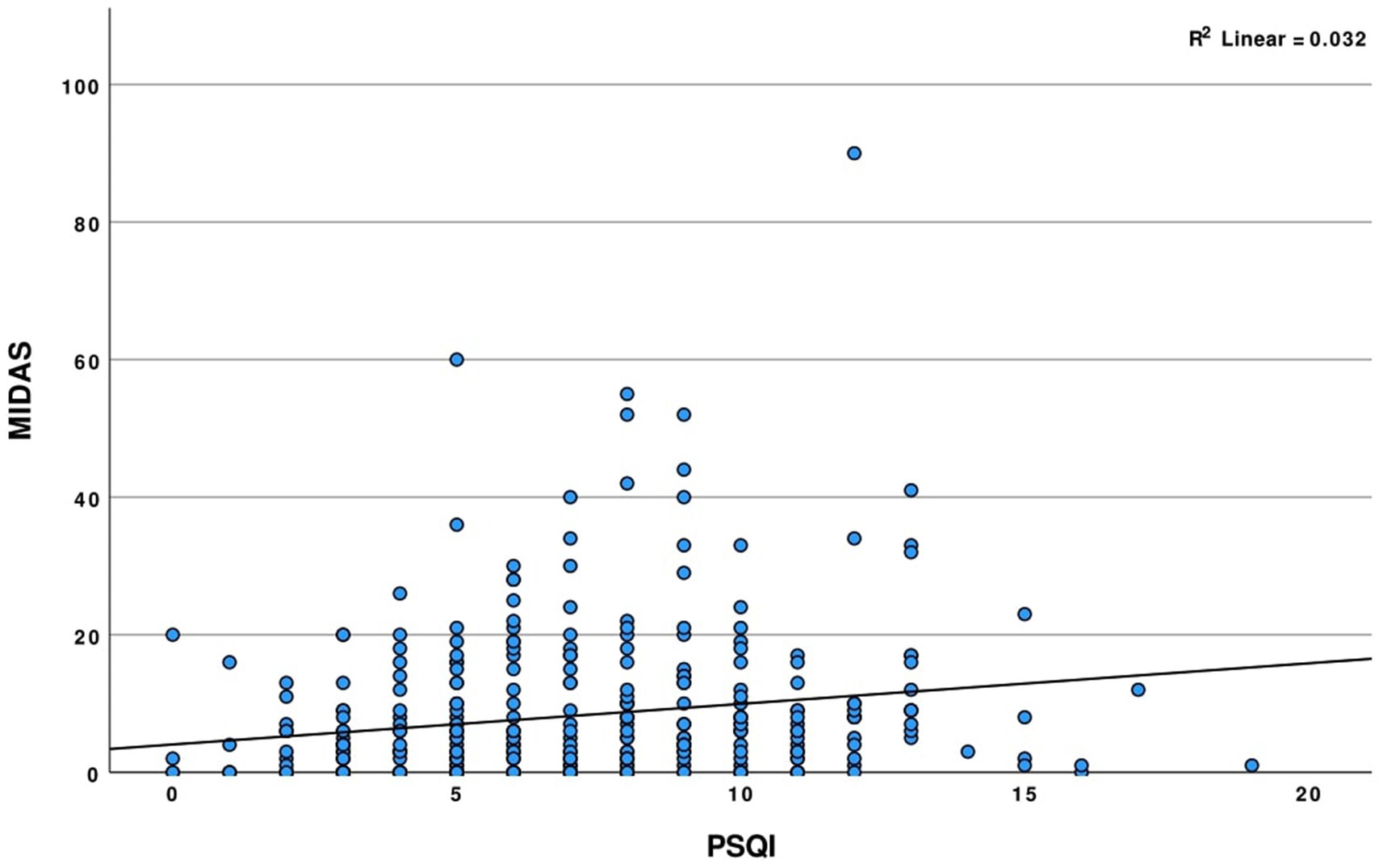
Figure 1. Scatter plot illustrating the correlation between MIDAS and PSQI scores among participants with migraine.
Multivariate linear regression analysis of sleep quality on migraine severity, represented as the MIDAS, is shown in Table 7. In total, three models were constructed based on the results of the univariate regression analysis, literature, and the clinical significance of these factors. This analysis revealed that the PSQI score under no-adjustment conditions, as in Model 1, was insignificant in predicting migraine severity. After adjusting for smoking, as in Model 2, a significant association between smoking and migraine severity was detected, whereby an incremental increase in smoking worsened migraine severity by 0.108 (beta coefficient = −0.108, p < 0.042). Model 3 further illustrated the significance of smoking as a predictor of migraine severity, despite adjusting for age, sex, and BMI.
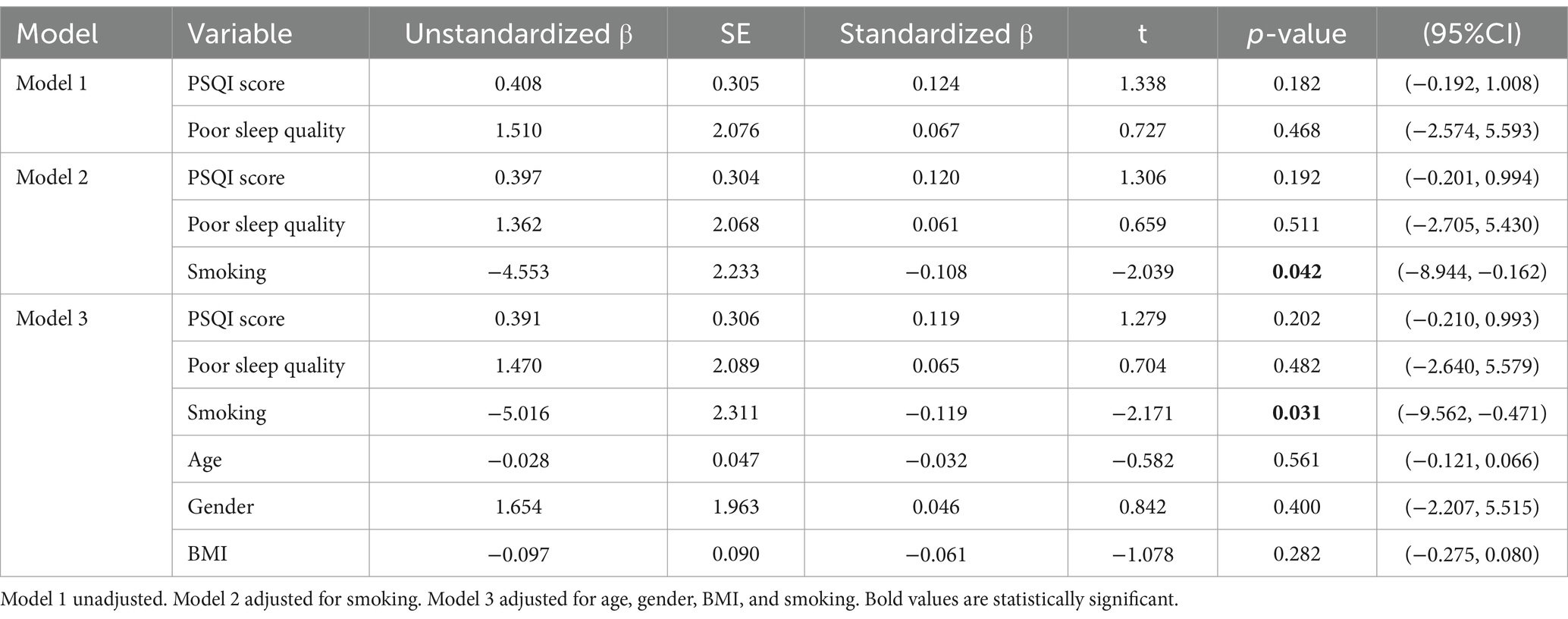
Table 7. Multivariate linear regression analysis of sleep quality on the severity of migraine (MIDAS).
Table 8 shows the results of the multivariate linear regression analysis. The MIDAS score was the only significant factor retained after univariate regression analysis for all demographics. Hence, all variables were adjusted in Model 2. A significant association between migraine severity and poor sleep quality in patients with migraine was detected in Models 1–2. For every 1-point increase in the MIDAS score (i.e., 1 day missed due to migraine headache), the PSQI score (i.e., sleeping difficulty) increased by 0.179 (beta coefficient = 0.179, p < 0.001) in all migraine patients.
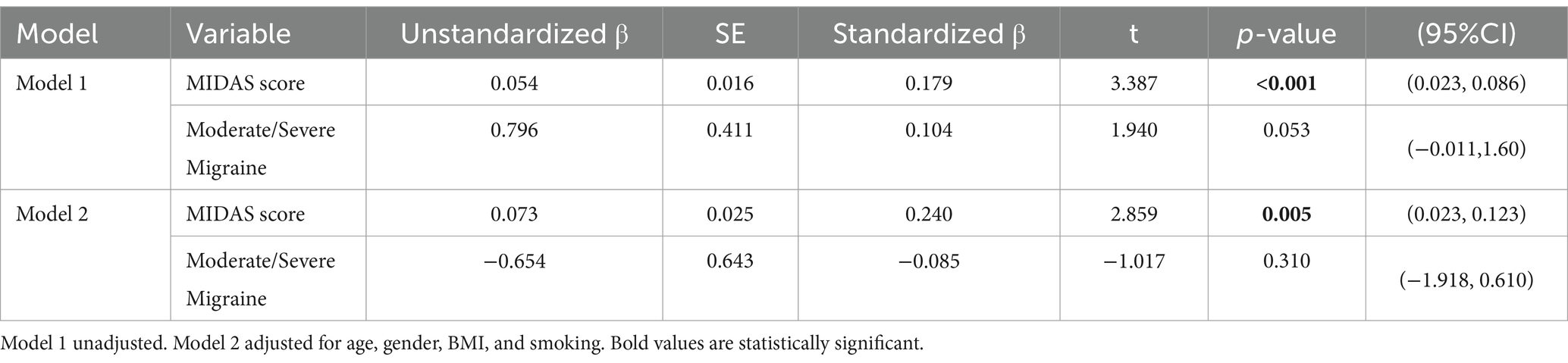
Table 8. Multivariate linear regression analysis of severity of migraine on the sleep quality (PSQI).
The relationship between migraine and sleep disturbances is complex (34). In this comparative study analyzing the association between migraine and sleep disturbance, a significant positive correlation was found between migraine severity and poor sleep quality among migraine patients. Moreover, our findings indicated that migraine severity directly influences sleep quality, emphasizing the need for integrated treatment approaches that address both sleep and migraine management. Such insights could aid in the development of more effective therapeutic strategies for improving the quality of life of individuals with migraine.
Stress is one of the most common triggers of migraine attacks, with or without aura. Although the influence of stress on the burden of migraine remains unclear, our findings demonstrate that it is more common in migraine patients who score higher on the MIDAS, indicating a possible causal relationship (35). Several studies have previously extensively investigated the influence of diet and eating habits on migraine; however, a definitive association has yet to be confirmed. Nevertheless, our findings indicate that certain foods, as well as irregular eating, can significantly influence the impact of migraine on quality of life. Additionally, food avoidance and other unhealthy eating habits are associated with stress, which negatively influences MIDAS scores (36). Pain is associated with the disruption of normal functioning in individuals with various comorbidities (37). According to Kim et al., distorted pain perception may be related to migraine-related disability. Consequently, our study showed that patients with migraine with better MIDAS scores demonstrated an ability to relieve pain (38). Headaches that trigger awakening from sleep showed a significant negative influence on MIDAS scores, which could be explained by the association between decreased REM sleep duration and the worsening of cutaneous allodynia symptoms that occur during a migraine attack, which could further reduce an individual’s quality of life (29). Finally, our study found that those with severe migraine disability had trouble falling asleep, sleep disturbances, and daytime dysfunction, further supporting the overall conclusion of this study.
The bidirectional nature of migraine and sleep quality, and the relationship thereof, have both been considerably scrutinized by researchers to uncover how sleep quality and migraine intertwine in a two-faceted manner (39–41). One case–control study in China assessed the association between migraine and sleep quality, noting that, despite the lack of a significant linear trend between poor sleep quality and MIDAS score, migraine patients with poor sleep quality showed higher MIDAS scores than those with good sleep quality (39). As such, their study successfully highlighted the unidirectional effect of sleep quality on migraine severity, which is consistent with the findings of our study. Further supporting the association between PSQI and MIDAS scores, another study showed that the MIDAS score and migraine frequency both exhibit a positive correlation with poor sleep quality (40). In contrast to the aforementioned unidirectional relationship, the extent of disability in patients with chronic migraine is thought to predict poor sleep quality (41). Contrary to expectations, our study failed to establish any bidirectional correlation between the MIDAS and PSQI scores, and a significant difference between the two MIDAS groups in terms of PSQI score was not observed, regardless of the MIDAS grade group.
The theory that smoking could be implicated in the precipitation and worsening of migraine has been investigated in several studies. Interestingly, the findings of these studies were inconsistent, as some studies found an association between smoking and migraine (42–45), whereas others found no association (46). For example, an association was identified between smoking habits and the prevalence of migraine. Smokers who consumed more cigarettes per day were found to have higher odds of experiencing migraine headaches, indicating that increased smoking frequency heightened the risk (42). Migraine patients with a high frequency of attacks (i.e., more than one attack per month) were significantly more prevalent in smokers (77%) than in nonsmokers (56%). Additionally, among students who were both smokers and migraine patients, 71% thought that smoking worsened migraine, while 59% thought that smoking precipitated migraine attacks, which agrees with our research findings (43). Furthermore, smoking >10 cigarettes per day was significantly related to migraine, with a higher severity of headaches reported among smokers than among nonsmokers (45).
Despite a vast wealth of scientific evidence, the correlation between sleep quality and migraine severity remains equivocal (34). One meta-analysis of 21 studies examining the relationship between the PSQI and MIDAS identified only a small insignificant effect size, rendering such a relationship non-existent (29). In the multivariate regression analysis of a study conducted on 120 migraine patients in Turkey, PSQI was found to be a significant determinant of MIDAS, in which a higher PSQI score resulted in more severe migraine attacks (47). Similarly, Safak et al. conducted a study on 150 migraine patients, in which they found that the PSQI was higher among migraine participants than among their non-migraine counterparts (48). With that said, the present study, having the largest sample size of migraine patients among the above-mentioned studies, illustrated that the PSQI score, in the presence or absence of adjustment conditions, cannot be confidently recommended as a tool to predict migraine severity.
A scientific study conducted in China with a sample of 134 individuals with migraine revealed a strong influence of sleep on the migraine-related burden between sleep quality and migraine-related burden (39). Previous studies have suggested that sleep, as the culprit, plays a significant role in increasing MIDAS scores, and may further contribute to the occurrence of migraine attacks, while other studies have suggested a bidirectional relationship between sleep quality and migraine (16, 49). Similarly, one systematic review published in 2020 acknowledged that despite extensive research, the exact nature of this connection remains elusive, with migraine potentially arising from sleep disturbances and sleep disruptions potentially triggering migraine (50). However, our study provides further evidence of the significant impact of migraine severity, as measured by the MIDAS score, on sleep quality. This finding supports the notion that migraine acts as an obstacle to achieving a restful sleep pattern, and confirms the directionality of this relationship.
All studies have limitations, and our study is no exception. One limitation of this study was that all components of sleep quality are merely subjective self-assessments without utilizing tools, such as polysomnography (PSG), to assess the parameters of sleep. Similarly, MIDAS was advantageous in addressing paid work or school/work, leisure time, and household responsibilities, which are all aspects that can be affected by migraine. A disadvantage of MIDAS, however, was for patients who do not vividly recall the necessary components that are assessed by MIDAS, such as the severity or the frequency of certain questions, thus leaving room for under or overestimation. Moreover, respiratory and sleep disorders, like COVID-19 and Obstructive Sleep Apnea (OSA), which can be potential influencers of sleep and headache, were not investigated (51, 52). A further limitation is that we collected the data of our participants through surveys; therefore, our survey was not accessible to individuals without internet access or devices necessary for participation. As with many cross-sectional studies, it is imperative to be aware of the limitations of the results in predicting outcomes. For example, establishing a true cause-and-effect relationship without longitudinal data is impossible. Nevertheless, this study provided considerable insight into the direct relationship between migraine severity and sleep quality.
The findings of this study suggest a notable correlation between poor sleep quality and increased migraine severity. Migraine severity is a predictor of poor sleep quality. This study underscores the need for integrated treatment approaches that combine migraine management and strategies to improve sleep quality. Future research should investigate the causal mechanisms and explore whether interventions targeting sleep disturbance can effectively reduce migraine severity. Smoking negatively affected migraine severity. As such, a definite understanding of the impact of lifestyle factors on migraine severity is crucial for enhancing the quality of life of migraine patients.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by the Institutional Review Board at King Abdullah International Medical Research Center (KAIMRC; Approval number: NRC23R/470/06). Written informed consent to participate in this study was provided by the patients/participants or patients/participants’ legal guardian/next of kin in accordance with the national legislation and the institutional requirements.
NA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. SA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. RA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. NNA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. YA: Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing, Conceptualization, Data curation. FA: Supervision, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors wish to thank the volunteers involved in the study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
IHS, International Headache Society criteria; MIDAS, Migraine Disability Assessment Scale; PSQI, Pittsburgh Sleep Quality Index; GBD, Global Burden of Disease; BMI, Body Mass Index; SPSS, Statistical Package for the Social Sciences; SD, Standard Deviation; IAU, Imam Abdulrahman bin Faisal University; C, Component; Kg, Kilograms; CI, Confidence interval; COVID-19, Coronavirus disease of 2019.
1. Olesen, J, Bes, A, Kunkel, R, Lance, JW, Nappi, G, Pfaffenrath, V, et al. The international classification of headache disorders. Cephalalgia. (2013) 33:629–808. doi: 10.1177/0333102413485658
2. Stovner, LJ, Nichols, E, Steiner, TJ, Abd-Allah, F, Abdelalim, A, Al-Raddadi, RM, et al. Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol. (2018) 17:954–76. doi: 10.1016/S1474-4422(18)30322-3
3. The World Health Organization. The World Health Report (2001). Available from: http://www.who.int/whr/2001/en/index.html (cited 2023 Apr 14)
4. Steiner, TJ, Stovner, LJ, and Vos, T. GBD 2015: Migraine is the third cause of disability in under 50s. J Headache Pain. (2016) 17:699. doi: 10.1186/s10194-016-0699-5
5. Duman, T, Dede, OH, Uluduz, D, Seydaoglu, G, Okuyucu, E, and Melek, I. Sleep changes during prophylactic treatment of migraine. Ann Indian Acad Neurol. (2015) 18:298–302. doi: 10.4103/0972-2327.160084
6. Krueger, JM, Frank, MG, Wisor, JP, and Roy, S. Sleep function: Toward elucidating an enigma. Sleep Med Rev. (2016) 28:46–54. doi: 10.1016/j.smrv.2015.08.005
7. Irwin, MR. Why sleep is important for health: a psychoneuroimmunology perspective. Annu Rev Psychol. (2015) 66:143–72. doi: 10.1146/annurev-psych-010213-115205
8. Denison, HJ, Jameson, KA, Sayer, AA, Patel, HP, Edwards, MH, Arora, T, et al. Poor sleep quality and physical performance in older adults. Sleep Health. (2021) 7:205–11.
9. Barbato, G. REM sleep: an unknown indicator of sleep quality. Int J Environ Res Public Health MDPI. (2021) 18:12976. doi: 10.3390/ijerph182412976
10. Zeitlhofer, J, Schmeiser-Rieder, A, Tribl, G, Rosenberger, A, Bolitschek, J, and Kapfhammer, G, et al. Sleep and quality of life in the Austrian population. Acta Neurol Scand. (2000) 102:249–57. doi: 10.1034/j.1600-0404.2000.102004249.x
11. Smitherman, TA. Foreword: Special collection on sleep disorders and migraine. Headache. (2018) 58:1028–9. doi: 10.1111/head.13349
12. Rafique, N, Al-Asoom, LI, Latif, R, Alsunni, AA, Salem, AM, Alkhalifa, ZH, et al. Prevalence of migraine and its relationship with psychological stress and sleep quality in female university students in Saudi Arabia. J Pain Res. (2020) 13:2423–30. doi: 10.2147/JPR.S270847
13. Paiva, T, Batista, A, and Martins, P. The Relationship Between Headaches and Sleep Disturbances. Headache. (1995) 35:590–6. doi: 10.1111/j.1526-4610.1995.hed3510590.x
14. Smitherman, TA, Kuka, AJ, Calhoun, AH, Walters, ABP, Davis-Martin, RE, Ambrose, CE, et al. Cognitive-behavioral therapy for insomnia to reduce chronic migraine: a sequential Bayesian analysis. Headache. (2018) 58:1052–9. doi: 10.1111/head.13313
15. Proserpio, P, and Agostoni, EC. Sleep and migraine. Neurol Sci. (2020) 41:437–8. doi: 10.1007/s10072-020-04644-7
16. Cho, S, Lee, MJ, Park, HR, Kim, S, Joo, EY, and Chung, CS. Effect of sleep quality on headache-related impact in primary headache disorders. J Clinical Neurol. (2020) 16:237–44. doi: 10.3988/jcn.2020.16.2.237
17. Saunders, K, Merikangas, K, Low, NCP, Korff, M, and Kessler, R. Impact of comorbidity on headache-related disability. Neurology. (2008) 70:538–47. doi: 10.1212/01.wnl.0000297192.84581.21
18. Buse, DC, Silberstein, SD, Manack, AN, Papapetropoulos, S, and Lipton, RB. Psychiatric comorbidities of episodic and chronic migraine. J Neurol. (2013) 260:1960–9. doi: 10.1007/s00415-012-6725-x
19. Schürks, M, Rist, PM, Bigal, ME, Buring, JE, Lipton, RB, and Kurth, T. Migraine and cardiovascular disease: systematic review and meta-analysis. BMJ. (2009) 339:b3914. doi: 10.1136/bmj.b3914
20. Rains, JCStudy group Aydinkoc PK. ABSTRACTS Quality of Sleep, Fatigue and Daytime Sleepiness in Migraine-A Controlled Study. Vienna, Austria: Cephalalgia. (2009).
21. Kelman, L, and Rains, JC. Headache and Sleep: Examination of Sleep Patterns and Complaints in a Large Clinical Sample of Migraineurs. Headache. (2005) 45:904–10. doi: 10.1111/j.1526-4610.2005.0519.x
22. Parashar, R, Bhalla, P, Rai, NK, Pakhare, A, and Babbar, R. Migraine: is it related to hormonal disturbances or stress? Int J Women's Health. (2014) 6:921–5. doi: 10.2147/IJWH.S62922
23. Seidel, S, Hartl, T, Weber, M, Matterey, S, Paul, A, Riederer, F, et al. Quality of sleep, fatigue and daytime sleepiness in migraine - a controlled study. Cephalalgia. (2009) 29:662–9. doi: 10.1111/j.1468-2982.2008.01784.x
24. Zhu, Z, Fan, X, Li, X, Tan, G, Chen, L, and Zhou, J. Prevalence and predictive factors for poor sleep quality among migraineurs in a tertiary hospital headache clinic. Acta Neurol Belg. (2013) 113:229–35. doi: 10.1007/s13760-012-0159-1
25. Rasmussen, BK. Migraine and tension-type headache in a general population: precipitating factors, female hormones, sleep pattern and relation to lifestyle. Pain. (1993) 53:65–72. doi: 10.1016/0304-3959(93)90057-V
26. Fox, AW. Migraine Chronobiology. RL Davis, editor. Headache. (1998) 38:436–41. doi: 10.1046/j.1526-4610.1998.3806436.x
27. Bruni, O, Russo, PM, Violani, C, and Guidetti, V. Sleep and migraine: an actigraphic study. Cephalalgia. (2004) 24:134–9. doi: 10.1111/j.1468-2982.2004.00657.x
28. Naughton, F, Ashworth, P, and Skevington, SM. Does sleep quality predict pain-related disability in chronic pain patients? The mediating roles of depression and pain severity. Pain. (2007) 127:243–52. doi: 10.1016/j.pain.2006.08.019
29. Stanyer, EC, Creeney, H, Nesbitt, AD, Holland, PR, and Hoffmann, J. Subjective sleep quality and sleep architecture in patients with migraine: a Meta-analysis. Neurology. (2021) 97:e1620–31. doi: 10.1212/WNL.0000000000012701
30. Olesen, J, and Lipton, RB. Headache classification update 2004. Curr Opin Neurol. (2004) 17:275–82. doi: 10.1097/00019052-200406000-00007
31. Mourad, D, Hajj, A, Hallit, S, Ghossoub, M, and Khabbaz, LR. Validation of the Arabic version of the migraine disability assessment scale among Lebanese patients with migraine. J Oral Facial Pain Headache. (2019) 33:47–53. doi: 10.11607/ofph.2102
32. Stewart, WF, Lipton, RB, Dowson, AJ, and Sawyer, J. Development and testing of the migraine disability assessment (MIDAS) questionnaire to assess headache-related disability. Neurology. (2001) 56:S20–8. doi: 10.1212/wnl.56.suppl_1.s20
33. Suleiman, KH, Yates, BC, Berger, AM, Pozehl, B, and Meza, J. Translating the Pittsburgh sleep quality index into Arabic. West J Nurs Res. (2010) 32:250–68. doi: 10.1177/0193945909348230
34. Waliszewska-Prosół, M, Nowakowska-Kotas, M, Chojdak-Łukasiewicz, J, and Budrewicz, S. Migraine and sleep-an unexplained association? Int J Mol Sci. (2021) 22:5539. doi: 10.3390/ijms22115539
35. Stubberud, A, Buse, DC, Kristoffersen, ES, Linde, M, and Tronvik, E. Is there a causal relationship between stress and migraine? Current evidence and implications for management. J Headache Pain. (2021) 22:155. doi: 10.1186/s10194-021-01369-6
37. Pradeep, R, Nemichandra, SC, Harsha, S, and Radhika, K. Migraine disability, quality of life, and its predictors. Ann Neurosci. (2020) 27:18–23. doi: 10.1177/0972753120929563
38. Kim, S, Bae, DW, Park, SG, and Park, JW. The impact of pain-related emotions on migraine. Sci Rep. (2021) 11:577. doi: 10.1038/s41598-020-80094-7
39. Duan, S, Ren, Z, Xia, H, Wang, Z, Zheng, T, and Liu, Z. Association between sleep quality, migraine and migraine burden. Front Neurol. (2022) 13:955298. doi: 10.3389/fneur.2022.955298
40. Singh, R, Joshi, A, Gupta, A, Mitra, A, and Kumar, RN. Exploratory study to understand association of emotional comorbidities and sleep with migraine. Int J Neurosci. (2022) 132:985–93. doi: 10.1080/00207454.2020.1858830
41. Garrigós-Pedrón, M, Segura-Ortí, E, Gracia-Naya, M, and La Touche, R. Predictive factors of sleep quality in patients with chronic migraine. Neurologia (Engl Ed). (2022) 37:101–9. doi: 10.1016/j.nrl.2018.11.004
42. Sarker, MA, Rahman, M, Harun-Or-Rashid, M, Hossain, S, Kasuya, H, Sakamoto, J, et al. Association of smoked and smokeless tobacco use with migraine: a hospital-based case-control study in Dhaka, Bangladesh. Tob Induc Dis. (2013) 11:15. doi: 10.1186/1617-9625-11-15
43. López-Mesonero, L, Márquez, S, Parra, P, Gámez-Leyva, G, Muñoz, P, and Pascual, J. Smoking as a precipitating factor for migraine: a survey in medical students. J Headache Pain. (2009) 10:101–3. doi: 10.1007/s10194-009-0098-2
44. Tietjen, GE, Brandes, JL, Peterlin, BL, Eloff, A, Dafer, RM, Stein, MR, et al. Allodynia in migraine: association with comorbid pain conditions. Headache. (2009) 49:1333–44. doi: 10.1111/j.1526-4610.2009.01521.x
45. Vlajinac, H, Šipetić, S, Džoljić, E, Maksimović, J, Marinković, J, and Kostić, V. Some lifestyle habits of female Belgrade university students with migraine and non-migraine primary headache. J Headache Pain. (2003) 4:67–71. doi: 10.1007/s10194-003-0033-x
46. Nazari, F, Safavi, M, and Mahmudi, M. Migraine and its relation with lifestyle in women. Pain Pract. (2010) 10:228–34. doi: 10.1111/j.1533-2500.2009.00343.x
47. Sengul, Y, Sengul, HS, Bakim, B, Yucekaya, SK, Yucel, S, and Akgun, M. Sleep disturbances and excessive daytime sleepiness in migraine: a comparison between comorbidities and disability. Sleep Biol Rhythms. (2015) 13:76–84. doi: 10.1111/sbr.12087
48. Şafak, D, Korkmazer, B, and Şahin, EM. The association between migraine and sleep quality. Konuralp Medical J. (2022) 14:124–31. doi: 10.18521/ktd.765038
49. Yang, CP, and Wang, SJ. Sleep in patients with chronic migraine. Curr Pain Headache Rep. (2017) 21:39. doi: 10.1007/s11916-017-0641-9
50. Tiseo, C, Vacca, A, Felbush, A, Filimonova, T, Gai, A, Glazyrina, T, et al. European headache Federation School of Advanced Studies (EHF-SAS). Migraine and sleep disorders: a systematic review. J Headache Pain. (2020) 21:126. doi: 10.1186/s10194-020-01192-5
51. Stewart, WF, Lipton, RB, Kolodner, K, Liberman, J, and Sawyer, J. Reliability of the migraine disability assessment score in a population-based sample of headache sufferers. Cephalalgia. (1999) 19:107–14. doi: 10.1046/j.1468-2982.1999.019002107.x
Keywords: sleep quality, migraine, Pittsburgh Sleep Quality Index, migraine disability assessment scale, association, migraine severity, sleep disorders, migraine prevalence
Citation: Almansour NA, Alsalamah SS, Alsubaie RS, Alshathri NN, Alhedyan YA and Althekair FY (2025) Association between migraine severity and sleep quality: a nationwide cross-sectional study. Front. Neurol. 16:1529213. doi: 10.3389/fneur.2025.1529213
Received: 16 November 2024; Accepted: 08 January 2025;
Published: 31 January 2025.
Edited by:
Vincenzo Guidetti, Sapienza University of Rome, ItalyReviewed by:
Cherubino Di Lorenzo, Sapienza University of Rome, ItalyCopyright © 2025 Almansour, Alsalamah, Alsubaie, Alshathri, Alhedyan and Althekair’s. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Razan S. Alsubaie, QWxzdWJhaWUxOTVAa3NhdS1ocy5lZHUuc2E=
†ORCID: Nura A. Almansour, https://orcid.org/0000-0005-2443-1299
Seham S. Alsalamah, https://orcid.org/0000-0002-7792-459X
Razan S. Alsubaie, https://orcid.org/0009-0001-6663-2348
Nada N. Alshathri, https://orcid.org/0009-0006-1942-418X
Yasmeen A. Alhedyan, https://orcid.org/0009-0001-8465-548X
Faisal Y. Althekair’s, https://orcid.org/0009-0007-7105-6692
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.