- Department of Rehabilitation, Shunyi Hospital, Beijing Hospital of Traditional Chinese Medicine, Beijing, China
Stroke patients are susceptible to malnutrition as a result of dysphagia, neurological impairments, and altered levels of consciousness. The nutritional status of individuals post-stroke is a critical determinant influencing the efficacy of rehabilitation outcomes. Therefore, there is great interest in the possible role of nutrients in promoting recovery after stroke. This article examines the enhancement of rehabilitation outcomes through the improvement of nutritional status. A comprehensive literature search was conducted using the PubMed, Cochrane, Web of Science, and Embase databases. Articles relevant to this topic, published from the inception of each database until November 2024, were identified. The selection was restricted to randomized controlled clinical trials, irrespective of language or publication date. The search specifically targeted studies involving stroke patients, encompassing both hemorrhagic and ischemic types, and interventions that combined nutritional supplementation with rehabilitation therapy. Studies with a focus on stroke prevention were excluded. Full-text articles that met the inclusion criteria were retrieved from the aforementioned sources. In instances where both a full report and a conference abstract were available for the same study, only the full report was considered. A total of 751 studies were considered for inclusion in this scoping review. Following a rigorous screening process, 13 studies were selected for detailed analysis. All selected studies were randomized controlled clinical trials. The findings indicate that supplementation with nutrients such as proteins, vitamins, essential amino acids, and antioxidants can enhance activities of daily living, improve balance function, and reduce neurological deficits in post-stroke patients. This review aims to synthesize current evidence regarding the effects of various nutrients and dietary regimens on limb rehabilitation in post-stroke patients, with the goal of providing new insights to facilitate the accelerated recovery of this population.
1 Introduction
Globally, one in four people will have a stroke in their lifetime, making strokes the second most common cause of death and the third most common cause of disability (1, 2). Since 2015, stroke has become the leading cause of death and disability in China. As a major chronic non-communicable disease, it poses a serious threat to national health. Over the past decade, stroke prevalence, recurrence, and mortality in China have steadily increased (3).
According to Global Burden of Disease (GBD) data, the prevalence of ischemic stroke in China increased from 1,100 per 100,000 individuals in 2010 to 1,256 per 100,000 individuals in 2019. The 12-month stroke recurrence rate among stroke survivors was reported to be 5.7%. The “China Health Statistics Yearbook 2020” indicates that the crude mortality rate of stroke in China in 2019 ranged from 129.41 to 158.63 per 100,000 individuals (3). The average age of stroke patients in China is approximately 65 years, which is notably lower than the average age of around 75 years in developed countries (4). Additionally, malnutrition is prevalent among elderly Chinese stroke patients and is associated with increased mortality (5). Malnutrition negatively impacts the rehabilitation outcomes of patients recovering from stroke and hinders the enhancement of their daily living abilities. Addressing malnutrition is essential for stroke recovery, as improving nutritional status may contribute to the rehabilitation process. Nevertheless, a direct causal relationship between nutritional status and rehabilitation efficacy has yet to be definitively established. To investigate whether enhancing the nutritional status of post-stroke patients could potentially improve rehabilitation outcomes, we conducted this scoping review.
1.1 Stroke patients at risk of malnutrition
Studies have found that both acute stroke patients and stroke survivors have certain nutritional risks and deficiencies. Based on the third national stroke registry data, 1.95 to 5.89% of acute stroke patients in China had moderate to severe malnutrition risk. The risk of malnutrition in acute stroke patients is associated with an increased risk of long-term death and severe disability (6). A randomized controlled trial (RCT) involving 323 participants demonstrated that the incidence of anemia among stroke patients during the recovery phase was 42.4%. Additionally, the incidence rates of total protein, albumin, and prealbumin levels falling below normal were 8, 17, and 31.9%, respectively (7). These findings indicate that stroke patients experience significant nutritional deficiencies. Furthermore, a meta-analysis encompassing 915 subjects revealed that malnutrition is particularly prevalent in patients with ischemic stroke and is independently correlated with an elevated risk of stroke-related pneumonia (8).
1.2 Stroke patients with malnutrition may have a poor prognosis
Malnutrition is an independent risk factor for poor prognosis in stroke patients (9). There are many problems associated with malnutrition, including imbalances in energy, protein, vitamins and minerals, loss of self-care ability, prolonged hospitalization, poor functional prognosis, and increased mortality (10, 11). Gomes et al. (12) determined that the risk of malnutrition, as assessed by the Malnutrition Universal Screening Tool (MUST), serves as an independent predictor of mortality, service level, and hospitalization costs within 6 months post-stroke. The most apparent manifestation of malnutrition is weight loss. Specifically, a weight reduction exceeding 3 kg following a stroke significantly elevates the risk of mortality in both the short and long term. Early intervention in such cases can substantially enhance clinical outcomes for patients (13). Nishioka et al. (14) conducted a cross-sectional survey involving 178 stroke recovery patients aged 65 and above, revealing that the enhancement of nutritional status in elderly stroke patients experiencing malnutrition during the recovery phase is associated with significant improvements in daily living activities. Similarly, in patients experiencing acute stroke, malnutrition has been found to be negatively correlated with activities of daily living (ADL) (15).
The extent of neurological deficits following a stroke is positively correlated with the degree of subsequent nutritional deterioration. This decline in nutritional status impedes neurological recovery, elevates the incidence of complications, increases hospitalization costs, and extends the duration of hospital stays (16). A RCT study (n = 277) found that the Geriatric Nutrition Risk Index (GNRI) score at admission was closely related to the neurological function 3 months after stroke. The higher the GNRI nutritional risk level, the worse the neurological prognosis in the recovery period (17).
1.3 Stroke patients’ risk factors for malnutrition
Numerous risk factors contribute to malnutrition in stroke patients, including swallowing disorders, neurological deficits, impaired consciousness, advanced age, female sex, pre-existing malnutrition, suboptimal family conditions or inadequate care, the presence of malignant tumors, delayed initiation of rehabilitation, and a history of severe alcoholism (18–20). Additionally, factors such as polypharmacy, feeding difficulties, chronic diseases, functional impairments, and elevated National Institutes of Health Stroke Scale (NIHSS) scores at admission are correlated with an increased risk of malnutrition in this patient population. Dysphagia is identified as the primary risk factor for malnutrition in patients who have experienced a stroke (12).
2 Methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Extension for Scoping Reviews statement was followed to report in this study.
2.1 Search strategy
An exhaustive search of the literature was conducted by a medical librarian (FWH) in the Cochrane Library, Ovid Embase, PubMed and Web of Science Core Collection databases to find relevant articles published from earliest database record to 25 November 2024. Databases were searched using a combination of controlled and free text terms for Strokes/Cerebrovascular Accidents, Nutrients, rehabilitation. Randomized controlled clinical trials were exclusively selected for inclusion, regardless of the language or date of publication.
2.2 Study selection
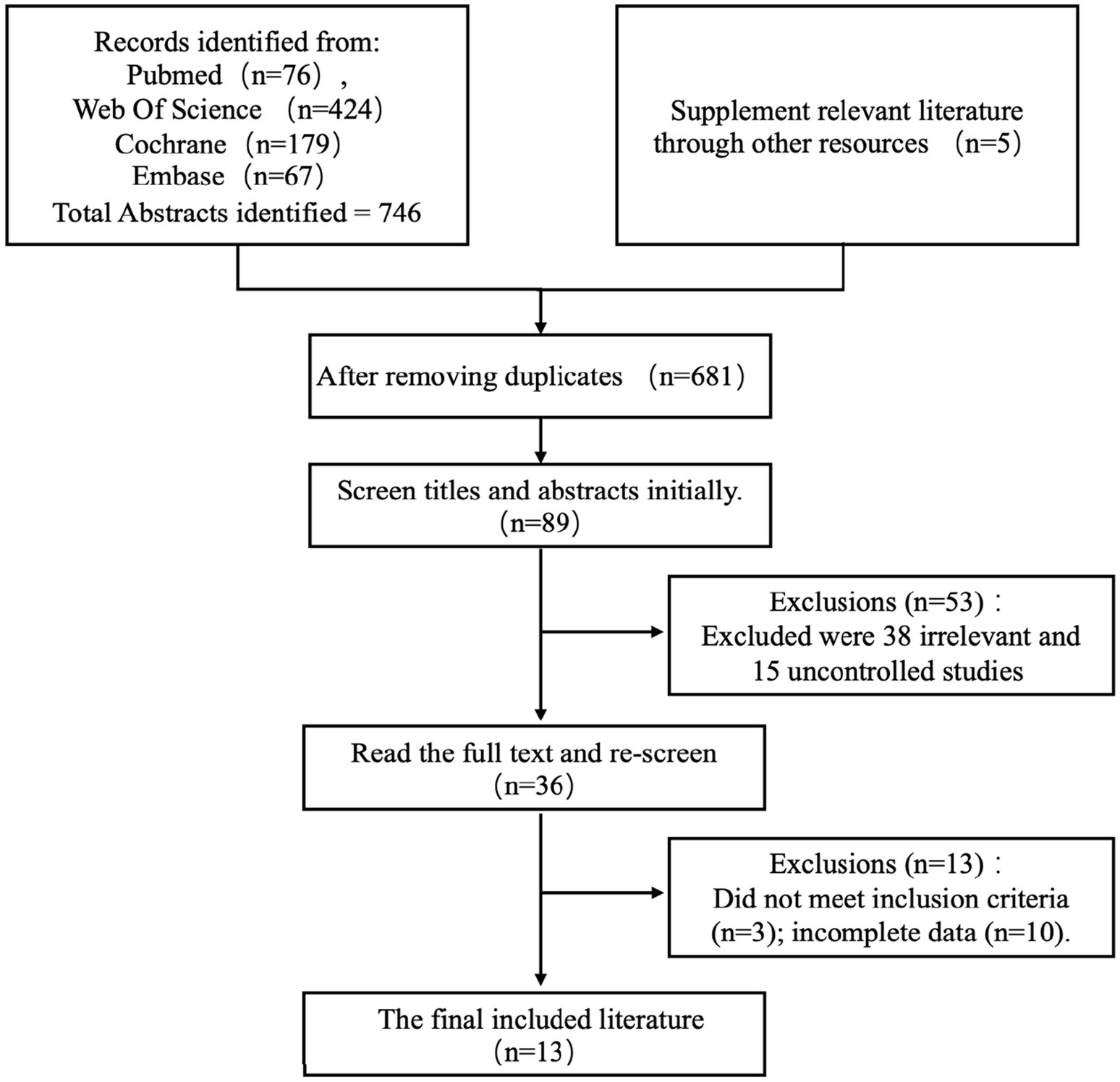
Citations from all databases were imported into the Endnote 20 library (Clarivate Analytics, Philadelphia, PA, United States). Two reviewers (CH and FCH) meticulously evaluated the collected titles and structured abstracts based on predefined criteria. The search was confined to studies involving patients who had experienced a stroke, encompassing both hemorrhagic and ischemic types, and interventions that integrated nutritional supplementation with rehabilitation therapy. Studies focused on stroke prevention were excluded. Complete articles that satisfied the selection criteria were obtained from the aforementioned sources. No exclusion criteria were applied regarding language or year of publication. In instances where both a full report and a conference abstract were available for the same study, only the full report was included. The suitability of articles for the final review was determined by two reviewers, with any disagreements resolved through consultation with a third reviewer (ZH). The selection process was guided by a PRISMA flow diagram (Figure 1).
Our search initially identified 751 titles. Following the removal of duplicates, 681 studies underwent detailed examination. From these, 36 reports, comprising both articles and abstracts, were selected for further consideration, and ultimately, 13 randomized controlled clinical trials were included in the final review. Three reviewers (CH, FCH, FWH) extracted and summarized the data into a table (Table 1).
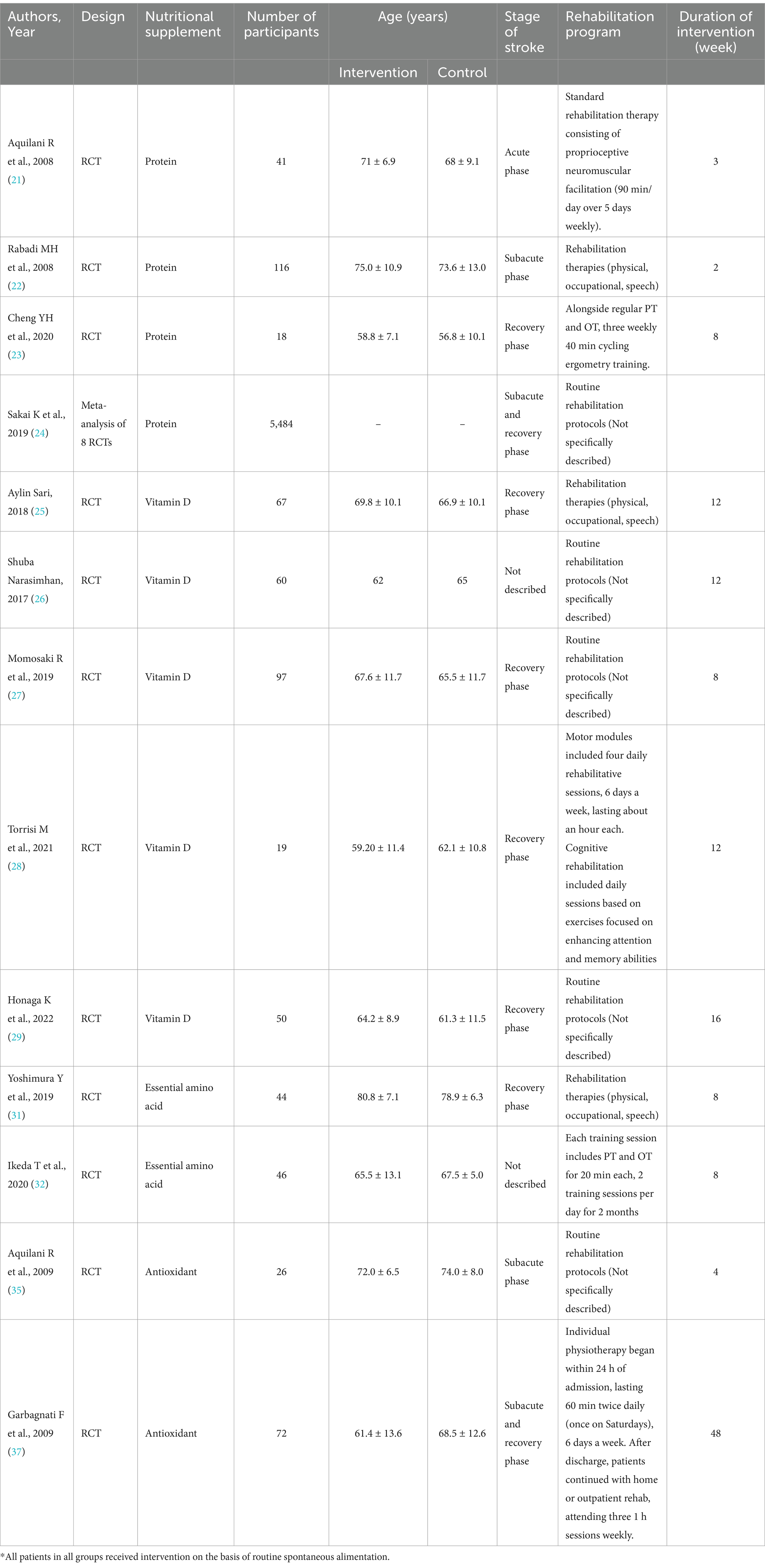
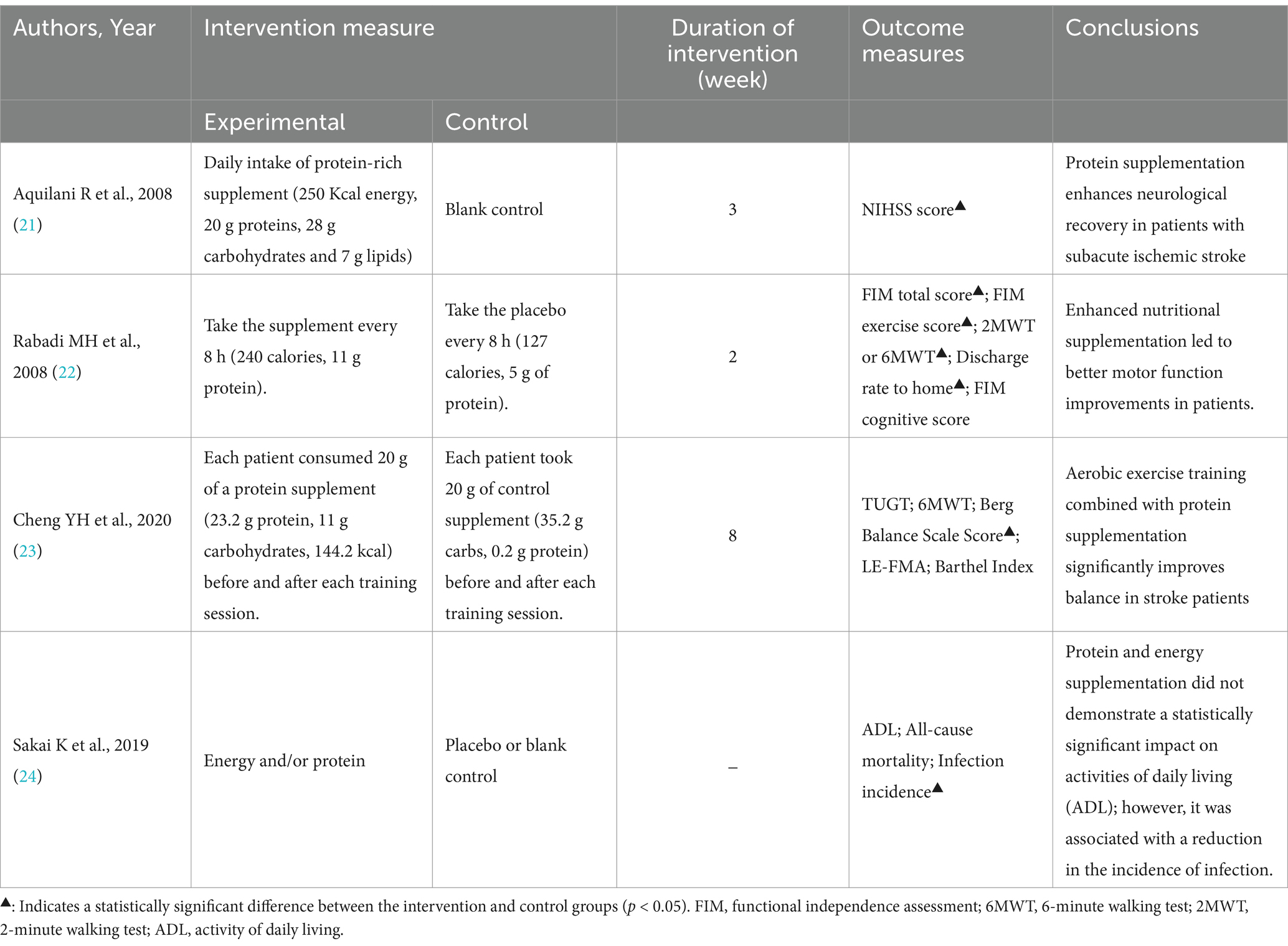
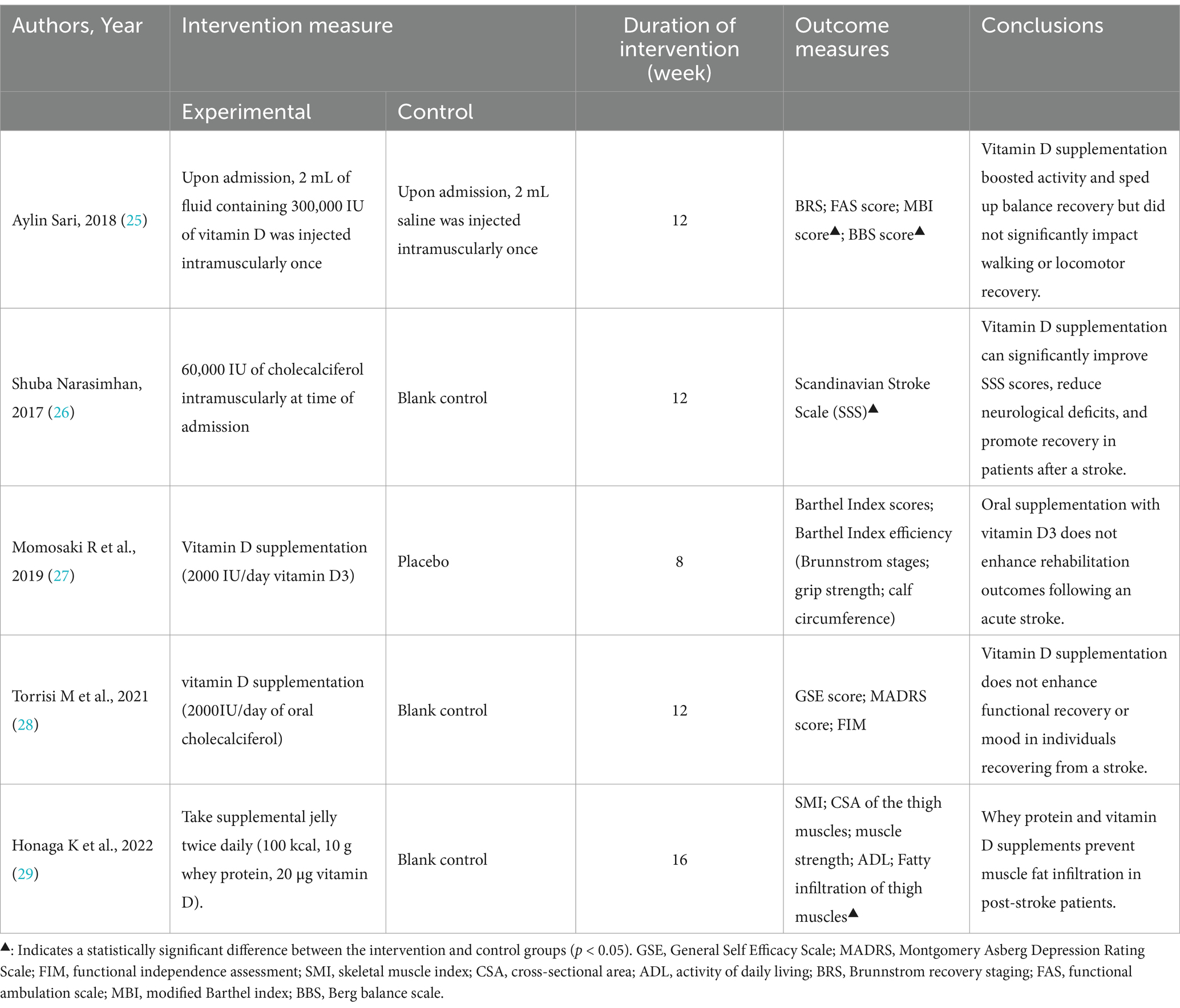
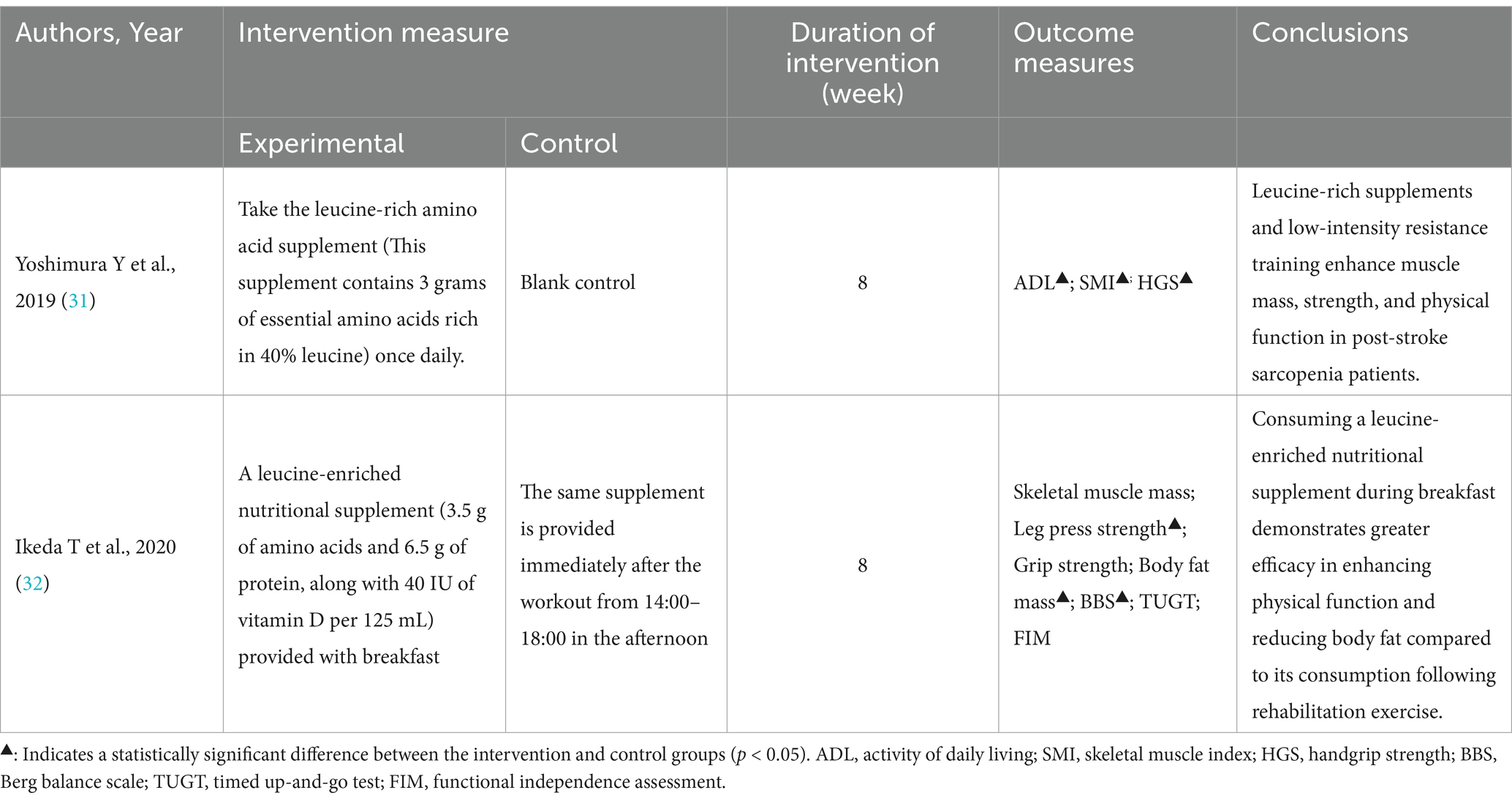
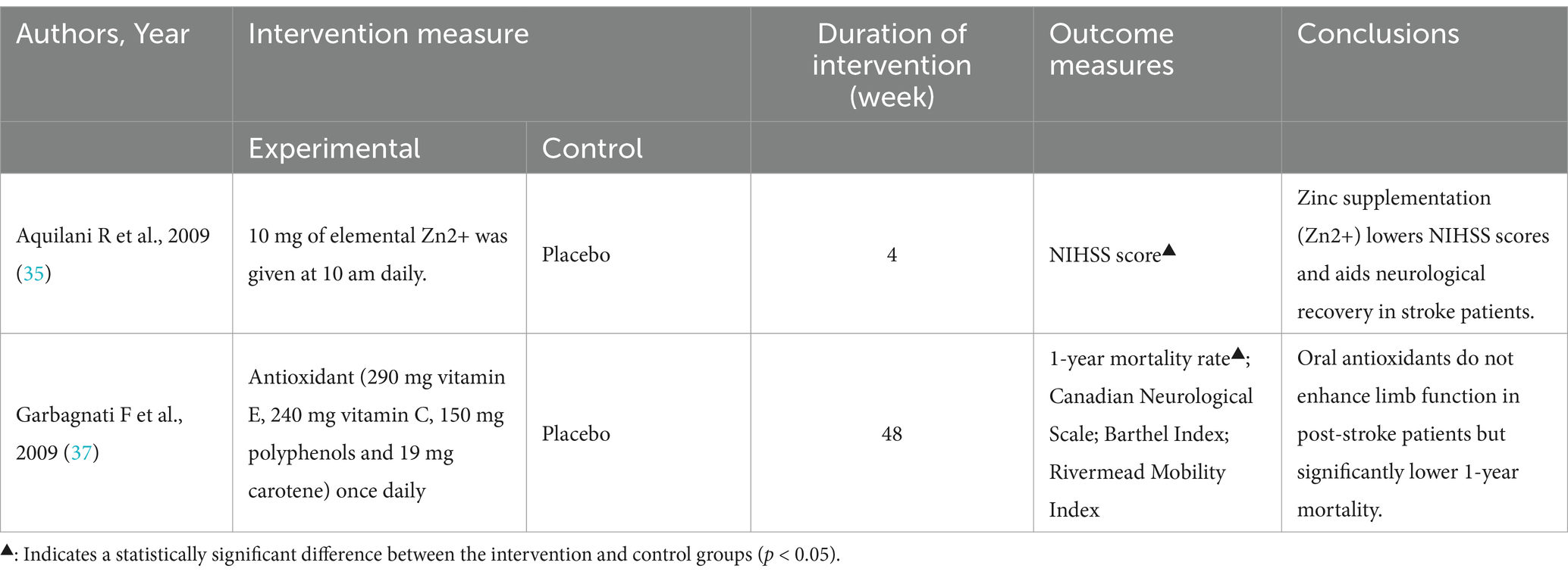
Table 1. Summary of studies reporting the effects of nutritional supplements on rehabilitation outcomes in stroke patients.
3 Results
Patients with ischemic stroke exhibit a high prevalence of malnutrition or are at significant risk for developing malnutrition. It is imperative to conduct nutritional risk screening and initiate early intervention promptly upon hospital admission. Emphasis should be placed on the nutritional management and support of these patients (16). Numerous randomized controlled trials (RCTs) have shown that providing nutritional support to stroke patients can significantly improve rehabilitation outcomes, such as improving limb mobility and cognitive levels in post-stroke patients, reducing infection risks, and NIHSS scores.
3.1 Protein
Whether protein supplementation can enhance neurological recovery in patients with subacute ischemic stroke, a randomized controlled trial (RCT) was conducted. The study randomly assigned diet-independent ischemic stroke patients to either a 21-day protein supplementation group (n = 20) or a natural diet control group (n = 21). Neurological recovery was assessed using the National Institutes of Health Stroke Scale (NIHSS). The findings indicated that increased protein intake was associated with a reduction in NIHSS scores among post-stroke patients (21). Another RCT showed that malnourished stroke patients receiving enhanced nutritional supplementation had improved motor function (total Functional Independence Measure (FIM) scores, FIM motor subscores, 2 min and 6 min timed walk tests, all significant p < 0.002) compared with patients receiving standard supplementation; however, there was no improvement in cognitive measures (FIM cognitive score) (22). Similar findings were reported in another RCT, which indicated that aerobic exercise training combined with protein supplementation can significantly enhance balance and motor coordination in stroke patients, as well as improve their daily living abilities (23).
A meta-analysis (RCT = 8, n = 5,484) published in 2019 demonstrated that, in comparison to rehabilitation alone, the integration of high-energy, high-protein dietary supplementation with rehabilitation significantly reduces the risk of infections, including pneumonia. However, this intervention did not yield a significant improvement in activities of daily living (ADL) (24). Further research, comprising more extensive and higher-quality randomized controlled trials, is necessary to elucidate the effects of protein supplementation on the rehabilitation outcomes of post-stroke patients (Table 2).
3.2 Vitamins D
Researchers suggest vitamin D supplements aid stroke recovery, with low levels linked to worse outcomes. An RCT study split ischemic stroke patients with low vitamin D into two groups: one received 300,000 IU vitamin D injections, the other got saline injections. Over 3 months, their recovery was assessed using the Brunnstrom Recovery Stage, Functional Walking Scale, Modified Barthel Index, and Berg Balance Scale. The results indicated that vitamin D supplementation significantly improved patients’ Berg Balance Scale and Modified Barthel Index scores compared to the control group, but had no significant impact on the Brunnstrom Recovery Stage or Functional Walking Scale. This suggests that vitamin D enhances balance and activity levels but does not affect walking or motor recovery (25). Another RCT study showed that Vitamin D supplementation can significantly improve SSS scores, reduce neurological deficits, and promote recovery in patients after a stroke. Furthermore, another RCT indicated that vitamin D supplementation can significantly enhance Scandinavian Stroke Scale (SSS) scores, reduce neurological deficits, and facilitate recovery in post-stroke patients (26).
However, the findings of another multicenter, randomized, double-blind, placebo-controlled trial presented contrasting results. In this study, 100 patients admitted to a rehabilitation ward following an acute stroke were randomly assigned to receive either vitamin D3 (2000 IU/day) or a placebo for 8 weeks. The outcomes indicated that oral vitamin D3 supplementation did not enhance the Barthel index score, Barthel index efficiency, hand grip strength, or calf circumference post-stroke, and had no significant impact on rehabilitation outcomes (27). Additionally, oral vitamin D supplementation did not significantly improve limb function recovery or alleviate depression in post-stroke patients. This was further examined in a 12-week randomized, double-blind, parallel, single-center clinical trial. Participants in the experimental group received a daily oral dose of 2000 IU of cholecalciferol, while the control group did not receive any vitamin D supplementation. Psychological and motor outcomes were assessed through standardized text evaluations. The findings indicated that vitamin D supplementation did not exert a significant impact on mood or functional recovery during the stroke rehabilitation period (28).
Although vitamin D supplementation has not been shown to improve muscle strength and activities of daily living, oral vitamin D supplementation has been shown to inhibit fat infiltration into muscle. A randomized controlled trial (RCT) involving 50 participants examined the impact of nutritional supplementation with whey protein and vitamin D on muscle mass and muscle quality in post-stroke patients. This single-blind, placebo-controlled study allocated the 50 patients into two groups: the high-protein (HP) group received a supplemented jelly containing 100 kcal, 10 g of whey protein, and 20 μg of vitamin D, administered twice daily for up to 16 weeks, while the control group received a placebo jelly. The cross-sectional area (CSA) of the thigh muscle, skeletal muscle index (SMI), muscle strength, activities of daily living (ADL), and some nutritional indicators in the blood were measured. Although there were no significant differences in CSA and SMI between the two groups, fat infiltration of the thigh muscle was significantly lower in the HP group. There were no significant differences in muscle strength and ADL between the two groups. Whey protein and vitamin D supplementation in post-stroke patients can inhibit fat infiltration into muscle (29) (Table 3).
3.3 Essential amino acids
Elevated concentrations of essential amino acids, including glutamate, aspartate, and γ-aminobutyric acid, alongside reduced levels of glycine in plasma, are correlated with unfavorable prognoses following ischemic stroke. This observation indicates that plasma amino acid neurotransmitters may serve as viable targets for intervention aimed at enhancing outcomes in ischemic stroke patients (30). A randomized controlled trial (RCT) was conducted involving an eight-week, two-group parallel intervention with randomized control and blinded outcome assessment in 44 elderly post-stroke patients diagnosed with sarcopenia. The findings indicated that supplementation with leucine-rich amino acids led to significant improvements in Functional Independence Measure (FIM) scores and grip strength among the post-stroke patients. However, there was no significant improvement observed in the skeletal muscle mass index (SMI) (31).
The timing of essential amino acid supplementation may also facilitate recovery. A randomized controlled trial (RCT) examined the effects of the timing of branched-chain amino acid (BCAA) supplementation combined with exercise intervention on physical function in stroke patients. Participants were randomized into two groups based on the timing of supplementation: breakfast (n = 23) and post-exercise (n = 23). In the breakfast group, supplementation was administered at 08:00, whereas in the post-exercise group, supplementation was provided immediately after exercise between 14:00 and 18:00. In both cohorts, the exercise intervention was administered bi-daily over a two-month period. The findings indicated that the timing of supplementation had a comparable impact on skeletal muscle mass across both groups. However, the ingestion of branched-chain amino acids (BCAAs) at breakfast was particularly efficacious in enhancing physical function and decreasing body fat mass. These results imply that the integration of BCAA consumption at breakfast with a structured exercise regimen is effective in facilitating recovery in post-stroke patients (32) (Table 4).
3.4 Antioxidants
Oxidative stress and inflammation contribute significantly to the cascade of stroke-related malnutrition and ischemic events in the brain. Ischemic damage results in neuronal death and cerebral infarction, which, through intercellular signaling, disrupt the neuroplasticity processes essential for functional recovery facilitated by multidisciplinary rehabilitation therapy. Nutritional interventions incorporating food components with antioxidative and anti-inflammatory properties have the potential to mitigate or prevent post-stroke malnutrition. These strategies may be essential for enhancing neuroplasticity, thereby facilitating improved rehabilitation outcomes in stroke patients (33).
Zinc is an essential trace element for human survival. Zinc plays a key role in neuronal proliferation, differentiation, neuronal migration and axonal growth (34). Improving neurological function after stroke through zinc supplementation is a promising therapeutic strategy. A randomized controlled trial (RCT) was conducted to investigate the potential contribution of zinc supplementation to neurological recovery in patients with stroke and low zinc intake. Twenty-six patients with subacute stroke were randomly assigned to either a control group or a zinc supplementation group, with the latter receiving 10 mg/day of zinc. After 30 days of treatment, neurological severity was assessed using the NIH Stroke Scale (NIHSS). The findings indicated that the improvement in NIHSS scores was significantly greater in the zinc supplementation group compared to the placebo group. These results suggest that normalizing zinc intake may enhance neurological recovery in stroke patients with initially low mineral intake (35). The results of animal experiments indicate that injecting the zinc chelator ZnEDTA 14 days after middle cerebral artery occlusion (MCAO) in adult male rats significantly reduced infarct volume and neuronal damage and improved neurological function (36).
A randomized, double-blind, placebo-controlled clinical trial demonstrated that n-3 polyunsaturated fatty acids can reduce the 1-year mortality rate in post-stroke patients. However, these fatty acids did not show significant improvement in neurological function, as measured by the Canadian Neurological Scale (CNS), nor in daily living activities, as assessed by the Barthel Index (BI) and Rivermead Mobility Index (RMI). The study involved the random allocation of 72 patients (47 males; mean age 65.3 ± 12.9 years), who were admitted to a rehabilitation hospital for the sequelae of their first ischemic stroke, into four subgroups. Patients in Group 1 received daily oral antioxidants (including: 290 mg vitamin E, 240 mg vitamin C, 150 mg polyphenols and 19 mg carotene), Group 2 received n-3 polyunsaturated fatty acids, Group 3 received both supplements, and Group 4 received a placebo, all for a duration of 12 months. The results indicated a trend towards a lower mortality rate in the subgroup treated with n-3 fatty acids at the 1-year follow-up (p = 0.060). However, there were no significant differences in rehabilitation outcomes, as measured by neurological function (Canadian Neurological Scale, CNS) and activities of daily living (Barthel Index, BI; Rivermead Mobility Index, RMI), between the groups (37) (Table 5).
4 Discussion
Nutritional intervention plays a crucial role in the rehabilitation process for stroke patients. Post-stroke individuals frequently experience malnutrition, which adversely affects their physical health and impedes their rehabilitation progress (38). Consequently, nutritional intervention is essential during the rehabilitation phase. This article elucidates the substantial influence of nutrient supplementation, including protein, essential amino acids, vitamin D, and antioxidants, on the rehabilitation outcomes of stroke patients.
Currently, pharmacological interventions for cerebral infarction primarily focus on enhancing cerebral microcirculation. However, a significant proportion of patients continue to experience varying degrees of neurological dysfunction, including hemiplegia and aphasia (39). While acute thrombolysis has demonstrated efficacy, its application is constrained by a narrow therapeutic window of 3 to 6 h, thereby limiting its availability to a small subset of patients (40, 41). Consequently, the majority of individuals with cerebral infarction are likely to endure persistent neurological impairments.
Hemiplegic stroke can result in a range of muscle abnormalities, characterized by a complex interplay of denervation, disuse, inflammation, remodeling, and spasticity, which collectively lead to phenotypic changes in muscle tissue and atrophy (42). The onset of muscle atrophy following a stroke significantly impedes the patient’s rehabilitation process. Research indicates that the muscle thickness and architecture of the lower leg muscles, such as the pennation angle (PA) and fascicle length (FL), are markedly reduced on the affected side compared to the unaffected side in stroke patients. Specifically, the thickness of the soleus and gastrocnemius muscles, as well as the pennation angle of the gastrocnemius, are associated with balance and motor function (43). These findings are corroborated by a meta-analysis (RCT = 15, n = 375), which identified stroke-related sarcopenia as a contributing factor to muscle dysfunction on the hemiplegic side (44). High protein intake, particularly through whey protein or branched-chain amino acid supplements, has been shown to significantly enhance skeletal muscle protein synthesis and improve muscle tissue quality. Research indicates that amino acids can mitigate excessive muscle breakdown in post-stroke patients by inhibiting the degradation of myofibrillar protein and skeletal muscle. Supplementation with amino acids can prevent muscle atrophy and facilitate rehabilitation by enhancing physical function, muscle strength, and muscle quality and function (45). It is well-established that therapeutic exercise is frequently employed in exercise rehabilitation programs for stroke patients to enhance physical function. Through structured limb exercises and appropriate activities, patients can improve muscle strength, cardiopulmonary endurance, walking ability, and daily living skills, thereby achieving the goals of injury prevention, functional improvement, and overall health promotion (46). Research indicates that rehabilitation exercise training plays a crucial role in maintaining brain function, enhancing brain plasticity, and increasing resistance to cerebral damage such as ischemia. Prompt and proactive exercise rehabilitation following a stroke has been shown to reduce cerebral infarction volume and ischemia-induced neuronal apoptosis, facilitate the remodeling of corticospinal neurons, and promote axonal growth and dendritic branching, thereby aiding neurological function recovery (47–49). Additionally, some studies have explored the integration of rehabilitation exercise with protein or amino acid supplementation, revealing that such supplementation enhances the adaptive effects and efficacy of exercise rehabilitation (50, 51), which aligns with our findings. Rehabilitation exercise contributes to muscle tissue growth and improved muscle strength. During the rehabilitation phase, protein or amino acid supplementation provides essential substrates for muscle tissue growth, significantly enhancing the efficiency of muscle protein synthesis and improving muscle quality, thus playing a synergistic role in promoting patient recovery.
Patients experiencing residual limb dysfunction post-stroke may exhibit diminished vitamin D synthesis due to prolonged bed rest and limited exposure to sunlight and ultraviolet radiation, rendering them more vulnerable to vitamin D deficiency. Beyond its role in regulating calcium and phosphorus metabolism, vitamin D also exerts numerous non-calcemic effects, including immunomodulation, neuroprotection, oxidative stress inhibition, and the regulation of cellular proliferation and apoptosis (52). The biologically active form of vitamin D, 1,25-dihydroxyvitamin D (1,25(OH)₂D), primarily functions through its interaction with the vitamin D receptor (VDR). Research indicates that following cerebral ischemia, there is a significant upregulation of VDR expression in microglia/macrophages surrounding the infarct area. Inactivation of VDR in these cells has been shown to markedly increase infarct volume and exacerbate neurological deficits. Microglia/macrophages deficient in VDR exhibit a pronounced pro-inflammatory phenotype, characterized by the secretion of elevated levels of TNF-α and IFN-γ. Supplementation with 1,25(OH)₂D, a bioactive form of vitamin D known to activate the vitamin D receptor (VDR), has been shown to effectively enhance VDR expression and suppress the expression of ischemia-induced cytokines such as TNF-α and IFN-γ, thereby mitigating secondary brain damage (53). Additionally, another study demonstrated an association between lower serum levels of 1,25(OH)₂D and an increased risk of recurrent stroke in patients with ischemic stroke (54). The present study revealed that, compared to rehabilitation therapy alone, the administration of high-dose vitamin D via intramuscular injection, in conjunction with rehabilitation therapy upon admission, significantly ameliorated neurological deficit symptoms in patients. Conversely, oral administration of low-dose vitamin D combined with rehabilitation therapy did not yield significant improvements in the neurological deficits of stroke patients. Consequently, further research is warranted to ascertain whether varying doses and methods of vitamin D administration differentially impact the amelioration of neurological deficits in stroke patients.
Following a stroke, vascular occlusion resulting from ischemia leads to the excessive production of reactive oxygen species (ROS), with oxidative stress being implicated in exacerbating neuronal damage and contributing to significant functional impairments (55). Oxidative stress is regarded as a critical environmental factor that adversely impacts neurogenesis by inhibiting all stages of adult neurogenesis (56, 57). This study demonstrates that the combination of antioxidants and rehabilitation therapy can decrease the NIHSS score, ameliorate neurological deficit symptoms, and reduce 1-year mortality rates in post-stroke patients. The potential mechanism underlying these improvements may involve rehabilitation-induced neural structural changes, such as neural sprouting, synapse formation, and dendritic branching (58). Antioxidants, including polyunsaturated fatty acids (such as ω-3 and DHA) and Zn2+, have been shown to mitigate oxidative stress and neuroinflammation, enhance cellular signaling, activate autophagy, and influence growth factors. These compounds facilitate cellular repair and survival by inducing and activating nutritional factors, antioxidant enzymes, DNA repair enzymes, and proteins associated with mitochondrial biogenesis. This process enhances the brain’s resilience to more intense stress when exposed to heightened stimulation (59–61). Consequently, the integration of antioxidants with rehabilitative exercise may promote cerebral remodeling and ameliorate neurological deficits following a stroke.
This study investigated the synergistic effects of rehabilitation exercise and nutritional supplementation, including protein, essential amino acids, vitamin D, and antioxidants, on enhancing exercise rehabilitation adaptation and performance. The findings suggest that various nutritional supplementation strategies can facilitate improvements in these areas. Nonetheless, the study has certain limitations. Firstly, the range of nutrients examined is restricted. Future research will aim to assess the impact of a broader spectrum of nutritional supplements on the rehabilitation of stroke patients. Secondly, the study did not address the treatment of dysphagia. Further research is required to develop nutritional supplementation plans and rehabilitation strategies specifically tailored for stroke patients experiencing dysphagia.
Author contributions
HC: Conceptualization, Data curation, Investigation, Software, Writing – original draft, Writing – review & editing. CF: Conceptualization, Data curation, Writing – review & editing. WF: Data curation, Investigation, Writing – review & editing. ZW: Data curation, Methodology, Writing – review & editing. DZ: Conceptualization, Methodology, Writing – review & editing. HZ: Conceptualization, Writing – review & editing, Funding acquisition.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by the Beijing Hospital of Traditional Chinese Medicine Shunyi Hospital research fund (Grant No. SYYJLC-202502).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2025.1502772/full#supplementary-material
References
1. Teasell, R, Salbach, NM, Foley, N, Mountain, A, Cameron, JI, Jong, A, et al. Canadian stroke best practice recommendations: rehabilitation, recovery, and community participation following stroke. Part one: rehabilitation and recovery following stroke; 6th edition update 2019. Int J Stroke. (2020) 15:763–88. doi: 10.1177/1747493019897843
2. GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the global Burden of disease study 2019. Lancet Neurol. (2021) 20:795–820. doi: 10.1016/S1474-4422(21)00252-0
3. Tu, W-J, Wang, L-D, Yan, F, Peng, B, Hua, Y, Liu, M, et al. China stroke surveillance report 2021. Mil Med Res. (2023) 10:33. doi: 10.1186/s40779-023-00463-x
4. Wu, S, Wu, B, Liu, M, Chen, Z, Wang, W, Anderson, CS, et al. Stroke in China: advances and challenges in epidemiology, prevention, and management. Lancet Neurol. (2019) 18:394–405. doi: 10.1016/S1474-4422(18)30500-3
5. Yuan, K, Zhu, S, Wang, H, Chen, J, Zhang, X, Xu, P, et al. Association between malnutrition and long-term mortality in older adults with ischemic stroke. Clin Nutr. (2021) 40:2535–42. doi: 10.1016/j.clnu.2021.04.018
6. Zhang, G, Pan, Y, Zhang, R, Wang, M, Meng, X, Li, Z, et al. Prevalence and prognostic significance of malnutrition risk in patients with acute ischemic stroke: results from the third China National Stroke Registry. Stroke. (2022) 53:111–9. doi: 10.1161/STROKEAHA.121.034366
7. Hu, D, Fu, Y, Ji, T, and Wu, M. Nutritional status and influencing factors of 323 patients with cerebral apoplexy. J Gen Nurs. (2024) 22:1345–8. doi: 10.12104/j.issn.1674-4748.2024.07.039
8. Li, D, Liu, Y, Jia, Y, Yu, J, Li, F, Li, H, et al. Association between malnutrition and stroke-associated pneumonia in patients with ischemic stroke. BMC Neurol. (2023) 23:290. doi: 10.1186/s12883-023-03340-1
9. Chen, Y, Yang, H, Lan, M, Wei, H, and Chen, Y. The controlling nutritional status score and risk factors associated with malnutrition in patients with acute ischemic stroke. Front Neurol. (2023) 14:1067706. doi: 10.3389/fneur.2023.1067706
10. Zhang, M, Ye, S, Huang, X, Sun, L, Liu, Z, Liao, C, et al. Comparing the prognostic significance of nutritional screening tools and ESPEN-DCM on 3-month and 12-month outcomes in stroke patients. Clin Nutr. (2021) 40:3346–53. doi: 10.1016/j.clnu.2020.11.001
11. Huang, LF, Zhu, ML, and Ye, YR. Association of nutritional indices and prognosis of stroke patients: a systematic review and meta-analysis. Eur Rev Med Pharmacol Sci. (2023) 27:5803–11. doi: 10.26355/eurrev_202306_32819
12. Gomes, F, Emery, PW, and Weekes, CE. Risk of malnutrition is an independent predictor of mortality, length of hospital stay, and hospitalization costs in stroke patients. J Stroke Cerebrovasc Dis. (2016) 25:799–806. doi: 10.1016/j.jstrokecerebrovasdis.2015.12.017
13. Sremanakova, J, Burden, S, Kama, Y, Gittins, M, Lal, S, Smith, CJ, et al. An observational cohort study investigating risk of malnutrition using the malnutrition universal screening tool in patients with stroke. J Stroke Cerebrovasc Dis. (2019) 28:104405. doi: 10.1016/j.jstrokecerebrovasdis.2019.104405
14. Nishioka, S, Wakabayashi, H, Nishioka, E, Yoshida, T, Mori, N, and Watanabe, R. Nutritional improvement correlates with recovery of activities of daily living among malnourished elderly stroke patients in the convalescent stage: a cross-sectional study. J Acad Nutr Diet. (2016) 116:837–43. doi: 10.1016/j.jand.2015.09.014
15. Nozoe, M, Yamamoto, M, Masuya, R, Inoue, T, Kubo, H, and Shimada, S. Prevalence of malnutrition diagnosed with GLIM criteria and association with activities of daily living in patients with acute stroke. J Stroke Cerebrovasc Dis. (2021) 30:105989. doi: 10.1016/j.jstrokecerebrovasdis.2021.105989
16. Xiaoqian, Li. Study on the correlation between nutritional status and TCM syndrome types in 215 elderly hospitalized patients with ischemic stroke. Thesis of Shandong University of Chinese Medicine. (2021).
17. Lielie, Z, Jianning, X, Xinyu, P, Xiangzhi, S, Jiacheng, Z, Dengchong, W, et al. Effectiveness of elderly nutritional risk index on neurological functional prognosis after stroke. Chin Rehabil Theory Pract. (2023) 29:1346–52. doi: 10.3969/j.issn.1006-9771.2023.11.013
18. Sabbouh, T, and Torbey, MT. Malnutrition in stroke patients: risk factors, assessment, and management. Neurocrit Care. (2018) 29:374–84. doi: 10.1007/s12028-017-0436-1
19. Dziewas, R, Michou, E, Trapl-Grundschober, M, Lal, A, Arsava, EM, Bath, PM, et al. European stroke organisation and European Society for Swallowing Disorders guideline for the diagnosis and treatment of post-stroke dysphagia. Eur Stroke J. (2021) 6:Lxxxix-cxv. doi: 10.1177/23969873211039721
20. Zeng, H, Cai, A, Zhao, W, Wu, J, Ding, Y, and Zeng, X. Factors and predictive model for malnutrition in poststroke disabled patients: a multicenter cross-sectional study. Nutrition. (2024) 123:112423. doi: 10.1016/j.nut.2024.112423
21. Aquilani, R, Scocchi, M, Iadarola, P, Franciscone, P, Verri, M, Boschi, F, et al. Protein supplementation may enhance the spontaneous recovery of neurological alterations in patients with ischaemic stroke. Clin Rehabil. (2008) 22:1042–50. doi: 10.1177/0269215508094244
22. Rabadi, MH, Coar, PL, Lukin, M, Lesser, M, and Blass, JP. Intensive nutritional supplements can improve outcomes in stroke rehabilitation. Neurology. (2008) 71:1856–61. doi: 10.1212/01.wnl.0000327092.39422.3c
23. Cheng, Y-H, Wei, L, Chan, WP, Hsu, C-Y, Huang, S-W, Wang, H, et al. Effects of protein supplementation on aerobic training-induced gains in cardiopulmonary fitness, muscle mass, and functional performance in chronic stroke: a randomized controlled pilot study. Clin Nutr. (2020) 39:2743–50. doi: 10.1016/j.clnu.2019.12.013
24. Sakai, K, Kinoshita, S, Tsuboi, M, Fukui, R, Momosaki, R, and Wakabayashi, H. Effects of nutrition therapy in older stroke patients undergoing rehabilitation: a systematic review and Meta-analysis. J Nutr Health Aging. (2019) 23:21–6. doi: 10.1007/s12603-018-1095-4
25. Sari, A, Durmus, B, Karaman, CA, Ogut, E, and Aktas, I. A randomized, double-blind study to assess if vitamin D treatment affects the outcomes of rehabilitation and balance in hemiplegic patients. J Phys Ther Sci. (2018) 30:874–8. doi: 10.1589/jpts.30.874
26. Narasimhan, S, and Balasubramanian, P. Role of vitamin D in the outcome of ischemic stroke- a randomized controlled trial. J Clin Diagn Res. (2017) 11:CC06-CC10. doi: 10.7860/JCDR/2017/24299.9346
27. Momosaki, R, Abo, M, and Urashima, M. Vitamin D supplementation and post-stroke rehabilitation: a randomized, double-blind, placebo-controlled trial. Nutrients. (2019) 11:1295. doi: 10.3390/nu11061295
28. Torrisi, M, Bonanno, L, Formica, C, Arcadi, FA, Cardile, D, Cimino, V, et al. The role of rehabilitation and vitamin D supplementation on motor and psychological outcomes in poststroke patients. Medicine (Baltimore). (2021) 100:e27747. doi: 10.1097/MD.0000000000027747
29. Honaga, K, Mori, N, Akimoto, T, Tsujikawa, M, Kawakami, M, Okamoto, T, et al. Investigation of the effect of nutritional supplementation with whey protein and vitamin D on muscle mass and muscle quality in subacute post-stroke rehabilitation patients: a randomized, single-blinded, placebo-controlled trial. Nutrients. (2022) 14:685. doi: 10.3390/nu14030685
30. Zhu, Z, Yang, P, Jia, Y, Wang, Y, Shi, M, Zhong, C, et al. Plasma amino acid neurotransmitters and ischemic stroke prognosis: a multicenter prospective study. Am J Clin Nutr. (2023) 118:754–62. doi: 10.1016/j.ajcnut.2023.06.014
31. Yoshimura, Y, Bise, T, Shimazu, S, Tanoue, M, Tomioka, Y, Araki, M, et al. Effects of a leucine-enriched amino acid supplement on muscle mass, muscle strength, and physical function in post-stroke patients with sarcopenia: a randomized controlled trial. Nutrition. (2019) 58:1–6. doi: 10.1016/j.nut.2018.05.028
32. Ikeda, T, Morotomi, N, Kamono, A, Ishimoto, S, Miyazawa, R, Kometani, S, et al. The effects of timing of a leucine-enriched amino acid supplement on body composition and physical function in stroke patients: a randomized controlled trial. Nutrients. (2020) 12:1928. doi: 10.3390/nu12071928
33. Ciancarelli, I, Morone, G, Iosa, M, Cerasa, A, Calabrò, RS, Iolascon, G, et al. Influence of oxidative stress and inflammation on nutritional status and neural plasticity: new perspectives on post-stroke Neurorehabilitative outcome. Nutrients. (2022) 15:108. doi: 10.3390/nu15010108
34. Sensi, SL, Paoletti, P, Bush, AI, and Sekler, I. Zinc in the physiology and pathology of the CNS. Nat Rev Neurosci. (2009) 10:780–91. doi: 10.1038/nrn2734
35. Aquilani, R, Baiardi, P, Scocchi, M, Iadarola, P, Verri, M, Sessarego, P, et al. Normalization of zinc intake enhances neurological retrieval of patients suffering from ischemic strokes. Nutr Neurosci. (2009) 12:219–25. doi: 10.1179/147683009X423445
36. Lee, JM, Zipfel, GJ, Park, KH, He, YY, Hsu, CY, and Choi, DW. Zinc translocation accelerates infarction after mild transient focal ischemia. Neuroscience. (2002) 115:871–8. doi: 10.1016/S0306-4522(02)00513-4
37. Garbagnati, F, Cairella, G, De Martino, A, Multari, M, Scognamiglio, U, et al. Is antioxidant and n-3 supplementation able to improve functional status in poststroke patients? Results from the Nutristroke trial. Cerebrovasc Dis. (2009) 27:375–83. doi: 10.1159/000207441
38. Sakai, K, Niimi, M, Momosaki, R, Hoshino, E, Yoneoka, D, Nakayama, E, et al. Nutritional therapy for reducing disability and improving activities of daily living in people after stroke. Cochrane Database Syst Rev. (2024) 8:Cd014852. doi: 10.1002/14651858.CD014852.pub2
39. Shehjar, F, Maktabi, B, Rahman, ZA, Bahader, GA, James, AW, Naqvi, A, et al. Stroke: molecular mechanisms and therapies: update on recent developments. Neurochem Int. (2023) 162:105458. doi: 10.1016/j.neuint.2022.105458
40. Jia, J, Jiao, W, Wang, G, Wu, J, Huang, Z, and Zhang, Y. Drugs/agents for the treatment of ischemic stroke: advances and perspectives. Med Res Rev. (2024) 44:975–1012. doi: 10.1002/med.22009
41. Phipps, MS, and Cronin, CA. Management of acute ischemic stroke. Management of acute ischemic stroke Bmj. (2020) 368:l6983. doi: 10.1136/bmj.l6983
42. Scherbakov, N, Von Haehling, S, Anker, SD, Dirnagl, U, and Doehner, W. Stroke induced sarcopenia: muscle wasting and disability after stroke. Int J Cardiol. (2013) 170:89–94. doi: 10.1016/j.ijcard.2013.10.031
43. Onat, Ş, Polat, CS, Gürçay, E, Özcan, DS, and Orhan, A. Muscle architecture and clinical parameters in stroke patients: an ultrasonographic study. J Clin Ultrasound. (2022) 50:713–8. doi: 10.1002/jcu.23202
44. Hunnicutt, JL, and Gregory, CM. Skeletal muscle changes following stroke: a systematic review and comparison to healthy individuals. Top Stroke Rehabil. (2017) 24:463–71. doi: 10.1080/10749357.2017.1292720
45. Ramasamy, DK, Dutta, T, Kannan, V, and Chandramouleeswaran, V. Amino acids in post-stroke rehabilitation. Nutr Neurosci. (2021) 24:426–31. doi: 10.1080/1028415X.2019.1641295
46. Liu, S, Liu, H, Yang, L, Wang, K, Chen, N, Zhang, T, et al. A review of rehabilitation benefits of exercise training combined with nutrition supplement for improving protein synthesis and skeletal muscle strength in patients with cerebral stroke. Nutrients. (2022) 14:4995. doi: 10.3390/nu14234995
47. Jiang, XF, Zhang, T, Sy, C, Nie, BB, Hu, XY, and Ding, Y. Dynamic metabolic changes after permanent cerebral ischemia in rats with/without post-stroke exercise: a positron emission tomography (PET) study. Neurol Res. (2014) 36:475–82. doi: 10.1179/1743132814Y.0000000350
48. Clark, TA, Sullender, C, Jacob, D, Zuo, Y, Dunn, AK, and Jones, TA. Rehabilitative training interacts with ischemia-instigated spine dynamics to promote a lasting population of new synapses in Peri-infarct motor cortex. J Neurosci. (2019) 39:8471–83. doi: 10.1523/JNEUROSCI.1141-19.2019
49. Joy, MT, and Carmichael, ST. Encouraging an excitable brain state: mechanisms of brain repair in stroke. Nat Rev Neurosci. (2021) 22:38–53. doi: 10.1038/s41583-020-00396-7
50. Rasmussen, BB, Tipton, KD, Miller, SL, Wolf, SE, and Wolfe, RR. An oral essential amino acid-carbohydrate supplement enhances muscle protein anabolism after resistance exercise. J Appl Physiol (1985). (2000) 88:386–92. doi: 10.1152/jappl.2000.88.2.386
51. Zielińska-Nowak, E, Cichon, N, Saluk-Bijak, J, Bijak, M, and Miller, E. Nutritional supplements and neuroprotective diets and their potential clinical significance in post-stroke rehabilitation. Nutrients. (2021) 13:2704. doi: 10.3390/nu13082704
52. Christakos, S, Dhawan, P, Verstuyf, A, Verlinden, L, and Carmeliet, G. Vitamin D: metabolism, molecular mechanism of action, and pleiotropic effects. Physiol Rev. (2016) 96:365–408. doi: 10.1152/physrev.00014.2015
53. Cui, P, Lu, W, Wang, J, Wang, F, Zhang, X, Hou, X, et al. Microglia/macrophages require vitamin D signaling to restrain neuroinflammation and brain injury in a murine ischemic stroke model. J Neuroinflammation. (2023) 20:63. doi: 10.1186/s12974-023-02705-0
54. Liu, H, Wang, J, and Xu, Z. Prognostic utility of serum 25-hydroxyvitamin D in patients with stroke: a meta-analysis. J Neurol. (2020) 267:3177–86. doi: 10.1007/s00415-019-09599-0
55. Zhao, Y, Zhang, X, Chen, X, and Wei, Y. Neuronal injuries in cerebral infarction and ischemic stroke: from mechanisms to treatment (review). Int J Mol Med. (2022) 49:15. doi: 10.3892/ijmm.2021.5070
56. Yuan, TF, Gu, S, Shan, C, Marchado, S, and Arias-Carrión, O. Oxidative stress and adult neurogenesis. Stem Cell Rev Rep. (2015) 11:706–9. doi: 10.1007/s12015-015-9603-y
57. Santos, R, Ruiz De Almodóvar, C, Bulteau, AL, and Gomes, CM. Neurodegeneration, neurogenesis, and oxidative stress. Oxidative Med Cell Longev. (2013) 2013:730581:1–2. doi: 10.1155/2013/730581
58. Carmichael, ST. Cellular and molecular mechanisms of neural repair after stroke: making waves. Ann Neurol. (2006) 59:735–42. doi: 10.1002/ana.20845
59. Winner, B, and Winkler, J. Adult neurogenesis in neurodegenerative diseases. Cold Spring Harb Perspect Biol. (2015) 7:a021287. doi: 10.1101/cshperspect.a021287
60. Valente, T, Hidalgo, J, Bolea, I, Ramirez, B, Anglés, N, Reguant, J, et al. A diet enriched in polyphenols and polyunsaturated fatty acids, LMN diet, induces neurogenesis in the subventricular zone and hippocampus of adult mouse brain. J Alzheimers Dis. (2009) 18:849–65. doi: 10.3233/JAD-2009-1188
Keywords: proteins, vitamin D, essential amino acids, antioxidants, nutritional supplement, rehabilitation, stroke
Citation: Chen H, Fu C, Fang W, Wang Z, Zhang D and Zhang H (2025) Influence of nutritional status on rehabilitation efficacy of patients after stroke—a scoping review. Front. Neurol. 16:1502772. doi: 10.3389/fneur.2025.1502772
Edited by:
Kosuke Oku, Kawasaki University of Medical Welfare, JapanCopyright © 2025 Chen, Fu, Fang, Wang, Zhang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hu Zhang, MTM3MTYwODg4NjZAMTYzLmNvbQ==
 Huan Chen
Huan Chen Caihong Fu
Caihong Fu