
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol., 27 March 2025
Sec. Neuroepidemiology
Volume 16 - 2025 | https://doi.org/10.3389/fneur.2025.1499564
This article is part of the Research TopicQuality of Stroke Care: What Could Be Improved, and How? - Volume IIView all 9 articles
Objective: To investigate independent risk factors for unplanned readmission of ischemic stroke patients within 31 days in Wenzhou, and establish a nomogram model for risk prediction.
Methods: A total of 3,035 patients with ischemic stroke were randomly grouped (in an 8:2 ratio) into 2,428 training set and 607validation set. Independent sample t-test, Pearson chi-square test, Fisher’s exact and multivariate logistic regression analysis were used to determine the factors associated with 31-day unplanned readmission in ischemic stroke, and the nomogram was established and validated.
Results: Six hundred and sixty nine patients (22.04%) had unplanned readmission. Atrial fibrillation, smoking, education of junior high school and below, length of stay >16 days, Hcy, and UA were independent risk factors for 31-day unplanned readmission in patients with ischemic stroke. The training set [AUC = 0.883 (95% CI = 0.867–0.899)] and validation set [AUC = 0.817 (95% CI = 0.777–0.858)], and the calibration curve closely resembled the ideal curve, demonstrating good agreement between the predicted and actual values, it shows that the prediction model has a good degree of differentiation and calibration. At the same time, the decision curve shows that the model has a high clinical net benefit rate.
Conclusion: The nomograph model established in this study to predict the risk of unplanned readmission of ischemic stroke patients within 31 days has good prediction ability.
Stroke remains a public health challenge, placing a significant financial burden on healthcare systems among survivors who are disabled as a result of stroke. In Western countries, stroke is the third leading cause of death after coronary heart disease and cancer (1). Ischemic stroke (IS) is the most common type of stroke, and accounts for 80% of the total incidence of stroke. Relative to many other diseases, stroke has a high readmission rate (2, 3). A cohort study in the United States showed that the short-term unplanned readmission rate of cerebral infarction patients was 12.4% (4). Lee et al. (5) showed that 9.2% of patients admitted to hospital for stroke in South Korea were readmitted and 7.6% were unplanned readmitted. A multi-center study in China reported that 28.8% of patients with IS were unplanned readmitted within 31 days of discharge (6).
Unplanned early readmission is an important indicator of hospital medical quality and nursing quality. Stroke incidence varies widely in the north and south regions, in China (7). According to the China Stroke Screening Survey (CNSSS), the incidence of IS in Zhejiang regions has been increasing year by year, and the incidence of IS is higher in males than females, and higher in rural areas than in urban areas (8). However, there is no study on unplanned readmission of IS patients in Zhejiang regions.
Therefore, the purpose of the study was two major aims. First, we investigated the risk factors of 31-day unplanned readmission in ischemic stroke patients, and unplanned readmission rate. Second, to establish a prognostic model for IS patients with unplanned readmission. In recent years, the nomogram as a forecasting method has played an important role in the development of personalized medicine. This study was based on a dataset of clinical studies to establish a nomogram of the risk of unplanned readmission in patients with IS.
This retrospective study was conducted at the Wenzhou TCM Hospital of Zhejiang Chinese Medical University between 2020 and 2022. Patients with ischemic stroke were identified using the hospital’s electronic medical record system, using the International Classification of Diseases Code (10th edition) (ICD-10) of the primary diagnostic record. After excluding subjects with missing data, a total of 3,035 patients inclusion in this study, of whom 669 were unplanned readmissions within 31 days of discharge (the unplanned readmission rate was 22.04%).
Unplanned readmitted: refers to the readmitted patients who are unpredictable at the time of discharge, excluding patients: planned readmitted and readmitted with new diseases different from the previous admission.
Inclusion criteria: ① The previous admission was diagnosed IS (ICD-10: I63); ② Age ≥18 years old; ③ The time between last discharge and readmission was within 31 days; ④ readmitted to hospital due to the same or related disease.
Exclusion criteria: ① Death or transfer to hospital after the previous hospitalization; ② Patients was planned to be admitted due to staging surgery, reexamination, and etc.
The selection method for 31-day unplanned readmission cases was first generated through the unplanned readmission report module in the electronic medical record system. Clinicians then examined the cases to determine whether they met the inclusion and exclusion criteria.
Clinical data of the patients were collected, including gender, age, BMI (≤24 kg/m2, >24 kg/m2), marital status (married, divorced, other), residential environment (city, countryside), smoking (no, yes), drinking (no, yes), education (high school and above, junior high school and below), hypertension (no, yes), diabetes (no, yes), hypertension (no, yes), atrial fibrillation (no, yes), operation (no, yes), length of stay (≤16 days, >16 days).
Laboratory examination data including homocysteine (Hcy), glycosylated hemoglobin (HbA1), fasting blood glucose (FBG), uric acid (UA), serumcreatinine (Scr), blood urea nitrogen (BUN), total cholesterol (TC), triglycerides (TG), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C).
This study was approved by the Medical Ethics Committee of the Wenzhou Hospital of Traditional Chinese Medicine and was conducted in accordance with the Declaration of Helsinki.
RStudio 4.1.1 and SPSS 25.0 software was used to the part of analyses in study. Continuous variables (normal distribution and uniform variance) were described by , independent sample t-test was used to comparisons between the groups; count variables were described by frequency (percentage), and were compared using the Pearson chi-square test and Fisher’s exact probability test. The variables that were significant in the univariate analysis were included in the multivariate logistic regression analysis to construct the prediction model. The nomogram prediction model was constructed by using RStudio software rms package, and the ability of the model to the predict 31-day unplanned readmission was evaluated by receiver operator characteristic (ROC). The bootstrap method was used to repeat the sampling 1,000 times for internal validation, and the prediction model was evaluated by calibration curves. Decision curves evaluate the clinical value of the prediction model. A p < 0.05 indicated that the difference was statistically significant.
The 3,035 patients were randomly allocated into training (2,428 patients) and validation set (607 patients) in an 8:2 ratio. There was no significant difference in the baseline data of age, gender, marital status education, smoking, drinking, hyperlipidemia, diabetes, hypertension, atrial fibrillation, operation, length of hospital stay between the training set and the verification set (p > 0.05) as shown in Table 1.
Within the training set, patients were further categorized into a 31-day unplanned readmission group (535 cases) and a non-31-day unplanned readmission group (1,893 cases). There was no statistically significant difference between the non-31-day unplanned readmission group and the 31-day unplanned readmission group in terms of gender, BMI, age, marital status, residential, drinking, hyperlipidemia, diabetes, HbA1c, FBG, Scr, BUN, TC, TG, LDL-C, and HDL-C (p > 0.05). In the 31-day unplanned readmission group, patients with smoking, junior high school education or below, hypertension, atrial fibrillation, surgery, and hospital stay >16 days accounted for a higher proportion of patients, and the levels of UA and Hcy were higher than those in the non-31-day unplanned readmission group, with statistical significance (p < 0.05) as shown in Tables 2, 3.
In the multivariate analysis, significant factors found were atrial fibrillation (OR = 1.811; 95% CI: 1.178–2.784), smoking (OR = 2.571; 95% CI: 1.896–4.924), education of junior high school and below (OR = 2.021; 95% CI: 1.533–2.664), length of stay >16 days (OR = 8.793; 95% CI: 6.603–11.709), Hcy (OR = 1.238; 95% CI: 1.199–1.279), and UA (OR = 1.020; 95% CI: 1.018–1.023), as shown in Table 4.
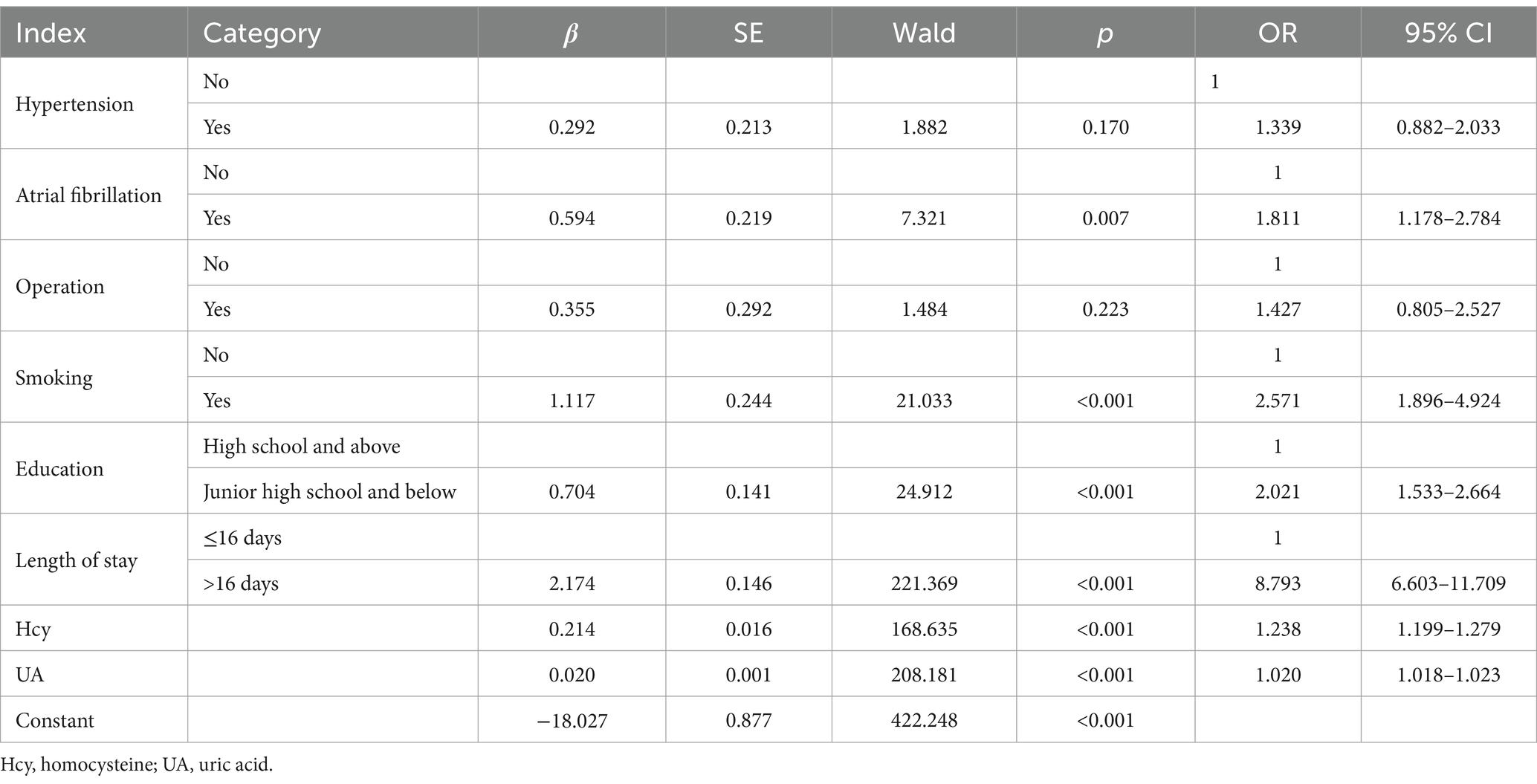
Table 4. Multiple logistic regression analysis of 31-day unplanned readmission in ischemic stroke patients.
Based on logistic regression results, a nomogram was constructed to determine the risk of 31-day unplanned readmission of IS patients after discharge. In the nomogram, the total score corresponding to each independent influencing factor is added to calculate the total score, and the predicted probability of 31-day unplanned readmission corresponding to the total score is obtained (Figure 1).
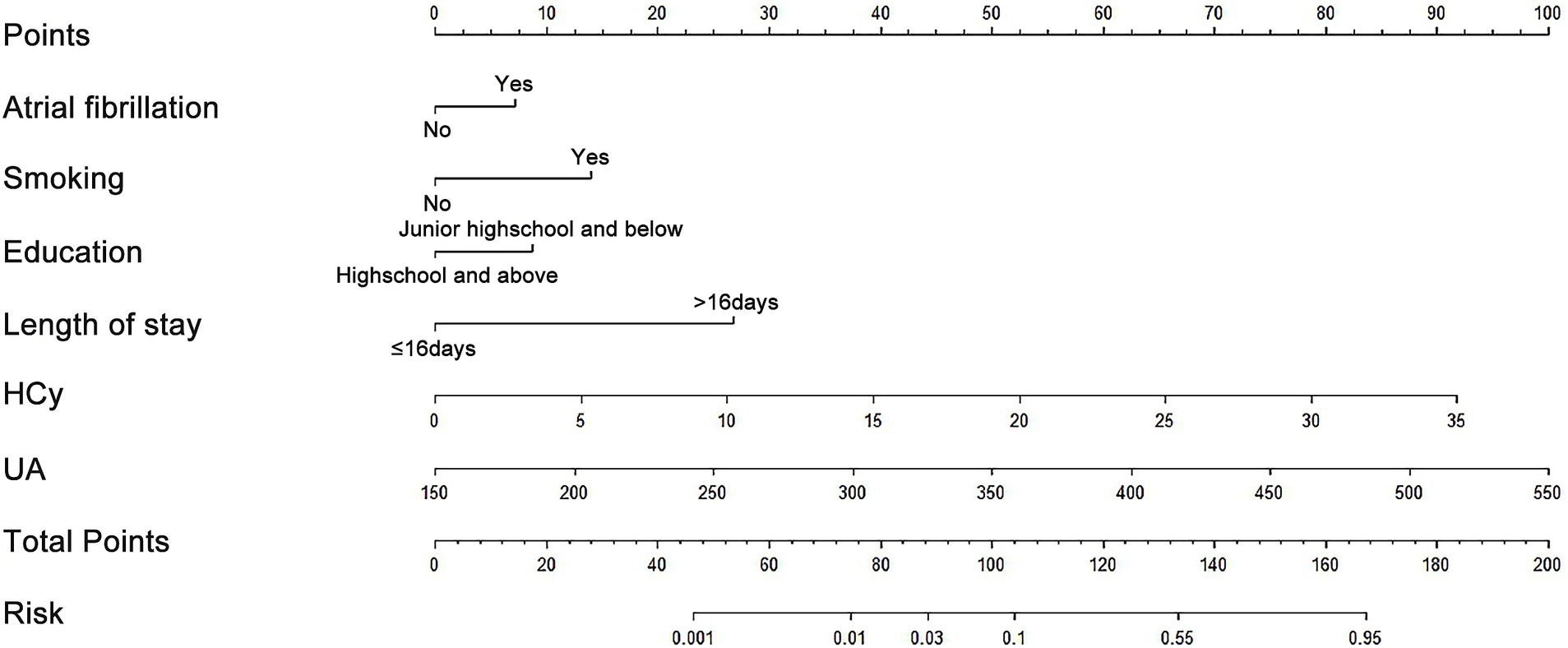
Figure 1. Nomogram model for predicting the risk of 31-day unplanned readmission in ischemic stroke patients.
For the training set, the AUC was 0.883 (95% CI = 0.867–0.899), with a sensitivity of 81.31% and a specificity of 79.29%; for the validation set, the AUC was 0.817 (95% CI = 0.777–0.858), with a sensitivity a sensitivity of 77.40% and a specificity of 77.20%, as shown in Figures 2a,b. The calibration curves of the training set and the verification set tend to be close to the ideal curve, and the actual values agree well with the predicted values (Figures 3a,b). Additionally, the decision curve analysis revealed that the nomogram model yielded great net benefits in a risk threshold range of 0–1 in the training set, and a risk threshold range of 0–0.7 in testing set (Figures 3c,d).
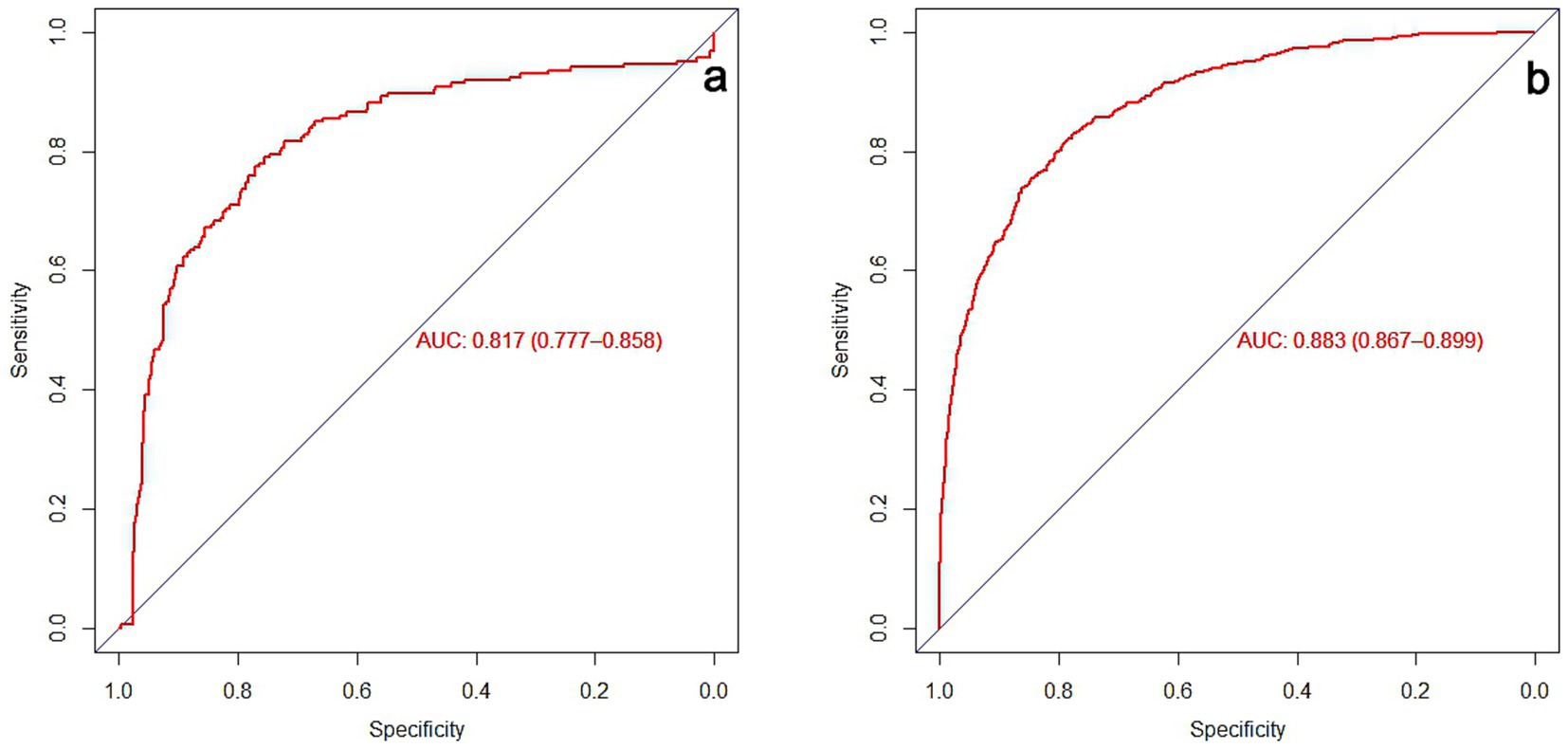
Figure 2. Prediction of 31-day unplanned readmission ROC curve for ischemic stroke patients. (a) Training set ROC curve. (b) Verification set ROC curve.
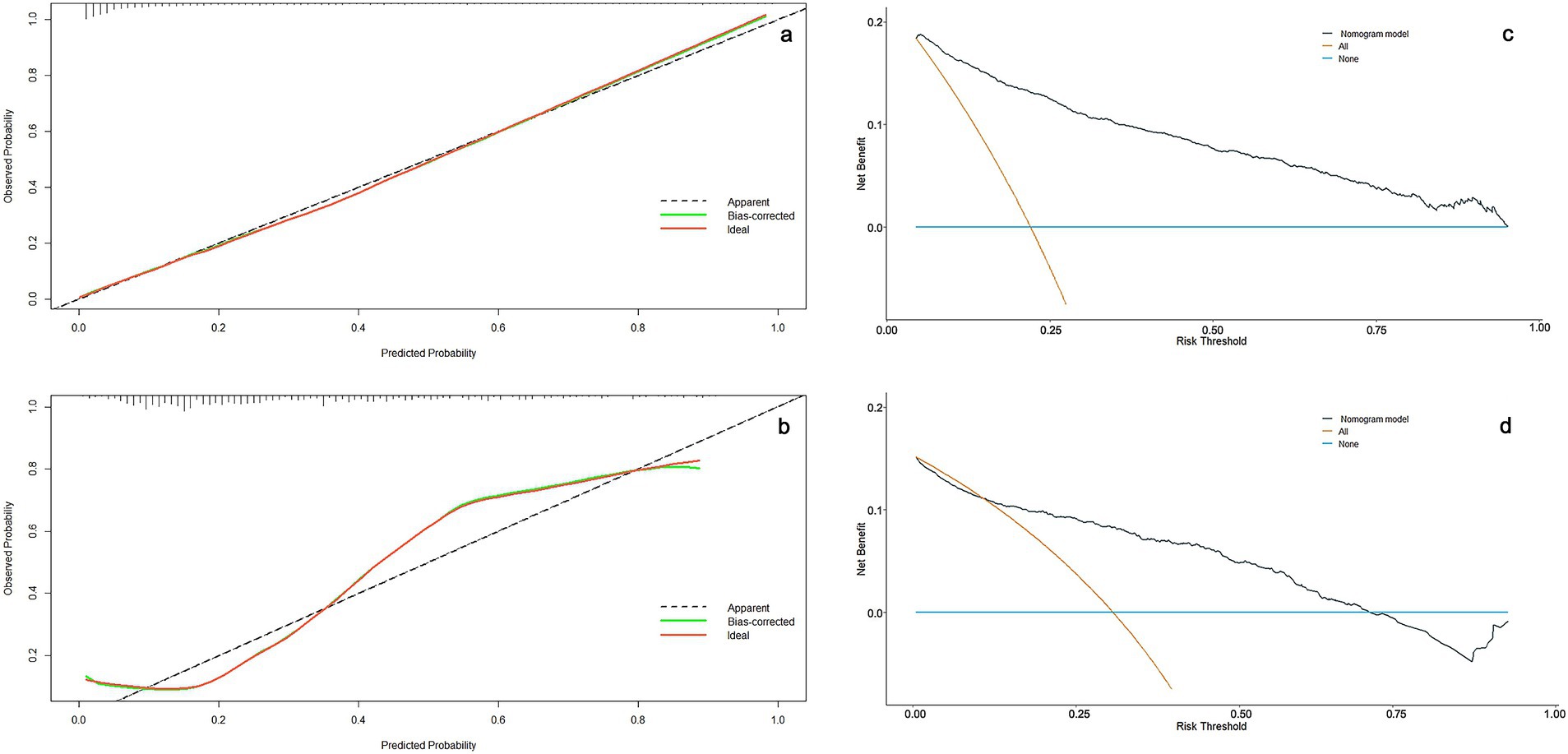
Figure 3. Nomogram calibration and decision curve for 31-day unplanned readmission of ischemic stroke. (a) Calibration curves for the nomogram model in the training set. (b) Calibration curves for the nomogram model in the validation set. The x-axis represents the predicted risk and the y-axis represents the actual observed. (c) Decision curves for the nomogram model in the training set. (d) Decision curves for the nomogram model in the validation set. The dark green line shows the risk model. The brown line indicates a 31-day unplanned readmission forecast for all patients. The blue line indicates a 31-day unplanned readmission forecast for no patients.
Readmissions are an internationally recognized measure of the quality of medical treatment and care (9–11). Hospital readmissions, especially unplanned readmissions, are considered to be outcomes that are not easily predicted (12). Because unplanned readmissions shortly after discharge are usually considered to be the result of unresolved issues at the time of discharge (5). As one of the most common clinical diseases, ischemic stroke not only has a high incidence, but also a serious condition, which imposes economic and health burdens on patients, society and health service systems around the world (13). Due to the high disease burden of ischemic stroke, it is important to study the relationship between stroke and hospital readmissions.
In recent years, the development of microsurgery has made great progress in the treatment of ischemic stroke, and the prognosis of patients has been greatly improved. However, short-term readmission rates after stroke remain high, with the 31-day readmission rate being around 15% in developed countries (14, 15). In this study, we investigated factors associated with 31-day readmission rate among patients with stroke in China. Among 3,035 patients with ischemic stroke, 22.04% had an unplanned readmission within 31 days, and it was comparable with Qiu’s et al. (16) report.
Complications not only increase the risk of ischemic stroke, but also affect the prognosis. Atrial fibrillation is the most common type of arrhythmia, and its association with ischemic stroke has been widely studied. Benjamin et al. (17) showed that patients with atrial fibrillation had a five-fold increased risk of ischemic stroke and a two-fold increased mortality. However, the relationship between atrial fibrillation and unplanned readmission in patients with ischemic stroke is rarely reported. Our findings showed that stroke patients with atrial fibrillation had a 1.887-fold increased risk of unplanned readmission, and indicated that clinicians should pay attention to the treatment and control of atrial fibrillation while treating stroke. China is a big tobacco country, and about one-third of the world’s tobacco is consumed by people in China, which is dominated by men (18). A number of studies have confirmed that smoking can cause a variety of diseases, mainly including cardiovascular disease, respiratory disease, cancer (19, 20). Smoking not only increases the risk of stroke, but also has a strong dose-dependent relationship (21). Chen et al. (22) reported that smoking could increase the risk of stroke recurrence in patients with cerebral infarction and transient ischemic attack, which was similar to our study results. Education of junior high school and below have an increased risk of unplanned readmission after stroke compared to education of high school and above. A prospective cohort study showed that low educational attainment was associated with an increased risk of stroke in both men and women (23). Moreover, a evidence from epidemiology and Mendelian randomization study reported that education had a protective effect on cardiovascular disease outcomes (24). Why educational attainment reduces stroke readmissions. Considering the reasons, it may have to do with the broad benefits of education, which higher levels of education are associated with healthier lifestyles/attitudes towards health care, safer working conditions and better health care. Medical staff should increase the frequency and time of health education in the face of patients with low education level. In order to improve the patients and their families to the disease of the degree of attention, and then improve the patients to the absence of cerebral infarction disease and recurrence knowledge. Patients with a stay of >16 days had a higher risk of unplanned readmission than patients with a stay of ≤16 days. A random forest algorithm research reported that the risk of readmission was low in patients (stroke) hospitalized for about 10 days, and longer or shorter length of hospital stay increased the risk of readmission (25). Studies in South Korea and the United States have reached similar conclusions (5, 15). The relationship between the length of hospital stay and readmission of stroke patients may be related to various factors such as the region, the type of disease studied, disease severity, and the level of medical treatment and nursing.
Among laboratory measures associated with ischemic stroke, our results showed that Hcy and UA were independent risk factors for unplanned reentry. A large number of previous studies have reported that Hcy is an independent risk factor for the occurrence and recurrence of ischemic stroke (26, 27). A meta-study found that high Hcy levels were positively associated with early hemorrhage transformation after IS, with no racial differences (28). UA has the dual properties of antioxidant and oxidation, on the one hand as an effective antioxidant can remove free radicals in the blood; On the other hand, oxidative stress can cause endothelial dysfunction and lead to cardiovascular diseases such as stroke (29). At present, the relationship between serum UA levels and stroke is also controversial. Sun et al. (30) found that UA therapy in patients with acute ischemic stroke can reduce the level of markers of oxidative stress. In contrast, a meta-study of 33,580 stroke patients showed (31) that increased UA levels increased the incidence and recurrence of IS, and there was no evidence to support a neuroprotective effect of UA. Han et al. study showed (32) that increased UA levels were associated with recurrence of IS and increased readmission risk of patients, which was similar to our study results.
Based on regression analysis, the nomogram prediction model integrates multiple independent risk factors together, and shows the proportion of the score by line segment on the same plane according to a certain probability (33, 34). At present, the nomogram model has been widely used in clinical medicine, especially in oncology (35). In this study, a nomogram prediction model was established based on the results of logistic multivariate regression analysis, and the area under ROC curve was 0.883 (95% CI = 0.867–0.899), indicating that the nomogram model had a good predicted values. The calibration curve showed that the nomogram model had good prediction accuracy. The decision curve results showed that the nomogram model had a higher clinical net benefit rate.
Limitations also exist in this study. Firstly, although this study is a large sample study, there may be some bias in the single-center, retrospective study. Secondly, although we studied the relationship between smoking and readmission in stroke patients. However, due to the retrospective study of this study, it is difficult for us to obtain the specific daily smoking amount of patients, so we cannot further study the relationship between smoking dose and readmission. Thirdly, medication adherence after discharge may also affect the incidence of recurrent ischemic stroke, our study did not analyze the effect of medication adherence. We will conduct a prospective, multicenter study to further validate the current model.
In this study, with 22.04% of ischemic stroke patients being readmitted within 31 days after discharge. Atrial fibrillation, smoking, education of junior high school and below, length of stay >16 days, Hcy, and UA were the most influential factors for readmission within 31 days. The nomogram prediction model based on the above risk factors has better predictive power, discernment, and higher clinical net benefit rate.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The studies involving humans were approved by the Ethics Review Committee of Wenzhou Traditional Chinese Medicine Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin due to the retrospective nature of this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
YM: Data curation, Formal analysis, Investigation, Writing – original draft. ZJ: Methodology, Supervision, Writing – review & editing. XYi: Data curation, Investigation, Writing – review & editing. XYe: Conceptualization, Data curation, Investigation, Writing – original draft.
The author(s) declare that no financial support was received for the research and/or publication of this article.
The authors gratefully acknowledge Editage (www.editage.com) for English language editing.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Wang, Y, Leifheit, EC, Goldstein, LB, and Lichtman, JH. Association of short-term hospital-level outcome metrics with 1-year mortality and recurrence for US Medicare beneficiaries with ischemic stroke. PLoS One. (2023) 18:e0289790. doi: 10.1371/journal.pone.0289790
2. Boehme, AK, Oka, M, Cohen, B, Elkind, MSV, Larson, E, and Mathema, B. Readmission rates in stroke patients with and without infections: incidence and risk factors. J Stroke Cerebrovasc Dis. (2022) 31:106172. doi: 10.1016/j.jstrokecerebrovasdis.2021.106172
3. Goicoechea, S, Walsh, M, Soult, M, Halandras, PM, Bechara, C, Aulivola, B, et al. Female gender increases risk of stroke and readmission after carotid endarterectomy and carotid artery stenting. J Vasc Surg. (2022) 75:1935–44. doi: 10.1016/j.jvs.2021.10.034
4. Bambhroliya, AB, Donnelly, JP, Thomas, EJ, Tyson, JE, Miller, CC, McCullough, LD, et al. Estimates and temporal trend for US nationwide 30-day hospital readmission among patients with ischemic and hemorrhagic stroke. JAMA Netw Open. (2018) 1:e181190. doi: 10.1001/jamanetworkopen.2018.1190
5. Lee, SA, Park, EC, Shin, J, Ju, YJ, Choi, Y, and Lee, HY. Patient and hospital factors associated with 30-day unplanned readmission in patients with stroke. J Investig Med. (2019) 67:52–8. doi: 10.1136/jim-2018-000748
6. Wen, T, Liu, B, Wan, X, Zhang, X, Zhang, J, Zhou, X, et al. Risk factors associated with 31-day unplanned readmission in 50,912 discharged patients after stroke in China. BMC Neurol. (2018) 18:218. doi: 10.1186/s12883-018-1209-y
7. Wang, W, Jiang, B, Sun, H, Ru, X, Sun, D, Wang, L, et al. Prevalence, incidence, and mortality of stroke in China: results from a nationwide population-based survey of 480,687 adults. Circulation. (2017) 135:759–71. doi: 10.1161/CIRCULATIONAHA.116.025250
8. Wang, A, Jia, B, Zhang, X, Huo, X, Chen, J, Gui, L, et al. Efficacy and safety of butylphthalide in patients with acute ischemic stroke: a randomized clinical trial. JAMA Neurol. (2023) 80:851–9. doi: 10.1001/jamaneurol.2023.1871
9. LGDR, V, Safanelli, J, Araujo, T, Schuch, HA, MHR, K, Nagel, V, et al. The cost of stroke in private hospitals in Brazil: a one-year prospective study. Arq Neuropsiquiatr. (2019) 77:393–403. doi: 10.1590/0004-282x20190056
10. Li, X, Tse, VC, Au-Doung, LW, Wong, ICK, and Chan, EW. The impact of ischaemic stroke on atrial fibrillation-related healthcare cost: a systematic review. Europace. (2017) 19:euw093–947. doi: 10.1093/europace/euw093
11. Kaufman, BG, Shah, S, Hellkamp, AS, Lytle, BL, Fonarow, GC, Schwamm, LH, et al. Disease burden following non-cardioembolic minor ischemic stroke or high-risk TIA: a GWTG-stroke study. J Stroke Cerebrovasc Dis. (2020) 29:105399. doi: 10.1016/j.jstrokecerebrovasdis.2020.105399
12. Elkind, MSV, Boehme, AK, Smith, CJ, Meisel, A, and Buckwalter, MS. Infection as a stroke risk factor and determinant of outcome after stroke. Stroke. (2020) 51:3156–68. doi: 10.1161/STROKEAHA.120.030429
13. Boehme, AK, Esenwa, C, and Elkind, MS. Stroke risk factors, genetics, and prevention. Circ Res. (2017) 120:472–95. doi: 10.1161/CIRCRESAHA.116.308398
14. Stein, LK, Agarwal, P, Thaler, A, Kwon, CS, Jette, N, and Dhamoon, MS. Readmission to a different hospital following acute stroke is associated with worse outcomes. Neurology. (2019) 93:15. doi: 10.1212/WNL.0000000000008446
15. Vahidy, FS, Donnelly, JP, McCullough, LD, Tyson, JE, Miller, CC, Boehme, AK, et al. Nationwide estimates of 30-day readmission in patients with ischemic stroke. Stroke. (2017) 48:1386–8. doi: 10.1161/STROKEAHA.116.016085
16. Qiu, X, Xue, X, Xu, R, Wang, J, Zhang, LI, Zhang, L, et al. Predictors, causes and outcome of 30-day readmission among acute ischemic stroke. Neurol Res. (2021) 43:9–14. doi: 10.1080/01616412.2020.1815954
17. Benjamin, EJ, Blaha, MJ, Chiuve, SE, Cushman, M, Das, S, Deo, R, et al. Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation. (2017) 135:e146–603. doi: 10.1161/CIR.0000000000000485
18. Chan, KH, Wright, N, Xiao, D, Guo, Y, Chen, Y, du, H, et al. Tobacco smoking and risks of more than 470 diseases in China: a prospective cohort study. Lancet Public Health. (2022) 7:e1014–26. doi: 10.1016/S2468-2667(22)00227-4
19. Scott, JG, Matuschka, L, Niemelä, S, Miettunen, J, Emmerson, B, and Mustonen, A. Evidence of a causal relationship between smoking tobacco and schizophrenia spectrum disorders. Front Psychiatry. (2018) 9:607. doi: 10.3389/fpsyt.2018.00607
20. Barbhaiya, M, Tedeschi, SK, Lu, B, Malspeis, S, Kreps, D, Sparks, JA, et al. Cigarette smoking and the risk of systemic lupus erythematosus, overall and by anti-double stranded DNA antibody subtype, in the nurses’ health study cohorts. Ann Rheum Dis. (2018) 77:196–202. doi: 10.1136/annrheumdis-2017-211675
21. Pan, B, Jin, X, Jun, L, Qiu, S, Zheng, Q, and Pan, M. The relationship between smoking and stroke: a meta-analysis. Medicine. (2019) 98:e14872. doi: 10.1097/MD.0000000000014872
22. Chen, J, Li, S, Zheng, K, Wang, H, Xie, Y, Xu, P, et al. Impact of smoking status on stroke recurrence. J Am Heart Assoc. (2019) 8:e011696. doi: 10.1161/JAHA.118.011696
23. Jackson, CA, Sudlow, C, and Mishra, GD. Education, sex and risk of stroke: a prospective cohort study in New South Wales Australia. BMJ Open. (2018) 8:e24070. doi: 10.1136/bmjopen-2018-024070
24. Xiuyun, W, Qian, W, Minjun, X, Weidong, L, and Lizhen, L. Education and stroke: evidence from epidemiology and Mendelian randomization study. Sci Rep. (2020) 10:21208. doi: 10.1038/s41598-020-78248-8
25. Wen, TC, Liu, BY, and Zhang, YN. Risk factors for unplanned readmission in ischemic stroke survivors within 31 days: a random forest algorithm research. Chin J Evid Based Med. (2019) 19:532–8. doi: 10.7507/1672-2531.201809094
26. Huang, X, Li, Y, Li, P, Li, J, Bao, H, Zhang, Y, et al. Association between percent decline in serum total homocysteine and risk of first stroke. Neurology. (2017) 89:2101–7. doi: 10.1212/WNL.0000000000004648
27. Anniwaer, J, Liu, MZ, Xue, KD, Maimaiti, A, and Xiamixiding, A. Homocysteine might increase the risk of recurrence in patients presenting with primary cerebra infarction. Int J Neurosci. (2018):654–9. doi: 10.1080/00207454.2018.1517762
28. Zhou, Z, Liang, Y, Qu, H, Zhao, M, Guo, F, Zhao, C, et al. Plasma homocysteine concentrations and risk of intracerebral hemorrhage: a systematic review and meta-analysis. Sci Rep. (2018) 8:2568. doi: 10.1038/s41598-018-21019-3
29. Zhou, Y, Zhao, M, Pu, Z, Xu, G, and Li, X. Relationship between oxidative stress and inflammation in hyperuricemia: analysis based on asymptomatic young patients with primary hyperuricemia. Medicine. (2018) 97:e13108. doi: 10.1097/MD.0000000000013108
30. Sun, ZJ, Feng, J, He, M, Wang, M, Zhang, Y, Wang, N, et al. Higher uric acid is associated with better discharge recovery and short-term outcome in stroke patients treated with thrombolysis. Neurol Sci. (2021) 42:3225–31. doi: 10.1007/s10072-020-04919-z
31. Tariq, MA, Shamim, SA, Rana, KF, Saeed, A, and Malik, BH. Serum uric acid—risk factor for acute ischemic stroke and poor outcomes. Cureus. (2019) 11:e6007. doi: 10.7759/cureus.6007
32. Zhu, HY, Zhao, SZ, Zhang, ML, Wang, Y, Pan, ZM, Cheng, HR, et al. Elevated serum uric acid increases the risk of ischemic stroke recurrence and its inflammatory mechanism in older adults. Front Aging Neurosci. (2022) 14:822350. doi: 10.3389/fnagi.2022.822350
33. Chen, Y, Zhou, D, Xiong, M, Xi, X, Zhang, W, Zhang, R, et al. Prediction and prognosis of adverse maternal and foetal/neonatal outcomes in pulmonary hypertension: an observational study and nomogram construction. Respir Res. (2022) 23:314. doi: 10.1186/s12931-022-02235-y
34. Cheng, L, Bai, W, Song, P, Zhou, L, Li, Z, Gao, L, et al. Development and validation of a nomograph model for post-operative central nervous system infection after craniocerebral surgery. Diagnostics. (2023) 13:2207. doi: 10.3390/diagnostics13132207
35. Zou, M, Dong, S, Liu, S, Du, C, Sun, Y, Dong, J, et al. Influencing factors of prognosis in children with pulmonary atresia with intact ventricle septum after transthoracic balloon dilation of pulmonary valve and construction of a nomograph prediction model. Biotechnol Genet Eng Rev. (2023) 113:4328–40. doi: 10.1080/02648725.2023.2210448
Keywords: unplanned readmission within 31 days, ischemic stroke, risk model, nomograph, pediatrics
Citation: Ma Y, Jin Z, Yi X and Ye X (2025) Risk factors analysis and nomograph model construction of unplanned readmission for ischemic stroke within 31 days in Wenzhou. Front. Neurol. 16:1499564. doi: 10.3389/fneur.2025.1499564
Received: 03 October 2024; Accepted: 11 March 2025;
Published: 27 March 2025.
Edited by:
Arinjita Bhattacharyya, University of Louisville, United StatesReviewed by:
Aksheev Bhambri, University of Texas Southwestern Medical Center, United StatesCopyright © 2025 Ma, Jin, Yi and Ye. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhili Jin, NzI5NTg5ODUxQHFxLmNvbQ==
†ORCID: Zhili Jin, orcid.org/0009-0003-1704-1300
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.