- 1School of Graduate, Heilongjiang University of Chinese Medicine, Harbin, China
- 2Department of Acupuncture II, The Second Affiliated Hospital of Heilongjiang University of Chinese Medicine, Harbin, China
Introduction: The aim of this study is to evaluate the effectiveness and safety of the combination therapy of acupuncture and medication in the treatment of perimenopausal insomnia (PMI). This research seeks to provide scientific evidence for clinical practice, optimize treatment protocols, and enhance the sleep quality and overall quality of life for women experiencing perimenopausal insomnia.
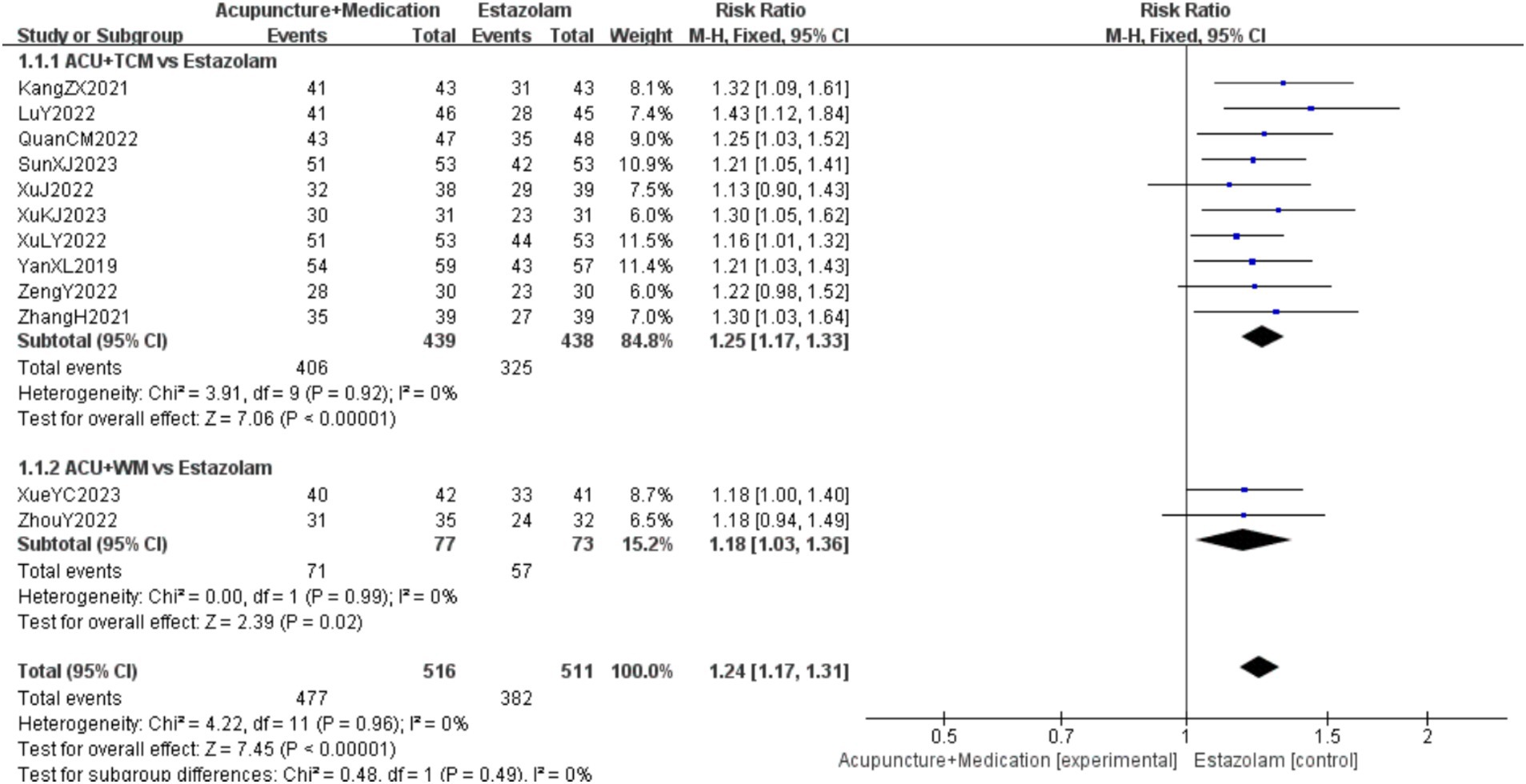
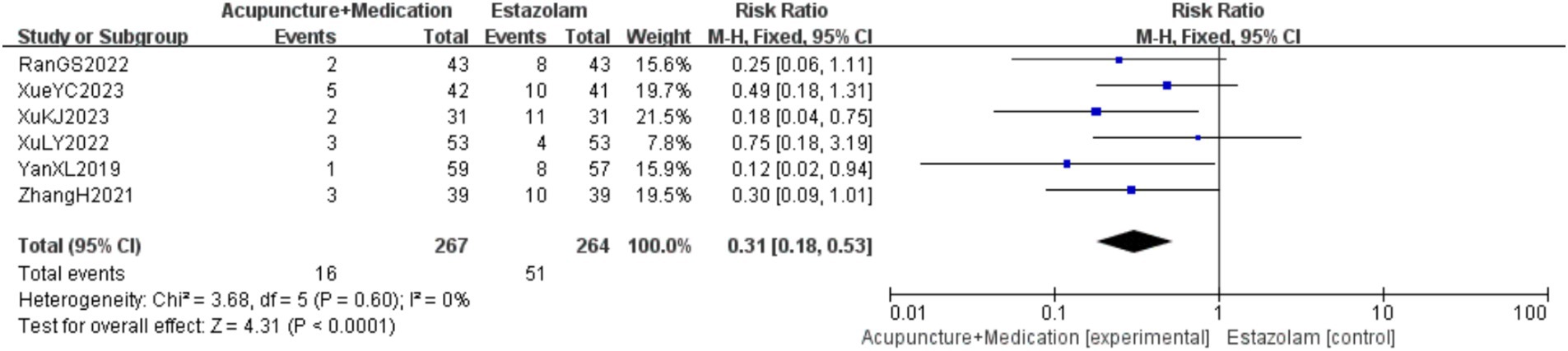
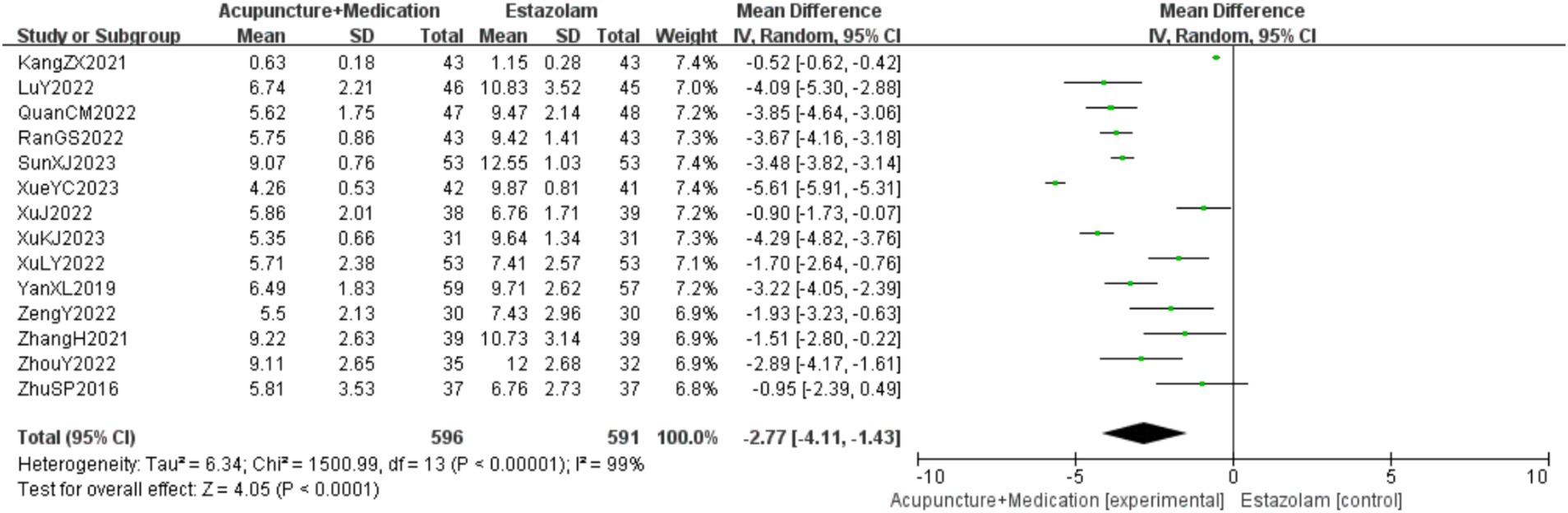
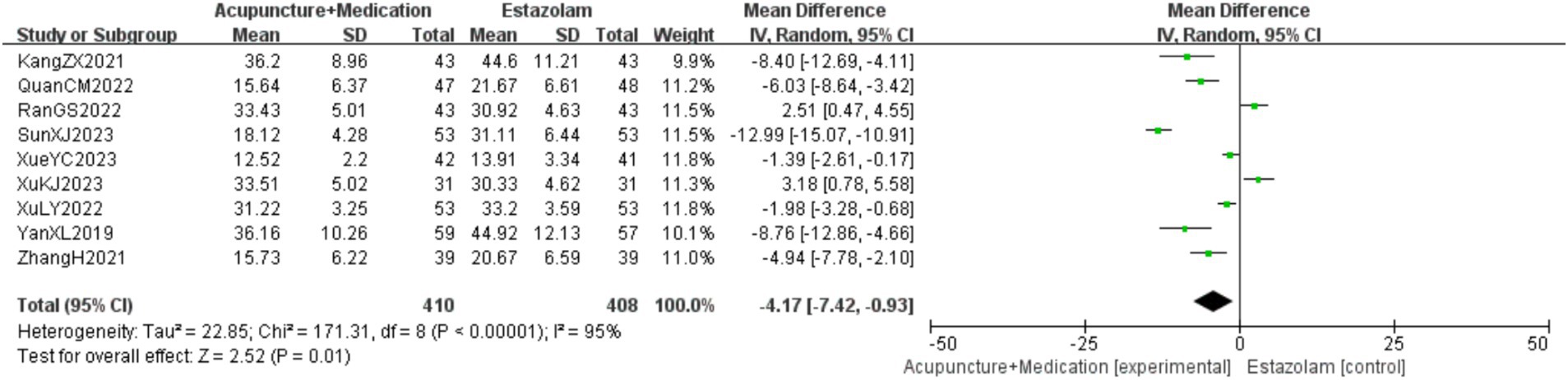
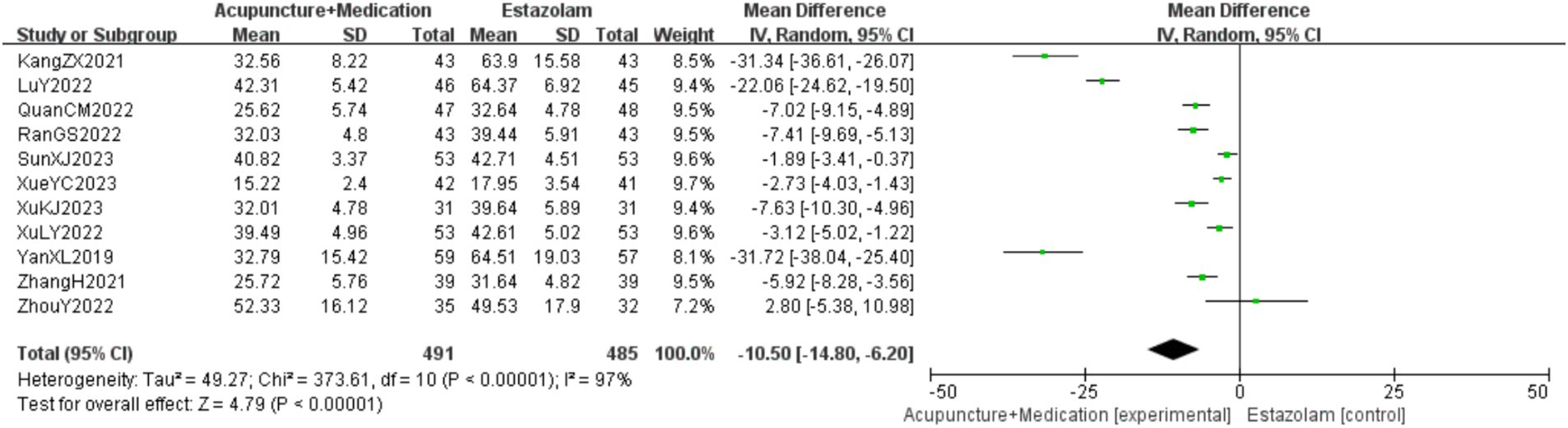
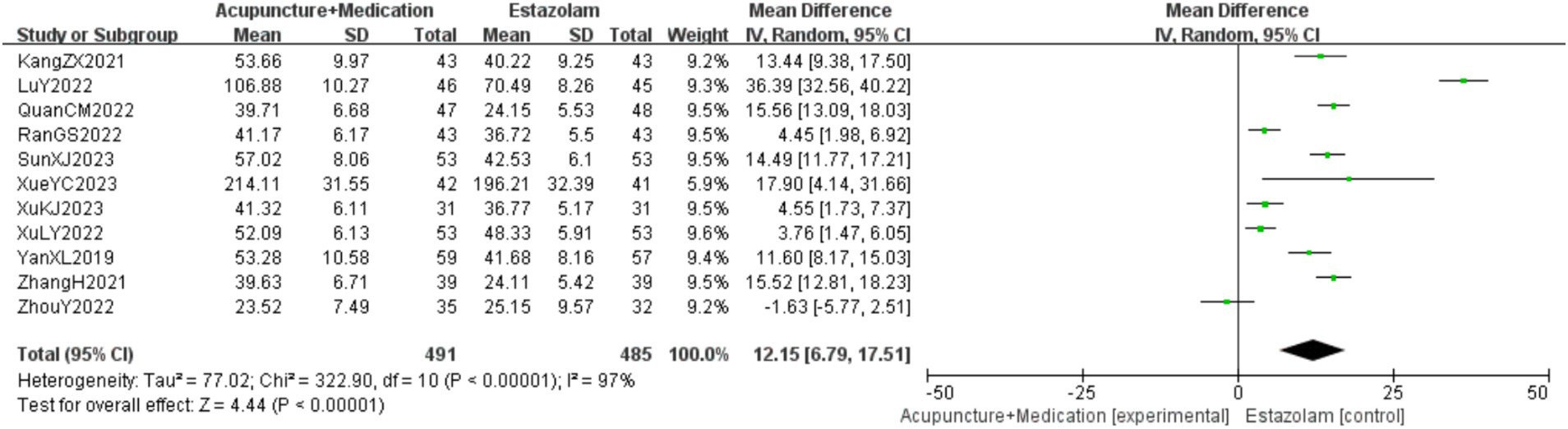
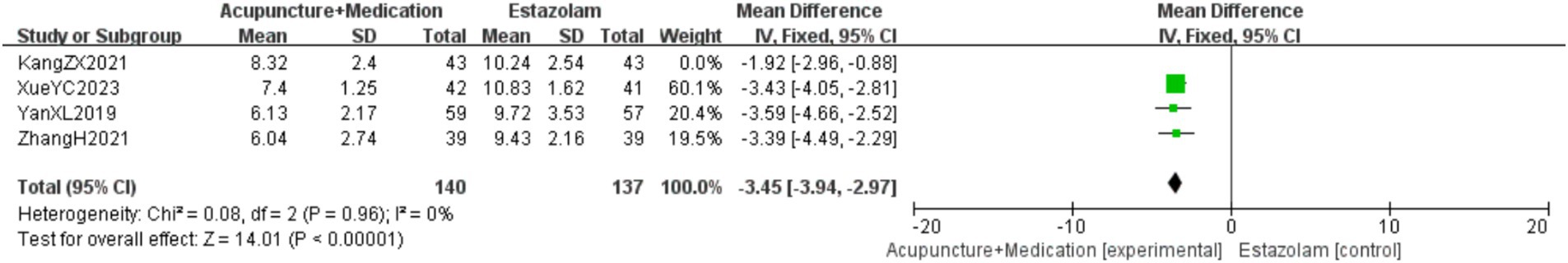
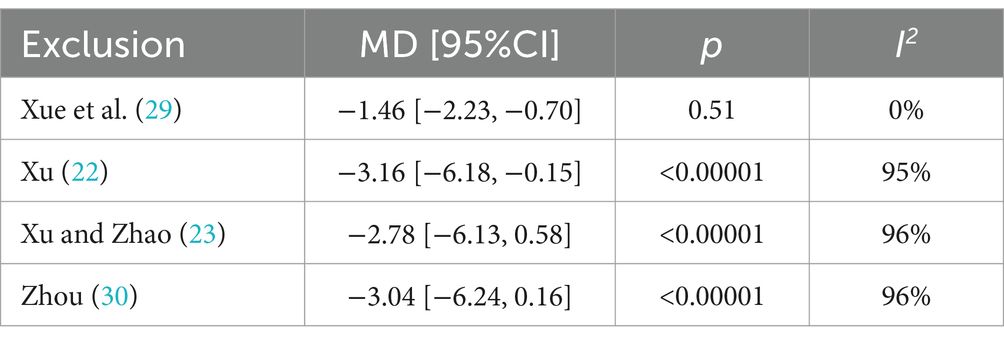
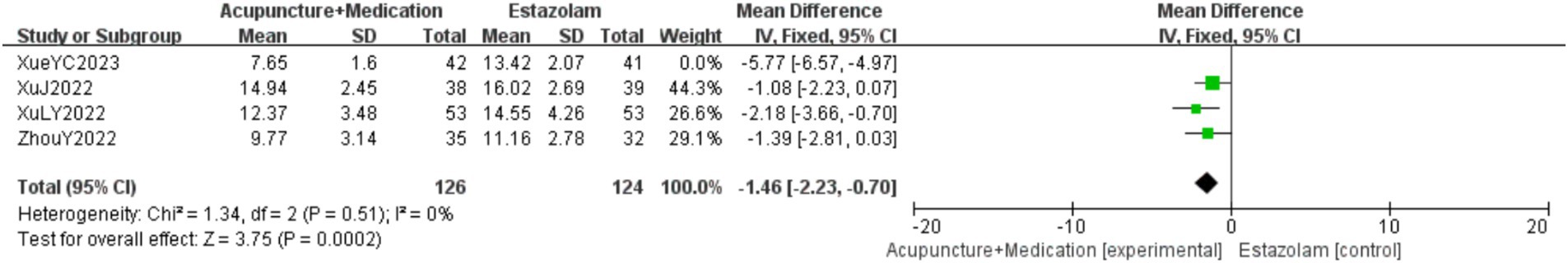
Methods and analysis: A comprehensive search was conducted across 8 databases, including the China National Knowledge Infrastructure (CNKI), Wanfang Academic Journal Full-text Database (Wanfang), Chongqing VIP Database (CQVIP), China Biology Medicine Disc (CBM), PubMed, Web of Science, Excerpta Medica Database (EMBASE), and Cochrane Library, from their establishment to July 1, 2024. Outcome measures were analyzed using Review Manager 5.4 and Stata 15.0 software. The included randomized controlled trials (RCTs) involved 1,187 patients with perimenopausal sleep disorders (596 in the experimental group and 591 in the control group). The analysis indicated that compared to Western medication alone, the combination therapy showed better efficacy [risk ratio (RR) = 1.24, 95% confidence interval (CI) (1.17, 1.31), p < 0.00001] and safety [RR = 0.31, 95%CI (0.18, 0.53), p < 0.0001]. It also demonstrated more significant improvements in Pittsburgh Sleep Quality Index (PSQI) [mean difference (MD) = −2.77, 95%CI (−4.11, −1.43), p < 0.0001], Hamilton Anxiety Rating Scale (HAMA) scores [MD = −3.45, 95%CI (−3.94, −2.97), p < 0.00001], Kupperman Menopausal Index (KMI) [MD = −1.46, 95%CI (−2.23, −0.70), p = 0.0002], Traditional Chinese Medicine Syndromes (TCMS) scores [MD = −2.45, 95%CI (−3.85, −1.04), p = 0.0006], and hormone levels, including Luteinizing Hormone (LH) [MD = −4.17, 95%CI (−7.42, −0.93), p = 0.01], Follicle-Stimulating Hormone (FSH) [MD = −10.50, 95%CI (−14.80, −6.20), p < 0.00001], and Estradiol (E2) [MD = 12.15, 95%CI (6.79, 17.51), p < 0.00001].
Discussion: The combination therapy demonstrates great efficacy and safety for PMI patients, representing an innovative integrative alternative treatment with high clinical application value.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/view/CRD42024564357, PROSPERO CRD42024564357.
1 Introduction
Before entering menopause, women undergo perimenopause—a critical transitional phase characterized by significant reproductive and hormonal changes (1). According to the STRAW staging criteria, perimenopause includes the early menopausal transition stage (−2) and the late menopausal transition stage (−1), marking the transition from the reproductive period to menopause. During this period, ovarian reserve gradually decreases, menstrual cycles become irregular, and hormone levels experience significant fluctuations (1). Perimenopausal syndrome (PMS), also known as menopausal syndrome (MPS), refers to a series of signs and psychological symptoms caused by women before and after menopause, such as palpitation, hot flashes, night sweats, vaginal dryness, breast pain, sleep disorders, which are rooted in the fluctuation and reduction of sex hormones (2, 3). Insomnia, as one of the common complaints of perimenopausal women, seriously threatens the quality of life of women around the world. In recent years, the prevalence of PMI has attracted increasing attention. Although developed countries have made significant progress in managing perimenopausal symptoms, developing countries still face high prevalence and limited treatment options (4, 5). In China, PMI affects a considerable proportion of the female population, many of whom experience moderate to severe symptoms, which not only interferes with daily activities and reduces the quality of life, but also leads to other health problems, such as depression, anxiety and cardiovascular disease (4, 6).
Currently, the main treatments for PMI include hormone replacement therapy (HRT) and non-hormonal therapies (7). HRT, one of the treatments for severe perimenopausal symptoms, may pose risks such as increased chances of breast cancer, thromboembolic events, and cardiovascular issues (8–10). Non-hormonal therapies, such as sleeping medications, have significant side effects and withdrawal reactions, making the quest for effective and safer alternative treatments crucial for improving PMI (11). Studies have shown that traditional Chinese treatments such as acupuncture and herbal medication are efficacious in improving PMI symptoms (12, 13). Therefore, another promising alternative method, acupuncture combined with medication, has been gradually explored by researchers. This method has shown the effect of relieving perimenopausal symptoms with fewer side effects (14, 15). The combination of acupuncture and medication, either Traditional Chinese Medication (TCM) or Western Medication (WM), can regulate neuroendocrine function, improve sleep quality, reduce levels of anxiety and depression, making it a well-supported option in treating PMI (14). This article aims to explore the effectiveness and safety of the combination therapy of acupuncture and medication in the treatment of PMI through a systematic review and meta-analysis, providing insights into its potential benefits and mechanisms of action.
2 Methods and analysis
2.1 Study registration
According to the guidelines (16), we registered the systematic review protocol in PROSPERO on July 13, 2024 (Registration Number: CRD42024564357).
2.2 Eligibility criteria
2.2.1 Study designs
Only published RCTs were considered for inclusion.
2.2.2 Participants
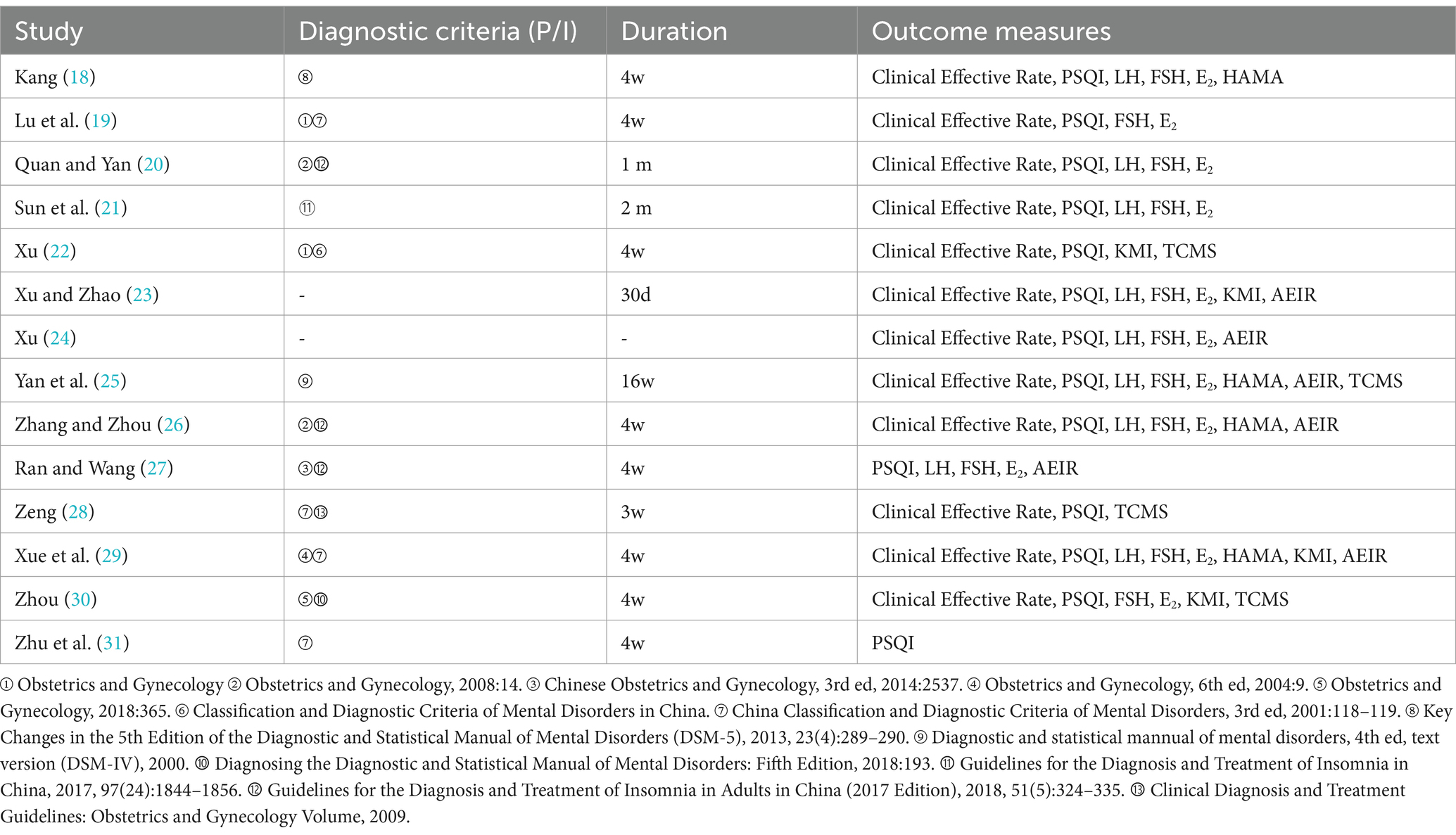
Only peri-menopausal women who met the diagnostic criteria of insomnia were considered for inclusion, with no restrictions on age, duration of the condition, ethnicity, country, or educational level. For specific details, refer to Table 1 and the accompanying note.
2.2.3 Interventions
The treatment group received the combination of acupuncture and medication (both TCM and WM are acceptable), while the control group was treated with WM (Estazolam).
2.2.4 Outcome measures
Primary outcome measures: Clinical Effective Rate, Adverse Event Incidence Rate (AEIR).
Secondary outcome measures: PSQI, LH, FSH, E2, HAMA scores, KMI, TCMS scores.
2.2.5 Language
Only articles reported in Chinese or English were included.
2.3 Search strategy
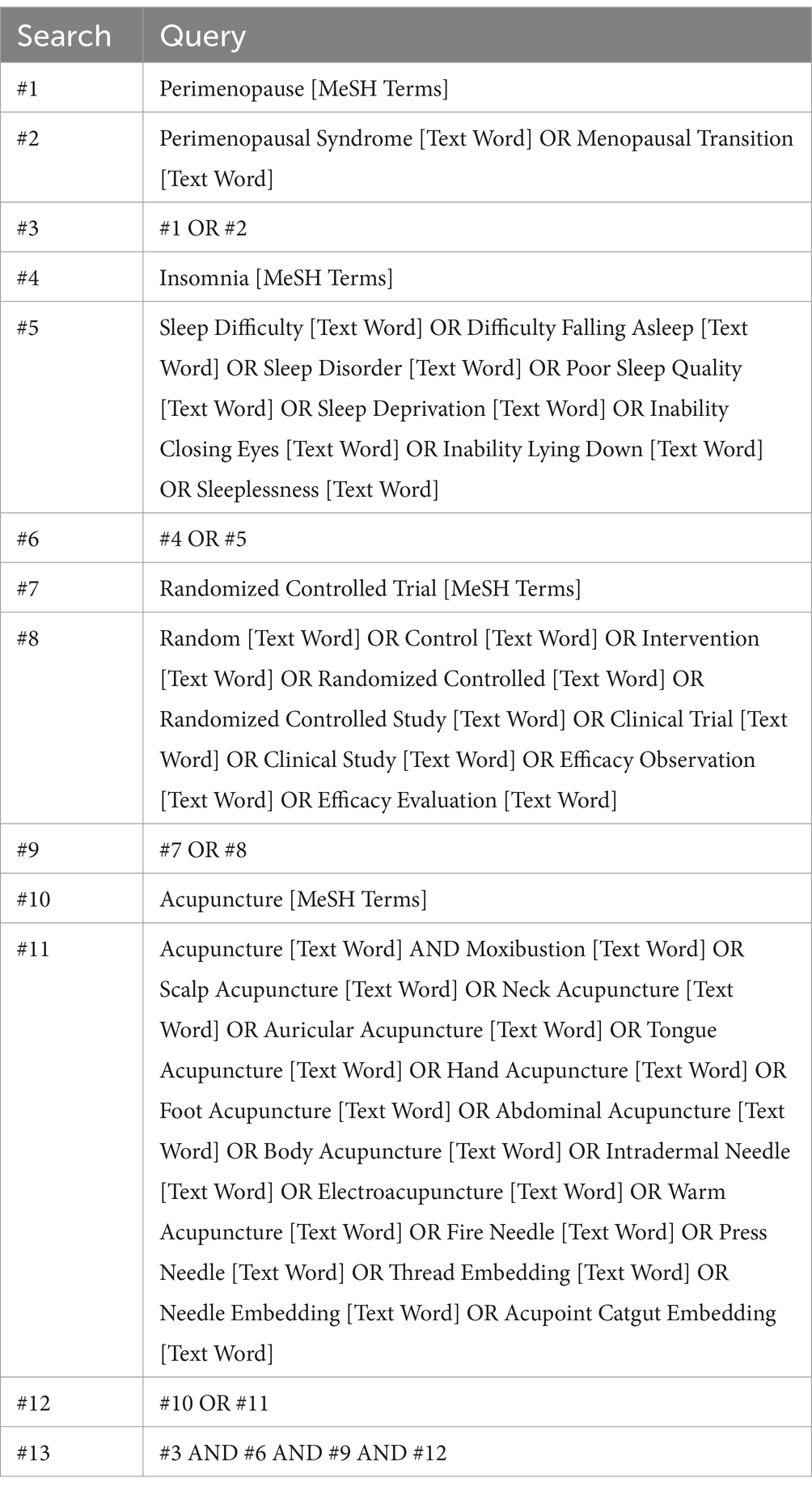
Searches were conducted in the databases of PubMed, Excerpta Medica Database (EMBASE), Cochrane Library, Web of Science, China Biology Medicine Disc (CBM), China National Knowledge Infrastructure (CNKI), Wanfang Academic Journal Full-text Database (Wanfang), and Chongqing VIP Database (CQVIP). The search, which was conducted up to July 1, 2024, utilized both MeSH terms and text word. The search terms include “acupuncture,” “combination therapy,” “perimenopause,” “insomnia,” “RCTs,” etc. Taking PubMed search strategy as an example, refer to Table 2.
2.4 Study selection
Two reviewers (SJ and YZ) independently screened the literature using Endnote 20 software. Studies that failed to meet the selection criteria were excluded. Those with uncertain eligibility underwent a detailed review to ascertain their suitability. Any discrepancies were resolved by consulting a third reviewer (YS).
2.5 Data organisation
Initially, data extraction was performed, with two reviewers (SJ and YZ) independently extracting and cross-checking the data. Any discrepancies were resolved by consulting a third reviewer (YS) who participated in the discussion and decision-making process. The data extraction encompasses the first author, publication date, interventions, sample size, age, course, acupuncture points, medication dosages, diagnostic criteria, duration, and outcome measures.
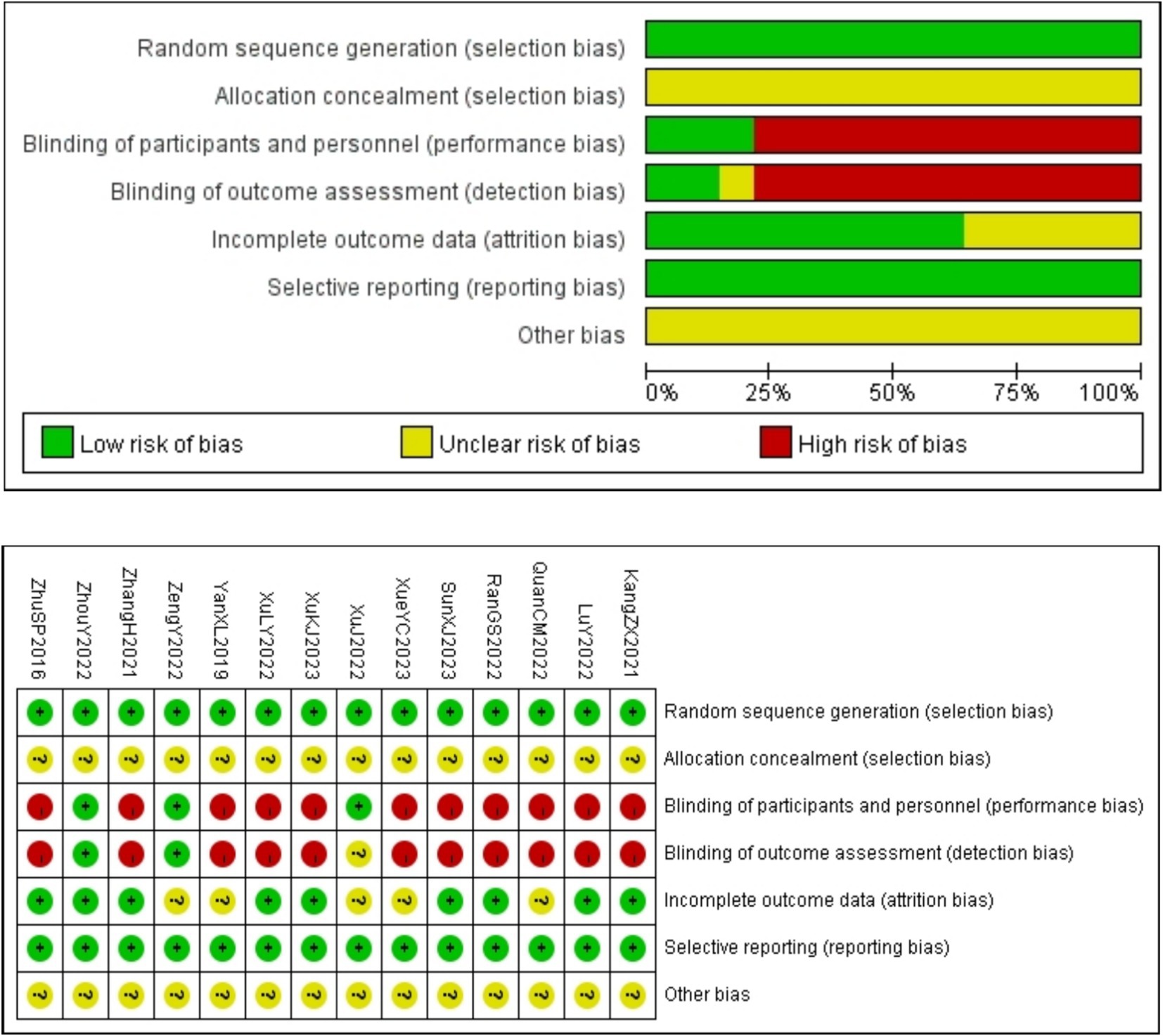
2.6 Quality assessment
The quality assessment of the included studies and the evaluation of risk of bias were conducted in accordance with the guidelines provided in the Cochrane Handbook for Systematic Reviews of Interventions (17). This includes seven items: (1) Generation of a random sequence (selection bias); (2) Concealment of allocation (selection bias); (3) Participant and personnel blinding (performance bias); (4) Outcome assessment blinding (detection bias); (5) Management of incomplete outcome data (attrition bias); (6) Selective data reporting (reporting bias); (7) Other potential biases (other bias). Each item was evaluated as having a “low,” “unclear,” or “high” risk of bias. In case of discrepancies, a third reviewer (SYZ) was consulted to reach a consensus.
2.7 Missing data handling
For missing data, we will prioritize contacting the original authors to obtain the missing information. If the data cannot be supplemented, we will use sensitivity analysis to explore the potential impact of missing data on the final effect evaluation and assess different data handling strategies (such as imputation or exclusion).
2.8 Data synthesis
Meta-analysis was performed using Review Manager 5.4 and Stata 15.0 software. The RR was used for dichotomous variables (count data), and the MD was applied for continuous variables (measurement data). The CI for all effect sizes were set at 95%.
2.9 Heterogeneity assessment
Heterogeneity was assessed using the I2 statistic and p-value. When I2 ≤ 50% and p > 0.1, it indicates low heterogeneity, and a fixed-effect model is applied. When I2 > 50% and p < 0.1, it suggests substantial heterogeneity, and a random-effects model is applied. If necessary, subgroup analysis, sensitivity analysis, and regression analysis are performed.
3 Results
3.1 Study selection
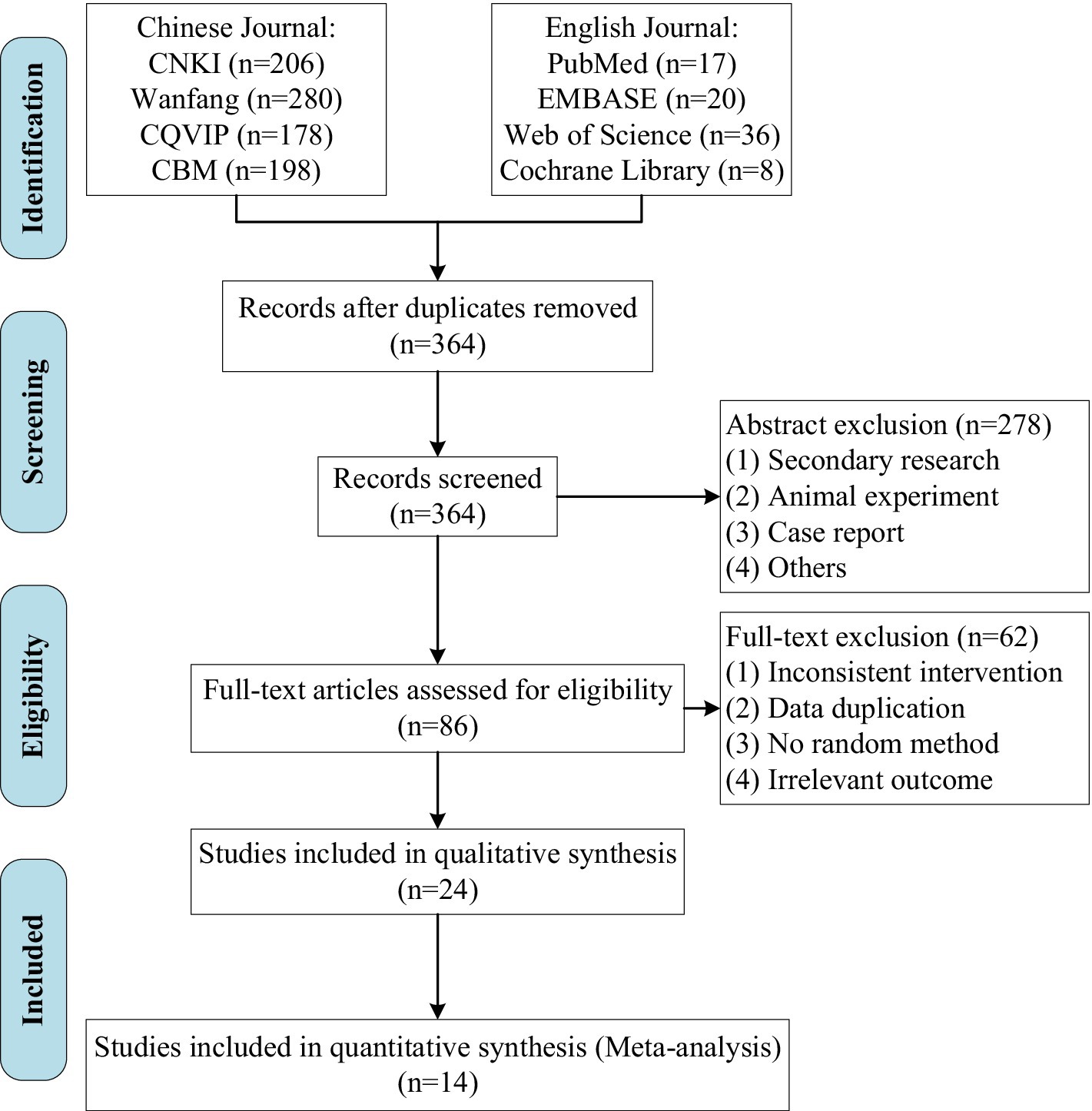
A total of 944 relevant studies were initially retrieved. After applying various inclusion criteria and exclusions, 14 studies (18–31) were ultimately included, as detailed in Figure 1.
3.2 Basic characteristics of the studies
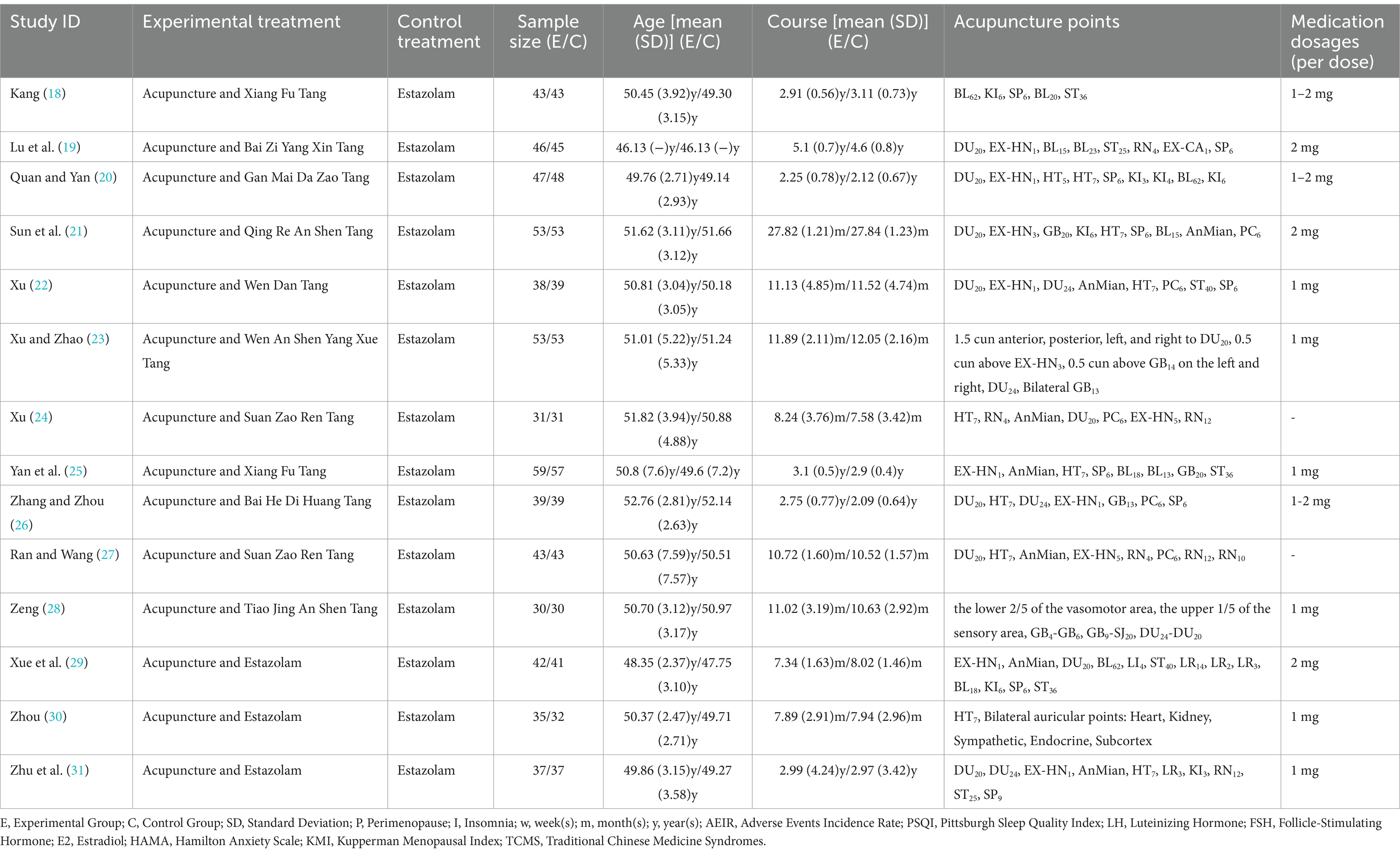
A total of 14 RCTs (18–31) on acupuncture combined with medication for the treatment of PMI included 1,187 patients (596 in the experimental group and 591 in the control group), with baseline data being largely similar. Among these, 12 studies (18–26, 28–30) reported clinical effective rate, 6 studies (23–27, 29) reported the incidence of adverse events, 14 studies (18–31) reported PSQI, 9 studies (18, 20, 21, 23–27, 29) reported LH levels, 11 studies (18–21, 23–27, 29, 30) reported FSH levels, 11 studies (18–21, 23–27, 29, 30) reported E2 levels, 4 studies (18, 25, 26, 29) reported HAMA scores, 4 studies (22, 23, 29, 30) reported KMI, and 4 studies (22, 25, 28, 30) reported TCMS scores. Regarding interventions, 11 studies (18–28) compared acupuncture combined with TCM against sole use of the WM (Estazolam), while 3 studies (29–31) compared acupuncture combined with WM (Estazolam) against sole use of the WM (Estazolam), as detailed in Tables 1, 3.
3.3 Risk of bias assessment
All 14 RCTs (18–31) employed random methods (10 studies (18, 20, 21, 23, 25–27, 29–31) used a random number table method, 2 studies (22, 28) used simple randomization, 1 study (24) used computer-generated randomization, and 1 study (19) used other random allocation schemes), ensuring proper randomization and thereby minimizing selection bias. However, none of the studies reported allocation concealment, which raises concerns about potential selection bias, as the allocation process could be inadvertently influenced by researchers or participants. Blinding was implemented in 3 studies (22, 28, 30) for both participants and personnel, and outcome assessment blinding was also reported in these same 3 studies (22, 28, 30), although the reporting in 1 study (22) was not entirely clear. Due to the specific nature of acupuncture procedures, it is practically impossible to implement blinding. However, since 3 studies (22, 28, 30) explicitly mentioned the use of blinding, we assessed them as low risk. The lack of blinding in the remaining studies may introduce performance and detection biases, potentially affecting the objectivity of the results. Additionally, 5 studies (20, 22, 25, 28, 29) had issues with missing outcome data. For the missing data, we will take appropriate measures for handling it in the subsequent analysis. No selective reporting bias was observed across the assessments, and no other types of bias were identified. Further details are provided in Figure 2.
3.4 Primary outcome measures
3.4.1 Clinical effective rate
A total of 1,027 patients in 12 studies (18–26, 28–30) reported the clinical effective rate of acupuncture combined with medication in treating PMI. Analysis of the extracted data revealed low heterogeneity (p = 0.96 > 0.1; I2 = 0%), so a fixed-effect model was selected. The results indicated that, compared to the control group, acupuncture combined with medication significantly improved insomnia symptoms in perimenopausal women [RR = 1.24, 95%CI (1.17, 1.31), Z = 7.45, p < 0.00001]. Subgroup analysis indicated that the effect of acupuncture combined with TCM [RR = 1.25, 95%CI (1.17, 1.33), Z = 7.06, p < 0.00001] might be slightly better than that of acupuncture combined with WM [RR = 1.18, 95%CI (1.03, 1.36), Z = 2.39, p = 0.02 < 0.05], but this advantage did not reach a significant difference due to small sample sizes, as detailed in Figure 3.
3.4.2 AEIR
A total of 531 patients in 6 studies (23–27, 29) reported the AEIR of acupuncture combined with medication in treating PMI. Analysis of the extracted data revealed low heterogeneity (p = 0.60 > 0.1; I2 = 0%), so a fixed-effect model was selected. The results indicated that, compared to the control group, the incidence of adverse events of the combination therapy was significantly reduced with statistical significance [RR = 0.31, 95%CI (0.18, 0.53), Z = 4.31, p < 0.0001], as detailed in Figure 4.
3.5 Secondary outcome measures
3.5.1 PSQI
A total of 1,187 patients in 14 studies (18–31) reported the PSQI of acupuncture combined with medication in treating PMI. Analysis of the extracted data revealed high heterogeneity (p < 0.00001; I2 = 99%), so a random-effects model was selected. The results indicated that, compared to the control group, combination therapy was more effective in improving PSQI with statistical significance [MD = −2.77, 95%CI (−4.11, −1.43), Z = 4.05, p < 0.0001]. Sensitivity analysis, as shown in the Supplementary image, indicated stable results. Systematically removing studies one at a time fails to make heterogeneity reduce significantly. Subgroup analysis was followed by regression analysis, as detailed in Figure 5.
3.5.2 LH
A total of 818 patients in 9 studies (18, 20, 21, 23–27, 29) reported the LH levels of acupuncture combined with medication in treating PMI. Analysis of the extracted data revealed high heterogeneity (p < 0.00001; I2 = 95%), so a random-effects model was selected. The results indicated that, compared to the control group, combination therapy was more effective in improving LH levels with statistical significance [MD = −4.17, 95%CI (−7.42, −0.93), Z = 2.52, p = 0.01 < 0.05]. Sensitivity analysis, as shown in the Supplementary image, indicated stable results. Systematically removing studies one at a time fails to make heterogeneity reduce significantly. After subgroup analysis, regression analysis was conducted, as detailed in Figure 6.
3.5.3 FSH
A total of 976 patients in 11 studies (18–21, 23–27, 29, 30) reported the FSH levels of acupuncture combined with medication in treating PMI. Analysis of the extracted data revealed high heterogeneity (p < 0.00001; I2 = 97%), so a random-effects model was selected. The results indicated that, compared to the control group, combination therapy was more effective in improving FSH levels with statistical significance [MD = −10.50, 95%CI (−14.80, −6.20), Z = 4.79, p < 0.00001]. Sensitivity analysis, as shown in the Supplementary image, indicated stable results. Systematically removing studies one at a time fails to make heterogeneity reduce significantly. After subgroup analysis, regression analysis was conducted, as detailed in Figure 7.
3.5.4 E2
A total of 976 patients in 11 studies (18–21, 23–27, 29, 30) reported the E2 levels of acupuncture combined with medication in treating PMI. Analysis of the extracted data revealed high heterogeneity (p < 0.00001; I2 = 97%), so a random-effects model was selectd. The results indicated that, compared to the control group, combination therapy was more effective in improving E2 levels with statistical significance [MD = 12.15, 95%CI (6.79, 17.51), Z = 4.44, p < 0.00001]. Sensitivity analysis, as shown in the Supplementary image, indicated stable results. Systematically removing studies one at a time fails to make heterogeneity reduce significantly. After subgroup analysis, regression analysis was conducted, as detailed in Figure 8.
3.5.5 HAMA
A total of 363 patients in 4 studies (18, 25, 26, 29) reported the HAMA scores of acupuncture combined with medication in treating PMI. Analysis of the extracted data revealed moderate heterogeneity (p = 0.07 < 0.1; I2 = 57%), so a random-effects model was selected. The results indicated that, compared to the control group, combination therapy was more effective in improving HAMA scores with statistical significance [MD = −3.11, 95%CI (−3.82, −2.40), Z = 8.59, p < 0.00001]. Subgroup analysis did not significantly reduce heterogeneity. Sensitivity analysis, as shown in the Supplementary image, indicated stable results. Systematically removing studies one at a time (Table 4), it was found that excluding Kang (18) significantly reduced heterogeneity (p = 0.96 > 0.1; I2 = 0%), suggesting that this study might be a source of heterogeneity. Change to a fixed-effect model [MD = −3.45, 95%CI (−3.94, −2.97), Z = 14.01, p < 0.00001], as detailed in Figure 9.
3.5.6 KMI
A total of 333 patients in 4 studies (22, 23, 29, 30) reported the KMI of acupuncture combined with medication in treating PMI. Analysis of the extracted data revealed high heterogeneity (p < 0.00001; I2 = 95%), so a random-effects model was selected. The results indicated that, compared to the control group, combination therapy was more effective in improving KMI with marginal statistical significance [MD = −2.64, 95%CI (−5.24, −0.03), Z = 1.98, p = 0.05]. Subgroup analysis did not significantly reduce heterogeneity. Sensitivity analysis, as shown in the Supplementary image, indicated stable results. Systematically removing studies one at a time (Table 5), it was found that excluding Xue et al. (29) significantly reduced heterogeneity (p = 0.51 > 0.1; I2 = 0%), suggesting that this study might be a source of heterogeneity. Change to a fixed-effect model [MD = −1.46, 95%CI (−2.23, −0.70), Z = 3.75, p = 0.0002 < 0.05], as detailed in Figure 10.
3.5.7 TCMS
A total of 320 patients in 4 studies (22, 25, 28, 30) reported the TCMS scores of acupuncture combined with medication in treating PMI. Analysis of the extracted data revealed high heterogeneity (p < 0.00001; I2 = 100%), so a random-effects model was selected. The results indicated that, compared to the control group, combination therapy was more effective in improving TCM scores but not statistically significant [MD = −10.11, 95%CI (−25.40, 5.17), Z = 1.30, p = 0.19 > 0.05]. Subgroup analysis did not significantly reduce heterogeneity. Sensitivity analysis, as shown in the Supplementary image, indicated stable results. Systematically removing studies one at a time (Table 6), it was found that excluding Yan et al. (25) reduced heterogeneity to a moderate level (p = 0.12 > 0.1; I2 = 52%), suggesting that this study might be a source of heterogeneity. The overall effect reached statistical significance [MD = −2.45, 95%CI (−3.85, −1.04), Z = 3.42, p = 0.0006 < 0.05], as detailed in Figure 11.
3.6 Subgroup analysis, sensitivity analysis and regression analysis
Two subgroups were created based on the different interventions: one for acupuncture combined with TCM and the other for acupuncture combined with WM. For outcome measures with significant heterogeneity remaining after subgroup analysis, sensitivity analysis was conducted to assess robustness, and studies were excluded one by one to identify the source of heterogeneity. Regression analysis was performed for those outcome measures where heterogeneity remained unresolved. The detailed results can be found in the Supplementary materials.
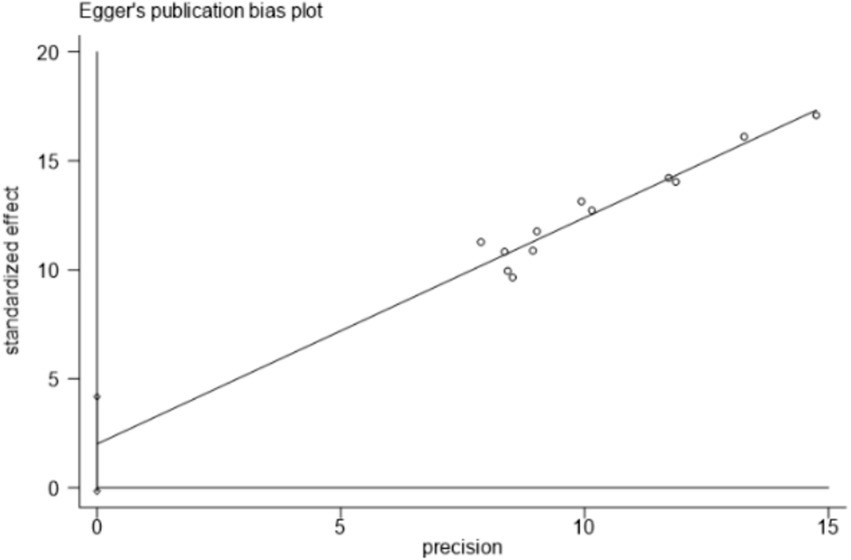
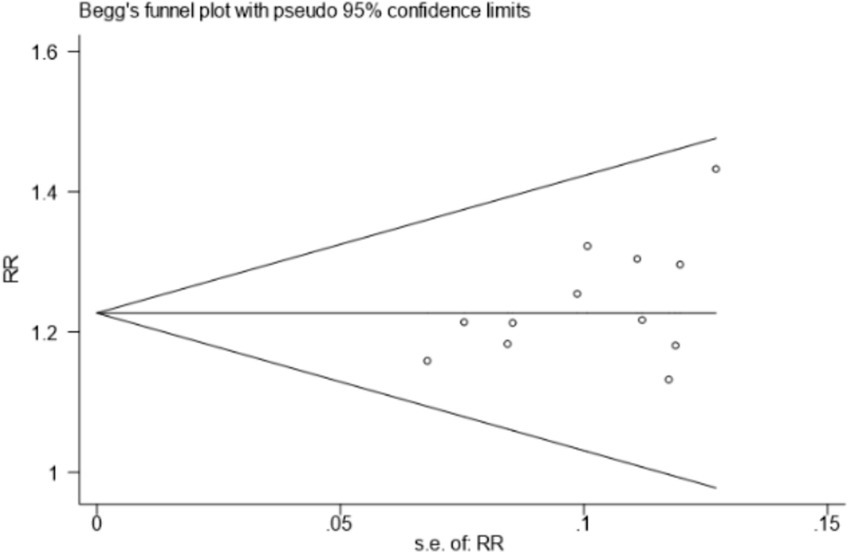
3.7 Assessment of publication bias
A funnel plot was generated using the clinical effective rate as an indicator to assess publication bias. The results showed that the scatter plot distribution was not completely symmetrical, suggesting a potential for publication bias. The Egger test using Stata 15.0 software showed that the scatter points deviated significantly from the regression line in the high precision area, indicating potential publication bias. However, further statistical testing of the regression analysis p-value suggested that there might not be significant publication bias (t = 2.07, p = 0.065 > 0.05). The Begg test revealed that the points were relatively evenly distributed and most points were close to the regression line, confirming that the study results were not significantly affected by publication bias, as detailed in Figures 12–14.
3.8 Quality of evidence grading
We utilized GRADEprofiler software to evaluate it. The assessment results showed that the quality of evidence is relatively high. Further details are provided in the Supplementary materials.
4 Discussion
PMI is closely related to a variety of physiological and psychological factors (2, 32). During perimenopause, ovarian function gradually decreases, with estrogen and progesterone levels fluctuate significantly, which not only affects women’s physiological functions, but also leads to a series of psychiatric symptoms such as insomnia and depression (33, 34), or even affects daily life. Sleep regulation is controlled by both lower and higher centers, and when hormonal fluctuations affect cortical function, the higher center’s regulation of the sleep center is weakened, leading to sleep structure disruption and insomnia (35, 36). In addition, the decline in estrogen may inhibit the synthesis and secretion of neurotransmitters such as 5-hydroxytryptamine (5-HT) and γ-aminobutyric acid (GABA), thereby affecting mood regulation and sleep quality (36). According to the Inner Canon of the Yellow Emperor (Huangdi Neijing), perimenopause is described as the cessation of menstruation, aligning with the concept of perimenopause. PMI falls under the category of gynecological disorders related to insomnia and is closely linked to various internal and external factors (6). The main pathogenesis, including liver and kidney deficiency, imbalance of yin and yang, deficiency of both the heart and spleen, and disharmony of qi and blood, may be closely related to changes in endocrine levels, leading to imbalances in qi and blood, emotional instability, and sleep disturbances (37). TCM adopts a syndrome differentiation approach, using acupuncture and herbal medication to regulate organ functions and improve sleep, which complements the management of hormone imbalances in WM. Recent studies have compared the distribution of Governor Meridian vessels with the hypothalamic–pituitary–adrenal (HPA) axis, finding that electroacupuncture stimulation at points along the Governor Meridian can effectively reduce HPA related hormones [cortisol (CORT), adrenocorticotrophin (ACTH), and corticotropin-releasing hormone (CRH)] and hypothalamic–pituitary-ovarian (HPO) axis related hormones (FSH and LH), alleviating clinical symptoms of PMI (38). In terms of herbal medication, commonly used formulas include Liuwei Dihuang Pill and Jiawei Yigan Powder, focusing on nourishing kidney yin, replenishing liver blood, and calming the mind, all showing great efficacy for PMI (39). Li (15) performed a meta-analysis, demonstrating that acupuncture combined with TCM is more effective and safe in treating PMI. In contrast, WM commonly uses sedative-hypnotic drugs, but long-term use can lead to tolerance and cognitive impairments such as memory decline (40). One study found that nighttime pressure on the Shenmen point (HT7) on the wrist increased the rhythm of urinary melatonin metabolites within 24 h without adverse effects, suggesting that acupoint stimulation might naturally improve sleep quality in insomnia patients and could be more advantageous than using WM alone (41). Zhao (42) confirmed through a meta-analysis that acupuncture combined with WM is highly effective. The mechanisms of acupuncture combined with medication for treating PMI are multifaceted, with fewer side effects, making this method simpler and potentially suitable as an alternative therapy for widespread clinical use (43).
For the definition and specific measurement methods of the outcome measure labeled “Clinical Effective Rate,” 7 studies (18, 20, 23, 25, 28–30) employed the “Guidelines for Clinical Research of New Traditional Chinese Medicines,” 1 study (19) utilized the “Guidelines for Clinical Research of New Traditional Chinese Medicine for Treating Insomnia,” 1 study (21) used the “Chinese Guidelines for the Diagnosis and Treatment of Insomnia,” and 1 study (22) incorporated both sets of guidelines. However, 2 studies (24, 26) did not specify the use of any internationally recognized evaluation criteria, which may introduce additional heterogeneity and lead to inconsistencies in treatment outcome assessments. To improve the comparability of future studies and the robustness of meta-analysis results, it is essential to establish clear, standardized, and internationally recognized criteria for evaluating efficacy.
Heterogeneity management revealed that the group variable significantly affected FSH and E2 levels, while the subgroups showed no significant difference in their impact on PSQI and LH levels, suggesting other potential sources of heterogeneity. The treatment approaches of acupuncture combined with TCM and acupuncture combined with WM involve significant differences in mechanisms and implementation, which may contribute to heterogeneous treatment effects. In addition, patient physiological characteristics and external factors (geographical and cultural differences, treatment adherence, and genetic background) may also impact the stability of the results. To more accurately identify and quantify the sources of heterogeneity, subsequent research may consider finer subgroup divisions and standardized assessment tools, or, when appropriate, the use of mixed-effects models and Bayesian methods for further exploration. By taking these factors into account, a more comprehensive understanding of the variability in intervention effects can be achieved, providing a basis for the individualized development of treatment plans.
This study has the following advantages: (1) This article comprehensively assessed the effectiveness and safety of combination therapy in treating PMI; (2) The search scope covered 8 databases, including both Chinese and English, making the results relatively comprehensive and extensive; (3) This study used established clinical outcome indicators.
This study still has some limitations: (1) The studies included are all in Chinese, which may introduce language bias and limit the generalizability of the findings to non-Chinese populations, especially given the ongoing shortage of high-quality blinded clinical trials; (2) During the data collection process, the same indicators in different studies use different units, and there are no internationally recognized conversion standards between some of these units, which poses difficulties for analysis; (3) Some indicators still show significant heterogeneity, and other potential subgroups should be considered; (4) Due to the lack of sufficient data and supporting literature, a more in-depth discussion on the relationship between effect size and the Minimal Clinically Important Difference (MCID) was not conducted; (5) Insufficient attention has been given to the high homogeneity of the included studies.
Considering the above limitations, future research should select databases in multiple languages to reduce bias caused by language differences; adopt strict inclusion criteria and refine subgroups; consider large-scale, multicenter RCTs to assess the effectiveness of integrated treatments in a more comprehensive manner; and expand data sources to enable a deeper exploration of the relationship between effect size and the Minimal Clinically Important Difference (MCID). By implementing these strategies, the clinical value of acupuncture combined with medication can be further established, promoting the development of individualized treatment plans and ultimately enhancing overall patient outcomes and quality of life.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
SJ: Data curation, Formal analysis, Methodology, Software, Visualization, Writing – original draft, Writing – review & editing. YZ: Data curation, Software, Writing – review & editing. YS: Funding acquisition, Methodology, Project administration, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. Heilongjiang Postdoctoral Scientific Research Developmental Fund (No. LBH-Q21183) and Heilongjiang University of Chinese Medicine Scientific Research Fund Project (No. 2019MS21).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2025.1476719/full#supplementary-material
References
1. Harlow, SD, Gass, M, Hall, JE, Lobo, R, Maki, P, Rebar, RW, et al. STRAW+ 10 collaborative group. Executive summary of the stages of reproductive aging workshop+ 10: addressing the unfinished agenda of staging reproductive aging. J Clin Endocrinol Metab. (2012) 97:1159–68. doi: 10.1210/jc.2011-3362
2. Dennerstein, L, Dudley, EC, Hopper, JL, Guthrie, JR, and Burger, HG. A prospective population-based study of menopausal symptoms. Obstet Gynecol. (2000) 96:351–8. doi: 10.1016/s0029-7844(00)00930-3
3. Santoro, N, Epperson, CN, and Mathews, SB. Menopausal symptoms and their management. Endocrinol Metab Clin. (2015) 44:497–515. doi: 10.1016/j.ecl.2015.05.001
4. Ruan, X, Cui, Y, Du, J, Jin, F, and Mueck, AO. Prevalence of climacteric symptoms comparing perimenopausal and postmenopausal Chinese women. J Psychosom Obstet Gynecol. (2017) 38:161–9. doi: 10.1080/0167482X.2016.1244181
5. Rasgon, N, Shelton, S, and Halbreich, U. Perimenopausal mental disorders: epidemiology and phenomenology. CNS Spectr. (2005) 10:471–8. doi: 10.1017/S1092852900023166
6. Sun, D, Shao, H, Li, C, and Tao, M. An analysis of the main reasons that perimenopausal and postmenopausal women in China have for seeking outpatient treatment and factors influencing their symptoms: a single-center survey. Clin Exp Obstet Gynecol. (2015) 42:146–51. doi: 10.12891/ceog1744.2015
7. Carpenter, J, Gass, ML, Maki, PM, Newton, KM, Pinkerton, JV, Taylor, M, et al. Nonhormonal management of menopause-associated vasomotor symptoms: 2015 position statement of the North American Menopause Society. Menopause. (2015) 22:1155–74. doi: 10.1097/GME.0000000000000546
8. Choi, E, Lee, JK, Baek, JK, Chung, Y, Kim, H, Yun, BH, et al. Hormone replacement therapy and breast cancer incidence in Korean women. Maturitas. (2024) 183:107946. doi: 10.1016/j.maturitas.2024.107946
9. Simon, T, and Jaillon, P. Hormone replacement therapy and cardiovascular risk in menopausal women. Arch Mal Coeur Vaiss. (2001) 94:132–8.
10. Canonico, M, Oger, E, Plu-Bureau, G, Conard, J, Meyer, G, Lévesque, H, et al. Hormone therapy and venous thromboembolism among postmenopausal women: impact of the route of estrogen administration and progestogens: the ESTHER study. Circulation. (2007) 115:840–5. doi: 10.1161/CIRCULATIONAHA.106.642280
11. Ovsyannikova, TV, Makarov, IO, and Kulikov, IA. Clinical efficacy of non-hormonal methods of therapy in perimenopausal women. Obstet Gynecol Reprod. (2016) 7:26–9.
12. Shi, R, Meng, W, Liu, Z, Xue, W, Chen, X, and Deng, Y. Exploring acupuncture as a treatment for insomnia in perimenopausal women with stable angina pectoris: a protocol for a randomized, double-blind, placebo-controlled clinical trial. PLoS One. (2024) 19:e0301827. doi: 10.1371/journal.pone.0301827
13. Gingrich, PM, and Fogel, CI. Herbal therapy use by perimenopausal women. J Obstet Gynecol Neonatal Nurs. (2003) 32:181–9. doi: 10.1177/0884217503251706
14. Cui, CH, Qu, Z, Chen, YJ, and Fu, SG. Clinical study on acupuncture combined with medicine for treatment of insomnia in Perimenopausal women with kidney deficiency and liver stagnation type. Chin Arch Tradit Chin Med. (2023) 41:78–81. doi: 10.13193/j.issn.1673-7717.2023.11.018
15. Li, Z, Yin, S, Feng, J, Gao, X, Yang, Q, and Zhu, F. Acupuncture combined with Chinese herbal medicine in the treatment of perimenopausal insomnia: a systematic review and meta-analysis. Medicine. (2023) 102:e35942. doi: 10.1097/MD.0000000000035942
16. Page, MJ, JE, MK, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
17. Higgins, JP, Altman, DG, Gøtzsche, PC, Jüni, P, Moher, D, Oxman, AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. (2011) 343:d5928. doi: 10.1136/bmj.d5928
18. Kang, ZX. Clinical study on acupuncture combined with modified Xiangfu decoction for treating Perimenopausal insomnia with liver qi stagnation syndrome. Pract Clin J Integ Tradition Chin Western Med. (2021) 21:35–6. doi: 10.13638/j.issn.1671-4040.2021.01.014
19. Lu, Y, Li, CC, Gao, T, and Guo, YY. Clinical observation on treatment of Peri-menopausal insomnia with Baizi Yangxin decoction and acupuncture. J Pract Tradition Chin Int Med. (2022) 36:8–10. doi: 10.13729/j.issn.1671-7813.Z20210186
20. Quan, CM, and Yan, QL. The effect of the Ganmai Dazao decoction plus Yuanluo acupuncture on female menopausal insomnia and its influence on serum neurotransmitter levels. Clin J Chin Med. (2022) 14:63–6. doi: 10.3969/j.issn.1674-7860.2022.25.017
21. Sun, XJ, Zhao, KN, Liu, BX, and Chen, L. Clinical observation of acupuncture combined with heat clearing and mind calming decoction in the treatment of perimenopausal insomnia. Guangxi J Tradition Chin Med. (2023) 46:27–9.
22. Xu, J. Clinical study of Wendan decoction combined with head acupuncture and Limbal acupuncture in the treatment of syndrome of phlegm-heat based Perimenopausal insomnia. Nanchang, China: Jiangxi University of Chinese Medicine (2022).
23. Xu, LY, and Zhao, YR. Therapeutic observation of Wen'an Shenyangxue decoction combined with Jinsan needle in the treatment of perimenopausal insomnia patients. Clin Educ Gen Pract. (2022) 20:425–8. doi: 10.13558/j.cnki.issn1672-3686.2022.005.012
24. Xu, KJ. The clinical effect of Suanzaoren decoction combined with acupuncture on perimenopausal insomnia. Mat Child Nurs. (2023) 3:5034–6. doi: 10.3969/j.issn.2097-0838.2023.20.086
25. Yan, XL, Yu, YD, and Yang, DD. Clinical efficacy of acupuncture combined with modified Xiangfu decoction in treatment of menopausal insomnia cause by liver qi stagnation. China J Chin Mat Med. (2020) 45:1460–4. doi: 10.19540/j.cnki.cjcmm.20191010.501
26. Zhang, H, and Zhou, Q. Efficacy of Baihe Dihuang decoction combined with Zhenjing Anshen acupuncture in the treatment of female menopausal insomnia and influence on anxiety and depression. World J Integ Tradition Western Med. (2021) 16:405–9. doi: 10.13935/j.cnki.sjzx.210303
27. Ran, GS, and Wang, Y. Clinical study on supplemented sour jujube decoction combined with acupuncture and Moxibustion in treating Perimenopausal insomnia. Henan Tradition Chin Med. (2022) 42:1644–7. doi: 10.16367/j.issn.1003-5028.2022.11.0348
28. Zeng, Y. Clinical observation of Perimenopausal sub-health insomnia by scalp acupuncture combined with Tiaojing Anshen decoction. Luzhou, China: Southwest Medical University (2022).
29. Xue, YC, Chen, L, and Hua, CF. Clinical effect of Jieyu Jianpi acupuncture combined with estazolam tablets on perimenopausal insomnia of liver spleen deficiency. Hebei J Tradit Chin Med. (2023) 45:1712–1716+1720. doi: 10.3969/j.issn.1002-2619.2023.10.030
30. Zhou, Y. Clinical observation of superficial needling on auricular point combine with Estazolam in the treatment of Perimenopausal insomnia with heart-kidney disharmony. Fuzhou, China: Fujian University of Traditional Chinese Medicine (2022).
31. Zhu, SP, Li, PP, and Zhu, XL. Observation of the therapeutic effect of Tiao Du an Shen acupuncture method on Perimenopausal insomnia. Modern J Integ Tradition Chin Western Med. (2016) 25:2885–8. doi: 10.3969/j.issn.1008-8849.2016.26.011
32. Smith, RL, Flaws, JA, and Mahoney, MM. Factors associated with poor sleep during menopause: results from the midlife Women's health study. Sleep Med. (2018) 45:98–105. doi: 10.1016/j.sleep.2018.01.012
33. Haufe, A, Baker, FC, and Leeners, B. The role of ovarian hormones in the pathophysiology of perimenopausal sleep disturbances: a systematic review. Sleep Med Rev. (2022) 66:101710. doi: 10.1016/j.smrv.2022.101710
34. de Zambotti, M, Colrain, IM, and Baker, FC. Interaction between reproductive hormones and physiological sleep in women. J Clin Endocrinol Metab. (2015) 100:1426–33. doi: 10.1210/jc.2014-3892
35. Freedman, RR, and Roehrs, TA. Sleep disturbance in menopause. Menopause. (2007) 14:826–9. doi: 10.1097/gme.0b013e3180321a22
36. Moline, ML, Broch, L, Zak, R, and Gross, V. Sleep in women across the life cycle from adulthood through menopause. Sleep Med Rev. (2003) 7:155–77. doi: 10.1053/smrv.2001.0228
37. Zhao, FY, Fu, QQ, Spencer, SJ, Kennedy, GA, Conduit, R, Zhang, WJ, et al. Acupuncture: a promising approach for comorbid depression and insomnia in perimenopause. Nat Sci Sleep. (2021) 13:1823–63. doi: 10.2147/NSS.S332474
38. Tang, Y, Zheng, QC, Huang, JF, and Chen, Y. Effect of acupuncture on the endocrine axis in patients with perimenopausal insomnia: a case series study. World J Acupunct Moxibustion. (2023) 33:97–101. doi: 10.1016/j.wjam.2022.05.007
39. Yao, ZY, and Chen, H. Recent development of Peri-menopausal insomnia treated by traditional Chinese medicine. Chin Arch Tradit Chin Med. (2014) 32:627–9. doi: 10.13193/j.issn.1673-7717.2014.03.062
40. Proserpio, P, Marra, S, Campana, C, Agostoni, EC, Palagini, L, Nobili, L, et al. Insomnia and menopause: a narrative review on mechanisms and treatments. Climacteric. (2020) 23:539–49. doi: 10.1080/13697137.2020.1799973
41. Nordio, M, and Romanelli, F. Efficacy of wrists overnight compression (HT 7 point) on insomniacs: possible role of melatonin? Minerva Med. (2008) 99:539–47.
42. Zhao, FY, Fu, QQ, Kennedy, GA, Conduit, R, Wu, WZ, Zhang, WJ, et al. Comparative utility of acupuncture and western medication in the management of perimenopausal insomnia: a systematic review and meta-analysis. Evid Based Complement Alternat Med. (2021) 2021:5566742. doi: 10.1155/2021/5566742
Keywords: acupuncture, medication, combination therapy, perimenopause, menopause, insomnia, systematic review, meta-analysis
Citation: Jiang S, Zhang Y and Sun Y (2025) The effectiveness and safety of acupuncture combined with medication in the treatment of perimenopausal insomnia: a systematic review and meta-analysis. Front. Neurol. 16:1476719. doi: 10.3389/fneur.2025.1476719
Edited by:
Xu Zhai, China Academy of Chinese Medical Sciences, ChinaReviewed by:
Hee Geun Jo, Gachon University, Republic of KoreaWendi Wang, China Institute of Sport Science, China
Jieying Zhang, First Teaching Hospital of Tianjin University of Traditional Chinese Medicine, China
Copyright © 2025 Jiang, Zhang and Sun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yingzhe Sun, c3VueWluZ3poZTE5ODdAc2luYS5jb20=
 Shengwen Jiang
Shengwen Jiang