
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol., 27 March 2025
Sec. Neurorehabilitation
Volume 16 - 2025 | https://doi.org/10.3389/fneur.2025.1467843
This article is part of the Research TopicIntegrated Clinical Management and Neurorehabilitation for Lumbosacral Spinal DiseasesView all 12 articles
Background: Numerous studies have confirmed the significant benefits of exercise rehabilitation in both preoperative and postoperative treatment of lumbar disc herniation. However, there is a prevalent fear or avoidance of exercise among patients with chronic low back pain prior to surgery, while research on exercise fear after lumbar fusion remains insufficient. This study aims to investigate the incidence and severity of exercise fear in patients with chronic low back pain and leg pain following lumbar fusion surgery, as well as analyze its underlying mechanism and associated risk factors.
Methods: A cross-sectional study was conducted on patients undergoing posterior lumbar fusion for lumbar disc herniation between May 2023 and January 2024. The Tampa Motor Phobia Scale (TSK-17) was utilized to assess motor fear among participants. Additionally, clinical and imaging risk factors were analyzed through multivariate regression analysis to determine relevant influencing factors.
Results: Following strict inclusion and exclusion criteria, a total of 178 patients who underwent posterior lumbar fusion were included in this study, comprising 104 males (58.4%). Kinesiophobia was defined as a TSK-17 score ≥ 37, which identified 65.2% (116/178) of the screened patients exhibiting motor phobia. Multivariate regression analysis revealed that motor phobia was strongly associated with age, higher levels of pain intensity, elevated Beck Depression Inventory (BDI) scores, lower General Self-Efficacy Scale (GSES) scores, increased number of surgical levels involved during operation, greater amount of postoperative incision drainage, higher degree of nerve root compression observed on preoperative lumbar MRI scans, as well as smaller area occupied by the paravertebral muscles in the lumbar region.
Conclusion: This study has identified a significantly high incidence of postoperative exercise fear in patients undergoing posterior lumbar fusion, along with potential risk factors. Therefore, it is crucial for clinicians to closely evaluate and monitor these patients in order to develop appropriate strategies for postoperative exercise rehabilitation.
Lumbar interbody fusion (LIF) is a primary surgical technique for treating Lumbar disc herniation (LDH), which has demonstrated significant efficacy and widespread clinical application (1). LIF surgery effectively alleviates clinical symptoms, prevents neurological function deterioration by fully decompressing the dural sac and nerve roots compressed by the intervertebral disc’s nucleus pulposus, and achieves stable internal fixation and reliable fusion (2, 3). With an increasing incidence of LDH in younger individuals and an aging population, there has been a steady rise in the number of LIF surgeries performed annually, leading to a growing demand for postoperative rehabilitation (4, 5). Numerous studies have confirmed that exercise rehabilitation plays a crucial role in both pre- and post-operative treatment of lumbar disc herniation (6). Postoperative exercise rehabilitation is an essential component of non-pharmacological therapy aimed at enhancing lower back muscle strength, improving lumbar spine stability, reducing postoperative pain, enhancing lumbar function recovery, and ultimately improving patients’ quality of life (7–9). Typically initiated upon patient awakening from anesthesia after lumbar surgery with focus on the first six months following surgery. Early exercises primarily involve axis turning as well as sitting-to-standing transitions training. Subsequently progressing to standing up from bed followed by walking exercises. Other therapeutic exercises include early ankle pump exercises along with single straight leg raises while double straight leg raises are introduced during intermediate stages. Later stages incorporate yoga ball training into the program (10).
Kinesiophobia refers to an excessive, irrational fear and avoidance of movement or activity that can be debilitating (11). During the acute stage of pain, fear of exercise serves as a defensive behavior strategy to protect the body from further injury (12). However, in the long term, it becomes detrimental as it may lead to decreased motor function and disability due to lack of physical activity, while also increasing the risk of depression and anxiety (13). Research has demonstrated a positive correlation between the severity of kinesiophobia and postoperative pain intensity and dysfunction, while negatively impacting quality of life (13, 14).
Kinesiophobia is prevalent in the preoperative phase of patients with chronic Low Back Pain (LBP) (15). Even after surgical intervention to relieve pathological compression, a significant number of patients continue to exhibit preoperative exercise psychology and behavior (16, 17). A study (12) revealed that LBP patients with high levels of exercise phobia had a 41% higher risk of physical disability compared to those without exercise phobia. Given that Lumbar Interbody Fusion (LIF) entails longer duration and greater trauma than simple discectomy or decompression, it results in worse lower back muscle strength and increased damage, making early motor rehabilitation particularly crucial (18). Currently, there is insufficient research on exercise fear among patients following LIF surgery, with most studies limited to investigating patient compliance with exercise rehabilitation training. Previous studies have identified kinesiophobia as an important factor influencing compliance with exercise rehabilitation in chronic LBP patients; however, few studies have explored the occurrence of kinesiophobia specifically in post-LIF surgery patients. Furthermore, existing studies primarily analyze the relationship between exercise fear and subjective variables such as pain, self-care ability, social support, and emotion while neglecting objective imaging variables. The decline in function observed in key core muscles like multifidus and erector spinae is closely associated with LBP (19). Fear of exercising can exacerbate low back pain symptoms after surgery; nevertheless, whether there exists a causal relationship between lumbar and dorsal muscles’ condition and post-surgery fear of exercising remains unexplored.
Therefore, the objective of this study is to comprehensively investigate the prevalence of kinesiophobia in patients following lumbar interbody fusion (LIF) by considering demographic characteristics, general clinical data, and imaging parameters. Additionally, we aim to analyze the factors influencing kinesiophobia and provide guidance for healthcare professionals to promptly implement intervention measures such as health education and exercise rehabilitation programs for high-risk individuals. Ultimately, our goal is to prevent delayed recovery or dysfunction of the lumbar spine caused by exercise phobia.
A cross-sectional study was conducted on patients with lumbar disc herniation who underwent posterior lumbar fusion surgery at our orthopedic center between May 2023 and January 2024. This study received ethical approval from our hospital’s Ethics Committee (Approval number: 2022-119), and all participants were provided with informed consent before voluntarily participating in the study.
The inclusion criteria for this study were as follows: (1) Lumbar disc herniation was diagnosed based on clinical symptoms, with a disease duration of more than 3 months, regardless of the presence or absence of lumbar spinal stenosis; (2) Pathological anatomical features corresponding to clinical symptoms were confirmed by clear and accurate MRI imaging; (3) Surgical indications for posterior lumbar interbody fusion were met: A history of lumbar intervertebral disc protrusion for more than 6 to 12 weeks, with no effect after systematic conservative treatment; or symptoms worsen or recur during conservative treatment; or severe pain, or the patient is in a forced position, affecting work or life; or single nerve paralysis or cauda equina nerve paralysis occurs, manifested as muscle paralysis or rectal and bladder symptoms; (4) Participants aged between 18 and 70 years old were included.
Exclusion criteria: (1) Cognitive impairment, disturbance of consciousness, or mental disorder will be grounds for exclusion; (2) Refusal to participate in the study will result in exclusion; (3) Communication disorders will lead to exclusion; (4) Inability to complete the planned operation due to any reason will be considered as an exclusion criterion; (5) Coexistence of other acute traumas such as spinal fracture and hip fracture will result in exclusion; (6) Lower limb muscle strength less than grade 3 before operation and less than grade 4 after operation will serve as an exclusion criterion; (7) Previous history of spinal surgery is a ground for exclusion; (8) Presence of severe osteoarthritis, infection, tuberculosis, malignant tumor, heart failure, pulmonary dysfunction, muscle atrophy or any medical condition that may interfere with exercise are all reasons for potential exclusions.
We extracted comprehensive clinical data from the patient’s electronic medical record system, encompassing gender, age, height, weight, marital status, education level, disease duration, occupation (manual or mental worker), primary caregiver information, operative segment details, number of postoperative wound drainage tubes employed, total postoperative wound drainage volume recorded, current analgesic usage patterns and comorbidities (Charlson comorbidity index score was calculated). Additionally collected were factors potentially influencing motor and neurologic recovery such as alcohol and smoking history pre- and post-hospitalization.
The clinical outcome data encompassed pain experienced during exercise, the onset of exercise-induced pain, and the Oswestry Disability Index (ODI) (20). Pain intensity was assessed using a visual analogue scale (VAS, 1–10). Subjective emotional factors that could potentially impact postoperative exercise were evaluated through the use of the General Self Efficacy Scale (GSES) (21) and Beck Depression Inventory (BDI-13) (22).
The Tampa Scale of Kinesiophobia (TSK-17) (23) was utilized to evaluate the presence of kinesiophobia, a self-reported questionnaire comprising 17 items categorized into four response options: strongly agree, agree, disagree, and strongly disagree. Each item was scored on a scale ranging from 1 to 4. Items 4, 8, 12, and 16 were reverse-scored. Total scores ranged from 17 to 68 with higher scores indicating greater severity of kinesiophobia. The TSK-17 is widely recognized as a reliable measure for assessing kinesiophobia (24, 25). A total TSK-17 score equal to or exceeding 37 indicates the presence of kinesiophobia. The Chinese version of TSK-17 (26) demonstrated strong internal consistency (Cronbach’s α coefficient = 0.82) and test–retest reliability (intraclass correlation coefficient ICC = 0.90). In this study, patients were classified into two groups based on their TSK-17 scores: the kinesiophobia group (TSK-17 score ≥ 37) and the non-kinesiophobia group (TSK-17 score ≤ 36).
The patient’s preoperative lumbar spine MRI was acquired from the hospital imaging system HIS for the assessment of nerve root compression and lumbar paravertebral core muscle area in the patient.
Grading of nerve root compression was assessed based on the research criteria established by Pfirrman et al. (27). The degree of nerve root compression was evaluated using MRI cross-sectional imaging of the segment with the most severe lumbar disc herniation, which was categorized into four grades ranging from 0 to III: grade 0 (normal) indicated no evident contact between the disc and the nerve root; Grade I (contact) denoted that although the disc was adjacent to the nerve root, there were no signs of deviation or deformation in the nerve root; Grade II (offset) indicated displacement of the nerve root due to disc compression; Grade III (compression) referred to flattening of the nerve root caused by compression from both nucleus pulposus and vertebral canal wall. Compared with measuring the sagittal diameter index (SI) (28, 29), this method is more intuitive and convenient to evaluate the degree of nerve root compression.
Lumbar core muscle area (bilateral multifidus and erector spinae) data were collected. Prior to the operation, all patients underwent a lumbar MRI plain scan using a Siemens 3.0 T MRI imager with T2 sequence parameters: repeat time of 3,500 ms, echo time of 94 ms, and a scan matrix of 256 × 51. The MRI scanning axis was kept parallel to the endplate of the lumbar spine, and fifteen images were scanned in axial position (3 images of the upper, central and lower part of each intervertebral space). In this study, the morphology and structure of the multifidus and erector spinae muscles at the central level of the L4/5 intervertebral space were measured on bilateral cross sections (Figure 1). Compared with the images of the upper and lower layers of the intervertebral space, the images of the central level of the intervertebral space avoided the vertebral body, and the muscle area imaging was fuller and clearer. To minimize potential bias caused by different body positions, patients were positioned in a prone position during the MRI examination. All imaging measurements were performed by an investigator who was not involved in patient treatment.
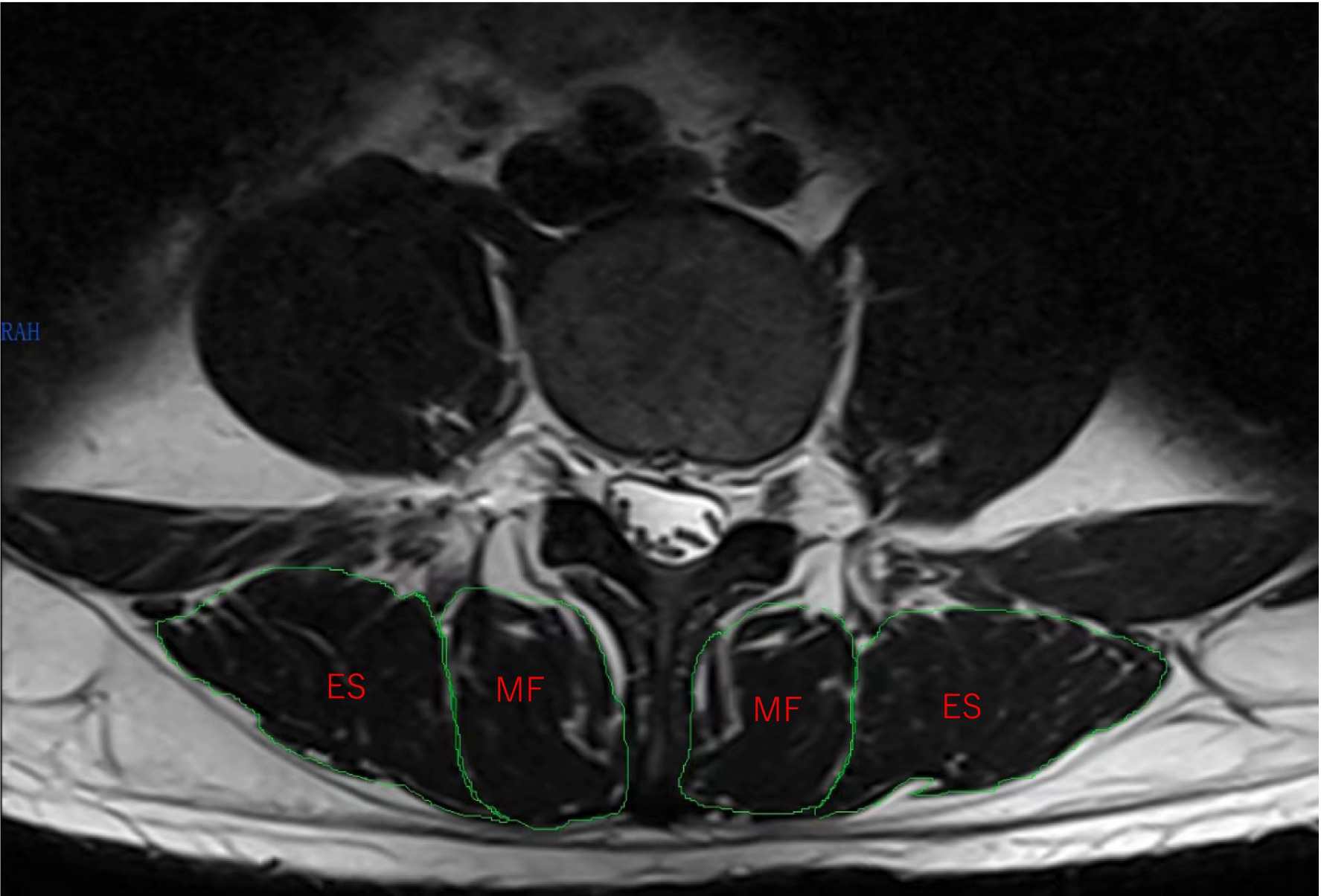
Figure 1. Cross-sectional magnetic resonance imaging of the fourth lumbar spine. MF, multifidus; ES, erector spinae.
The statistical analysis was performed using SPSS 25.0 software. Continuous variables with a normal distribution were described as mean ± standard deviation (X ± S) and compared using an independent t-test. Non-normally distributed continuous variables were described as median (quartile) [M (P25, P75)], and group comparisons were analyzed using the Mann–Whitney U test. Categorical variables were presented as frequency (%) and analyzed using either Pearson chi-square test or Fisher’s exact test. Binary logistic regression was employed to analyze the factors influencing postoperative kinesiophobia in patients. A significance level of α = 0.05 was used, with p < 0.05 considered statistically significant.
Between May 2023 and January 2024, patients who met the predefined inclusion and exclusion criteria were consecutively enrolled in the study, with prospective collection of their postoperative information. During this period, a total of 1,022 patients were admitted to our hospital for spinal diseases. Among them, we initially enrolled 193 patients with lumbar interbody fusion (LIF), but excluded 12 patients who had undergone MRI at other hospitals and 3 patients who experienced postoperative cerebrospinal fluid leakage and subsequently withdrew from the study. Ultimately, a total of 178 eligible patients were included in the analysis. The demographic characteristics, clinical profiles, and imaging parameters of these enrolled participants are presented in Table 1.
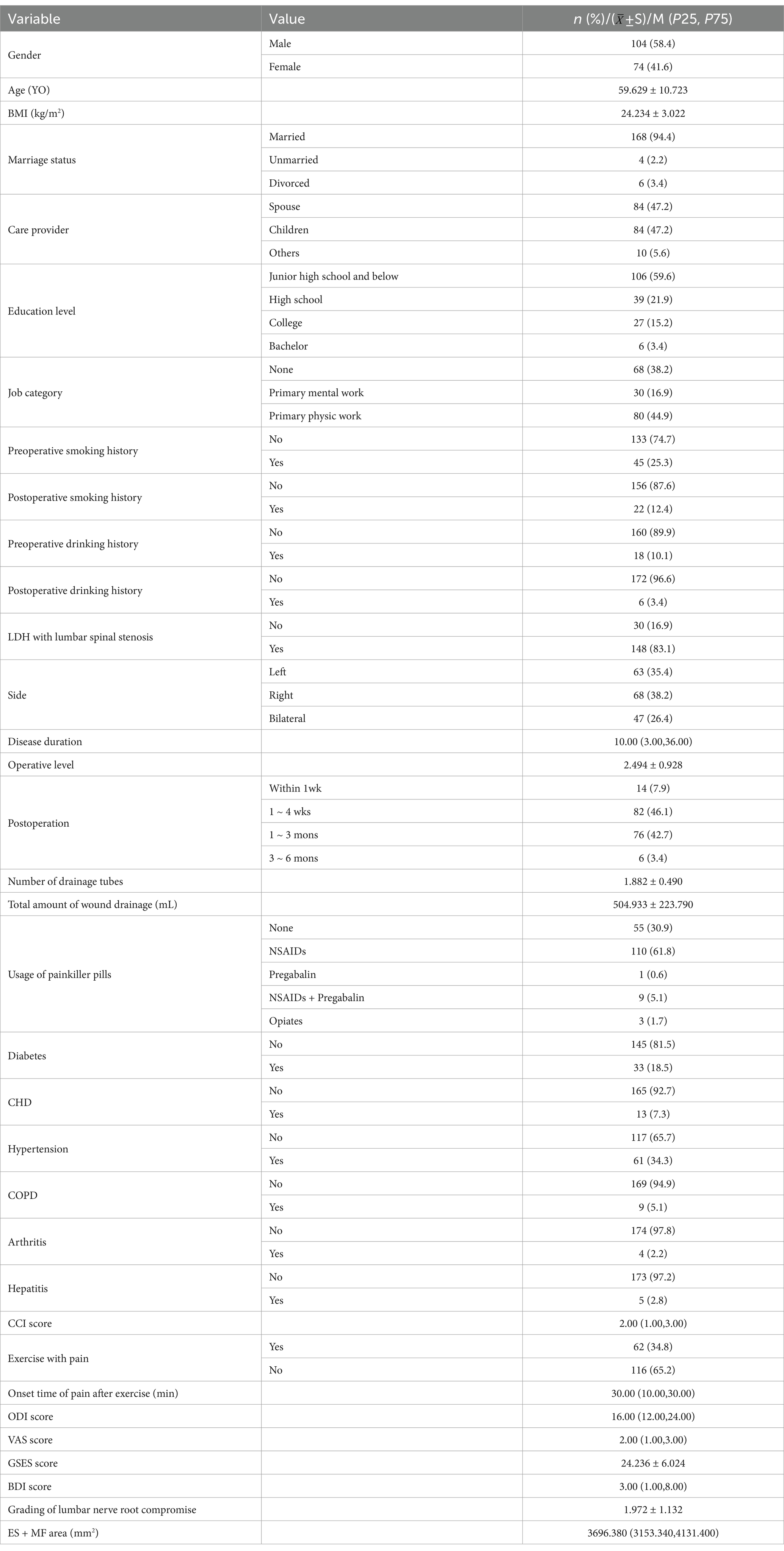
Table 1. Fundamental demographic, clinical characteristics, and imaging parameters of the enrolled patients.
Among the 178 elderly patients, a total of 116 individuals were screened for TSK-17 scores ≥37 points, revealing that motor phobia was present in 65.2% of these patients following LIF (Table 1). The results from univariate analysis demonstrated significant differences between the kinesiophobia group and the non-kinesiophobia group in terms of age, number of surgical levels, postoperative drainage volume, VAS score, GSES score, BDI score, ODI score, degree of nerve root compression and total ES + MF area (p < 0.05) (Table 2).
In order to further investigate the correlation between the 9 variables exhibiting single factor differences and the occurrence of kinesiophobia, as well as to explore their relationship, we employed a binary logistic regression model (Table 3). The occurrence of kinesiophobia was considered as the dependent variable, while the 9 variables with single factor differences were treated as independent variables. All data were standardized prior to conducting binary logistic regression analysis.

Table 3. Influencing factors of kinesiophobia in patients after LIF: binary logistic regression analysis.
The binary logistic regression analysis revealed that advanced age (OR = 3.883 (1.678–8.985), p = 0.002), higher VAS score (OR = 4.401 (1.706–11.357), p = 0.002), elevated BDI score (OR = 3.969 (1.225–12.859), p = 0.022), reduced GSES score (OR = 0.330 (0.135–0.807), p = 0.015), increased number of operative levels (OR = 2.106 (1.058–4.194), p = 0.034) and increased postoperative incision drainage (OR = 3.724 (1.374–10.294), p = 0.011), greater degree of nerve root compression on preoperative lumbar MRI (OR = 4.916 (2.257–10.710), p<0.001), and smaller lumbar paravertebral muscle area (OR=0.508 (0.262-0.984), p = 0.045) were independent risk factors for postoperative motor phobia. However, Oswestry Disability Index (OID)score was not an independent factor affecting postoperative kinesiophobia (p > 0.05).
Lumbar disc herniation is a degenerative disease of the lumbar spine, characterized by low back pain (LBP) as the primary symptom, and it is a prevalent clinical condition in orthopedics. This condition primarily affects individuals between 25 to 55 years old, with a higher incidence among males than females. Approximately 10 to 20% of patients require surgical intervention (30), and postoperative exercise rehabilitation plays a crucial role in facilitating early return to work. However, fear and avoidance behaviors toward exercise after surgery hinder compliance with rehabilitation exercises, impede the recovery of lower back muscles (31), and fail to alleviate residual pain symptoms postoperatively, leading to prolonged impairment of motor function and perpetuating a vicious cycle (31). In this study, motor phobia was observed in 65.2% of patients following lumbar interbody fusion (LIF), which aligns closely with findings reported by Kemani et al. (31) but slightly exceeds those reported by Svensson et al. (32) and Lv et al. (33) for simple lumbar discectomy and elderly patients with primary osteoporosis, respectively. Notably, the prevalence of kinesiophobia among patients with chronic heart failure or chronic obstructive pulmonary disease surpasses that reported by Fatih et al. (34). The rationale behind this discrepancy may be attributed to LIF being more invasive compared to simple lumbar discectomy; furthermore, patients undergoing LIF may possess an increased desire for self-protection when compared to non-surgical counterparts due to perceiving safety as paramount during physical activities given the high-risk nature associated with LIF surgery (35).
The incidence of kinesiophobia varies across different countries, regions, surgical procedures, and disease types. This study reveals a high prevalence of kinesiophobia among patients after lumbar interbody fusion (LIF) in our region. Given the increasing age of individuals with lumbar disc herniation and the aging population, it is crucial to recognize the significant detrimental effects of kinesiophobia. The objective of this study was to investigate the incidence of kinesiophobia in LIF patients and identify associated risk factors to gain further insights into its underlying mechanisms. Our findings indicate that advanced age, higher visual analog scale (VAS) scores for pain intensity, elevated Beck Depression Inventory (BDI) scores, increased General Self-Efficacy Scale (GSES) scores, multiple operative segments involved, greater postoperative incision drainage volume, reduced paravertebral muscle area size, and heightened preoperative nerve root compression levels are all independent risk factors for postoperative motor phobia in LIF patients.
The present study revealed a positive correlation between age and the incidence of motor phobia following LIF, which aligns with Alpalha et al.’s findings (36) that physically frail patients and the elderly, particularly those residing in nursing homes, exhibit higher levels of kinesiophobia. Furthermore, previous studies (34) have demonstrated that age significantly influences kinesiophobia levels in patients with chronic heart failure (44.3%) and chronic obstructive pulmonary disease (47.7%). Jenevi et al. (16) observed that individuals aged 56–65 years displayed higher levels of kinesiophobia compared to other age groups, while those over 65 years exhibited even greater levels. Additionally, advanced age may be associated with reduced cognitive function and health information processing abilities (37). Bilgin et al.’s research (26), involving a questionnaire survey on 504 non-surgical patients suffering from neck and low back pain, indicated that individuals with lower educational attainment tend to experience heightened kinesiophobia. However, our study did not identify education level as an independent risk factor for kinesiophobia among LIF patients; furthermore, no significant differences were found in the incidence of post-LIF kinesiophobia across different education levels. These results are consistent with John et al.’s findings (16), suggesting variations in health education experiences related to lumbar spine conditions among subjects with differing educational backgrounds. Notably, individuals with lower educational attainment may benefit from systematic exercise programs and pain self-management health education training conducted by medical professionals (including redefining pain physical examination procedures, scientifically assessing pain severity levels, implementing appropriate pain response measures tailored to individual needs) leading to a reduction in their overall level of kinesiophobia (38).
In this study, there was a positive correlation between the severity of depression (as measured by BDI) and the prevalence of exercise fear following lumbar interbody fusion (LIF), which aligns with findings reported by Bilgin et al. (39). Patients with severe lumbar disc herniation often experience prolonged low back pain, leading to reduced engagement in daily activities and social interactions. Consequently, they develop apprehension toward postoperative exercise rehabilitation due to concerns about potential harm to their bodies. Moreover, depression can intensify pain perception, thereby contributing to the development of exercise phobia associated with pain. Notably, individual self-efficacy emerged as a protective factor against kinesiophobia in our study. Self-efficacy refers to an individual’s confidence in their ability to achieve desired outcomes and diminished self-efficacy has been identified as a predictor for long-term disability (40). Previous research has confirmed that self-efficacy acts as a mediating variable between pain-related fear and avoidance behavior among patients with chronic low back pain (41). Individuals with high levels of self-efficacy exhibit greater activity levels, work endurance, efficiency in exercising/stretching routines, and coping strategies. Furthermore, exercise fear and avoidance can impede individuals’ participation in meaningful activities while increasing negative affective states and reducing self-efficacy levels; ultimately exacerbating pain symptoms and perpetuating a vicious cycle.
Pain is a significant influential factor in the development of kinesiophobia (11), and this study’s findings align with this notion. However, our study revealed that the presence and timing of pain during exercise were not independent factors contributing to kinesiophobia; rather, it was the intensity of pain that emerged as an independent determinant. This implies that individuals experiencing higher levels of pain exhibit greater fear toward engaging in physical activity, with such fear stemming from heightened levels of pain-related apprehension. Previous research has indicated that even after successful surgical interventions, 10 to 40% of patients continue to report persistent pain complaints (37). The persistence of postoperative residual pain can be attributed to various factors including preoperative physiological and anatomical damage severity, surgical variables, as well as psychological and social influences. The fear-avoidance model (42) elucidates the underlying psychological mechanisms whereby individuals with elevated levels of pain-related fear demonstrate biased attentional and cognitive evaluations toward their discomfort, thereby perpetuating both their experience of pain and functional impairments. Notably, individuals exhibiting high levels of pain-related fear exhibit increased activation within the anterior insula and central cingulate cortex when evaluating painful stimuli as potential threats.
Therefore, the intensity of pain stimulus is perceived as heightened, leading to increased vigilance toward pain signals in both internal and external environments. Even after physiological healing has occurred, individuals continue to interpret pain as indicative of tissue damage progression. However, it should be noted that fear associated with pain does not always result in avoidance behavior; patients experiencing mild to moderate pain may modify their behavior based on self-determined goals. When individuals perceive the value of engaging in target behaviors to outweigh the importance of avoiding pain, they reject avoidance behavior and prioritize participation in exercise training for rehabilitation (43).
In this study, the majority of subjects underwent surgery between 1 and 12 weeks postoperatively, during which time they had their wound drainage tubes removed and were able to ambulate. The patients’ wound healing varied over time, despite following rehabilitation exercise instructions tailored to their specific postoperative period with gradually increasing difficulty. However, patients who were closer to the operation date still expressed concerns about poor wound healing and bleeding caused by exercise. Previous studies have indicated a strong correlation between increased placement of drainage tubes after surgery and higher rates of surgical site infection (44). Additionally, greater incision drainage following surgery may indicate more vascular injury, impaired coagulation function, and lower hemoglobin levels in patients (45). Consequently, such patients tend to be more cautious after surgery as they associate exercise with potential harm or injury and may therefore avoid it altogether. It is important to note that inappropriate exercises like weight lifting, twisting movements, rugby or other contact sports pose certain risks for screw displacement as well as recurrent disc herniation or rupture after lumbar surgery (46). Patients undergoing multiple surgical segments with several postoperative incisions require guidance from professional rehabilitation therapists for safe exercise practices. This approach not only helps alleviate fear associated with exercising but also prevents unnecessary sports-related injuries.
However, in certain individuals, the recovery of pathological anatomical features in the lumbar spine does not necessarily exhibit a direct correlation with a reduction in pain complaints. This is exemplified by “Failed back surgery syndrome” (FBSS), which denotes persistent axial or peripheral pain following anatomically successful surgical procedures (47). Although LIF can alleviate compression of the intervertebral disc on the nerve root within the spinal canal, it may not instantaneously eradicate nerve root symptoms. A retrospective analysis conducted by Jonsson et al. (11) revealed that 40% of patients experienced enduring back or leg pain after undergoing lumbar disc surgery (48), thereby partially impeding their active movement behavior.
The paravertebral muscle area at the L4 and L5 levels exhibited a significant association with kinesiophobia, as numerous studies have demonstrated that low back pain (LBP) is linked to alterations in paravertebral muscles. A smaller paravertebral muscle area corresponds to weaker lumbar and back muscle strength, which is a crucial factor contributing to low back pain, lumbar degeneration, and dysfunction (49, 50). In this study, we specifically focused on the lumbar core muscles and aimed to establish a direct correlation between paravertebral muscles and exercise phobia. Our findings revealed that both total areas of the paravertebral muscles acted as protective factors against postoperative kinesiophobia. This observation further supports the relationship between the lumbar motor core muscle area and kinesiophobia. Additionally, research has indicated that atrophy of the paraspinal muscles can lead to altered biomechanical properties and lumbar instability, potentially representing the pathological mechanism underlying impaired motor function in patients with lumbar disc herniation (LDH). Furthermore, surgical treatment itself may reduce the cross-sectional area of paraspinal muscles resulting in weakness (51) and stiffness (52).
Additionally, low back pain resulting from the compression of nerve roots in the lumbar intervertebral disc’s nucleus pulposus is a prevalent manifestation among typical patients with lumbar disc herniation (LDH) (53). This condition significantly restricts their engagement in meaningful daily activities prior to surgery. These pain and movement disorders are typically chronic in nature. Although most radicular pain is immediately relieved after surgery, patients may require more time to adapt due to sudden changes in their movement habits post-surgery. Therefore, for the rehabilitation treatment of LIF patients, it may be necessary to implement multimodal rehabilitation measures such as cognitive-behavioral intervention therapy, exercise rehabilitation, and case management (54, 55) to alleviate postoperative pain and fear while facilitating an early return to work.
This study has several inherent limitations. Firstly, this study only included patients with lumbar disc herniation (LDH) from a single center, which may introduce selection bias and limit generalizability to other populations. Secondly, we did not investigate the exercise environment of the included patients, which could potentially act as a confounding factor. Lastly, due to the short follow-up period in this study, it is not representative of exercise fear experienced by patients 1–2 years or longer after lumbar interbody fusion (LIF) surgery nor does it capture dynamic changes in exercise fear at different time points post-surgery. Despite these limitations, this study holds clinical relevance as it provides real-world observations on post-LIF patients in China. In future research endeavors, multi-center studies with larger sample sizes are warranted along with cohort or case–control studies exploring psychological and physiological factors.
In conclusion, our findings indicate that motor phobia is present in 65.2% of patients with lumbar disc herniation (LDH) following lumbar interbody fusion (LIF). Furthermore, the results of multivariate analysis reveal that advanced age, greater pain severity, higher scores on the Beck Depression Inventory (BDI), lower scores on the General Self-Efficacy Scale (GSES), increased number of surgical levels, higher incidence of postoperative incision drainage, elevated transverse nerve root compression observed on preoperative lumbar magnetic resonance imaging (MRI), and reduced area of the lumbar paravertebral muscles are independently associated with motor phobia. To enhance postoperative functional recovery in LDH patients undergoing LIF and reduce disability rates while improving their quality of life, early identification of individuals at high risk for kinesiophobia is crucial. Implementing interventions such as cognitive-behavioral therapy, exercise rehabilitation management, and preoperative adaptive exercise training should be considered.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
The studies involving humans were approved by the ethic committee of Hunan Provincial People’s Hospital, the First Affiliated Hospital of Hunan Normal University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
YP: Conceptualization, Writing – original draft. QQ: Data curation, Writing – original draft. CY: Formal analysis, Writing – original draft. MD: Data curation, Writing – original draft. HZ: Formal analysis, Writing – original draft. JW: Investigation, Writing – review & editing. HQ: Supervision, Writing – review & editing.
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the Science project of Hunan Provincial Health Commission (No. 202204072615).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Resnick, DK, Choudhri, TF, Dailey, AT, Groff, MW, Khoo, L, Matz, PG, et al. Guidelines for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 7: intractable low-back pain without stenosis or spondylolisthesis. J Neurosurg Spine. (2005) 2:670–2. doi: 10.3171/spi.2005.2.6.0670
2. Fang, X, Zhang, M, Wang, L, and Hao, Z. Comparison of PLIF and TLIF in the treatment of LDH complicated with spinal stenosis. J Healthcare Eng. (2022) 2022:1–5. doi: 10.1155/2022/9743283
3. Li, Y, Wu, Z, Guo, D, You, H, and Fan, X. A comprehensive comparison of posterior lumbar interbody fusion versus posterolateral fusion for the treatment of isthmic and degenerative spondylolisthesis: a meta-analysis of prospective studies. Clin Neurol Neurosurg. (2020) 188:105594. doi: 10.1016/j.clineuro.2019.105594
4. Martin, BI, Mirza, SK, Spina, N, Spiker, WR, Lawrence, B, and Brodke, DS. Trends in lumbar fusion procedure rates and associated hospital costs for degenerative spinal diseases in the United States, 2004 to 2015. Spine. (2019) 44:369–76. doi: 10.1097/BRS.0000000000002822
5. Wang, X, Zhang, A, Yao, W, Qiu, H, and Feng, F. Bibliometric analysis of transforaminal lumbar interbody fusion: research status, trends, and future directions. EFORT Open Rev. (2023) 8:906–18. doi: 10.1530/EOR-23-0155
6. El Melhat, AM, Youssef, ASA, Zebdawi, MR, Hafez, MA, Khalil, LH, and Harrison, DE. Non-surgical approaches to the Management of Lumbar Disc Herniation Associated with radiculopathy: a narrative review. J Clin Med. (2024) 13:974. doi: 10.3390/jcm13040974
7. Barbosa, TP, Raposo, AR, Cunha, PD, Cruz Oliveira, N, Lobarinhas, A, Varanda, P, et al. Rehabilitation after cervical and lumbar spine surgery. EFORT Open Rev. (2023) 8:626–38. doi: 10.1530/EOR-23-0015
8. Lee, CS, Kang, KC, Chung, SS, Park, WH, Shin, WJ, and Seo, YG. How does back muscle strength change after posterior lumbar interbody fusion? J Neurosurg Spine. (2017) 26:163–70. doi: 10.3171/2016.7.SPINE151132
9. Tarnanen, SP, Neva, MH, Häkkinen, K, Kankaanpää, M, Ylinen, J, Kraemer, WJ, et al. Neutral spine control exercises in rehabilitation after lumbar spine fusion. J Strength Cond Res. (2014) 28:2018–25. doi: 10.1519/JSC.0000000000000334
10. Skrobot, W, Liedtke, E, Krasowska, K, Dzik, KP, Flis, DJ, Samoraj-Dereszkiewicz, A, et al. Early rehabilitation program and vitamin D supplementation improves sensitivity of balance and the postural control in patients after posterior lumbar interbody fusion: a randomized trial. Nutrients. (2019) 11:2202. doi: 10.3390/nu11092202
11. Meulders, A. From fear of movement-related pain and avoidance to chronic pain disability: a state-of-the-art review. Curr Opin Behav Sci. (2019) 26:130–6. doi: 10.1016/j.cobeha.2018.12.007
12. Trocoli TOBotelho, RV. Prevalence of anxiety, depression and kinesiophobia in patients with low back pain and their association with the symptoms of low back spinal pain. Rev Bras Reumatol. (2016) 56:330–6. doi: 10.1016/j.rbre.2016.02.010
13. Hey, HWD, Lim, JXY, Ong, JZ, and Luo, N. Epidemiology of neck pain and its impact on quality-of-life-a population-based, cross sectional study in Singapore. Spine. (2021) 46:1572–80. doi: 10.1097/BRS.0000000000004071
14. Luque-Suarez, A, Martinez-Calderon, J, and Falla, D. Role of kinesiophobia on pain, disability and quality of life in people suffering from chronic musculoskeletal pain: a systematic review. Br J Sports Med. (2019) 53:554–9. doi: 10.1136/bjsports-2017-098673
15. Jadhakhan, F, Sobeih, R, and Falla, D. Effects of exercise/physical activity on fear of movement in people with spine-related pain: a systematic review. Front Psychol. (2023) 14:1213199. doi: 10.3389/fpsyg.2023.1213199
16. John, JN, Ugwu, EC, Okezue, OC, Ekechukwu, END, Mgbeojedo, UG, John, DO, et al. Kinesiophobia and associated factors among patients with chronic non-specific low back pain. Disabil Rehabil. (2023) 45:2651–9. doi: 10.1080/09638288.2022.2103747
17. Jakobsson, M, Hagströmer, M, Lotzke, H, von Rosen, P, and Lundberg, M. Fear of movement was associated with sedentary behaviour 12 months after lumbar fusion surgery in patients with low back pain and degenerative disc disorder. BMC Musculoskelet Disord. (2023) 24:874. doi: 10.1186/s12891-023-06980-z
18. Kawaguchi, Y, Yabuki, S, Styf, J, Olmarker, K, Rydevik, B, Matsui, H, et al. Back muscle injury after posterior lumbar spine surgery. Topographic evaluation of intramuscular pressure and blood flow in the porcine back muscle during surgery. Spine. (1996) 21:2683–8. doi: 10.1097/00007632-199611150-00019
19. Freeman, MD, Woodham, MA, and Woodham, AW. The role of the lumbar multifidus in chronic low back pain: a review. PM R. (2010) 2:142–6. doi: 10.1016/j.pmrj.2009.11.006
20. Smeets, R, Köke, A, Lin, CW, Ferreira, M, and Demoulin, C. Measures of function in low Back pain/disorders: low Back pain rating scale (LBPRS), Oswestry disability index (ODI), progressive Isoinertial lifting evaluation (PILE), Quebec Back pain disability scale (QBPDS), and Roland-Morris disability questionnaire (RDQ). Arthritis Care Res. (2011) 63:S158–73. doi: 10.1002/acr.20542
21. Salsman, JM, Schalet, BD, Merluzzi, TV, Park, CL, Hahn, EA, Snyder, MA, et al. Calibration and initial validation of a general self-efficacy item bank and short form for the NIH PROMIS(®). Quality Life Res. (2019) 28:2513–23. doi: 10.1007/s11136-019-02198-6
22. Beck, AT, Rial, WY, and Rickels, K. Short form of depression inventory: cross-validation. Psychol Rep. (1974) 34:1184–6. doi: 10.1177/003329417403403s01
23. Mesaroli, G, Vader, K, Rosenbloom, BN, Birnie, KA, and Stinson, J. Sensibility and measurement properties of the Tampa scale of Kinesiophobia to measure fear of movement in children and adults in surgical settings. Disabil Rehabil. (2023) 45:2390–7. doi: 10.1080/09638288.2022.2090624
24. Dupuis, F, Cherif, A, Batcho, C, Massé-Alarie, H, and Roy, JS. The Tampa scale of Kinesiophobia: a systematic review of its psychometric properties in people with musculoskeletal pain. Clin J Pain. (2023) 39:236–47. doi: 10.1097/AJP.0000000000001104
25. Vlaeyen, JWS, Kole-Snijders, AMJ, Boeren, RGB, and van Eek, H. Fear of movement/(re)injury in chronic low back pain and its relation to behavioral performance. Pain. (1995) 62:363–72. doi: 10.1016/0304-3959(94)00279-N
26. Wei, X, Xu, X, Zhao, Y, Hu, W, Bai, Y, and Li, M. The Chinese version of the Tampa scale for Kinesiophobia was cross-culturally adapted and validated in patients with low back pain. J Clin Epidemiol. (2015) 68:1205–12. doi: 10.1016/j.jclinepi.2015.07.003
27. Pfirrmann, CW, Dora, C, Schmid, MR, Zanetti, M, Hodler, J, and Boos, N. MR image-based grading of lumbar nerve root compromise due to disk herniation: reliability study with surgical correlation. Radiology. (2004) 230:583–8. doi: 10.1148/radiol.2302021289
28. Thelander, U, Fagerlund, M, Friberg, S, and Larsson, S. Describing the size of lumbar disc herniations using computed tomography. A comparison of different size index calculations and their relation to sciatica. Spine. (1994) 19:1979–84. doi: 10.1097/00007632-199409000-00020
29. Ren, X, Liu, H, Hui, S, Wang, X, and Zhang, H. Forecast of pain degree of lumbar disc herniation based on back propagation neural network. Open Life Sci. (2023) 18:20220673. doi: 10.1515/biol-2022-0673
30. Ito, T, Takano, Y, and Yuasa, N. Types of lumbar herniated disc and clinical course. Spine. (2001) 26:648–51. doi: 10.1097/00007632-200103150-00017
31. Kemani, MK, Hägg, O, Jakobsson, M, and Lundberg, M. Fear of movement is related to low Back disability during a two-year period in patients who have undergone elective lumbar spine surgery. World Neurosurg. (2020) 137:e416–24. doi: 10.1016/j.wneu.2020.01.218
32. Svensson, GL, Lundberg, M, Ostgaard, HC, and Wendt, GK. High degree of kinesiophobia after lumbar disc herniation surgery: a cross-sectional study of 84 patients. Acta Orthop. (2011) 82:732–6. doi: 10.3109/17453674.2011.636674
33. Lyu, FF, Ying, H, Zhang, M, Xia, LR, Liu, Q, and Cai, L. Prevalence and influencing factors of kinesiophobia in older patients with primary osteoporosis: a cross-sectional survey. Geriatric Nurs. (2024) 57:58–65. doi: 10.1016/j.gerinurse.2024.03.007
34. Enzin, F, Dikici, İC, and Tülüce, D. The relationship between kinesiophobia and adaptation to illness in different chronic illnesses. Chronic Illn. (2023) 20:504–14. doi: 10.1177/17423953231221837
35. General Office of the National Health Commission. (n.d.) “Notice on issuing and distributing Measures for the hierarchical Management of Surgery in medical institutions”. Available online at: http://www.nhc.gov.cn/yzygj/s7657/202212/5eb7ddbaa8004a4497c5f29d3a2a5b4d.shtml (Accessed December 19, 2022).
36. Alpalhão, V, Cordeiro, N, and Pezarat-Correia, P. Kinesiophobia and fear avoidance in older adults: a scoping review on the state of research activity. J Aging Phys Act. (2022) 30:1075–84. doi: 10.1123/japa.2021-0409
37. Staccini, P, and Lau, AYS. Consuming health information and vulnerable populations: factors of engagement and ongoing usage. Yearb Med Inform. (2022) 31:173–80. doi: 10.1055/s-0042-1742549
38. Louw, A, Diener, I, Butler, DS, and Puentedura, EJ. The effect of neuroscience education on pain, disability, anxiety, and stress in chronic musculoskeletal pain. Arch Phys Med Rehabil. (2011) 92:2041–56. doi: 10.1016/j.apmr.2011.07.198
39. Bilgin, S, Cetin, H, Karakaya, J, and Kose, N. Multivariate analysis of risk factors predisposing to Kinesiophobia in persons with chronic low Back and neck pain. J Manip Physiol Ther. (2019) 42:565–71. doi: 10.1016/j.jmpt.2019.02.009
40. Fors, M, Öberg, B, Lindbäck, Y, Enthoven, P, and Abbott, A. What mediates treatment effects in a Presurgery physiotherapy treatment in surgical candidates with degenerative lumbar spine disorders? A mediation and conditional process analysis of the PREPARE randomized controlled trial. Clin J Pain. (2021) 37:168–76. doi: 10.1097/AJP.0000000000000901
41. Mansell, G, Den Hollander, M, Lotzke, H, Smeets, R, and Lundberg, M. A person-Centred Prehabilitation program based on cognitive Behavioural physical therapy for patients scheduled for lumbar fusion surgery: a mediation analysis to assess fear of movement (kinesiophobia), self-efficacy and catastrophizing as mediators of health outcomes. European J Pain. (2022) 26:1790–9. doi: 10.1002/ejp.2004
42. Vlaeyen, JWS, Crombez, G, and Linton, SJ. The fear-avoidance model of pain. Pain. (2016) 157:1588–9. doi: 10.1097/j.pain.0000000000000574
43. Rogers, CJ, Hackney, ME, Zubkoff, L, and Echt, KV. The use of patient-led goal setting in the intervention of chronic low back pain in adults: a narrative review. Pain Manag. (2022) 12:653–64. doi: 10.2217/pmt-2021-0118
44. Tan, T, Lee, H, Huang, MS, Rutges, J, Marion, TE, Mathew, J, et al. Prophylactic postoperative measures to minimize surgical site infections in spine surgery: systematic review and evidence summary. Spine J. (2020) 20:435–47. doi: 10.1016/j.spinee.2019.09.013
45. Wang, C, Wang, X, Yang, Z, Shi, J, and Niu, N. Comparative study on the selection of drainage methods in posterior lumbar interbody fusion. BMC Surg. (2023) 23:207. doi: 10.1186/s12893-023-02106-3
46. Rogerson, A, Aidlen, J, and Jenis, LG. Persistent radiculopathy after surgical treatment for lumbar disc herniation: causes and treatment options. Int Orthop. (2019) 43:969–73. doi: 10.1007/s00264-018-4246-7
47. Scholz, J, Finnerup, NB, Attal, N, Aziz, Q, Baron, R, Bennett, MI, et al. The IASP classification of chronic pain for ICD-11: chronic neuropathic pain. Pain. (2019) 160:53–9. doi: 10.1097/j.pain.0000000000001365
48. Jonsson, E, Olafsson, G, Fritzell, P, Hägg, O, and Borgström, F. A profile of low Back pain: treatment and costs associated with patients referred to orthopedic specialists in Sweden. Spine. (2017) 42:1302–10. doi: 10.1097/BRS.0000000000002089
49. Keller, A, Brox, JI, Gunderson, R, Holm, I, Friis, A, and Reikerås, O. Trunk muscle strength, cross-sectional area, and density in patients with chronic low back pain randomized to lumbar fusion or cognitive intervention and exercises. Spine. (2004) 29:3–8. doi: 10.1097/01.BRS.0000103946.26548.EB
50. Kızılgöz, V, Aydın, S, Karavaş, E, Kantarcı, M, and Kahraman, Ş. Are paraspinal muscle quantity, lumbar indentation value, and subcutaneous fat thickness related to disc degeneration? An MRI-based study. Radiography. (2023) 29:428–35. doi: 10.1016/j.radi.2023.02.004
51. Pourtaheri, S, Issa, K, Lord, E, Ajiboye, R, Drysch, A, Hwang, K, et al. Paraspinal muscle atrophy after lumbar spine surgery. Orthopedics. (2016) 39:e209–14. doi: 10.3928/01477447-20160129-07
52. Häkkinen, A, Kuukkanen, T, Tarvainen, U, and Ylinen, J. Trunk muscle strength in flexion, extension, and axial rotation in patients managed with lumbar disc herniation surgery and in healthy control subjects. Spine. (2003) 28:1068–73. doi: 10.1097/01.BRS.0000061994.36719.5E
53. Emch, TM, and Modic, MT. Imaging of lumbar degenerative disk disease: history and current state. Skeletal Radiol. (2011) 40:1175–89. doi: 10.1007/s00256-011-1163-x
54. Cheng, H, Liu, J, Shi, L, and Hei, X. The rehabilitation-related effects on the fear, pain, and disability of patients with lumbar fusion surgery: a systematic review and meta-analysis. Neurospine. (2023) 20:278–89. doi: 10.14245/ns.2245056.528
Keywords: kinesiophobia, lumbar interbody fusion, low back pain, rehabilitation, cross-sectional study
Citation: Pan Y, Qi Q, Yang C, Dai M, Zhang H, Wen J and Qiu H (2025) Fear of movement in patients after lumbar spine fusion and an analysis of factors: a cross-sectional study. Front. Neurol. 16:1467843. doi: 10.3389/fneur.2025.1467843
Received: 24 July 2024; Accepted: 21 February 2025;
Published: 27 March 2025.
Edited by:
Jianjun Sun, Peking University Third Hospital, ChinaReviewed by:
Hao Zhou, Guizhou Provincial People’s Hospital, ChinaCopyright © 2025 Pan, Qi, Yang, Dai, Zhang, Wen and Qiu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jie Wen, Y2FzaHdqQHFxLmNvbQ==; Hailing Qiu, MzY0MDUyNTMyQHFxLmNvbQ==
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.