- Life Science and Clinical Medicine Research Center, Affiliated Hospital of Youjiang Medical University for Nationalities, Baise, Guangxi, China
Introduction: Post-stroke depression (PSD) can lead to poorer functional outcomes and prognosis. Brain inflammation is a risk factor for PSD. Statins might be beneficial due to their anti-inflammatory properties. Different studies have yielded varying results regarding the effects of statins. Therefore, this meta-analysis aims to clarify the effect of statins on PSD.
Methods: Objectives: To evaluate the relationship between PSD and the use of statins. Data Sources: Databases including PubMed, Web of Science, Embase, and Cochrane Library. Eligibility Criteria: Original observational cohort studies. Participants: Patients with ischemic stroke. Interventions: Use of statins. Appraisal and Synthesis Methods: Forest plot to display pooled results; I2 test to evaluate heterogeneity.
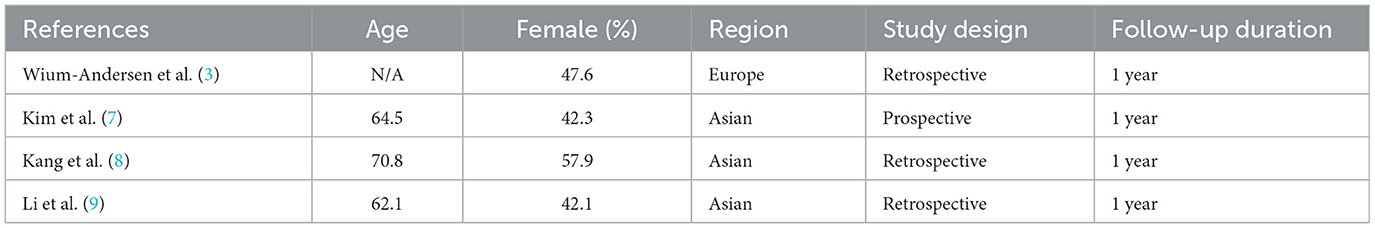
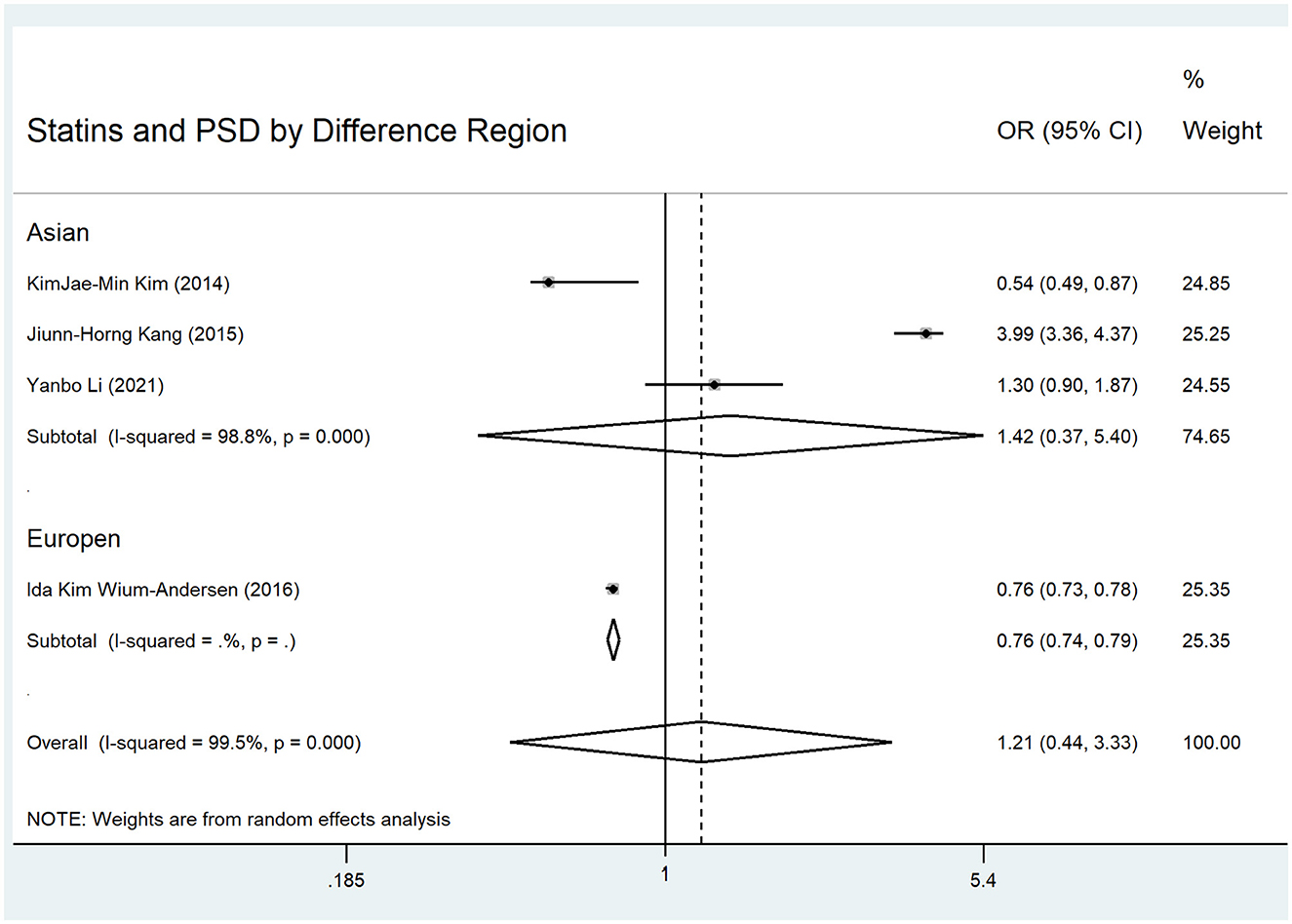
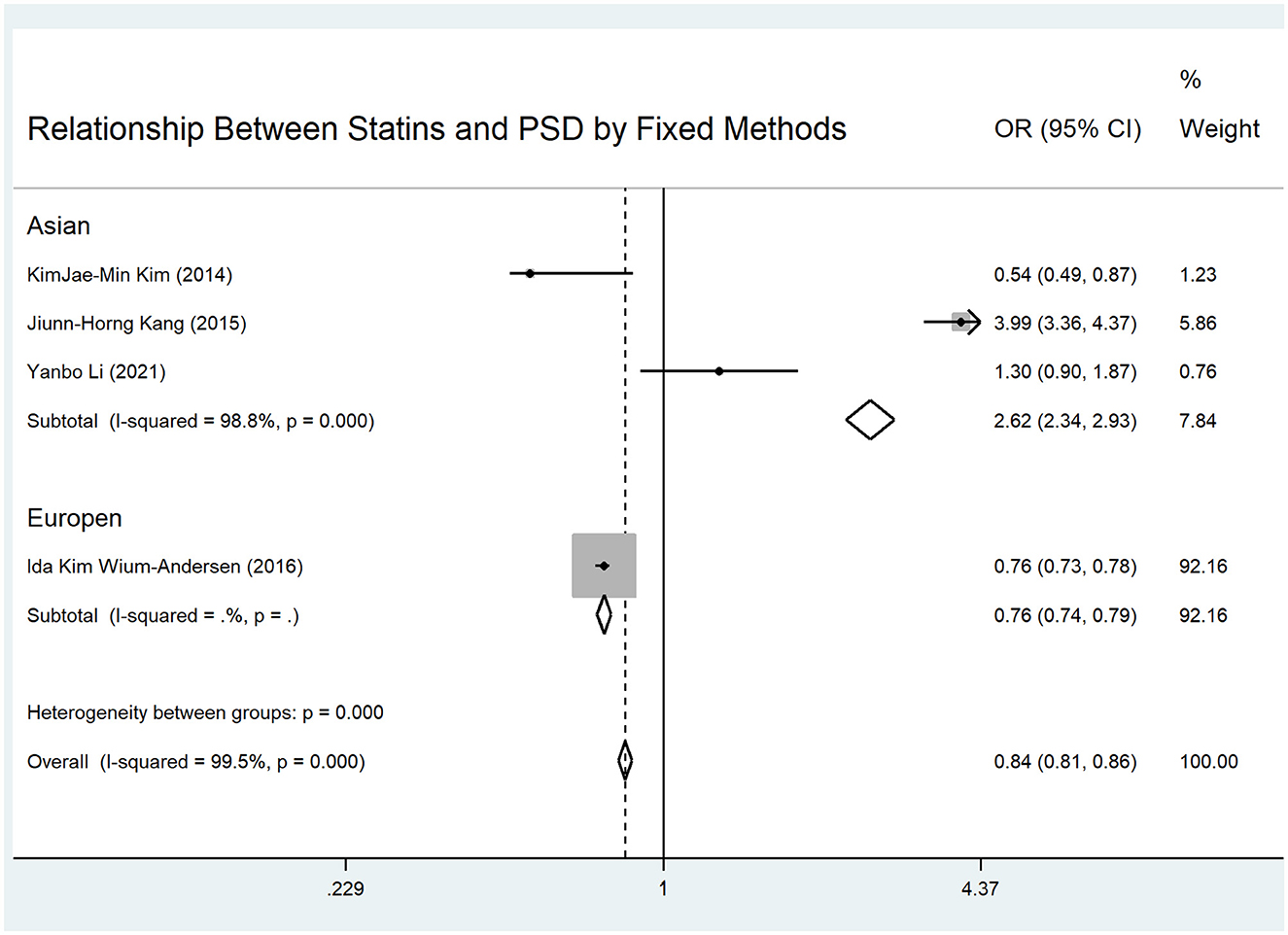
Results: Of the 37 studies selected, four were eligible. The four studies included 93,893 patients (with statins: 45,598) and more than 17,470 PSD patients. The mean age ranged from 62.1 to 70.8 years. The percentage of female participants ranged from 42.1% to 57.9%. For PSD in different regions, the pooled OR for all regions using random-effects methods was 1.21 (95% CI: 0.44–3.33). The pooled OR for Asian populations was 1.42 (95% CI: 0.37–5.40), and for European populations, it was 0.76 (95% CI: 0.73–0.78). The pooled OR for all regions using fixed-effects methods was 0.84 (95% CI: 0.81–0.86). The pooled OR for Asian populations was 2.62 (95% CI: 2.34–2.93).
Conclusion: Depending on the pooling method used, statin use in Asia either increased or had no relationship with PSD. For European patients, statin use reduced the incidence of PSD.
Introduction
Post-stroke depression (PSD) is a common complication for stroke patients (1). Stroke patients have an eight times higher incidence of depression than the general population (2, 3). PSD can lead to poorer functional outcomes, prognosis, and cognitive impairment (2). These can further lead to a reduced quality of life and increased mortality. Although antidepressants are a standard treatment for depression, the longer treatment cycle and adverse effects result in poor compliance among some patients (2). Therefore, several studies have investigated novel drugs, such as statins, known for their anti-inflammatory properties, for the treatment of PSD (3–9).
Some studies have found that brain inflammation is a risk factor for PSD (3). Therefore, anti-inflammation has become a new target for PSD treatment. Statins exhibit anti-inflammatory effects on the brain by reducing levels of IL-6 and IL-8 (3–6). Consequently, statins have emerged as a candidate drug for post-stroke depression (PSD) due to their anti-inflammatory and neuroprotective properties (3, 4). Some studies have explored the relationship between statins and PSD in clinical cohorts (3, 5–9). However, it is puzzling that these studies have produced distinct results regarding this relationship. Choi et al.'s study concluded that statins have no effect on the incidence of PSD (5). Studies by Kang et al. and Kim et al. both found that statins could decrease the incidence of PSD (6, 7). Conversely, Kang et al.'s study indicated that statins could increase the incidence of PSD (8). Li et al.'s study suggested that pre-stroke use of statins could decrease the incidence of PSD, but continued use post-stroke might increase the incidence (9). One large cohort study in Denmark suggested that statins reduced the incidence of PSD (3). These complex conclusions make it difficult to evaluate whether PSD patients could benefit from statins. The differing regions of the aforementioned studies, with varying demographic, environmental, or genetic factors, could partly explain the divergent results. Asian and Danish populations exhibited different reactions to statins due to varying baseline low-density lipoprotein levels and metabolic differences (10). Additionally, lower cholesterol levels, which could cause PSD by altering neurotransmitters and the hypothalamus-pituitary axis, might offset the anti-inflammatory effects of statins (5, 10). Furthermore, statin use's type, dose, and duration could also have differential effects on PSD (6, 9).
Statins are a common long-term treatment for stroke patients. As a standard treatment for stroke prevention, statins are necessary to clarify the relationship between statins and PSD. Therefore, we conducted this systematic review and meta-analysis to explore whether statins affect the incidence of PSD and whether this relationship is affected by different regions, doses, or types of statins.
Methods
The meta-analysis was designed according to the MOOSE (Meta-analysis Of Observational Studies in Epidemiology) guidelines. Eligible study articles were screened and evaluated, data were collected and analyzed, and results were reported.
Search strategy
We searched PubMed, Web of Science, Embase, and Cochrane Library. First, we selected articles published before July 31, 2024. We used the keywords [(“statin”/exp OR statins) AND depression AND (“stroke”/exp OR “ischemic stroke” OR (“cerebrovascular disease”/exp)] for our search. We then obtained articles to evaluate statin use's effect on PSD incidence.
Inclusion and exclusion criteria
The inclusion criteria were: (1) patients with ischemic stroke; (2) intervention involving the use of statins; (3) cohort study design; and (4) outcomes including the incidence of post-stroke depression. The outcomes include the value of ORs.
The exclusion criteria were: (1) Studies lacked sufficient sample power when involving fewer than 50 patients; (2) Studies that did not report outcomes as odds ratios (ORs) or lacked sufficient data to calculate ORs were excluded; (3) animal studies; and (4) case reports, letters, comments, meeting reports, and unpublished studies.
Study selection
We (Chaohua Cui, Jue Li, and Weicong Chen) independently screened the eligible studies. We initially selected articles after reading their titles and abstracts. Then, after reading the full texts, we further excluded articles that did not have suitable outcome data. We further supplemented qualitative studies using references from these articles and related review articles. We did not exclude studies based on language or geographic location. Disagreements regarding the same study were resolved through discussion.
Data collection and quality evaluation
We (Jue Li and Weicong Chen) independently extracted the data, including the name of the author, date of publication, name of the journal, region of the study, number of subjects, age of subjects, study design, timing of statin use, duration of statin use, follow-up time, and values of the ORs and 95% CIs. The regions of the study were divided into Asia and Europe. The study designs were divided into prospective and retrospective cohorts. The timing of statin use was divided into pre-onset and post-onset. The duration of statin use was divided into 1 month and 1 year. The follow-up times were divided into < than 1 year, 1 year, and more than 1 year.
Two authors (Chaohua Cui and Jue Li) independently evaluated the quality of the studies using the Newcastle–Ottawa Scale. The scale ranges from 1 to 9 stars. Studies with more than five stars were considered to be of good quality. A high-quality article indicates better accuracy of intervention factors, better representativeness of the cohort, more suitable comparability of the control, better baseline balance, accuracy in evaluating PSD, sufficient follow-up time, and integrity and rationale for patients lost to follow-up. Disagreements regarding the same study were resolved through discussion.
Statistical analysis
We pooled the OR and 95% CI values using forest plots and conducted subgroup analyses by region (Asia, Europe). Heterogeneity was assessed using the I2 test. If the I2 value was ≥50%, the data were considered to exhibit significant heterogeneity based on previous research (11). The Der Simonian-Laird random-effects method was employed to pool the data, given the anticipated heterogeneity across observational studies. Publication bias was assessed using Egger's test; p < 0.05 indicated significant publication bias, and the results were displayed with Egger's publication bias plot. Additionally, sensitivity analysis was performed using the trim and fill method, and the results were displayed using a funnel plot. All data were processed using the statistical software Stata/MP 14 (Stata Corp, College Station, TX, USA).
Results
Study identification and description
We identified 37 articles from the databases and downloaded 11 of them. Ultimately, our meta-analysis included four eligible studies (Supplementary Figure 1). These four studies included 93,893 patients (45,598 with statins and 48,295 without statins). Three of the studies included 17,470 patients with post-stroke depression. The mean age of the patients ranged from 62.1 to 70.8 years. The percentage of female participants ranged from 42.1% to 57.9%. Three studies were conducted in Asia and one in Europe. All included studies were of good quality (Table 1 and Supplementary Table 1).
Statin use and PSD risk
In examining statin use and PSD incidence within the first year, the pooled OR of the four eligible studies (3, 7–9) with random-effects methods was 1.21 (95% CI: 0.44–3.33), which was not statistically significant. The I2 was 99.5%, indicating significant heterogeneity among the studies (Figure 1). In the regional subgroup analysis, the OR for the Asian subgroup (7–9) was 1.42 (95% CI: 0.37–5.40), which was not statistically significant. The I2 was 98.8%, indicating significant heterogeneity (Figure 1). The pooled OR of the four eligible studies (3, 7–9) with fixed-effects methods was 0.84 (95% CI: 0.81–0.86), which was statistically significant. The I2 was 99.5%, indicating significant heterogeneity (Figure 2). In the regional subgroup analysis with fixed-effects methods, the OR for the Asian subgroup (7–9) was 2.62 (95% CI: 2.34–2.93), which was statistically significant. The I2 was 98.8%, indicating significant heterogeneity (Figure 2). The results of fixed-effects methods differed from those of random-effects methods because the former do not account for heterogeneity between studies. The OR for the Europe subgroup was 0.76 (95% CI: 0.73–0.78), which was statistically significant.
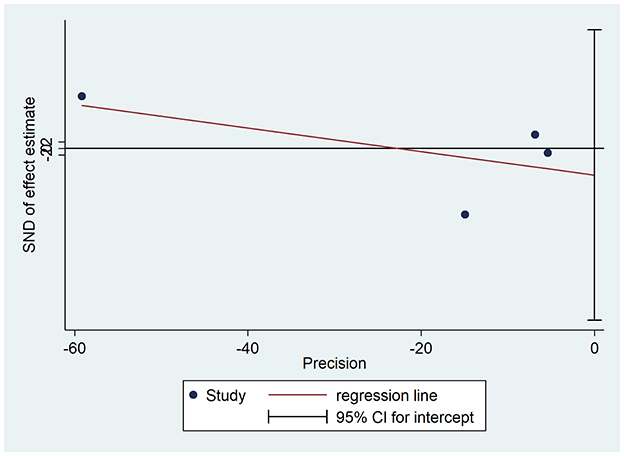
All pooled studies' publication bias and sensitivity analysis results are shown as funnel plots in Figure 3 and Supplementary Figure 2. The study did not show significant publication bias (Figure 3). The test of H0 showed no small-study effects (P = 0.513). The sensitivity analysis did not alter the statistical significance for the 95% CI (Supplementary Figure 2). The test for heterogeneity showed Q = 589.681 with 3 degrees of freedom (p < 0.001), indicating significant heterogeneity between the studies. After the trim process, the pooled OR using fixed-effects methods was 0.757 (95% CI: 0.734–0.780), and the pooled OR using random-effects methods was 0.716 (95% CI: 0.291–1.761).
Differences in statin use duration and PSD risk
One study by Kim et al. found a reduction in PSD within the first year after onset, but it did not affect PSD at baseline (2 weeks after onset) 7. Another study by Wium-Andersen et al. demonstrated that statins reduced PSD within both 1 and 10 years (3). However, another study suggested that statins did not affect PSD between 6 and 64 months (5). Another study indicated that using statins both before and after onset could increase PSD, while using them only before onset could decrease PSD (9). An additional study indicates that statin-associated PSD may be dose-sensitive or time-dependent in stroke patients (8). Overall, the findings suggest that both the duration and timing of statin use may influence PSD outcomes, with effects varying across studies.
Discussion
Our meta-analysis identified a complex relationship between statin use and PSD, highlighting notable differences between Asian and European populations, which may be influenced by dosage, duration, and metabolic factors. The pooled data using random-effects methods showed that statin use was unrelated to PSD. In the regional subgroup analysis using random-effects methods, statin use was not related to PSD in Asian patients but reduced PSD in European patients. These studies did not exhibit significant publication bias. Significant heterogeneity (I2 > 99%) was observed between studies, which could stem from differences in populations, statin types, or study designs. However, the pooled results were credible, as sensitivity analyses did not alter the statistical significance. The duration of statin use and PSD onset timing could have distinct effects.
The pooled results using random-effects methods showed that statins did not increase the incidence of PSD. However, the pooled results using fixed-effects methods showed that statins reduced the incidence of PSD. The differing results of the three Asian studies influenced the overall conclusion (7–9). Additionally, the pooled results of the Asian studies affected the overall regional results. A single European study with a large population showed that statins reduced the incidence of PSD (3). However, this study did not receive sufficient weight in the random-effects analysis (25.35%). In the fixed-effects analysis, this study received a significant weight (92.16%). The other Asian studies had similar weight changes between fixed- and random-effects methods. Therefore, the pooled results of fixed- and random-effects methods yielded distinct outcomes. Although the fixed-effects method might not be suitable for the meta-analysis as it does not account for heterogeneity between studies, given the significant population differences between studies, the weighting of the four studies in the fixed-effects analysis appears more reasonable. Even though these studies had significant heterogeneity, we cannot ignore the pooled results from the fixed-effects analysis. The European study with a large population deserved the highest weight, particularly in the pooled results.
The pooled results for the Asian subgroup presented a more complex scenario. Kang et al.'s study, which included more patients, significantly impacted the pooled results for Asians (8). Therefore, the pooled results using fixed-effects methods were similar to Kang's. Interestingly, statins had utterly opposite effects on PSD between Asian and European patients.
The differing metabolic characteristics of statins, variations in cholesterol levels, and population differences between Asian and European patients may partly explain these results (10). Asian patients have been observed to be more sensitive to statins (10). Statins may affect PSD by influencing cholesterol levels, which subsequently impact brain function. According to our previous and other studies, lower doses of statins may achieve better effects in Asian stroke patients (11–14). Therefore, Asian patients taking statins could have lower cholesterol levels. Lower cholesterol levels could cause depression in stroke patients (4, 5). However, the critical point is whether the influence of serum cholesterol on the CNS reaches a threshold that causes functional impairment, which could then lead to depression (5). Therefore, the extent to which statins reduce serum cholesterol could affect the association between statin use and PSD.
The average LDL-C levels in Western societies significantly exceed those in Asian societies (5). Consequently, statins may reduce serum cholesterol levels more effectively in Asians compared to Europeans and Americans. This may also account for the varying relationships between statins and PSD across different regions. Based on these findings, low-dose statins could represent a practical approach for Asian patients. Due to their reduced effect on serum cholesterol levels in Asian patients, low-dose statins might have a diminished impact on post-stroke depression.
The multifaceted effects of statins may also be attributed to their anti-inflammatory properties (15). Inflammation in the brain is a key mechanism underlying depression (3). Statins exert immune-modulating and anti-inflammatory effects on the central nervous system (15). Statins may alleviate depression through their anti-inflammatory effects in the brain (3, 7). However, for patients with PSD, the anti-inflammatory effects are not unequivocally beneficial. One study found that statins reduced the risk of both early-onset and late-onset PSD (3). Other studies have identified distinct roles of inflammatory reactions during the acute and chronic stages of ischemic stroke (15, 16). Furthermore, studies have observed varying effects of statins at different stages of stroke (6, 9). These findings suggest that the use of statins may necessitate different strategies and approaches at various stages of PSD in patients. The specifics of these strategies and approaches require further investigation.
This study has several limitations. First, our meta-analysis included four prospective and retrospective observational studies. The data were aggregated from various types of studies that differed in design and execution, leading to substantial heterogeneity. However, sensitivity analysis indicated that the studies did not alter the pooled results. Therefore, the pooled results are credible. Randomized controlled trials are needed to further validate the results. Secondly, the majority of studies originate from Asia. Studies from other regions are required to balance the current Asia-centric data pool. Thirdly, statins may have varying effects at different stages post-stroke. Therefore, further exploration of the relationship between statins and PSD could provide actionable insights for clinicians managing PSD at various stages of stroke recovery. Differences in stroke type and location could also result in varying effects of statins on patients (17, 18), warranting further study.
Conclusion
In conclusion, this analysis indicates that statins may provide distinct benefits related to PSD, contingent upon patient population and treatment specifics. Clinicians may consider dose adjustments and population-specific guidelines to optimize PSD management; however, further research is necessary to substantiate these findings.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author/s.
Author contributions
CC: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Software, Supervision, Validation, Writing – original draft, Writing – review & editing. JL: Conceptualization, Data curation, Investigation, Writing – original draft, Writing – review & editing. WC: Data curation, Investigation, Methodology, Software, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by the Liuzhou Scientific Research Technological Development Programs (2022CAC0118) and the Specific Research Project of Guangxi for Research Bases and Talents (AD23026241).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2024.1486367/full#supplementary-material
References
1. Teoh V, Sims J, Milgrom J. Psychosocial predictors of quality of life in a sample of community-dwelling stroke survivors: a longitudinal study. Top. Stroke Rehabil. (2009) 16:157–66. doi: 10.1310/tsr1602-157
2. Blumberger DM, Vila-Rodriguez F, Thorpe KE. Effectiveness of theta burst versus high-frequency repetitive transcranial magnetic stimulation in patients with depression (THREE-D): a randomised non-inferiority trial (vol 391, pg 1683, 2018). Lancet. (2018) 391:E24. doi: 10.1016/S0140-6736(18)30295-2
3. Wium-Andersen IK, Wium-Andersen MK, Jorgensen MB, Osler M. Anti-inflammatory treatment and risk for depression after first-time stroke in a cohort of 147 487 Danish patients. J Psychiatry Neurosci. (2017) 42:320–30. doi: 10.1503/jpn160244
4. Swiger KJ, Martin SS. PCSK9 inhibitors and neurocognitive adverse events: exploring the FDA directive and a proposal for < i>N < /i>-of-1 trials. Drug Saf. (2015) 38:519–26. doi: 10.1007/s40264-015-0296-6
5. Choi MH, Lim TS, Yoon BS, Son KS, Hong JM, Lee JS. Low testosterone level as a predictor of poststroke emotional disturbances: anger proneness and emotional incontinence. J Stroke Cerebrovasc Dis. (2018) 27:3549–54. doi: 10.1016/j.jstrokecerebrovasdis.2018.08.014
6. Kang HJ, Bae KY, Kim SW, Kim JT, Park MS, Cho KH, et al. Effects of interleukin-6, interleukin-18, and statin use, evaluated at acute stroke, on post-stroke depression during 1-year follow-up. Psychoneuroendocrinology. (2016) 72:156–60. doi: 10.1016/j.psyneuen.2016.07.001
7. Kim JM, Stewart R, Kang HJ, Bae KY, Kim SW, Shin IS, et al. A prospective study of statin use and poststroke depression. J Clin Psychopharmacol. (2014) 34:72–9. doi: 10.1097/JCP.0000000000000051
8. Kang JH, Kao LT, Lin HC, Tsai MC, Chung SD. Statin use increases the risk of depressive disorder in stroke patients: a population-based study. J Neurol Sci. (2015) 348:89–93. doi: 10.1016/j.jns.2014.11.013
9. Li YB, Guo YJ, Zhou MK, Ma M, Fang J, He L. Paradoxical effect of statin medication on depressive disorder in first-ever ischemic stroke patients: possible antidepressant-like effect prestroke and the opposite in continuous medication poststroke. Int Clin Psychopharmacol. (2021) 36:147–53. doi: 10.1097/YIC.0000000000000352
10. Liao JK. Safety and efficacy of statins in Asians. Am J Cardiol. (2007) 99:410–14. doi: 10.1016/j.amjcard.2006.08.051
11. Cui C, Li Y, Bao J, Dong S, Gao L, He L. Low dose statins improve prognosis of ischemic stroke patients with intravenous thrombolysis. BMC Neurol. (2021) 21:220. doi: 10.1186/s12883-021-02259-9
12. Cui C, Li C, Long T, Lao Z, Xia T. Unsupervised machine learning revealed that repeat transcranial magnetic stimulation is more suitable for stroke patients with statin. Neurol Ther. (2024) 13:857–68. doi: 10.1007/s40120-024-00615-8
13. Arboix A, García-Eroles L, Oliveres M, Targa C, Balcells M, Massons J. Pretreatment with statins improves early outcome in patients with first-ever ischaemic stroke: a pleiotropic effect of statins or a beneficial effect of hypercholesterolemia? BMC Neurol. (2010) 10:47. doi: 10.1186/1471-2377-10-47
14. Biffi A, Devan WJ, Anderson CD, Cortellini L, Furie KL, Rosand J, et al. Statin treatment and functional outcome after ischemic stroke case-control and meta-analysis. Stroke. (2011) 42:1314–9. doi: 10.1161/STROKEAHA.110.605923
15. McFarland AJ, Anoopkumar-Dukie S, Arora DS, Grant GD, McDermott CM, Perkins AV, et al. Molecular mechanisms underlying the effects of statins in the central nervous system. Int J Mol Sci. (2014) 15:20607–37. doi: 10.3390/ijms151120607
16. Wimmer I, Zrzavy T, Lassmann H. Neuroinflammatory responses in experimental and human stroke lesions. J Neuroimmunol. (2018) 323:10–18. doi: 10.1016/j.jneuroim.2018.07.003
17. Arboix A, Arbe G, García-Eroles L, Oliveres M, Parra O, Massons J. Infarctions in the vascular territory of the posterior cerebral artery: clinical features in 232 patients. BMC Res Notes. (2011) 4:329. doi: 10.1186/1756-0500-4-329
Keywords: post-stroke depression, statins, incidence, stage and region, type and dose
Citation: Cui C, Li J and Chen W (2025) Statins and the incidence of post-stroke depression: a systematic review and meta-analysis. Front. Neurol. 15:1486367. doi: 10.3389/fneur.2024.1486367
Received: 26 August 2024; Accepted: 17 December 2024;
Published: 07 January 2025.
Edited by:
Nishant K. Mishra, Yale University, United StatesReviewed by:
Adria Arboix, Sacred Heart University Hospital, SpainPriya Dev, Banaras Hindu University, India
Copyright © 2025 Cui, Li and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chaohua Cui, Y2NoYWl3cEAxNjMuY29t
†These authors have contributed equally to this work
 Chaohua Cui
Chaohua Cui Jue Li†
Jue Li†