- 1Department of Rehabilitation Medicine, Changchun University of Chinese Medicine, Changchun, Jilin, China
- 2Tongliao City Hospital, Tongliao, Inner Mongolia, China
- 3Encephalopathy Center, The Third Affiliated Clinical Hospital of Changchun University of Chinese Medicine, Changchun, Jilin, China
- 4Changchun University of Chinese Medicine, Changchun, Jilin, China
Background: Post-stroke spasticity (PSS) is a common complication after stroke and is an important cause of high rates of disability after stroke. At present, modern medicine has made great progress in the treatment of PSS, ‘early detection, early treatment’ has become a general consensus for the treatment of PSS in the clinic. Clarifying the risk factors of PSS can help to detect and treat the functional disorders caused by PSS at an earlier stage.
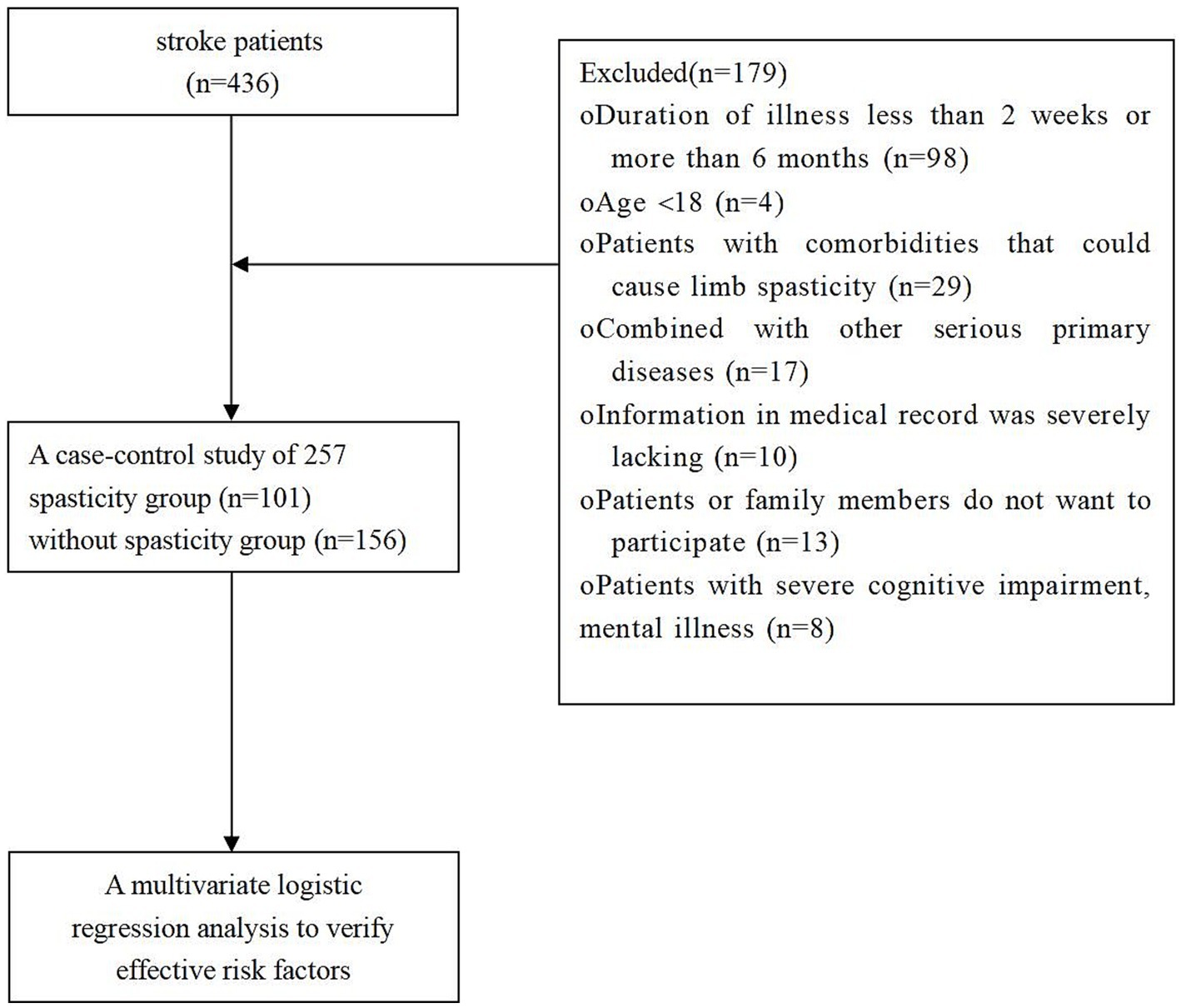
Methods: This is a retrospective study. 436 stroke patients who visited the Neurology Department of the Third Affiliated Clinical Hospital of Changchun University of Chinese Medicine from June 2020 to November 2020 were selected as study subjects, and finally 257 patients were included in the final analysis, and divided into 101 cases with spasticity and 156 cases without spasticity, depending on whether or not the stroke victim had a spasm at the time of admission.
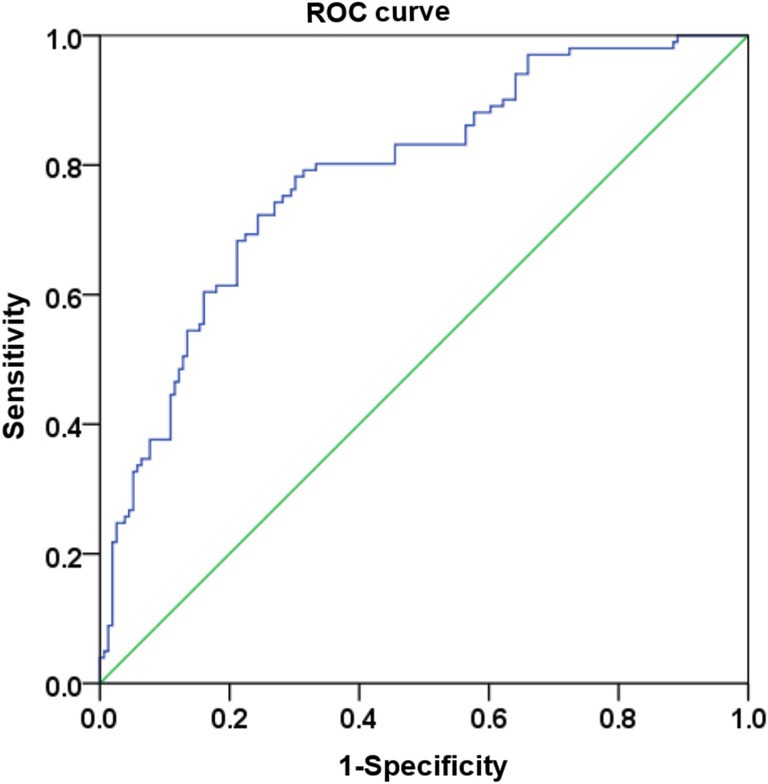
Results: The multivariate regression analysis showed that basal ganglia as the cerebral hemorrhage or infarction site (OR = 4.930, 95%CI = 2.743–8.86, p = 0.000), cerebral hemorrhage or infarction volume (OR = 1.087, 95%CI = 1.016–1.164, p = 0.016) and NIHSS scores (OR = 1.232, 95%CI = 1.089–1.393, p = 0.001) are independent influencing factors and independent risk factors for spasticity (p < 0.05). A risk prediction model for spasticity in stroke patients is derived with the multivariate logistic regression analysis Logit (P) = 1.595 * Basal ganglia +0.084 * infarct volume + 0.208 * NIHSS scores – 2.092. An evaluation of the goodness of fit using the ROC curve showed AUC (95% CI) = 0.786 (0.730–0.843), an indication of a high degree of model fit.
Conclusion: Independent risk factors for Post-stroke spasticity include basal ganglia as the cerebral hemorrhage or infarction site, cerebral hemorrhage or infarction volume and NIHSS scores.
1 Introduction
Cerebral apoplexy, or stroke, is the third leading cause of disability in adults and the second leading cause of deaths globally (1, 2). Post-stroke spasticity (PSS) is a form of increased muscle tone where pathological changes in the upper motor neurons lead to impaired sensory and motor controls. It is a motor disorder characterized by a velocity-dependent increase in tonic stretch reflexes with tendon hyperreflexia resulting in abnormal postures and movement patterns in stroke patients. It is a major contributing factor to high post-stroke disability rates (3–5). Studies have found the treatment cost to be higher in stroke patients with PSS than those without PSS (6). The pathogenesis of PSS is complex and various researchers have proposed different ideas and definitions (7–9). At present, modern medicine has made great progress in the treatment of PSS, including botulinum toxin injections, intrathecal baclofen pumps, etc., and “early detection, early treatment” has become a general consensus for the treatment of PSS in the clinic (10, 11). This study was analyzed from the perspective of prevention. Through the investigation and study of the relevant samples, the study aims to understand the incidence of spasticity after stroke, screen the relevant risk factors of spasticity and construct a risk prediction model, which will further provide a reliable theoretical basis for exploring the early rehabilitation therapies, reducing the incidence of spasticity and slowing down the degree of spasticity. Therefore, this study investigated and studied the relevant samples to understand the incidence of PSS, and screened the relevant risk factors of spasticity to provide additional reliable theoretical basis for the effective prevention of PSS in clinical practice.
2 Methods
This is a retrospective study. A total of 436 stroke patients who visited the Neurology Department of the Third Affiliated Clinical Hospital of Changchun University of Chinese Medicine from June 2020 to November 2020 were selected as study subjects, and finally 257 patients were included in the final analysis, and divided into 101 cases with spasticity and 156 cases without spasticity, depending on whether the individual patient experienced spasticity in the 6 months after the stroke (Any muscle considered to be in spasticity if a value of 1 or more in any muscle in the Modified Ashworth Scale) (Figure 1). From the electronic database of medical records, the investigators recorded information such as the age and gender of study subjects, their medical history in terms of smoking, drinking, hypertension, diabetes, and hyperlipidemia, their dominant hands (left or right hand), as well as observed and recorded the cerebral hemorrhage or infarction by side (left or right), the site of cerebral hemorrhage or infarction (frontal lobe, parietal lobe, temporal lobe, occipital lobe, thalamus, hippocampus, basal ganglia, cerebellum, midbrain, etc.). The volume of the cerebral hemorrhage or infarction was derived from MRI examinations and FLAIR images were used to measure the size of the focal area. Post-processing software was applied on the disclosed relevant sequence to outline the contours of the cerebral hemorrhage or infarction at each layer of the cerebral hemorrhage or infarction in order to automatically calculate the area, these areas were then added layer by layer, and finally multiplied by the layer thickness and inter-layer spacing to obtain the cerebral hemorrhage or infarction volume. Neurological deficit scores (NIHSS scores) and modified Ashworth scores assessed on admission in patients’ e-cases were collected. The data were summarized in a database of observation tables using Excel, then validated and checked for errors before statistical analyses were performed.
2.1 Diagnostic criteria
Based on the diagnostic criteria for cerebral infarction and cerebral hemorrhage in the Chinese Guidelines for Diagnosis and Treatment of Acute Ischemic Stroke 2018 (12) and the Chinese Guidelines for Diagnosis and Treatment of Subarachnoid Hemorrhage 2019 (13). All cases were confirmed by cranial CT or MRI. The modified Ashworth method was used to evaluate the severity of limb spasticity. A final diagnosis was then carried out to confirm if there was limb spasticity.
2.2 Inclusion criteria
(1) Met the diagnostic criteria for cerebral hemorrhage or infarction; (2) Course of disease was between 2 weeks to 6 months; (3) Age ≥ 18; (4) Consciousness and stable vital signs. (5) Patients or family members gave informed consent and participated voluntarily.
2.3 Exclusion criteria
(1) Patients with comorbidities that could cause limb spasticity; (2) Individuals with severe primary diseases such as impairment of liver, kidney, hematopoietic system, and endocrine system; (3) Individuals with severe cognitive impairment, mental illness; (4) Pregnant and lactating women; (5) Information in medical record was severely lacking.
2.4 Sample size estimation method
The sample size for this trial was estimated by calculating the required sample size based on logistic regression analysis in Medical Statistics, Second Edition (14): requires a minimum sample size of more than 10 times the number of independent variables, so as to reflect more realistically the relationship between the independent variable and the dependent variable.
Sample size = number of independent variables × 10.
In the formula: the number of independent variables is 20.
Therefore, it was calculated that at least 200 were required for this survey. The total number of cases finally collected in this study was 257 which fulfils the requirement of study design.
2.5 Data processing
Statistical analyses of the data were performed using SPSS 27.0. Measurement data with a normal distribution was presented as _x ± s while data with a non-normal distribution was presented as M (IQR), and the Mann–Whitney U test was used to compare between the groups. Count data was represented by n(%), and the chi-square test or Fisher’s exact test was used for comparisons between the groups. Logistic regression was used to identify the factors that affect PSS. The difference is considered statistically significant if p < 0.05.
3 Results
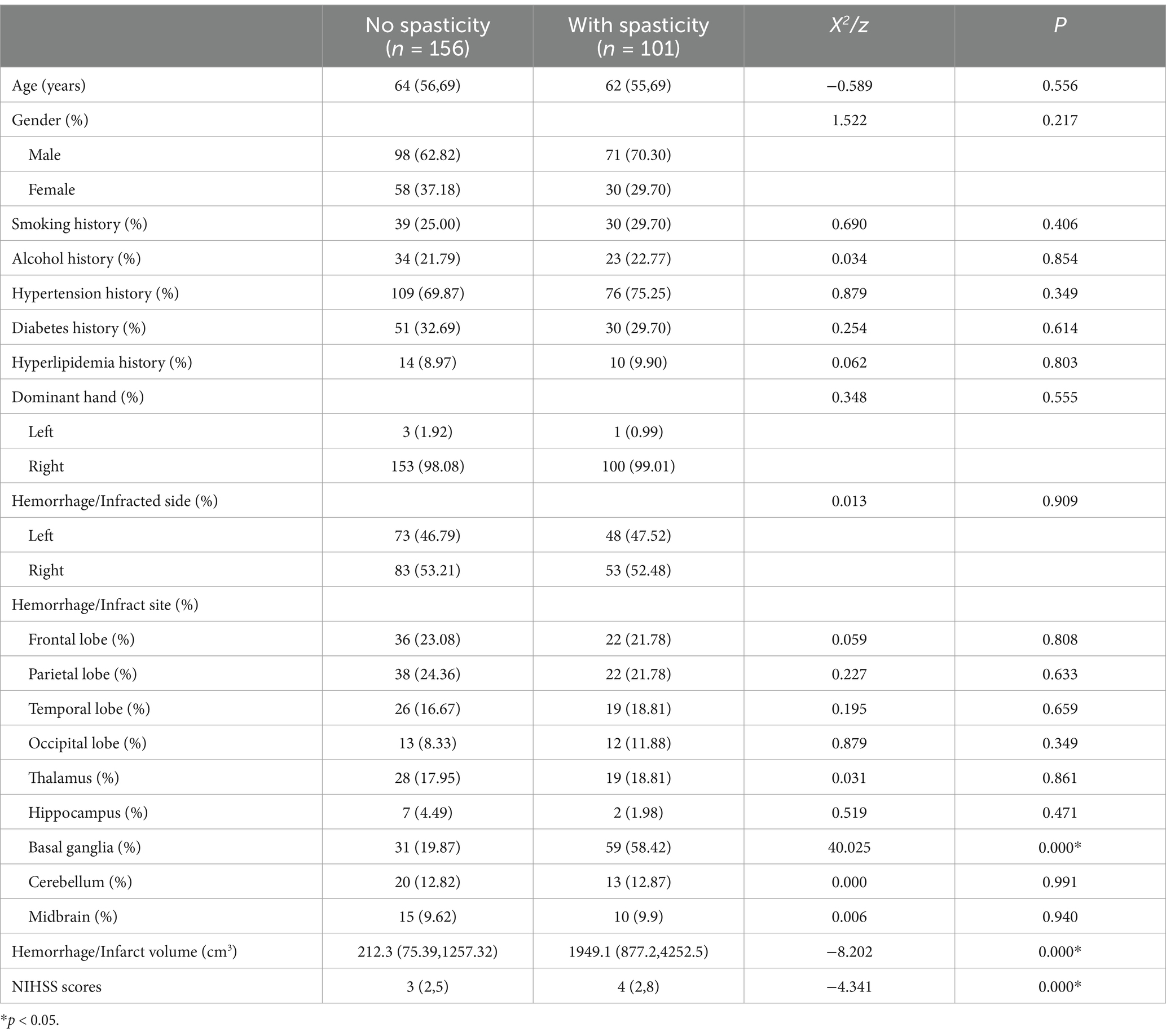
As seen in Table 1, comparisons between the groups showed that the differences in involvement of basal ganglia, cerebral hemorrhage or infarction volume, and NIHSS scores to be statistically significant (p < 0.05), an indication that these may be factors that affect spasticity. However, the impact of confounding factors for spasticity was not accounted for. Therefore, a multivariate regression analysis that took into account the effects of confounding factors was carried out to identify independent factors that affect spasticity.
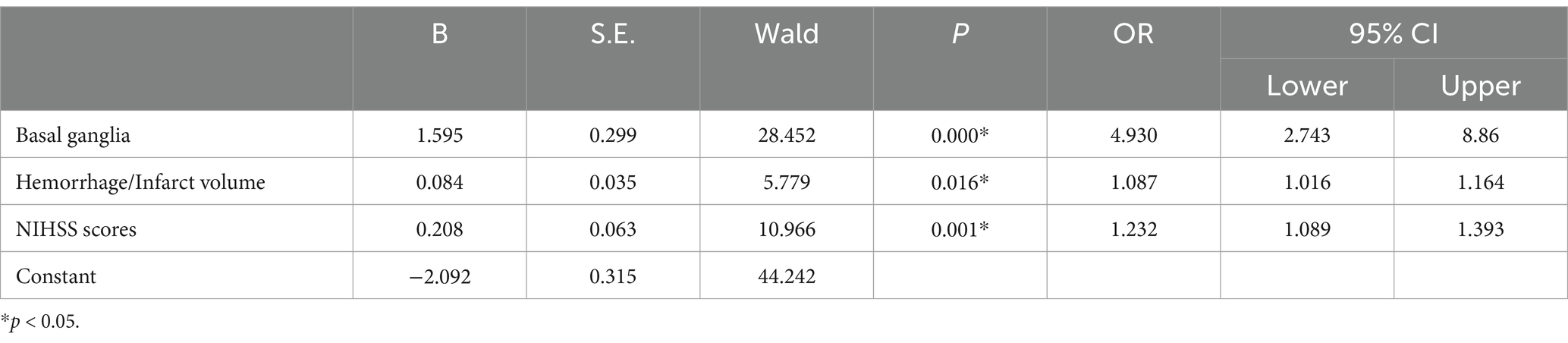
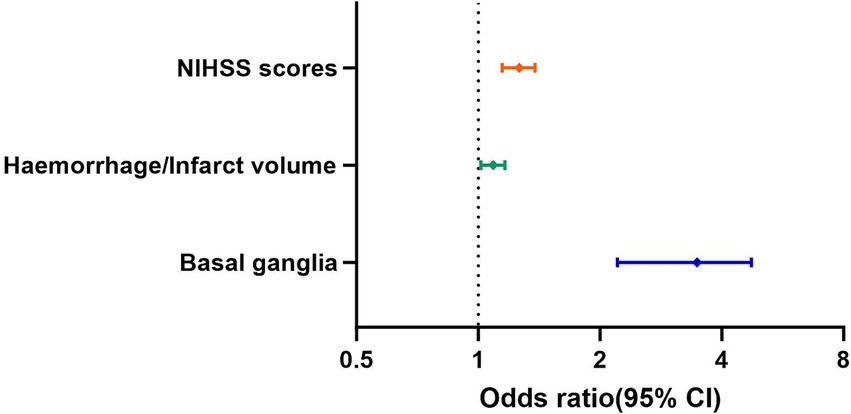
As seen in Table 2, results from the multivariate regression analysis showed that basal ganglia as the cerebral hemorrhage or infarction site, cerebral hemorrhage or infarction volume and NIHSS scores are independent influencing factors and independent risk factors for spasticity (p < 0.05) (Figure 2). Specifically, spasticity is more likely to occur when the cerebral hemorrhage or infarction site is the basal ganglia, the larger the area of cerebral hemorrhage or infarction the more likely it is to lead to spasticity, while a higher NIHSS scores indicates a higher probability of spasticity. All other indicators are not independent influencing factors for spasticity.
A risk prediction model for spasticity in stroke patients is derived with the multivariate logistic regression analysis: Logit (P) = 1.595 * Basal ganglia +0.084 * infarct volume + 0.208 * NIHSS scores – 2.092. The Hosmer-Lemeshow test results in Table 3 are X2 = 13.828, and p = 0.086, which means that there is no significant difference between the predicted value and the actual value in the Hosmer-Lemeshow test. An evaluation of the goodness of fit using the ROC curve showed AUC (95% CI) = 0.786 (0.730–0.843), an indication of a high degree of model fit (Figure 3).
4 Discussion
Spasticity is a common post-stroke complication, and approximately one-third of stroke patients will experience spasticity within 3 months of onset of stroke (15–17). Spasticity is harmful to stroke patients, requiring them to undergo long-term rehabilitation and causing a series of physical and psychological problems that seriously affect their motor function and daily living activities (18, 19). Studies have shown that patients with PSS often suffer from psychological problems such as depression and anxiety, cognitive impairment such as memory loss, and poor concentration (20–24). Post-spasm pain can also lead to sleep disorders. All these seriously affect the patient’s quality of life.
In recent years, as modern medical science and technology develops, more clinical treatments for PSS have emerged, such as oral antispasmodics, botulinum toxin injections, physiotherapy, antispastic positioning, as well as acupuncture, moxibustion and traditional Chinese medicine (25–31). Currently, the most rapid and effective western medical treatments for spasticity are oral anti-spasmodic drugs and local injection of botulinum toxin (32, 33). The early stage of PSS has also achieved better clinical outcomes through antispastic positioning (25). Acupuncture and moxibustion, massage (tuina) and traditional Chinese medicine have the advantages of simplicity and speed, and have achieved remarkable efficacy in the clinical treatment of PSS (34). If the point of treatment is too late, resulting in abnormal movement patterns and postures that have developed, the only way to treat it is through surgery, which is effective but has the disadvantages of a high coefficient of difficulty and high treatment costs (35, 36). Therefore, early detection of spasticity and carrying out effective and rapid treatment are currently the focus of clinical treatment of PSS, which not only reduces related complications, but also shortens the treatment cycle and reduces the burden on the patient’s family. Clarifying the risk factors of PSS can help to detect and treat the functional disorders caused by PSS at an earlier stage, improve the rehabilitation efficacy of the patients, and enhance their ability to return to their families and society.
There are many risk factors for PSS (37–39). NIHSS scores is an important indicator for assessing post-stroke neurological damage. A higher NIHSS scores means a more severe decline in the patient’s neurological functions (40, 41). Studies have shown that PSS patients have relatively higher NIHSS scores (15). This study found the NIHSS scores to be significantly higher in the group with PSS when compared to the group with no PSS. There is a significant correlation between the incidence of PSS and NIHSS scores (p < 0.05). In the multivariate analysis, NIHSS scores is an independent risk factor for PSS (OR = 1.515), and consistent with the findings of Ryu et al. (42). Relevant studies have also found (42) NIHSS scores to be a significant predictor of the occurrence of PSS. Basal ganglia refers to a group of nerve nuclei located deep in the brain, and comprises of the striatum, caudate nucleus, and globus pallidus. These sub-components play key roles in motor, emotional, cognitive, and focus. A damaged basal ganglia can lead to symptoms like muscle tone disorders, and spasticity (43, 44). Studies have demonstrated a close relationship between the site of brain injury and the occurrence of spasticity (45). This study found the proportion of basal ganglia injury to be higher in patients with PSS than those without PSS. There was a significant correlation between the incidence of PSS and basal ganglia injury (p < 0.05). Based on the relevant multivariate analysis, basal ganglia injury is an independent influencing factor for the incidence of PSS (OR = 6.693). Studies worldwide have also confirmed (46, 47) that patients with basal ganglia injury have the highest risk of PSS. The size of cerebral hemorrhage or infarction also has a correlation with the occurrence of PSS, and this study showed that there was a significant difference in the comparison of the size of cerebral hemorrhage or infarction between patients with spasticity after stroke and those without spasticity (p < 0.05), suggesting that large cerebral hemorrhage or infarction may be one of the factors influencing the development of limb spasticity after stroke. Related studies have shown that patients with less spasticity after stroke have smaller areas of cerebral hemorrhage or infarction, while the opposite is true for patients with severe spasticity (47, 48).
Some studies have found that the incidence of spasticity is higher in hemorrhagic strokes than in ischemic strokes, which may be related to the fact that hemorrhagic strokes have a higher degree of disability (49). Hemorrhagic stroke and ischemic stroke have very different pathological mechanisms. In addition to early local cerebral hemorrhage, hemorrhagic stroke is accompanied by a variety of pathological changes in the brain tissue in the hemorrhage area, such as ischemia, hypoxia, inflammatory response, neuronal degeneration, necrosis and apoptosis (50). Hemorrhagic stroke and ischemic stroke have different degrees and extent of damage to the central nervous system, and the onset of spasticity in different stroke types was not further analyzed in this study, the effects of cerebral hemorrhage and cerebral ischemia on spasticity will be further specifically analyzed in future studies. Other researchers have found that stroke patients with a history of previous stroke, that is, patients who are not the first stroke, have a higher proportion of spasticity, and the reason is related to the aggravation of brain tissue damage after a second stroke, and further neurological function damage leads to an increased likelihood of spasticity (51). It is now generally accepted that the incidence of spasticity is relatively low in the acute phase of stroke, and the incidence will gradually increase as the stroke course progresses and lengthens (52). Therefore, in this study, patients in the recovery period after stroke were selected as the research subjects to further clarify the importance of prevention of spasticity after stroke and early rehabilitation intervention on the recovery of neurological function after stroke.
This study retrospectively analyzed data on the patient’s conditions and used multivariate logistic regression to identify factors that may influence spasticity, including the involvement of basal ganglia, cerebral hemorrhage or infarction volume, and NIHSS scores. Independent influencing factors for spasticity (p < 0.05) include basal ganglia as the cerebral hemorrhage or infarction site, cerebral hemorrhage or infarction volume, and NIHSS scores. Due to the limited time and funding, this study has shortcomings in areas like study design and methods, and the results cannot comprehensively encompass all risk factors for PSS. Furthermore, this study adopts a retrospective approach, and is not able to dynamically track and observe the development of spasticity. In selecting the sample, only patients from a single center were selected for the study, so the generalization of the results to patients in other geographical regions should be approached with caution. In future research, a multicenter study with a larger sample size and longer follow-up duration will be conducted for a more comprehensive and in-depth investigation on the risk factors of PSS. A more scientific study plan will be adopted to provide a better scientific basis with regards to the prevention of PSS.
5 Conclusion
Independent risk factors for Post-stroke spasticity include basal ganglia as the cerebral hemorrhage or infarction site, cerebral hemorrhage or infarction volume and NIHSS scores.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Third Affiliated Clinical Hospital of Changchun University of Chinese Medicine. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
CZ: Data curation, Writing – original draft. LL: Writing – review & editing. LQ: Methodology, Writing – review & editing. GJ: Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by the National Key Research and Development Program of the China Key Project (No. 2018YFC1706002) and the Science and Technology Development Project of Jilin Province (No. 20210203061SF), which were supported by the Ministry of Science and Technology of the People’s Republic of China and Science and Technology Hall of Jilin Province.
Acknowledgments
We thank all participants who participated in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
2. Hankey, GJ. The global and regional burden of stroke. Lancet Glob Health. (2013) 1:e239–40. doi: 10.1016/S2214-109X(13)70095-0
3. Burridge, JH, Wood, DE, Hermens, HJ, Voerman, GE, Johnson, GR, Wijck, FV, et al. Theoretical and methodological considerations in the measurement of spasticity. Disabil Rehabil. (2005) 27:69–80. doi: 10.1080/09638280400014592
4. Doussoulin, A, Rivas, C, Bacco, J, Sepúlveda, P, Carvallo, G, Gajardo, C, et al. Prevalence of spasticity and postural patterns in the upper extremity post stroke. J Stroke Cerebrovasc Dis. (2020) 29:105253. doi: 10.1016/j.jstrokecerebrovasdis.2020.105253
5. Lance, JW. The control of muscle tone, reflexes, and movement. Neurology. (1980) 30:1303–13. doi: 10.1212/wnl.30.12.1303
6. Lundström, E, Smits, A, Borg, J, and Terént, A. Four-fold increase in direct costs of stroke survivors with spasticity compared with stroke survivors without spasticity: the first year after the event. Stroke. (2010) 41:319–24. doi: 10.1161/strokeaha.109.558619
7. Li, S, and Francisco, GE. New insights into the pathophysiology of post-stroke spasticity. Front Hum Neurosci. (2015) 9:192. doi: 10.3389/fnhum.2015.00192
8. Li, S, Francisco, GE, and Rymer, WZ. A new definition of Poststroke spasticity and the interference of spasticity with motor recovery from acute to chronic stages. Neurorehabil Neural Repair. (2021) 35:601–10. doi: 10.1177/15459683211011214
9. Pandyan, AD, Gregoric, M, Barnes, MP, Wood, D, Wijck, FV, Burridge, J, et al. Spasticity: clinical perceptions, neurological realities and meaningful measurement. Disabil Rehabil. (2005) 27:2–6. doi: 10.1080/09638280400014576
10. Balaratnam, MS, and Stevenson, VL. Intrathecal baclofen pumps: what the neurologist needs to know. Pract Neurol. (2022) 22:practneurol-2021-003184–246. doi: 10.1136/practneurol-2021-003184
11. Lindsay, C, Ispoglou, S, Helliwell, B, Hicklin, D, Sturman, S, and Pandyan, A. Can the early use of botulinum toxin in post stroke spasticity reduce contracture development? A randomised controlled trial. Clin Rehabil. (2021) 35:399–409. doi: 10.1177/0269215520963855
12. Chinese Medical Association Neurology Branch and Cerebrovascular Disease Group of the Neurology Branch of the Chinese Medical Association. Chinese guidelines for diagnosis and treatment of acute ischemic stroke 2018. Chin J Neurol. (2018) 51:666–82. doi: 10.3760/cma.j.issn.1006-7876.2018.09.004
13. Chinese Medical Association Neurology Branch and Cerebrovascular Disease Group of the Neurology Branch of the Chinese Medical Association. Chinese guidelines for the diagnosis and treatment of intracerebral hemorrhage (2019). Chin J Neurol. (2019) 52:994–1005. doi: 10.3760/cma.j.issn.1006-7876.2019.12.003
15. Cheng, H, Fang, X, Liao, L, Tao, Y, and Gao, C. Prevalence and factors influencing the occurrence of spasticity in stroke patients: a retrospective study. Neurol Res. (2023) 45:166–72. doi: 10.1080/01616412.2022.2127249
16. Nam, KE, Lim, SH, Kim, JS, Hong, BY, Jung, HY, Lee, JK, et al. When does spasticity in the upper limb develop after a first stroke? A nationwide observational study on 861 stroke patients. J Clin Neurosci. (2019) 66:144–8. doi: 10.1016/j.jocn.2019.04.034
17. Shin, YI, Kim, SY, Lee, HI, Kim, DY, Lee, J, Sohn, MK, et al. Association between spasticity and functional impairments during the first year after stroke in Korea: the KOSCO study. Am J Phys Med Rehabil. (2018) 97:557–64. doi: 10.1097/phm.0000000000000916
18. Hotter, B, Padberg, I, Liebenau, A, Knispel, P, Heel, S, Steube, D, et al. Identifying unmet needs in long-term stroke care using in-depth assessment and the post-stroke checklist - the managing aftercare for stroke (MAS-I) study. Eur Stroke J. (2018) 3:237–45. doi: 10.1177/2396987318771174
19. Schinwelski, MJ, Sitek, EJ, Wąż, P, and Sławek, JW. Prevalence and predictors of post-stroke spasticity and its impact on daily living and quality of life. Neurol Neurochir Pol. (2019) 53:449–57. doi: 10.5603/PJNNS.a2019.0067
20. Glaess-leistner, S, Ri, SJ, Audebert, HJ, and Wissel, J. Early clinical predictors of post stroke spasticity. Top Stroke Rehabil. (2021) 28:508–18. doi: 10.1080/10749357.2020.1843845
21. Kjörk, EK, Gustavsson, M, El-manzalawy, N, and Sunnerhagen, KS. Stroke-related health problems and associated actions identified with the post-stroke checklist among nursing home residents. BMC Cardiovasc Disord. (2022) 22:50. doi: 10.1186/s12872-022-02466-3
22. Opara, J, Taradaj, J, Walewicz, K, Rosińczuk, J, and Dymarek, R. The current state of knowledge on the clinical and methodological aspects of extracorporeal shock waves therapy in the Management of Post-Stroke Spasticity-Overview of 20 years of experiences. J Clin Med. (2021) 10:261. doi: 10.3390/jcm10020261
23. Poomalai, G, Prabhakar, S, and Sirala Jagadesh, N. Functional ability and health problems of stroke survivors: an explorative study. Cureus. (2023) 15:e33375. doi: 10.7759/cureus.33375
24. Wissel, J, Schelosky, LD, Scott, J, Christe, W, Faiss, JH, and Mueller, J. Early development of spasticity following stroke: a prospective, observational trial. J Neurol. (2010) 257:1067–72. doi: 10.1007/s00415-010-5463-1
25. Brusola, G, Garcia, E, Albosta, M, Daly, A, Kafes, K, and Furtado, M. Effectiveness of physical therapy interventions on post-stroke spasticity: an umbrella review. NeuroRehabilitation. (2023) 52:349–63. doi: 10.3233/nre-220275
26. Cai, Y, Zhang, CS, Liu, S, Wen, Z, Zhang, AL, Guo, X, et al. Add-on effects of Chinese herbal medicine for post-stroke spasticity: a systematic review and meta-analysis. Front Pharmacol. (2019) 10:734. doi: 10.3389/fphar.2019.00734
27. Güntürk, E, Ögüt, H, Güler, H, and Turhanoğlu, AD. The effect of oral baclofen and botulinum toxin treatments in hemiplegic spasticity on the nociceptive flexor reflex: a randomized clinical trial. Turk J Phys Med Rehabil. (2022) 68:524–31. doi: 10.5606/tftrd.2022.9596
28. Lee, JI, Günther, A, Paus, S, Royl, G, Weyen, U, Wissel, J, et al. Improvement of the treatment of patients with spastic movement disorder after stroke. Nervenarzt. (2024) 95:133–40. doi: 10.1007/s00115-023-01571-8
29. Ou-yang, LJ, Chen, PH, Lee, CH, Li, TY, Wu, YT, Jhou, HJ, et al. Effect and optimal timing of extracorporeal shock-wave intervention to patients with spasticity after stroke: a systematic review and Meta-analysis. Am J Phys Med Rehabil. (2023) 102:43–51. doi: 10.1097/phm.0000000000002019
30. Tian, Y, Yan, X, Wang, H, Dang, C, and Sun, Y. Efficacy of acupuncture therapy for spastic paralysis in post-stroke patients: a systematic review and meta-analysis. Int J Neurosci. (2023) 1-8:1–8. doi: 10.1080/00207454.2023.2292955
31. Wissel, J, and Kivi, A. Post-stroke spastic movement disorder and botulinum toxin a therapy: early detection and early injection. Ann Rehabil Med. (2023) 47:326–36. doi: 10.5535/arm.23108
32. Johnstone, A, Grigoras, I, Petitet, P, Capitão, LP, and Stagg, CJ. A single, clinically relevant dose of the GABA(B) agonist baclofen impairs visuomotor learning. J Physiol. (2021) 599:307–22. doi: 10.1113/jp280378
33. Mihai, EE, Popescu, MN, Iliescu, AN, and Berteanu, M. A systematic review on extracorporeal shock wave therapy and botulinum toxin for spasticity treatment: a comparison on efficacy. Eur J Phys Rehabil Med. (2022) 58:565–74. doi: 10.23736/s1973-9087.22.07136-2
34. Liao, OP, Huang, XY, Wang, C, Zhou, LF, Jiang, SY, Zhou, YL, et al. Features of different contemporary acupuncture and moxibustion schools in the treatment of post-stroke spastic paralysis. Zhongguo Zhen Jiu. (2023) 43:1081–5. doi: 10.13703/j.0255-2930.20220905-k0002
35. Hurth, H, Morgalla, M, Heinzel, J, Daigeler, A, Kolbenschlag, J, and Schuhmann, M. Surgical procedures for treatment of spasticity. Nervenarzt. (2023) 94:1116–22. doi: 10.1007/s00115-023-01568-3
36. Wissel, J, Verrier, M, Simpson, DM, Charles, D, Guinto, P, Papapetropoulos, S, et al. Post-stroke spasticity: predictors of early development and considerations for therapeutic intervention. PM R. (2015) 7:60–7. doi: 10.1016/j.pmrj.2014.08.946
37. Huang, DX. A study to investigate the incidence and risk factors of post-stroke myasthenia gravis. [master’s thesis].[(Fuzhou(Fujian Province)]. Fujian University of Chinese Medicine (2016).
38. Ma, JH. Analysis of risk factors for spastic paralysis after cerebral infarction and correlation study of Chinese medicine evidence elements. [Master’s thesis].[Changsha(HuNan Province)]: Hunan University of Chinese Medicine (2023).
39. Tedesco Triccas, L, Kennedy, N, Smith, T, and Pomeroy, V. Predictors of upper limb spasticity after stroke? A systematic review and meta-analysis. Physiotherapy. (2019) 105:163–73. doi: 10.1016/j.physio.2019.01.004
40. Kazi, SA, Siddiqui, M, and Majid, S. Stroke outcome prediction using admission Nihss in anterior and posterior circulation stroke. J Ayub Med Coll Abbottabad. (2021) 33:274–8.
41. Kwah, LK, and Diong, J. National institutes of health stroke scale (NIHSS). J Physiother. (2014) 60:61. doi: 10.1016/j.jphys.2013.12.012
42. Ryu, JS, Lee, JW, Lee, SI, and Chun, MH. Factors predictive of spasticity and their effects on motor recovery and functional outcomes in stroke patients. Top Stroke Rehabil. (2010) 17:380–8. doi: 10.1310/tsr1705-380
43. Albin, RL, Young, AB, and Penney, JB. The functional anatomy of basal ganglia disorders. Trends Neurosci. (1989) 12:366–75. doi: 10.1016/0166-2236(89)90074-x
44. Picelli, A, Tamburin, S, Gajofatto, F, Zanette, G, Praitano, M, Saltuari, L, et al. Association between severe upper limb spasticity and brain lesion location in stroke patients. Biomed Res Int. (2014) 2014:162754. doi: 10.1155/2014/162754
45. Bavikatte, G, Subramanian, G, Ashford, S, Allison, R, and Hicklin, D. Early identification, intervention and Management of Post-stroke Spasticity: expert consensus recommendations. J Cent Nerv Syst Dis. (2021) 13:11795735211036576. doi: 10.1177/11795735211036576
46. Fernández-de-las-peñas, C, Pérez-bellmunt, A, Llurda-almuzara, L, Plaza-manzano, G, De-la-llave-rincón, AI, and Navarro-santana, MJ. Is dry needling effective for the Management of Spasticity, pain, and motor function in post-stroke patients? A systematic review and Meta-analysis. Pain Med. (2021) 22:131–41. doi: 10.1093/pm/pnaa392
47. Jin, Y, and Zhao, Y. Post-stroke upper limb spasticity incidence for different cerebral infarction site. Open Med. (2018) 13:227–31. doi: 10.1515/med-2018-0035
48. Kerzoncuf, M, Viton, JM, Pellas, F, Cotinat, M, Calmels, P, Milhe de Bovis, V, et al. Poststroke postural sway improved by botulinum toxin: a multicenter randomized double-blind controlled trial. Arch Phys Med Rehabil. (2020) 101:242–8. doi: 10.1016/j.apmr.2019.04.024
49. Keep, RF, Hua, Y, and Xi, G. Intracerebral haemorrhage: mechanisms of injury and therapeutic targets. Lancet Neurol. (2012) 11:720–31. doi: 10.1016/s1474-4422(12)70104-7
50. Qin, J, Gong, G, Sun, S, Qi, J, Zhang, H, Wang, Y, et al. Functional recovery after transplantation of induced pluripotent stem cells in a rat hemorrhagic stroke model. Neurosci Lett. (2013) 554:70–5. doi: 10.1016/j.neulet.2013.08.047
51. Liu, Z, Ji, Y, Zhang, L, Luo, GJ, and Tang, DZ. Study on the correlation between blood glucose level and prognosis in patients with diabetes mellitus combined with acute cerebral infarction. China Drugs and Clin. (2021) 21:3983–5. doi: 10.11655/zgywylc2021.24.011
Keywords: stroke, spasticity, influence factors, post-stroke spasticity, retrospective study
Citation: Zhu C, Li L, Qiu L and Ji G (2024) Risk factors for post-stroke spasticity: a retrospective study. Front. Neurol. 15:1478206. doi: 10.3389/fneur.2024.1478206
Edited by:
Hrvoje Budincevic, University Hospital Sveti Duh, CroatiaReviewed by:
Krishnan Padmakumari Sivaraman Nair, Royal Hallamshire Hospital, United KingdomManuel F. Mas, University of Puerto Rico, Puerto Rico
Copyright © 2024 Zhu, Li, Qiu and Ji. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Guangcheng Ji, d2FuZ2UxMjA3QHNpbmEuY29t
 Chuanxi Zhu
Chuanxi Zhu Lingxu Li
Lingxu Li Long Qiu
Long Qiu Guangcheng Ji
Guangcheng Ji