- 1Yitzhak Shamir Medical Center, Tel Aviv, Israel
- 2The Sagol Center for Hyperbaric Medicine and Research, Assaf Harofeh Medical Center, Ramle, Israel
- 3School of Medicine, Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel
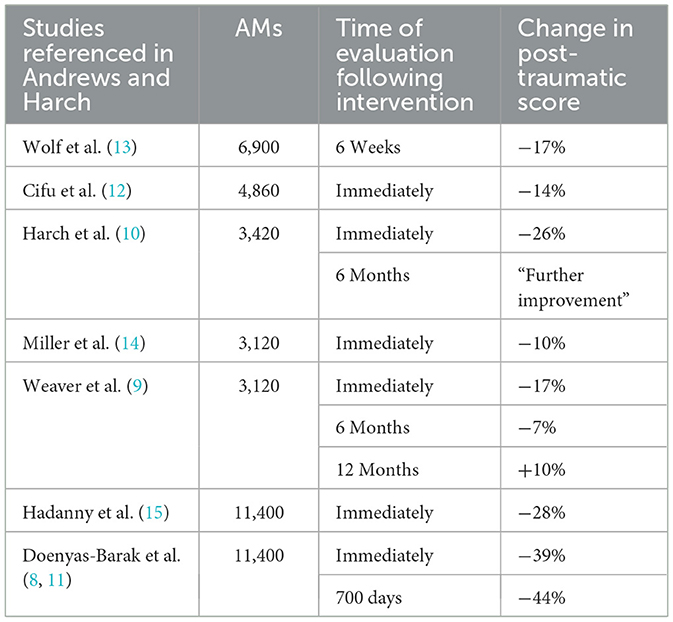
In their manuscript “Systematic Review and Dosage Analysis: Hyperbaric Oxygen Therapy Efficacy in the Treatment of Post-Traumatic Stress Disorder,” (1). Andrews and Harch describe a dose-response curve of hyperbaric oxygen therapy on the post-traumatic symptoms of patients with PTSD. The authors calculated “atmosphere-minutes” (AMs) given in each protocol using a formula that multiplies the atmospheric pressure, fraction of oxygen, session length, and number of sessions. They have found a linear dose-response relationship, with increased symptomatic improvement corresponding to increasing cumulative oxygen doses from 1,002 to 11,400 atmosphere-minutes of oxygen. For example, while the mean decrease in post-traumatic symptom load was 17% to 18% when prescribing 3,000 to 7,000 AMs, it was 30% at 11,400 AMs.
The authors then state that the greater symptomatic response was accompanied by a reversible exacerbation of emotional symptoms at the highest oxygen doses in 30%−39% of subjects. They offer considering sticking to lower doses to avoid emotional exacerbation. However, clinical practice suggests otherwise.
And indeed, the so called “symptom worsening,” frequently accompanied by recollection of previously inaccessible memories, is very common during intensive protocols, necessitating careful and experienced support. While the authors regard memory recollection and the accompanying distress as adverse effects, it may represent an “on-target” effect associated with the direct impact of hyperbaric oxygen therapy (HBOT) on hippocampal-based memory processing in individuals with PTSD (2, 3).
The hippocampus may be more sensitive to HBOT than any other brain region. Studies on hippocampal cell cultures have shown that fluctuations in both pressure and oxygen levels can directly induce orthodromic activity and neural plasticity (4). An increase in hypoxia-inducible factor (HIF) levels related to HBOT has also been shown to contribute to improved hippocampal functions and memory performance (5–7). Furthermore, improved hippocampus activity and connectivity demonstrated in brain imaging following HBOT among veterans with PTSD also support this notion (8).
However, for neuroplasticity to be induced and for long-lasting rather than temporary improvement of symptoms to occur, a long treatment course may be needed. Thus, while short-term response to HBOT using lower AMs may be fair, it is the long-term effect and improvement persistence that may better reflect the structural effect of the different protocols.
Most of the studies in the Andrews and Harch manuscript that evaluated the effect of HBOT on PTSD assessed the short-term effects after treatment completion (Table 1). Only three of the studies also evaluated long-term effects at intervals of 6 months to 2 years. Weaver et al. (9) provided 3,120 AMs and reported a 17% decrease immediately after completion of the HBOT treatment protocol, and attenuation of the improvement to 7% after 6 months and a 10% worsening of symptoms at 12 months. In contrast, in Harch et al. (10), an intensive protocol with twice-daily sessions and 3,420 AMs was prescribed, reporting a 26% decrease in symptoms evaluated immediately after the treatment course completion and “further improvement” at the 6-month evaluation. But Harch also reported transient worsening in some symptoms among 7 of the 30 study participants (of whom 23 had PTSD). It is not clear if the symptom worsening was occurred in the post-traumatic population.
In Doenyas-Barak et al. (11), the short term improvement was 39% and the improvement persisted together with improved social and occupational function 2 years after completion of the 11,400 AMs protocol. Cifu et al. (12) stated in their manuscript that a second evaluation of 3-month time periods following HBOT would be reported; however, no such publication could be found.
To conclude, higher AMs may be necessary not just for better short-term response, but also for changes in brain activity and memory perception that may contribute to long-lasting effects. In addition, given the almost linear correlation between dose and response, the question is whether longer courses are needed to achieve even better respond.
Author contributions
KD-B: Writing – original draft. SE: Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Andrews SR, Harch PG. Systematic review and dosage analysis: hyperbaric oxygen therapy efficacy in the treatment of posttraumatic stress disorder. Front Neurol. (2024) 15:1360311. doi: 10.3389/fneur.2024.1360311
2. Doenyas-Barak K, Kutz I, Lang E, Levi G, Efrati S. Memory surfacing among veterans with PTSD receiving hyperbaric oxygen therapy. Undersea Hyper Med. (2023) 50:395.
3. Efrati S, Hadanny A, Daphna-Tekoah S, Bechor Y, Tiberg K, Pik N, et al. Recovery of repressed memories in fibromyalgia patients treated with hyperbaric oxygen–case series presentation and suggested Bio-Psycho-Social mechanism. Front Psychol. (2018) 9:848. doi: 10.3389/fpsyg.2018.00848
4. Garcia III AJ, Putnam RW, Dean JB. Hyperbaric hyperoxia and normobaric reoxygenation increase excitability and activate oxygen-induced potentiation in CA1 hippocampal neurons. J Appl Physiol. (2010) 109:804–19. doi: 10.1152/japplphysiol.91429.2008
5. Adamcio B, Sperling S, Hagemeyer N, Walkinshaw G, Ehrenreich H. Hypoxia inducible factor stabilization leads to lasting improvement of hippocampal memory in healthy mice. Behav Brain Res. (2010) 208:80–4. doi: 10.1016/j.bbr.2009.11.010
6. Hassouna I, Ott C, Wüstefeld L, Offen N, Neher RA, Mitkovski M, et al. Revisiting adult neurogenesis and the role of erythropoietin for neuronal and oligodendroglial differentiation in the hippocampus. Mol Psychiatry. (2016) 21:1752–67. doi: 10.1038/mp.2015.212
7. Xing J, Lu J. HIF-1α activation attenuates IL-6 and TNF-α pathways in hippocampus of rats following transient global ischemia. Cell Physiol Biochem. (2016) 39:511–20. doi: 10.1159/000445643
8. Doenyas-Barak K, Catalogna M, Kutz I, Levi G, Hadanny A, Tal S, et al. Hyperbaric oxygen therapy improves symptoms, brain's microstructure and functionality in veterans with treatment resistant post-traumatic stress disorder: a prospective, randomized, controlled trial. PLoS ONE. (2022) 17:e0264161. doi: 10.1371/journal.pone.0264161
9. Weaver LK, Wilson SH, Lindblad AS, Churchill S, Deru K, Price RC, et al. Hyperbaric oxygen for post-concussive symptoms in United States military service members: a randomized clinical trial. Under Hyper Med. (2018) 45:1–28.
10. Harch PG, Andrews SR, Fogarty EF, Lucarini J, Van Meter KW. Case control study: hyperbaric oxygen treatment of mild traumatic brain injury persistent post-concussion syndrome and post-traumatic stress disorder. Med Gas Res. (2017) 7:156–74. doi: 10.4103/2045-9912.215745
11. Doenyas-Barak K, Kutz I, Levi G, Lang E, Beberashvili I, Efrati S. Hyperbaric oxygen therapy for veterans with treatment-resistant PTSD: a longitudinal follow-up study. Mil Med. (2023) 188:e2227–e33. doi: 10.1093/milmed/usac360
12. Cifu DX, Hart BB, West SL, Walker W, Carne W. The effect of hyperbaric oxygen on persistent postconcussion symptoms. J Head Trauma Rehabil. (2014) 29:11–20. doi: 10.1097/HTR.0b013e3182a6aaf0
13. Wolf G, Cifu D, Baugh L, Carne W, Profenna L. The effect of hyperbaric oxygen on symptoms after mild traumatic brain injury. J Neurotrauma. (2012) 29:2606–12. doi: 10.1089/neu.2012.2549
14. Miller RS, Weaver LK, Bahraini N, Churchill S, Price RC, Skiba V, et al. Effects of hyperbaric oxygen on symptoms and quality of life among service members with persistent postconcussion symptoms: a randomized clinical trial. JAMA Intern Med. (2015) 175:43–52. doi: 10.1001/jamainternmed.2014.5479
15. Hadanny A, Bechor Y, Catalogna M, Daphna–Tekoah S, Sigal T, Cohenpour M, et al. Hyperbaric oxygen therapy can induce neuroplasticity and significant clinical improvement in patients suffering from fibromyalgia with a history of childhood sexual abuse—randomized controlled trial. Front Psychol. (2018) 9:2495. doi: 10.3389/fpsyg.2018.02495
Keywords: hyperbaric oxygen therapy (HBOT), posttraumatic stress disorder (PTSD), treatment response, memory, treatment dose
Citation: Doenyas-Barak K and Efrati S (2024) Optimizing hyperbaric oxygen therapy for PTSD—The importance of dose and duration for sustained benefits. Front. Neurol. 15:1447742. doi: 10.3389/fneur.2024.1447742
Received: 10 July 2024; Accepted: 12 September 2024;
Published: 26 September 2024.
Edited by:
David F. Tate, The University of Utah, United StatesReviewed by:
Dawn Kernagis, University of North Carolina at Chapel Hill, United StatesCopyright © 2024 Doenyas-Barak and Efrati. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Keren Doenyas-Barak, a2VyZW5kb2VueWFzQGdtYWlsLmNvbQ==
 Keren Doenyas-Barak
Keren Doenyas-Barak Shai Efrati
Shai Efrati