- 1Art Healing and Cognitive Science Research Center, Department of Music, School of Arts and Design, Yanshan University, Qinhuangdao, China
- 2YSU and DCU Joint Research Centre for the Arts, Music College, Daegu Catholic University, Daegu, Republic of Korea
Sleep is essential to human health, yet 27% of the global population suffers from sleep issues, which often lead to fatigue, depression, and impaired cognitive function. While pharmacological treatments exist, non-pharmacological approaches like music therapy have shown promise in enhancing sleep quality. This review, analyzing 27 studies with various experimental paradigms, confirms that music therapy significantly improves subjective sleep quality, largely by alleviating anxiety and regulating mood through perceptual pathways. However, the effects on objective sleep measures remain inconclusive, suggesting that individual differences may play a significant role. Future research should focus on refining intervention designs that integrate both subjective and objective sleep assessments to better elucidate the physiological and psychological mechanisms of music therapy. Key recommendations include personalized music selection, development of age-appropriate interventions, and minimization of external interferences to maximize therapeutic outcomes. Additionally, incorporating variables like psychological status, lifestyle, and environmental factors may offer a more comprehensive understanding of music therapy’s long-term adaptability and effectiveness for diverse populations. This review offers critical research directions and practical support for future applications of music therapy in sleep health.
1 Introduction
Good sleep is essential for maintaining optimal cognitive function, immune response, and overall health (1). However, according to a World Health Organization survey, 27% of the global population suffers from sleep disorders (2), with insomnia frequently causing significant negative impacts on individuals’ physical and mental well-being (3). Sleep disorders mainly involve issues related to sleep quality, sleep duration, and abnormal behaviors, including conditions such as insomnia, hypersomnia, and sleep apnea syndrome. Insomnia-related sleep deprivation is a primary factor contributing to suboptimal health (4). As one of the most prevalent clinical issues (5), sleep-related problems can further lead to other health concerns, such as impaired concentration and memory loss (6), and increase the risk of diabetes, cancer, cardiovascular diseases (7), and neurological disorders (8). Additionally, these issues indirectly interfere with daily tasks, making sleep problems one of the leading causes of traffic accidents (9). Furthermore, sleep problems are often comorbid with mental health issues such as depression (10) and anxiety (11), with a bidirectional relationship that can exacerbate existing conditions and hinder the efficacy of psychological interventions (12, 13).
This widespread health issue has drawn global researchers’ attention, prompting a range of potential solutions, among which music as a non-pharmacological intervention has garnered significant interest. Music therapy (MT), which are low-cost and free of side effects, have been demonstrated to improve sleep quality (14–17). MT’s calming effect on the parasympathetic nervous system can reduce anxiety, blood pressure, heart rate, and respiratory frequency (18), all of which are indicators commonly affected in sleep disorders. These findings support the hypothesis that MT can effectively alleviate sleep disturbances, reduce insomnia symptoms, facilitate sleep onset, and enhance sleep quality (19, 20). This discovery has rapidly captured worldwide researchers’ interest, with the type of music most effective for sleep disorders emerging as a key research focus. Sleep-promoting music may share common objective musical characteristics (21). Empirical studies focusing on intrinsic musical parameters, such as rhythm (22), timbre (23), pitch (24), and genre (25–27), have gained scholarly attention. For example, Ryu et al. found that sleep-inducing music with tempos of 60–80 beats per minute could improve sleep quality (28, 29). The second prominent research focus is on exploring experimental paradigms to verify the efficacy of MT, with neural signal detection emerging as a promising empirical model. Musical input directly affects brain wave patterns and peaks (30), and Electroencephalography (EEG) signals provide an observable means of identifying sleep stages (31), offering a feasible empirical paradigm for inducing, monitoring, and modulating sleep states in music-based conditions. The third frequently discussed topic is the impact of demographic factors on intervention effectiveness. Existing evidence indicates that intervention outcomes may vary by participants’ age or health conditions, indirectly suggesting potential variations in music intervention efficacy across individuals, age groups, and health conditions (32, 33).
It is evident that current research on MT’s impact on sleep disorders is extensive, diverse, and of significant value. However, these studies have yet to be systematically organized and synthesized. To offer a comprehensive understanding and insight into this field, this review aims to systematically consolidate and integrate empirical research on music’s effects on sleep health in recent years. By focusing on three widely discussed aspects—types of music, experimental paradigms, and demographic variables—this review provides a theoretical foundation for music’s therapeutic value in sleep disorders, guiding future empirical research and clinical practice toward more in-depth and comprehensive explorations.
2 Methods
2.1 Inclusion and exclusion criteria
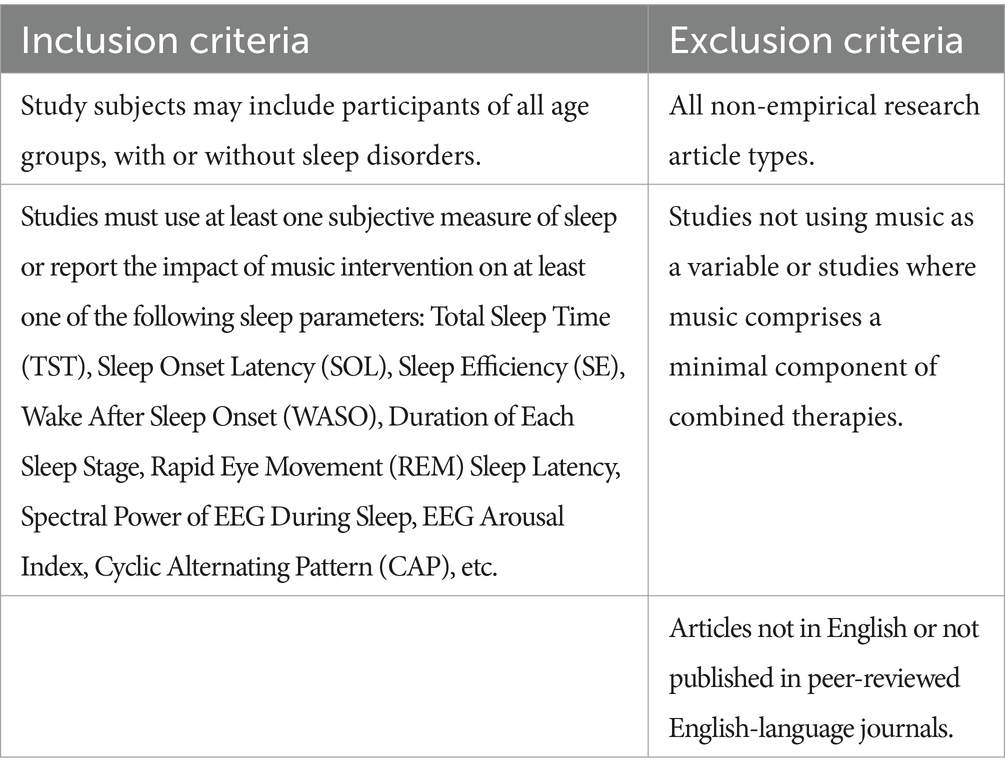
This review employs the meta-narrative review approach, a method that integrates different types of research and methodologies, providing a multi-perspective research view. This approach offers valuable insights into understanding the research progress within a specific field, guiding future research directions, and supporting decision-making (34, 35). The primary aim of this review is to investigate the intervention potential of MT for sleep issues by exploring various sleep-related disorders and diverse populations. Additionally, we aim to provide readers with more detailed insights into the efficacy of MT by analyzing gaps in prior research and suggesting research designs and methodological considerations that may be better suited for future studies. Therefore, empirical studies that align with the research theme are included in this review (Table 1).
2.2 Literature search strategy
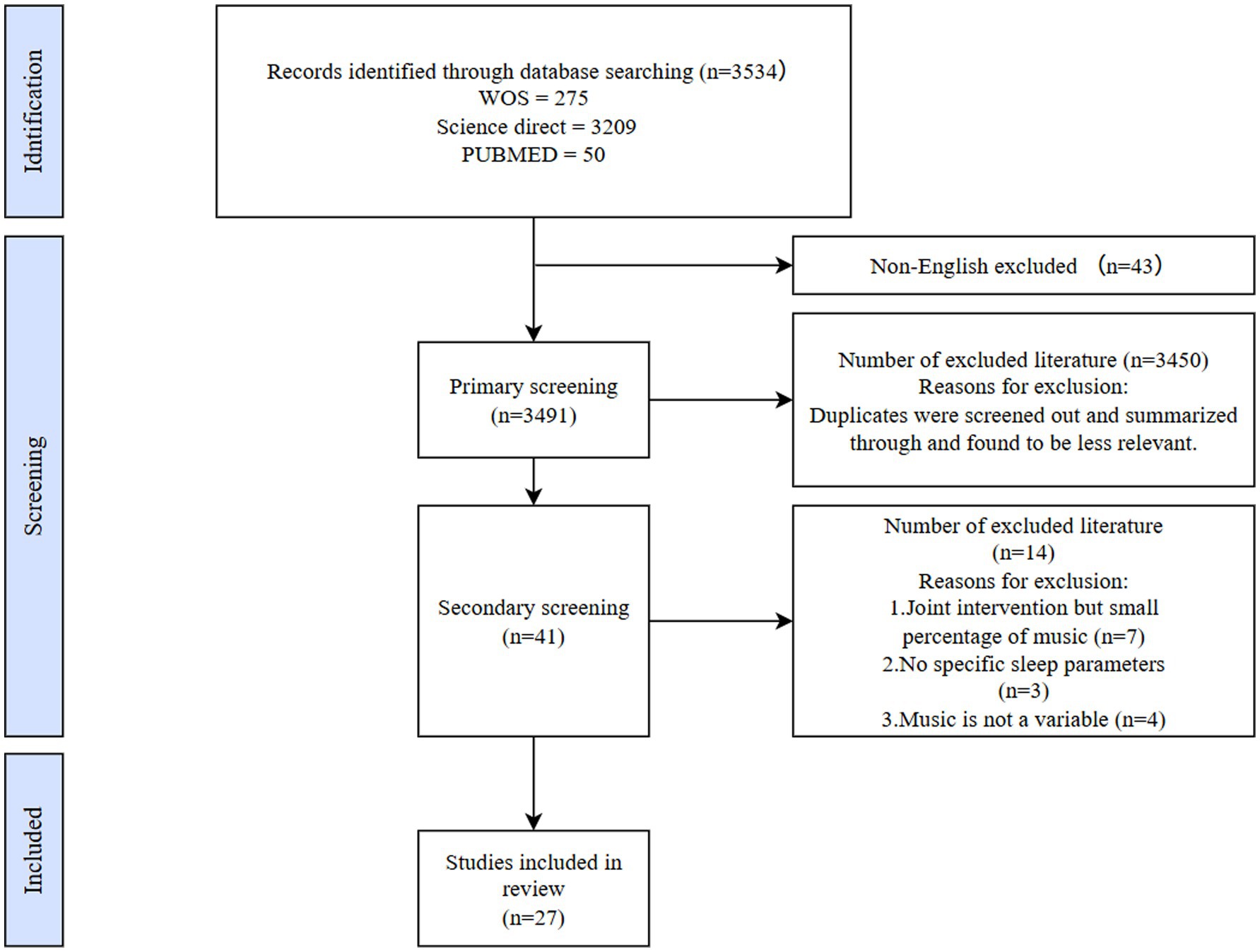
Data for this review were sourced from three databases: Web of Science (WOS), ScienceDirect, and PubMed. The search query was: TS = (“music” OR “musical” OR “music therapy”) AND (“sleep” OR “sleep quality” OR “insomnia” OR “sleep disorders”). The search period was limited to 2019–2023, with the final search conducted on November 10, 2023. Based on this strategy, a total of 3,534 articles were identified. The specific screening process is illustrated in Figure 1. Ultimately, only 27 studies met the inclusion and exclusion criteria and were selected for further analysis (Figure 1).
3 Results
We extracted data on the types of sleep issues studied, sample size and characteristics, intervention designs, sleep measurement methods, and music materials, summarizing the main findings. The measurements and results are presented in Tables 2–4 according to the progression of this study’s content. In all these studies, a recurring topic is which type of MT is effective for specific types of sleep disorders. Therefore, this review also discusses the data from two perspectives: “Mechanisms of Music Therapy” and “Categories of Sleep Disorders Affected by Music Therapy.”
3.1 Effectiveness of music therapy
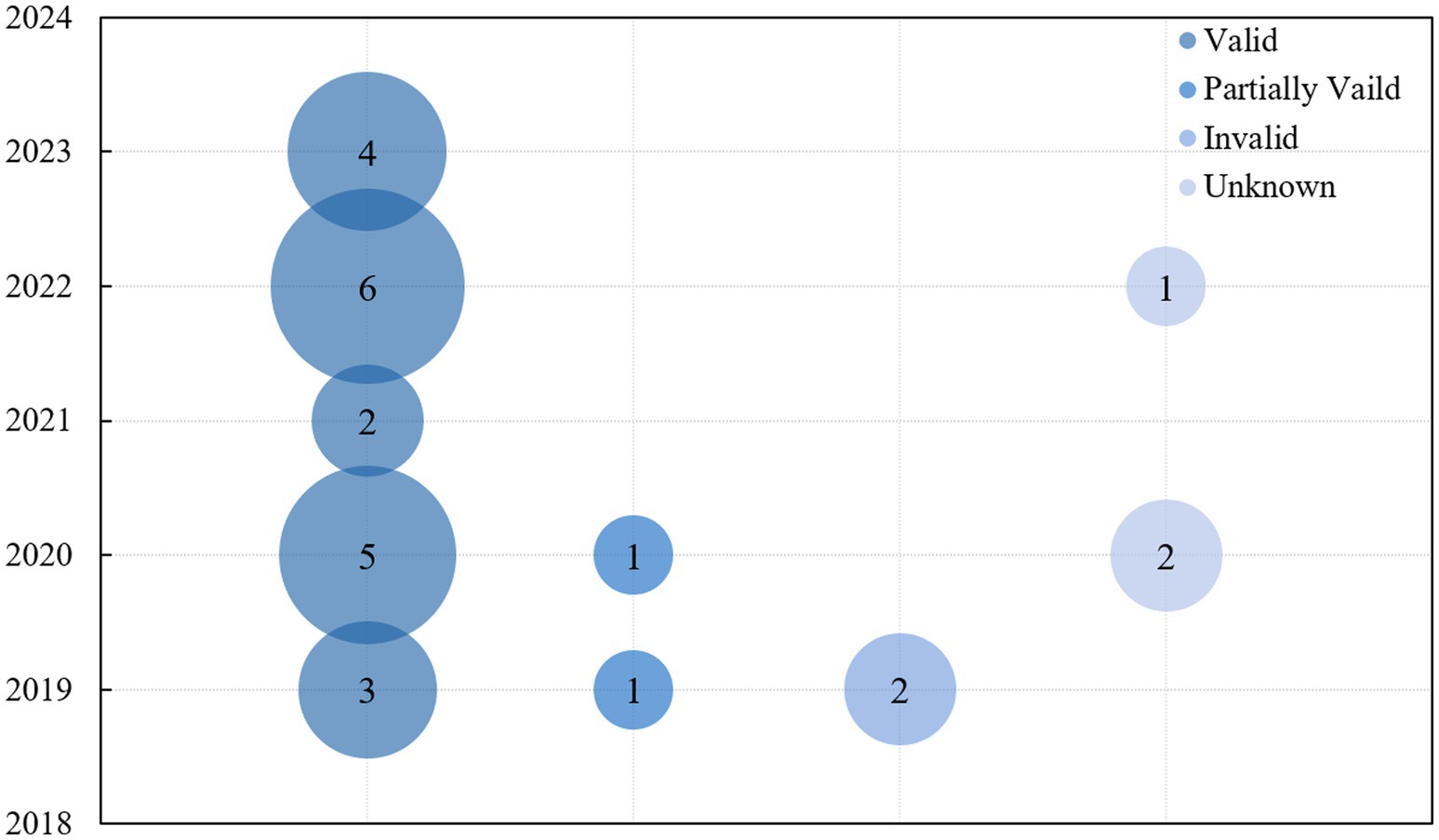
We first focused on the effectiveness of music therapy. To provide a clear visualization of the data from the 27 studies included in this review, intervention-related metrics were integrated and presented through graphical representations. Figure 2 illustrates the distribution of the 27 studies by publication year and their reported effectiveness. Specifically, the studies were categorized into three groups: 20 were identified as effective, 2 as partially effective, and 5 as either ineffective or inconclusive. The bubble chart (Figure 2) uses four distinct colors to represent these categories, while the vertical axis corresponds to the publication year. The size of each bubble reflects the number of studies published in that particular year.
Notably, studies categorized as “effective” accounted for the majority, comprising 74% of the total, while “partially effective” and “ineffective/inconclusive” studies were fewer in number. This distribution underscores the widespread recognition of the therapeutic benefits of music therapy. Over time, the proportion of studies reporting positive outcomes has steadily increased, particularly since 2019, indicating a robust and ongoing validation of music therapy’s efficacy.
3.2 Mechanisms of music therapy
We first focused on the methods used in current research developments. Overall, the influence of music therapy on sleep is primarily characterized through objective sleep monitoring (physiological aspect) and subjective sleep measurement (psychological aspect). Additionally, understanding effective music materials and target populations is essential for a comprehensive grasp of current methodologies.
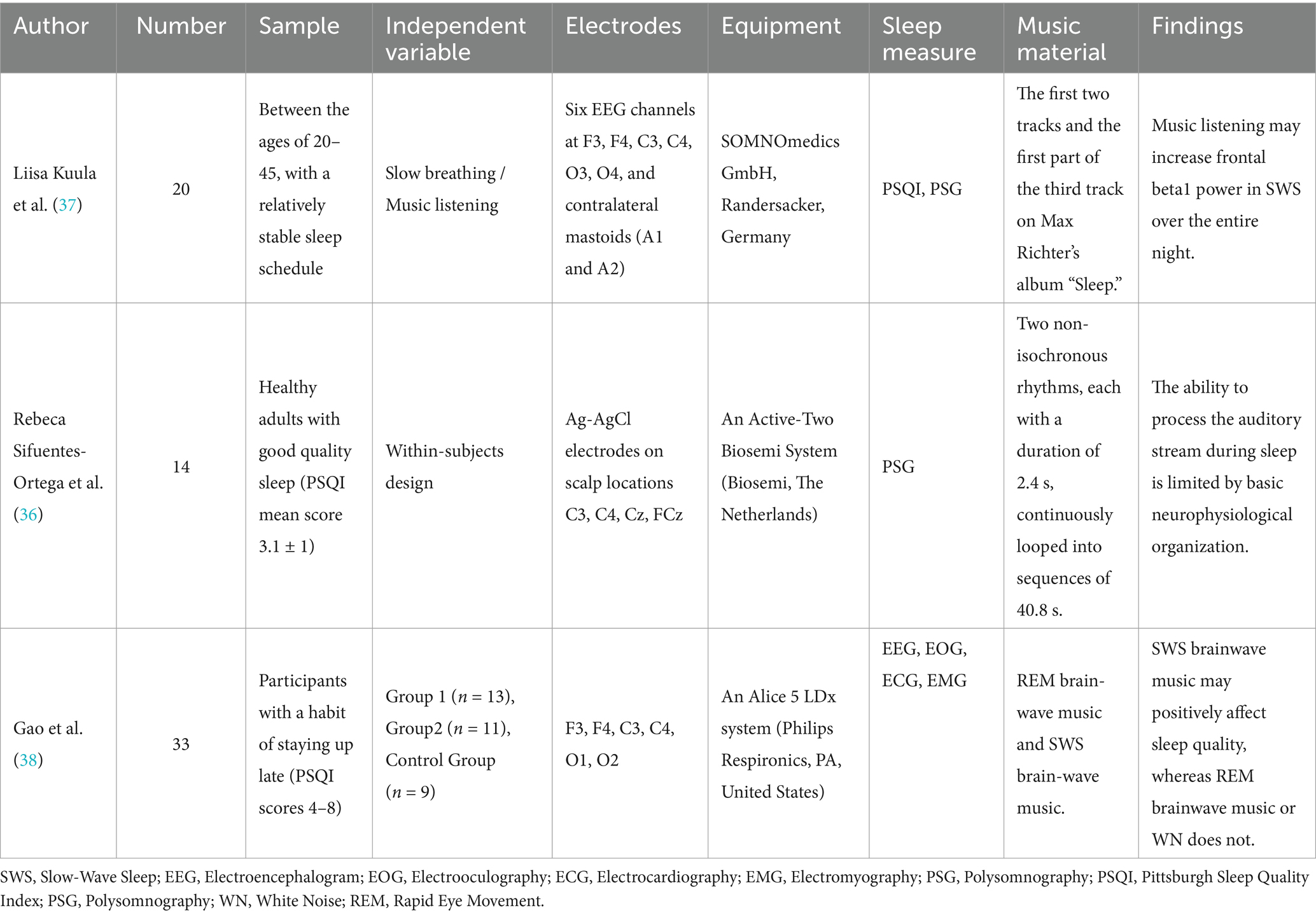
3.2.1 Objective sleep monitoring
Among the 27 empirical studies included in this review, 15 utilized objective sleep monitoring, employing methods such as EEG [6 studies, including 2 with Quantitative Electroencephalography (QEEG)], polysomnography (5 studies), and actigraphy (4 studies). Detailed indicators for these studies are shown in Table 2. Passive music listening’s effect on brain waves during sleep is particularly noteworthy. Sifuentes-Ortega et al. (36) focused on EEG responses across different sleep stages, analyzing music’s modulation effect on brainwave frequencies. Their results demonstrated that in the wakeful state, music induced marked EEG frequency responses to different rhythms; this effect was retained during REM sleep but disappeared in NREM sleep (36). Similarly, Kuula et al. (37) reaffirmed the significance of brainwave representation in a randomized controlled trial investigating the overall impact of music and slow pre-sleep breathing on sleep quality. The results showed that music increased the percentage of stage N3 throughout the night, significantly correlating with the power spectral density in specific EEG bands, suggesting that music may improve sleep structure by increasing the proportion of deep sleep (37).
Notably, the application of brainwave monitoring extends beyond the objective representation of sleep states. Brainwave music, generated by integrating brainwave frequencies with music, produced positive effects in a study involving subjects with frequent late nights. This intervention successfully reduced EEG power spectral density in the Delta wave band and shortened sleep onset latency, thereby improving sleep quality, whereas the control group (REM brainwave music and white noise) did not exhibit similar effects (38).
3.2.2 Subjective sleep measurement
Among the 27 studies included in this review, 16 conducted subjective sleep measurement using various scales. The Pittsburgh Sleep Quality Index (PSQI) was used in 12 studies, the Richards-Campbell Sleep Questionnaire (RCSQ) in 2 studies, the Insomnia Severity Index (ISI) in 1 study, the Sleep Disturbance Scale for Children (SDSC) in 1 study, the Verra and Snyder-Halpern Sleep Scale (VSH) in 1 study, the Jenkins Sleep Scale (JSS) in 1 study, and sleep diaries in 1 study (25). Additionally, eight studies evaluated participants’ anxiety levels (14, 23, 24, 39–43), while five studies focused on patients’ depressive symptoms (23, 24, 39, 43, 44).
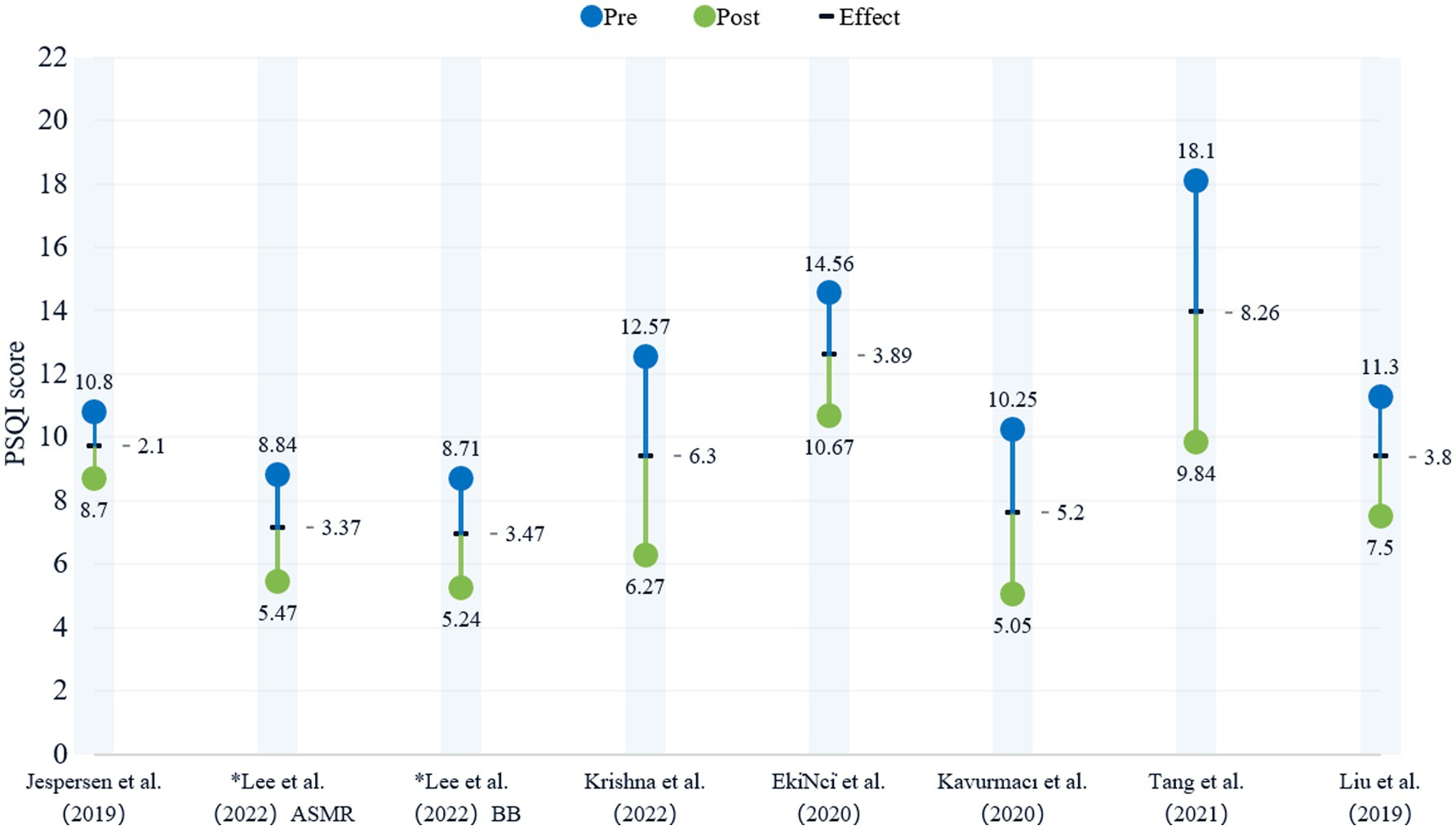
Given that the PSQI was the most commonly used tool in these studies, it is discussed separately. However, only 8 groups from 7 studies provided complete pre-and post-intervention PSQI data. To illustrate this, a bead plot was created, where * indicates two experimental groups within the same study. Blue and green represent the PSQI scores before and after the intervention, respectively, with the specific differences in scores marked in black. As shown in Figure 3, PSQI scores significantly decreased following music therapy, with an average reduction of 4.55. Three studies reported a reduction greater than this average. Notably, participants with higher baseline PSQI scores, such as cancer patients, showed more substantial improvements in sleep quality compared to those with lower baseline scores.
3.2.3 Categories of effective music therapy materials
MT positively impacts sleep by regulating individuals’ emotions and cognitive states. Among the 27 studies, classical music was the most frequently used material (25, 39–45), followed by binaural auditory beats (BB) (23, 39, 46), Autonomous Sensory Meridian Response (ASMR) sounds (23, 46), and natural sounds (47, 48). From the perspective of musical characteristics, most studies opted for slower instrumental or pure music, rather than songs with lyrics or fast-tempo tracks.
3.2.4 Target populations
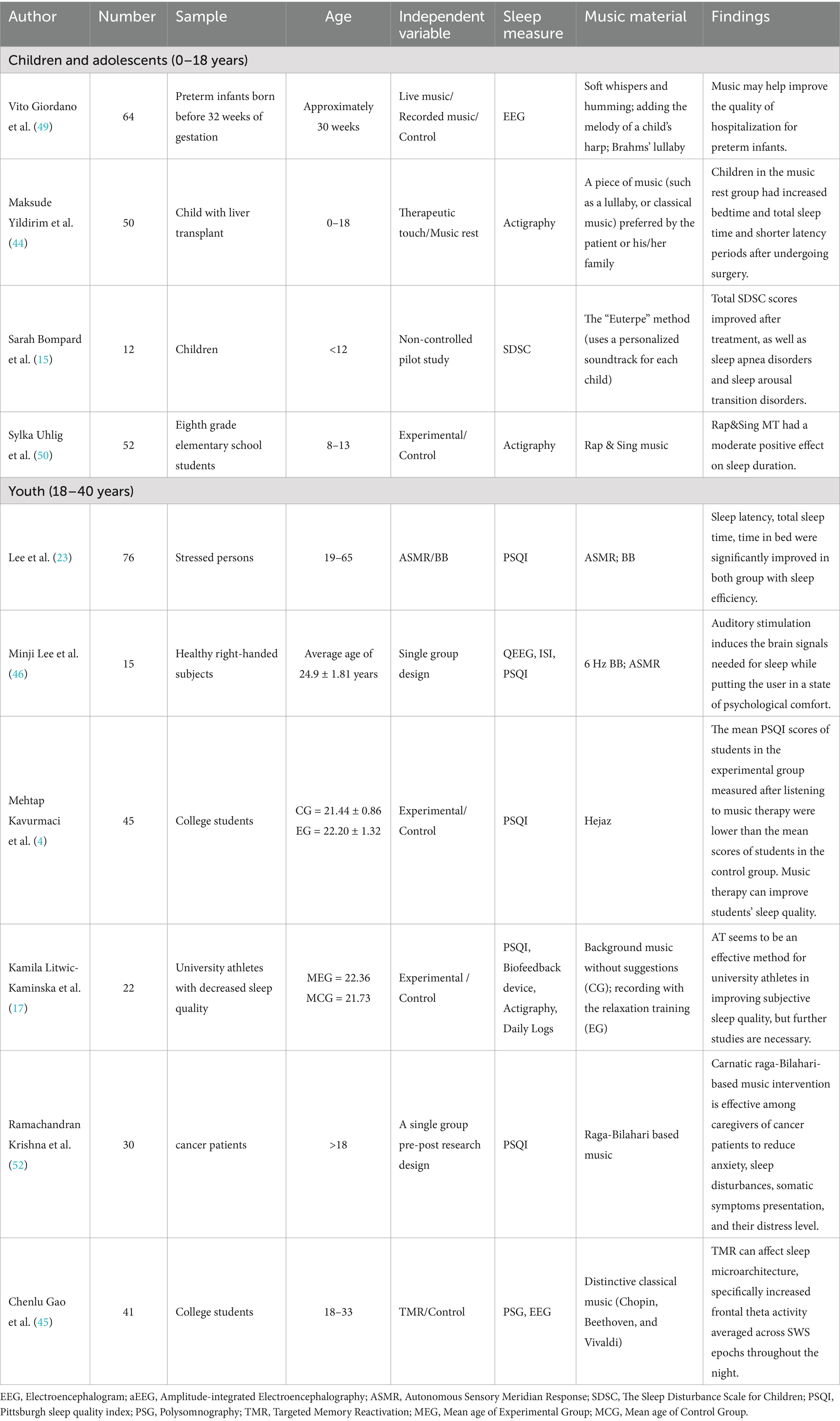
To present the effects of MT on different age groups clearly, participants were categorized into four groups: children and adolescents (0–18 years), young adults (18–40 years), and middle-aged and older adults (over 40 years). Table 3 documents sample size, participant demographics, age range, independent variables, sleep monitoring methods, music materials, and results for each age group.
3.2.4.1 Children and adolescents (0–18 years)
The youngest population successfully impacted by MT in this review was preterm infants. Preterm infants typically require care in the Neonatal Intensive Care Unit (NICU), where the environment may adversely affect their sleep (49). Giordano et al. (49) randomly assigned 64 preterm infants to a live music group, a recorded MT group, and a control group. Amplitude-integrated Electroencephalography (aEEG) was used as the primary assessment measure to monitor the Quiet Sleep (QS) stage. In the live music group, a certified music therapist used touch, vocal interaction, and a small harp, while the recorded music group listened to “Brahms’ Lullaby.” Results showed significant improvements in both music groups during the first and second quiet sleep stages, whereas no changes were observed in the control group (49).
The sleep quality of slightly older children also benefited from MT. Children (0–18 years) who had undergone liver transplants were divided into a therapeutic touch group (N = 25) and a music relaxation group (N = 25) for three consecutive days of therapeutic touch and music relaxation sessions (20 min each). Sleep was assessed before and after each session using actigraphy. Results indicated that post-operative bed time, total sleep time, and sleep efficiency improved in the therapeutic touch group, while the music relaxation group showed increases in bed time and total sleep time, highlighting the positive effects of both interventions on sleep in liver transplant children (44).
Additionally, Bompard et al. (15) utilized an innovative “Euterpe” music therapy method (incorporating sound and various types of sensory stimuli) for children with developmental disabilities. This personalized music creation combined the child’s vocal memories with family scenes, maternal voice, and other familiar sounds. After 12 days of treatment, subjective assessments of sleep quality were made using the Sleep Disturbance Scale for Children (SDSC). Results indicated significant improvement in sleep quality among children with developmental delays (15).
Adolescents also experienced positive effects. A group of adolescents (N = 52) participated in weekly rap MT sessions (45 min each) over 4 months, conducted by a music therapist. Sleep variables were objectively assessed using actigraphy. Results showed a general reduction in total sleep time across participants, though rap MT did not significantly improve overall sleep quality. However, it did have a modest positive impact on sleep duration (50).
3.2.4.2 Young adults (18–40 years)
Among young adults, university students were the primary focus in recent studies. Litwic-Kaminska et al. (17) conducted music therapy sessions for college athletes during pre-sleep training, involving 31 student athletes with PSQI scores ≥5. The experimental group listened to a self-produced recording based on Autogenic Training (AT) to aid relaxation, while the control group listened to background music. During the sessions, pulse, heart rate, skin conductance, and temperature were recorded using four sensors on the fingers, and breathing was measured via an abdominal sensor. Both objective (sensors) and subjective (PSQI) assessments indicated that overall sleep quality significantly improved in the experimental group, with no notable change in the control group (17).
Lee et al. (23, 46) conducted two interrelated studies within 5 years to verify the effectiveness of ASMR and BB as MT materials. The first study involved 76 stressed adults, with sleep quality subjectively assessed using PSQI and ISI. Results showed that both ASMR and BB significantly improved sleep quality (46). The second study involved 15 healthy adult males, using EEG to monitor sleep metrics. This study combined ASMR and BB as “Combined Stimuli” (CS) for sleep induction. Results indicated that CS induced brain activity at 6 Hz, within the theta frequency range, associated with stage 1 of non-REM sleep (NREM) (23).
Music has also shown promise in promoting sleep while activating memory. A study with 50 undergraduate students used polysomnography (PSG) for objective sleep monitoring. The Targeted Memory Reactivation (TMR) group listened to classical music pieces by Chopin, Beethoven, and Vivaldi, while the control group listened to white noise before sleep and during slow-wave sleep. Results revealed that the TMR group experienced increased theta activity in the frontal cortex during slow-wave sleep, indicating that TMR influenced microstructural sleep characteristics, especially enhancing average frontal theta activity throughout the night (45). Additionally, studies confirm that the Hejaz melody exerts a soothing and calming effect throughout the night, improving sleep quality in university students (4). Lastly, Snipes et al. (51) introduced supplementary methods (such as slow breathing exercises) to enhance MT. EEG data analysis showed that the combined use of these methods increased the likelihood of deep sleep, enhancing delta power during the Slow Wave Sleep (SWS) stage, thereby promoting higher quality deep sleep (51).
3.2.4.3 Middle-aged and older adults (>40 years)
Krishna et al. (52) conducted a novel study with 30 cancer caregivers, including 20 middle-aged and older caregivers, using Bilahari Raga from Carnatic music as the therapeutic material. This month-long MT intervention demonstrated significant effects in reducing caregivers’ anxiety and improving sleep quality (52). It is noteworthy that in the empirical studies included in this review, sleep disorders in middle-aged and older adults commonly co-occur with pain and anxiety stemming from various health conditions, which will be discussed in detail in section 4.2.3.
3.3 Categories of sleep disorder effected by music therapy
Previous studies have identified several key areas within sleep-related issues and provided valuable insights into the efficacy of MT. However, consensus on defining categories of insomnia remains elusive. The International Classification of Sleep Disorders (Third Edition, ICSD-3) includes insomnia disorders such as chronic insomnia, short-term insomnia, and other insomnia types (53), and this classification standard has been widely recognized in the medical field as authoritative. In the included studies, however, insomnia categories are primarily determined by referencing established scales or multiple physiological indicators (e.g., polysomnography, ISI, or PSQI results). Furthermore, this categorization is complicated by the coexistence of various comorbidities. To better illustrate the results, we reclassified the studies based on ICSD-3 standards (Table 4 presents sample size, participant demographics, independent variables, sleep monitoring methods, music materials, and outcomes). Specifically, in the 27 studies included in this review, categories of sleep disorder effected by MT were as follows:
1. Chronic Insomnia (1 study included): ICSD-3 defines chronic insomnia as having symptoms for at least 3 months, occurring at least 3 times per week (53). Participants with insomnia duration meeting this criterion were classified accordingly.
2. Mild Insomnia (2 studies included): Participants with ISI scores between 8 and 15 exhibited only mild insomnia symptoms and did not meet the diagnostic criteria for insomnia disorder per international standards, thus classified as mild insomnia.
3. Other Insomnia (14 studies included): Studies addressing sleep issues arising from comorbid conditions but without a specific definition of insomnia symptoms were grouped under other insomnia.
4. Non-Pathological Health Concerns (10 studies included): Studies focused on enhancing sleep quality in healthy individuals were classified within this category.
3.3.1 Chronic insomnia
Jespersen et al. (25) conducted the only recent study specifically addressing chronic insomnia. They performed a three-week randomized controlled trial involving 57 patients with chronic insomnia (average insomnia duration of 10.3 years). Participants were randomly assigned to a music group, an audiobook control group, and a waitlist control group. Objective sleep indicators were assessed using polysomnography and actigraphy. Subjective sleep measurements (including ISI and PSQI) revealed that the music group experienced a significant reduction in insomnia severity and an improvement in quality of life compared to the control groups. However, objective sleep measurements indicated no significant differences in sleep parameters across groups, and further analysis showed no impact of music on the amount of time spent in different sleep stages. Although music had a notable effect on sleep perception and quality of life in chronic insomnia patients, there was no significant impact on objective sleep metrics or insomnia severity (25).
3.3.2 Mild insomnia
Similar to chronic insomnia, research attention on mild insomnia remains limited. Lee et al. (39) conducted a trial using music embedded with binaural beats (BB) for subclinical insomnia patients with ISI scores below 15. The results indicated an increase in δ and θ power and a decrease in α power during exposure to BB-enhanced music, suggesting that music listening promoted relaxation and sleep. The increase in θ waves also indicated that BB might induce sleepiness (39). Additionally, Ho et al. (47) employed an innovative intervention for mild insomnia by using an audio pillow with embedded speakers to deliver brainwave entrainment sounds (α and θ beats) that synchronized with brain activity. This technology allowed for observation of sleep stage proportions. Results showed that participants using the audio pillow experienced a slight reduction in time spent in stages 1 and 2, with an increase in time spent in stage 3 and REM sleep. Although these changes were not significantly different from the control group, the audio pillow group showed a significantly shorter sleep onset latency, indicating a positive effect on falling asleep. Furthermore, there was no significant change in melatonin levels before and after the experiment, suggesting that light, rather than sound, might be the primary influence on melatonin production during sleep induced by the audio pillow (47).
3.3.3 Other insomnia disorders
Insomnia commonly coexists with various physiological and psychological disorders, accounting for 51.85% of the studies reviewed.
3.3.3.1 Sleep structure in patients with schizophrenia
Schizophrenia patients often experience abnormal sleep structures, such as deficits in SWS and reduced REM sleep duration (54, 55). Lu et al. (40) conducted a MT intervention for patients with chronic schizophrenia experiencing sleep disturbances. The severity of sleep disturbances was evaluated using the PSQI, with patients scoring above 5 included in the study. Patients attended MT sessions in the activity room from 9:00 to 10:00 PM over 4 weeks. Results indicated a significant reduction in PSQI scores in the MT group, though the effect on sleep quality improvement was less pronounced for older patients (40).
3.3.3.2 Sleep issues in asymptomatic COVID-19 patients
Asymptomatic COVID-19 patients often experience insomnia due to prolonged negative emotions, viral infection, and subsequent isolation, which can lead to sleep disturbances, anxiety, and depression. Wang et al. (24) conducted a study involving 200 asymptomatic COVID-19 patients, where the treatment group practiced Baduanjin Qigong (i.e., 八段锦气功) and received Five Elements music therapy. Specific music pieces were chosen based on the effects of different modes on internal organ functions, such as using the “Yu” (i.e., 羽) tone to nourish kidney yin, “Shang”(i.e., 商) tone to moisten the lungs, and “Zhi” (i.e., 徵) tone to clear heart fire. These musical pieces were played at designated times to aid in adjusting patients’ physical and emotional states. The results showed that the combined intervention significantly improved sleep quality compared to patients who received only standard care (24).
3.3.3.3 Sleep issues in medical settings
Patients in medical settings often experience poor sleep quality due to hospital noise, lighting, temperature, and care interruptions (56), which can contribute to insomnia. This issue has received significant attention in the literature.
Liu et al. (48) conducted a controlled study on osteosarcoma patients, where the MT group received a combination of mindfulness-based stress reduction (MBSR) and diverse music selections, including calming natural background music, rhythmic upbeat music, and soothing hopeful tunes. The control group received standard care only. Each session began with 30 min of MT by a professional music therapist, followed by MBSR led by a psychologist, and concluded with another 30 min of music. Pain (Wong-Baker Faces Pain Rating Scale, WBRS), anxiety (Hamilton Anxiety Rating Scale, HAM-A), and sleep quality (PSQI) were assessed before and after treatment. Results indicated that MT significantly reduced pain and anxiety levels and improved sleep quality in osteosarcoma patients (48). Similarly, a study involving hematologic cancer patients divided participants into control (n = 30) and experimental groups (n = 30). Before the intervention, both groups had poor sleep quality with average PSQI scores of 14.50 ± 2.70 (control) and 14.56 ± 2.00 (experimental). The experimental group received MT (30–40 min each night for 1 week), while the control group did not receive MT. Results showed a significant reduction in PSQI and State–Trait Anxiety Inventory (STAI) scores in the MT group, indicating that MT effectively improved sleep quality and reduced anxiety in elderly cancer patients (57).
Six-step music therapy was also shown to alleviate pain, reduce anxiety, and improve sleep quality in patients undergoing platinum-based chemotherapy for lung cancer. The study included 100 small-cell lung cancer patients randomly assigned to a MT group or a control group. Music selections were chosen based on patient preferences, and the six steps included: (1) improvisation (group MT); (2) music-assisted progressive muscle relaxation (individual pre-sleep therapy); (3) music imagery (individual therapy during chemotherapy); (4) music breathing exercises (group therapy after each chemotherapy injection); (5) instrument playing (group therapy during chemotherapy); and (6) rhythmic activities (group therapy). Patients completed the Self-Rating Anxiety Scale (SAS), Visual Analog Score (VAS), and PSQI before chemotherapy, the first day post-chemotherapy, and 5 days post-chemotherapy. The MT group showed significantly reduced anxiety and pain scores, with higher PSQI scores than the control group (14).
Interestingly, Kim et al. (42) demonstrated the efficacy of a single MT session for post-operative elderly patients in the ICU. A total of 133 patients were randomly assigned to an Interactive Music Therapy (IMT) group, a Passive Listening (PL) group, and a control group. The IMT group received a 20-min interactive music session led by a music therapist, followed by individual evening music listening, while the PL group received only evening music listening, and the control group received standard care without MT. Melatonin and cortisol levels were measured before surgery, on the day of surgery, and the day after. Sleep quality was assessed using the RCSQ. Results indicated an increase in melatonin levels in the IMT group, while cortisol levels showed no significant difference between groups. Interactive music was found to significantly improve subjective sleep quality in ICU post-operative elderly patients (42).
Moreover, the positive effects of MT have been repeatedly validated in other patient groups, including those undergoing Mitral Valve Replacement (MVR) surgery (41), heart failure patients (43), and burn patients (58). After 30-min music therapy sessions, early post-operative MVR patients experienced significant reductions in pain (VAS) and anxiety (SAS), with Verran and Snyder-Halpern (VSH) results indicating improved sleep duration and subjective sleep quality scores compared to the control group (41). Heart failure patients who listened to music for 30 min daily for 3 months reported significantly improved subjective sleep quality (assessed by PSQI) compared to the control group, suggesting MT’s efficacy in improving sleep for heart failure patients (43). In a 4-day randomized controlled trial with burn patients, the passive MT group (listening to an mp3 recording of the Huseyni melody played by the OTAG Music Center) reported significantly better sleep quality (measured by RCSQ) and reductions in pain and anxiety compared to the reflexology massage group and control group (58).
3.3.4 Non-pathological health concerns
Sleep issues among healthy individuals also warrant attention. Pramita et al. (59) conducted a study on 15 healthy males with a history of delayed sleep onset to assess the impact of specific frequency music on sleep structure. Participants underwent sleep studies over a week with and without music intervention, measuring parameters such as EEG, Electrocardiogram (ECG), and Electromyography (EMG). Results indicated that the music group exhibited increased alpha power during sleep compared to the non-music group. Music at a frequency of 432 Hz had a significant relaxing effect on the brain, though its impact on sleep onset latency remained unclear, particularly among individuals with delayed sleep onset (59). Another study used EEG to objectively monitor sleep and found that Sundanese music from West Java, Indonesia, promoted calm and relaxation in brain activity, positively contributing to daytime sleep quality (60).
4 Discussion
This study reviews empirical research from the past 5 years on the effects of music therapy (MT) on sleep, offering new theoretical support for future applications and research in MT. We included 27 recent empirical studies to examine effective categories and mechanisms of MT. The analysis revealed that MT significantly improved subjective sleep quality, though its effects on objective sleep metrics varied, suggesting that music primarily influences sleep quality through subjective pathways, such as emotional regulation and anxiety relief. In terms of effectiveness, the majority of studies (74%) showed positive results, with music therapy’s effectiveness being increasingly validated in recent years. Unlike previous meta-analyses that focused mainly on randomized controlled trials, this review included a variety of experimental paradigms, extending the evaluation dimensions to provide a comprehensive assessment of MT ‘s effects.
4.1 Gaps in the methodology
4.1.1 Objective sleep monitoring
There is no perfect sleep assessment method, but objective evaluation remains crucial for accuracy (61). Combining objective and subjective approaches can enhance assessment reliability. Music therapy’s effects on physiological metrics are often represented through measures like sleep onset latency, total sleep duration, and specific sleep stages (e.g., deep sleep) (52, 62). It has been demonstrated that music significantly shortens sleep onset time and extends the duration of NREM sleep (37). Furthermore, the use of various physiological signal monitoring techniques has enriched our understanding of the physiological mechanisms of MT. Music intervention may aid in reducing cortical arousal levels, helping individuals to enter stable sleep more rapidly. Insomnia patients typically exhibit heightened cortical activity before and during NREM sleep, which can hinder natural sleep onset (63). Despite its value, objective sleep monitoring has not received adequate attention. Future studies should further apply objective tools like EEG to monitor the impact of different types of music on brain activity in insomnia patients, providing quantitative data to support a theoretical framework for music intervention mechanisms (49).
4.1.2 Subjective sleep measurement
Subjective sleep measurement methods are well-established, with many validated tools available. Instruments such as the PSQI, RCSQ, and ISI are widely used to assess individuals’ personal sleep experiences (64). PSQI, due to its universal applicability, reliability, and validity, is the most commonly used subjective sleep assessment tool. Interestingly, reported sleep quality often correlates with various emotional factors. MT has been shown to positively affect sleep quality, as evidenced by an average reduction of 4.55 in PSQI scores. Notably, greater improvements were observed in studies exceeding this average reduction, as well as among participants with higher baseline PSQI scores, such as cancer patients, as demonstrated in Tang et al. (14). The positive effect of MT on sleep quality is also linked with improvements in quality of life (50, 65), relief from anxiety and depression (57), and enhanced life satisfaction (18). Combining subjective sleep measurement with psychological assessment tools offers an excellent perspective for investigating the psychological mechanisms of MT’s impact on sleep. Future research could integrate subjective sleep quality and emotional assessment tools to further verify MT‘s positive impact on overall health.
4.1.3 Categories of effective music therapy materials
MT encompasses a diverse array of therapeutic approaches, emphasizing personalization and context-specific application. Different music materials used during MT can have varied impacts on sleep quality, making it essential to explore the most effective therapeutic approaches. The most commonly used music materials in the reviewed studies were classical music, natural sounds, and 432 Hz audio. Music materials typically share features such as a slow tempo, minimal rhythm changes, and moderate pitch variation (66). Tempo synchronized with the average heart rate (60–80 bpm) is an important indicator, aiding relaxation (67, 68). Additionally, emerging audio technologies (e.g., BB, audio entrainment, and brainwave music) have shown promising results in improving mild insomnia. MT interventions are generally set to play music 30 min to an hour before sleep, with a duration of 20–30 min, to help individuals reach a relaxed state conducive to sleep onset without disrupting sleep structure (15, 20). The music volume during MT should be controlled at 40–50 decibels to avoid disturbing natural sleep (20).
Many researchers also prefer using participants’ preferred music to improve relaxation and reduce negative emotions, which can facilitate sleep. However, such music may induce Involuntary Musical Imagery (INMI, or “Earworm”), due to familiarity, melody characteristics, and lyrical content differences (69). INMI is the spontaneous recollection and repetition of a melody in one’s mind (69), a phenomenon common in daily life (70). Studies suggest that INMI could lead to continuous “replaying” of melodies in the mind, potentially disrupting relaxation and negatively impacting sleep (71, 72). Additionally, specific groups, such as musicians and individuals with obsessive-compulsive disorder (70), may experience INMI symptoms more frequently. This raise concerns that familiar, preferred music might bias sleep intervention outcomes. However, no recent studies have addressed this issue. Avoiding familiar or popular music in favor of playlists curated by professional music therapists could potentially reduce INMI’s interference, a hypothesis that should be tested in clinical studies to clarify INMI’s actual impact in MT.
4.1.4 Target populations
Existing research suggests that m MT has varied effects on sleep improvement across different age groups. Research on middle-aged and older adults is more common, focusing primarily on music’s role in addressing age-related sleep issues (e.g., insomnia, reduced sleep quality) (40). These studies typically demonstrate that MT improves sleep quality in middle-aged and older adults by reducing anxiety and alleviating mood fluctuations, but such improvements may not be fully applicable to younger populations (57). For example, a study on cancer caregivers found that music in specific modes effectively reduced anxiety and improved sleep quality, though the same effect might not apply to other healthy adults (52).
In comparison, studies on MT for sleep among children, adolescents, and young adults are limited. Existing research indicates that certain groups, such as preterm infants (49) and children with developmental delays (15), may be more responsive to music’s positive effects. Adolescents, as a unique group, have complex sleep intervention needs, and MT has shown limited effects on their overall sleep quality, possibly only improving specific sleep variables (e.g., sleep duration) (50). This effect has been shown to occur indirectly through relaxation and anxiety relief (17). In healthy young adults without sleep disorders, music’s impact on deep sleep enhancement appears limited (37).
In summary, while MT demonstrates certain positive effects on sleep across different age groups, current research on children, adolescents, and young adults remains insufficient. Future studies should address the specific needs of these age groups to develop more targeted MT strategies, optimizing the application of MT across diverse age demographics.
4.2 Gaps in the research
Insomnia is one of the most common health issues and the most prevalent sleep disorder among the general population (73). While the effectiveness of traditional treatments, such as medication and cognitive behavioral therapy, has been established, only a small percentage of patients pursue these approaches, largely because they are predominantly accessible in academic and research settings (74). Against this background, MT presents considerable potential as a convenient and flexible non-pharmacological intervention (75).
4.2.1 Potential bias in subjective and objective insomnia evaluation standards
A primary gap in current research is the inconsistency in evaluation standards. Insomnia diagnosis relies mostly on subjective assessments of sleep insufficiency, yet discrepancies often arise between subjective complaints and objective measurements. Studies on music’s effects on objective sleep metrics are limited, and results show variability compared to subjective sleep quality (16). This variability may result from factors like the protective role of positive emotions (63), heightened cortical arousal in insomniacs (76), and limitations in assessment methods.
Music improves sleep quality by modulating brain activity. It reduces beta waves linked to tension, enhances alpha waves associated with relaxation, and promotes parasympathetic activity, lowering cortical arousal and facilitating relaxation (77, 78). However, insomniacs’ heightened sensitivity to stimuli during sleep often prevents deep sleep, reducing MT’s effectiveness on objective measures (63). These findings are consistent with Chang et al. (19). Some studies suggest music improves both subjective and objective sleep, as shown by reduced N1 duration. However, this evidence comes from nap studies and excludes rapid eye movement (REM) sleep, leaving its relevance to general sleep disorders unclear (16).
Music also improves subjective sleep perception through emotional regulation. It activates the auditory cortex and limbic system (e.g., the amygdala), reduces anxiety, and induces dopamine release, enhancing positive emotions and subjective sleep evaluations (79, 80). Yet, these subjective improvements do not always align with physiological changes. Insomniacs often experience sleep illusion, perceiving wakefulness despite EEG data indicating light sleep (81, 82).
Limitations in assessment tools worsen the gap between subjective and objective evaluations. Polysomnography (PSG), while effective at capturing physiological states, fails to represent the restorative experience central to sleep perception (80–82). These limitations contribute to inconsistent findings and hinder a full evaluation of MT’s effects. Combining subjective and objective methods is essential for bridging this gap and better understanding MT’s impact.
4.2.2 Variability in classification standards leading to imbalanced focus on different sleep problems
This review’s investigation into effective intervention categories was limited by the inconsistency in sleep disorder definitions across included studies. Researchers seem to employ varied standards, such as ICSD-3, ISI, and PSQI, resulting in insufficient focus on specific sleep disorders, making it challenging to cluster studies into a cohesive theoretical framework. Inconsistent standards may also lead to insufficient inclusion of certain conditions (83), restricting comprehensive attention to sleep disorders. For instance, chronic insomnia places a heavy burden on individuals and society, manifesting in reduced quality of life, increased absenteeism, and decreased work productivity (84). Moreover, chronic insomnia is often comorbid with physical and mental disorders (73, 85, 86). However, relying solely on insomnia duration as a criterion poses theoretical limitations and lengthens the experimental cycle, limiting the scope of investigation (25). Similarly, while mild insomnia lacks the prominent features of sleep disorders, it can develop into more severe sleep issues if not addressed early (87, 88). Therefore, effective intervention for subclinical insomnia is key to preventing the progression of insomnia. Since 2019, only two studies have used ISI scores (ISI = 8–15) to define mild insomnia when selecting participants. This metric is feasible but not fully aligned with international sleep disorder standards. Objective sleep monitoring results in these two studies showed positive effects of music, including reduced sleep onset latency (47) and increased theta wave power (39), confirming MT’s efficacy for mild insomnia patients. Nonetheless, the possibility of bias cannot be ruled out. To overcome this limitation, future studies should adopt standardized and replicable diagnostic criteria to ensure consistency and comparability in research outcomes.
4.2.3 Difficulty in controlling variables due to comorbidity
Emotions and pain significantly impact sleep quality, with insomnia and poor sleep quality often exacerbating negative emotions, such as anxiety and depression, while high sleep quality is associated with positive emotions (63). Moreover, there is a bidirectional relationship between anxiety and future insomnia, as insomnia can further exacerbate future anxiety (89). Multiple studies confirm MT’s effectiveness in promoting sleep and managing pain and anxiety (14, 24, 41–43, 48, 57, 58). In this review, 25% of the studies involved participants with comorbid conditions, where sleep disturbances were often accompanied by one or more disorders, such as schizophrenia, COVID-19, osteosarcoma, hematologic cancer, lung cancer, heart failure, and burns. These conditions often trigger persistent anxiety and pain, further impacting sleep quality. Postoperative patients, for instance, are prone to insomnia due to physical trauma and pain during recovery. Pain not only causes physical discomfort but also induces negative emotions, such as anxiety, which in turn disrupt sleep. This dual effect underscores the importance of pain management in postoperative recovery. Effective pain control can reduce anxiety and significantly improve sleep quality, possibly due to the protective value of positive emotions induced by music, particularly for subjective sleep perception (63). For postoperative patients, hospital noise, especially at night, can severely disturb sleep. Reducing noise levels in hospital environments can effectively alleviate sleep disturbances in hospitalized cancer patients (90). Although the positive outcomes have been repeatedly validated, these symptoms differ from the symptoms of insomnia as defined by authoritative medical standards, and their causes are influenced by diverse and individual factors. Sleep studies on patients with multiple comorbidities face challenges in variable control, highlighting the need for refined research designs and control strategies in future studies, particularly to determine how to isolate the effects of comorbidities on sleep during interventions to enhance the scientific rigor and reliability of research results.
4.2.4 Mechanisms and efficacy in non-pathological health conditions require further exploration
Some studies in this review specifically focused on healthy individuals, exploring the sleep-promoting effects of music under non-pathological conditions. Results indicated that music positively influenced subjective sleep experience, reduced sleep onset latency, and improved daytime nap quality in healthy individuals (59, 60). Although MT has been widely applied among populations with sleep disorders, its mechanisms and efficacy in healthy individuals without sleep disorders remain underexplored (15, 16). Emotional regulation through music may be a key pathway for enhancing sleep quality in healthy individuals (16, 63). Stress and negative emotions from daily life can influence sleep onset speed and depth (60, 63). Music can effectively reduce sympathetic nervous system activity, helping listeners enter a relaxed state (17, 37). In studies with healthy populations, specific types of music have been shown to promote higher quality sleep by modulating brainwave activity (17, 60). When healthy individuals listen to calming music before bed (e.g., slow-tempo instrumental music) (4, 37), Sundanese music (60), or music with a frequency of 432 Hz (4, 17, 59), they commonly report shorter sleep onset latency, prolonged deep sleep stages, and higher subjective sleep quality. However, current research mainly focuses on music materials as variables in discussing improvements in sleep quality among non-pathological populations. Future studies should consider other influencing factors, such as psychological state, lifestyle, and environmental factors, to comprehensively reveal the mechanisms and long-term efficacy of non-pathological health interventions.
5 Conclusion
This study reviewed empirical research from the past 5 years on music therapy’s effects on sleep, providing theoretical support and directional recommendations for the application and development of music therapy. By analyzing 27 studies with different experimental paradigms, we found that music therapy significantly enhances subjective sleep quality, particularly through subjective perception pathways like emotional regulation and anxiety relief. However, the effects of music therapy on objective sleep metrics were inconsistent, suggesting that the mechanisms through which music improves sleep are complex and may involve substantial individual differences. Unlike traditional meta-analyses, this review expanded the evaluation dimensions and comprehensively assessed various research findings, offering a broader perspective on the complex mechanisms underlying music therapy.
Despite its promising potential for promoting sleep, future research on music therapy still faces several directional challenges and opportunities. First, in terms of sleep monitoring, it is essential to integrate subjective and objective sleep assessment methods to jointly reveal the physiological and psychological effects of music therapy. Additionally, the current selection of intervention materials for music therapy remains relatively limited; future studies should further explore more precise and personalized music materials to maximize therapeutic efficacy and reduce unnecessary adverse effects, such as the potential interference from Involuntary Musical Imagery (INMI). Furthermore, research on different age groups and populations (e.g., children, adolescents, healthy individuals, and patients with multiple comorbidities) is limited. Expanding studies to include these participant groups could help develop tailored music therapy programs that meet diverse needs.
In conclusion, the multiple effects of music therapy on improving sleep quality are preliminarily established, but further exploration of its mechanisms and applicability is necessary through more standardized, rigorous experimental designs and diversified evaluation dimensions. Future research should incorporate various intervention variables, including music materials, psychological state, lifestyle, and environmental factors, to provide more scientifically robust empirical support for the broader application of music therapy in sleep health.
6 Limitation
This review has several limitations that may affect the general applicability of its findings. On one hand, regarding literature selection, this study included only empirical research from the past 5 years. Although this time limitation ensures the timeliness of the included studies, it also results in a relatively small number of overall studies. While the selected studies cover a diverse range of participant groups, the limited number of studies may not fully represent the effects of music therapy on patients with various types of sleep disorders. Future research could consider expanding the timeframe to gain a more comprehensive perspective.
On the other hand, the ambiguous definitions of sleep disorders in the included studies, along with differences in research design and methodology, may also affect the integration of results. The types of music used, duration of trials, and evaluation metrics varied across studies, complicating the overall assessment of effectiveness. As theory progresses, future research could address this limitation by providing diverse insights on these aspects.
Author contributions
QG: Writing – original draft, Writing – review & editing, Methodology. ML: Writing – review & editing, Data curation, Supervision, Validation, Visualization. XW: Supervision, Validation, Writing – review & editing. XY: Writing – review & editing, Investigation. MinY: Data curation, Resources, Writing – review & editing. JL: Data curation, Investigation, Writing – review & editing. BW: Writing – review & editing, Data curation, Supervision, Validation, Methodology. DY: Supervision, Validation, Writing – review & editing. XR: Supervision, Validation, Writing – review & editing. MiaY: Investigation, Writing – review & editing. SL: Investigation, Writing – review & editing. NL: Resources, Writing – review & editing. JH: Data curation, Writing – review & editing. QX: Conceptualization, Writing – review & editing.
Funding
The authors declare financial support was received for the research, authorship, and/or publication of this article. The project was funded by the Hebei Provincial Social Science Fund Project under the title “A Study on the Model of Music Cognitive Science Empowering the Capital Elderly Care Industry” (Grant No. HB23YS029).
Acknowledgments
We thank the MUAI research team, Yanshan University, China for their invaluable help and support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Leong, RLF, and Chee, MWL. Understanding the need for sleep to improve cognition. Annu Rev Psychol. (2022) 74:27–57. doi: 10.2139/ssrn.4035172
2. Zhou, L, Kong, J, Li, X, and Ren, Q. Sex differences in the effects of sleep disorders on cognitive dysfunction. Neurosci Biobehav Rev. (2023) 146:105067. doi: 10.1016/j.neubiorev.2023.105067
3. Irish, LA, Kline, CE, Gunn, HE, Buysse, DJ, and Hall, MH. The role of sleep hygiene in promoting public health: a review of empirical evidence. Sleep Med Rev. (2015) 22:23–36. doi: 10.1016/j.smrv.2014.10.001
4. Kavurmaci, M, Dayapoğlu, N, and Tan, M. Effect of music therapy on sleep quality. Altern Ther Health Med. (2020) 26:22–6.
5. Scammell, TE, Arrigoni, E, and Lipton, JO. Neural circuitry of wakefulness and sleep. Neuron. (2017) 93:747–65. doi: 10.1016/j.neuron.2017.01.014
6. Banks, S, and Dinges, DF. Behavioral and physiological consequences of sleep restriction. J Clin Sleep Med. (2007) 3:519–28. doi: 10.5664/jcsm.26918
7. Medic, G, Wille, M, and Hemels, M. Short-and long-term health consequences of sleep disruption. Nat Sci Sleep. (2017) 9:151–61. doi: 10.2147/Nss.S134864
8. Hertenstein, E, Feige, B, Gmeiner, T, Kienzler, C, Spiegelhalder, K, Johann, A, et al. Insomnia as a predictor of mental disorders: a systematic review and meta-analysis. Sleep Med Rev. (2019) 43:96–105. doi: 10.1016/j.smrv.2018.10.006
9. Philip, P, Chaufton, C, Orriols, L, Lagarde, E, Amoros, E, Laumon, B, et al. Complaints of poor sleep and risk of traffic accidents: a population-based case-control study. PLoS One. (2014) 9:e114102. doi: 10.1371/journal.pone.0114102
10. Riemann, D, Krone, LB, Wulff, K, and Nissen, C. Sleep, insomnia, and depression. Neuropsychopharmacology. (2020) 45:74–89. doi: 10.1038/s41386-019-0411-y
11. Cox, RC, and Olatunji, BO. A systematic review of sleep disturbance in anxiety and related disorders. J Anxiety Disord. (2016) 37:104–29. doi: 10.1016/j.janxdis.2015.12.001
12. Alvaro, PK, Roberts, RM, and Harris, JK. A systematic review assessing Bidirectionality between sleep disturbances, anxiety, and depression. Sleep. (2013) 36:1059–68. doi: 10.5665/sleep.2810
13. Chellappa, SL, and Aeschbach, D. Sleep and anxiety: from mechanisms to interventions. Sleep Med Rev. (2022) 61:101583. doi: 10.1016/j.smrv.2021.101583
14. Tang, H, Chen, L, Wang, Y, Zhang, Y, Yang, N, and Yang, N. The efficacy of music therapy to relieve pain, anxiety, and promote sleep quality, in patients with small cell lung cancer receiving platinum-based chemotherapy. Support Care Cancer. (2021) 29:7299–306. doi: 10.1007/s00520-021-06152-6
15. Bompard, S, Liuzzi, T, Staccioli, S, D’Arienzo, F, Khosravi, S, Giuliani, R, et al. Home-based music therapy for children with developmental disorders during the Covid-19 pandemic. J Telemed Telecare. (2023) 29:211–6. doi: 10.1177/1357633X20981213
16. Cordi, MJ, Ackermann, S, and Rasch, B. Effects of relaxing music on healthy sleep. Sci Rep. (2019) 9:9079. doi: 10.1038/s41598-019-45608-y
17. Litwic-Kaminska, K, Kotyśko, M, Pracki, T, Wiłkość-Dębczyńska, M, and Stankiewicz, B. The effect of autogenic training in a form of audio recording on sleep quality and physiological stress reactions of university athletes—pilot study. Int J Environ Res Public Health. (2022) 19:16043. doi: 10.3390/ijerph192316043
18. Harmat, L, Takács, J, and Bódizs, R. Music improves sleep quality in students. J Adv Nurs. (2008) 62:327–35. doi: 10.1111/j.1365-2648.2008.04602.x
19. Chang, ET, Lai, HL, Chen, PW, Hsieh, YM, and Lee, LH. The effects of music on the sleep quality of adults with chronic insomnia using evidence from polysomnographic and self-reported analysis: a randomized control trial. Int J Nurs Stud. (2012) 49:921–30. doi: 10.1016/j.ijnurstu.2012.02.019
20. Lai, HL, and Good, M. Music improves sleep quality in older adults. J Adv Nurs. (2005) 49:234–44. doi: 10.1111/j.1365-2648.2004.03281.x
21. Pan, BY. The use of music therapy/music to address sleep quality and sleep disorders: a systematic literature review. Montreal: Concordia University (2017).
22. Sheibani, N, Zakerian, SA, Alimohammadi, I, Azam, K, and Pirposhteh, EA. The effect of listening to Iranian pop and classical music, on mental and physiological drowsiness. Sleep Biol Rhythms. (2022) 20:275–85. doi: 10.1007/s41105-021-00369-y
23. Lee, M, Lee, HJ, Ahn, J, Hong, JK, and Yoon, IY. Comparison of autonomous sensory meridian response and binaural auditory beats effects on stress reduction: a pilot study. Sci Rep. (2022) 12:1–8. doi: 10.1038/s41598-022-24120-w
24. Wang, X, Yin, X, Liu, P, Wang, A, Mu, W, Xu, J, et al. The effect of Baduanjin qigong combined with five-elements music on anxiety and quality of sleep in asymptomatic patients with Covid-19 infection: a randomised controlled trial. Heliyon. (2023) 9:e18962. doi: 10.1016/j.heliyon.2023.e18962
25. Jespersen, KV, Otto, M, Kringelbach, M, van Someren, E, and Vuust, P. A randomized controlled trial of bedtime music for insomnia disorder. J Sleep Res. (2019) 28:e12817. doi: 10.1111/jsr.12817
26. Shum, A, Taylor, BJ, Thayala, J, and Chan, MF. The effects of sedative music on sleep quality of older community-dwelling adults in Singapore. Complement Ther Med. (2014) 22:49–56. doi: 10.1016/j.ctim.2013.11.003
27. Liao, J, Yang, YF, Cohen, L, Zhao, YC, and Xu, Y. Effects of Chinese medicine five-element music on the quality of life for advanced cancer patients: a randomized controlled trial. Chin J Integr Med. (2013) 19:736–40. doi: 10.1007/s11655-013-1593-5
28. Ryu, M, Park, JS, and Park, H. Effect of sleep-inducing music on sleep in persons with percutaneous transluminal coronary angiography in the cardiac care unit. J Clin Nurs. (2012) 21:728–35. doi: 10.1111/j.1365-2702.2011.03876.x
29. Chen, CK, Pei, YC, Chen, NH, Huang, LT, Chou, SW, Wu, KP, et al. Sedative music facilitates deep sleep in young adults. J Altern Complement Med. (2014) 20:312–7. doi: 10.1089/acm.2012.0050
30. Wang, Y, Duan, W, Dong, D, Ding, L, and Lei, X. A test-retest resting, and cognitive state EEG dataset during multiple subject-driven states. Sci Data. (2022) 9:566. doi: 10.1038/s41597-022-01607-9
31. Huang, J, Ren, L, Zhou, X, and Yan, K. An improved neural network based on Senet for sleep stage classification. IEEE J Biomed Health Inform. (2022) 26:4948–56. doi: 10.1109/Jbhi.2022.3157262
32. Lazic, SE, and Ogilvie, RD. Lack of efficacy of music to improve sleep: a polysomnographic and quantitative EEG analysis. Int J Psychophysiol. (2007) 63:232–9. doi: 10.1016/j.ijpsycho.2006.10.004
33. Koenig, J, Jarczok, MN, Warth, M, Harmat, L, Hesse, N, Jespersen, KV, et al. Music listening has no positive or negative effects on sleep quality of normal sleepers: results of a randomized controlled trial. Nord J Music Ther. (2013) 22:233–42. doi: 10.1080/08098131.2013.783095
34. Grant, MJ, and Booth, A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J. (2009) 26:91–108. doi: 10.1111/j.1471-1842.2009.00848.x
35. Mulrow, CD. The medical review article: state of the science. Ann Intern Med. (1987) 106:485. doi: 10.7326/0003-4819-106-3-485
36. Sifuentes-Ortega, R, Lenc, T, and Nozaradan, S. Partially preserved processing of musical rhythms in REM but not in NREM sleep. Cereb Cortex. (2022) 32:1508–19. doi: 10.1093/cercor/bhab303
37. Kuula, L, Halonen, R, Kajanto, K, Lipsanen, J, Makkonen, T, Peltonen, M, et al. The effects of Presleep slow breathing and music listening on polysomnographic sleep measures – a pilot trial. Sci Rep. (2020) 10:7427. doi: 10.1038/s41598-020-64218-7
38. Gao, D, Long, S, Yang, H, Cheng, Y, Guo, S, Yu, Y, et al. Sws brain-wave music may improve the quality of sleep: an EEG study. Front Neurosci. (2020) 14:67. doi: 10.3389/fnins.2020.00067
39. Lee, E, Bang, Y, Yoon, IY, and Choi, HY. Entrapment of binaural auditory beats in subjects with symptoms of insomnia. Brain Sci. (2022) 12:339. doi: 10.3390/brainsci12030339
40. Lu, MJ, Chen, WY, and Li, DJ. Efficacy of music therapy and predictors of sleep disturbance among patients with chronic schizophrenia: a prospective study. Arch Psychiatr Nurs. (2022) 40:1–7. doi: 10.1016/j.apnu.2022.04.001
41. Zhang, QL, Xu, N, Huang, ST, Lin, ZW, Chen, LW, Cao, H, et al. Music therapy for early postoperative pain, anxiety, and sleep in patients after mitral valve replacement. Thorac Cardiovasc Surg. (2020) 68:498–502. doi: 10.1055/s-0040-1713352
42. Kim, J, Choi, D, Yeo, MS, Yoo, GE, Kim, SJ, and Na, S. Effects of patient-directed interactive music therapy on sleep quality in postoperative elderly patients: a randomized-controlled trial. Nature and science of. Sleep. (2020) 12:791–800. doi: 10.2147/NSS.S286375
43. Burrai, F, Sanna, GD, Moccia, E, Morlando, F, Cosentino, ER, Bui, V, et al. Beneficial effects of listening to classical music in patients with heart failure: a randomized controlled trial. J Card Fail. (2020) 26:541–9. doi: 10.1016/j.cardfail.2019.12.005
44. Yildirim, M, and Yayan, EH. The effect of therapeutic touch and music rest on sleep parameters in children with liver transplantation. J Pediatr Nurs. (2023) 69:e65–72. doi: 10.1016/j.pedn.2022.12.008
45. Gao, C, Fillmore, P, and Scullin, MK. Classical music, educational learning, and slow wave sleep: a targeted memory reactivation experiment. Neurobiol Learn Mem. (2020) 171:107206. doi: 10.1016/j.nlm.2020.107206
46. Lee, M, Song, CB, Shin, GH, and Lee, SW. Possible effect of binaural beat combined with autonomous sensory Meridian response for inducing sleep. Front Hum Neurosci. (2019) 13:425. doi: 10.3389/fnhum.2019.00425
47. Ho, CMB, Jeong, H, Lim, YH, and Park, SJ. Effects of audio brain entrainment on Korean people with mild insomnia. Appl Psychophysiol Biofeedback. (2023) 48:207–16. doi: 10.1007/s10484-022-09570-2
48. Liu, H, Gao, X, and Hou, Y. Effects of mindfulness-based stress reduction combined with music therapy on pain, anxiety, and sleep quality in patients with osteosarcoma. Braz J Psychiatry. (2019) 41:540–5. doi: 10.1590/1516-4446-2018-0346
49. Giordano, V, Goeral, K, Schrage-Leitner, L, Berger, A, and Olischar, M. The effect of music on AEEG Cyclicity in preterm neonates. Children. (2021) 8:208. doi: 10.3390/children8030208
50. Uhlig, S, Groot, J, Jansen, E, and Scherder, E. Rap & Sing Music Therapy and sleep in adolescents: a single-blind cluster randomized controlled trial. Nord J Music Ther. (2019) 28:60–70. doi: 10.1080/08098131.2018.1542613
51. Snipes, S, Krugliakova, E, Meier, E, and Huber, R. The Theta paradox: 4-8 Hz EEG oscillations reflect both sleep pressure and cognitive control. J Neurosci. (2022) 42:8569–86. doi: 10.1523/Jneurosci.1063-22.2022
52. Krishna, R, Rajkumar, E, Romate, J, Allen, JG, and Monica, D. Effect of Carnatic raga-Bilahari based music therapy on anxiety, sleep disturbances and somatic symptoms among caregivers of cancer patients. Heliyon. (2022) 8:e10681. doi: 10.1016/j.heliyon.2022.e10681
53. Sateia, MJ. International classification of sleep disorders-third edition: highlights and modifications. Chest. (2014) 146:1387–94. doi: 10.1378/chest.14-0970
54. Lauer, CJ, and Krieg, JC. Slow-wave sleep and ventricular size: a comparative study in schizophrenia and major depression. Biol Psychiatry. (1998) 44:121–8. doi: 10.1016/S0006-3223(97)00342-9
55. Singareddy, RK, and Balon, R. Sleep and suicide in psychiatric patients. Ann Clin Psychiatry. (2001) 13:93–101. doi: 10.3109/10401230109148954
56. Beswick, AD, Wylde, V, Bertram, W, and Whale, K. The effectiveness of non-pharmacological sleep interventions for improving inpatient sleep in hospital: a systematic review and meta-analysis. Sleep Med. (2023) 107:243–67. doi: 10.1016/j.sleep.2023.05.004
57. Ekinci, M, and Gökalp, K. Effect of music therapy on anxiety and sleep quality of geriatric Haematological oncology patients. The Turkish. Turk J Geriatr. (2020) 23:546–54. doi: 10.31086/tjgeri.2020.193
58. Kabuk, A, Şendir, M, and Filinte, G. The effect of reflexology massage and passive music therapy intervention before burn dressing on pain, anxiety level and sleep quality. Burns. (2022) 48:1743–52. doi: 10.1016/j.burns.2021.10.012
59. Dubey, P, Kumar, Y, Singh, R, Jha, K, and Kumar, R. Effect of music of specific frequency upon the sleep architecture and electroencephalographic pattern of individuals with delayed sleep latency: a daytime nap study. J Family Med Prim Care. (2019) 8:3915. doi: 10.4103/jfmpc.jfmpc_575_19
60. Kusumandari, D E, Suhendra, M A, Rizqyawan, M I, et al. Effect of Sundanese music on daytime sleep quality based on EEG signal. The 4th biomedical Engineering’S recent Progress in biomaterials, drugs development, health, and medical devices: Proceedings of the international symposium of biomedical engineering (ISBE). AIP Publishing: Padang, Indonesia, (2019).
61. Ibáñez, V, Silva, J, and Cauli, O. A survey on sleep assessment methods. PeerJ. (2018) 6:e4849. doi: 10.7717/peerj.4849
62. Chan, MF, Chan, EA, and Mok, E. Effects of music on depression and sleep quality in elderly people: a randomised controlled trial. Complement Ther Med. (2010) 18:150–9. doi: 10.1016/j.ctim.2010.02.004
63. Baglioni, C, Spiegelhalder, K, Lombardo, C, and Riemann, D. Sleep and emotions: a focus on insomnia. Sleep Med Rev. (2010) 14:227–38. doi: 10.1016/j.smrv.2009.10.007
64. Buysse, DJ, Reynolds, CF, Monk, TH, et al. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. (1989) 28:193–213. doi: 10.1016/0165-1781(89)90047-4
65. Ong, JC, Ulmer, CS, and Manber, R. Improving sleep with mindfulness and acceptance: a metacognitive model of insomnia. Behav Res Ther. (2012) 50:651–60. doi: 10.1016/j.brat.2012.08.001
66. Yamasato, A, Kondo, M, Hoshino, S, Kikuchi, J, Okino, S, and Yamamoto, K. Characteristics of music to improve the quality of sleep. Music Med. (2019) 11:195. doi: 10.47513/mmd.v11i3.643
67. Lee, CH, Lai, CL, Sung, YH, Lai, MY, Lin, CY, and Lin, LY. Comparing effects between music intervention and aromatherapy on anxiety of patients undergoing mechanical ventilation in the intensive care unit: a randomized controlled trial. Qual Life Res. (2017) 26:1819–29. doi: 10.1007/s11136-017-1525-5
68. Ellis, RJ, Koenig, J, and Thayer, JF. Getting to the heart: autonomic nervous system function in the context of evidence-based music therapy. Music Med. (2012) 4:90–9. doi: 10.1177/1943862112437766
69. Jakubowski, K, Finkel, S, Stewart, L, and Müllensiefen, D. Dissecting an earworm: melodic features and song popularity predict involuntary musical imagery. Psychol Aesthet Creat Arts. (2017) 11:122–35. doi: 10.1037/aca0000090
70. Beaman, CP, and Williams, TI. Earworms (stuck song syndrome): towards a natural history of intrusive thoughts. Br J Psychol. (2010) 101:637–53. doi: 10.1348/000712609X479636
71. Halpern, AR, and Bartlett, JC. The persistence of musical memories: a descriptive study of earworms. Music Percept. (2011) 28:425–32. doi: 10.1525/mp.2011.28.4.425
72. Hyman, IE, Burland, NK, Duskin, HM, et al. Going Gaga: investigating, creating, and manipulating the Song stuck in my head. Appl Cogn Psychol. (2013) 27:204–15. doi: 10.1002/acp.2897
73. Morin, CM. Chronic insomnia: recent advances and innovations in treatment developments and dissemination. Can Psychol. (2010) 51:31–9. doi: 10.1037/a0018715
74. Baglioni, C, Battagliese, G, Feige, B, Spiegelhalder, K, Nissen, C, Voderholzer, U, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. (2011) 135:10–9. doi: 10.1016/j.jad.2011.01.011
75. Trahan, T, Durrant, SJ, Müllensiefen, D, and Williamson, VJ. The music that helps people sleep and the reasons they believe it works: a mixed methods analysis of online survey reports. PLoS One. (2018) 13:e0206531. doi: 10.1371/journal.pone.0206531
76. Bastien, CH, St-Jean, G, Morin, CM, et al. Chronic psychophysiological insomnia: Hyperarousal and/or inhibition deficits? An ERPs investigation. Sleep. (2018) 31:887–98. doi: 10.1093/sleep/31.6.887
77. Asif, A, Majid, M, and Anwar, SM. Human stress classification using EEG signals in response to music tracks. Comput Biol Med. (2019) 107:182–96. doi: 10.1016/j.compbiomed.2019.02.015
78. Chee, ZJ, Chang, CYM, Cheong, JY, Malek, FHBA, Hussain, S, de Vries, M, et al. The effects of music and auditory stimulation on autonomic arousal, cognition and attention: a systematic review. Int J Psychophysiol. (2024) 199:112328. doi: 10.1016/j.ijpsycho.2024.112328
79. Putkinen, V, Nazari-Farsani, S, Seppälä, K, Karjalainen, T, Sun, L, Karlsson, HK, et al. Decoding music-evoked emotions in the auditory and motor cortex. Cereb Cortex. (2021) 31:2549–60. doi: 10.1093/cercor/bhaa373
80. Dickson, GT, and Schubert, E. How does music aid sleep? Literature review. Sleep Med. (2019) 63:142–50. doi: 10.1016/j.sleep.2019.05.016
81. Hermans, LWA, Leufkens, TR, Van Gilst, MM, et al. Sleep EEG characteristics associated with sleep onset misperception. Sleep Med. (2019) 57:70–9. doi: 10.1016/j.sleep.2019.01.031
82. Trimmel, K, Eder, HG, Böck, M, Stefanic-Kejik, A, Klösch, G, and Seidel, S. The (mis) perception of sleep: factors influencing the discrepancy between self-reported and objective sleep parameters. J Clin Sleep Med. (2021) 17:917–24. doi: 10.5664/jcsm.9086
83. Mai, E. Insomnia: Prevalence, impact, pathogenesis, differential diagnosis, and evaluation. Psychiatr Clin North Am. (2009) 7:491–8. doi: 10.1176/foc.7.4.foc491
84. Morin, C, Leblanc, M, Daley, M, et al. Epidemiology of insomnia: prevalence, self-help treatments, consultations, and determinants of help-seeking behaviors. Sleep Med. (2006) 7:123–30. doi: 10.1016/j.sleep.2005.08.008
85. Roth, T, Jaeger, S, Jin, R, Kalsekar, A, Stang, PE, and Kessler, RC. Sleep problems, comorbid mental disorders, and role functioning in the National Comorbidity Survey Replication. Biol Psychiatry. (2006) 60:1364–71. doi: 10.1016/j.biopsych.2006.05.039
86. Ohayon, MM, and Reynolds, CF. Epidemiological and clinical relevance of insomnia diagnosis algorithms according to the Dsm-iv and the international classification of sleep disorders (ICSD). Sleep Med. (2009) 10:952–60. doi: 10.1016/j.sleep.2009.07.008
87. Leblanc, M, Mérette, C, Savard, J, et al. Incidence and risk factors of insomnia in a population-based sample. Sleep. (2018) 32:1027–37. doi: 10.1093/sleep/32.8.1027
88. Jarrin, DC, Chen, IY, Ivers, H, and Morin, CM. The role of vulnerability in stress-related insomnia, social support and coping styles on incidence and persistence of insomnia. J Sleep Res. (2014) 23:681–8. doi: 10.1111/jsr.12172
89. Jansson-Fröjmark, M, and Lindblom, K. A bidirectional relationship between anxiety and depression, and insomnia? A prospective study in the general population. J Psychosom Res. (2008) 64:443–9. doi: 10.1016/j.jpsychores.2007.10.016
Keywords: sleep, sleep disorders, music therapy, insomnia, meta-narrative review
Citation: Gou Q, Li M, Wang X, Yuan X, Yang M, Li J, Wang B, Yang D, Ren X, Yang M, Liu S, Liu N, Han J and Xu Q (2025) Meta-narrative review: the impact of music therapy on sleep and future research directions. Front. Neurol. 15:1433592. doi: 10.3389/fneur.2024.1433592
Edited by:
Jun Lu, First Affiliated Hospital of Jilin University, ChinaReviewed by:
Weijun Li, Liaoning Normal University, ChinaYinghua He, FR Acupuncture & Chinese Medicine Clinic, United States
Xuexing Luo, Macau University of Science and Technology, Macao SAR, China
Copyright © 2025 Gou, Li, Wang, Yuan, Yang, Li, Wang, Yang, Ren, Yang, Liu, Liu, Han and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qiujian Xu, eHVxaXVqaWFuQHlzdS5lZHUuY24=
†These authors have contributed equally to this work
 Qiaoqiao Gou
Qiaoqiao Gou Meihui Li2†
Meihui Li2† Xiaoyu Wang
Xiaoyu Wang Xinran Yuan
Xinran Yuan Mingyi Yang
Mingyi Yang Junrui Li
Junrui Li Dan Yang
Dan Yang Xiubo Ren
Xiubo Ren Miaomiao Yang
Miaomiao Yang Siqi Liu
Siqi Liu Ningning Liu
Ningning Liu Jiaqi Han
Jiaqi Han Qiujian Xu
Qiujian Xu