
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol. , 26 June 2024
Sec. Experimental Therapeutics
Volume 15 - 2024 | https://doi.org/10.3389/fneur.2024.1408360
Objective: This study aimed to evaluate the efficacy and safety of buccal acupuncture on postoperative analgesia, perioperative stress response and adverse events in elderly patients undergoing laparoscopic radical gastrectomy.
Methods: It was a prospective, outcome assessor-blinded, randomized controlled trial, involving 90 patients aged 65–80 years who were treated with an elective laparoscopic radical gastrectomy. They were randomly assigned to buccal acupuncture group (Group B) and control group (Group C). Buccal acupuncture was applied to patients of Group B before the induction of general anesthesia, while no additional application was given to those in Group C. Patient-controlled intravenous analgesia (PCIA) with sufentanil was postoperatively performed in both groups. Sufentanil consumption and the Visual Analog Scale (VAS) score within 48 h postoperatively were assessed as primary outcomes. Secondary outcomes included peripheral levels of stress markers, intraoperative consumptions of anesthetic drugs and postoperative recovery.
Results: Patients in Group B presented significantly lower VAS scores within 24 h and less consumption of sufentanil within 48 h postoperatively (both p < 0.01). The awaking time, time to extubation and length of stay were significantly shorter in Group B than in Group C (p = 0.005, 0.001 and 0.028, respectively). Compared with Group C, stress response and inflammatory response within 24 h postoperatively were also significantly milder in Group B.
Conclusion: The use of buccal acupuncture before general anesthesia induction favors the postoperative analgesic effect and recovery in elderly patients undergoing laparoscopic radical gastrectomy, the mechanism of which involves relieving postoperative stress response and inflammatory response.
Clinical trial registration: This study was registered in the Chinese Clinical Trial Registry (www.chictr.org.cn) on 15/06/2023 (ChiCTR2300072500).
Laparoscopic radical gastrectomy is an effective minimally invasive procedure for the treatment of gastric cancer, but may cause moderate-to-severe abdominal wall pain and visceral pain that negatively affects postoperative rehabilitation (1). Appropriate postoperative pain management was beneficial for the patients’ recovery (2, 3). Patient-controlled intravenous analgesia (PCIA) with opioids was usually given to manage this postoperative pain (4). However, adverse events of PCIA like nausea, vomiting, lethargy, respiratory depression, skin pruritus and gastrointestinal dysfunction should be concerned (5). Kim et al. (6) showed that the combined use of non-steroidal anti-inflammatory drugs (NSAIDs) in patients treated with laparoscopic radical gastrectomy achieved an acceptable postoperative analgesia and a reduced consumption of postoperative opioids, but increased incidences of anastomotic leakage, duodenal stump leakage and intra-abdominal bleeding. Before anesthesia, rectus abdominis or rectus abdominis plane block combined with PCIA provides an effective postoperative analgesia for patients treated with laparoscopic radical gastrectomy (7, 8). However, nerve blocks have disadvantages of block failure, wrong-site blocks, nerve injury and local anesthetic poisoning. Postoperative epidural analgesia offers the same analgesic effect as PCIA on patients undergoing laparoscopic radical gastrectomy, whereas the former significantly increases the incidence of postoperative hypotension and urinary storage (9, 10). An effective and safe postoperative analgesia regimen is urgently needed for patients undergoing laparoscopic radical gastrectomy.
Postoperative pain, a type of inflammatory pain, is caused by peripheral tissue damage involving central and peripheral sensitization mechanisms (11, 12). Habibi et al. (13) and Ezzatvar et al. (14) indicated that central sensitization is the main cause of prolonged pain and poor analgesic effect. Perioperative acupuncture was reported to achieve the postoperative analgesic effect with less consumptions of analgesic drugs, by blocking harmful stimuli, reducing peripheral and central sensitization and inhibiting neuroplasticity (15). Acupuncture is a traditional Chinese medicine (TCM) technique with the recognized function in relieving pain (16, 17). The TCM theory believes that a congenital holographic system on the cheek is a continuous projection of the human body (Figure 1A) (18). Based on this, buccal acupuncture, as an emerging pain-free acupuncture therapy, stimulates 16 specific acupoints on the cheek to treat physical and mental diseases, including the chronic pain (Figure 1B). A growing body of evidence has supported the regulatory effects of buccal acupuncture on postoperative analgesia and viscera function with a high safety (19, 20). The present study explored the influence of buccal acupuncture before general anesthesia induction on postoperative analgesia and perioperative stress response in elderly patients undergoing laparoscopic radical gastrectomy and the underlying mechanism.
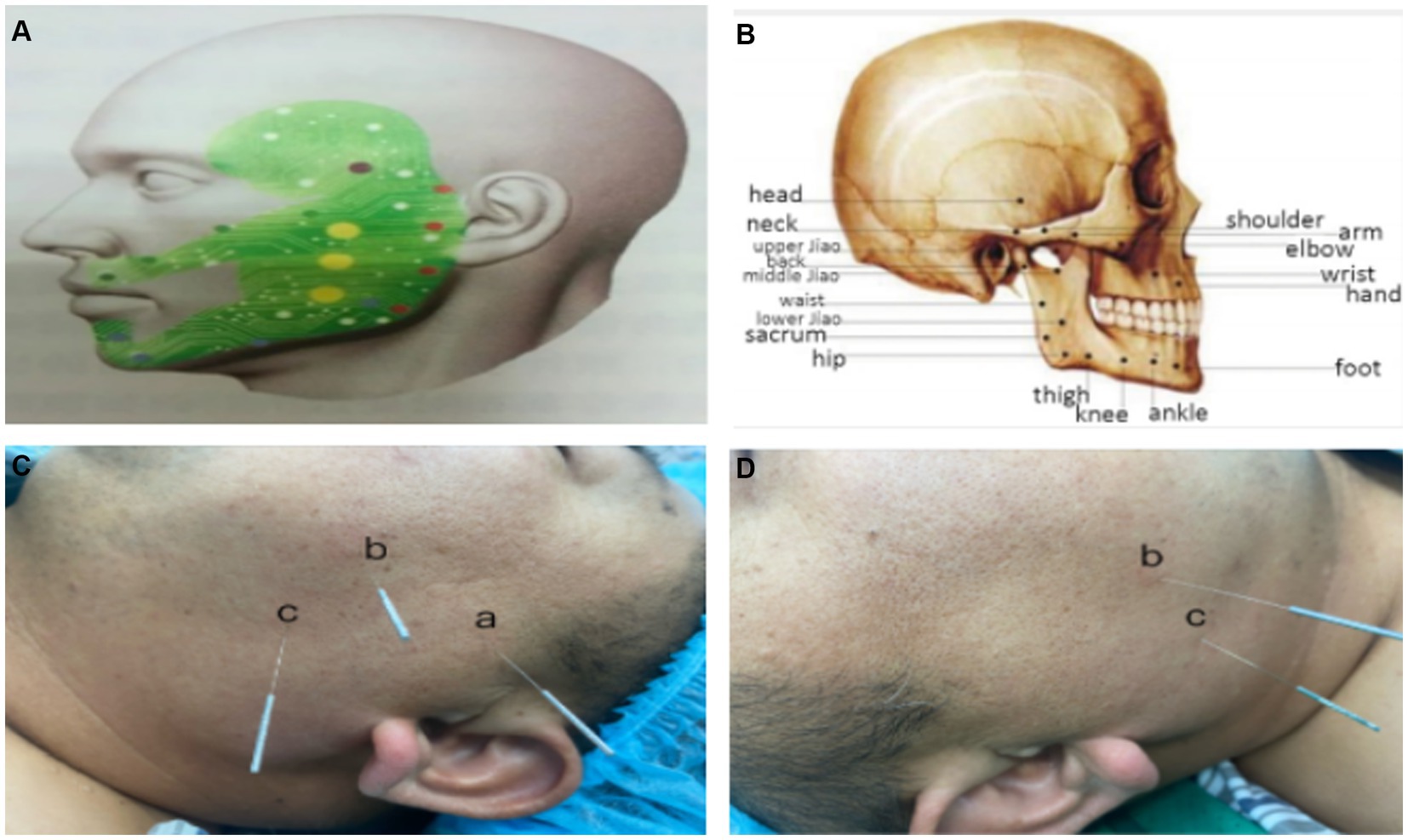
Figure 1. Buccal acupuncture and acupoints. (A,B) A biological holographic model of buccal acupuncture (A) (18), and acupoints on the cheek (B) (19). (C,D) Buccal acupoints of a (Shoulder point), b (Middle Jiao point), c (Lower Jiao point) on the left cheek (C), and b (Middle Jiao point), c (Lower Jiao point) on the right cheek (D). Acupoint a is situated on the midpoint of temporozygomatic suture for relieving the left shoulder pain; b is situated on the midpoint of Upper Jiao (the cross of the posterior coronoid of the mandible and the lower edge of the zygomatic arch) and Lower Jiao (anterior oblique line of the mandible); c is situated on the anterior oblique line of the mandible.
It was a prospective, outcome assessor-blinded, single-arm, randomized controlled trial (RCT) conducted by the Department of Anesthesiology in the Affiliated Jiangning Hospital of Nanjing Medical University, following the Consolidated Standards of Reporting Trials (CONSORT) statement (21). Ethical approval for this study (2023-03-019-K01) was provided by the Institutional Ethics Committee of the Affiliated Jiangning Hospital of Nanjing Medical University. This study was registered in the Chinese Clinical Trial Registry on 15/06/2023 (CTRI registration number—ChiCTR2300072500). Written informed consent was provided by all participants. Surgical procedures and follow-up within 48 h were performed by the same group of surgeons and a nurse anesthetist who were blinded to group allocation.
Ninety patients with an age of 65–80 years, body mass index (BMI) of 22–28 kg/m2, and the American society of Anesthesiologists (ASA) physical status of Class II – III who were treated with an elective laparoscopic radical gastrectomy were enrolled. Exclusion criteria: (1) cardiac, hepatic, pulmonary or renal insufficiency; (2) diabetes mellitus, neurological diseases, blood disorders or immune system disorders; (3) mental illnesses, hearing or language disorders; (4) medical history of chronic pain, history of psychotropic or analgesic medication, drug use or alcohol dependence; (5) acute head and facial injuries, soft tissue diseases, or infection; (6) suspected intubation difficulty with the Mallampati Scoring of Class II and above (22); (7) coagulation abnormalities or long-term use of anticoagulants; (8) intraoperative falling of the acupuncture needle; (9) intraoperative conversion to transabdominal surgery; (10) intraoperative bleeding greater than 500 mL or operative time longer than 5 h; (11) postoperative awaking time longer than 2 h or transferred to intensive care unit (ICU); (12) unusually sensitive to the pain or using tramadol for rescue analgesia more than 3 times.
Based on our pre-experiment with 10 participants per group, the mean consumption of sufentanil within 48 h postoperatively could be reduced to 9 μg (12%) in Group B. Assuming a 10% dropout rate at a power value of 80% and an α of 0.05, the sample size of at least 45 per group was needed. In the present study, 60 cases for each group were designed. A CONSORT flow diagram of participant enrollment was displayed in Figure 2.
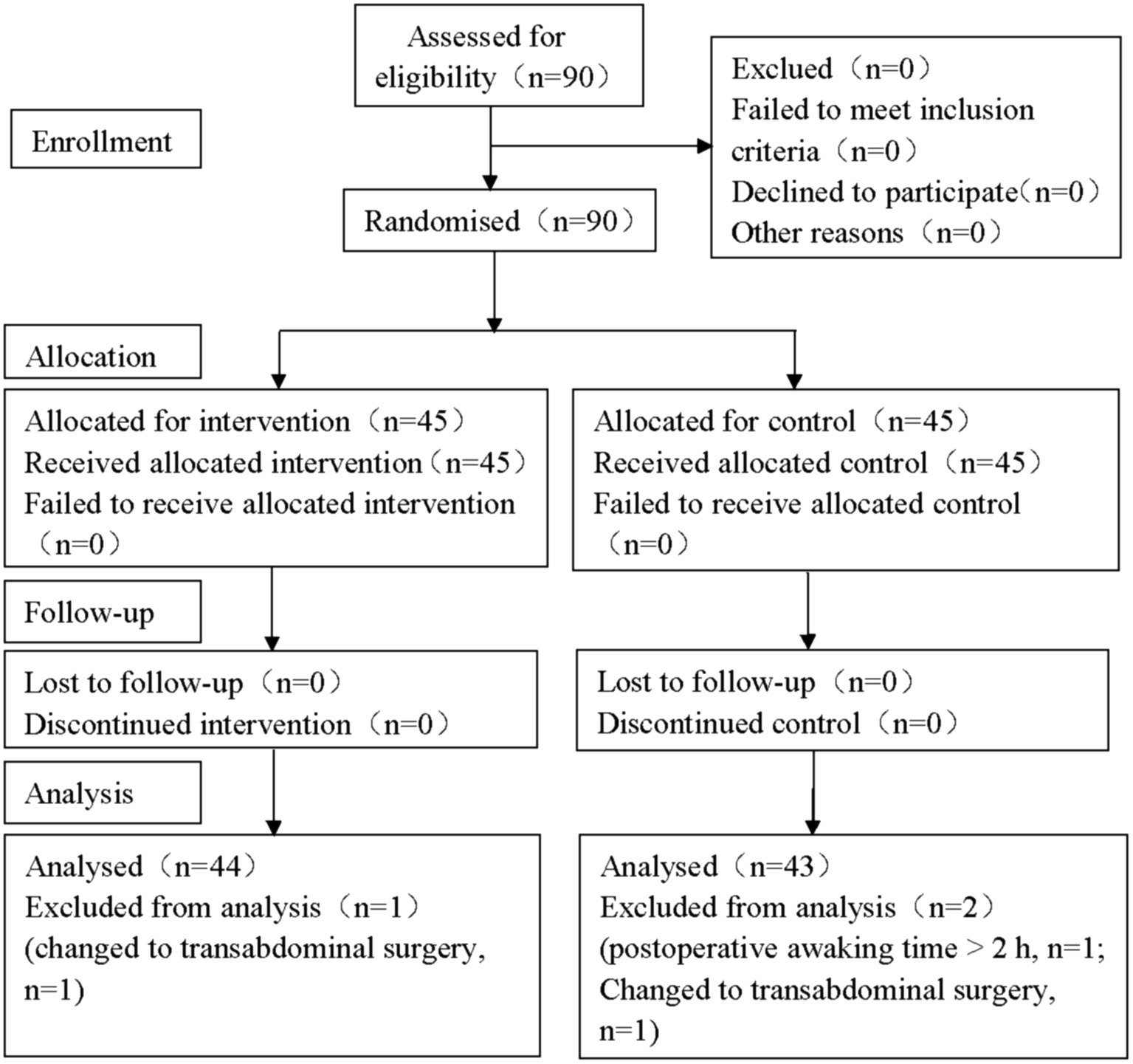
Figure 2. CONSORT flow diagram of participant enrollment. In the study, a total of 90 participants were initially screened and 3 of them were excluded during the trial. Finally, there were 87 participants included in the statistical analysis (43 in Group C and 44 in Group B, respectively). CONSORT: The Consolidated Standards of Reporting Trials.
Patients were randomly divided into two groups using a random table generated by SPSS 26.0. Ninety sealed envelopes were prepared by a statistician who did not participate in the study. To ensured that the assessor was not aware of the patients’ grouping, all patients’ head and face were covered with a disposable sterile medium and fixed using an anesthesia head frame. To assure concealment of allocation, the random number was kept in sealed and opaque envelopes, and opened up by an anesthesiologist who was not involved in this study.
Patients in Group B were intervened by buccal acupuncture before general anesthesia induction by the same chief physician. After routine facial disinfection, five buccal acupuncture needles (Gauge 02, 0.18 mm × 30 mm, Maanshan Bond Medical Instruments Co., Ltd., China) were inserted to 5–15 mm depth for 30 min through five acupoints of the left shoulder point and bilateral points of Middle Jiao and Lower Jiao (Figures 1C, D) (23). No interventions were performed in Group C.
Preoperative fasting involved at least 12 h for food and 6 h for fluids. After entering the operating room, patients were managed by the peripheral intravenous placement and monitoring of electrocardiogram (ECG), heart beat (HR), pulse oxygen saturation (SpO2), end-tidal carbon dioxide partial pressure (PETCO2) and bispectral index (BIS). Radial artery puncture and catheterization were performed under local anesthesia to monitor the invasive arterial blood pressure (IBP). After 5-min oxygen delivery at 8 L/min by an oxygen mask, general anesthesia induction was performed using midazolam (0.05 mg/kg), etomidate (0.15 mg/kg), cisatracurium (0.2 mg/mg) and sufentanil (0.4 μg/kg). Mechanical ventilation via tracheal cannula was implemented, with the mode of intermittent positive-pressure ventilation (IPPV), tidal volume (VT) of 8 mL/kg, respiratory rate (RR) of 14 times/min, ratio of the duration of inspiratory and expiratory phases (I:E ratio) of 1:2, inhaled oxygen concentration of 60% and intraoperative PETCO2 of 35–45 mmHg. Anesthesia was maintained by intraoperative venous pumping of propofol (3–6 mg/kg/h), remifentanil (0.1–0.3 μg/kg/min) and cisatracurium (0.1–0.2 mg/kg/h), with BIS value of 45–60. Uradil (12.5 mg/time), neo-synephrine (100 μg/time), esmolol (30 mg/time) and atropine (0.25 mg/time) were given in cases of intraoperative hypertension (20% increase in the mean arterial blood pressure (MAP) or SBP > 160 mmHg), hypotension (20% decrease in MAP than baseline or SBP < 90 mmHg), tachycardia and bradycardia (HR <50 beats/min), respectively. The infusion of cisatracurium was terminated 30 min before surgery, and that of propofol and remifentanil was stopped at the last stitch of skin suture. The PCIA pump was connected with the intravenous line for 150 mL of normal saline containing sufentanil (2.0 μg/kg) and palosetron (0.25 mg), 5 mL of load volume, 2 mL/h of background dose and 1 mL of bolus dose. Tramadol (1 mg/kg) was additionally given to patients with a poor anesthetic effect of PCIA [postoperative Visual Analogue Scale (VAS) score > 3 points]. All patients were postoperatively transferred to postanesthesia care unit (PACU) for recovery. The tracheal catheter was extubated until the recovery of the consciousness, muscle strength, swallowing reflex and spontaneous breathing, VT > 5 mL/kg and RR > 12 times/min. Patients with the Steward score of 4 points and above were transferred to the ward (24).
The primary outcomes included sufentanil consumption within 48 h postoperatively and the VAS scores at 2 h (T1), 6 h (T2), 24 h (T3) and 48 h (T4) postoperatively.
The secondary outcomes included: (1) intraoperative consumptions of propofol, remifentanil and vasoactive drugs; (2) postoperative awakening time, time to extubation and length of stay; (3) number of presses of the PCIA device, number of effective presses and case number of rescue analgesia within 48 h postoperatively; (4) peripheral levels of blood glucose (BG), adrenaline (E), noradrenaline (NE), C-reactive protein (CRP), Cortisol (Cor), interleukin-6 (IL-6) and interleukin-10 (IL-10) before general anesthesia induction (T0) and at T1, T2, T3 and T4; (5) adverse events like postoperative nausea and vomiting (PONV), drowsiness, respiratory depression (SpO2 < 90%) and skin pruritus within 48 h postoperatively.
Data analysis was performed by the SPSS 26.0 (SPSS Inc., Chicago, IL, United States). Continuous variables were tested for normality, and those meeting the normal distribution were presented as mean ± standard deviation (SD). Differences between the two groups were analyzed by the independent samples t-test. Categorical variables were presented as numbers (%), and differences between groups were analyzed by the Chi-square or Fisher’s exact test. A statistically significant difference was considered with the p < 0.05.
A total of 90 participants were initially screened. After excluding 2 cases in Group C (one case of longer than 2 h of postoperative awaking, and one of intraoperative conversion to transabdominal surgery) and 1 case in Group B (intraoperative conversion to transabdominal surgery), 43 cases in Group C and 44 in Group B were finally enrolled in our study (Figure 2).
There were no significant differences in baseline characteristics between Group B and Group C, including sex, age, body mass index (BMI), ASA classification, operative time, intraoperative bleeding and intraoperative infusion volume (all p > 0.05, Table 1).
Compared with those of Group C, intraoperative consumptions of propofol, remifentanil, neo-synephrine, urapidil, esmolol and atropine were significantly lower in Group B (p < 0.05, Table 2).
Compared with those of Group C, patients in Group B were graded with significantly lower VAS scores at T1, T2 and T3 (p < 0.05), but shared similar VAS scores at T4 (p > 0.05, Table 3).
The number of presses of the PCIA device, number of effective presses and case number of rescue analgesia within 48 h postoperatively were significantly lower in Group B than in Group C (p < 0.05, Table 4). Moreover, sufentanil was significantly less consumed in Group B (p < 0.01, Table 4).
At T1, T2 and T3, significantly lower peripheral levels of BG, E, NE, CRP, Cor and IL-6, and higher IL-10 level were detected in Group B compared with those of Group C (p < 0.01, Table 5). However, no significant differences in them were detected at T0 and T4 between groups (p > 0.05).
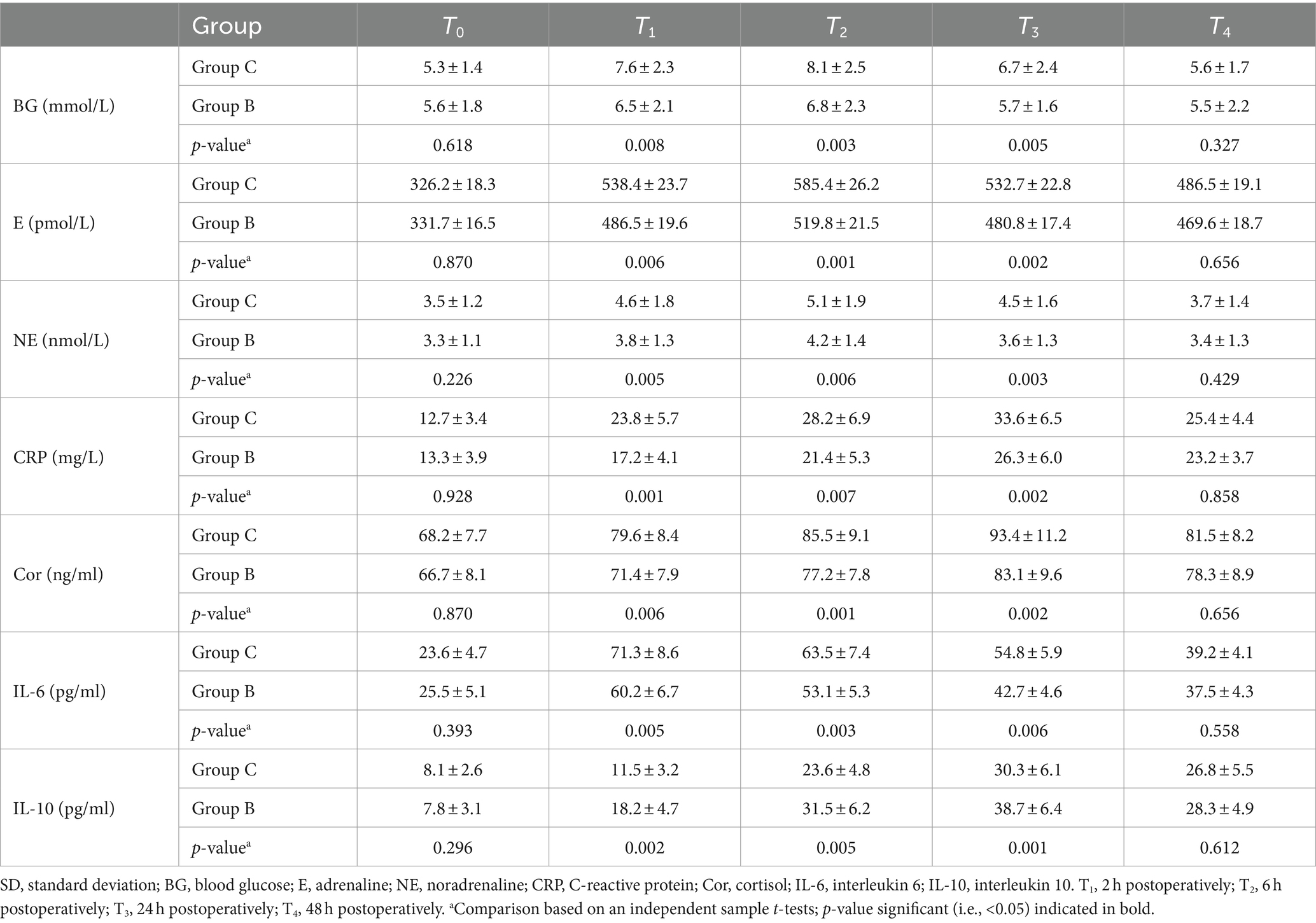
Table 5. Postoperative blood testing in Group C (n = 43) and Group B (n = 44) postoperatively (mean ± SD).
Significantly shorter postoperative awakening time, time to extubation and length of stay in Group B than those of Group C were detected (p < 0.05, Table 6). The incidence of PONV within 48 h postoperatively was significantly lower in Group B than in Group C (p < 0.01), while those of drowsiness, respiratory depression and skin pruritus were similar (p > 0.05; Table 6).
Buccal acupuncture is a new type of microneedling created by Wang Yongzhou (23), abiding by the theory that the physiology of the human body can be projected onto a holographic acupoint system visualized on the cheek. In a clinical trial involving 630 patients with limb pain and 100 patients with visceral pain, buccal acupuncture was validated for its rapid, reliable and systemic therapeutic efficacy. Moreover, various races can benefit from buccal acupuncture (18). In the present study, we proved that the use of buccal acupuncture before general anesthesia induction significantly reduced the consumption of intraoperative anesthetic drugs and postoperative analgesic drugs, and alleviated perioperative stress response and inflammatory response in elderly patients undergoing laparoscopic radical gastrectomy.
The 6th–10th thoracic vertebrae (T6–T10) provide the sensory innervation of the stomach, causing abdominal wall and visceral pain after surgery (25). Appropriate postoperative analgesia methods were conducive to patients’ recovery (2, 3). The traditional Chinese medicine (TCM) theory believed that the liver, gallbladder, spleen and stomach are harbored in the Middle Jiao, and the lower abdomen and urogenital reproduction in the Lower Jiao. Yi et al. (20) showed that the aging curve of the analgesic effect of buccal acupuncture was inherent and specific, and did not change with the number of treatments. In addition, they reported an obvious analgesic effect of buccal acupuncture starting at 5 min and peaking at 30 min. The analgesic effect of buccal acupuncture manifested as a temporal change with the rapid onset of analgesia, and increased in pain threshold and stability without being influenced by multiple times of acupunctures. We performed buccal acupuncture on the acupoints of the left shoulder point, bilateral acupoints of Middle Jiao and Lower Jiao for 30 min before general anesthesia induction in patients treated with laparoscopic radical gastrectomy. Consistent with previous data, the VAS scores within 24 h postoperatively were significantly lower in patients treated with buccal acupuncture than those of controls (17).
Surgical procedures of laparoscopic radical gastrectomy, anesthesia stimulation, establishment of CO2 pneumoperitoneum and hypercapnia resulted in perioperative stress response, intraoperative hemodynamic fluctuations and postoperative pain (11, 12). Kurni et al. (26) verified that stress-related indicators like plasma Cor level are positively correlated with the intensity and duration of stimuli. The use of buccal acupuncture before general anesthesia induction significantly lowered peripheral levels of BP, E, NE, Cor and CRP within 24 h postoperatively, indicating the relieved postoperative stress response. Surgical trauma aggravated postoperative pain and inflammatory response by releasing inflammatory mediators, which could be alleviated by an effective preoperative regional anesthesia to inhibit the transmission of trauma and pain stimulation to the advanced center (14, 27). IL-6 is the earliest released and highly sensitive proinflammatory factor, closely related to the severity of surgical trauma, body immune status and prognosis (28). IL-10, as an inflammatory suppressor, inhibits nuclear factor activity and promotes neutrophil apoptosis (29). In this study, decreased IL-6 and increased IL-10 levels within 24 h postoperative in Group B suggested the role of buccal acupuncture in balancing the pro- and anti-inflammatory signals.
The regulatory effect of buccal acupuncture on inflammatory response is probably attributed to the blockage of pain signal to the central nervous system (15). Wang et al. (17) demonstrated the synergistic analgesic effect of acupuncture by relieving oxidative stress and inflammatory response, with the direct or indirect involvement of the nervous and humoral system. In a white rabbit model of rheumatoid arthritis (30), buccal acupuncture effectively relieved the pain by affecting the release of β-endorphin (β-EP) and cholecystokinin octapeptide (CCK-8) in cerebrospinal fluid. β-EP produces the analgesic effect by blocking pain signals via sensitizing the endogenous opioid peptide (EOP) receptors in neuronal terminals, or activating receptors with gray matter distribution around the brainstem aqueduct (31, 32). CCK-8 is a strong endogenous anti-opioid peptide with the central anti-opioid analgesic effect. It contributes to pain relief through reducing the total number of μ receptors, decreasing the affinity of κ receptors and inhibiting the binding force between opioid and receptors (33). Characterized by the analgesic time-effect, the use of buccal acupuncture in rabbits increased the content of 5-HT and decreases the ratio of NE/5-HT in the hypothalamus (30, 34).
The safety profile of buccal acupuncture was examined. There were no significant differences in the incidences of drowsiness, respiratory depression and skin pruritus between groups. The significantly lower incidence of PONV in Group B than in Group C could be explained by the greater consumption of postoperative analgesic drugs when PCIA was used alone (35). Additionally, blockage of Qi movement in the Middle Jiao caused gastrointestinal symptoms (36). We believed that buccal acupuncture on bilateral acupoints of the Middle Jiao effectively removed Qi stagnation and thus relieved PONV (37).
There were some limitations in this study. First of all, it was a prospective, outcome assessor-blinded RCT. We failed to find a suitable placebo in the control group to achieve double blinding. However, during the operation, all patients’ head and face were covered by a surgical scarf and head frame, so that the assessor was not aware of the patients’ grouping. Secondly, the exclusion of patients with suspected intubation difficulty (Mallampati Scoring of Class II and above) may cause potential biases. At last, the use of tramadol for postoperative salvage analgesia may influence the occurrence of PONV. Taken together, buccal acupuncture reduces perioperative consumption of analgesic drugs and favors the postoperative analgesic effect and recovery in elderly patients undergoing laparoscopic radical gastrectomy with a high safety. This method can provide reference for postoperative analgesia in other surgical patients.
In conclusion, the use of buccal acupuncture before general anesthesia induction reduces perioperative consumption of analgesic drugs and favors the postoperative analgesic effect and recovery in elderly patients undergoing laparoscopic radical gastrectomy by relieving postoperative stress response and inflammatory response, which acceptable efficacy and safety.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Medical Ethics Committee of Jiangning Hospital affiliated to Nanjing Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
D-xZ: Data curation, Methodology, Visualization, Investigation, Writing – original draft. Y-lY: Investigation, Conceptualization, Methodology, Writing – original draft. LY: Data curation, Investigation, Writing – original draft. Y-yZ: Investigation, Methodology, Writing – original draft. Y-yX: Data curation, Software, Writing – original draft. WW: Conceptualization, Funding acquisition, Methodology, Project administration, Writing – review & editing. JL: Conceptualization, Formal analysis, Supervision, Writing – review & editing. W-yY: Supervision, Validation, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research was supported by the Plan of Science and Technology benefit to the people of Jiangning district in Nanjing (no. 2023078S).
We are grateful to all participants involved in this study for their cooperation. We are also very grateful to those who help us with the writing of the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Caruso, S, and Scatizzi, M. Laparoscopic gastrectomy for gastric cancer: has the time come for considered it a standard procedure? Surg Oncol. (2022) 40:101699. doi: 10.1016/j.suronc.2021.101699
2. Cook, CE, Bailliard, A, Bent, JA, Bialosky, JE, Carlino, E, Colloca, L, et al. An international consensus definition for contextual factors: findings from a nominal group technique. Front Psychol. (2023) 14:1178560. doi: 10.3389/fpsyg.2023.1178560
3. Griswold, D, Learman, K, Rossettini, G, Palese, A, Ickert, E, Wilhelm, M, et al. Identifying priority gaps in contextual factors research and force-based manipulation. An international and interdisciplinary Delphi study. J Man Manip Ther. (2024) 32:118–26. doi: 10.1080/10669817.2023.2255820
4. Wang, N, Zhou, H, Song, X, and Wang, J. Comparison of oxycodone and sufentanil for patient-controlled intravenous analgesia after laparoscopic radical gastrectomy: a randomized double-blind clinical trial. Anesth Essays Res. (2016) 10:557–60. doi: 10.4103/0259-1162.186603
5. Dinges, HC, Schubert, AK, Rücker, G, Otto, S, Waldmann, S, Wiesmann, T, et al. Equianalgesic potency ratios of opioids used in patient-controlled analgesia: a network meta-analysis. J Opioid Manag. (2022) 18:567–86. doi: 10.5055/jom.2022.0751
6. Kim, SJ, Jeon, CH, Lee, HH, Song, KY, and Seo, HS. Impact of postoperative NSAIDs (IV-PCA) use on short-term outcomes after laparoscopic gastrectomy for the patients of gastric cancer. Surg Endosc. (2023) 37:1123–31. doi: 10.1007/s00464-022-09600-4
7. Shi, DW, Zhou, XD, Wang, FJ, Wang, J, Liu, Y, Niu, Y, et al. Opioid-sparing effect of multi-point incision-based rectus sheath block in laparoscopic-assisted radical gastrectomy: a randomized clinical trial. J Clin Med. (2023) 12:1414. doi: 10.3390/jcm12041414
8. Yoon, S, Song, GY, Lee, J, Lee, HJ, Kong, SH, Kim, WH, et al. Ultrasound-guided bilateral subcostal transversus abdominis plane block in gastric cancer patients undergoing laparoscopic gastrectomy: a randomised-controlled double-blinded study. Surg Endosc. (2022) 36:1044–52. doi: 10.1007/s00464-021-08370-9
9. Kikuchi, S, Kuroda, S, Nishizaki, M, Matsusaki, T, Kuwada, K, Kimura, Y, et al. Comparison of the effects of epidural analgesia and patient-controlled intravenous analgesia on postoperative pain relief and recovery after laparoscopic gastrectomy for gastric Cancer. Surg Laparosc Endosc Percutan Tech. (2019) 29:405–8. doi: 10.1097/SLE.0000000000000605
10. Yanagimoto, Y, Takiguchi, S, Miyazaki, Y, Mikami, J, Makino, T, Takahashi, T, et al. Comparison of pain management after laparoscopic distal gastrectomy with and without epidural analgesia. Surg Today. (2016) 46:229–34. doi: 10.1007/s00595-015-1162-y
11. O'Neill, A, and Lirk, P. Multimodal Analgesia. Anesthesiol Clin. (2022) 40:455–68. doi: 10.1016/j.anclin.2022.04.002
12. Rossettini, G, Campaci, F, Bialosky, J, Huysmans, E, Vase, L, and Carlino, E. The biology of placebo and nocebo effects on experimental and chronic pain: state of the art. J Clin Med. (2023) 12:4113. doi: 10.3390/jcm12124113
13. Habibi, BA, Kim, C, and Elsharkawy, H. Persistent and chronic perioperative pain after Cancer surgery. Curr Oncol Rep. (2022) 24:215–22. doi: 10.1007/s11912-021-01152-5
14. Ezzatvar, Y, Dueñas, L, Balasch-Bernat, M, Lluch-Girbés, E, and Rossettini, G. Which portion of physiotherapy treatments' effect is attributable to contextual effects in people with musculoskeletal pain?: a meta-analysis of randomised placebo-controlled trials. J Orthop Sports Phys Ther. (2024) 54:391–9. doi: 10.2519/jospt.2024.12126
15. Ling, F, Qi, W, Li, X, Zhou, J, Xiong, J, Zhao, Y, et al. Bibliometric analysis of acupuncture therapy for Cancer pain over the past 10 years. J Pain Res. (2023) 16:985–1003. doi: 10.2147/JPR.S395421
16. Fu, S, Liu, F, Zhi, X, Wang, Y, Liu, Y, Chen, H, et al. Applications of functional near-infrared spectroscopy in non-drug therapy of traditional Chinese medicine: a review. Front Neurosci. (2024) 17:1329738. doi: 10.3389/fnins.2023.1329738
17. Wang, F, Peng, P, Zheng, Y, Cheng, S, and Chen, Y. Effect of acupuncture on postoperative pain in patients after laparoscopic cholecystectomy: a randomized clinical trial. Evid Based Complement Alternat Med. (2023) 2023:3697223–10. doi: 10.1155/2023/3697223
18. Liu, GS, Li, N, Meng, RX, and Wang, PS. Analgesic effect of buccal acupuncture on patients after lumbar spinal fusion: a randomized controlled trial. Zhongguo Zhen Jiu. (2023) 43:743–6. Chinese. doi: 10.13703/j.0255-2930.20220903-k0003
19. Shan, HH, Chen, HF, Lu, XH, Zhang, XM, Liu, SL, Chang, XL, et al. Buccal acupuncture combined with ultrasound-guided dry needle-evoked inactivation of trigger points to treat cervical and shoulder girdle myofascial pain syndrome. J Back Musculoskelet Rehabil. (2023) 36:1139–50. doi: 10.3233/BMR-220321
20. Yi, Y, Huijun, YE, Huiling, Z, and Lihua, J. Clinical observation on 90 cases of primary dysmenorrhea treated by buccal acupuncture therapy: a randomized controlled study. J Tradit Chin Med. (2024) 44:172–81. doi: 10.19852/j.cnki.jtcm.20231110.001
21. Calvert, M, Blazeby, J, Altman, DG, Revicki, DA, Moher, D, Brundage, MD, et al. Reporting of patient-reported outcomes in randomized trials: the CONSORT PRO extension. JAMA. (2013) 309:814–22. doi: 10.1001/jama.2013.879
22. Lee, A, Fan, LT, Gin, T, Karmakar, MK, and Ngan Kee, WD. A systematic review (Meta-analysis) of the accuracy of the Mallampati tests to predict the difficult airway. Anesth Analg. (2006) 102:1867–78. doi: 10.1213/01.ane.0000217211.12232.55
23. Wang, YZ . Buccal Acupuncture Therapy. Beijing People’s Health Publishing House; (2017) pp. 20–104.
24. Xu, F, Zhang, Q, Xuan, D, Zhao, S, Wang, Y, Han, L, et al. Daytime variation in non-cardiac surgery impacts the recovery after general anesthesia. Ann Med. (2023) 55:1134–43. doi: 10.1080/07853890.2023.2187875
25. Ebara, G, Sakuramoto, S, Matsui, K, Nishibeppu, K, Fujita, S, Fujihata, S, et al. Efficacy and safety of patient-controlled thoracic epidural analgesia alone versus patient-controlled intravenous analgesia with acetaminophen after laparoscopic distal gastrectomy for gastric cancer: a propensity score-matched analysis. Surg Endosc. (2023) 37:8245–53. doi: 10.1007/s00464-023-10370-w
26. Kurni, M, Kaloria, N, Hazarika, A, Jain, K, Gupta, SK, and Walia, R. Comparison of midazolam and Propofol infusion to suppress stress response in patients with severe traumatic brain injury: a prospective, randomized controlled trial. Korean J Neurotrauma. (2023) 19:70–81. doi: 10.13004/kjnt.2023.19.e4
27. Kunigo, T, Murouchi, T, Yamamoto, S, and Yamakage, M. Spread of injectate in ultrasound-guided serratus plane block: a cadaveric study. JA Clin Rep. (2018) 4:10. doi: 10.1186/s40981-018-0147-4
28. Marino, Y, Arangia, A, Cordaro, M, Siracusa, R, D'Amico, R, Impellizzeri, D, et al. Analysis of the influence of IL-6 and the activation of the Jak/Stat3 pathway in fibromyalgia. Biomedicines. (2023) 11:792. doi: 10.3390/biomedicines11030792
29. van Helvoort, EM, van der Heijden, E, van Roon, JAG, Eijkelkamp, N, and Mastbergen, SC. The role of Interleukin-4 and Interleukin-10 in osteoarthritic joint disease: a systematic narrative review. Cartilage. (2022) 13:19476035221098167. doi: 10.1177/19476035221098167
30. Jie, W, Fang, X, Pu, R, Su, C, Zhang, Y, Pu, Y, et al. Analgesic effect of buccal acupuncture on acute arthritis in rabbits and underlying mechanisms. Zhong Nan Da Xue Xue Bao Yi Xue Ban. (2017) 42:517–21. doi: 10.11817/j.issn.1672-7347.2017.05.006
31. Tao, S, Wang, X, Liao, C, Xiong, Y, Tang, J, Jiang, N, et al. The efficacy of Moxibustion on the serum levels of CXCL1 and β-EP in patients with rheumatoid arthritis. Pain Res Manag. (2021) 2021:1–10. doi: 10.1155/2021/7466313
32. Chen, Y, Li, D, Li, N, Loh, P, Guo, Y, Hu, X, et al. Role of nerve signal transduction and neuroimmune crosstalk in mediating the analgesic effects of acupuncture for neuropathic pain. Front Neurol. (2023) 14:1093849. doi: 10.3389/fneur.2023.1093849
33. Yang, Y, Li, Q, He, QH, Han, JS, Su, L, and Wan, Y. Heteromerization of μ-opioid receptor and cholecystokinin B receptor through the third transmembrane domain of the μ-opioid receptor contributes to the anti-opioid effects of cholecystokinin octapeptide. Exp Mol Med. (2018) 50:1–16. doi: 10.1038/s12276-018-0090-5
34. Imai, T, Nagai, S, Michikawa, T, Inagaki, R, Kawabata, S, Ito, K, et al. Impact of lumbar surgery on pharmacological treatment for patients with lumbar Spinal Canal stenosis: a single-center retrospective study. J Clin Med. (2023) 12:2385. doi: 10.3390/jcm12062385
35. Wang, W, Liu, Y, Yang, X, Sun, J, Yue, Z, Lu, D, et al. Effects of Electroacupuncture for opioid-induced constipation in patients with Cancer in China: a randomized clinical trial. JAMA Netw Open. (2023) 6:e230310. doi: 10.1001/jamanetworkopen.2023.0310
36. Gouveia, F, Oliverira, C, and Losa, N. Acupuncture in the management of intraoperative nausea and vomiting. J Acupunct Meridian Stud. (2016) 9:325–9. doi: 10.1016/j.jams.2016.09.005
Keywords: buccal acupuncture, elderly, laparoscopic radical gastrectomy, analgesia, stress response
Citation: Zhu D-x, Yang Y-l, Yang L, Zhao Y-y, Xie Y-y, Wang W, Lv J and Yu W-y (2024) Effects of buccal acupuncture on postoperative analgesia in elderly patients undergoing laparoscopic radical gastrectomy: a randomized controlled trial. Front. Neurol. 15:1408360. doi: 10.3389/fneur.2024.1408360
Received: 28 March 2024; Accepted: 06 June 2024;
Published: 26 June 2024.
Edited by:
José Aparecido Da Silva, University of Brasilia, BrazilCopyright © 2024 Zhu, Yang, Yang, Zhao, Xie, Wang, Lv and Yu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wei Wang, d2FuZ3dlaTIwMjRAMTYzLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.