
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Neurol., 19 July 2024
Sec. Neurorehabilitation
Volume 15 - 2024 | https://doi.org/10.3389/fneur.2024.1406475
 Wai Ching Lam1,2
Wai Ching Lam1,2 Dongjue Wei2
Dongjue Wei2 Huijuan Li2
Huijuan Li2 Liang Yao3
Liang Yao3 Shiping Zhang2
Shiping Zhang2 Michael X. Y. Lai2
Michael X. Y. Lai2 Ya Zheng4
Ya Zheng4 Jerry W. F. Yeung5
Jerry W. F. Yeung5 Alexander Y. L. Lau6,7
Alexander Y. L. Lau6,7 Aiping Lyu8
Aiping Lyu8 Zhaoxiang Bian8
Zhaoxiang Bian8 Angela M. Cheung9*
Angela M. Cheung9* Linda L. D. Zhong1,2,8*
Linda L. D. Zhong1,2,8*Importance: Acupuncture has been used to treat neurological and neuropsychiatric symptoms in China and other parts of the world. These symptoms, such as fatigue, headache, cognitive impairment, anxiety, depression, and insomnia, are common in people experiencing long COVID.
Objective: This study aims to explore the feasibility of acupuncture in the treatment of neurological and neuropsychiatric symptoms in long COVID patients.
Data Sources: A systematic search was conducted in four English and four Chinese databases from inception to 23 June 2023. Literature selection and data extraction were conducted by two pairs of independent reviewers.
Study Selection: Randomized controlled trials (RCTs) that explored the effect of acupuncture on fatigue, depression, anxiety, cognitive abnormalities, headache, and insomnia were included.
Data Extraction and Synthesis: RCTs that explored the effect of acupuncture on fatigue, depression, anxiety, cognitive abnormalities, headache, and insomnia were included. A meta-analysis was performed using R software. Heterogeneity was measured using I2. Subgroup analyses were performed focusing on the duration of treatment and acupuncture modalities. The systematic review protocol was registered on PROSPERO (registration number: CRD42022354940).
Main outcomes and measures: Widely adopted clinical outcome scales included the Fatigue Scale for assessing fatigue, the Hamilton Depression Rating Scale for evaluating depression, the Mini-Mental State Examination for assessing cognitive impairment, the Visual Analog Scale for headache severity, and the Pittsburgh Sleep Quality Index for measuring insomnia.
Results: A total of 110 RCTs were included in the systematic review and meta–analysis. Overall, acupuncture was found to improve the scores of the Fatigue Scale (vs. medication: mean differences (MD): −2.27, P < 0.01; vs. sham acupuncture: MD: −3.36, P < 0.01), the Hamilton Depression Rating Scale (vs. medication: MD: −1.62, 95%, P < 0.01; vs. sham acupuncture: MD: −9.47, P < 0.01), the Mini–Mental State Examination (vs. medication: MD: 1.15, P < 0.01; vs. sham acupuncture: MD: 1.20, P < 0.01), the Visual Analog Scale (vs. medication: MD: −1.05, P < 0.01; vs. waitlist: MD: −0.48, P=0.04), and the Pittsburgh Sleep Quality Index (vs. medication: MD: −2.33, P < 0.01; vs. sham acupuncture: MD: −4.19, P < 0.01).
Conclusion and relevance: This systematic review suggested acupuncture as a potentially beneficial approach for the treatment of neurological and neuropsychiatric symptoms, as assessed using clinical scales, and it may have applicability in long COVID patients. Further well-designed clinical studies specifically targeting long COVID patients are needed to validate the role of acupuncture in alleviating long COVID symptoms.
Systematic Review Registration: PROSPERO, identifier [CRD42022354940].
• Question: Would acupuncture be potentially beneficial for neurological and neuropsychiatric symptoms in long COVID patients?
• Findings: In this meta-analysis of 110 studies, it was found that acupuncture, compared to medication or sham acupuncture, could improve the measurement scores of symptoms, including fatigue, depression, cognitive impairment, headache, and insomnia, among long COVID patients. Approximately 7.8% of patients who received acupuncture treatment reported the incidence of adverse effects.
• Meaning: This systematic review suggested that acupuncture could be explored as an alternative approach for addressing neurological and neuropsychiatric complications in long COVID patients.
Approximately 10–30% of people have lingering symptoms after an acute SARS-CoV-2 infection, making it challenging for them to return to work and resume their normal daily activities (1). These include neurological symptoms such as fatigue, cognitive impairment, brain fog, and loss of smell and neuropsychiatric symptoms such as anxiety and depression, as well as physical symptoms such as dyspnea, cough, myalgia, and arthralgia—a phenomenon colloquially termed “long COVID” (2–6).
One of the most significant impairments in patients with long COVID are neurological and neuropsychiatric symptoms (7). In a meta-analysis of more than 10,000 patients selected from 18 published studies, nearly one-third of patients experienced neurological and neuropsychiatric symptoms such as fatigue, cognitive dysfunction, and sleep disturbances, 3 months after the onset of acute COVID-19 infection (8). Similarly, another review that studied neuropsychiatric symptoms of COVID-19 found depression, anxiety, cognitive abnormalities, fatigue, sleep disturbances, and headache to be the most commonly reported long COVID-related neuropsychiatric symptoms reported between 4 weeks and 6 months after the onset of acute COVID-19 infection (9).
Given the unclear pathophysiology of long COVID, physicians have been using clinical strategies adapted from the treatment of similar symptoms/conditions with some measure of success (10). Acupuncture, a common technique for treating neurological and neuropsychiatric symptoms in traditional Chinese medicine, has been widely used in clinical practice. There is an increasing body of evidence showing that acupuncture may help alleviate neurological and neuropsychiatric symptoms not only in patients with acute pain (11) but also in those with specific chronic conditions (12–15), as well as those with severe diseases such as cancer-related insomnia and fatigue (16, 17).
Although previous systematic reviews have suggested acupuncture as an effective and safe treatment for patients with various neurological and neuropsychiatric disorders, these studies are not appropriate for providing evidence for long COVID as they included patients with multiple primary diseases or chronic conditions. Contrarily, many of the long COVID patients were generally well before the onset of acute COVID infection. To provide insights into the management of a newly emerging condition, our systematic review aimed to summarize and analyze the efficacy and safety of acupuncture in treating the common neurological and neuropsychiatric symptoms that are found in long COVID patients, namely fatigue, insomnia, depression, anxiety, cognitive abnormalities, and headache, based on data from randomized controlled trials (RCTs).
We performed the systematic review in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (18). We searched PubMed, Embase, Cochrane Library, Web of Science, China National Knowledge Infrastructure (CNKI), Wanfang Database, Chinese Scientific Journal Database (VIP), and Chinese Biomedical Literature Database (CBM) databases from inception to 23 June 2023 and identified randomized controlled trials (RCTs) examining the use of acupuncture in patients experiencing fatigue, depression, anxiety, cognitive dysfunction, headache, and insomnia, provided these symptoms were not caused by other chronic conditions. The selection of these symptoms was based on published studies that reported the common symptoms of long COVID (8, 9, 19, 20). We also carried out backward and forward searching to identify additional studies from citations. The completed search formula for each database is depicted in Supplementary Table 1.
Detailed inclusion and exclusion criteria are listed in Supplementary Table 2. RCTs reporting patients with at least one of the targeted neurological or neuropsychiatric symptoms (fatigue, depression, anxiety, cognitive abnormalities, headache, and insomnia) were included. Studies were excluded if the symptoms were caused by other chronic disorders.
Two pairs of reviewers (MXYL and YZ, DW and WCL) reviewed the title and abstract of each article and selected studies for a full-text review based on the inclusion and exclusion criteria. Conflicts were resolved through discussions and the involvement of a third researcher (LLZ).
Three reviewers (HL, WCL, and MXYL) extracted participant characteristic data from the selected studies using a standardized data extraction form. We extracted the following information from each included article: first author, year of publication, type and duration of the diseases, diagnostic criteria for the neurological and neuropsychiatric symptoms, number of participants, demographic data of participants, characteristics of the acupuncture and control groups, outcome data, duration of follow-ups, number of dropouts, and reports of adverse effects. Given that the number of participants and dropouts might vary at different stages in the same study, we considered the sample size included in the intention-to-treat analysis and the number of dropouts at the end of interventions.
All reviewers underwent comprehensive training for conducting assessments using the guidance document developed by the Cochrane Risk-of-Bias Tool for Randomized Trials (RoB 2) Development Group (21). The training encompassed a detailed understanding of the assessment process, including the nuances of each bias domain and the application of the tool's criteria. Two reviewers (DW and MXYL) assessed the potential risk of bias for all included studies in five different domains: (1) bias arising from the randomization process; (2) bias due to deviations from intended interventions; (3) bias due to missing outcome data; (4) bias in the measurement of the outcome; and (5) bias in the selection of the reported result. Each domain was assessed for risk of bias as “low risk,” “some concerns,” or “high risk,” and an overall consensus about the risk of bias was reached. In cases where a high risk of bias was identified, detailed documentation of the particular concerns within each domain was undertaken. A third review author (WCL) acted as an adjudicator in the event of disagreement.
We conducted a systematic review and meta-analysis for the following symptoms: fatigue, depression, anxiety, mild cognitive impairment, headache, and insomnia. For the meta-analysis, mean differences (MDs) with 95% confidence intervals (CIs) were adopted as the effect size for continuous outcomes. Forest plots were generated to visually assess the effect size, corresponding 95% CIs, and heterogeneity. Heterogeneity was assessed by conducting the chi-squared test and I2. The values of I2 <25%, 25–50%, and >50% indicated low, moderate, and high heterogeneity, respectively. A random model was used if there was significant heterogeneity (I2 >50%); otherwise, a fixed model was used. Subgroup analyses were based on the type of acupuncture (electro-acupuncture or manual acupuncture), treatment duration (short-term: ≤ 4 weeks or long-term: >4 weeks), and the type of medication. Sensitivity analyses were performed by limiting our analyses to high-quality studies to determine the robustness of the meta-analysis. Funnel plots were utilized, and Begg's test was conducted to detect the publication bias when at least 10 studies were reporting the outcome(s). The statistical analysis was performed by a statistician (LHJ) using R software, version 4.3.2.
A total of 13,831 records were identified from eight databases (Figure 1). After excluding duplicate records, 10,764 records were screened. A total of 2,168 full-text records were assessed for eligibility through preliminary screening. Finally, 110 studies met the inclusion and exclusion criteria and were included in our review and quantitative synthesis.
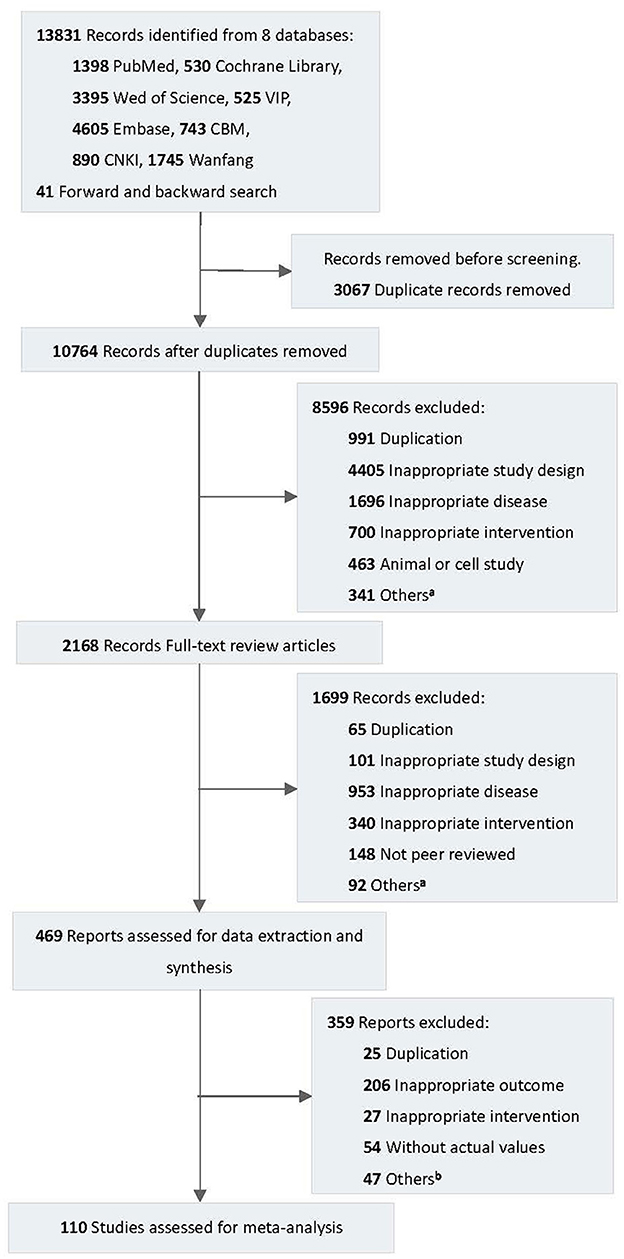
Figure 1. Flow diagram of the study selection process. VIP, Chinese Scientific Journal Database; CBM, Chinese Biomedical Literature Database; CNKI, China National Knowledge Infrastructure. aIncludes protocol, conference abstract, etc. bIncludes non-peered reviewed articles, incomparable type of data, etc.
Out of 110 RCTs included in our study, the sample sizes ranged from 30 to 440. A total of 11 studies specifically concerned fatigue, 32 concerned depression or anxiety, 7 concerned mild cognitive impairment, 18 concerned headache, and 42 concerned insomnia. The overall treatment duration varied from 10 days to 4 months. Most of the trials were two-armed, with the exception of one four-armed trial and 14 three-armed trials. The detailed characteristics of each study are presented in Supplementary Table 3.
Figure 2 shows the overall risk of bias, and the details of each study are shown in Supplementary Figure 1. A total of 79 out of 110 studies reported the randomization process. Approximately 84% of the 79 articles specified the generation of random sequences and 82% stated the allocation concealment. A total of 31 studies were rated as having a high risk of performance bias or unclear performance bias (blinding of participants and personnel). Out of these 79 studies, 64 performed single blinding of patients by using true and sham techniques for stimulating acupoints, and 59 studies reported using blinded assessors. No study was double-blinded as it is difficult to blind the acupuncture therapist. Other biases were caused by unreported dropouts or a large number of dropouts affecting the results (22–27), a change in protocol during the course of the trial (22, 28–35), potential carryover effects in crossover studies (23, 25, 26, 28, 33, 35–50), and problems associated with the statistical analysis of results and the tendency to draw optimistic conclusions (25, 26, 28, 35, 36, 38, 42, 43, 47, 51–55). In conclusion, the assessment of the risk of bias highlights crucial methodological considerations. These revelations necessitate meticulous consideration when interpreting the outcomes of the meta-analysis.
A total of 110 studies with 8,514 participants were included in the meta-analysis. The results of the meta-analysis are presented in Table 1. The forest plots of the meta-analysis are shown in Figures 3–7.
Outcome 1. Fatigue Scale (FS-14)
Comparison 1. Acupuncture vs. medication
One study compared acupuncture and medication for the treatment of fatigue as measured using the FS-14 (0–14 scores) and found that acupuncture could relieve the symptoms of fatigue (MD: −2.27, 95% CIs: −2.85 to −1.69, P < 0.01) (Figure 3) (56).
Comparison 2. Acupuncture vs. sham acupuncture
Five trials that compared acupuncture with sham acupuncture were included (57–61). The result indicated that acupuncture could reduce the scores of the FS−14 and improve fatigue symptoms compared to sham acupuncture (MD: −3.36, 95% CIs: −4.91 to −1.79, P < 0.01), although heterogeneity was present (I2 = 95%).
Outcome 2. Fatigue Assessment Instrument (FAI)
Two studies compared acupuncture with moxibustion (62, 63). The pooled analysis indicated that acupuncture is inferior to moxibustion in treating fatigue symptoms (MD: 27.46, 95% CIs: 20.17 to 34.75, I2 = 0%, P < 0.01).
Outcome 3. Visual Analog Scale (VAS)
Four studies compared acupuncture with sham acupuncture (59, 64–66), and the results showed that acupuncture could decrease chronic fatigue–related pain (MD: −36.02, 95% CIs: −63.30 to −8.75, I2 = 88%, P = 0.01).
Outcome 1. Hamilton Depression Rating Scale (HAMD)
Comparison 1. Acupuncture vs. medication
Twelve studies involving 738 participants were included in this pooled analysis (28, 36–38, 51, 52, 67–72). The results showed that acupuncture was better than medication in improving depressive symptoms (MD: −1.62, 95% CIs: −3.07 to −0.17, P < 0.01). However, there was substantial heterogeneity among these studies (I2 = 85%) (Figure 4).
The subgroup analysis based on treatment duration (≤ 4 weeks vs. >4 weeks) indicated that short–term efficacy of acupuncture was better (≤ 4 weeks: MD: −2.96, 95% CIs: −5.47 to −0.45; >4 weeks: MD: −0.68, 95% CIs: −2.40 to 1.03) than medication. The subgroup analysis of electro–acupuncture or manual acupuncture failed to show significant benefits for treating depression compared with medication (electro–acupuncture: MD: −0.89, 95% CIs: −1.82 to 0.05; manual acupuncture: MD: −1.80, 95% CIs: −3.84 to 0.24) (Supplementary Figure 2). However, there was heterogeneity among the subgroups of ≤ 4 weeks, >4 weeks, and manual acupuncture.
A sensitivity analysis was conducted on the remaining high–quality studies assessed by the RoB 2 Development Group to investigate the influence of study quality on the effect size. The result of the sensitivity analysis showed that acupuncture was not superior to medication (fluoxetine) in treating depression (MD: −1.32, 95% CIs: −6.23, 3.59; P <0.01). However, the heterogeneity was still significant (I2 = 93%) (Supplementary Figure 3).
Comparison 2. Acupuncture vs. sham acupuncture
In four studies (73–76), acupuncture was shown to have better effectiveness than sham acupuncture in relieving depressive symptoms (MD: −9.47, 95% CIs: −13.74 to −5.19, I2=95%, P < 0.01).
Comparison 3. Acupuncture vs. waitlist
One study reported that acupuncture was more effective in relieving depressive symptoms than the control waitlist group (MD: −3.80, 95% CIs: −6.96 to −0.64, P = 0.02) (77).
Comparison 4. Acupuncture plus medication vs. medication
Two studies reported that acupuncture with medication was more effective in relieving depressive symptoms than medication alone (MD: −4.87, 95% CIs: −9.53 to −0.21, I2 = 35%, P < 0.01) (78, 79).
Comparison 5. Acupuncture plus rTMS vs. sham acupuncture plus rTMS
One study compared acupuncture plus Repetitive Transcranial Magnetic Stimulation (rTMS) with sham acupuncture plus rTMS (80). The acupuncture plus rTMS group demonstrated better efficacy (MD: −4.28, 95% CIs: −6.63, −1.93, P < 0.01).
Outcome 2. Hamilton Anxiety Rating Scale (HAM–A)
Nine studies compared acupuncture with medication using the HAM–A scores (30–35, 39, 81, 82). These studies did not show any significant difference between the two groups (MD: −0.65, 95% CIs: −1.65, 0.35, I2 = 83%, P < 0.01).
Two studies compared acupuncture with sham acupuncture and did not show any significant difference between the two groups (MD: −7.78, 95% CIs: −17.06, 1.51, I2 = 93%, P = 0.10) (73, 75).
One study compared acupuncture with Cranial Electrotherapy Stimulation (CES) (82). There was no significant difference between the two groups (MD: −0.41, 95% CIs: −1.02, 0.20, P = 0.19).
Outcome 3. Self–Rating Depression Scale (SDS)
Four studies compared acupuncture with medication using the SDS and found no significant difference between the two groups (MD: −0.45, 95% CIs: −6.30, 5.41, I2 = 86%, P = 0.88) (22, 29, 38, 70).
Four studies compared acupuncture with sham acupuncture, and it was found that acupuncture could reduce the scores of the SDS (MD: −13.57, 95% CIs: −19.24, −7.90, I2 = 90%, P < 0.01) (29, 74, 83, 84).
Outcome 1. Mini-Mental State Examination (MMSE)
Comparison 1. Acupuncture vs. medication
Five studies compared acupuncture with medication using the MMSE (ranging from 0 to 30) (23, 85–88) and showed that acupuncture was slightly better than medication in improving mild cognitive impairment (MD: 1.15, 95% CIs: 0.88 to 1.41, P < 0.01), without significant heterogeneity (I2 = 0%) (Figure 5).
Comparison 2. Acupuncture vs. sham acupuncture
A pooled analysis of two studies indicated that acupuncture could slightly relieve the symptoms of mild cognitive impairment compared with sham acupuncture (MD: 1.20, 95% CIs: 0.50 to 1.90, I2=0%, P <0.01) (53, 89).
Comparison 3. Acupuncture vs. waitlist
One study indicated that acupuncture could relieve cognitive impairment symptoms compared with the waitlist (MD: 2.38, 95% CIs: 1.43 to 3.33, P < 0.01) (89).
Outcome 1. Headache diary records (headache frequency per month)
Two studies compared the overall scores between acupuncture and medication (24, 90), and no significant difference was reported (MD: 0.03, 95% CIs: −0.86 to 0.91, I2 = 0%, P = 0.95) (Figure 6).
Four studies compared acupuncture with sham acupuncture (54, 91–93), and no obvious difference was found between the two groups (MD: −3.35, 95% CIs: −7.13 to 0.44, I2 = 83%, P = 0.08).
Two studies compared acupuncture with the waitlist control (93, 94), and no significant difference was detected (MD: −3.77, 95% CIs: −8.67 to 1.12, I2 = 93%, P = 0.13).
One study compared acupuncture with Transcutaneous Electrical Nerve Stimulation (TENS) (95), and it showed that TENS was better than acupuncture for relieving headache (MD: 6.61, 95% CIs: 3.66 to 9.56, P < 0.01).
Outcome 2. VAS
Comparison 1. Acupuncture vs. medication
Two studies compared acupuncture with medication using the VAS scores for headache. The results showed that acupuncture is slightly better than medication therapy in reducing headache (MD: −1.05, 95% CIs: −1.48 to −0.62, I2 = 0%, P <0.01) (55, 96).
Comparison 2. Acupuncture vs. sham acupuncture
Six studies compared acupuncture with sham acupuncture (40, 54, 97–100). The results showed that acupuncture was not superior to sham acupuncture for relieving headache (MD: −0.74, 95% CIs: −1.70 to 0.23, I2 = 84%, P = 0.13).
Comparison 3. Acupuncture vs. waitlist
One study compared acupuncture with waitlist control (101). It showed a slight difference between the two groups (MD: −0.48, 95% CIs: −0.93 to −0.03, P = 0.04).
Outcome 3. Migraine Disability Assessment Scale (MIDAS)
One study compared acupuncture with medication using the MIDAS and showed that acupuncture could reduce the overall scores after treatment compared with medication (MD: −10.30, 95% CIs: −16.82 to −3.78, P <0.01) (102).
One study compared acupuncture with sham acupuncture (103). There was no significant difference reported between the two groups (MD: −9.00, 95% CIs: −20.86 to 2.86, P = 0.14).
One study compared acupuncture with the waitlist (101). It failed to show any significant difference between the two groups (MD: −9.60, 95% CIs: −24.69 to 5.49, P = 0.21).
Outcome 1. Pittsburgh Sleep Quality Index (PSQI)
Comparison 1. Acupuncture vs. medication
A total of 18 studies were included in the analysis of insomnia measured using the PSQI (0–21 scores) (25, 26, 41–46, 48, 104–112). Acupuncture was reported to have better efficacy for insomnia than medication (MD: −2.33, 95% CIs: −2.99 to −1.67, I2 = 87%, P < 0.01) (Figure 7).
The subgroup analysis showed that there was a slight difference between the electro–acupuncture and manual acupuncture groups (electro–acupuncture: MD: −2.71, 95% CIs: −3.81 to −1.61; manual acupuncture: MD: −2.31, 95% CIs: −3.00 to −1.61; P =0.54) (Supplementary Figure 2). In addition, alprazolam showed better efficacy than other medications. A second subgroup analysis was not conducted in the present study because the treatment duration of all included studies was <4 weeks.
A sensitivity analysis was carried out exclusively on studies with a low risk of bias. Among six high–quality studies, it was shown that acupuncture provided a slight benefit for treating insomnia compared with medication (estazolam) (MD: −3.44, 95% CI: −4.39, −2.50, P < 0.01). This result was consistent with the findings of the total meta–analysis (Supplementary Figure 3).
Comparison 2. Acupuncture vs. sham acupuncture
A total of 21 studies compared the efficacy of acupuncture with that of sham acupuncture (27, 60, 76, 84, 113–129). The overall meta–analysis result showed that acupuncture had better efficacy for treating insomnia (MD: −4.19, 95% CIs: −5.33 to −3.05, I2=93%, P < 0.01). The results of the two subgroup analyses indicated that manual acupuncture had better efficacy than electro–acupuncture, and acupuncture was found to be more effective in the short term than in the long term (Supplementary Figure 2).
The sensitivity analyses solely included high–quality studies, which showed that acupuncture was beneficial for treating insomnia compared with sham acupuncture (MD: −4.36, 95% CI: −5.22, −3.50, P < 0.01). The finding was consistent with the result of the meta–analysis (Supplementary Figure 3).
Comparison 3. Acupuncture vs. non–invasive intervention
One study compared acupuncture with acupressure (49). There was no difference between the two groups (MD: 0.74, 95% CIs: −0.63 to 2.11, P = 0.29).
Comparison 4. Acupuncture plus rTMS vs. sham acupuncture plus rTMS
One study compared acupuncture plus rTMS with sham acupuncture plus rTMS (80). The acupuncture plus rTMS group showed better efficacy (MD: −2.38, 95% CIs: −4.40, −0.36, P = 0.02).
Outcome 2. Insomnia Severity Index (ISI)
One study compared acupuncture with medication using the ISI and showed that acupuncture could reduce the overall scores after treatment compared with medication (MD: −2.20, 95% CIs: −3.71 to −0.69, P <0.01) (130).
Four studies compared acupuncture with sham acupuncture. The acupuncture group did not show better efficacy (MD: −5.19, 95% CIs: −10.46 to 0.09, I2 = 97%, P = 0.05) (83, 122, 130, 131).
Outcome 3. Score changes measured using the Epworth Sleepiness Scale (ESS)
Two studies compared acupuncture with medication using the ESS and showed that acupuncture could reduce the overall scores compared with medication (MD: −4.64, 95% CIs: −5.80 to −3.48, I2 = 0%, P < 0.01) (47, 50).
A total of 45 out of 110 (40.91%) included studies reported that patients with adverse effects were observed in both acupuncture and control groups (Supplementary Table 3). Among the 2,917 patients included in the 45 studies, 227 (7.78%) experienced adverse effects during acupuncture treatment, including instances of local bleeding, hematoma, needling pain, and dizziness. These effects were generally mild in severity, and the patients recovered well after rest or simple treatment. A total of 115 patients out of 1,153 (9.97%) taking Western medication reported adverse effects. It was reported that the incidence of acupuncture-related adverse effects was not significantly higher than that of medication treatment. A total of 14 patients out of 2,917 (0.48%) receiving acupuncture treatment withdrew from the clinical trial due to intolerance to acupuncture or adverse effects. A total of 9 patients out of 2,917 (0.31%) receiving acupuncture treatment reported severe adverse effects, but all of these effects were found to not be due to the intervention.
The Begg's tests did not show any significant difference, and the p-values were 0.6209 (acupuncture vs. medication for insomnia), 0.3021 (acupuncture vs. sham acupuncture for insomnia), and 0.6810 (acupuncture with medication for depression). The visual inspection of the funnel plots also did not reveal any substantial asymmetry in these comparisons (Supplementary Figure 4).
Our systematic review is the first to assess the efficacy and safety of acupuncture for relieving neurological and neuropsychiatric symptoms that are common in long COVID patients. Our results showed that, compared to medication or sham acupuncture, acupuncture improves the symptoms of fatigue, depression, cognitive impairment, headache, and insomnia but not anxiety. In addition to statistical relevance, clinical significance should also be considered. For the scales with statistical significance, the improvement in scores was within specific thresholds, such as 5–10% from the baseline scores. However, clinicians are advised to take an overall clinical perspective by reviewing the relevant scales to understand the comprehensive impact on the patient's health (132).
Our study included 110 original studies involving 8,514 participants and used multiple clinical scales to assess the effects of acupuncture on target symptoms. Before the submission of our manuscript, an additional search across databases was conducted, and it failed to uncover any published clinical trials applying acupuncture to treat long COVID patients. By identifying and critically evaluating evidence from RCTs, we aim to provide comprehensive and the best available evidence for clinicians and decision-makers.
Previous meta-analyses have demonstrated consistent conclusions regarding the effectiveness of acupuncture in treating fatigue (133), depression (134), mild cognitive impairment (135), migraine (136), and insomnia (137). Our study refined the scope by adjusting the eligibility criteria to include long COVID patients. In patients with fatigue, compared with the control groups, both acupuncture and moxibustion revealed significant improvements in chronic fatigue and related pain symptoms. In patients with depression and cognitive impairment, weak significant effects in the HAMD and MMSE suggested the potential advantages of acupuncture compared to the medication, sham acupuncture, and blank groups. However, it is important to mention that the sensitivity analyses among high-quality studies demonstrated that acupuncture was not superior to fluoxetine in treating depression. In patients with headache, the pooled analysis results showed that acupuncture could be beneficial in alleviating the pain intensity of headaches but ineffective in reducing headache frequency. In our findings related to patients with insomnia, we found that acupuncture could be effective not only in lowering the PSQI and ISI scores but also in helping patients recover from “daytime sleepiness.”
There were certain differences in the analysis results among the subgroups based on various treatment durations, which might have been caused by different compliance rates and the severity of the disease. However, these differences were not significant. In addition to the comparison between short-term and long-term treatment effects, we also investigated whether there could be a significant difference in the treatment effects between manual acupuncture and electro-acupuncture. Theoretically, the effectiveness of manual acupuncture could vary largely depending on the technique of the acupuncturists, while electro-acupuncture provides relatively stable and standard stimulation at the acupoint. However, our results did not demonstrate major variations between the two approaches.
Despite obtaining favorable results with acupuncture, fewer clinical research studies have been conducted on long COVID patients. There are two case studies published by Michael et al. (138) and Robert et al. (139). These studies described the use of acupuncture for the treatment of long COVID and showed the potential benefit of acupuncture for patients with chronic long COVID symptoms. Although several published studies have evaluated various pharmacological and non-pharmacological interventions for treating neurological and neuropsychiatric symptoms of long COVID, including conventional medications (140, 141), synbiotics (142), herbal formulas (143, 144), and physical and mindfulness training (145, 146), a lack of consensus on specific treatment protocols for long COVID patients remains.
According to our safety data, acupuncture can be considered relatively safe, with minor adverse effects occurring in 1 out of 13 patients; these adverse effects are mild and subside after rest or simple treatment. This finding is similar to that of another systematic review, which reported an overall risk of 9.31%, suggesting that patients experience at least one adverse effect during a series of acupuncture treatments (147). The occurrence of adverse effects in patients receiving acupuncture treatment is slightly lower than that in patients taking Western medication, which can be taken into consideration when recommending respective treatments to patients.
During the COVID-19 epidemic, several versions of acupuncture guidance have been developed and issued by professional bodies for recovery from COVID-19 (148, 149). However, the recommendations were solely based on the traditional Chinese medicine theory of restoring qi and the normal functions of the organs. From a biological mechanism perspective, studies suggested that neurological and neuropsychiatric symptoms in long COVID patients could be caused by the devastating effects of direct viral neuro-invasion and/or systemic inflammation and cell-mediated immune mechanisms (150). Moreover, long-term social isolation with changes in living habits could potentially contribute to these symptoms. Acupuncture works through multiple mechanisms, including the alleviation of inflammation levels, the modulation of immune response, and the regulation of nitric oxide production for blood flow (151).
This review has several limitations that must be acknowledged. First, the original studies included in our systematic review did not specifically involve long COVID patients, which may limit the direct applicability of our findings. While we adjusted the eligibility criteria to reflect conditions similar to those experienced by long COVID patients, the absence of direct evidence from this specific group remains a significant constraint. Second, there were variations in the sample sizes, acupuncture protocols, and the clinical scales used to measure outcomes. Such variability can introduce biases and complicate the interpretation and generalizability of our findings. Third, our meta-analysis excluded studies with incomparable measures, which might have led to selection bias and limited our ability to comprehensively assess the efficacy of acupuncture across all potential outcome measures. Finally, the adverse effects in some original studies were underreported, which means that the safety profile of acupuncture might not have been completely captured. Our study has certain strengths, that is, the total sample size was large, it involved a comprehensive search strategy to identify and select studies without language restriction, and it included data across various age groups and disease durations.
This systematic review suggested acupuncture as a potentially beneficial approach for the treatment of neurological and neuropsychiatric symptoms associated with long COVID, as assessed using clinical scales, and it may have applicability in long COVID patients. Further well-designed clinical studies specifically targeting long COVID patients are needed to validate the role of acupuncture in alleviating long COVID symptoms.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
WL: Writing – original draft, Writing – review & editing. DW: Writing – original draft, Writing – review & editing. HL: Writing – original draft, Writing – review & editing. LY: Writing – review & editing. SZ: Writing – review & editing. ML: Writing – original draft, Writing – review & editing. YZ: Writing – review & editing. JY: Writing – review & editing. AYLL: Writing – review & editing. AL: Writing – review & editing. ZB: Writing – review & editing. AC: Writing – review & editing. LZ: Funding acquisition, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was financially supported by the Chinese Medicine Development Fund (Ref. No. 22B2-011A) and the Health and Medical Research Fund (Ref. No. 20211471). The funding organizations had no role in designing and analyzing the study.
AC received support from the University of Toronto KY and Betty Ho Chair in Integrative Medicine.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2024.1406475/full#supplementary-material
1. Taquet M, Dercon Q, Luciano S, Geddes JR, Husain M, Harrison PJ. Incidence, co-occurrence, and evolution of long-COVID features: a 6-month retrospective cohort study of 273,618 survivors of COVID-19. PLoS Med. (2021) 18:e1003773. doi: 10.1371/journal.pmed.1003773
2. Nalbandian A, Sehgal K, Gupta A, Madhavan MV, McGroder C, Stevens JS, et al. Post-acute COVID-19 syndrome. Nat Med. (2021) 27:601–15. doi: 10.1038/s41591-021-01283-z
3. Soriano JB, Murthy S, Marshall JC, Relan P, Diaz JV. A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect Dis. (2022) 22:e102–7. doi: 10.1016/S1473-3099(21)00703-9
4. Davis HE, Assaf GS, McCorkell L, Wei H, Low RJ, Re'em Y, et al. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. eClinicalMedicine. (2021) 38:101019. doi: 10.1016/j.eclinm.2021.101019
5. Michelen M, Manoharan L, Elkheir N, Cheng V, Dagens A, Hastie C, et al. Characterising long COVID: a living systematic review. BMJ Glob Health. (2021) 6:e005427. doi: 10.1136/bmjgh-2021-005427
6. Lopez-Leon S, Wegman-Ostrosky T, Perelman C, Sepulveda R, Rebolledo PA, Cuapio A, et al. More than 50 long-term effects of COVID-19: a systematic review and meta-analysis. Sci Rep. (2021) 11:16144. doi: 10.1038/s41598-021-95565-8
7. Perlis RH, Santillana M, Ognyanova K, Safarpour A, Lunz Trujillo K, Simonson MD, et al. Prevalence and Correlates of Long COVID Symptoms Among US Adults. JAMA Netw Open. (2022) 5:e2238804. doi: 10.1001/jamanetworkopen.2022.38804
8. Premraj L, Kannapadi NV, Briggs J, Seal SM, Battaglini D, Fanning J, et al. Mid and long-term neurological and neuropsychiatric manifestations of post-COVID-19 syndrome: a meta-analysis. J Neurol Sci. (2022) 434:120162. doi: 10.1016/j.jns.2022.120162
9. Frontera JA, Simon NM. Bridging knowledge gaps in the diagnosis and management of neuropsychiatric sequelae of COVID-19. JAMA Psychiatry. (2022) 79:811. doi: 10.1001/jamapsychiatry.2022.1616
10. Schrimpf A, Braesigk A, Lippmann S, Bleckwenn M. Management and treatment of long COVID symptoms in general practices: an online-based survey. Front Public Health. (2022) 10:937100. doi: 10.3389/fpubh.2022.937100
11. Wang Y, Du R, Cui H, Zhang L, Yuan H, Zheng S. Acupuncture for acute migraine attacks in adults: a systematic review and meta-analysis. BMJ Evid Based Med. (2023) 28:228–40. doi: 10.1136/bmjebm-2022-112135
12. You J, Li H, Xie D, Chen R, Chen M. Acupuncture for chronic pain-related depression: a systematic review and meta-analysis. Pain Res Manage. (2021) 2021:1–10. doi: 10.1155/2021/6617075
13. Jianyu Y, Haiyan LI, Dingyi X, Mingren C, Rixin C. Efficacy of acupuncture therapy for post-stroke fatigue: a systematic review and meta-analysis. J Tradit Chin Med. (2023) 43:27–33.
14. Wang ZZ, Sun Z, Zhang ML, Xiong K, Zhou F. Systematic review and meta-analysis of acupuncture in the treatment of cognitive impairment after stroke. Medicine. (2022) 101:e30461. doi: 10.1097/MD.0000000000030461
15. Lee SH, Lim SM. Acupuncture for insomnia after stroke: a systematic review and meta-analysis. BMC Complement Altern Med. (2016) 16:228. doi: 10.1186/s12906-016-1220-z
16. Zhang J, Zhang Z, Huang S, et al. Acupuncture for cancer-related insomnia: a systematic review and meta-analysis. Phytomedicine. (2022) 102:154160. doi: 10.1016/j.phymed.2022.154430
17. Zhang Y, Lin L, Li H, Hu Y, Tian L. Effects of acupuncture on cancer-related fatigue: a meta-analysis. Support Care Cancer. (2018) 26:415–25. doi: 10.1007/s00520-017-3955-6
18. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
19. Badenoch JB, Rengasamy ER, Watson C, Jansen K, Chakraborty S, Sundaram RD, et al. Persistent neuropsychiatric symptoms after COVID-19: a systematic review and meta-analysis. Brain Commun. (2022) 4:fcab297. doi: 10.1093/braincomms/fcab297
20. Desai AD, Lavelle M, Boursiquot BC, Wan EY. Long-term complications of COVID-19. Am J Physiol-Cell Physiol. (2022) 322:C1–C11. doi: 10.1152/ajpcell.00375.2021
21. Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. (2019) 366:l4898. doi: 10.1136/bmj.l4898
22. Wang W, Lu X, Ng S, Hong L, Zhao Y, Lin YN, et al. Effects of electro-acupuncture on personality traits in depression: a randomized controlled study. Chin J Integr Med. (2013) 19:777–82. doi: 10.1007/s11655-013-1594-4
23. Liu XP, Liu ZY, Lou JR, Wang JS, Mi Y, Ma Z, et al. Intervention of electrical acupuncture in mild cognitive dysfunction. Xinjiang Zhongyiyao. (2010) 28:25–8.
24. Giannini G, Favoni V, Merli E, Nicodemo M, Torelli P, Matrà A, et al. A randomized clinical trial on acupuncture versus best medical therapy in episodic migraine prophylaxis: the ACUMIGRAN study. Front Neurol. (2020) 11:570335. doi: 10.21203/rs.3.rs-32721/v1
25. He T, Lai XS, Chen YQ. Acupuncture in the treatment of insomnia complicated with anxiety or depression: a report of 30 cases. J Anhui TCM College. (2010) 29:39–40.
26. Zhao CF, Huang YS. Clinical efficacy of acupuncture for primary insomnia. Guide of China Med. (2017) 15:217. doi: 10.1007/s11726-017-1037-4
27. Zhang L, Tang Y, Hui R, Zheng H, Deng Y, Shi Y, et al. The effects of active acupuncture and placebo acupuncture on insomnia patients: a randomized controlled trial. Psychol Health Med. (2020) 25:1201–15. doi: 10.1080/13548506.2020.1738015
28. Li SJ, Liu T. Clinical observation on treatment of melancholia by acupuncture following principle of relieving depression and regulating mentality. Zhongguo Zhong Xi Yi Jie He Za Zhi. (2007) 27:155–7.
29. Fu W-b, Fan L, Zhu X-p, He Q, Wang L, Zhuang L-x, et al. Depressive neurosis treated by acupuncture for regulating the liver–a report of 176 cases. J Tradit Chin Med. (2009) 29:83–6. doi: 10.1016/S0254-6272(09)60037-6
30. Zhao Y, Zou W, Teng W, Dai XH. Clinical study of Tongdu Tiaoshen acupuncture for the treatment of generalized anxiety disorder. JCAM. (2014) 30:24–6.
31. Chen Y, Fan ZQ. Randomized control study on combination of ear acupoint bloodletting and electroacupuncture for treating mild to moderate generalized anxiety disorder. J Mod Med Health. (2013) 29:1928–30.
32. Che LN. Therapeutic effect of acupuncture for the treatment of generalized anxiety disorder patients. Med J Chin People's Health. (2015) 27:86–7.
33. Wang GM. Acupuncture in the treatment of generalized anxiety disorder: a report of 21 cases. Henan Trad Chin Med. (2007) 27:55–6.
34. Zhou XF, Li Y, Zhu H, Chen LL. Impacts of acupuncture at twelve meridians acupoints on brain waves of patients with general anxiety disorder. Zhongguo Zhen Jiu. (2013) 33:395–8.
35. Zheng ZY, Zhu CX. Clinical study on acupuncture using back-shu points for anxiety. J Liaoning Coll TCM. (2004) 6:208.
36. Wei L, Zheng ZY, Liu D, Chen HL, Jin H, Yang JF. RCTs of Fuyang Yiyin acupuncture in treating depression. JCAM. (2021) 37:30–4.
37. Xie YC, Li YH. Observation on therapeutic effect of acupuncture at Zhongwan (CV 12) and Si-guan points combined with reinforcing-reducing manipulation of respiration for treatment of depression. Zhongguo Zhen Jiu. (2009) 29:521–4.
38. Zhu PY, Xue H. Clinical observation on the efficacy of acupuncture for relieving the depressed liver and regulating qi in the treatment of depression among seafarers. Chin J Naut Med & Hyperbar Med. (2016) 23:360−1.
39. Liu HJ, Luo WZ, Mei SY, Yuan Q, Jin R. Therapeutic observation of acupuncture for the treatment of generalized anxiety disorder. J Guangzhou Univer Trad Chin Med. (2007) 24:119–22.
40. Sozen A, Yilmaz M, Koyuncuoglu HR, Yurekli VA, Uzar E, Kutluhan S. Effectiveness of acupuncture for the treatment of chronic daily headache: a sham-controlled clinical trial. Acta Medica Mediterranea. (2013) 29:167–72.
41. Chen Q, Chen XJ, Zhou ZY, Chen LF. Efficacy of moxibustion on back-shu points for chronic insomnia: a randomized controlled clinical trial. Chin Arch Trad Chin Med. (2013) 31:2483–5.
42. Yang ZQ. Combination of behavioral therapy and acupuncture for insomnia caused by incoordination between heart and kidney: clinical observation on 37 cases. Guid J Trad Chin Med Pharm. (2011) 17:57–9.
43. Zhou DP. Preliminary observation and analysis of clinical efficacy of acupuncture for insomnia. Contemp Med. (2016) 22:24–5.
44. Xu YY, Lin XM. Clinical study on acupuncture of six points in regulating spirit and sleep three-needle points for primary insomnia of liver fire disturbing heart type. J New Chin Med. (2020) 52:151–3.
45. Liu F, Wang L, Wei QP, Wang ZH, Chen DM, Li CY, et al. Clinical curative observation of applying acupuncture at Shen-You time to regulate 196 cases of insomnia. J Sich Trad Chin Med. (2015) 33:174–6.
46. Tu JH, Chung WC, Yang CY, Tzeng DS, A. comparison between acupuncture versus zolpidem in the treatment of primary insomnia. Asian J Psychiatr. (2012) 5:231–5. doi: 10.1016/j.ajp.2011.12.003
47. Guo J, Wang LP, Wu X. Effect of acupuncture on daytime arousal of patients with primary insomnia. Beijing J Trad Chin Med. (2008) 27:497–9.
48. Luo WZ, Zhang QZ, Lai XS. Effect of acupuncture treatment of relieving depression and regulating mind on insomnia accompanied with depressive disorders. Zhongguo Zhen Jiu. (2010) 30:899−903.
49. Li X. Effect observation of conical stone needle on foot combined with Bian anvil for insomnia. Zhongguo Zhen Jiu. (2016) 36:181–3.
50. Wu X, Hu H, Xing J, Zhou M, Xie ZY. Effect of pricking Shenmai (BL 62) and Zhaohai (KI 6) on daytime arousal of patients with chronic insomnia: a randomized controlled trial. WJAM. (2014) 24:1–5+23. doi: 10.1016/S1003-5257(15)60019-8
51. Yang Y, Zhang J. Acupuncture at five-zang back-shu points and Geshu for depression: a randomized controlled trial. Beijing J Trad Chin Med. (2015) 34:14–7.
52. Zhang LJ, Zhao H. Clinical observation of acupunture in treating depression and effect on serum cell factors. Chinj J Inform Trad Chin Med. (2007) 14:15–7.
53. Tan TT, Wang D, Huang JK, Zhou XM, Yuan X, Liang J, et al. Modulatory effects of acupuncture on brain networks in mild cognitive impairment patients. Neural Regen Res. (2017) 12:250–8. doi: 10.4103/1673-5374.200808
54. Karst M, Reinhard M, Thum P, Wiese B, Rollnik J, Fink M. Needle acupuncture in tension-type headache: a randomized, placebo-controlled study. Cephalalgia. (2001) 21:637–42. doi: 10.1046/j.1468-2982.2001.00198.x
55. Feng XX, Huang KY, Chen L, Zhou K. Clinical efficacy of the shallow puncture and more-twirling acupuncture method in migraine treatment and its effects on serum 5-HT and β-EP levels. Technol Health Care. (2023) 31:533–40. doi: 10.3233/THC-236047
56. Jiang S, Fan X. Study of acupuncture on chronic fatigue syndrome. Trauma Crit Care Medicine. (2017) 5:350–3.
57. Wang JJ, Song YJ, Wu ZC, Chu XO, Wang QM, Wang XJ, et al. Randomized controlled clinical trials of acupuncture treatment of chronic fatigue syndrome. Zhen Ci Yan Jiu. (2009) 34:120–4.
58. Chen SS, Liu R, Wu B, Chen S, Guo F, Xue X, et al. Acupuncture on back-shu points of five zang for chronic fatigue syndrome: a randomized control trial. World J Acupunct - Moxibustion. (2018) 28:237–41. doi: 10.1016/j.wjam.2018.12.007
59. Zheng SH, Zheng SZ, Jiao JK, Ren R, Wei LL, Yang LX, et al. Randomized controlled clinical trial of back-shu point and front-mu point acupuncture for treatment of chronic fatigue syndrome. Liaon J Trad Chin Med. (2012) 39:726–8.
60. Song X-J, Zhu Y-H, Wu P, Du L, Li Z-W. Effects of electroacupuncture on sleep quality, daytime fatigue and serum cortisol in chronic insomnia. CJTCMP. (2021) 36:5693–6.
61. Li ZX, Zhang Y, Yan L da, Lai MQ, Xu HY, Wu T, et al. Effect of electroacupuncture at back-shu points of five zang on fatigue status and cortical excitability in chronic fatigue syndrome. Zhongguo Zhen Jiu. (2022) 42:1205–10.
62. Ma J, Yue S, Wang XX, Fan D, Chen HL, Zhang L. Clinical study of smokeless moxibustion for treatment of chronic fatigue syndrome. J Clini Med. (2018) 5:106–107+109.
63. Tian L, Wang J, Luo C, et al. Moxibustion at Gaohuang (BL 43) for chronic fatigue syndrome: a randomized controlled trial. Zhongguo Zhen Jiu. (2015) 35:1127–30.
64. An GX. Clinical analysis of back-shu point and front-mu point acupuncture for treatment of chronic fatigue syndrome. Chin J Basic Med Trad Chin Med. (2014) 20:970–971+991.
65. Song YJ, Wang JJ, Wang QM, Wang XH, Wu ZC, Meng H. Randomized controlled study on influence of acupuncture for pain degree of patients with chronic fatigue syndrome. Chin J Inform TCM. (2010) 17:6–8.
66. Zhu YH, Liang FR, Cheng CS, Wu X, Wang HW, Bao KY, et al. randomized controlled trial of electroacupuncture for chronic fatigue syndrome. SHJTCM. (2008) 42:48−50.
67. Ma Q, Zhou DA, Wang LP. Clinical curative effect and factor analysis of depression treated by acupuncture. Zhongguo Zhen Jiu. (2011) 31:875−8.
68. Yan M, Mao X, Wu JL. Comparison of electroacupuncture and amitriptyline in treating depression. Chin J Clini Rehabil. (2004) 8:3548–9.
69. Luo RH, Xu K, Huang YS. Clinical observations on acupuncture treatment for depression. Shanghai J Acupunct Moxibust. (2009) 28:69–71.
70. Du Y, Li G, Yan H, Zhang X, Huang L. Clinical study on needling method for regulating mental activities and soothing liver for treatment of melancholia. Zhongguo Zhen Jiu. (2005) 25:151–4.
71. Yi Y, Xu F, Xie H. Correlation between the liver meridian and the frontal lobe in depression by needling at taichong (LV3): a resting-state fMRI study. Zhongguo Zhong Xi Yi Jie He Za Zhi. (2011) 31:1044–50.
72. Duan D, Tu Y, Chen L. Assessment of effectiveness of electroacupuncture and fluoxetine for treatment of depression with physical symptoms. Zhongguo Zhen Jiu. (2008) 28:167–70.
73. Liu C, Zhao Y, Qin S, Wang X, Jiang Y, Wu W. Randomized controlled trial of acupuncture for anxiety and depression in patients with chronic insomnia. Ann Transl Med. (2021) 9:1426. doi: 10.21037/atm-21-3845
74. Ma J, Tao SP, Chu XY, et al. Efficacy and safety of acupuncture treatment on depression by unblocking du meridian and relieving depression: a randomized controlled trial. Liaon J Trad Chin Med. (2020) 47:180–2.
75. Yin P, Ma J, Wu HG, Xu SF. Clinical observation of Jie Yu Tong Fu needling for depression coupled with constipation. Shan J Acupunct Moxibust. (2018) 37:159–64.
76. Zhao FY, Xu Y, Yue LP, et al. Manual acupuncture for patients with major depressive disorder and comorbid insomnia: evidence from polysomnography and serum biomarkers. WJAM. (2020) 30:5–12. doi: 10.1016/j.wjam.2020.02.003
77. Wong YK, Wu JM, Zhou G, Zhu F, Zhang Q, Yang XJ, et al. Antidepressant monotherapy and combination therapy with acupuncture in depressed patients: a resting-state functional near-infrared spectroscopy (fNIRS) study. Neurotherapeutics. (2021) 18:2651–63. doi: 10.1007/s13311-021-01098-3
78. Duan DM, Tu Y, Jiao S, Qin W. The relevance between symptoms and magnetic resonance imaging analysis of the hippocampus of depressed patients given electro-acupuncture combined with Fluoxetine intervention - a randomized, controlled trial. Chin J Integr Med. (2011) 17:190–9. doi: 10.1007/s11655-011-0666-6
79. Gao Y, Tong QY, Ma W, Wang GT, Li YJ, Cai W, et al. Tiaoqi Jieyu acupuncture for treatment-resistant depression: a randomized controlled trial. Zhongguo Zhen Jiu. (2023) 43:417–21.
80. Yan L da, Zhou P, Lai MQ, Wu M, Zhang Y, Tang RD, et al. Effect of acupuncture combined with low frequency rTMS on comorbid mild-to-moderate depressive disorder and insomnia: a randomized controlled trial. Zhongguo Zhen Jiu. (2023) 43:374–8.
81. Zhao RZ, Qin LN, Zhao S. Therapeutic observation of An Shen Jie Lu acupuncture for the treatment of generalized anxiety disorder. Beijing J Trad Chin Med. (2018) 37:123–5.
82. Liu EJ, Zhang WL, Wang JB, Zhao FG, Bai YP. Acupuncture combined with cranial electrotherapy stimulation on generalized anxiety disorder: a randomized controlled trial. Zhongguo Zhen Jiu. (2020) 40:1187–90.
83. Yan L da, Li ZX, Zhang Y, Liang XS, Li JJ, Wu M, et al. Effect of Shugan Tiaoshen acupuncture combined with western medication on depression-insomnia comorbidity due to COVID-19 quarantine: a multi-central randomized controlled trial. Zhongguo Zhen Jiu. (2023) 43:255–60.
84. Zhang LX, Hui RT, Tang Y, Shi YZ, Xiao XJ, Zhou SY, et al. Effects of acupuncture on insomnia with depression. CJTCMP. (2020) 35:4271–4.
85. Zhao L, Zhang FW, Zhang H, Zhao Y, Zhou B, Chen WY, et al. Mild cognitive impairment disease treated with electroacupuncture: a multi-center randomized controlled trial. Zhongguo Zhen Jiu. (2012) 32:779–84.
86. Zhao L, Zhang FW, Zhang H, Luo Z, Zhu MJ, Xiao XQ, et al. Therapy of acusector tongdoutiaosui method on recognitive function of mild recognitive dysfunction patients. Chin J Gerontol. (2010) 30:1321–3.
87. Zhang H, Zhao L, Yang S, Chen Z, Li Y, Peng X, et al. Clinical observation on effect of scalp electroacupuncture for mild cognitive impairment. J Tradit Chin Med. (2013) 33:46–50. doi: 10.1016/S0254-6272(13)60099-0
88. Li YX, Wu MM, Hu SQ Li S, Wang F. Clinical efficacy and mechanism explore of Yuanluo Tongjing acupuncture method combined with western medicine in the treatment of amnestic mild cognitive impairment. CJTCMP. (2023) 38:1379–83.
89. Chen YQ, Wu HG, Yin P, Xu J, Huang ET, Xu SF. Tongdu Tiaoshen acupuncture method for mild cognitive impairment: a randomized controlled trial. Zhongguo Zhen Jiu. (2019) 39:1141−5.
90. Streng A, Linde K, Hoppe A, Pfaffenrath V, Hammes M, Wagenpfeil S, et al. Effectiveness and tolerability of acupuncture compared with metoprolol in migraine prophylaxis. Headache. (2006) 46:1492–502. doi: 10.1111/j.1526-4610.2006.00598.x
91. Zhang YJ, Liu L, Jing XH, Wang LP. Clinical study on the effect of acupuncture on heat pain threshold in migraine without aura. Chin J Pain Med. (2019) 25:276–81.
92. Wang Y, Xue CC, Helme R, Da Costa C, Zheng Z. Acupuncture for Frequent Migraine: A Randomized, Patient/Assessor Blinded, Controlled Trial with One-Year Follow-Up. Evid Based Complement Alternat Med. (2015) 2015:920353. doi: 10.1155/2015/920353
93. Linde K, Streng A, Jürgens S, Hoppe A, Brinkhaus B, Witt C, et al. Acupuncture for patients with migraine: a randomized controlled trial. JAMA. (2005) 293:2118–25. doi: 10.1001/jama.293.17.2118
94. Melchart D, Streng A, Hoppe A, Brinkhaus B, Witt C, Wagenpfeil S, et al. Acupuncture in patients with tension-type headache: randomised controlled trial. BMJ. (2005) 331:376–82. doi: 10.1136/bmj.38512.405440.8F
95. Allais G, De Lorenzo C, Quirico PE, Lupi G, Airola G, Mana O, et al. Non-pharmacological approaches to chronic headaches: transcutaneous electrical nerve stimulation, lasertherapy and acupuncture in transformed migraine treatment. Neurol Sci. (2003) 24:S138–142. doi: 10.1007/s100720300062
96. Cai YW, Pei J, Fu QH, Xu J, Shen FJ, Zhan YJ, et al. Electroacupuncture at Siguan points for migraine of liver yang hyperactivity: a randomized controlled trial. Zhongguo Zhen Jiu. (2022) 42:498–502.
97. Wang J, Qin X, Xie W, Wang W. Migraine without aura treated with balance acupuncture therapy:a randomized controlled trial. Zhongguo Zhen Jiu. (2017) 37:805–9.
98. Zheng H, Gao T, Zheng QH, Lu LY, Hou TH, Zhang SS, et al. Acupuncture for patients with chronic tension-type headache: a randomized controlled trial. Neurology. (2022) 99:e1560–9. doi: 10.1212/WNL.0000000000200670
99. Liu L, Lyu TL, Fu MY, Wang LP, Chen Y, Hong JH, et al. Changes in brain connectivity linked to multisensory processing of pain modulation in migraine with acupuncture treatment. Neuroimage Clin. (2022) 36:103168. doi: 10.1016/j.nicl.2022.103168
100. Karst M, Rollnik JD, Fink M, Reinhard M, Piepenbrock S. Pressure pain threshold and needle acupuncture in chronic tension-type headache–a double-blind placebo-controlled study. Pain. (2000) 88:199–203. doi: 10.1016/S0304-3959(00)00315-8
101. Musil F, Pokladnikova J, Pavelek Z, Wang B, Guan X, Valis M. Acupuncture in migraine prophylaxis in Czech patients: an open-label randomized controlled trial. Neuropsychiatr Dis Treat. (2018) 14:1221–8. doi: 10.2147/NDT.S155119
102. Ferro EC, Biagini AP, da Silva ÍEF, Silva ML, Silva JRT. The combined effect of acupuncture and Tanacetum parthenium on quality of life in women with headache: randomised study. Acupunct Med. (2012) 30:252–7. doi: 10.1136/acupmed-2012-010195
103. Xu S, Yu L, Luo X, Wang M, Chen G, Zhang Q, et al. Manual acupuncture versus sham acupuncture and usual care for prophylaxis of episodic migraine without aura: multicentre, randomised clinical trial. BMJ. (2020) 368:m697. doi: 10.1136/bmj.m697
104. Yin Y, Zhang YP, Yang ZX Li JY. Penetration needling on complementary acupoints for insomnia. WJAM. (2017) 27:8–12. doi: 10.1016/S1003-5257(18)30004-7
105. Liu Y, Feng H, Liu W, Mao H, Mo Y, Yin Y, et al. Regulation action and nerve electrophysiology mechanism of acupuncture on arousal state in patients of primary insomnia. Zhongguo Zhen Jiu. (2017) 37:19–23.
106. Pan Y, Luo J, Zhang HL. Study on the effect of acupuncture at Sishencong (EX-HN 1) and Baihui (GV 20) on the serum amino acids neurotransmitters of insomnia patients. WJAM. (2017) 27:23–7. doi: 10.1016/S1003-5257(17)30095-8
107. Liu F, Chen TY Li CY. Clinical efficacy of long-time acupuncture at Sishencong (EX-HN1) during Shen-You time for insomnia. Xinli Yisheng. (2016) 22:140–2.
108. Wu WZ, Zheng SY, Liu CY, Qin S, Wang XQ, Hu JL, et al. Effect of Tongdu Tiaoshen acupuncture on serum GABA and CORT levels in patients with chronic insomnia. Zhongguo Zhen Jiu. (2021) 41:721–4.
109. Ji X, Wang Q, Zhu W. Expressions of neurotransmitters in patients of insomnia differentiated as liver stagnation transforming into fire treated with acupuncture. Zhongguo Zhen Jiu. (2015) 35:549–52.
110. Wang YP, Wen X, Feng XL, He TY. Yinyang Ruyin acupuncture on refractory insomnia: a randomized controlled trial. Zhongguo Zhen Jiu. (2019) 39:1155–9.
111. Wang J, Wang J, Wang L, Zhang Y. Senile insomnia treated with integrated acupuncture and medication therapy: a randomized controlled trial. Zhongguo Zhen Jiu. (2015) 35:544–8.
112. Zhang X, Han Z, Su T, Di L, Wang Y, Luo G, et al. Combination of acupuncture improves the effect of estazolam on senile insomnia. Int J Clin Exp Med. (2019) 12:13408–17.
113. Zhao JY, Wang FC. Effects of acupuncturing Sanyinjiao (SP6) on PSQI and PSG in patients with primary insomnia. CJTCMP. (2018) 33:5683–6.
114. Wang XQ, Qin S, Wu WZ, Liu CY, Shang HT, Wan QY, et al. Effect of electroacupuncture on serum melatonin and dopamine in aged insomnia. Zhongguo Zhen Jiu. (2021) 41:501–4.
115. Wang YK Li T, Ha LJ, Lv ZW, Wang FC, Wang ZH, et al. Effectiveness and cerebral responses of multi-points acupuncture for primary insomnia: a preliminary randomized clinical trial and fMRI study. BMC Complement Med Ther. (2020) 20:254. doi: 10.1186/s12906-020-02969-6
116. Xi HQ, Wu WZ, Liu CY, Wang XQ, Qin S, Zhao YN, et al. Effect of acupuncture at Tiaoshen acupoints on hyperarousal state in chronic insomnia. Zhongguo Zhen Jiu. (2021) 41:263–7.
117. Xiao BB, Luo XJ, Shen YT. Efficacy observation on refractory insomnia treated with the balance needling therapy. Zhongguo Zhen Jiu. (2013) 33:101–4.
118. Yin X, Li W, Wu H, Dong B, Ma J, Li S, et al. Efficacy of electroacupuncture on treating depression-related insomnia: a randomized controlled trial. Nat Sci Sleep. (2020) 12:497–508. doi: 10.2147/NSS.S253320
119. Zhao YN, Wu WZ, Wang XQ, Xu YQ, Jiang YY, Liu CY. To observe the effect of Tiaoshen acupuncture on hyperarousal in patients with chronic insomnia. World J Tradit Chin Med. (2021) 23:2538–43.
120. Chen XQ, Huang B, Wu X. Acupuncture for sleep disorder in chronic fatigue syndrome: a randomized controlled clinical trial. Lishizhen Med Materia Medica Res. (2015) 26:1669–72.
121. Luo D, Wu YN, Cai L, Li MY, Duan Q, Ma R, et al. Clinical efficacy of liver-soothing and mind-regulating acupuncture for depression related insomnia. Chin J Gerontol. (2017) 37:3837–9.
122. Yeung WF, Chung KF, Zhang SP, Yap TG, Law ACK. Electroacupuncture for primary insomnia: a randomized controlled trial. Sleep. (2009) 32:1039–47. doi: 10.1093/sleep/32.8.1039
123. Zhang LX, Zhou SY, Zhen QH, Deng YL, Hui RT, Hu YP, et al. Clinical randomized control study of acupuncture treatment for insomnia with anxiety. World Chinese Medicine. (2018) 13:1570–4.
124. Dong B, Chen ZQ, Ma J, Yin P, Li SS, Xu SF. Clinical curative observation of applying acupuncture at Yintang (EX-HN3), Baihui (Du20) and Dazhui (Du14) with periosteal puncture method in the treatment of primary insomnia. J Sich Trad ChinMed. (2018) 36:176–8.
125. Zhao FY, Zhang ZY, Xia XJ, Fang H, Ying-xia H, Hai-xia Y, et al. Memory response to manual acupuncture in chronic insomniacs: evidence from event-related potentials. J Acup Tuina Sci. (2018) 16:382–8. doi: 10.1007/s11726-018-1078-3
126. Li Y, Zheng DC. Clinical research of abdominal acupuncture for insomnia. Liaon J Trad Chin Med. (2010) 37:914–6.
127. Huo YS, Chen ZY, Yin XJ, Jiang TF, Wang GL, Cui YX, et al. Tiaoshen acupuncture for primary insomnia: a pilot randomized controlled trial. Zhongguo Zhen Jiu. (2023) 43:1008–13.
128. Zhang L, Deng Y, Hui R, Tang Y, Yu S, Li Y, et al. The effects of acupuncture on clinical efficacy and steady-state visual evoked potentials in insomnia patients with emotional disorders: a randomized single-blind sham-controlled trial. Front Neurol. (2022) 13:1053642. doi: 10.3389/fneur.2022.1053642
129. Chen Z, Jiang T, Yin X, Li B, Tan Z, Guo J. The increased functional connectivity between the locus coeruleus and supramarginal gyrus in insomnia disorder with acupuncture modulation. Front Neurosci. (2023) 17:1131916. doi: 10.3389/fnins.2023.1131916
130. Feng H, Liu Y, Xu H, Liu YH, Chen GL, Liu WJ. Effect of acupuncture and estazolam on episodic memory and sleep structure in patients with chronic insomnia disorder: a randomized controlled trial. Zhongguo Zhen Jiu. (2020) 40:707–12.
131. Yin X, Gou M, Xu J, Dong B, Yin P, Masquelin F, et al. Efficacy and safety of acupuncture treatment on primary insomnia: a randomized controlled trial. Sleep Med. (2017) 37:193–200. doi: 10.1016/j.sleep.2017.02.012
132. Guyatt GH, Osoba D, Wu AW, Wyrwich KW, Norman GR. Clinical Significance Consensus Meeting Group. Methods to explain the clinical significance of health status measures Mayo. Clin Proc. (2002) 77:371–83. doi: 10.4065/77.4.371
133. Fang Y, Yue BW, Ma HB, Yuan YP. Acupuncture and moxibustion for chronic fatigue syndrome: a systematic review and network meta-analysis. Medicine. (2022) 101:e29310. doi: 10.1097/MD.0000000000029310
134. Zhang Z, Li S, Meng H, Wang Y, Zhang Y, Wu M, et al. Efficacy and safety of acupuncture in the treatment of depression: A systematic review of clinical research. Anat Rec. (2021) 304:2436–53. doi: 10.1002/ar.24783
135. He W, Li M, Han X, Zhang W. Acupuncture for mild cognitive impairment and dementia: an overview of systematic reviews. Front Aging Neurosci. (2021) 13:647629. doi: 10.3389/fnagi.2021.647629
136. Giovanardi CM, Cinquini M, Aguggia M, Allais G, Campesato M, Cevoli S, et al. Acupuncture vs. pharmacological prophylaxis of migraine: a systematic review of randomized controlled trials. Front Neurol. (2020) 11:576272. doi: 10.3389/fneur.2020.576272
137. Kim SA, Lee SH, Kim JH, van den Noort M, Bosch P, Won T, et al. Efficacy of acupuncture for insomnia: a systematic review and meta-analysis. Am J Chin Med. (2021) 49:1135–50. doi: 10.1142/S0192415X21500543
138. Hollifield M, Cocozza K, Calloway T, Lai J, Caicedo B, Carrick K, et al. Improvement in long-COVID symptoms using acupuncture: a case study. Medical Acup. (2022) 34:172–6. doi: 10.1089/acu.2021.0088
139. Trager RJ, Brewka EC, Kaiser CM, Patterson AJ, Dusek JA. Acupuncture in multidisciplinary treatment for post-COVID-19 syndrome. Medical Acup. (2022) 34:177–83. doi: 10.1089/acu.2021.0086
140. Putilina MV, Teplova NV, Bairova KI, Petrikeeva AE, Shabalina NI. The result of prospective randomized study CITADEL - the efficacy and safety of drug cytoflavin in postcovid rehabilitation. Zh Nevrol Psikhiatr Im S S Korsakova. (2021) 121:45–51. doi: 10.17116/jnevro202112110145
141. McIntyre RS, Phan L, Kwan ATH, Mansur RB, Rosenblat JD, Guo Z, et al. Vortioxetine for the treatment of post-COVID-19 condition: a randomized controlled trial. Brain. (2024) 147:849–57. doi: 10.1093/brain/awad377
142. Lau RI, Su Q, Lau ISF, Ching JYL, Wong MCS, Lau LHS, et al. A synbiotic preparation (SIM01) for post-acute COVID-19 syndrome in Hong Kong (RECOVERY): a randomised, double-blind, placebo-controlled trial. Lancet Infect Dis. (2024) 24:256–65. doi: 10.1016/S1473-3099(23)00685-0
143. Cunqing Y, Fengmei L, Guiping Y, Yufeng H, Shuangbin Z, Jianghua W, et al. Effectiveness of Xiaoyao capsule on sleep disorders and mood disturbance in patients in recovery from coronavirus disease 2019: a randomized controlled trial. J Tradit Chin Med. (2023) 43:343–51.
144. Li L, An XD, Zhang Q, Tao JX, He J, Chen Y, et al. Shumian capsule improves symptoms of sleep mood disorder in convalescent patients of Corona Virus Disease 2019. J Tradit Chin Med. (2021) 41:974–81.
145. Tartibian B, Khayat SMA, Maleki BH, Chehrazi M. The Effects of exercise training on recovery of biochemical and hematological outcomes in patients surviving COVID-19: a randomized controlled assessor-blinded trial. Sports Med Open. (2022) 8:152. doi: 10.1186/s40798-022-00546-4
146. Samper-Pardo M, León-Herrera S, Oliván-Blázquez B, Méndez-López F, Domínguez-García M, Sánchez-Recio R. Effectiveness of a telerehabilitation intervention using ReCOVery APP of long COVID patients: a randomized, 3-month follow-up clinical trial. Sci Rep. (2023) 13:7943. doi: 10.1038/s41598-023-35058-y
147. Bäumler P, Zhang W, Stübinger T, Irnich D. Acupuncture-related adverse events: systematic review and meta-analyses of prospective clinical studies. BMJ Open. (2021) 11:e045961. doi: 10.1136/bmjopen-2020-045961
148. Zhong LLD, Wong YP, Leung CY, Peng B, Lin ZX, Wong Taam VC, et al. Effects of Chinese medicine for COVID-19 rehabilitation: a multicenter observational study. Chin Med. (2022) 17:99. doi: 10.1186/s13020-022-00654-z
149. Liu W, Guo S, Wang F, Hao Y. Understanding of guidance for acupuncture and moxibustion interventions on COVID-19 (Second edition) issued by CAAM. World J Acup - Moxibustion. (2020) 30:1–4. doi: 10.1016/j.wjam.2020.03.005
150. Crook H, Raza S, Nowell J, Young M, Edison P. Long covid—mechanisms, risk factors, and management. BMJ. (2021) 374:n1648. doi: 10.1136/bmj.n1648
Keywords: acupuncture, long COVID, fatigue, depression, anxiety, headache, insomnia, cognitive impairment
Citation: Lam WC, Wei D, Li H, Yao L, Zhang S, Lai MXY, Zheng Y, Yeung JWF, Lau AYL, Lyu A, Bian Z, Cheung AM and Zhong LLD (2024) The use of acupuncture for addressing neurological and neuropsychiatric symptoms in patients with long COVID: a systematic review and meta-analysis. Front. Neurol. 15:1406475. doi: 10.3389/fneur.2024.1406475
Received: 25 March 2024; Accepted: 01 July 2024;
Published: 19 July 2024.
Edited by:
Andrea Martinuzzi, Eugenio Medea (IRCCS), ItalyReviewed by:
Mingxiao Yang, Dana-Farber Cancer Institute, United StatesCopyright © 2024 Lam, Wei, Li, Yao, Zhang, Lai, Zheng, Yeung, Lau, Lyu, Bian, Cheung and Zhong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Angela M. Cheung, YW5nZWxhLmNoZXVuZ0B1aG4ub24uY2E=; Linda L. D. Zhong, bGluZGEuemhvbmdAbnR1LmVkdS5zZw==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.