
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol., 26 July 2024
Sec. Neurorehabilitation
Volume 15 - 2024 | https://doi.org/10.3389/fneur.2024.1382696
This article is part of the Research TopicAssessment and Treatment Interventions for Traumatic Brain InjuryView all 21 articles
Background: After craniotomy, patients require rehabilitation efforts for the recovery process, and neurologists are mostly engaged for that (in the management of post-craniotomy complications). However, neurologists are not always available for care after neurosurgery during follow-up (situation of our institute). The objectives of the study were to compare the effects of two different types of care (nurse-led and neurologist-led) on various long-term outcomes in patients who have undergone craniotomy due to traumatic brain injuries.
Methods: Electronic medical records of patients (aged ≥18 years) who underwent craniotomy for traumatic brain injuries and their caregivers were extracted and retrospectively reviewed. Patients received nurse-led care (NL cohort, n = 109) or neurologist-led care (GL cohort, n = 121) for 6 months after craniotomy.
Results: Before the nurse-or neurologist-led care (BC), all patients had activities of daily living (ADL) ≤ 11, ≤ 50 quality of life (QoL), and 69% of patients had definitive anxiety, 87% of patients had definitive depression, and all caregivers had Zarit Burden interview scores ≥50. Nurse-led post-surgical care was associated with improved ADL and QoL, relieved anxiety and depression of patients, relieved the burden on caregivers, and the higher overall satisfaction of patients and their caregivers after 6-months of care (AC) as compared to their BC condition (p < 0.05) and also compared to those of patients in the GL cohort under AC condition (p < 0.01). Patients in the GL cohort reported pressure sores (p = 0.0211) and dizziness [15 (12%) vs. 5 (5%)] after craniotomy during follow-up than those in the NL cohort.
Conclusion: ADL, QoL, and psychological conditions of patients who undergo craniotomy for traumatic brain injuries must be improved and the burdens of their caregivers must be relived. Not only is the care provided by nursing staff equivalent to that offered by neurologists, but in some aspects, it is superior for patients who have undergone craniotomy for traumatic brain injuries and their caregivers during follow-up.
China has a higher number of patients with traumatic brain injuries than most other countries (1). Traumatic brain injury is a major condition that requires several healthcare professionals to provide care in the trauma department (2). In addition, prehospital facilities are insufficient for Chinese emergency care (3). Craniotomy is performed to control intracranial pressure in patients with severe traumatic brain injuries (4). In addition to general postoperative adverse effects (e.g., nausea, vomiting, dizziness), coma, paralysis, mental disabilities, and personality changes are generally reported threats to traumatic brain injuries after craniotomy (2, 5). Craniotomy places patients with traumatic brain injuries at risk of many serious complications, which may affect the outcomes of surgery (6).
Nursing interventions are crucial after neurosurgery and related to patient safety (7). After craniotomy, if nursing care is not sufficiently provided to the patients and the disease conditions of patients are not identified properly and timeously, the possible treatment would be affected, possibly resulting in cognitive impairment or death (8). Improper nursing poses a serious threat after craniotomy in patients with traumatic brain injuries (9). After craniotomy, patients require rehabilitation efforts for the recovery process (10) and neurologists are mostly engaged in the management of post-craniotomy complications (11). However, neurologists are not always available for care after neurosurgery during follow-up (situation of our institute). In addition, in COVID-19 pandemic surgical disciplines have faced serious issues including patients who required surgical care and postoperative follow-up care (12). An important issue is covered as health systems are facing a dire shortage of staff throughout the world. This deserves further scrutiny as to which extent process management can be improved. The findings indicate that the interpersonal skills and communication style of nurses may be more appreciated by patients and caregivers (13). Excellent patient outcomes and high patient satisfaction are two main pillars of the high-value medical care for neurosurgical care of patients (14). In many places, notably the US, post-operative care is typically performed by neurosurgeons with neurologists rarely contributing long-term. Additionally, long-term care varies vastly between settings, largely dependent on infrastructure for patients with a variety of neurodegenerative diseases.
The aim of the retrospective study is to compare the effects of two different types of care (nurse-led and neurologist-led) on various the long-term outcomes (daily living activities (ADL), quality of life (QoL), depression, and anxiety of patients and burden of their caregivers) in patients who have undergone craniotomy due to traumatic brain injuries.
Patients (aged ≥18 years) who underwent craniotomy for traumatic brain injuries were included in the study. Patient underwent decompressive hemicraniectomy, or craniotomy with cranial flap repositioning, or both.
Patients with incomplete details were excluded from the study.
A total of 109 patients received nurse-led care after craniotomy for 6 months (NL cohort). A total of 121 patients received neurologist-led care for 6 months after craniotomy (GL cohort). In addition to care, all patients received regular treatment prescribed by a consulting neurosurgeon.
Every day a follow-up visits made in ward by neurologist. In the GL cohort medical follow-up is provided by the neurologist alone, and/or by the neurologist assisted by a neurosurgeon and by a physical medicine physician. Neurologist-led care include usual hospital care (counseling of patients and their caregivers regarding threats and adverse effects of surgeries and injuries) and follow-up of patients (routine check-up). During hospital stay minimum 5 min/day provided to patients by neurologists.
Every day at least two follow-up visits made in ward by staff nurse. In NL cohort medical follow-up is provided by staff nurse oneself. Nurses are minimum postgraduate in nursing care and have minimum 3 years of experiences. Nursing-led care include counseling and education of patients and their caregivers regarding threats and adverse effects of surgeries and injuries. During hospital stay minimum 10 min/day provided to patients by nurses.
After discharge from the hospital, follow-up visits, and telephone consultations with caregivers, and the patients received care from nurses or neurologists. There were no restrictions on telephone consultations with nurses or neurologists for the patients and their caregivers. During the follow-up visit, patients and their caregivers were provided care, counselling, and related instructions for half an hour by a nurse or neurologist. The selection of nurse-led care and neurologist-led care for patients is based on availabilities of professionals in the institutes (in our institutes neurologists are in short to provide follow-up care). There was no crossover between nurse- and neurologist-led aftercare.
GCS score was evaluated before craniotomy. GCS scores were between 3 and 15, with 3 being the worst and 15 being good (15).
ADL was evaluated for six basic activities: toileting, bathing, dressing, eating, moving, and continence of defecation. Each item is scored from 1 to 3 (1 = complete dependence, 2 = partial dependence, and 3 = complete independence). The total score is 18. The higher the score, the higher the ADL (16).
Physical, emotional, and social functions; somatic pain; general health status; energy; and mental health were used to evaluate QoL. The total score ranged from 0 to 100. The higher the score, the higher the QoL (17).
Seven items were evaluated using the Hospital Anxiety and Depression Scale. Each item has a score ranging from 1 to 3. The total scores for anxiety and depression were 21. The higher the score, the higher the anxiety and depression. A score of >7 was considered anxiety and depression, and a score of >11 was considered definitive anxiety and definitive depression (18).
Questionnaires were administered to caregivers to evaluate their psychological burden due to the patient’s condition. It consists of a total of 22 items, and each item is rated on a 0 to 4 scale. The total score was 88, with a higher score indicating a higher burden on caregivers (19).
ADL, QoL, Hospital Anxiety and Depression Scale, and Zarit Burden interview were performed after craniotomy before any professional-led care (nurse-led care or neurologist-led care, BC) and after 6-months of any professional-led care (nurse-led care or neurologist-led care, AC).
During the 6-months of any professional-led care, any adverse effects due to surgery and/or treatments were noticed and analyzed.
The institute has a print format to evaluate satisfaction. This included emergency care, pre-surgery counseling, surgery, and professional-led post-surgical care. Each item had a score of 0, 1, 2, 3, and 4. 0, completely dissatisfied; 1, dissatisfied; 2, partially satisfied; 3, satisfied; 4, completely satisfied. The total score is 16. The higher the score, the higher the overall satisfaction of patients and caregivers. The overall satisfaction score was evaluated after professional-led postsurgical care for 6 months.
InStat 3.01 (GraphPad Software Inc., San Diego, CA, United States) was used for the statistical analysis. Categorical, continuous normal, and continuous non-normal variables are presented as frequencies with percentages in parentheses, mean ± standard deviation (SD), and medians with Q3–Q1 in parentheses, respectively. All results were considered significant if the p-value was less than 0.05. The Kolmogorov–Smirnov method was adopted to check the normality of continuous variables. If at least one column failed in the normality test with p < 0.05, a nonparametric test (Mann–Whitney test or Kruskal-Wallis’ test) was performed; otherwise, parametric tests (paired t-test or unpaired t-test) were performed for continuous variables. Fisher’s exact test or chi-square test (χ2-test) was used for the statistical analysis of categorical variables. Dunn’s multiple comparison test was used for post hoc analysis. The Quartile Calculator1 was used to calculate the Q3 (third quartile) and Q1 (first quartile) values. All results were considered significant if the p-value was less than 0.05.
For retrospective study electronic medical records of patients were searched to extract data. From January 18, 2019, to February 20, 2023, 245 patients (age ≥ 18 years) underwent craniotomy for traumatic brain injuries at the Shanxi Bethune Hospital, Taiyuan, Shanxi, China and the referring institutes. Data from 15 patients were incomplete in hospital records. Therefore, these patients were excluded from this study. ADL, QoL, the Hospital Anxiety and Depression Scale of patients, Zarit Burden interview of caregivers, and the overall satisfaction score of patients and caregivers for a total of 230 patients and their caregivers were included in the study. The flowchart of the study is shown in Figure 1.
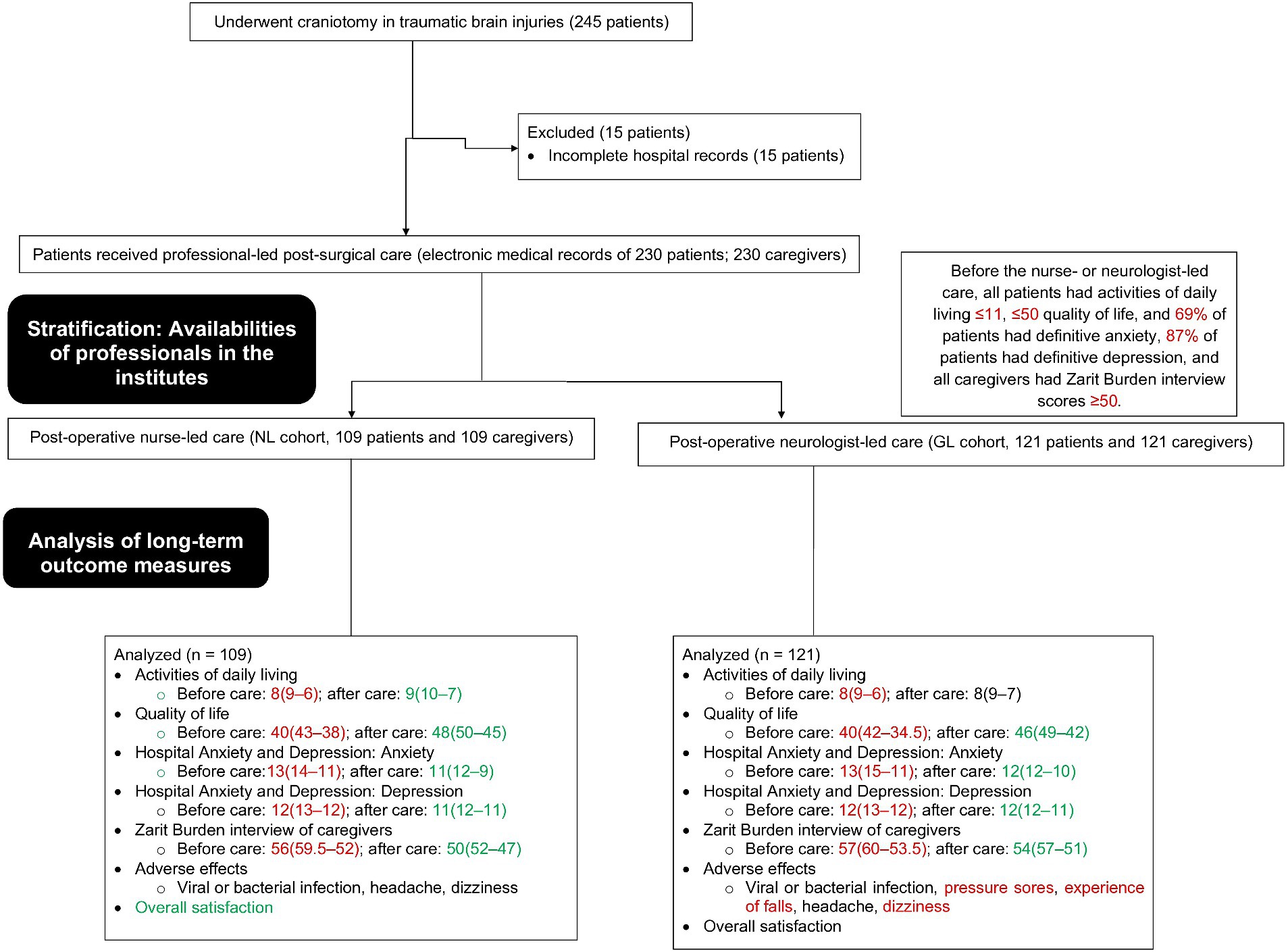
Figure 1. The study flow chart. Red color indicates worse results. Green color indicates favorable results. Black color indicates not favorable but not worse results.
The number of male patients was higher than that of female patients. Most patients had motor vehicle accidents due to traumatic brain injuries. All patients had a GCS score < 10 before the operation. Most of the patients underwent surgery on the dominant side. At BC, all patients had an ADL of 11 or fewer, all patients had a QoL of 50 or less, and most of them had definitive anxiety (69%) and depression (87%). Age, sex, reason for traumatic brain injuries, Glasgow Coma Scale score before the operation, surgery side, ADL, QoL, anxiety, and depression of patients were statistically similar between cohorts at BC (p > 0.05, Table 1).
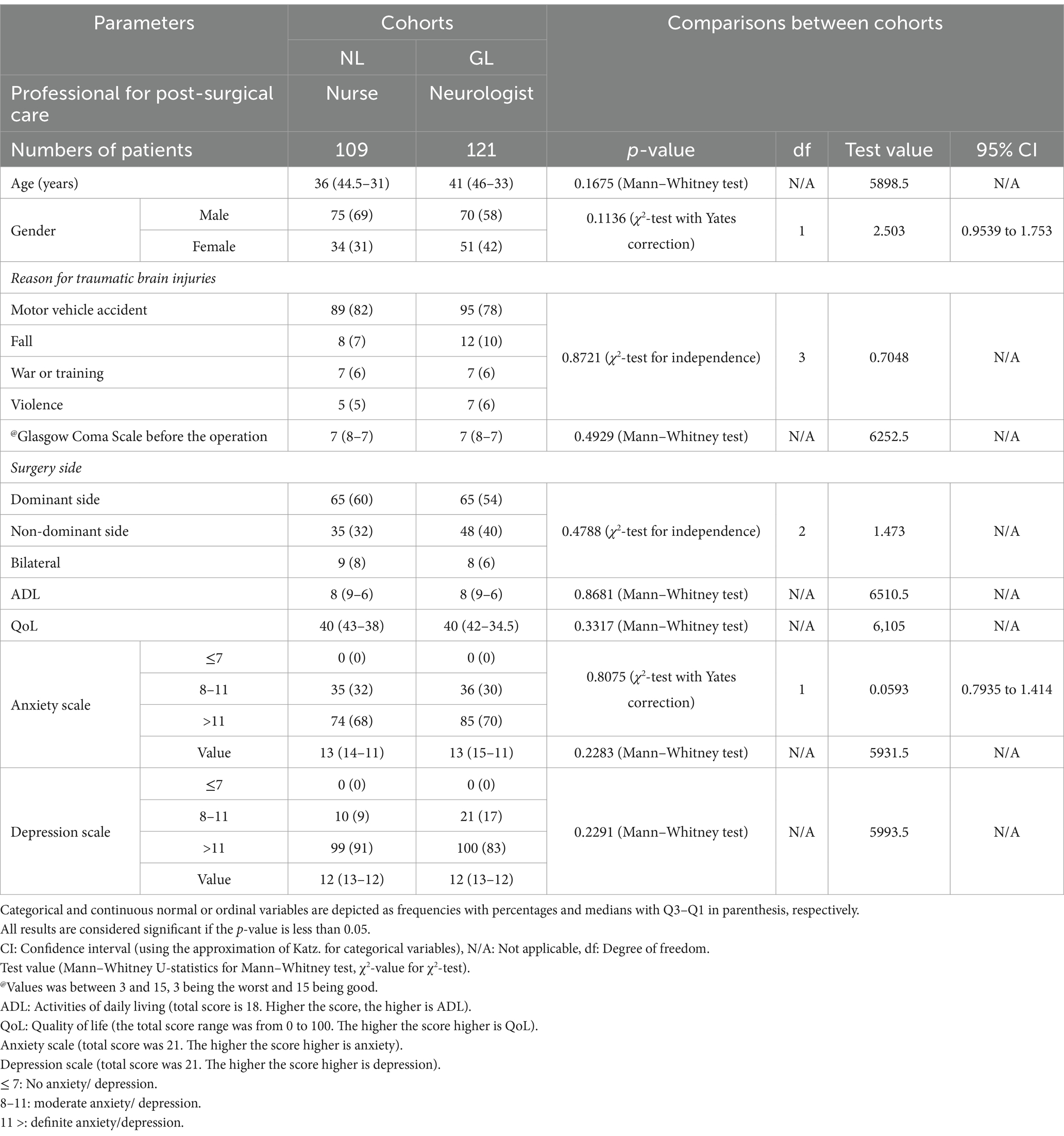
Table 1. Demographic and clinical conditions of patients after craniotomy for traumatic brain injuries before professional-led post-surgical care.
All caregivers had Zarit Burden Interview scores of 50 or more at the BC. One patient had a caregiver. Most of the caregivers were spouses. The details of comorbidities of caregivers were not available in the hospital records. Age, sex, education, and Zarit Burden interview scores of caregivers were statistically the same between both cohorts (p > 0.05, Table 2).
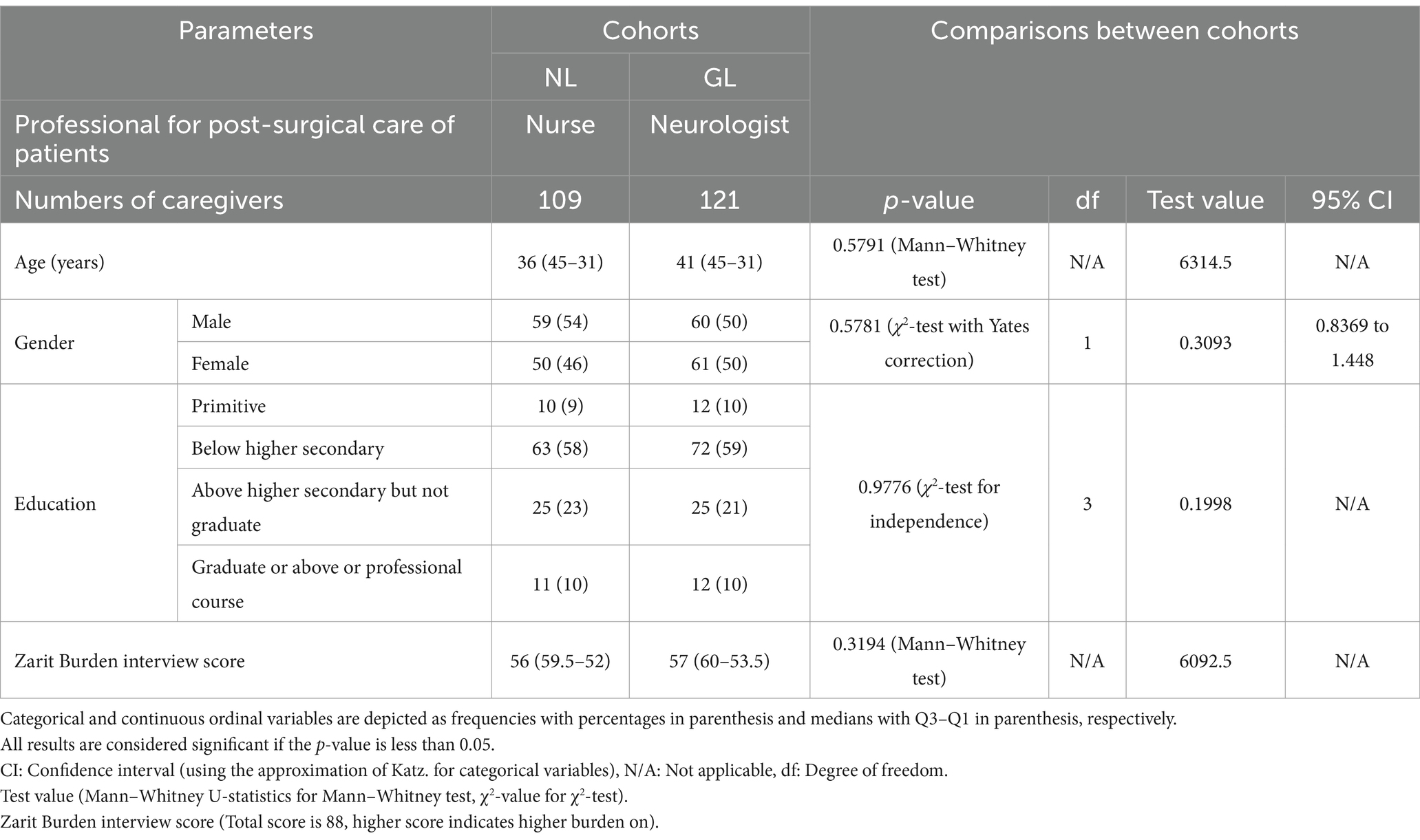
Table 2. Available demographic and clinical conditions of caregivers of patients after craniotomy for traumatic brain injuries before professional-led post-surgical care of patients.
Nurse-led post-surgical care was associated with improved ADL of patients with AC condition as compared to their BC condition and also compared to those of the GL cohort in the AC condition. Neurologist-led care was not successful in improving ADL at AC condition compared with their BC condition. Nurse-led care and neurologist-led care were associated with improved QoL, relieved anxiety and depression in patients, and relieved the burden on caregivers of patients at AC condition compared to their BC conditions. In addition, patients in the NL cohort had a better QoL and less anxiety than those in the GL cohort in the AC condition. Caregivers of patients in the NL cohort had fewer burdens than those of caregivers of patients in the GL cohort in the AC condition. The overall satisfaction scores of patients and their caregivers were higher for nurses than that scores for neurologists. The details of the outcome measure of patients and their caregivers after craniotomy for traumatic brain injuries before and after professional-led post-surgical care are presented in Table 3.
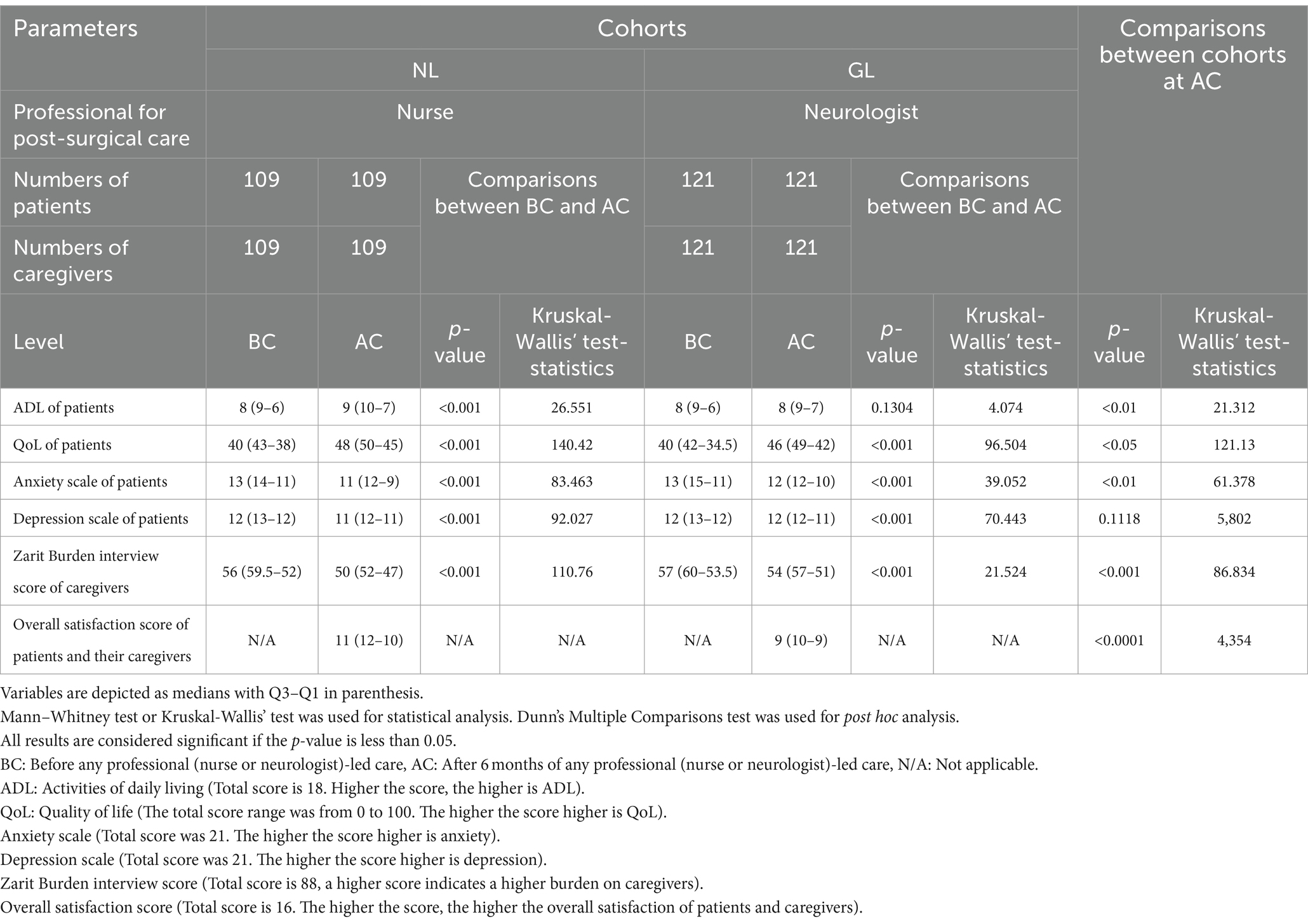
Table 3. The outcome measures of patients and their caregivers after craniotomy for traumatic brain injuries before and after professional-led post-surgical care.
Nurse-led care and neurologist-led care both successfully decreased anxiety and depression from definite anxiety (score > 11) to moderate anxiety (score 8–11) in the AC condition compared with their BC conditions. In addition, nurse-led care was more successful in decreasing the anxiety of patients with definite anxiety (score > 11) to moderate anxiety (score 8–11) in the AC condition than those did by neurologist-led care. Nurse-led care or neurologist-led care failed to complete reduce anxiety or depression in patients (score ≤ 7) at the AC condition. The details of the hospital anxiety and depression scales are presented in Table 4.
None of the patients died during the study. Headache was commonly reported in patients in both cohorts. Pressure sores, dizziness, and experience of falls were reported to be higher in patients in the GL cohort than in those in the NL cohort. The total numbers of adverse events and adverse effects per patient were higher in patients in the GL cohort than those in the NL cohort. The details of adverse effects during the six months of any professional-led care and follow-up period (extra six months) are reported in Table 5.
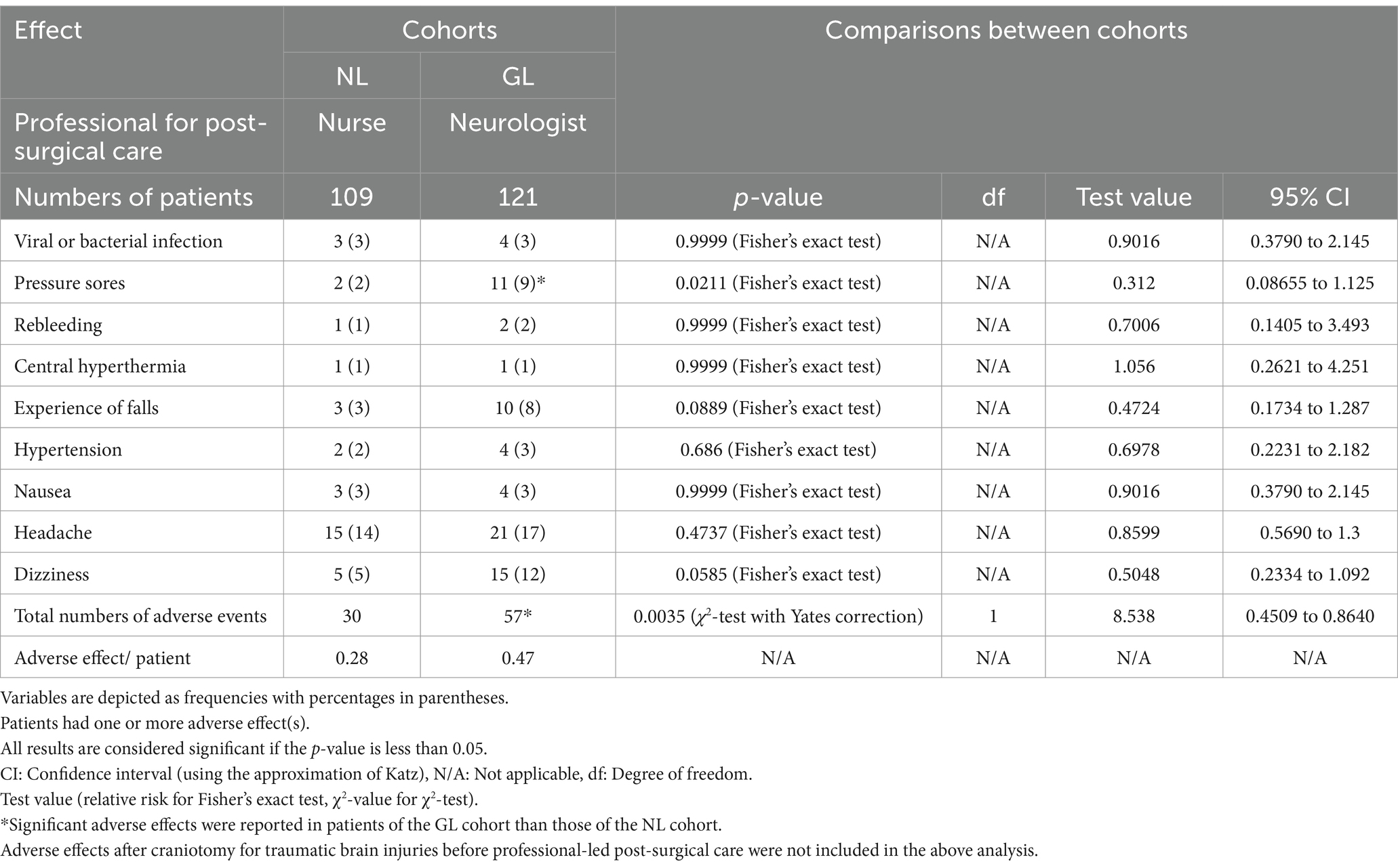
Table 5. The details of adverse effects during the six months of any professional-led care and follow-up period.
At BC condition, all patients had ≤11 ADL and ≤ 50 QoL, and most patients had definitive anxiety and depression. In addition, at BC condition all caregivers of patients had Zarit Burden interview scores ≥50. After craniotomy for traumatic brain injuries, the patients had worse ADL, QoL, anxiety, and depression. The outcome results of the patients after craniotomy for traumatic brain injuries are consistent with those of a case–control study (9), a propensity matching study (2), an observational study (17), and a pilot study (7). ADL and QoL of patients after craniotomy for traumatic brain injuries must be improved and anxiety and depression of patients after craniotomy for traumatic brain injuries must be relieved. In addition, after craniotomy for traumatic brain injuries, the burden on caregivers of patients must be relieved.
Nurse-led care improved ADL and QoL and relieved anxiety and depression in patients with AC conditions as compared to their BC conditions and those of patients of the GL under AC conditions. The results of the NL cohort were consistent with those of a case–control study (9) and a trial on multiple sclerosis (13). In addition, nurse-led care relieved the burden on caregivers of patients with AC conditions compared to the BC conditions and those of caregivers of patients with the GL cohort under AC conditions. Nurse-led care and neurologist-led care are associated with the improvement of ADL and QoL, relief of anxiety and depression in patients after craniotomy for traumatic brain injuries, and relief of burden on caregivers. Moreover, nurse-led care is superior to neurologist-led care in the follow-up of patients after craniotomy for traumatic brain injuries, regarding the improvement of ADL, QoL, and psychological conditions of patients and burdens of their caregivers. Frequent visits of nurses to patients and caregivers than those of neurologists are the reasons for these results.
Patients in the GL cohort reported pressure sores, dizziness, experience of falls, higher numbers of total adverse effects, and higher adverse effects per patient during six months of care and a follow-up period than those in the NL cohort. Neurologists are not always available for care after neurosurgery during follow-up to provide mobility to patients (situation of our institute). This would lead to a high risk of pressure sores, falls while walking, and dizziness in patients of the GL cohorts (20). Nurse-led care during follow-up decreases adverse effects after craniotomy for traumatic brain injuries compared with neurologist-led follow-up care.
The overall satisfaction scores of patients and their caregivers were higher for nurses than for neurologists. Compared with neurologists, nurses provide more time to patients and their caregivers. The results of the overall satisfaction scores of patients and their caregivers of the current study are consistent with a trial on multiple sclerosis (13). In addition, nurses have better communication skills and require fewer waiting times than neurologists (21). Nurses provide advanced skills to various complex medical conditions, with potential to enhance the health, cognitive functioning, and quality of life (22). Nurses can also develop interpersonal relationships. This would increase the satisfaction of the patients and caregivers.
These interpretations of the results cannot be extrapolated as an indication of the best treatment for the recovery of these patients, which must include multidisciplinary management, where in addition to neurological doctors and nurses, many other professionals participate, such as neuropsychologists, rehabilitators, physiotherapists, speech therapists, etc. Each of them will contribute in each area to try to maximize the possibilities of functional recovery. However, it is obvious that the local context may prevent having all the resources available and that these are optimized and, in this situation, directed in the best possible way.
Both nurse-led and neurologist-led care were unsuccessful in completely removing anxiety or depression in patients (score ≤ 7) at AC. This suggests that additional treatment interventions may be needed to address these (anxiety and depression) issues of patients.
In the current study research outcome measures such as ADL, QoL, the Hospital Anxiety and Depression Scale of patients, and Zarit Burden interview of caregivers, as well as the overall satisfaction score of patients and caregivers were evaluated. The objectives of study were to evaluate long-term outcome measures of patients who have undergone craniotomy due to traumatic brain injuries. These (ADL, QoL, the Hospital Anxiety and Depression Scale of patients, and Zarit Burden interview of caregivers) are good predictors of long-term outcome measures (2).
The study claims that this article is a retrospective study, and it is well known that retrospective studies look at past data to conclude the present. In the daily work of hospitals, many aspects are not routinely evaluated, such as ADL and Zarit Burden interviews. In general practice, these indicators mentioned in the article are obtained through retrospective research. The possible justification for the same is that in the daily work of our hospital many aspects, such as ADL and Zarit Burden interviews are routinely evaluated.
The compilation of the comparative studies on professional-led post-surgical care after craniotomy (neurosurgeries) for traumatic brain injuries used in the current study for re-iteration of research findings (current research or past researches) is presented in Table 6.
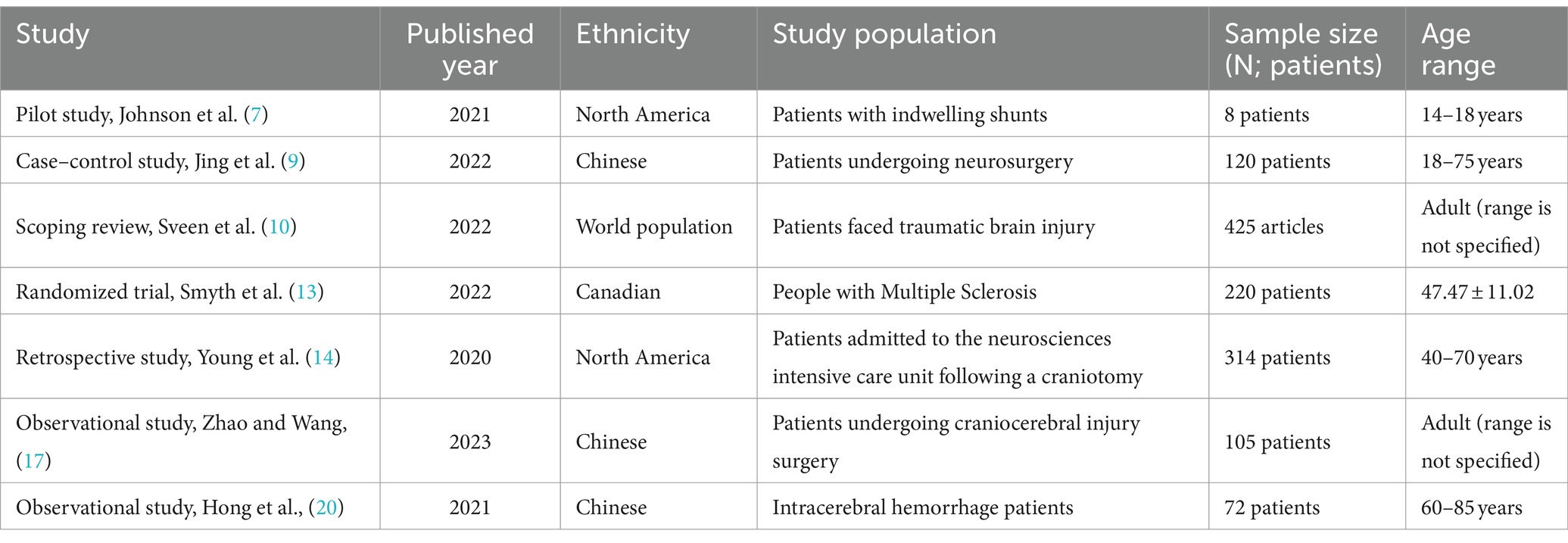
Table 6. Comparative studies on professional-led post-surgical care after craniotomy (neurosurgeries) for traumatic brain injuries.
In the study the results obtained in the late care of patients undergoing surgery for a traumatic brain injury are compared depending on whether these cares were provided by neurologists or nursing staff. The reason for raising this dilemma and this analysis seems to be the lack of medical personnel in the area of origin of the study. However, there are few limitations of this study, for example, its retrospective design and lack of randomized trials, with inherent limitations in obtaining information and biases in its analysis. The study has small cohorts which limits generalizability. Future research should consider incorporating more objective measures and providing more detailed information on adverse effects.
The activities of daily living and quality of life of patients after craniotomy for traumatic brain injuries must be improved, and anxiety and depression of patients after craniotomy for traumatic brain injuries must be relieved. Burden of caregivers of patients must be relieved after craniotomy for traumatic brain injuries. Nurse-led care and neurologist-led care are associated with improvement in quality of life, relief of anxiety and depression in patients after craniotomy for traumatic brain injuries, and relief of burden on caregivers of patients. Nurse-led care is superior to neurologist-led care in six months of the follow-up of patients after craniotomy for traumatic brain injuries, regarding the improvement of activities of daily living, quality of life, and psychological conditions of patients and burdens of their caregivers. Nurse-led care during follow-up decreases adverse effects after craniotomy for traumatic brain injuries compared with neurologist-led follow-up care. Patients and their caregivers may have higher satisfaction for nurses than neurologists with follow-up care after craniotomy for traumatic brain injuries. So is the consideration that patients after craniotomy for traumatic brain injuries have of nurse-led care. This study provides additional context and support for the benefits of nurse-led care after craniotomy in traumatic brain injuries.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The study protocol was designed and approved by the human ethics committee of the Shanxi Bethune Hospital and the Chinese Neurotrauma Scholar Association (Approval number 2019YJ18 dated January 11, 2019). The study follows the laws of China and the v2008 Declarations of the Helsinki. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
JW: Conceptualization, Methodology, Software, Visualization, Writing – original draft, Writing – review & editing. ZW: Methodology, Project administration, Resources, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. SS: Methodology, Resources, Software, Visualization, Writing – original draft, Writing – review & editing. JR: Data curation, Investigation, Methodology, Software, Supervision, Visualization, Writing – original draft, Writing – review & editing. XR: Conceptualization, Data curation, Formal analysis, Funding acquisition, Methodology, Writing – original draft, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by Shanxi Bethune Hospital (No: 2019YJ18).
The authors are thankful to the medical and nursing staff of the Shanxi Bethune Hospital, Taiyuan, Shanxi, China.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
NL cohort, Patients received nurse-led care after craniotomy for 6 months in follow-up plus regular treatment; GL cohort, Patients received neurologist-led care after craniotomy for 6 months in follow-up plus regular treatment; ADL, Activities of daily living; QoL, Quality of life; SD, Standard deviation; BC, Before any professional (nurse or neurologist)-led care; AC, After 6-months of any professional (nurse or neurologist)-led care; Q1, First Quartile; Q3, Third Quartile; χ2-test, Chi-square test; GCS, Glasgow Coma Scale.
1. Jiang, JY, Gao, GY, Feng, JF, Mao, Q, Chen, LG, Yang, XF, et al. Traumatic brain injury in China. Lancet Neurol. (2019) 18:286–95. doi: 10.1016/S1474-4422(18)30469-1
2. Guo, Z, Ding, W, Cao, D, Chen, Y, and Chen, J. Decompressive craniectomy vs. craniotomy only for traumatic brain injury: a propensity-matched study of long-term outcomes in neuropsychology. Front Neurol. (2022) 13:813140. doi: 10.3389/fneur.2022.813140
3. Kou, K, Hou, XY, Sun, JD, and Chu, K. Current pre-hospital traumatic brain injury management in China. World J Emerg Med. (2014) 5:245–54. doi: 10.5847/wjem.j.issn.1920-8642.2014.04.001
4. Jehan, F, Azim, A, Rhee, P, Khan, M, Gries, L, O'Keeffe, T, et al. Decompressive craniectomy versus craniotomy only for intracranial hemorrhage evacuation: a propensity matched study. J Trauma Acute Care Surg. (2017) 83:1148–53. doi: 10.1097/TA.0000000000001658
5. Ning, M, Chen, F, Zheng, H, Wu, X, Fu, Z, Zhou, J, et al. Use of head and neck magnetic resonance angiography to explore neurological function recovery and impact of rehabilitation nursing on patients with acute stroke. World Neurosurg. (2021) 149:470–80. doi: 10.1016/j.wneu.2020.11.116
6. Shepetovsky, D, Mezzini, G, and Magrassi, L. Complications of cranioplasty in relationship to traumatic brain injury: a systematic review and meta-analysis. Neurosurg Rev. (2021) 44:3125–42. doi: 10.1007/s10143-021-01511-7
7. Johnson, A, Marks, J, and Little, J. A pilot project: improving the transition care process for neurosurgical adolescent patients with indwelling shunts to adult care. J Pediatr Nurs. (2021) 60:164–7. doi: 10.1016/j.pedn.2021.05.003
8. Miryutova, NF, Vorobyev, VA, Minchenko, NN, Samoilova, IM, Zaitsev, AA, Mareeva, LV, et al. The integral estimation of health problems and effectiveness of stage rehabilitation in patients after ischemic stroke. Vopr Kurortol Fizioter Lech Fiz Kult [in Russian]. (2019) 96:5–16. doi: 10.17116/kurort2019960615
9. Jing, J, Lu, Y, Dong, J, and Zhang, LX. Effect of detailed nursing interventions on the activities of daily living of patients and satisfaction ratings of the neurosurgery department. Asian J Surg. (2022) 45:2439–40. doi: 10.1016/j.asjsur.2022.05.090
10. Sveen, U, Guldager, R, Soberg, HL, Andreassen, TA, Egerod, I, and Poulsen, I. Rehabilitation interventions after traumatic brain injury: a scoping review. Disabil Rehabil. (2022) 44:653–60. doi: 10.1080/09638288.2020.1773940
11. Sarwal, A. Neurologic complications in the postoperative neurosurgery patient. Continuum. (2021) 27:1382–404. doi: 10.1212/CON.0000000000001039
13. Smyth, P, Watson, KE, Al Hamarneh, YN, and Tsuyuki, RT. The effect of nurse practitioner (NP-led) care on health-related quality of life in people with multiple sclerosis – a randomized trial. BMC Neurol. (2022) 22:275. doi: 10.1186/s12883-022-02809-9
14. Young, JS, Chan, AK, Viner, JA, Sankaran, S, Chan, AY, Imershein, S, et al. A safe transitions pathway for post-craniotomy neurological surgery patients: high-value care that bypasses the intensive care unit. J Neurosurg. (2022) 134:1386–91. doi: 10.3171/2020.3.JNS192133
15. Ghelichkhani, P, Esmaeili, M, Hosseini, M, and Seylani, K. Glasgow coma scale and FOUR score in predicting the mortality of trauma patients; a diagnostic accuracy study. Emergency. (2018) 6:e42. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6289152/pdf/emerg-6-e42.pdf
16. Zhang, Y, Xiong, Y, Yu, Q, Shen, S, Chen, L, and Lei, X. The activity of daily living (ADL) subgroups and health impairment among Chinese elderly: a latent profile analysis. BMC Geriatr. (2021) 21:30. doi: 10.1186/s12877-020-01986-x
17. Zhao, B, and Wang, H. Effect of integrated perioperative rehabilitation intervention under the fast-track surgery concept on stress and complications in patients undergoing craniocerebral injury surgery. Front Surg. (2023) 9:1014211. doi: 10.3389/fsurg.2022.1014211
18. Li, G, Han, X, Gao, L, Tong, W, Xue, Q, Gong, S, et al. Association of anxiety and depressive symptoms with memory function following traumatic brain injury. Eur Neurol. (2021) 84:340–7. doi: 10.1159/000513195
19. Li, Q, Zhang, L, Chen, C, Gan, Y, Jiang, L, Li, S, et al. Caregiver burden and influencing factors among family caregivers of patients with glioma: a cross-sectional survey. J Clin Neurosci. (2022) 96:107–13. doi: 10.1016/j.jocn.2021.11.012
20. Hong, Y, Yan, H, and Wurichayihu, ZG. The effects of comprehensive nursing interventions on the negative emotions, quality of life, and nursing satisfaction in intracerebral hemorrhage patients. Am J Transl Res. (2021) 13:4860–7. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8205747/pdf/ajtr0013-4860.pdf
21. Fan, QQ, Feng, XQ, and Jin, JF. Nursing rounds: a quality improvement project to improve outpatient satisfaction. J Nurs Manag. (2021) 29:177–85. doi: 10.1111/jonm.13131
Keywords: anxiety, burden on caregivers, craniotomy, cognitive conditions, daily living activity, depression, nurse, neurologist
Citation: Wang J, Wu Z, Shi S, Ren J and Ren X (2024) Nurse-led care versus neurologist-led care for long-term outcomes of patients who underwent craniotomy in traumatic brain injuries: an efficacy analysis. Front. Neurol. 15:1382696. doi: 10.3389/fneur.2024.1382696
Received: 06 February 2024; Accepted: 08 July 2024;
Published: 26 July 2024.
Edited by:
Sarah C. Hellewell, Curtin University, AustraliaReviewed by:
Sorayouth Chumnanvej, Mahidol University, ThailandCopyright © 2024 Wang, Wu, Shi, Ren and Ren. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhiping Wu, emhpcGluZy53d3VAZ21haWwuY29t
†ORCID: Jingjing Wang, https://orcid.org/0009-0006-3138-4408
Zhiping Wu, https://orcid.org/0009-0001-5573-9238
Shufang Shi, https://orcid.org/0009-0004-2103-4135
Jiangyan Ren, https://orcid.org/0009-0008-6616-2869
Xiaojia Ren, https://orcid.org/0009-0006-4086-2715
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.