
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Neurol., 18 June 2024
Sec. Artificial Intelligence in Neurology
Volume 15 - 2024 | https://doi.org/10.3389/fneur.2024.1371332
This article is part of the Research TopicExploring the Future of Neurology: How AI is Revolutionizing Diagnoses, Treatments, and BeyondView all 10 articles
 Cunxiao Guo1†
Cunxiao Guo1† Yongdan Cun1,2†
Yongdan Cun1,2† Bo Xia3
Bo Xia3 Suyu Chen1
Suyu Chen1 Can Zhang1
Can Zhang1 Yiping Chen1
Yiping Chen1 Exian Shan1
Exian Shan1 Pengyue Zhang1*
Pengyue Zhang1* Xiantao Tai1*
Xiantao Tai1*Objective: This paper summarizes the research progress into stimulation methods used in rehabilitation equipment for pediatric cerebral palsy (CP) for the past 20 years from 2003 to 2023. We also provide ideas for innovative research and development of artificial intelligence-based rehabilitation equipment.
Methods: Through a certain search strategy, Keywords are searched in the China National Knowledge Network Database (CNKI), the Wanfang Database knowledge service platform, the Chongqing VIP information service, PubMed, Web of Science, Cochrane, ScienceDirect, Medline, Embase, and IEEE database. A total of 3,049 relevant articles were retrieved, and 49 articles were included that mentioned research and development of rehabilitation equipment. We excluded articles that were not specific to children with CP, were duplicated or irrelevant literature, were missing data, the full article was not available, the article did not describe the method of stimulation used with the rehabilitation equipment on children with CP, were not Chinese and English, and were the types of reviews and commentaries.
Results: Physical stimulation is the main stimulation method of rehabilitation equipment for children with CP. Force stimulation is the main mode of physical stimulation, and there are 17 articles that have verified the clinical efficacy of force stimulation-based equipment.
Conclusion: Research on the stimulation mode of pediatric cerebral palsy rehabilitation equipment is likely to focus on simulating the force of the Chinese medicine called “tuina manipulation.” When this method is combined with artificial intelligence and personalized direction we believe this will lay the foundation for future development of a novel therapy for children with CP.
Cerebral palsy (CP) is a group of persistent central motor and postural development disorders and activity limitation syndromes caused by non-progressive brain damage in developing fetuses or infants, which is accompanied by sensory, perceptual, cognitive, communication, and behavioral disorders, as well as epilepsy and secondary muscle and bone problems. According to domestic and foreign reports, the prevalence of cerebral palsy is 1.4%~3.2%, and the prevalence of CP in children aged 1~6 years old in China is 2.46‰ (1, 2). The prevalence of CP in boys is higher than that in girls (2.25% vs. 1.59%), and higher in rural areas than in urban areas (2.75% vs. 1.90%).
There are significant disparities in the prevalence of CP across various geographical regions, and the incidence is observed to be increasing annually (3). The rehabilitation cycle for CP is prolonged and arduous, compounded by a shortage of rehabilitation educators (4, 5). According to the “Lancet” Global Burden of Diseases (GBD) study on rehabilitation published in 2020, China has over 460 million patients with rehabilitation needs, the highest of any country in the world, followed by India and the United States (6). According to data from the “China Health Statistics Yearbook” in 2022, the percentage of Chinese rehabilitation physicians (assistants) out of the total number of practicing (assistant) physicians is 1.3% in 2021 (7). Moreover, in many low-and middle-income areas, there exists a shortage of trained rehabilitation professionals, with fewer than 10 skilled practitioners per one million population (8). Rehabilitation equipment based on artificial intelligence (AI) technology is expected to solve the major bottleneck problem of insufficient rehabilitation teachers for CP. Therefore, we conducted a search across relevant research databases and information services on rehabilitation equipment for children with CP over the past 20 years. Subsequently, we reviewed the stimulation methods employed in conjunction with the equipment. The purpose is to provide a basis for the selection of stimulation methods for the development of rehabilitation equipment for children with CP. Through equipment research and development to solve the contradiction between the increasing demand for treatment of children with CP and the shortage of rehabilitation teachers. The development of AI will provide assistance for the development of intelligent decision support and intelligent treatment equipment.
1. Research object: CP, there are no racial and gender restrictions.
2. Intervention measures: rehabilitation equipment for children with CP stimulation.
3. Rehabilitation equipment research and development stage: published research and development design or clinical application stage; the rehabilitation equipment entering the clinical application stage needed to have rigorous clinical trial design and verification of its safety or effectiveness.
4. Type of literature included in the study: original articles, Clinical Trials/CTs, randomized CTs/RCTs, non-RCTs, and conference papers.
1. Articles that do not involve children with CP.
2. Repeatedly published articles that are not related to the research topic.
3. Articles with missing data or the full text were not available.
4. Articles on rehabilitation equipment for children with CP where no stimulation method was described.
5. Articles other than Chinese and English were excluded.
6. Type of literature excluded in the study: reviews and commentaries.
The China National Knowledge Network Database (CNKI), the Wanfang database knowledge service platform, the Chongqing VIP information service, PubMed, Web of Science, Cochrane, ScienceDirect, Medline, Embase, and IEEE database were searched. The keywords were “cerebral palsy OR pediatric cerebral palsy,” “cerebral palsy rehabilitation equipment,” “cerebral palsy equipment,” “cerebral palsy intelligent tuina clothing,” “intelligent tuina suit for cerebral palsy,” “rehabilitation equipment,” and “stimulation mode.” The search strategy of the databases and information services and platforms is shown in Table 1.
The search was for relevant articles published between 1 January 2003 to 1 December 2023. A total of 3,049 articles were retrieved. Through the application of inclusion and exclusion criteria and by reviewing the titles and abstracts, it was found that 2,885 articles were repetitive or unrelated to the research topic, or their full text was unavailable, or non-Chinese and English, or the types of reviews, and commentaries. We obtained 164 potentially relevant articles but after reading the full text, 115 articles did not meet the stated inclusion criteria and were excluded. The final number of relevant articles that adhered to the criteria and were included in this study was 49 articles (Figure 1).
In the literature screening, two researchers independently screened the relevant literature and extracted the data in strict accordance with the inclusion and exclusion criteria, and then cross-checked by two researchers to discuss the differences or ask third-party experts.
Two reviewers independently assessed the methodological quality of clinical trials of rehabilitation equipment for children with CP, using Physiotherapy Evidence Database (PEDro) Scale, PEDro scores were categorized as follows: <4, poor; 4~5, fair; 6~8, good; and 9~10, excellent (9).
We used the Oxford Center for Evidence-Based Medicine Levels of Evidence Working Group (OCEBM) to evaluate the evidence types in clinical trials of rehabilitation equipment for children with CP. It is divided into I (high-level evidence) to V (low-level evidence). Systematic reviews are usually classified as grade I clinical practice evidence, followed by randomized trials and blinded studies, which are classified as grade II. Grade III of cohort, follow-up and non-randomized studies; finally, the case series, case–control study, and mechanism-based reasoning are taken as the IV and V levels. Studies at levels I to IV may be downgraded due to research quality, inaccuracy, indirectness, inconsistency between studies, or small impact; if there is a significant impact, these studies may be escalated.
The 49 articles that met the inclusion criteria were divided into four types according to the nature of the stimulation method used with the rehabilitation equipment. Physical stimulation included electricity, force, sound and light. Chemical stimulation included treatment with acids, alkalis and drugs. Biological stimuli included treatment with bacteria and viruses. The final type was psychosocial stimulation. According to the above classifications, 34 articles of physical stimulation were found, including 25 articles on force stimulation (10–34), 5 articles on electromagnetic stimulation (35–39), 2 articles on acoustic stimulation (40, 41), 1 article which combined force and electricity (42) and 1 article that combined force and magnetic tuina (43). There were no articles that employed biological stimulation, and 5 articles involved psychosocial stimulation (44–48). The other 10 articles reported a combination of two or more stimuli (49–56). One article used a combination of botulinum toxin stimulation with electrical and chemical stimulations (57), and another article used a combination of mechanical, magnetic, and psychosocial stimulations (58) (Figure 2).
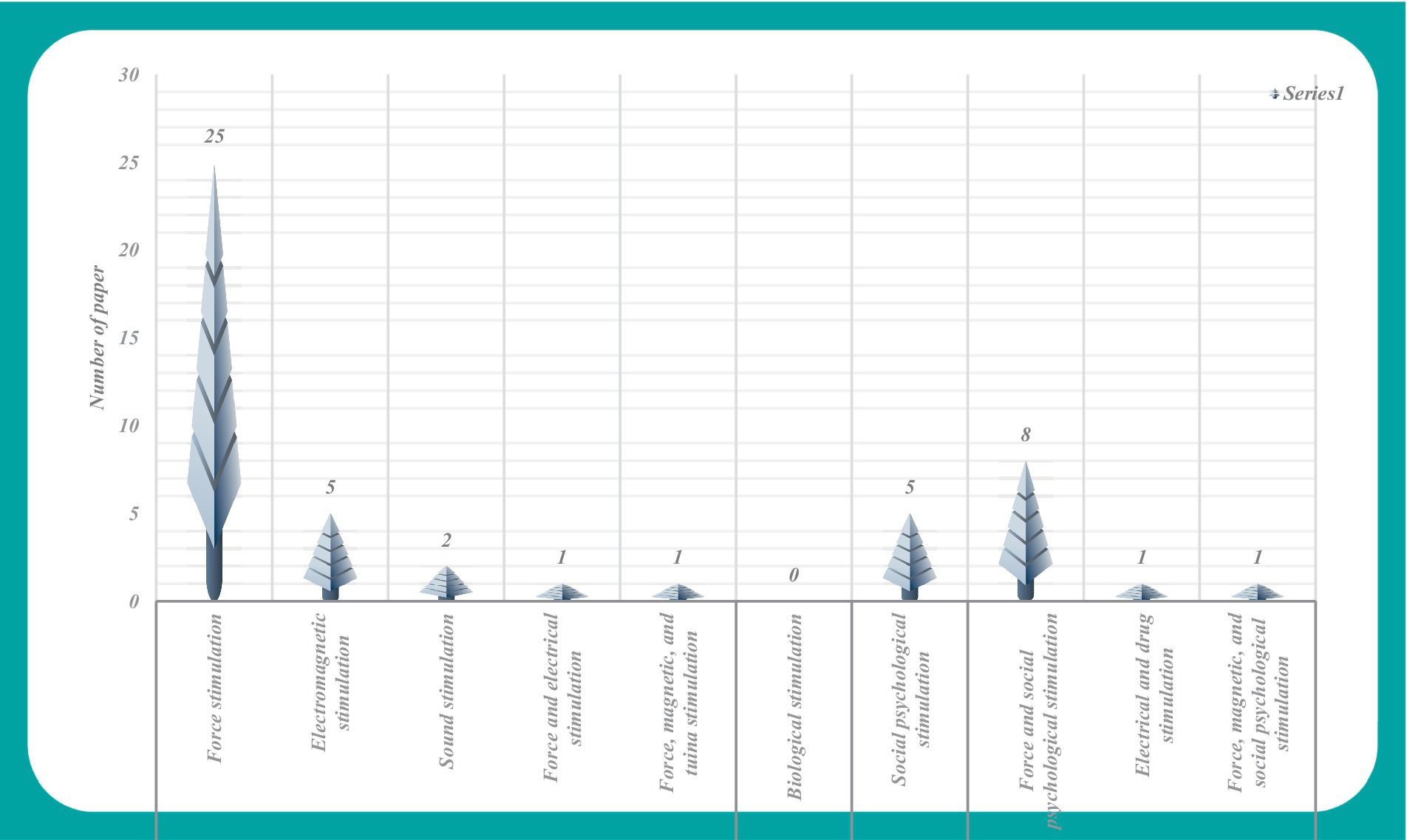
Figure 2. Literature analysis chart of stimulation methods used with rehabilitation equipment for children with CP.
In Figure 2, the analysis of research and development trends in rehabilitation equipment for children with CP reveals the prevalent use of force stimulation methods within the category of physical stimulation. The integration of force stimulation with psychosocial stimulation was the second most popular approach used in the relevant literature. However, it is noteworthy that the application of alternative stimulation methods appears comparatively limited within the current landscape of research and development in this field.
Figure 3 shows the design factors described in the 49 relevant articles. These design factors included functionality of the equipment, interest, portability, safety/security, wearability, user requirements, comfort, ease of operation, adjustability, materials, modeling, cost, color, and durability. The analysis of the design factors, revealed the design factor that was most prevalent was the function of the equipment. The other design factors were related to the experience of the children with CP using the equipment and the safety of the equipment, which provided a reference for the proposed future research and development of rehabilitation equipment for children with CP.
The data from Figures 2, 3 show that articles involving force stimulation constitute 51.02% of the research corpus to date. This may be attributed to the perceived advantages of force stimulation in terms of simplicity and ease of implementation. Noteworthy factors considered in device development include design elements such as interest, portability, safety, and wearability, which underscore the multifaceted approach to advancing this field of research.
Force stimulation emerges as a prevalent modality within the category of physical stimulation because it offers versatility across various applications. The literature review revealed specific force stimulation modes, which included auxiliary fixation force, weight-bearing force, and the utilization of exoskeleton robots or rehabilitation robots. An exhaustive analysis of force stimulation methods is conducted within the framework of these four force stimulation modes and is presented in Tables 2, 3.
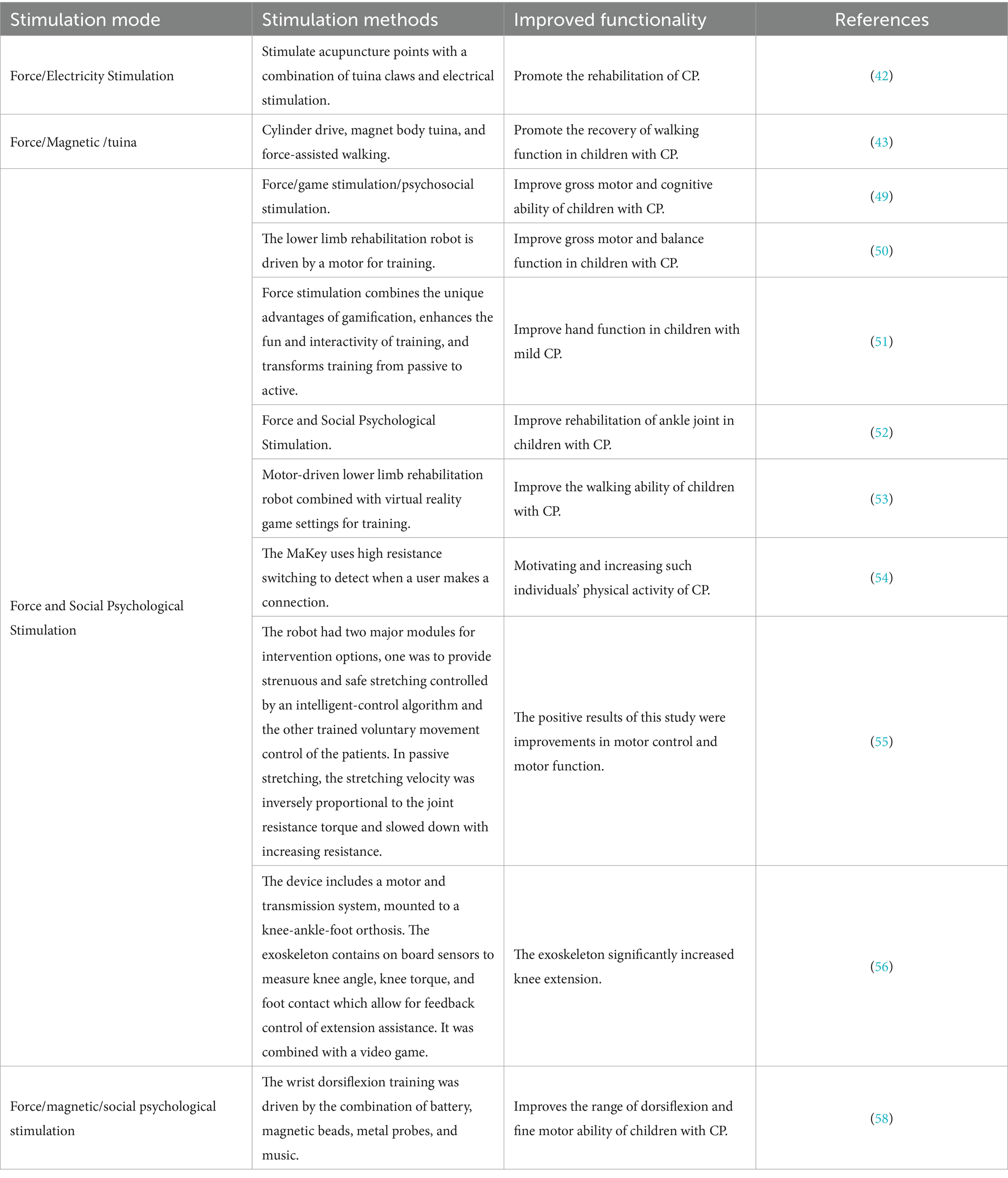
Table 3. Analysis table of force combined with other forms of stimulation of rehabilitation equipment for pediatric CP.
Table 2 shows that the stimulation method of force has evolved from the initial fixed force and weight-bearing force of the auxiliary device to the passive force of the auxiliary device, and finally to the upper and lower limb exoskeleton robot/lower limb rehabilitation robot. Force stimulation has been quantified from no quantification to further quantification within the range of joint functional activity. Different amounts of stimulation have different focuses on the improvement of function. The auxiliary fixation force is mainly used to correct the posture and gradually establish the walking function whereas the weight-bearing force mainly improves walking and balance function. The power of the auxiliary device is quantified in the amount of force stimulation, and the function is gradually improved. This is mainly used to improve the motor function of the upper and lower limbs, followed by the improvement of muscle strength training, blood circulation, and balance coordination function. The upper and lower extremity exoskeletons and rehabilitation robots are more abundant and perfect in the realization of functions. Targeted training is carried out for the flexion and extension of a specific joint such as the wrist, knee, and ankle in the upper and lower limbs. Even some devices can also increase the repeatability and interest of children with CP in limb function training based on certain task settings.
Table 3 reveals that the amalgamation of force-based stimulation with electrical, magnetic, tuina, and psychosocial stimulation modes yields a synergistic effect. This integrated approach proves beneficial in enhancing cognition, movement, balance, gait, and overall physical function among children with CP, which fosters a heightened interest in their training endeavors. The combination of stimulation methods aligns with the distinctive characteristics of individual pediatric patients, and addresses pertinent clinical requirements. However, a noteworthy limitation lies in the insufficient consideration of the equipment’s applicability scope and adjustability. Simultaneously, it is worth noting that the force stimulation of simulated tuina manipulation is utilized in the fusion of multiple stimulation methods. The effect of tuina manipulation is based on the fundamental theory of traditional Chinese medicine (TCM), which stimulates certain parts or acupoints of the human body to achieve the effect of preventing and treating diseases. Nevertheless, how to objectively quantify the amount of stimulation and repeatability needs to be solved.
The research and development (R&D) of equipment is generally divided into four stages according to its development stage. The first stage is prototype development where the main consideration is how many devices have been certified by the Food and Drug Administration. The second stage is the feasibility study, where the number of trials is small and usually with a prototype device to assess its safety and clinical feasibility. The third stage is the clinical trial, which determines the effectiveness of the treatment. The final stage is the commercialization stage, which can be popularized and applied (59). In this article, there are 19 articles involving devices entering the clinical trial stage, of which 17 are force stimulation-based devices. Table 4 shows that the sample size of the test is smaller in the 17 force stimulation-based literatures. The intervention measures were mainly based on original equipment, and the outcome indicators were mainly gross motor function measures (GMFM-88), Fine motor function measure (FMFM), Modified Ashworth scale (MAS), Modified Tardieu Scale (MTS), etc. Data from the clinical trial of the equipment, verified the effectiveness of the equipment, which laid a foundation for its popularization and wide application. However, during each R&D stage there is a better understanding of the existing equipment including its limitations and frequently there needs to be modifications and improvements. Thus the equipment usually undergoes a long process from R&D to listing.
In order to further evaluate the entry of 17 force-stimulated devices into clinical trials, the clinical trial methodology was evaluated using the PEDro Scale (Table 5). OCEBM was used to analyze the type of evidence (Table 6).
Table 5 shows that the methodological level of clinical trials of force stimulation equipment is mainly 4–5 (Fair), and the level of 6–8 (Good) is limited. Table 6 suggests that there are 7 articles of Level 2 and Level 4 in the evidence type of force stimulation clinical trials, and 3 articles of Level 3. Tables 5, 6 show that high-level evidence types are not necessarily high-quality methodologies. Therefore, in order to make the results more reliable in the clinical trial design of pediatric cerebral palsy equipment, the methodology needs to be further improved.
The World Health Organization released information that 50% of rehabilitation needs have not been met, and there are inadequate numbers of rehabilitation physicians for children with CP particularly in low-and middle-income countries. With the development of AI, the R&D of rehabilitation equipment combined with medicine and engineering has shown a vigorous trend of development. Children with CP have a long rehabilitation cycle because of their life-long motor disability, as well as a wide variety of associated impairments.
The R&D of rehabilitation equipment for adjuvant treatment of children with CP has emerged as a prominent focus of research and is increasingly capturing public attention. The stability, durability, and reproducibility of AI technology (60) are highly likely hold significant importance for the treatment of CP. Equipment development can be tailored for children with regard to the mode of stimulation and the amount of stimulation, which can be quantified and controlled. This paper analyzes the stimulation methods of rehabilitation equipment for children with CP, to provide a reference for the R&D of rehabilitation equipment for children with CP.
Upon assessing the relevant articles identified in our literature search, it is evident that the stimulation mode of the equipment primarily revolves around physical stimulation. Specifically, force stimulation is widely employed. This approach offers the advantages of straightforward operation, a broad application range, and the absence of toxic side effects associated with physical factor stimulation (61). Force stimulation is easily achievable, controllable, and devices employing force stimulation, as featured in 17 of the relevant articles, have undergone clinical trials to assess their efficacy. The essential prerequisites for these trials include the design of sample size, the test plan, treatment course, and outcome index, all of which yield reliable data crucial for driving the subsequent development of equipment. However, in the follow-up studies, the sample size, methodological quality and evidence type of equipment clinical trials need to be strengthened. The integration of force stimulation with other stimulation methods can harness the advantages of various approaches, particularly the combination of force and social-psychological stimulation, aligning more closely with the modern medical model’s development. Some articles include electromagnetic stimulation, psychosocial stimulation, and acoustic stimulation. Electromagnetic stimulation offers the advantage of simplicity and ease of implementation. Especially for stroke treatment is widely used, such as tDCS can be easily applied simultaneously with other therapies (62). It has good tolerance, safety, portability, and suitable for different levels of patients (63), but the stimulation threshold for children with CP requires further refinement. Non-invasive electromagnetic stimulation presents an appealing option for treating children with CP, yet the safety requirements necessitate further strengthening. Psychosocial stimulation is utilized independently, and its functionality is relatively straightforward. Articles employing acoustic stimulation predominantly utilize ultrasonic stimulation. The application of acoustic stimulation in cerebral palsy rehabilitation equipment remains relatively limited and is still in its infancy. Acoustic stimulation offers certain advantages in regulating neurological function, Studies have confirmed that noninvasive ultrasound deep brain stimulation (UDBS) enables modulation of the subthalamic nucleus (STN) or the globus pallidus (GP) neural activity and leads to neuroprotection in PD mice, potentially serving as a noninvasive strategy for the clinical treatment of PD (64). Noninvasive modulation of neuronal activity is an important translational application of focused ultrasound (FUS). it elicited action potentials with millisecond latencies compared with electrical stimulation, suggesting ion channel-mediated mechanisms (65). However, its application for children with CP requires clarification. Furthermore, stimulation parameters as well as safety thresholds necessitate further definition with this method.
The search described in this paper possesses two limitations. Firstly, a relatively small number of potentially relevant articles were excluded due to the unavailability of full texts. Secondly, variations in professional perspectives may result in disparities in article inclusion, data extraction, and analysis.
In conclusion, research on the stimulation mode of rehabilitation equipment for children with CP is mainly based on the force stimulation in physical stimulation. The force used is mainly based on external forces such as fixation, correction, and active or passive movement. The R&D of equipment with more choice of force stimulation conforms to the advantages and characteristics of force. At present, the force stimulation method of simulating pediatric tuina manipulation on children with CP is less used. With the development and integration of AI, the research on the stimulation method of rehabilitation equipment for children with CP will focus on the force of simulating tuina manipulation, and the combination of AI and personalization will be the trend for future equipment development. The application of this stimulation method can not only objectively quantify the stimulation amount of tuina manipulation, but also make treatment by tuina manipulation uniform and reproducible, and thereby benefit from this unique form of Chinese traditional medicine. Thus, AI is likely to go a long way in solving the bottleneck problem of insufficient numbers rehabilitation teachers.
At present, through the combination of TCM and AI, some scholars have objectively quantified the four diagnostic methods of TCM (observation, auscultation, inquiry and palpation), developed an expert decision support system for children with CP, realized intelligent diagnosis, and solved the objectification of the four diagnostic methods of TCM for children with CP, the standardization of syndrome differentiation and the intelligentization of rehabilitation decision-making (66). The key to intelligent “treatment” is the key technologies such as acupoint selection (67), manipulation selection, intelligent recognition and automatic adjustment of acupoints in TCM. Finally, an intelligent tuina device for the diagnosis and treatment of CP in children is formed, which lays a foundation for the construction of a three-level linkage intelligent rehabilitation network for cerebral palsy such as hospital-grassroots community-family.
CG: Writing – review & editing, Writing – original draft, Formal analysis, Data curation, Conceptualization. YoC: Writing – review & editing, Writing – original draft, Formal analysis, Data curation, Conceptualization. BX: Writing – original draft, Writing – review & editing. SC: Writing – original draft, Methodology. CZ: Writing – original draft, Methodology. YiC: Writing – original draft, Methodology. ES: Writing – original draft, Methodology. PZ: Supervision, Writing – original draft. XT: Writing – original draft, Supervision.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. The study was supported by the National Natural Science Foundation of China (82374614), the Yunnan Key Laboratory of Acupuncture and Tuina Prevention and Treatment of Encephalopathy (2019YGZ04), the Yunnan Provincial Science and Technology Project (202102AA100016), Yunnan Basic Research Traditional Chinese Medicine Joint Special Project (202001AZ070001-002), and Yunnan province innovation team of prevention and treatment for brain diseases with acupuncture and tuina (202405AS350007).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Children Rehabilitation Committee of China Rehabilitation Medical Association, Children Cerebral Palsy Rehabilitation Committee of China Rehabilitation Association for the Disabled, Children Rehabilitation Committee of Rehabilitation Physician Branch of Chinese Physician Association, Editorial Board of ‘Chinese Cerebral Palsy Rehabilitation Guideline’ meeting . Chinese rehabilitation guideline for cerebral palsy (2022) chapter 1: introduction. J Chin Appl Clin Paediatr. (2022) 37:887–92. doi: 10.3760/cma.j.cn101070-20220505-00500
2. Li, XJ, Qiu, HB, Jiang, ZM, Pang, W, Guo, J, Zhu, LL, et al. Epidemiological characteristics of cerebral palsy in children in twelve provinces and cities of China. J Chin Appl Clin Paediatr. (2018) 33:378–83. doi: 10.3760/cma.j.issn.2095-428X.2018.05.013
3. Yang, S, Xia, J, Gao, J, and Wang, L. Increasing prevalence of cerebral palsy among children and adolescents in China 1988-2020: a systematic review and meta-analysis. J Rehabil Med. (2021) 53:jrm00195. doi: 10.2340/16501977-2841
4. The National Health Commission, the Development and Reform Commission, the Ministry of Education, the Civil Affairs Bureau, the Finance Bureau, the Medical Insurance Bureau, the Chinese Medicine Bureau, and the China Disabled Persons ' Federation . Notice on Issuing Opinions on Accelerating the Development of Rehabilitation Medical Work (2021). Available at: https://www.gov.cn/zhengce/content/2022-3/29/content_5682255.htm (Accessed 18 June 2021).
5. General Office of the State Council . Notice of the General Office of the State Council on printing and distributing the '14th Five-Year' development plan of traditional Chinese medicine. (2022). Available at: https://www.gov.cn/zhengce/content/2022-03/29/content_5682255.htm (Accessed 29 March 2022).
6. Cieza, A, Causey, K, Kamenov, K, Hanson, SW, Chatterji, S, and Vos, T. Global estimates of the need for rehabilitation based on the global burden of disease study 2019: a systematic analysis for the global burden of disease study 2019. Lancet. (2020) 396:2006–17. doi: 10.1016/S0140-6736(20)32340-0
7. Statistical Information Center . 2022 China Health Statistical Yearbook. (2020). Available at: http://www.nhc.gov.cn/mohwsbwstjxxzx/tjtjnj/202305/6ef68aac6bd14c1eb9375e01a0faa1fb.shtml (Accessed 18 June 2021).
8. World Health Organization . Rehabilitation; World Health Organization: Geneva, Switzerland. (2019). Available at: https://www.who.int/news-room/fact-sheets/detail/rehabilitation (Accessed 30 January 2023).
9. Cashin, AG, and McAuley, JH. Clinimetrics: physiotherapy evidence database (PEDro) scale. J Physiother. (2020) 66:59. doi: 10.1016/j.jphys.2019.08.005
10. Zhang, XX, Chen, ZY, and Sun, F. Research on the development of rehabilitation auxiliary equipment for sitting posture maintenance of cerebral palsy children. Health Relat Vocat Educ. (2011) 29:155–7. doi: 10.3969/j.issn.1671-1246.2011.17.092
11. Lan, Z, Wang, XT, Yan, HP, Zhang, XF, Ma, Y, Li, GL, et al. Comprehensive rehabilitation training aids for cerebral palsy. Patent no: CN201320864880.8. (2014).
12. Sahinoğlu, D, Coskun, G, and Bek, N. Effects of different seating equipment on postural control and upper extremity function in children with cerebral palsy. Prosthet Orthot. (2017) 41:85–94. doi: 10.1177/0309364616637490
14. Zhou, YP, and Lu, Y. Development and clinical application of a rehabilitation training device for children with cerebral palsy. Smart Healthcare. (2018) 4:28–30. doi: 10.19335/j.cnki.2096-1219.2018.32.013
15. Wu, GQ, Hu, SF, Cheng, Y, and Liu, H. An intelligent wearable rehabilitation robot for children with cerebral palsy. Patent no: CN20171035 1691.3 (2020).
16. Holley, D, Johnson, M, Harris, G, and Beardsley, S. A modular low-clearance wrist orthosis for improving wrist motion in children with cerebral palsy. Annu Int Conf IEEE Eng Med Biol Soc. (2014) 2014:3069–72. doi: 10.1109/EMBC.2014.6944271
17. Washabaugh, EP, Guo, J, Chang, C, Remy, CD, and Krishnan, C. A portable passive rehabilitation robot for upper-extremity functional resistance training. IEEE Trans Biomed Eng. (2019) 66:496–508. doi: 10.1109/TBME.2018.2849580
18. Chong, YZ, Teoh, BY, Chong, HF, Alawi, M, Chong, PN, Heng, YT, et al. Development of low cost upper and lower extremities rehabilitation system with interactive feedback for children with movement disorders. (2016). In: 2016 IEEE EMBS Conference on Biomedical Engineering and Sciences.
19. Lotfian, M, Kharazi, MR, Mirbagheri, A, Dadashi, F, Nourian, R, and Mirbagheri, MM. Therapeutic effects of an anti-gravity treadmill (AlterG) training on gait and lower limbs kinematics and kinetics in children with cerebral palsy. IEEE Int Conf Rehabil Robot. (2017) 2017:170–4. doi: 10.1109/ICORR.2017.8009241
20. Patane, F, Rossi, S, Del, SF, Taborri, J, and Cappa, P. WAKE-up exoskeleton to Assist children with cerebral palsy: design and preliminary evaluation in level walking. IEEE Trans Neural Syst Rehabil Eng. (2017) 25:906–16. doi: 10.1109/TNSRE.2017.2651404
21. Noroozi, S, Mehrabi, R, Lotfian, M, Nooshiravan, F, Shahroki, A, Irani, A, et al. "Therapeutic effects of an anti-gravity treadmill (AlterG) training on neuromuscular abnormalities associated with spasticity in children with cerebral palsy," (2020). In: 2020 42nd annual international conference of the IEEE engineering in Medicine & Biology Society (EMBC), Montreal, QC, Canada, pp. 3856–3859.
22. Gu, QY, Ni, YF, Ge, XY, Wang, FY, Lu, MJ, and Xu, XJ. Application of pneumatic hand rehabilitation equipment in rehabilitation of hand function in children with spastic hemiplegia cerebral palsy. Chin J Rehabil Theory Pract. (2023) 29:93–7. doi: 10.3969/j.issn.1006-9771.2023.01.014
23. Holley, D, Theriault, A, Kamara, S, Anewenter, V, Hughes, D, and Johnson, MJ. Restoring ADL function after wrist surgery in children with cerebral palsy: a novel bilateral robot system design. IEEE Int Conf Rehabil Robot. (2013) 2013:6650463. doi: 10.1109/ICORR.2013.6650463
24. Dittli, J, Vasileiou, C, Asanovski, H, Lieber, J, Lin, JB, Meyer-Heim, A, et al. Design of a compliant, stabilizing wrist mechanism for a pediatric hand exoskeleton. IEEE Int Conf Rehabil Robot. (2022) 2022:1–6. doi: 10.1109/ICORR55369.2022.9896550
25. Lerner, ZF, Gasparri, GM, Bair, MO, Lawson, JL, Luque, J, Harvey, TA, et al. An untethered ankle exoskeleton improves walking economy in a pilot study of individuals with cerebral palsy. IEEE Trans Neural Syst Rehabil Eng. (2018) 26:1985–93. doi: 10.1109/TNSRE.2018.2870756
26. Lerner, ZF, Damiano, DL, and Bulea, TC. Relationship between assistive torque and knee biomechanics during exoskeleton walking in individuals with crouch gait. IEEE Int Conf Rehabil Robot. (2017) 2017:491–7. doi: 10.1109/ICORR.2017.8009296
27. Lerner, ZF, Damiano, DL, Park, HS, Gravunder, AJ, and Bulea, TC. A robotic exoskeleton for treatment of crouch gait in children with cerebral palsy: design and initial application. IEEE Trans Neural Syst Rehabil Eng. (2017) 25:650–9. doi: 10.1109/TNSRE.2016.2595501
28. Sarajchi, M, and Sirlantzis, K. Design and control of a single-leg exoskeleton with gravity compensation for children with unilateral cerebral palsy. Sensors. (2023) 23:6103. doi: 10.3390/s23136103
29. Conner, BC, Spomer, AM, Steele, KM, and Lerner, ZF. Factors influencing neuromuscular responses to gait training with a robotic ankle exoskeleton in cerebral palsy. Assist Technol. (2023) 35:463–70. doi: 10.1080/10400435.2022.2121324
30. Cheng, S, Hu, DY, Zheng, L, and Liang, Z. Development of lower limb rehabilitation training Equipmen. China Med Dev. (2023) 38:49. doi: 10.3969/j.issn.1674-1633.2023.06.005
31. Van Kammen, K, Reinders-Messelink, HA, Elsinghorst, AL, Wesselink, CF, Meeuwisse-de Vries, B, van der Woude, LH, et al. Amplitude and stride-to-stride variability of muscle activity during Lokomat guided walking and treadmill walking in children with cerebral palsy. Eur J Paediatr Neurol. (2020) 29:108–17. doi: 10.1016/j.ejpn.2020.08.003
32. Conner, BC, Schwartz, MH, and Lerner, ZF. Pilot evaluation of changes in motor control after wearable robotic resistance training in children with cerebral palsy. J Biomech. (2021) 126:110601. doi: 10.1016/j.jbiomech.2021.110601
33. Gilliaux, M, Renders, A, Dispa, D, Holvoet, D, Sapin, J, Dehez, B, et al. Upper limb robot-assisted therapy in cerebral palsy: a single-blind randomized controlled trial. Neurorehabil Neural Repair. (2015) 29:183–92. doi: 10.1177/1545968314541172
34. Diot, CM, Thomas, RL, Raess, L, Wrightson, JG, and Condliffe, EG. Robotic lower extremity exoskeleton use in a non-ambulatory child with cerebral palsy: a case study. Disabil Rehabil Assist Technol. (2021) 18:497. doi: 10.1080/17483107.2021.1878296
35. Ren, PY, Qu, JQ, Han, P, Xu, CX, Li, Y, Zhou, L, et al. Intelligent self-evolving neuromodulation device and method for the treatment of spastic cerebral palsy. Patent no: CN2020105 42871.1. (2022).
36. Abidin, AZ, Agarwal, S, Chattopadhyay, S, Poddar, A, and Ganesh, B. A study on portable functional electrical device for small muscles. (2010). In:Students' Technology Symposium (TechSym), 2010 IEEE
37. Xuan, H . Analysis of curative effect of brain dysfunction therapeutic apparatus in adjuvant treatment of children with spastic cerebral palsy. J Mod Med Health. (2014) 30:3724–6. doi: 10.3969/j.issn.1009_5519.2014.24.019
38. Liang, GJ, Gu, Q, Li, MD, and Su, M. Repetitive transcranial magnetic stimulationcan improve the effectiveness of constraint -induced movement therapy for hemiplegic children with cerebral palsy. Chin J Phys Med Rehabil. (2020) 42:515–8. doi: 10.3760/cma.j.issn.0254-1424.2020.06.007
39. Gillick, B, Rich, T, Nemanich, S, Chen, CY, Menk, J, Mueller, B, et al. Transcranial direct current stimulation and constraint-induced therapy in cerebral palsy: a randomized, blinded, sham-controlled clinical trial. Eur J Paediatr Neurol. (2018) 22:358–68. doi: 10.1016/j.ejpn.2018.02.001
40. Cai, JN, Cai, YW, Luo, X, Chen, W, and Liao, SH. Ultrasound treatment equipment for brain rehabilitation. Patent no: CN201721740492.3. (2019).
41. Zhang, HM, Zhao, XK, Zhang, Y, Tang, J, Zhang, L, Zhang, L, et al. Effects of transcranial ultrasound therapy on balance and walking in children with dyskinetic cerebral palsy. Zhongguo Kangfu Lilun Yu Shijian. (2017) 23:595–8. doi: 10.3969/j.issn.1006-9771.2017.05.023
42. Xiao, CY, Guan, ZH, Ye, Y, and Cl, Chen. An acupoint tuina electrical stimulation device for rehabilitation treatment of children with cerebral palsy Patent no: CN202210196389.6. (2022).
43. ZhY, Yan, Li, T, Wu, CH, Yi, C, and Liu, XX. A walking recovery instrument for children with cerebral palsy and its use method. Patent no: CN201910488800.5. (2019).
44. Zhipeng, MA . Research on key Technologies of Human-Robot Interaction for robot-assisted cerebral palsy rehabilitation training system[master’s thesis]. (2020). China university of mining and technology.
45. Huang, H, Ragonesi, CB, Stoner, T, Peffley, T, and Galloway, JC. Modified toy cars for mobility and socialization: case report of a child with cerebral palsy. Pediatr Phys Ther. (2014) 26:76–84. doi: 10.1097/PEP.0000000000000001
46. Montesano, L, Díaz, M, Bhaskar, S, and Minguez, J. Towards an intelligent wheelchair system for users with cerebral palsy. IEEE Trans Neural Syst Rehabil Eng. (2010) 18:193–202. doi: 10.1109/TNSRE.2009.2039592
47. Shen, LI, Liu, XM, Chen, J, Li, WW, and Qiao, HI. Effect of MOTOmed virtual scenario training on children with spastic cerebral palsy. J Bengbu Med Coll. (2020) 45:1565–8. doi: 10.13898/j.cnki.issn.1000-2200.2020.11.029
48. Arnoni, JLB, Pavao, SL, dos Santos Silva, FP, and Rocha, NACF. Effects of virtual reality in body oscillation and motor performance of children with cerebral palsy: a preliminary randomized controlled clinical trial. Complement Ther Clin Pract. (2019) 35:189–94. doi: 10.1016/j.ctcp.2019.02.014
49. Deng, HY . The effect of wearable device games on gross motor and cognitive ability of children with cerebral palsy[master’s thesis]. Zhejiang Normal University. (2019).
50. Chen, JH . Effects of robot assisted gait training for the motor function of children with spastic cerebral palsy [master’s thesis]. Zhengzhou University. (2021).
51. He, J. Research on product design of hand function training for children with mild cerebral palsy based on gamification[master’s thesis]. Southwest Jiaotong University. (2021).
52. Wang, RL, Zhou, ZH, Xi, YC, Wang, QN, Wang, NH, and Huang, Z. Preliminary study of robot-assisted ankle rehabilitation for children with cerebral palsy. Beijing Da Xue Xue Bao. (2018) 50:207–12. doi: 10.3969/j.issn.1671-167X.2018.02.002
53. Fu, WS, Song, YC, Wu, BA, Qu, CH, and Zhao, JF. Virtual reality combined with robot-assisted gait training to improve walking ability of children with cerebral palsy: a randomized controlled trial. Technol Health. (2022) 30:1525–33. doi: 10.3233/THC-212821
54. Lin, CY, and Chang, YM. Increase in physical activities in kindergarten children with cerebral palsy by employing MaKey-MaKey-based task systems. Res Dev. (2014) 35:1963–9. doi: 10.1016/j.ridd.2014.04.028
55. Wu, YN, Ren, Y, Hwang, M, Gaebler-Spira, DJ, and Zhang, LQ. Efficacy of robotic rehabilitation of ankle impairments in children with cerebral palsy. Annu Int Conf IEEE Eng Med Biol Soc. (2010) 2010:4481–4. doi: 10.1109/IEMBS.2010.5626043
56. Bulea, TC, Lerner, ZF, Gravunder, AJ, and Damiano, DL. Exergaming with a pediatric exoskeleton: facilitating rehabilitation and research in children with cerebral palsy. IEEE Int Conf Rehabil Robot. (2017) 2017:1087–93. doi: 10.1109/ICORR.2017.8009394
57. Zhang, QL . The late development of Myo guide EMG and electrical stimulation guided injection instrument [master’s thesis]. (2013) Kunming Medical University
58. Tan, LH, Hu, XL, and Li, WB. Application of self-made wrist rehabilitation training device on wrist function in children with cerebral palsy. Chin J Phys Med Rehabil. (2017) 39:763–5. doi: 10.3760/cma.j.issn.0254-1424.2017.10.011
59. Maciejasz, P, Eschweiler, J, Gerlach-Hahn, K, Jansen-Troy, A, and Leonhardt, S. A survey on robotic devices for upper limb rehabilitation. J Neuro Oncol. (2014) 11:3. doi: 10.1186/1743-0003-11-3
60. Yan, TT, and Zheng, W. Application progress of artificial intelligence technology in cognitive and social function rehabilitation of children with autism spectrum disorder. Chin J Rehabil Med. (2019) 34:994–8. doi: 10.3969/j.issn.1001-1242.2019.08.024
61. Yue, SW . Progress in physical therapy. Chin J Rehabil Med. (2020) 35:1153–7. doi: 10.3969/j.issn.1001-1242.2020.10.001
62. Zhao, Q, Wang, J, Li, Z, Song, L, and Li, X. Effect of anodic transcranial direct current stimulation combined with speech language therapy on nonfluent Poststroke aphasia. Neuromodulation. (2021) 24:923–9. doi: 10.1111/ner.13337
63. Bikson, M, Esmaeilpour, Z, Adair, D, Kronberg, G, Tyler, WJ, Antal, A, et al. Transcranial electrical stimulation nomenclature. Brain Stimul. (2019) 12:1349–66. doi: 10.1016/j.brs.2019.07.010
64. Zhou, H, Niu, L, Meng, L, Lin, Z, Zou, J, Xia, X, et al. Noninvasive ultrasound deep brain stimulation for the treatment of Parkinson's disease model mouse. Research. (2019) 2019:1748489. doi: 10.34133/2019/1748489
65. Hoffman, BU, Baba, Y, Lee, SA, Tong, CK, Konofagou, EE, and Lumpkin, EA. Focused ultrasound excites action potentials in mammalian peripheral neurons in part through the mechanically gated ion channel PIEZO2. Proc Natl Acad Sci USA. (2022) 119:e2115821119. doi: 10.1073/pnas.2115821119
66. Shan, EX, Zhang, PY, and Gao, L. Expert consensus on four-diagnosis quantitative index system of TCM for child cerebral palsy. Chin J Tradition Chin Med Inform. (2023) 30:1–10. doi: 10.19879/j.cnki.1005-5304.2023095
Keywords: cerebral palsy, artificial intelligence, rehabilitation equipment, stimulation mode, review
Citation: Guo C, Cun Y, Xia B, Chen S, Zhang C, Chen Y, Shan E, Zhang P and Tai X (2024) An analysis of stimulation methods used in rehabilitation equipment for children with cerebral palsy. Front. Neurol. 15:1371332. doi: 10.3389/fneur.2024.1371332
Received: 16 January 2024; Accepted: 31 May 2024;
Published: 18 June 2024.
Edited by:
Eishi Asano, Wayne State University, United StatesReviewed by:
Corina Sporea, Carol Davila University of Medicine and Pharmacy, RomaniaCopyright © 2024 Guo, Cun, Xia, Chen, Zhang, Chen, Shan, Zhang and Tai. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Pengyue Zhang, enB5MTk4MDIwMDBAMTYzLmNvbQ==; Xiantao Tai, dGFpeGlhbnRhb0AxNjMuY29t
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.