- 1Department of Cardiology, The First College of Clinical Medical Sciences, China Three Gorges University, Yichang, Hubei, China
- 2Institute of Cardiovascular Diseases, China Three Gorges University, Yichang, Hubei, China
Background: While cerebral infarction in children is rare, its prognosis is poor, and this condition can seriously burden society and families. A correlation between patent foramen ovale (PFO) and ischemic stroke has not been found in pediatric patients.
Case presentation: We report a 7-year-old boy who suffered from multiple cerebral infarctions. Subsequently, the patient was diagnosed with an abnormal shunt of PFO. He underwent PFO closure and was followed up for 1 year. The patient did not experience any further cerebral infarction.
Conclusions: With this case report, we want to illustrate that although the incidence rate of ischemic cerebral infarction in adolescents is very low, we should not neglect the role of PFO. Therefore, after exclusion other causes of cerebral infarction, PFO should be considered in adolescent and adult stroke patients with adult closure criteria in the same way.
Background
Cerebral infarction occurs very rarely in adolescents, but the prognosis is usually poor. A patent foramen ovale (PFO) is a highly prevalent finding in cryptogenic ischemic stroke, particularly in adults, and the association between PFO and ischemic stroke has been documented in a large number of observational studies. However, this correlation has not been confirmed in pediatric patients. With the development of ultrasound technology, an increasing number of cases have been found to be related to paradoxical embolization through PFO and embolie strokes. Here, we report a young child with a cerebral infarction who presented with paradoxical embolism through PFO.
Case presentation
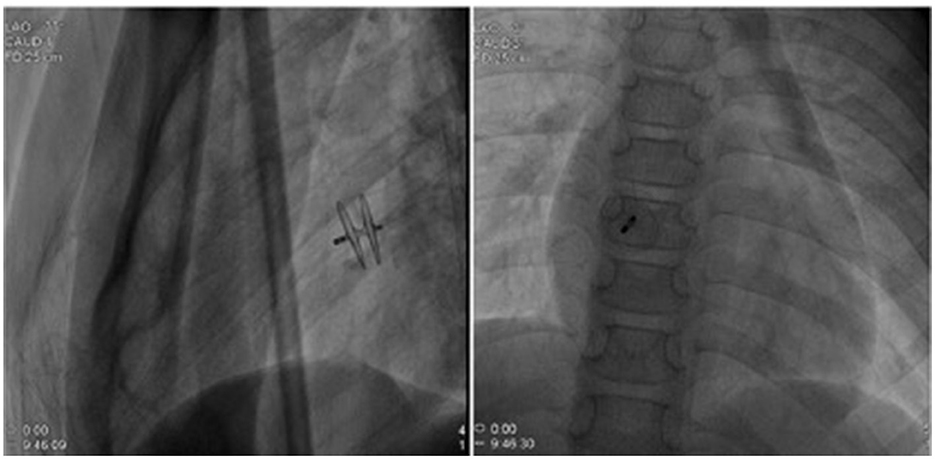
A 7-year-old boy was referred to our center due to headache and left limb weakness. Craniocerebral magnetic resonance imaging revealed multiple patchy abnormal signals in the bilateral paraventricular basal ganglia area and the right half oval center. Softening lesions were considered, and no notable abnormalities were observed in the cerebral blood vessels (Figure 1). Transthoracic echocardiography indicated a right to left shunt signal with a width of ~2.5 mm in the middle of the atrial septum. Transesophageal echocardiography revealed a fissure-like echo at the foramen ovale of the atrial septum, with a width of ~2.2 mm and a length of ~15 mm (Figure 2). Right ventricular contrast-enhanced ultrasound indicates that a large amount of microbubble echoes were observed in the second cardiac cycle of the left heart in a resting state. During the Valsalva maneuver, a large amount of microbubble echoes were observed in the first cardiac cycle of the left heart (Figure 3, Left). The transcranial doppler (TCD) foaming experiment indicated that there was no microbubble echo in the resting state, and a large number of microbubble echoes were observed within 10 s during the Valsalva maneuver. Bilateral lower limb venous ultrasound showed no obvious thrombosis or plaque formation. The laboratory examination (included D-dimer) and electrocardiogram (ECG) showed no abnormalities. Inquire about the patient's medical history. The patient has no family history of coagulation disorders. A detailed medical history inquiry revealed that at the age of 2 years, the child experienced headaches, unclear language, and left limb weakness. Emergency cranial magnetic resonance imaging showed patchy and slightly longer T1 and T2 signal shadows in the bilateral basal ganglia area, with a larger range on the right side and a maximum cross-sectional size of approximately 1.5 × 1.2 cm. Bilateral abnormal signals in the basal ganglia area were observed, indicating demyelination changes. The relationship between recurrent cerebral infarction and abnormal shunting caused by PFO is considered in patients. The PFO closure decision was adopted after a detailed discussion. This procedure was performed under local anesthesia with the implantation of an 18 mm Amplatzer PFO device (Figure 4). The patient was discharged the next day. Antiplatelet therapy was administered 6 months after PFO closure. Follow-up after 1 year did not reveal any further symptoms of headache or limb weakness. After PFO closure, no new infarct was found on cranial MRI. The right ventricular contrast-enhanced ultrasound was negative, and the TCD foaming test was negative (Figure 3, Right).
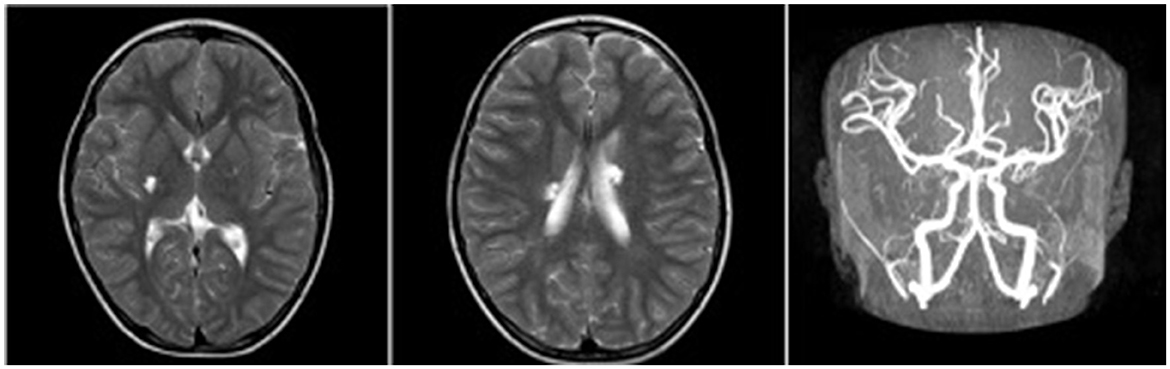
Figure 1. Craniocerebral MRI revealed multiple patchy abnormal signals in the bilateral paraventricular basal ganglia area and the right half oval center, and cerebral MRA showed no abnormalities.
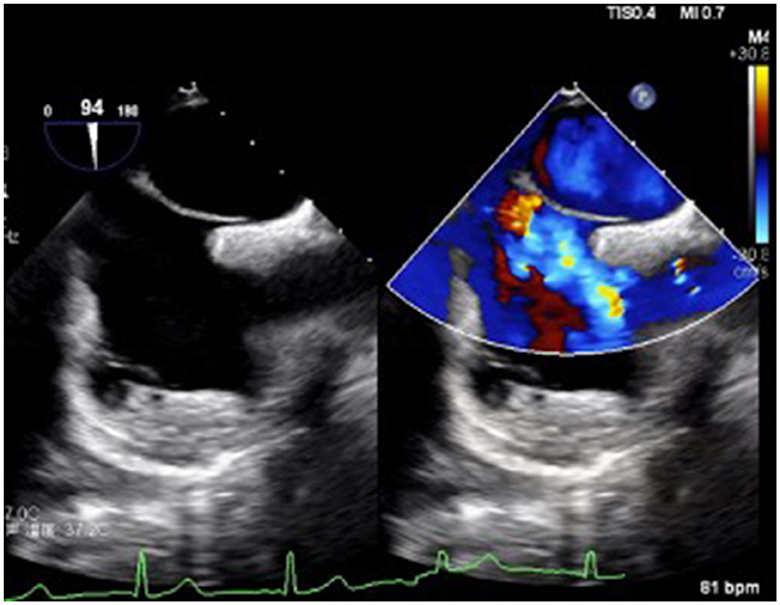
Figure 2. TEE revealed a foramen ovale of the atrial septum, with a width of ~2.2 mm and a length of ~15 mm.
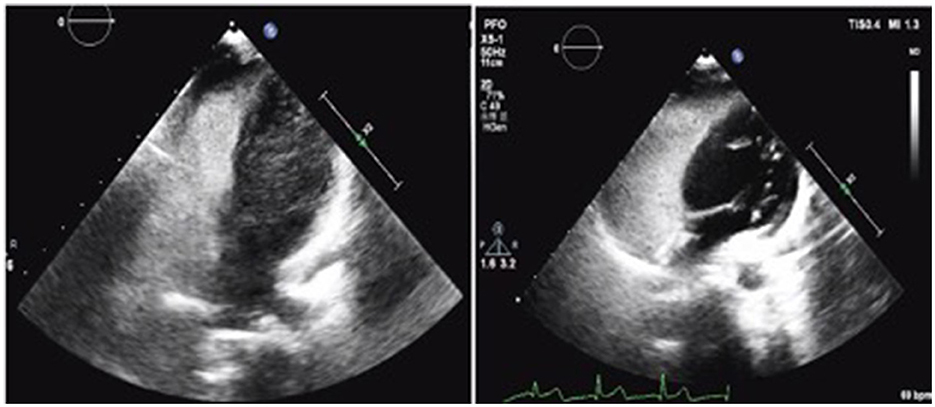
Figure 3. (Left) Before PFO closure, right ventricular contrast-enhanced ultrasound indicated positive results. (Right) After 6 months of PFO closure, the right ventricular contrast-enhanced ultrasound was negative, and the TCD foaming test was negative.
Discussion and conclusions
The foramen ovale is a separation between the septum primum and septum secundum at the anterior–superior portion of the septum, which is present in the fetus and enables the venous blood to bypass the non-functioning fetal lung and go directly to the left side of the heart. After birth, this communication closes in the majority of people but remains patent in 25–30% (1). The PFO, while frequently clinically silent and only open when the pressure increases on the right cardiac cavities, such as during a Valsalva maneuver, can exert pathological effects by allowing thrombi to transit from the venous to the arterial circulation (paradoxical embolization) (2).
Among adolescent patients, the incidence rate of arterial ischemic stroke (AIS) is estimated to be 0.6 per 100,000, indicating an important cause of morbidity and mortality among adolescents, and the risk of recurrence is also high (3). In these patients, the cause of cardiac embolism was discovered in 15%, with 50% suffering from PFO (3). In adults, the correlation between cryptogenic stroke and PFO has been validated. Multiple studies have shown that PFO closure can significantly reduce the risk of cryptogenic AIS recurrence compared to medical antithrombotic therapy (4–6). However, the pathogenic role of PFO in childhood remains controversial. The pediatric guidelines only suggest that cryptogenic stroke may benefit from PFO closure.
Our case shows multiple cryptogenic strokes in a 7-year-old boy, possibly due to an abnormal shunt of PFO. The etiology of stroke in children is complex, and the common diseases of ischemic stroke in children include congenital heart malformations, sickle cell disease, infections, and collagen tissue abnormalities (7). However, nearly half of these cases are found in previously healthy children, known as cryptogenic stroke. In adults, the mechanisms of PFO causing ischemic stroke mainly include paradoxical embolism, in situ thrombosis, and arrhythmias. Paradoxical embolism is the most common mechanism, and embolism from the venous system or right atrium can directly access the arterial system through PFO, leading to ischemic stroke (8). In situ thrombosis refers to the formation of thrombi in the tunnel of PFO, and some studies suggest that PFO patients in a hypercoagulable state have a higher risk of stroke (9). There are also some reports of thrombi attached to the atrial septum and foramen ovale (10). Previous studies have found that PFO can alter left atrial electrical activity and easily lead to the occurrence of some atrial arrhythmias (11). In addition, Hanley et al. observed that some high-risk foramen ovale are associated with the occurrence of atrial fibrillation (AF) (12). There is currently insufficient clinical evidence to demonstrate the correlation between PFO and stroke in pediatric stroke patients compared to adult stroke patients. However, there are still some small studies indicating that cryptogenic stroke may benefit from PFO closure (13).
To summarize, with this case report, we want to illustrate that PFO meeting the adult criteria for closure should be considered the same way in adolescents as in adult stroke patients after careful evaluation to rule out other causes of stroke (including hypercoagulable state, other sources of cardiac embolism, and intracranial and extracranial arterial lesions including dissection). There was no significant difference in safety and effectiveness of this treatment.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee of Yichang Central People's Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin. Written informed consent was obtained from the individual(s), and minor(s)' legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Author contributions
Z-qZ: Writing – review & editing, Writing – original draft. J-wD: Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the National Natural Science Foundation of China (Grant Nos. 81770456 and 81400794) and the Medical and Health Research Project of Yichang city, China (Grant No. A21-2-015).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Rana BS, Thomas MR, Calvert PA, Monaghan MJ, Hildick-Smith D. Echocardiographic evaluation of patent foramen ovale prior to device closure. JACC Cardiovasc Imaging. (2010) 3:749–60. doi: 10.1016/j.jcmg.2010.01.007
2. Sultan FA, Allen S, Sharif M, Mookadam F. Paradoxical thrombus ‘caught in the act': case report and review of the literature. Am J Med. (2017) 130:e23–5. doi: 10.1016/j.amjmed.2016.07.022
3. Rambaud T, Legris N, Bejot Y, Bellesme C, Lapergue B, Jouvent E, et al. Acute ischemic stroke in adolescents. Neurology. (2020) 94:e158–69. doi: 10.1212/WNL.0000000000008783
4. Carroll JD, Saver JL, Thaler DE, Smalling RW, Berry S, MacDonald LA, et al. Closure of patent foramen ovale versus medical therapy after cryptogenic stroke. N Engl J Med. (2013) 368:1092–100. doi: 10.1056/NEJMoa1301440
5. Poli S, Siebert E, Mbroh J, Poli K, Krumbholz M, Mengel A, et al. Closure or medical therapy of patent foramen ovale in cryptogenic stroke: prospective case series. Neurol Res Pract. (2021) 3:16. doi: 10.1186/s42466-021-00114-3
6. Meier B, Kalesan B, Mattle HP, Khattab AA, Hildick-Smith D, Dudek D, et al. Percutaneous closure of patent foramen ovale in cryptogenic embolism. N Engl J Med. (2013) 368:1083–91. doi: 10.1056/NEJMoa1211716
7. Ganesan V, Prengler M, McShane MA, Wade AM, Kirkham FJ. Investigation of risk factors in children with arterial ischemic stroke. Ann Neurol. (2003) 53:167–73. doi: 10.1002/ana.10423
8. Mojadidi MK, Zaman MO, Elgendy IY, Mahmoud AN, Patel NK, Agarwal N, et al. Cryptogenic stroke and patent foramen ovale. J Am Coll Cardiol. (2018) 71:1035–43. doi: 10.1016/j.jacc.2017.12.059
9. Ballerini L, Cifarelli A, Ammirati A, Gimigliano F. Patent foramen ovale and cryptogenic stroke. A critical review. J Cardiovasc Med. (2007) 8:34–8. doi: 10.2459/01.JCM.0000247433.82322.df
10. Nombera NR, Guerra M, MLÁG A, Bernal MA. A thrombus trapped in a patent foramen ovale: a migrant out of the ordinary. Arch Cardiol Mex. (2023) 93:497–8. doi: 10.24875/ACME.M23000450
11. Sun H, Zhou C, Xu L, Xu T. A meta-analysis of the association of atrial septal abnormalities and atrial vulnerability. Medicine. (2021) 100:e27165. doi: 10.1097/MD.0000000000027165
12. Hanley PC, Tajik AJ, Hynes JK, Edwards WD, Reeder GS, Hagler DJ, et al. Diagnosis and classification of atrial septal aneurysm by two-dimensional echocardiography: report of 80 consecutive cases. J Am Coll Cardiol. (1985) 6:1370–82. doi: 10.1016/s0735-1097(85)80228-x
Keywords: patent foramen ovale (PFO), cerebral infarction, paradoxical embolism, young child, case report
Citation: Zhang Z-q and Ding J-w (2024) Where the cerebral infarction meets child, be vigilant about patent foramen ovale: a case report. Front. Neurol. 15:1363867. doi: 10.3389/fneur.2024.1363867
Received: 31 December 2023; Accepted: 30 April 2024;
Published: 17 May 2024.
Edited by:
Pierluigi Zoccolotti, Sapienza University of Rome, ItalyReviewed by:
Andrew T. Lovering, University of Oregon, United StatesAli Sazci, Okan University, Türkiye
Copyright © 2024 Zhang and Ding. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jia-wang Ding, ZGluZ2ppYXdhbmdAMTYzLmNvbQ==
 Zai-qiang Zhang
Zai-qiang Zhang Jia-wang Ding1,2*
Jia-wang Ding1,2*