
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
STUDY PROTOCOL article
Front. Neurol., 15 September 2024
Sec. Experimental Therapeutics
Volume 15 - 2024 | https://doi.org/10.3389/fneur.2024.1358859
This article is part of the Research TopicComplementary and Alternative Therapy for Pain Disorders: From Bench to Clinical PracticeView all 18 articles
 Junning Zhang1,2*
†
Junning Zhang1,2*
† Yuehan Ren1
†
Yuehan Ren1
† Weizhen Wu1
†
Weizhen Wu1
† Yi Yuan1
Yi Yuan1 Jiale Wang3
Jiale Wang3 Yi Tang4
Yi Tang4 Yunqiao Zhou4
Yunqiao Zhou4 Yizhuo Qiao5
Yizhuo Qiao5 Baoqin Liu6*
Baoqin Liu6*Background: Cancer patients frequently suffer pain as one of their symptoms. It includes acute and chronic pain and is one of the most feared symptoms for patients. About one-third of adults actively undergoing cancer treatment suffer from pain related to their condition. Cancer pain control remains suboptimal due to a lack of assessment, knowledge, and access. Fire needle therapy, a traditional Chinese medicine, offers a potentially beneficial addition to current pain management approaches. This protocol outlines a systematic review and meta-analysis to compile evidence and examine the pain-relieving effects and safety of fire needle therapy for cancer patients.
Methods and analysis: We will systematically search China National Knowledge Infrastructure (CNKI), Wanfang Database, China Biology Medicine disc (CBM), China Science and Technology Journal Database (CSTJ or VIP), PubMed, Web of Science, Embase, Cochrane Central Registry of Controlled Trials (CENTRAL), Chinese Clinical Trial Registry (Chictr), Opengrey, Worldcat, and Scopus from inception through July 2023. Random control trials (RCTs) include all types of cancer patients (age ≥ 18 years) complaining of pain. The primary outcome will be changes in pain intensity measured by Visual Analogue Scale (VAS), Numerical Rating Scale (NRS), Neuropathic Pain Scale (NPS), or Brief Pain Inventory (BPI). Secondary outcomes include quality of life (EORTC QLQ-C30 and GCQ), performance status (KPS), times of burst pain, treatment response rate, the dose reduction of analgesic drugs, and side effects rates. Utilizing the Cochrane risk bias measurement tool: Risk of Bias 2 (RoB 2), the trials’ quality will be evaluated, and meta-analysis will be performed using RevMan software (version 5.4).
Discussion: This systematic review will be the first comprehensive review of the literature to provide a meta-analysis of fire needle therapy for cancer pain, including only Random control trials (RCTs). For the sake of transparency and to avoid future duplication, the publication of this protocol offers a clear illustration of the procedures utilized in this evaluation. The results of our future studies may provide a new approach and theoretical basis for the treatment of cancer pain by medical oncology professionals.
Systematic review registration: https://www.crd.york.ac.uk/prospero/, identifier CRD42023418609.
Pain is a prevalent symptom among cancer patients (1). It includes acute pain and chronic pain (2). Cancerous tumors can cause pain by pressing on nerves, bones, or organs, and releasing chemicals that can cause pain (2, 3). The cancer’s destruction of surrounding tissue can also lead to pain (2). Around one-third of adults undergoing active cancer treatment suffer from pain related to their condition (4). Cancer pain can have a significant effect on a patient’s day-to-day activities as well. Cancer pain can lead to sleep disturbances (5), fatigue, nausea, and vomiting (6), all of which can make it difficult to carry out normal activities and enjoy life. Pain can also contribute to feelings of depression and anxiety, further affecting a patient’s quality of life (7). In addition to the physical toll cancer pain takes on patients, it can also have a significant economic burden (8). The cost of pain medications and other treatments can be quite high, and patients may also incur additional expenses related to managing their pain, such as travel to medical appointments or modifications to their home or workplace. This can place a strain on patients and their families, both emotionally and financially (9).
There are many treatments available for pain such as pharmacological agents, nerve blocks, psychological therapies, physiotherapy, alternative remedies, and surgery (10–12). What’s more, a new treatment option, contextual effects (placebo and nocebo effects), should be in the spotlight (13). It has been identified to modulate chronic pain as well as musculoskeletal pain (14, 15). Pain patients use the contextual effect to explain the effects of treatment, while it has been applied in the fields of rehabilitation, physical therapy, and nursing (16–19). For the treatment of cancer pain, the WHO proposed three-step analgesic approach is a major part of this (20). For mild pain, non-opioid analgesics like paracetamol or ibuprofen are used in the first stage; for moderate pain, weak opioids like codeine or tramadol are used in the second step; and for severe pain, strong opioids like morphine or fentanyl are used in the third step (21).
However, there are several restrictions and disadvantages to this strategy. First, due to inadequate opioid prescription or therapy, many patients do not experience sufficient pain relief (22, 23). Second, opioids have serious adverse effects, including addiction, constipation, nausea, drowsiness, and respiratory depression (11, 24). Third, due to supply problems and regulatory restrictions, opioids are frequently unavailable or unaffordable in low- and middle-income nations (25). Consequently, other treatments have been explored and created to decrease reliance on opioids. Fire needle therapy is one of them.
By burning a specific needle till it becomes red and immediately penetrating the skin at the body’s acupuncture point, fire needle therapy is a form of traditional Chinese medicine that heals illnesses (26). Fire needle therapy, which combines acupuncture, direct moxibustion, and needling into one method, is known for its simplicity, practicality, efficiency, and quickness (27, 28). Fire needle therapy has the significant efficacy in treating pain and has sufficient theoretical basis for treating cancer pain (29). According to studies, the use of a fire needle eliminates or improves pathological alterations such as local tissue edema, hyperemia, exudation, and adhesion by stimulating the illness site and reflex point. This boosts metabolism and blood flow while reducing inflammation (30). Fire needle therapy can reduce the levels of pain transmitters in the central and peripheral nerve systems, including substance P and 5-hydroxytryptamine (31, 32). In particular, TNF(tumor necrosis factor) and interleukin-1 levels can both be decreased with fire needle therapy (33). Additionally, it can encourage the body to release more of a vascular endothelial growth factor that is necessary for damage recovery (34). In terms of Traditional Chinese medicine, the acupoints targeted by the fire needle therapy may help to regulate the flow of qi (life force energy) in the body, which could have a positive effect on pain perception (27).
As a result, based on the most recent research, we designed this study to evaluate the efficacy and safety of fire needle therapy in the management of pain in cancer patients. We will also look into the efficient fire needle points and treatment regimens to recommend more usable therapies for clinical care.
This review protocol is registered in the International Prospective Register of Systematic Reviews (PROSPERO) as CRD42023418609. Reporting standard followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) protocols (See Supplementary material).
Only RCTs with cancer pain patients treated with fire needle therapy are eligible for inclusion, and there will be no language restrictions during the search process.
The treatment group will receive fire needle therapy without any restrictions on the depth, frequency, intensity, or area of application of needling. Fire needle therapy either used alone or combined with other therapies (e.g., modern medicine, other acupuncture methods) will be included. RCTs compared fire needle therapy directly with different types of TCM (e.g., herbal decoction, another form of acupuncture) will be excluded from this study.
All the active therapies will be part of the control group. Sham fire needling, no treatment, usual care, oral analgesics, and other active therapies may be included. Placebo, blank controls will be considered for inclusion.
Considering that the population of our study is cancer patients presenting with pain, the results of the evaluation of pain-related scales will be chosen as our primary outcome indicators for analysis, including visual analog scale (VAS), numerical rating scale (NRS), Neuropathic Pain Scale (NPS) and Brief Pain Inventory (BPI). Secondary outcome indicators such as Karnofsky performance status (KPS), the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire (EORTC-QLQC30), the General Comfort Questionnaire (GCQ), times of burst pain, treatment response rate, the dose reduction of analgesic drugs, and side effect rates will be included for analysis. If trials involved any of the above outcome indicators will be included in the analysis.
• Duplicate studies;
• Studies that report only abstracts but not complete data;
• Articles with obvious statistical or logical errors.
The following databases will be searched from their inception through July 2023: China National Knowledge Infrastructure (CNKI), Wanfang Database, China Biology Medicine disc (CBM), China Science and Technology Journal Database (CSTJ or VIP), PubMed, Web of Science, Embase, Cochrane Central Registry of Controlled Trials (CENTRAL), Chinese Clinical Trial Registry (Chictr), Opengrey, Worldcat, and Scopus.
Any eligible studies potentially overlooked will also be manually identified by scanning the reference lists of related systematic reviews and conference proceedings.
See Supplementary material for details.
Duplicates were found and eliminated using Zotero software after gathering the search results from these databases. Then, two independent reviewers (JN Z and YH R) will browse the titles and abstracts of the studies, and studies that do not meet the eligibility criteria based on the titles and abstracts will be excluded. The remaining studies’ complete texts will be located and reviewed for the last round of selection. The arbiter (WZ W) shall resolve any differences of opinion on the data selection. The method for finding and screening studies will be depicted in a PRISMA flow diagram (see Figure 1).
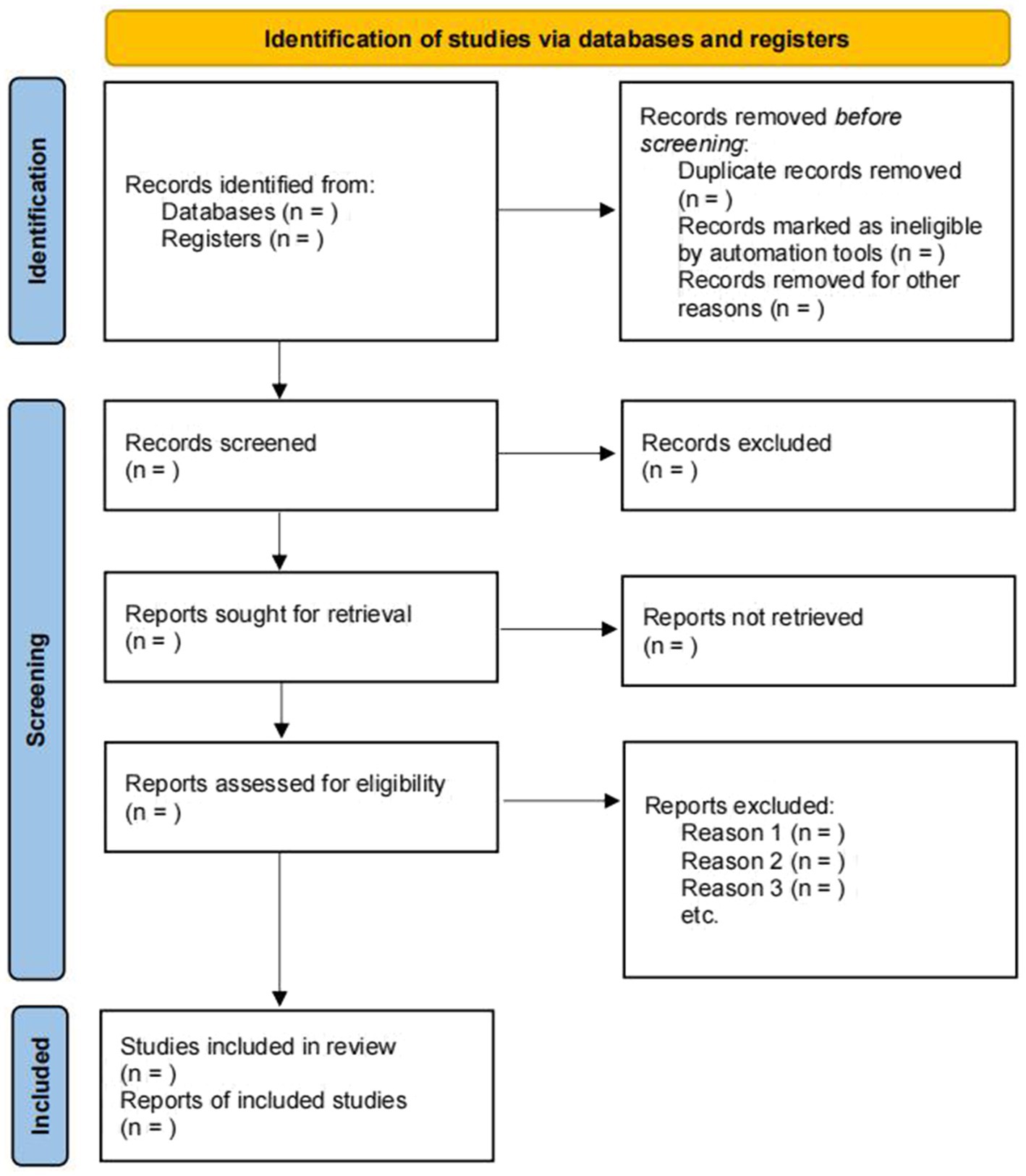
Figure 1. Flowchart of the literature review and selection process (35).
Two reviewers JN Z and YH R will use a standardized data extraction form to extract the following information for each included RCT:
• Basic information about the RCT: such as title, authors, date of publication, and number of subjects involved;
• Criteria for inclusion of subjects: such as restrictions on demographic information, diagnostic criteria for disease, age, sex, ethnicity, the severity of disease, and duration of disease;
• Details of interventions and controls: such as the method of fire needle therapy, site of acupuncture, dose, duration of treatment, and combined intervention regimen;
• Outcome indicators: names, definitions, and results of outcome indicators;
• Methodology entries: randomized methods, blinded methods (including blinding of physicians, patients, and outcome assessors), allocation concealment, missing data, selective reporting.
A third investigator (WZ W) will make judgments about any differences and questions. Following a transfer of data, the synthesis will be performed using RevMan software (version 5.4, Cochrane Collaboration, Oxford, United Kingdom) (36).
Two authors (JN Z and YH R) will independently evaluate the risk of bias using the Cochrane risk bias measurement tool: Risk of Bias 2 (RoB 2). The following biases will be assessed. The tool consists of the following 5 domains, randomization process, deviations from intended interventions, missing outcome data, measurement of the outcome, and selection of the reported result. The authors classified studies as low risk of bias, some concerns or high risk of bias.1 The arbiter (WZ W) will resolve any disagreements regarding the bias assessment. The quality assessment results will be illustrated in a risk-of-bias graph and a risk-of-bias summary table.
Data synthesis for the meta-analysis will be accomplished using the RevMan version 5.4 software. Referring to Chapter 10 of the Cochrane Handbook for Systematic Reviews of Interventions,2 we chose to use a fixed-effects model or a random-effects model based on the magnitude of heterogeneity. When heterogeneity was significant (I square ≥ 50%, or p < 0.05), a random-effects model was used; when it was not significant (I square < 50% and p ≥ 0.05), a fixed-effects model was used. A 95% confidence interval (CI) will be used to determine the mean difference (MD) for continuous data. The risk ratio (RR) with 95% confidence interval (CI) will be utilized for dichotomous data. Weighted mean difference (WMD) will be used in subgroup analyses comparing different treatments, and standardized mean difference (SMD) will be used in subgroup analyses comparing the efficacy of the same treatment in different populations.
If the full text of an article is not available, the reviewers will attempt to contact the author to obtain it. If the author cannot be contacted, this article will be excluded from the analysis. The state of relevant articles for which the authors were contacted will be reported in the study results and provide a descriptive summary of the main results of the relevant articles.
For heterogeneity among the outcomes of the included studies, the Chi2 test will be used. The following I2 thresholds will be applied in this study:
• I2:0–40%: probably not significant;
• I2:30–60%: possibly moderate heterogeneity;
• I2:50–90%: possibly significant heterogeneity;
• I2:75–100%: possibly substantial heterogeneity.
The statistical value of I2 will depend on the magnitude of its influence factors and the strength of evidence of heterogeneity (such as the p-value of the Chi2 test). The effects of clinical and statistical heterogeneity will be addressed when examining the analysis results (37).
A random-effects model will be applied if significant statistical heterogeneity is discovered; otherwise, a fixed-effects model will be applied. Also, we will assess clinical heterogeneity, including study population, study design, and treatment protocols. The results of the synthesis will be visualized in the form of a forest plot. If heterogeneity is too great, quantitative analysis will be abandoned in favor of qualitative analysis.
If over 10 RCTs are included in the meta-analysis, publication bias will be evaluated using funnel plots. If there are less than 10 RCTs in the meta-analysis, we will employ Egger’s test and Begg’s test for publication bias.
If the data permits, we will perform the following subgroup analyses:
• The depth, frequency, and intensity of different piercings;
• Cancer pain of the patient (different cancers).
To assess the impact of study design, sample size, and methodological quality, a sensitivity analysis will be performed and, where possible, the robustness of the data synthesis will be determined.
Considering the type of study we included as a randomized controlled trial, randomized controlled trials should be initially rated as high-quality evidence according to the GRADE approach. However, due to limitations in five aspects, the quality of evidence may be downgraded to some extent. These five aspects include: study design limitations (downgrade 1–2 levels), inconsistency of results (downgrade 1–2 levels), indirectness (downgrade 1 level), imprecision (downgrade 1 level), and publication bias (downgrade 1 level). The degree of the downgrade will be determined with reference to the Chapter V of the Cochrane Handbook for Systematic Reviews of Interventions (38), and related literature (39).
This meta-analysis data processing phase will utilize published clinical trial data without direct patient or public participation.
Because the data used in the study are not individualized, ethical approval is not required for this study. Necessary protocol revisions will be documented in a comprehensive review. The study findings will be published in peer-reviewed journals and potentially presented at applicable conferences.
In recent years, due to changes in living environment, the incidence of cancer continues to rise and about 69% of patients suffer cancer pain, including pain caused by cancer, cancer-related, lesions and anti-cancer treatment (40). Cancer pain can occur at any stage from early to late stage of cancer, seriously affecting patients’ treatment and daily life (41). The WHO’s three-step analgesic ladder for cancer pain control is the primary approach for managing cancer pain, with opioids as the core component of the analgesia. However, long-term use of opioids can cause adverse reactions such as constipation, nausea, and vomiting, as well as many problems such as addiction, dependence, and poor tolerance (42). Compared with Western medicine, acupuncture therapy in the treatment of cancer pain is not only effective but also has the advantages of safety, simple operation, small adverse reactions, no dependence, and addiction (43).
Research has shown that pain relief from acupuncture is associated with neuro-humoral factors (44), which can relieve pain by encouraging the release of endogenous opioid peptides, increasing local endorphin levels and peripheral opioid receptor activity during inflammatory responses, and suppressing the synthesis of endogenous pain (45, 46). The stimulation amount of fire needle is much greater than that of traditional acupuncture (29). Thus, fire needle therapy may be able to treat pain that cannot be relieved by ordinary acupuncture (47). Several studies have found that fire needle alone or combined with Western medicine can significantly relieve the pain symptoms of cancer pain patients and reduce the NRS score (47, 48). Compared to using only Western medicine, fire needling alone or in combination with Western medicine demonstrates higher efficacy and lower incidence of adverse effects (48–51). In conclusion, fire needle is an appropriate treatment for cancer pain and should be gradually promoted in clinical practice.
There are some limitations of fire needle therapy. Firstly, there is a fearfulness in patients and a poor reception of that. Secondly, the efficacy and safety of fire-needle therapy need further research and proof. Thirdly, there are potential risks including pain, skin lesions, allergy, and other adverse reactions (52, 53).
This review aims to present information on the different acupuncture points and fire needle therapy that can be used to treat pain in cancer patients. It will cover more than just the effects of fire needling on symptoms in patients with cancer pain. This study may have practical implications for utilizing fire needle therapy in oncology. It could help guide the application of fire needling as an alternative treatment for cancer pain management, thus helping clinicians determine whether fire needle therapy is an effective option to incorporate into pain management programs for cancer patients.
However, this study has many limitations. Additional factors that could influence the results include the participants’ experience and expectations with acupuncture, the potential diversity of individualized treatments, and the minimization of inclusion and exclusion criteria (54). In addition, the current study may have some methodological or research quality problems, which may lead to the fact that the exactness of the evidence that we end up with in our study may not be very high. To solve the above problems, we will set strict inclusion and exclusion criteria in the literature screening and data extraction stage, and try to select only the higher quality-studies. Quality assessment will be conducted to differentiate the quality of studies. We will also improve the certainty of evidence by designing and implementing high-quality original studies when conditions permit. In the meantime, we will call for more high-quality studies of RCTs, pending further evidence accumulation.
JZ: Conceptualization, Formal analysis, Investigation, Writing – original draft, Writing – review & editing. YR: Software, Writing – original draft, Writing – review & editing. WW: Data curation, Writing – original draft, Writing – review & editing. YY: Writing – original draft, Writing – review & editing. JW: Writing – review & editing. YT: Writing – review & editing. YZ: Writing – review & editing. YQ: Writing – review & editing. BL: Funding acquisition, Writing – original draft, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2024.1358859/full#supplementary-material
1. Kurtin, S, and Fuoto, A. Pain management in the cancer survivor. Semin Oncol Nurs. (2019) 35:284–90. doi: 10.1016/j.soncn.2019.04.010
2. Russo, MM, and Sundaramurthi, T. An overview of cancer pain: epidemiology and pathophysiology. Semin Oncol Nurs. (2019) 35:223–8. doi: 10.1016/j.soncn.2019.04.002
3. Yoon, SY, and Oh, J. Neuropathic cancer pain: prevalence, pathophysiology, and management. Korean J Intern Med. (2018) 33:1058–69. doi: 10.3904/kjim.2018.162
4. van den Beuken-van Everdingen, MHJ, Hochstenbach, LMJ, Joosten, EAJ, Tjan-Heijnen, VCG, and Janssen, DJA. Update on prevalence of pain in patients with cancer: systematic review and meta-analysis. J Pain Symptom Manag. (2016) 51:1070–1090.e9. doi: 10.1016/j.jpainsymman.2015.12.340
5. Jakobsen, G, Engstrøm, M, Fayers, P, Hjermstad, MJ, Kaasa, S, Kloke, M, et al. Sleep quality with WHO Step III opioid use for cancer pain. BMJ Support Palliat Care. (2019) 9:307–15. doi: 10.1136/bmjspcare-2017-001399
6. Henson, LA, Maddocks, M, Evans, C, Davidson, M, Hicks, S, and Higginson, IJ. Palliative care and the management of common distressing symptoms in advanced cancer: pain, breathlessness, nausea and vomiting, and fatigue. J Clin Oncol. (2020) 38:905–14. doi: 10.1200/JCO.19.00470
7. Li, XM, Xiao, WH, Yang, P, and Zhao, HX. Psychological distress and cancer pain: Results from a controlled cross-sectional survey in China. Sci Rep. (2017) 7:39397. doi: 10.1038/srep39397
8. Bao, Y, Zhang, H, Hartung, DM, Witkin, LR, and Paice, JA. Medicare part D coverage restrictions and patient cost-sharing for opioids commonly used for cancer pain, 2015-2021. JCO Oncol Pract. (2022) 18:e1574–86. doi: 10.1200/OP.21.00867
9. Cassileth, BR, and Keefe, FJ. Integrative and behavioral approaches to the treatment of cancer-related neuropathic pain. Oncologist. (2010) 15:19–23. doi: 10.1634/theoncologist.2009-S504
10. Coveler, AL, Mizrahi, J, Eastman, B, Apisarnthanarax, SJ, Dalal, S, McNearney, T, et al. Pancreas cancer-associated pain management. Oncologist. (2021) 26:e971–82. doi: 10.1002/onco.13796
11. Swarm, RA, Paice, JA, Anghelescu, DL, Are, M, Bruce, JY, Buga, S, et al. Adult cancer pain, version 3.2019, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw. (2019) 17:977–1007. doi: 10.6004/jnccn.2019.0038
12. Candido, KD, Kusper, TM, and Knezevic, NN. New cancer pain treatment options. Curr Pain Headache Rep. (2017) 21:12. doi: 10.1007/s11916-017-0613-0
13. Cook, CE, Bailliard, A, Bent, JA, Bialosky, JE, Carlino, E, Colloca, L, et al. An international consensus definition for contextual factors: findings from a nominal group technique. Front Psychol. (2023) 14:1178560. doi: 10.3389/fpsyg.2023.1178560
14. Rossettini, G, Campaci, F, Bialosky, J, Huysmans, E, Vase, L, and Carlino, E. The biology of placebo and nocebo effects on experimental and chronic pain: state of the art. J Clin Med. (2023) 12:4113. doi: 10.3390/jcm12124113
15. Rossettini, G, Colombi, A, Carlino, E, Manoni, M, Mirandola, M, Polli, A, et al. Unraveling negative expectations and nocebo-related effects in musculoskeletal pain. Front Psychol. (2022) 13:789377. doi: 10.3389/fpsyg.2022.789377
16. Rossettini, G, Palese, A, Geri, T, Mirandola, M, Tortella, F, and Testa, M. The knowledge of contextual factors as triggers of placebo and nocebo effects in patients with musculoskeletal pain: findings from a national survey. Front Psych. (2019) 10:478. doi: 10.3389/fpsyt.2019.00478
17. Hohenschurz-Schmidt, D, Thomson, OP, Rossettini, G, Miciak, M, Newell, D, Roberts, L, et al. Avoiding nocebo and other undesirable effects in chiropractic, osteopathy and physiotherapy: an invitation to reflect. Musculoskeletal Sci Prac. (2022) 62:102677. doi: 10.1016/j.msksp.2022.102677
18. Rossettini, G, Emadi Andani, M, Dalla Negra, F, Testa, M, Tinazzi, M, and Fiorio, M. The placebo effect in the motor domain is differently modulated by the external and internal focus of attention. Sci Rep. (2020) 8:12296. doi: 10.1038/s41598-018-30228-9
19. Palese, A, Cadorin, L, Testa, M, Geri, T, Colloca, L, and Rossettini, G. Contextual factors triggering placebo and nocebo effects in nursing practice: findings from a national cross-sectional study. J Clin Nurs. (2019) 28:1966–78. doi: 10.1111/jocn.14809
20. World Health Organization. Cancer Pain Relief: With a Guide to Opioid Availability. 2nd ed. Geneva, Switzerland: World Health Organization (1996).
21. World Health Organization. (2020) Palliative care. Available from: https://www.who.int/health-topics/palliative-care
22. Ju, C, Wei, L, Man, KKC, Wang, Z, Ma, TT, Chan, AYL, et al. Global, regional, and national trends in opioid analgesic consumption from 2015 to 2019: a longitudinal study. Lancet Public Health. (2022) 7:e335–46. doi: 10.1016/S2468-2667(22)00013-5
23. Marshall, VK, Chavez, MN, Rigg, KK, Lubrano di Ciccone, B, Rajasekhara, S, Efre, A, et al. Framing cancer survivors’ access to and use and disposal of prescribed opioids within the opioid epidemic. Oncol Nurs Forum. (2022) 50:25–34. doi: 10.1188/23.ONF.25-34
24. Degenhardt, L, Grebely, J, Stone, J, Hickman, M, Vickerman, P, Marshall, BDL, et al. Global patterns of opioid use and dependence: harms to populations, interventions, and future action. Lancet. (2019) 394:1560–79. doi: 10.1016/S0140-6736(19)32229-9
25. Coghlan, R, Shamieh, O, and Bloomer, MJ. Inequities of palliative care availability and access to opioids in low- and middle-income countries. Palliat Med. (2021) 36:NP1–2. doi: 10.1177/02692163211034083
26. He, P . Mechanisms and clinical applications of fire acupuncture. Chinese Med Modern Distance Educ China. (2004) 2:20–4. doi: 10.3969/j.issn.1672-2779.2004.10.010
27. Zhou, J, Li, M, Zhu, L, Yue, Y, and Luo, L. Mechanism of fire needling therapy and clinical applications. J Liaoning Univ Tradit Chin Med. (2016) 18:86–8. doi: 10.13194/j.issn.1673-842x.2016.07.026
28. Yang, J, Zhang, Q, Hu, J, and Guo, J. Similarities and differences in clinical application of fire needle and moxibustion. China J Trad Chinese Med Pharmacy. (2022) 37:2034–8. Available at: https://kns.cnki.net/kcms2/article/abstract?v=nouGVBS_tgdGulTGVRIGo98zxHE1Ugu9GUkuFOLXV1w8PZVeroZ2nCJ-s9MbMqB864136gGNRIqbKM7N-21wGsqx4oFgovenMcGocs_8b1ievkg0YaMwwcjTWkqryhn69N5lgYDXdZ1XADxISNODoQ==&uniplatform=NZKPT
29. Zhu, X, Li, Z, and Wang, X. Clinical application of fire-needling in treatment of cancer pain. J Clinical Acupuncture and Moxibustion. (2018) 34:73–5.
30. Du, X, Wen, X, Liu, D, Huang, F, Ji, X, Zhang, T, et al. Preliminary study on the therapeutic effect and effect mechanism of fire-needling. J Clinical Acupuncture and Moxibustion. (2018) 34:1–4. Available at: https://kns.cnki.net/kcms2/article/abstract?v=nouGVBS_tgdJlQ_ln_MOW-qjQ9Gno_62IGIPgnKPVoX8lt66-JaiemDRW8_AXvxsY9PHplryeL-KGM8DGWyd55lmmAIF6G4MLbxkSdZyYrey-AJhWtqbfTFxw3diFF-_mIZJCHo6I0S4JMN6BqJ64g==&uniplatform=NZKPT
31. Han, JS . Acupuncture and endorphins. Neurosci Lett. (2004) 361:258–61. doi: 10.1016/j.neulet.2003.12.019
32. Janssens, LA, Rogers, PA, and Schoen, AM. Acupuncture analgesia: a review. Vet Rec. (1988) 122:355–8. doi: 10.1136/vr.122.15.355
33. Han, R, Yang, J, Zhang, T, and Zhang, W. Effect of fire-needle intervention on serum IL-1 and TNF-α levels of rheumatoid arthritis rats. Acupuncture Res. (2012) 37:114–8. doi: 10.13702/j.1000-0607.2012.02.008
34. Li, W . Treatment of 25 cases of rheumatoid arthritis by fire needle. Shanxi J Trad Chinese Med. (2002) 3:38. doi: CNKI:SUN:SHIX.0.2002-03-029
35. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ, (2021). 372:n71. doi: 10.1136/bmj.n71
36. The Cochrane Collaboration Review Manager 5 (RevMan 5). Copenhagen: Nordic Cochrane Centre: The Cochrane Collaboration; (2020).
37. Higgins, JPT, Thomas, J, Chandler, J, Cumpston, M, Li, T, Page, MJ, et al. (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.4 (updated August 2023). Cochrane, (2023). Available from: https://training.cochrane.org/online-learning/core-software/revman
38. Higgins, JP, Thomas, J, Chandler, J, Cumpston, M, Li, T, and Page, MJ. Overviews of reviews. Cochrane Handbook for Systematic Reviews of Interventions. 6.2. Cochrane; (2021). Available from: training.cochrane.org/handbook
39. Meader, N, King, K, Llewellyn, A, Norman, G, Brown, J, Rodgers, M, et al. A checklist designed to aid consistency and reproducibility of GRADE assessments: development and pilot validation. Syst Rev. (2014) 3:82. doi: 10.1186/2046-4053-3-82
40. Zheng, C, Chen, X, Weng, L, Guo, L, Xu, H, Lin, M, et al. Benefits of mobile apps for cancer pain management: systematic review. JMIR Mhealth Uhealth. (2020) 8:e17055. doi: 10.2196/17055
41. Camps Herrero, C, Batista, N, Díaz Fernández, N, Escobar Álvarez, Y, Gonzalo Gómez, A, Isla Casado, D, et al. Breakthrough cancer pain: review and calls to action to improve its management. Clin Transl Oncol. (2020) 22:1216–26. doi: 10.1007/s12094-019-02268-8
42. Geng, G, Jia, L, Jia, Y, Jiang, Y, Li, J, Li, P, et al. Expert consensus on the treatment of opioid adverse reactions in Chinese medicine. Chin J Clin Oncol. (2019) 46:321–3. doi: 10.3969/j.issn.1000-8179.2019.07.238
43. Yang, J, Wahner-Roedler, DL, Zhou, X, Johnson, LA, Do, A, Pachman, DR, et al. Acupuncture for palliative cancer pain management: systematic review. BMJ Support Palliat Care. (2021) 11:264–70. doi: 10.1136/bmjspcare-2020-002638
44. Chen, S . The combination of Chinese and Western medical research pioneered in China and its inspiration (II) - The famous physiologist Han Jisheng and the study of the principles of acupuncture analgesia and anesthesia. Chinese J Integrated Trad Western Med. (2016) 36:1157–61. doi: CNKI:SUN:ZZXJ.0.2016-10-001
45. Taguchi, R, Taguchi, T, and Kitakoji, H. Involvement of peripheral opioid receptors in electroacupuncture analgesia for carrageenan-induced hyperalgesia. Brain Res. (2010) 1355:97–103. doi: 10.1016/j.brainres.2010.08.014
46. Fang, J, and Shao, X. New trains of thoughts about acupuncture analgesia—acupuncture analgesia may involve multi-dimensional regulation of pain. Acupuncture Res. (2017) 42:85–9. doi: 10.13702/j.1000-0607.2017.01.016
47. Zhang, Q, Yuan, Y, Zhang, M, Qiao, B, Cui, Y, Wang, Y, et al. Efficacy and safety of acupuncture-point stimulation combined with opioids for the treatment of moderate to severe cancer pain: a network meta-analysis of randomized controlled trials. Front Oncol. (2023) 13:1166580. doi: 10.3389/fonc.2023.1166580
48. Zhang, Z, and Ni, Y. Effect of oxycontin combined with fire needling in treating cancer pain. World J Integrated Trad Western Med. (2020) 15:753–6. doi: 10.13935/j.cnki.sjzx.200442
49. Bai, W, Liu, E, Fang, C, Luo, Z, Zhang, Z, Xu, M, et al. Clinical study on the treatment of cancer pain based on the theory of “fire can be unblocked, and if it is unblocked, there will be no pain” by quenching with milli-fire needles. Chinese Manipulation and Rehab Med. (2019) 10:14–7.
50. Liu, X . The effect of fire acupuncture on the quality of life of patients with breast cancer. World Latest Med Inform. (2018) 18:136–70. Available at: https://kns.cnki.net/kcms2/article/abstract?v=nouGVBS_tgeJyoa-IHg-0RNqUMxqBRKknvHFQJ7bxAe7UBR2V-N-uJJX3BWlVVrHXOkU5OxSxSjMYJ7BsqAx8cKg76MBvR1cw4KS8K7cu3eIki7IIOXdiOO2guK9fxwrT8a494aynvpd4bAIP6-jMg==&uniplatform=NZKPT
51. Mi, J, Deng, T, and Zhou, D. Clinical efficacy of fire-acupuncture-based combined with three-step pain relief method in the treatment of gastric cancer pain. Liaoning J Trad Chinese Med. (2010) 37:2018–9. doi: 10.13192/j.ljtcm.2010.10.166.mijp.061
52. Liu, L, Sun, X, Lu, Y, Kun, SJ, Xing, M, Chen, X, et al. Fire needle therapy for the treatment of psoriasis: a quantitative evidence synthesis. J Altern Complement Med. (2021) 27:24–37. doi: 10.1089/acm.2019.0409
53. Zhang, J, Lin, P, Guo, C, Ma, C, Liu, Y, Wang, Y, et al. Effects and safety of fire needle adjuvant chemical peels therapy in acne vulgaris: a systematic review and meta-analysis. J Dermatol Treat. (2023) 34:2240455. doi: 10.1080/09546634.2023.2240455
Keywords: fire needle therapy, cancer pain, protocol, systematic review, complementary and alternative medicine, efficacy, safety
Citation: Zhang J, Ren Y, Wu W, Yuan Y, Wang J, Tang Y, Zhou Y, Qiao Y and Liu B (2024) Fire needle therapy for the treatment of cancer pain: a protocol for the systematic review and meta-analysis. Front. Neurol. 15:1358859. doi: 10.3389/fneur.2024.1358859
Received: 20 December 2023; Accepted: 08 April 2024;
Published: 15 September 2024.
Edited by:
Michael Furian, Swiss TCM University, SwitzerlandReviewed by:
Giacomo Rossettini, University of Verona, ItalyCopyright © 2024 Zhang, Ren, Wu, Yuan, Wang, Tang, Zhou, Qiao and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Junning Zhang, anVubmluZ3poYW5nQGZveG1haWwuY29t; Baoqin Liu, YmFvcWlubGl1NTI5QDEyNi5jb20=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.