
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol. , 04 April 2024
Sec. Neuroepidemiology
Volume 15 - 2024 | https://doi.org/10.3389/fneur.2024.1348011
Introduction: The relationship between oxidative balance score (OBS), an emerging integrative metric for assessing individual redox homeostasis, and the prevalence of stroke in the general population remains unknown. We aimed to explore these relationships in the National Health and Nutrition Examination Survey (NHANES). We investigated the relationship between the oxidative balance score (OBS) and stroke prevalence using NHANES data from 1999–2018.
Methods: We included eligible individuals from NHANES 1999–2018. OBS calculations were based on previously validated methods, and stroke diagnoses were based on self-reports in questionnaires. Multivariable logistic regression analyses were used to examine the independent associations of overall, dietary, and lifestyle OBS with stroke prevalence. In addition, restricted cubic spline (RCS), stratified analysis, and sensitivity analysis were used.
Results: We included 25,258 participants aged 20–85 years, in which the prevalence of stroke was 2.66%. After adjusting for all confounders, overall and dietary OBS, but not lifestyle OBS, were inversely associated with the prevalence of stroke [odds ratios and 95% confidence intervals of 0.97 (0.96, 0.99) and 0.98 (0.96, 0.99) for overall and dietary OBS, respectively, both p < 0.05]. In addition, there was a dose-response relationship between overall and dietary OBS and stroke prevalence. The RCS showed that these relationships were linear. Stratified analyses indicated that socioeconomic status (SES) significantly influenced the relationship between all OBS and stroke prevalence.
Conclusion: Dietary OBS, but not lifestyle OBS, had an inverse relationship with the prevalence of stroke in the general population. SES significantly influenced the protective effect of OBS against stroke. These findings emphasize the importance of integrated antioxidant properties from diet for stroke prevention.
Stroke, including ischemic and hemorrhagic stroke, is the leading cause of disability and death worldwide (1). Global stroke statistics reveal that stroke is the second most common cause of disability and mortality, and its disease burden is substantial in both low- and high-income countries (2). Stroke is the disease leading to the highest disability-adjusted life-years lost in China, with approximately 2 million new cases each year (3). The incidence of stroke is highest in the elderly population; however, recent epidemiologic studies have shown that the incidence of stroke in young adults (<50 years of age) is increasing dramatically (4). Evidence-based findings suggest that up to 85% of strokes are preventable; therefore, identifying modifiable risk factors for stroke is a major instrument for stroke prevention and management of stroke populations (5).
Oxidative stress is an important component of the pathogenesis of stroke, which is inextricably associated with neuroinflammation and ischemia-reperfusion injury (6, 7). Dietary and other lifestyle modifications, which are recognized as central in stroke prevention, are closely linked to homeostasis of the individual’s redox state. There is a large body of evidence linking nutritional deficiencies and poor lifestyles such as obesity status and harmful alcohol consumption to stroke risk and prognosis (8–10). However, whether there are independent and/or combined effects of oxidative stress-related dietary components and lifestyle on the prevalence of stroke in the general population remains unstudied.
The oxidative balance score (OBS) is an emerging indicator in recent years for assessing the homeostasis of an individual’s redox balance, which consists of a dietary OBS, and a lifestyle OBS (11). OBS has demonstrated its clinical relevance in extensive epidemiologic studies and is associated with a variety of diseases such as cancer (12), chronic kidney disease (13), and depression (14). Exploring whether OBS is associated with the prevalence of stroke in the general population could help potential stroke prevention strategies based on OBS. We here explore these relationships using a nationwide population-based survey, the National Health and Nutrition Examination Surveys (NHANES).
NHANES was originally designed and conducted to collect information about the health and nutrition of the US household population, which is a major program of the National Center for Health Statistics (NCHS). NHANES is designed as a serial (2 years cycle from 1999 onwards), multistage, complex, probability-sampling cross-sectional study. The NHANES was reviewed and approved by the NCHS Ethics Review Board (ERB) (The ERB approval protocol numbers for each cycle can be found here: https://www.cdc.gov/nchs/nhanes/irba98.htm) and therefore do not require additional ethical review consent. In addition, written consent was obtained from all participants for this survey. More information is available on the official NHANES website.
We first excluded pregnant participants (n = 1,547) among those aged 20–85 years (n = 55,081) in NHANES 1999–2018 (including 10 consecutive cycles). Next, we excluded participants with missing information on OBS (n = 25,940) and stroke (n = 77). We also ruled out those with missing covariates (n = 1,547). Finally, we included 25,258 participants for further analysis (Figure 1).
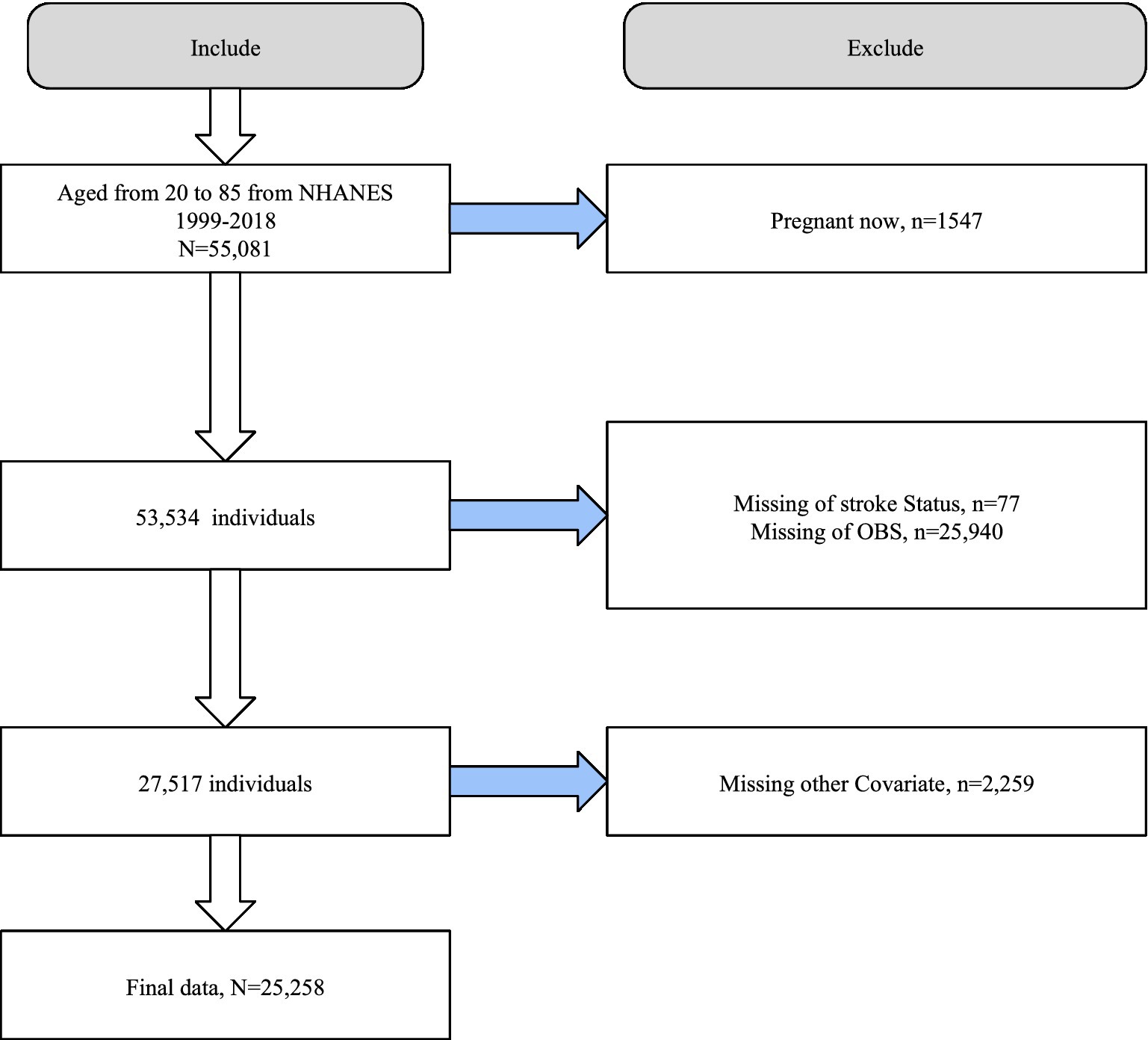
Figure 1. Flowchart of the study population selection process. OBS, oxidation balance score; NHANES, the National Health and Nutrition Examination Survey.
Numerous studies have explored the potential value of OBS using NHANES, and we used previously well-validated OBS components and calculations to define our OBS (15). The OBS consists of a dietary OBS composed of 16 dietary components and a lifestyle OBS composed of 4 lifestyle components. Of the 20 components, 5 of them were pro-oxidants (dietary iron and total fat intake, serum nicotine, BMI, alcohol consumption) and the others were antioxidants. In NHANES, two 24 h dietary review interviews were included (the first dietary recall interview was conducted in person and the second interview was conducted by telephone 3–10 days later), and we used the average intake from the two interviews. We did not include intake of nutrients from dietary supplements and medications based on the previous study. Physical activity was measured in metabolic equivalents [MET] based on the information in the questionnaire. We used serum nicotine as a measure of active and passive smoking to accurately reflect individual smoking levels.
We assigned scores to all OBS components based on a gender-specific approach. Antioxidant fractions were assigned scores of 0, 1, and 2 based on a lowest-to-highest distribution in tertiles, as opposed to pro-oxidants. We manually calculated the range of values corresponding to the tertiles of each component in the final included population. We assigned scores of 0, 1, and 2 to the >3, 2–3, and ≤2 drinks/day distributions of alcohol consumption in the past year for men, and scores of 0, 1, and 2 to the >2, 1–2, and ≤1 drinks/day for women. The component and score assignments of OBS are summarized in Table 1.
We defined an individual’s stroke status based on the question in the NHANES questionnaire: “Has a doctor or other health professional ever told you that you had a stroke?” (16). The diagnosis of such questionnaire-based self-reported illnesses has been shown to have good agreement and has been widely used in NHANES-related epidemiologic studies (17).
We selected several important potential covariates based on previous studies, including age, gender (male or female), ethnicity, education level, marital status (single or non-single), family income to poverty (PIR), total daily energy intake (kcal/day), diabetes, and hypertension. The ethnicity consists of Mexican American, non-Hispanic black, non-Hispanic white, other Hispanic, or other races. The educational level of an individual was categorized as <high school, high school, and >high school. A diagnosis of diabetes was based on one of a doctor saying someone has diabetes, a blood glucose/glucose tolerance test that meets the American Diabetes Association’s criteria (18), or being on anti-diabetic medication. Hypertension was diagnosed by self-reported hypertension, a blood pressure ≥130/85 mmHg, or taking antihypertensive medication.
All analyses were performed using EmpowerStats (X&Y Solutions, Inc., Boston, MA) and R software 4.2.3. Given the complex design of the NHANES and in an effort to make our sample representative of the entire US population, we weighted our analyses accordingly to the NHANES analysis guidelines (19). In the baseline analysis, the continuous variables (mean ± standard error) and categorical variables (percentage) were used to characterize the study population. The student’s t-test for continuous variables or chi-square test for categorical variables was applied.
In the multivariable adjusted logistic regression analysis, we constructed three models. The crude model was not adjusted for any covariates. Adjusted model 1 was a partially adjusted model that adjusted for age, gender, race, marital status, PIR, education level, and total energy intake. Adjusted model 2 was further adjusted for diabetes and hypertension based on adjusted model 1.
To explore the potential nonlinear relationship between OBS and stroke, we performed smooth curve fitting using restricted cubic spline (RCS). Finally, we used stratified analyses to explore the consistency of the results within subgroups for each variable and performed sensitivity analyses using tertiles and quintiles of OBS to indicate whether the results were stable. In all analyses, p < 0.05 was considered statistically significant.
Of the 25,258 participants included (mean age 46.04 years, 51.29% male), stroke was diagnosed in 673 subjects, corresponding to a prevalence of 2.66%. We first performed a baseline analysis of the included population according to the quartiles of the OBS. We found that as quartiles of OBS rose, participants had significantly higher PIR, energy intake, proportion of non-Hispanic white population, proportion of non-singles, and education levels, while diabetes, hypertension, and stroke populations were significantly lower. However, participants’ age and sex proportions did not change significantly with OBS. In addition, dietary and lifestyle OBS increased significantly with increasing quartiles of OBS (Table 2).
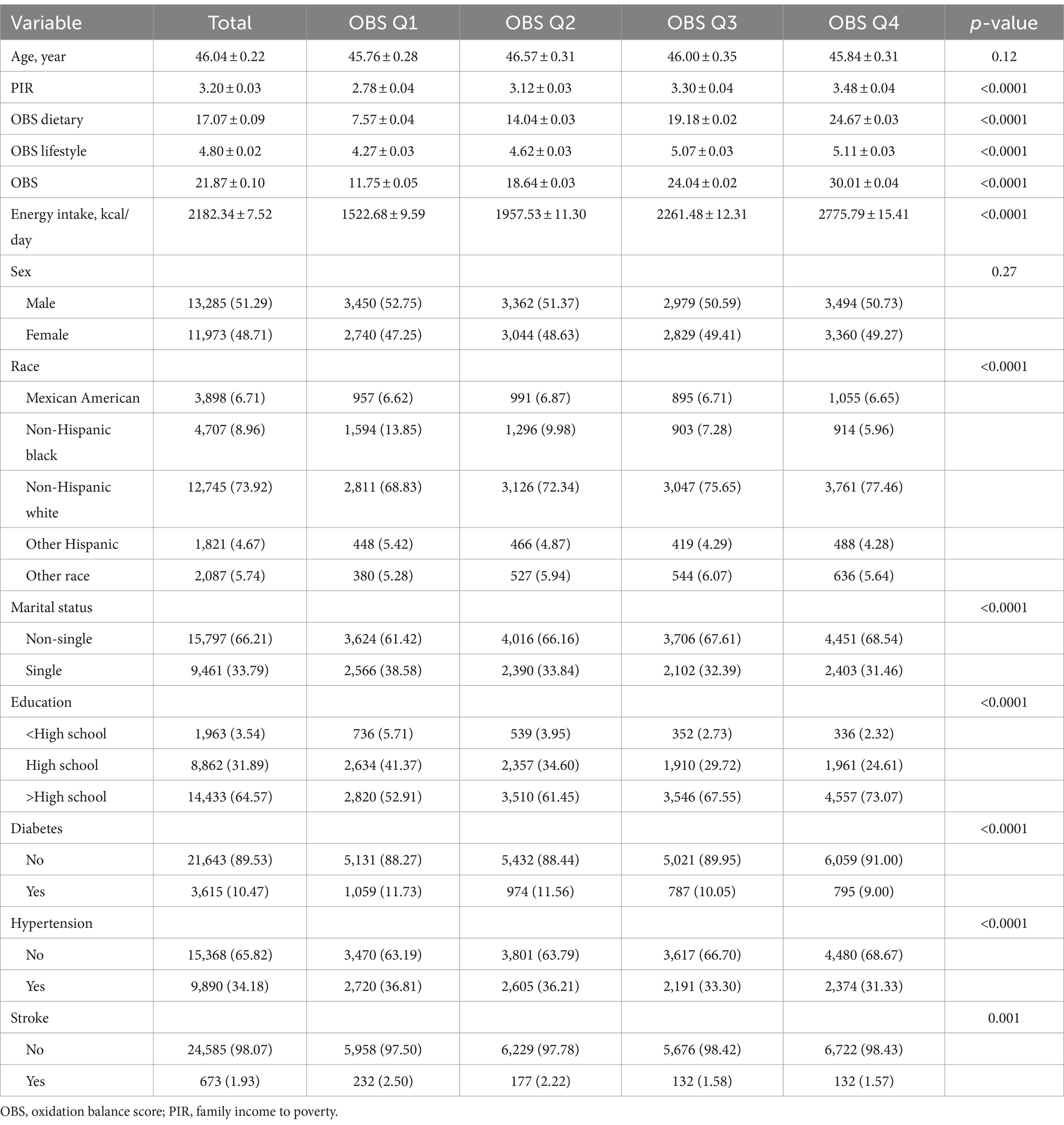
Table 2. Baseline characteristics of the included population, grouped according to quartiles of the OBS.
We summarized the baseline characteristics of the population grouped according to stroke status in Supplementary Table S1. There were significant differences in age, PIR, total energy intake, sex, race, education, diabetes, and hypertension status in individuals with stroke compared to the stroke-free population, while there were no differences in marital status. Of note, OBS, dietary OBS, and lifestyle OBS were all lower in people with stroke (p < 0.0001, < 0.0001, and = 0.005, respectively).
To explore whether OBS (including dietary and lifestyle OBS) is independently associated with the odds of stroke in the general population, we developed three multivariable models with stepwise adjustment. We treated OBS as continuous and categorical variables in quartiles, respectively, where the number of participants and the range of values for all quartiles of OBS were listed in Supplementary Table S2. First, when not adjusting for any confounders, we found that dietary OBS but not lifestyle OBS was inversely associated with stroke. When used as a continuous variable, each unit increase in dietary OBS was associated with 3% lower odds of stroke [odds ratio (OR) and 95% confidence interval (CI) = 0.97 (0.96, 0.98), p < 0.0001]. Similarly, overall OBS showed a similar trend [OR and 95% CI = 0.97 (0.96, 0.98), p < 0.0001]. However, there was no significant association for lifestyle OBS [OR and 95% CI = 1.01 (0.95, 1.07) p = 0.7358]. When treated as categorical variables, both dietary and overall OBS showed a significant dose-response relationship with stroke risk (both p for trend <0.05). Compared to Q1, dietary OBS was associated with a 40% reduction in the prevalence of stroke in both Q3 and Q4, while similarly, overall OBS was associated with a 32 and 37% reduction in risk in Q3 and Q4, respectively. However, we did not observe similar changes in lifestyle OBS.
We then adjusted for age, sex, race, education level, marital status, PIR, and total daily energy intake in adjusted model 1. Similar associations with stroke prevalence were still observed in diet and overall OBS. Notably, we found that lifestyle OBS was also negatively associated with stroke prevalence [OR and 95% CI = 0.92 (0.86, 0.98), p = 0.0119] and exhibited a dose-response relationship (p for trend = 0.0063).
Finally, we additionally adjusted for diabetes and hypertension status based on model 1. In the fully adjusted model, dietary OBS remained independently and inversely associated with stroke prevalence, with each unit increase in OBS associated with a 2% reduction in stroke risk. Similarly, we observed a dose-response relationship between dietary OBS and stroke risk (p for trend = 0.0271), with dietary OBS at Q3 associated with a 31% reduction in stroke prevalence, and Q4 also marginally associated with a reduced risk of stroke compared to Q1 (OR = 0.73, p = 0.0677). A similar trend was observed for overall OBS. A 1-unit increase in an individual’s overall OBS was associated with a 3% reduction in stroke risk, and Q3 and Q4 OBS were associated with 28 and 32% reductions in stroke prevalence. However, we found that the association between lifestyle OBS and stroke risk disappeared after adjusting for all confounders (all p > 0.05) (Table 3).
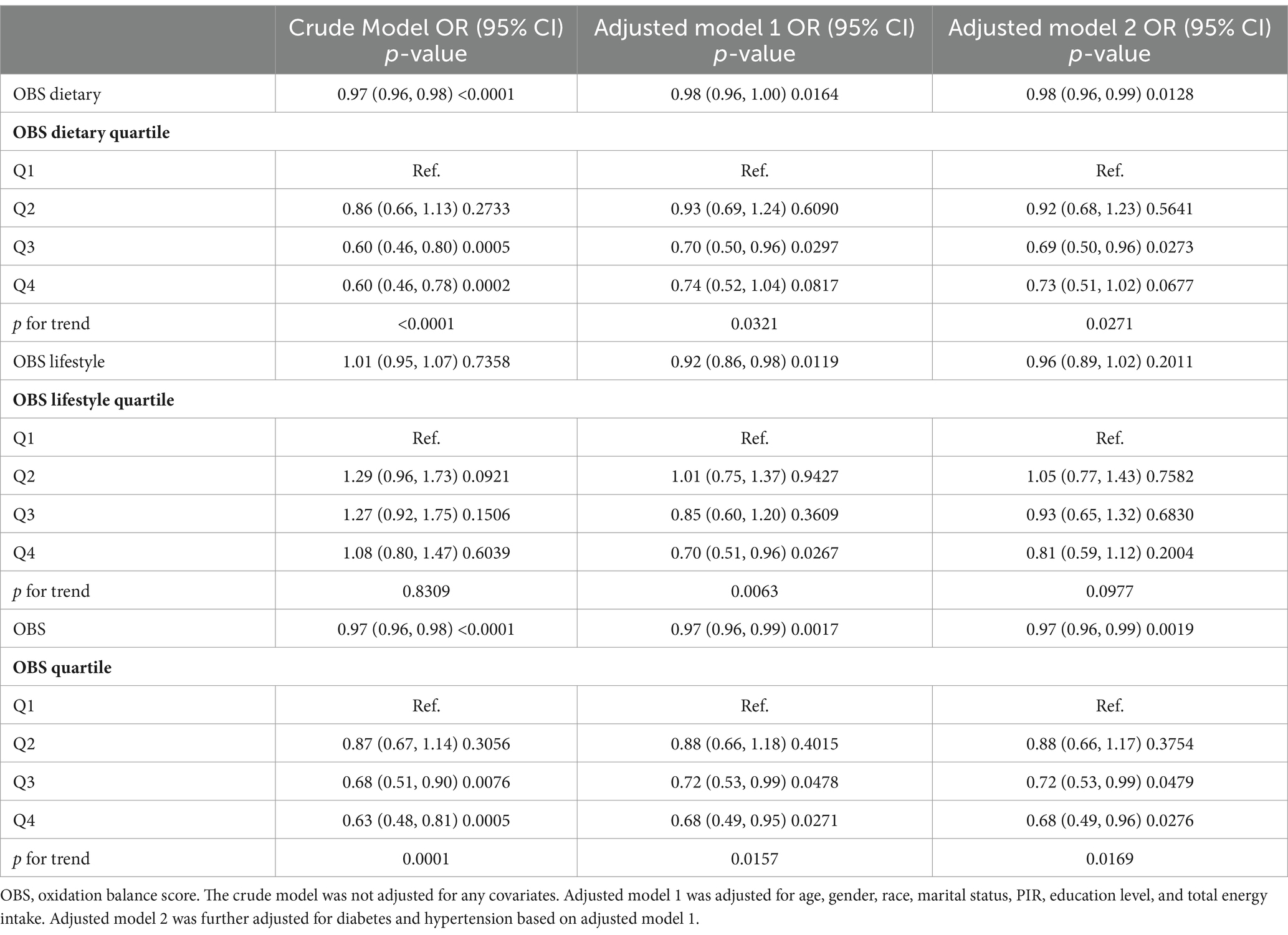
Table 3. Multivariable-adjusted logistic regression models examining the relationship between OBS and stroke prevalence.
To explore whether there was a nonlinear relationship between all OBS and stroke risk, we performed an exploration using the RCS model. We found that both dietary and overall OBS were linearly associated with stroke risk in the general population (p nonlinear = 0.6555 and 0.5987, respectively). Furthermore, the development of stroke would likely be at a relatively low risk after dietary and overall OBS exceeded 17 and 22 points, respectively. Consistently, we found no significant association between lifestyle OBS and the prevalence of stroke (Figure 2).
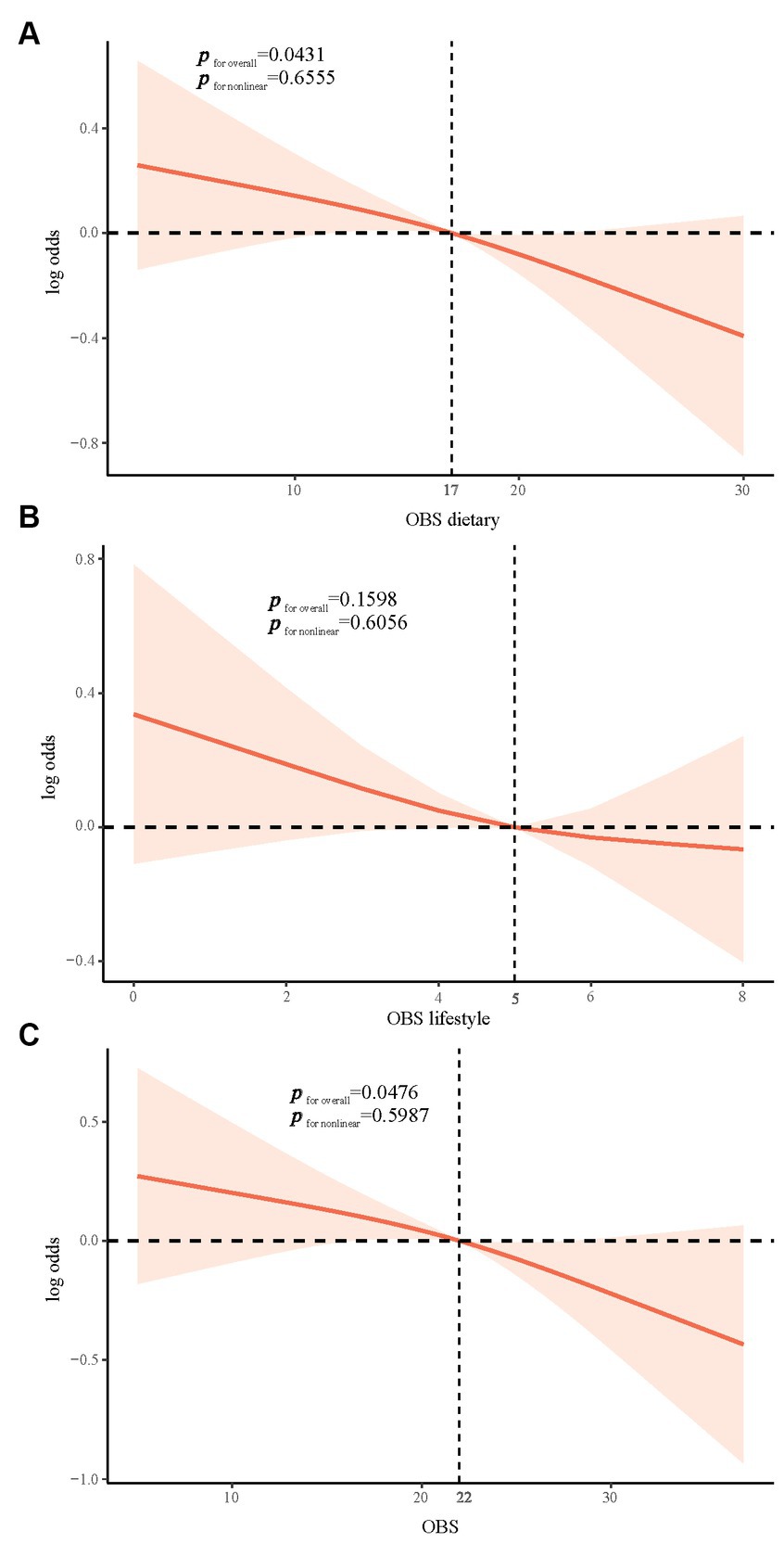
Figure 2. RCS model exploring nonlinear relationships. Linear associations in dietary and overall OBS are shown in (A and C), No significant association in lifestyle OBS is shown in (B). OBS, oxidation balance score; RCS, restricted cubic spline.
In stratified analyses, we found no multiplicative interaction between most of the variables and OBS (p for interaction >0.05). However, we nonetheless found several factors that may influence the relationship between OBS and stroke. In the association between dietary OBS and the prevalence of stroke, we found a significant interaction between PIR and this relationship (p for interaction = 0.002), and a marginal effect of education level (p for interaction = 0.054) (Figure 3A). Similarly, we observed the effect of PIR and education level on the relationship in stratified analyses for lifestyle OBS (p for interaction = 0.058 and 0.009 for PIR and education level, respectively) and overall OBS (p for interaction = 0.002 and 0.042 for PIR and education level, respectively) (Figures 3B,C). The associations of OBS, dietary OBS, and lifestyle OBS with the prevalence of stroke were only present in participants with a PIR >3 and an education level above high school.
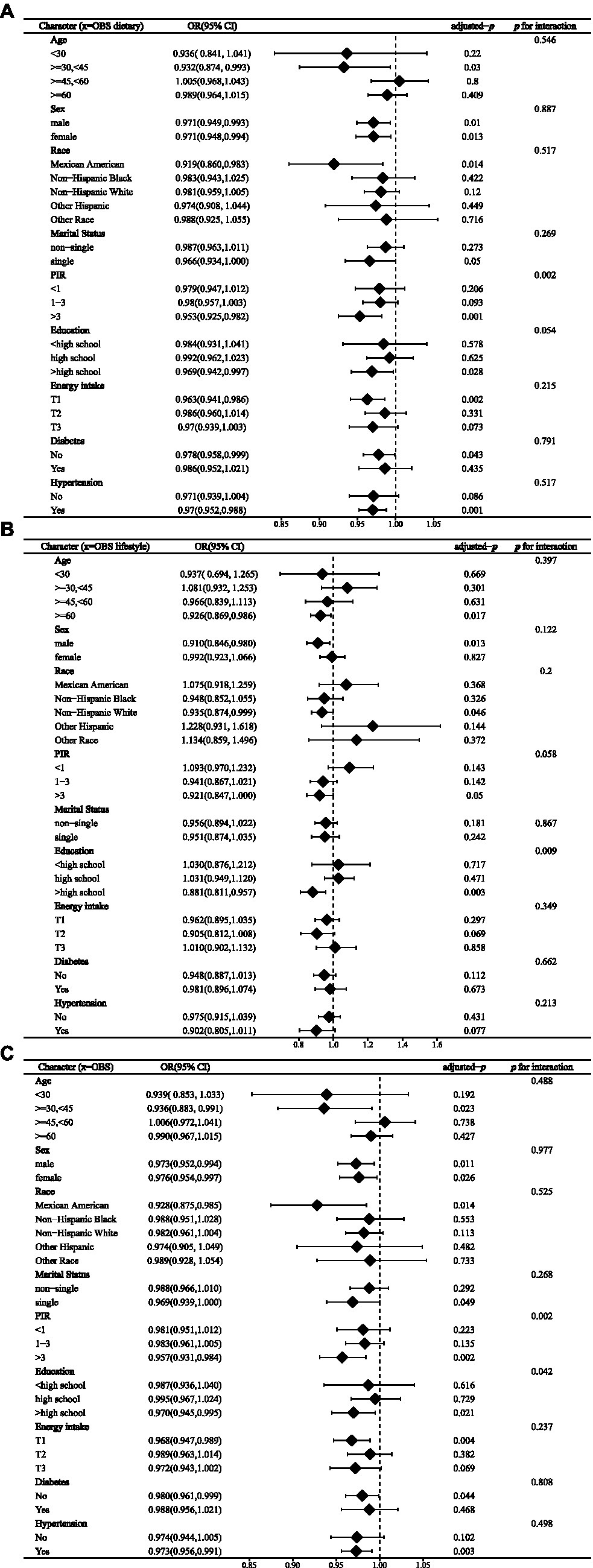
Figure 3. Stratified analysis of OBS components and stroke prevalence: interaction with PIR and education level in dietary OBS (A), lifestyle OBS (B), and overall OBS (C). PIR, family income to poverty; OR, odds ratio.
We conducted sensitivity analyses by treating all OBS as categorical variables in tertiles or quintiles to verify the stability of the findings. We obtained similar results, although the dose-response relationship was lost for dietary OBS under tertiles (p for trend = 0.1707). This may indicate that the association of dietary OBS on stroke was significant but relatively flat and that more significant changes are needed to be associated with a reduction in stroke prevalence. Similarly, lifestyle OBS remained unassociated with stroke prevalence (all p > 0.05) (Supplementary Tables S3, S4).
In this nationally representative population-based study, we found that an emerging measure of individual redox homeostasis, OBS, was inversely associated with the prevalence of self-reported stroke. Specifically, dietary OBS was significantly associated with stroke, but not lifestyle OBS. The RCS model revealed that OBS and dietary OBS were linearly associated with stroke prevalence in the general population. Another important finding was that participants’ socioeconomic status (SES) was a key factor influencing these relationships, including lifestyle OBS with stroke prevalence. Our study suggests that higher diet-based antioxidant profiles in the general population are associated with a reduction in the development of stroke, and these findings emphasize the plausibility of stroke prevention by adjusting daily dietary antioxidant levels.
Diet/nutrition-related strategies have been shown to have a significant impact on stroke prevention in the general population. Of these, the Mediterranean diet has been the most extensively studied for stroke prevention. The Mediterranean diet is a healthy, light, yet nutritionally complete diet. It is characterized by an adequate intake of fruits, vegetables, and whole grains, and also include legumes/nuts, skim milk, olive oil and some fish, as well as small amounts of red meat, salt, and carbohydrates (20). The Mediterranean diet has proven benefits for cardiovascular health as well as disease prevention (21). Adherence to the Mediterranean diet has been reported to reduce the risk of first stroke (22) and post-stroke cardiometabolic health (23). In addition, extensive body of research suggests that a variety of indicators reflecting dietary habits or quality are also associated with the risk of developing stroke. A recent epidemiologic study using NHANES indicated that stroke survivors had lower levels of nutrient intake and overall diet quality (as indicated by the Healthy Eating Index-2015) than a matched control population (24). Another indicator of diet quality, the Dietary Inflammation Index, has also been shown to be associated with risk of stroke (25), post-stroke depression (26), and increased carotid plaque vulnerability (27). Similarly, a meta-analysis incorporating 12 prospective cohort studies demonstrated that Dietary Approaches to Stop Hypertension dietary patterns were inversely associated with the risk of stroke development (relative risk 0.88, 95% CI 0.83–0.93) (28). These studies underscore the importance of dietary/nutritional factors in stroke prevention.
We showed for the first time that OBS was independently associated with the prevalence of stroke in the general population in a large, real-world epidemiologic study. The OBS is an emerging scoring system composed of multiple dietary and lifestyle sources of antioxidants and pro-oxidants that reflect an individual’s exogenous redox homeostasis, with a higher level representing an individual’s overall antioxidant profile at a higher level (11). Although the composition of OBS components in the current literature is diverse, OBS has been shown in numerous observational studies to be associated with cardiovascular risk factors (29), multiple cancers (12, 30), and all-cause/factor-specific mortality (31). In our study, the components of OBS were determined based on previous studies using NHANES (15, 32), thus ensuring reliability and applicability. Our OBS consists of 16 dietary (including macro- and micronutrients) and 4 lifestyle antioxidants and pro-oxidants, all of which have been shown in the literature to have potential antioxidant/pro-oxidant properties (11, 32). The comprehensive inclusion of dietary and lifestyle sources of antioxidants and pro-oxidants allowed for a more adequate assessment of exogenous redox homeostasis in individuals by the OBS in our study.
While no studies have explored the relationship between OBS and stroke risk, numerous clinical studies have shown that dietary antioxidants are strongly associated with the development of stroke, albeit with controversy. Earlier studies have shown that the intake of certain dietary antioxidants is associated with a reduced risk of stroke (33, 34). However, recent evidence suggests that dietary antioxidants are not associated with stroke risk and even increase the risk of certain stroke types (35, 36). However, these studies only examined the relationship between one or specific dietary antioxidants and the risk of stroke, unlike the integrated assessment of dietary antioxidants and pro-oxidants in our study. Recent studies have similarly used NHANES to show inverse associations of otherwise measured dietary antioxidant properties with risk of stroke (37) and post-stroke depression/all-cause mortality (38), consistent with our study.
Surprisingly, we did not find an association between lifestyle OBS and stroke prevalence. Lifestyle OBS consists of BMI, physical activity, alcohol consumption, and serum nicotine. A large meta-analysis that included 4.43 million people showed a “J” shaped relationship between BMI and the risk of stroke, with BMI >25 kg/m2 being associated with an increased risk of stroke (39). Similarly, heavy alcohol consumption was associated with an increased risk of stroke, whereas light-moderate alcohol intake was associated with a decreased risk of stroke (10). Smoking or electronic nicotine delivery systems use have also been shown to be associated with the risk of stroke (40, 41), although the association between serum nicotine levels and the risk of stroke remains unclear. Physical activity, on the other hand, is recognized as an effective means in stroke prevention (42). We were unable to provide a specific explanation at this time, but this may be due to the heterogeneity of our inclusion population compared to previous studies, as well as the differences in lifestyle OBS as a composite measure compared to individual lifestyles. In addition, we can draw insights from the stratified analysis. Although lifestyle OBS was not associated with stroke prevalence in the overall population, we observed significant associations in specific subgroups such as those ≥60 years of age, men, non-Hispanic white population, and those with >high school education. This suggests that the impact of an individual’s lifestyle OBS on the prevalence of stroke in the general population is age-, sex-, race-, and education-specific. It also highlights the need for lifestyle-based stroke prevention strategies to take these demographic and SES factors into account.
Another important finding of our study was that SES significantly influenced the relationship between OBS (including dietary and lifestyle OBS) and stroke development. A recent study using NHANES showed a significantly inverse association of PIR with stroke risk (43). Our study showed that PIR significantly/marginally influenced the relationship between OBS and stroke risk, and that a protective effect of OBS was present only in participants with a PIR >3. Another study using NHANES showed that poverty was more common among stroke survivors and was associated with lower dietary quality, which may also partly explain the protective effect of OBS only among those with higher incomes (24). In addition, educational attainment has also been shown to be significantly associated with stroke risk in previous studies (44, 45). These findings were consistent with previous studies indicating a significant effect of SES on individuals with stroke, either alone or by influencing the relationship.
OBS was revealed in previous studies to be associated with oxidative stress and inflammatory biomarkers in the blood. Multiple previous studies have shown that OBS was correlated with levels of biomarkers reflecting systemic oxidative stress levels such as F2-isoprostanes, fluorescent oxidative products, and γ-glutamyltransferase (46–49). OBS has also been revealed to have a possible negative correlation with several biomarkers of systemic inflammation such as C-reactive protein, and interleukin-6 levels (47, 50). Thus, OBS may serve as a validated measure of the redox status of an individual’s diet and lifestyle, which then indirectly reflects the level of systemic oxidative stress and chronic inflammation, which are critical in the pathogenesis of stroke (6, 51).
Our study has several strengths. Firstly, this represents a pioneering real-world exploration of the relationship between an emerging composite of antioxidant and pro-oxidant metrics reflecting diet and lifestyle and the prevalence of stroke in the general population. These findings may illuminate potential pathways for the implementation of future OBS-based stroke prevention strategies, contributing to the primordial prevention of stroke. This has important public health implications for reducing the disease burden of stroke. Secondly, our study made extensive adjustments for numerous potential confounders, thereby minimizing the impact of confounding. Our study was based on a nationwide epidemiological survey, and the use of appropriate weighting methods allowed our sample to be representative of the overall population. This ensures the representativeness and generalizability of our findings.
However, there are weaknesses to be acknowledged. Firstly, due to the cross-sectional nature of the study, we were unable to establish causality and may still be subject to unadjusted residual confounders. Secondly, the diagnosis of stroke in our study was reliant on self-reporting via questionnaires, which could introduce information bias. Nonetheless, a large body of previous NHANES studies that have utilized questionnaires for diagnosis have reported convincing agreement. Additionally, our analysis did not include the intake of nutrients from dietary supplements and medications, consistent with previous research approaches. This decision was based on prior studies suggesting that the inclusion of such data does not significantly alter the associations under investigation. However, it is important to recognize that this could affect the estimation of total nutrient intake and potentially influence the observed associations. Future research could benefit from incorporating these factors to provide a more comprehensive assessment.
In conclusion, while our findings provide valuable insights, they should be interpreted with caution. Further research, especially large prospective cohort studies, is needed to substantiate and expand upon our conclusions.
In a nationally representative population-based study, we found that overall OBS and dietary OBS, but not lifestyle OBS, were inversely associated with the prevalence of stroke in the general population. SES, including PIR and educational attainment, significantly influenced these associations. These findings may contribute to further exploration of stroke prevention strategies targeting OBS.
Publicly available datasets were analyzed in this study. This data can be found here: Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS), National Health and Nutrition Examination Survey (NHANES), https://wwwn.cdc.gov/nchs/nhanes/Default.aspx, NHANES 1999–2018.
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the patients/participants or patients/participants’ legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
JC: Writing – original draft, Conceptualization, Methodology, Formal analysis, Software. JL: Methodology, Formal analysis, Writing – review & editing. ZG: Writing – original draft, Conceptualization, Methodology. JF: Methodology, Formal analysis, Writing – review & editing. SL: Writing – review & editing, Formal analysis. QZ: Writing – review & editing. KP: Writing – review & editing. YW: Writing – review & editing, Conceptualization, Methodology, Project administration, Funding acquisition.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research was funded by National Natural Science Foundation of China (81502139) and Medical Health Science and Technology Project of Zhejiang Province (2023RC174).
The authors thank all the participants in the NHANES for providing data for this study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2024.1348011/full#supplementary-material
1. Campbell, BCV, and Khatri, P. Stroke. Lancet. (2020) 396:129–42. doi: 10.1016/s0140-6736(20)31179-x
2. Saini, V, Guada, L, and Yavagal, DR. Global epidemiology of stroke and access to acute ischemic stroke interventions. Neurology. (2021) 97:S6–S16. doi: 10.1212/wnl.0000000000012781
3. Wu, S, Wu, B, Liu, M, Chen, Z, Wang, W, Anderson, CS, et al. Stroke in China: advances and challenges in epidemiology, prevention, and management. Lancet Neurol. (2019) 18:394–405. doi: 10.1016/s1474-4422(18)30500-3
4. Ekker, MS, Boot, EM, Singhal, AB, Tan, KS, Debette, S, Tuladhar, AM, et al. Epidemiology, aetiology, and management of ischaemic stroke in young adults. Lancet Neurol. (2018) 17:790–801. doi: 10.1016/s1474-4422(18)30233-3
5. Sarikaya, H, Ferro, J, and Arnold, M. Stroke prevention—medical and lifestyle measures. Eur Neurol. (2015) 73:150–7. doi: 10.1159/000367652
6. Orellana-Urzúa, S, Rojas, I, Líbano, L, and Rodrigo, R. Pathophysiology of ischemic stroke: role of oxidative stress. Curr Pharm Des. (2020) 26:4246–60. doi: 10.2174/1381612826666200708133912
7. Candelario-Jalil, E, Dijkhuizen, RM, and Magnus, T. Neuroinflammation, stroke, blood-brain barrier dysfunction, and imaging modalities. Stroke. (2022) 53:1473–86. doi: 10.1161/strokeaha.122.036946
9. Wang, X, Huang, Y, Chen, Y, Yang, T, Su, W, Chen, X, et al. The relationship between body mass index and stroke: a systemic review and meta-analysis. J Neurol. (2022) 269:6279–89. doi: 10.1007/s00415-022-11318-1
10. Larsson, SC, Wallin, A, Wolk, A, and Markus, HS. Differing association of alcohol consumption with different stroke types: a systematic review and meta-analysis. BMC Med. (2016) 14:178. doi: 10.1186/s12916-016-0721-4
11. Hernández-Ruiz, Á, García-Villanova, B, Guerra-Hernández, E, Amiano, P, Ruiz-Canela, M, and Molina-Montes, E. A review of a priori defined oxidative balance scores relative to their components and impact on health outcomes. Nutrients. (2019) 11:774. doi: 10.3390/nu11040774
12. Park, YM, Shivappa, N, Petimar, J, Hodgson, ME, Nichols, HB, Steck, SE, et al. Dietary inflammatory potential, oxidative balance score, and risk of breast cancer: findings from the sister study. Int J Cancer. (2021) 149:615–26. doi: 10.1002/ijc.33581
13. Ilori, TO, Wang, X, Huang, M, Gutierrez, OM, Narayan, KM, Goodman, M, et al. Oxidative balance score and the risk of end-stage renal disease and cardiovascular disease. Am J Nephrol. (2017) 45:338–45. doi: 10.1159/000464257
14. Liu, X, Liu, X, Wang, Y, Zeng, B, Zhu, B, and Dai, F. Association between depression and oxidative balance score: National Health and Nutrition Examination Survey (NHANES) 2005–2018. J Affect Disord. (2023) 337:57–65. doi: 10.1016/j.jad.2023.05.071
15. Xu, Z, Xue, Y, Wen, H, and Chen, C. Association of oxidative balance score and lung health from the National Health and Nutrition Examination Survey 2007–2012. Front Nutr. (2022) 9:961950. doi: 10.3389/fnut.2022.961950
16. Andres, W, Rothstein, A, Elser, H, Sloane, KL, Gottesman, RF, Kasner, SE, et al. Trends in the prevalence of stroke among community-dwelling individuals in the US, 1999–2018. JAMA Neurol. (2023) 80:646–8. doi: 10.1001/jamaneurol.2023.0742
17. Shi, Y, Zhang, J, and Huang, Y. Prediction of cardiovascular risk in patients with chronic obstructive pulmonary disease: a study of the National Health and Nutrition Examination Survey database. BMC Cardiovasc Disord. (2021) 21:417. doi: 10.1186/s12872-021-02225-w
18. ElSayed, NA, Aleppo, G, Aroda, VR, Bannuru, RR, Brown, FM, Bruemmer, D, et al. 2. Classification and diagnosis of diabetes: standards of care in diabetes-2023. Diabetes Care. (2023) 46:S19–s40. doi: 10.2337/dc23-S002
19. Johnson, CL, Paulose-Ram, R, Ogden, CL, Carroll, MD, Kruszon-Moran, D, Dohrmann, SM, et al. National Health and Nutrition Examination Survey: analytic guidelines, 1999–2010. Vital and Health Statistics. Series 2. Hyattsville, MD U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics (2013). 1–24.
20. Widmer, RJ, Flammer, AJ, Lerman, LO, and Lerman, A. The Mediterranean diet, its components, and cardiovascular disease. Am J Med. (2015) 128:229–38. doi: 10.1016/j.amjmed.2014.10.014
21. Martínez-González, MA, Gea, A, and Ruiz-Canela, M. The Mediterranean diet and cardiovascular health. Circ Res. (2019) 124:779–98. doi: 10.1161/circresaha.118.313348
22. English, C, MacDonald-Wicks, L, Patterson, A, Attia, J, and Hankey, GJ. The role of diet in secondary stroke prevention. Lancet Neurol. (2021) 20:150–60. doi: 10.1016/s1474-4422(20)30433-6
23. Bayes, J, Peng, W, Adams, J, and Sibbritt, D. The effect of the Mediterranean diet on health outcomes in post-stroke adults: a systematic literature review of intervention trials. Eur J Clin Nutr. (2023) 77:551–60. doi: 10.1038/s41430-022-01212-4
24. Zoellner, ER, Patterson, MA, Sharrief, AZ, Savitz, SI, Tucker, WJ, and Miketinas, DC. Dietary intake and quality among stroke survivors: NHANES 1999–2018. J Nutr. (2023) 153:3032–40. doi: 10.1016/j.tjnut.2023.08.015
25. Zhuo, S, Zhang, B, Zhang, J, Yang, M, and Yu, Z. Effects of dietary inflammatory index, blood lead levels, and flavonoid intake on stroke risk in older Americans: a cross-sectional study. J Stroke Cerebrovasc Dis. (2023) 32:107336. doi: 10.1016/j.jstrokecerebrovasdis.2023.107336
26. Ghazizadeh, H, Yaghooti-Khorasani, M, Asadi, Z, Zare-Feyzabadi, R, Saeidi, F, Shabani, N, et al. Association between dietary inflammatory index (DII®) and depression and anxiety in the Mashhad stroke and heart atherosclerotic disorder (MASHAD) study population. BMC Psychiatry. (2020) 20:282. doi: 10.1186/s12888-020-02663-4
27. Peng, M, Wang, L, Xia, Y, Tao, L, Liu, Y, Huang, F, et al. High dietary inflammatory index is associated with increased plaque vulnerability of carotid in patients with ischemic stroke. Stroke. (2020) 51:2983–9. doi: 10.1161/strokeaha.120.029035
28. Feng, Q, Fan, S, Wu, Y, Zhou, D, Zhao, R, Liu, M, et al. Adherence to the dietary approaches to stop hypertension diet and risk of stroke: a meta-analysis of prospective studies. Medicine. (2018) 97:e12450. doi: 10.1097/md.0000000000012450
29. Lakkur, S, Judd, S, Bostick, RM, McClellan, W, Flanders, WD, Stevens, VL, et al. Oxidative stress, inflammation, and markers of cardiovascular health. Atherosclerosis. (2015) 243:38–43. doi: 10.1016/j.atherosclerosis.2015.08.032
30. Dash, C, Bostick, RM, Goodman, M, Flanders, WD, Patel, R, Shah, R, et al. Oxidative balance scores and risk of incident colorectal cancer in a US prospective cohort study. Am J Epidemiol. (2015) 181:584–94. doi: 10.1093/aje/kwu318
31. Kong, SY, Goodman, M, Judd, S, Bostick, RM, Flanders, WD, and McClellan, W. Oxidative balance score as predictor of all-cause, cancer, and noncancer mortality in a biracial US cohort. Ann Epidemiol. (2015) 25:256–262.e1. doi: 10.1016/j.annepidem.2015.01.004
32. Zhang, W, Peng, SF, Chen, L, Chen, HM, Cheng, XE, and Tang, YH. Association between the oxidative balance score and telomere length from the National Health and Nutrition Examination Survey 1999–2002. Oxid Med Cell Longev. (2022) 2022:1345071. doi: 10.1155/2022/1345071
33. Vokó, Z, Hollander, M, Hofman, A, Koudstaal, PJ, and Breteler, MM. Dietary antioxidants and the risk of ischemic stroke: the Rotterdam study. Neurology. (2003) 61:1273–5. doi: 10.1212/01.wnl.0000090458.67821.a3
34. Hariri, M, Maghsoudi, Z, Darvishi, L, Askari, G, Hajishafiee, M, Ghasemi, S, et al. B vitamins and antioxidants intake is negatively correlated with risk of stroke in Iran. Int J Prev Med. (2013) 4:S284–9.
35. Martens, LG, Luo, J, Willems van Dijk, K, Jukema, JW, Noordam, R, and van Heemst, D. Diet-derived antioxidants do not decrease risk of ischemic stroke: a Mendelian randomization study in 1 million people. J Am Heart Assoc. (2021) 10:e022567. doi: 10.1161/jaha.121.022567
36. Maggio, E, Bocchini, VP, Carnevale, R, Pignatelli, P, Violi, F, and Loffredo, L. Vitamin E supplementation (alone or with other antioxidants) and stroke: a meta-analysis. Nutr Rev. (2023). doi: 10.1093/nutrit/nuad114 [Epubh ahead of print]
37. Yang, C, Jia, X, Wang, Y, Fan, J, Zhao, C, Yang, Y, et al. Association between dietary total antioxidant capacity of antioxidant vitamins and the risk of stroke among US adults. Antioxidants. (2022) 11:2252. doi: 10.3390/antiox11112252
38. Xu, Q, Qian, X, Sun, F, Liu, H, Dou, Z, and Zhang, J. Independent and joint associations of dietary antioxidant intake with risk of post-stroke depression and all-cause mortality. J Affect Disord. (2023) 322:84–90. doi: 10.1016/j.jad.2022.11.013
39. Liu, X, Zhang, D, Liu, Y, Sun, X, Hou, Y, Wang, B, et al. A J-shaped relation of BMI and stroke: systematic review and dose-response meta-analysis of 4.43 million participants. Nutr Metab Cardiovasc Dis. (2018) 28:1092–9. doi: 10.1016/j.numecd.2018.07.004
40. Larsson, SC, Burgess, S, and Michaëlsson, K. Smoking and stroke: a mendelian randomization study. Ann Neurol. (2019) 86:468–71. doi: 10.1002/ana.25534
41. Awad, K, Mohammed, M, Martin, SS, and Banach, M. Association between electronic nicotine delivery systems use and risk of stroke: a meta-analysis of 1,024,401 participants. Arch Med Sci. (2023) 19:1538–40. doi: 10.5114/aoms/171473
42. Middleton, LE, Corbett, D, Brooks, D, Sage, MD, Macintosh, BJ, McIlroy, WE, et al. Physical activity in the prevention of ischemic stroke and improvement of outcomes: a narrative review. Neurosci Biobehav Rev. (2013) 37:133–7. doi: 10.1016/j.neubiorev.2012.11.011
43. Fan, J, Ma, W, Liu, J, Li, W, Wang, W, Gu, J, et al. Associations between socioeconomic status and stroke in American adults: a population-based study. Prev Med Rep. (2023) 35:102354. doi: 10.1016/j.pmedr.2023.102354
44. Qureshi, AI, Suri, MF, Saad, M, and Hopkins, LN. Educational attainment and risk of stroke and myocardial infarction. Med Sci Monit. (2003) 9:CR466–73.
45. Ma, Z, Zhang, Y, Zhou, C, Liu, D, Gu, S, and Zuo, H. Independent and combined effect of income and education attainment on the incidence of stroke events: a large-scale cohort study from rural communities in China. Neurol Res. (2023) 45:627–33. doi: 10.1080/01616412.2023.2176630
46. Annor, FB, Goodman, M, Okosun, IS, Wilmot, DW, Il’yasova, D, Ndirangu, M, et al. Oxidative stress, oxidative balance score, and hypertension among a racially diverse population. J Am Soc Hypertens. (2015) 9:592–9. doi: 10.1016/j.jash.2015.05.014
47. Kong, SY, Bostick, RM, Flanders, WD, McClellan, WM, Thyagarajan, B, Gross, MD, et al. Oxidative balance score, colorectal adenoma, and markers of oxidative stress and inflammation. Cancer Epidemiol Biomarkers Prev. (2014) 23:545–54. doi: 10.1158/1055-9965.Epi-13-0619
48. Lakkur, S, Bostick, RM, Roblin, D, Ndirangu, M, Okosun, I, Annor, F, et al. Oxidative balance score and oxidative stress biomarkers in a study of Whites, African Americans, and African immigrants. Biomarkers. (2014) 19:471–80. doi: 10.3109/1354750x.2014.937361
49. Cho, AR, Kwon, YJ, Lim, HJ, Lee, HS, Kim, S, Shim, JY, et al. Oxidative balance score and serum γ-glutamyltransferase level among Korean adults: a nationwide population-based study. Eur J Nutr. (2018) 57:1237–44. doi: 10.1007/s00394-017-1407-1
50. Marks, KJ, Hartman, TJ, Judd, SE, Ilori, TO, Cheung, KL, Warnock, DG, et al. Dietary oxidative balance scores and biomarkers of inflammation among individuals with and without chronic kidney disease. Nephron Extra. (2018) 8:11–23. doi: 10.1159/000490499
Keywords: stroke, NHANES, oxidative stress, oxidative balance score, prevention
Citation: Chen J, Liu J, Gu Z, Fan J, Lei S, Zhang Q, Pan K and Wang Y (2024) Adherence to oxidative balance score is inversely associated with the prevalence of stroke: results from National Health and Nutrition Examination Survey 1999–2018. Front. Neurol. 15:1348011. doi: 10.3389/fneur.2024.1348011
Received: 18 December 2023; Accepted: 11 March 2024;
Published: 04 April 2024.
Edited by:
Bianca Weinstock-Guttman, University at Buffalo, United StatesReviewed by:
Miguel Murguía-Romero, National Autonomous University of Mexico, MexicoCopyright © 2024 Chen, Liu, Gu, Fan, Lei, Zhang, Pan and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yongjie Wang, MTEwMTgxOTZAemp1LmVkdS5jbg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.