
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
OPINION article
Front. Neurol., 05 October 2023
Sec. Neuro-Otology
Volume 14 - 2023 | https://doi.org/10.3389/fneur.2023.1289357
In a recent study of patients with Ménière disease (MD), Xia et al. (1) investigated the anatomical variations of the inner ear hypothesis relating to development of endolymphatic hydrops (ELH). These authors also examined the role abnormalities of the jugular bulb (JB) may play in the pathogenesis of ELH. The large series of patients and controls were thoroughly studied with computed tomography (CT) and radiological indices were compared between the MD ears and control ears. The authors concluded that the anatomical variations observed in the vestibular aqueduct (VA) rather than abnormalities in the JB may predispose patients to MD.
The VA is a bony canal in the osseous labyrinth containing the endolymphatic duct and sac. Enlargement of the VA has been deemed the most common congenital inner ear malformation that is also associated with sensorineural hearing loss (2, 3). CT is an imaging method with high spatial resolution that provides exceptional detail of bone, allowing for detailed depiction of the osseous VA at the expense of radiation. Furthermore, CT cannot show the membranous labyrinth including the VA. With MR imaging, the signal intensity for each tissue depends on the intrinsic composition of that tissue (i.e., fluid content) and on the radiofrequency pulse applied to the tissue to generate images. Because the membranous labyrinth (investing the osseous labyrinth) of the inner ear is filled with fluid (lymph), MR imaging has been typically used to delineate the vestibulocochlear lymph space (4). In this respect, previous researchers have used advanced gadolinium-enhanced MR imaging studies to investigate ELH, with emphasis on diagnosis of Ménière disease (5–7). Off-label use of high-dose gadolinium compounds that may be ototoxic, the intravenous or interventional, intratympanic administration of contrast material, delayed and time-consuming imaging that may be associated with enhancement of the surrounding structures (i.e., vessels), and high-strength 3.0 T MR units have arisen as certain limitations to routine clinical use of these imaging protocols, however (8).
In our clinical and imaging practices, we recommend that MR imaging be considered in patients with otovestibular symptoms, suggestive of MD. To this end, we have advocated a simple MR imaging protocol of the inner ear that would employ the 3D-constructive interference in steady state (3D-CISS) sequence (or equivalent fast gradient-echo pulse sequence). The CISS sequence is readily available in most high-strength (1.5 T or above) MR units and allows for fast acquisition of submillimeter high resolution images and multiplanar reconstructions that facilitate delineation of fine structures in the inner ear, and the JB. Because of a direct cisternographic effect that enables direct depiction of the vestibulocochlear lymph space, visualization of the minute anatomic structures in the membranous labyrinth (including the VA) and the acoustic nerves is feasible, sparing the administration of gadolinium material (9). Additional, post-processing maximum intensity projection (MIP) images with a slab thickness 4–5 mm generated form the original MR data may further increase conspicuity of the fine inner ear structures (Figure 1).
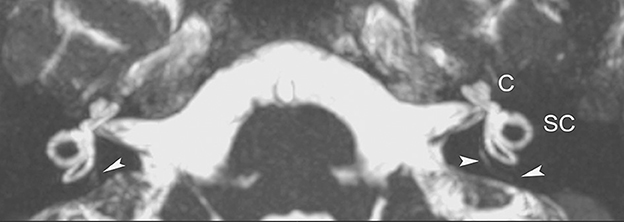
Figure 1. Axial non gadolinium-enhanced 3D-CISS image (with MIP technique) delineates normal anatomy of the inner auditory canal and the membranous labyrinthine structures on both sides, in a 16-year-old patient with vertigo and left ear tinnitus. At this image level, portions of the VA (arrowheads) can be seen. C, coclea; SC, semicircular canals.
We have found the single MR sequence approach both simple and efficacious and recommend this fast imaging survey for exploring inner ear abnormalities, in patients with symptoms that may be related to MD. Perhaps, the authors would agree with us that dedicated MR imaging protocols could be complementary to CT studies of the inner ear to acquire high resolution images of the integrated osseous and membranous labyrinthine anatomic structures. Besides, abnormalities of the osseous labyrinth may not be uncommon, especially in patients with otovestibular symptoms, and changes in the petrous bone structures (i.e., early labyrinthitis ossificans, otosclerosis) may need to be thoroughly studied on the high-resolution CT (HRCT) images.
DT: Conceptualization, Formal analysis, Resources, Supervision, Validation, Writing—original draft, Writing—review and editing. ST: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Software, Validation, Writing—original draft, Writing—review and editing. VM: Data curation, Resources, Supervision, Validation, Visualization, Writing—review and editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Xia K, Lei P, Liu Y, Li J, Wang M, Leng Y, et al. Comparison of radiological abnormalities between the jugular bulb and the vestibular aqueduct in patients with Ménière's disease. Front Neurol. (2023) 14:1184232. doi: 10.3389/fneur.2023.1184232
2. Quirk B, Youssef A, Ganau M, D'Arco F. Radiological diagnosis of the inner ear malformations in children with sensorineural hearing loss. BJR Open. (2019) 1:20180050. doi: 10.1259/bjro.20180050
3. Tong KA, Harnsberger HR, Dahlen RT, Carey JC, Ward K. Large vestibular aqueduct syndrome: a genetic disease? Am J Roentgenol. (1997) 168:1097–101. doi: 10.2214/ajr.168.4.9124122
4. Suárez Vega VM, Dominguez P, Caballeros Lam FM, Leal JI, Perez-Fernandez N. Comparison between high-resolution 3D-IR with real reconstruction and 3D-FLAIR sequences in the assessment of endolymphatic hydrops in 3 tesla. Acta Otolaryngol. (2020) 140:883–8. doi: 10.1080/00016489.2020.1792550
5. Han Z, Qiu X, Huang Y, Sun Q, Ding H, Xie J, et al. Correlation between grading methods of the cochlear endolymphatic hydrops and hearing loss in Meniere's disease using three-dimensional real inversion recovery sequences. Acta Otolaryngol. (2023) 143:370–5. doi: 10.1080/00016489.2023.2209134
6. Nakashima T, Naganawa S, Sugiura M, Teranishi M, Sone M, Hayashi H, et al. Visualization of endolymphatic hydrops in patients with Meniere's disease. Laryngoscope. (2007) 117:415–20. doi: 10.1097/MLG.0b013e31802c300c
7. van Steekelenburg J, van Weijnen A, de Pont L, Vijlbrief OD, Bommelje C, Koopman JP, et al. Value of endolymphatic hydrops and perilymph signal intensity in suspected Ménière disease. Am J Neuroradiol. (2020) 41:529–34. doi: 10.3174/ajnr.A6410
8. de Pont L, van Steekelenburg J, Verbist B, van Buchem MA, Blom HM, Hammer S. State of the art imaging in Menière's disease. Tips and tricks for protocol and interpretation. Curr Radiol Rep. (2020) 8:25. doi: 10.1007/s40134-020-00365-z
Keywords: MRI, inner ear, labyrinth, Ménière disease, hearing loss
Citation: Theodorou DJ, Theodorou SJ, Ahnoula E and Mitsios V (2023) Simplified MR imaging of the inner ear in patients with Ménière's disease. Front. Neurol. 14:1289357. doi: 10.3389/fneur.2023.1289357
Received: 05 September 2023; Accepted: 21 September 2023;
Published: 05 October 2023.
Edited by:
Brian John McKinnon, University of Texas Medical Branch at Galveston, United StatesReviewed by:
Hans Thomeer, University Medical Center Utrecht, NetherlandsCopyright © 2023 Theodorou, Theodorou, Ahnoula and Mitsios. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Daphne J. Theodorou, ZGFwaG5lX3RoZW9kb3JvdUBob3RtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.