- 1The First School of Clinical Medicine, Guangxi University of Traditional Chinese Medicine, Nanning, China
- 2Department of Rehabilitation Medicine, The First Affiliated Hospital of Guangxi Medical University, Nanning, China
- 3The First Affiliated Hospital of Guangxi University of Traditional Chinese Medicine, Nanning, China
- 4Department of Traditional Chinese Medicine, Nanning Maternal and Child Health Hospital, Nanning, China
- 5Sainz College of New Medicine, Guangxi University of Traditional Chinese Medicine, Nanning, China
Background: Shoulder-hand syndrome (SHS) is a common complication after stroke, and SHS-induced pain significantly hampers patients’ overall recovery. As an alternative therapy for pain relief, acupuncture has certain advantages in alleviating pain caused by SHS after stroke. However, choosing the best treatment plan from a variety of acupuncture options is still a serious challenge in clinical practice. Therefore, we conducted this Bayesian network meta-analysis to comprehensively compare the effectiveness of various acupuncture treatment methods.
Methods: We systematically searched for randomized controlled trials (RCTs) of acupuncture treatment in patients with post-stroke SHS published in PubMed, Embase, Cochrane, and Web of Science until 9 March 2023. We used the Cochrane bias risk assessment tool to assess the bias risk in the included original studies.
Results: A total of 50 RCTs involving 3,999 subjects were included, comprising 19 types of effective acupuncture interventions. Compared to single rehabilitation training, the top three interventions for VAS improvement were floating needle [VAS = −2.54 (95% CI: −4.37 to −0.69)], rehabilitation + catgut embedding [VAS = −2.51 (95% CI: −4.33 to −0.68)], and other multi-needle acupuncture combinations [VAS = −2.32 (95% CI: −3.68 to −0.94)]. The top three interventions for improving the Fugl–Meyer score were eye acupuncture [Meyer = 15.73 (95% CI: 3.4627.95)], other multi-needle acupuncture combinations [Meyer = 12.22 (95% CI: 5.1919.34)], and traditional western medicine + acupuncture + traditional Chinese medicine [Meyer = 11.96 (95% CI: −0.59 to 24.63)].
Conclusion: Multiple acupuncture methods are significantly effective in improving pain and upper limb motor function in post-stroke SHS, with relatively few adverse events; thus, acupuncture can be promoted.
Systematic Review Registration: https://www.crd.york.ac.uk/prospero/, CRD42023410957.
1 Introduction
Stroke is a leading cause of disability in old people. The absolute number of stroke events worldwide increased by 70.0% from 1990 to 2019, making stroke the third leading cause of disability-adjusted life years (DALYs) (1, 2). Despite early treatment, patients with strokes often have residual sequelae, mainly characterized by hemiparesis. Shoulder hand syndrome (SHS) is a common complication after stroke, with main clinical manifestations including severe pain in the affected shoulder, along nerve distributions and injury regions, hand swelling, and sensory impairment. The incidence rate of SHS is approximately 2%–50%, with a peak incidence at 1–6 months after stroke (3, 4). Hence, this period is critical for the recovery of patients. Severe pain significantly undermines patients’ motivation for recovery, which is detrimental to the expected recovery and their return to society and family, thereby imposing a huge burden on clinical medical work (5).
Currently, treatments for post-stroke SHS pain mainly include oral medication, ganglion radiofrequency ablation, and nerve block. Oral medication can cause adverse reactions such as fatigue, liver and kidney damage, and gastrointestinal dysfunction (6–8). Nerve radiofrequency ablation and nerve block have certain analgesic effects, but as more invasive treatments, they only provide temporary pain relief and patients cannot benefit from them in the medium to long term (9). Therefore, optimizing treatment strategies for post-stroke SHS is a focus of clinical physicians. Chinese medicine acupuncture, through its unique theory of meridians, plays a positive role in treating pain, arthritis, and recovery after stroke. It is safe and effective with few adverse reactions, and it has been internationally recognized as an effective supplement and alternative therapy for pain treatment (10–12).
There are many types of acupuncture, including electroacupuncture, fire needling, warming needles, and catgut embedding. These diversified acupuncture methods have been introduced by some researchers into the treatment of post-stroke SHS, even in combination with other treatments (13). However, selecting the best acupuncture plan in clinical practice remains challenging. Therefore, we conducted this Bayesian network meta-analysis on acupuncture treatment for post-stroke SHS in the hope of providing the best acupuncture combination regimen and basis to assist in medical decision-making.
2 Methods
2.1 Study registration
This network meta-analysis was conducted based on the preferred reporting items for systematic reviews and meta-analyses (PRISMA-NMA) (14). This study has been registered on PROSPERO, and the registration website is https://www.crd.york.ac.uk/prospero/, (ID: CRD42023410957).
2.2 Eligibility criteria
2.2.1 Inclusion criteria
P (population): patients meeting the diagnostic criteria for post-stroke SHS, regardless of age, race, and gender. Post-stroke SHS is diagnosed according to the “Rehabilitation Evaluation and Treatment of Stroke” and the “2016 China Stroke Diagnosis and Treatment Consensus” (14, 15).
The diagnostic criteria of stroke were formulated according to the “2016 China Stroke Diagnosis and Treatment Consensus.” Diagnostic points are as follows: ① acute onset; ② focal neurological deficit (such as weakness or numbness of one side of face or limb, language disorder); a few patients have comprehensive neurological deficit, which may be accompanied by headache, vomiting, elevated blood pressure, and different degrees of consciousness disorder; ③ symptoms or signs of unlimited duration (when imaging shows responsible lesions) or lasting more than 24 h (when imaging shows no responsible lesions); ④ stroke diagnosed by CT or MRI of the head, with non-cerebral vascular causes excluded.
The diagnostic criteria for shoulder-hand syndrome after stroke were the criteria established by “Rehabilitation Evaluation and Treatment of Stroke.” The diagnosis points are as follows: ① patients have unilateral shoulder and hand pain, skin flushing, skin temperature rising, and finger bending limitation after stroke. ② No evidence of local trauma, infection, and peripheral vascular disease.
I (intervention): studies that use acupuncture in the treatment group.
C (comparison): studies that use rehabilitation, medication, or conventional acupuncture in the control group.
O (outcome): the primary outcome measures are the visual analog scale (VAS) for pain and the Fugl–Meyer motor function assessment scale; the secondary outcome measures are the Barthel index (BI) and shoulder-hand syndrome evaluation scale (SHSS).
S (study design): randomized controlled trials (RCTs).
2.2.2 Exclusion criteria
P (population): studies with severe problems in the diagnostic criteria for post-stroke SHS or SHS caused by other diseases.
I (intervention): (1) studies analyzing the effects of different frequencies and intensities of an intervention method, which are isolated from other intervention methods and cannot be used to estimate the effect size and (2) studies that do not include acupuncture in any of the groups.
C (comparison): none.
O (outcome): studies with serious bias in outcome measure scoring (such as those without baseline assessment or incomplete outcome data).
S (study design): (1) full conference abstracts not published through peer review; (2) studies with a sample size of <10, which are unlikely to achieve ideal statistical power; (3) crossover design studies. As the crossover design can generally achieve the preset statistical power with only a small sample size, we can only extract the results of the first phase of the trial in a systematic review. However, some crossover design studies have a small sample size and do not report the independent results of the first phase, so these studies need to be excluded.
2.3 Data sources and search strategy
RCTs on acupuncture treatment for post-stroke SHS are retrieved from PubMed, Cochrane, Embase, Web of Science, VIP (Chinese), Wanfang (Chinese), CNKI (Chinese), and Chinese Biomedical (Chinese) databases. There are no restrictions on language and publication years, and the retrieval date is until 12 March 2023. The retrieval is conducted in the form of “subject word + free word,” the search terms for the Chinese databases include “stroke,” “shoulder-hand syndrome,” “painful malnutrition syndrome,” “painful nutritional disorder,” “complex regional pain syndrome,” “reflex sympathetic dystrophy syndrome,” “acupuncture,” “electroacupuncture,” “warming needle,” “fire needling,” “floating needle,” and “catgut embedding “. The search strategy for the English databases is shown in Supplementary Table S1.
2.4 Study selection
The retrieved studies were imported into EndNote, and duplicate publications were excluded. Then, the titles and abstract were checked to preliminarily select the original studies that met the criteria and download the full text. The full texts were read to select the original RCT studies that met the criteria of this systematic review. The study selection was independently conducted by two researchers (XT and XH), and any disputes were arbitrated by a third researcher (HY) after the search was completed.
2.5 Data extraction
Data extraction was independently performed by two researchers (NW and YJ), and a third researcher (JH) was asked to arbitrate disputes, if any. A data extraction electronic spreadsheet was developed to extract data, including the title, English abstract, first author, year of publication, study design, author’s country, diagnostic criteria, interventional protocol, type of stroke, treatment time, number of cases, gender, age, disease course, follow-up time, outcome measures, selection bias, implementation bias, measurement bias, loss to follow-up bias, reporting bias, and other biases.
2.6 Assessment of study quality/risk of bias in studies
Quality assessment was conducted by two researchers (JH and XH) using Cochrane’s bias risk assessment tool RoB 2.0 (16, 17) to assess the risk of bias in the 50 included original studies. The assessment tool includes the following seven items: randomization process, method of identifying or recruiting participants, bias due to deviation from the expected intervention, missing outcome data, bias in outcome measurement, reporting selection bias, and overall bias. The risk of bias in each domain is classified into three levels: low risk of bias, high risk of bias, and some concerns. After completion, a cross-check would be conducted, and if there was a dispute, a third researcher (TH) was asked to assist in adjudicating. Finally, the risk of bias graph was plotted.
2.7 Outcomes
The primary outcome measures are the visual analog scale (VAS) for pain and the Fugl–Meyer upper limb motor function assessment scale. The secondary outcome measures are the Barthel index (BI) and the shoulder-hand syndrome evaluation scale (SHSS). Since our outcome measures are all continuous variables, and there seem to be differences among the studies at baseline, we used the change from baseline to post-treatment as the effect size in the meta-analysis.
2.8 Synthesis methods
This study used a Bayesian random-effects model to compare the effect estimates of various to compare their effectiveness. The Markov chain Monte Carlo method was used for modeling, with four Markov chains running simultaneously, and the annealing times were set to 20,000. The modeling was completed after 50,000 simulation iterations. The deviance information criterion (DIC) was used to compare model fit and global consistency. If there is a closed loop in the network, we would use the node-splitting method to analyze local consistency. In addition, we ranked these interventions based on the surface under the cumulative ranking curve (SUCRA) values, and a league table was generated to compare the differences in effectiveness between various interventions. A funnel plot was used to intuitively reflect the heterogeneity among the studies. Analyses were completed in Stata 15.0 (Stata Corporation, College Station, TX) and R 4.2.0 (R Development Core Team, Vienna, http://www.R-project.org). A p-value of <0.05 indicates a statistically significant difference.
3 Results
3.1 Study selection
A total of 4,697 relevant articles were retrieved from the databases, including 162 from English databases and 4,535 from Chinese databases. A total of 558 duplicate articles were marked in EndNote and eliminated. After reading the titles and abstracts of the remaining 4,139 articles, we finally determined to download the full texts of 66 articles. According to a full-text review, 50 RCTs (18–67) were eligible and included in this systematic review (as shown in Figure 1; Supplementary Table S2).
3.2 Study characteristics
This study included 50 articles in total, involving 3,999 patients with SHS after stroke, and 2 of them were multi-center RCTs (41, 42). The included articles were published between 2002 and 2022, covering 19 acupuncture treatment methods. There were 11 types of acupuncture combined with other treatments. None of the original studies we included had conflicts of interest. The basic information of the included studies can be found in Table 1.
3.3 Detailed explanation of intervention methods
This systematic review covers 19 acupuncture treatment methods (routine acupuncture).
Point-toward-point needle insertion, warming needles, electroacupuncture, fire needling, Jin’s three-needle technique, floating needle, eye acupuncture, silver needle, trocar needle, spoon-like needle, thumbtack needle, abdominal acupuncture, scalp acupuncture, contralateral blood-letting and contralateral needling, catgut embedding, wrist-ankle acupuncture, balancing acupuncture, eightfold method of the sacred tortoise, four special acupuncture techniques (18, 44, 55, 56, 64), and four special needle insertion methods (36, 42, 46, 47, 60, 63, 66). Affected limb movement during acupuncture was reported in three studies (24, 44, 67). The detailed intervention methods are provided in Supplementary Table S3.
3.4 Results of bias risk assessment
In our 50 included studies, 43 were assessed as having “some concerns” for overall bias and 7 had a high risk of bias. The high risk of bias in the seven studies was because the intervention implementers knew the intervention. Since there was no detailed information on allocation concealment in these 50 RCTs, 43 studies were classified as “some concerns.” Due to the experimental environment, five studies deviated from the predetermined intervention measures and were assessed as having “some concerns.” During the implementation of the intervention, because the evaluators knew the intervention, seven studies were classified as high risk and four as some concerns. The detailed bias risk assessment results are presented in Figure 2.
4 Meta-analysis
4.1 VAS
4.1.1 Correlation between intervention methods
This review included 38 studies (19–22, 28–34, 37, 39–46, 48, 50, 52–67) that reported the pain relief effect of multiple acupuncture methods for post-stroke SHS using the VAS scale. The main intervention methods included Treat 5 (western medicine + rehabilitation + acupuncture), Treat 6 (electroacupuncture), Treat 1 (rehabilitation), Treat 3 (routine acupuncture), and Treat 14 (acupuncture on the non-affected limb). With the development of acupuncture in recent years, Treat 7 (warming needle), Treat 8 (fire needling), Treat 9 (Jin’s three-needle technique), Treat 10 (floating needle) have also gradually started to be explored for their use in pain relief in SHS after stroke. A detailed comparison of the intervention methods is illustrated in Figure 3.
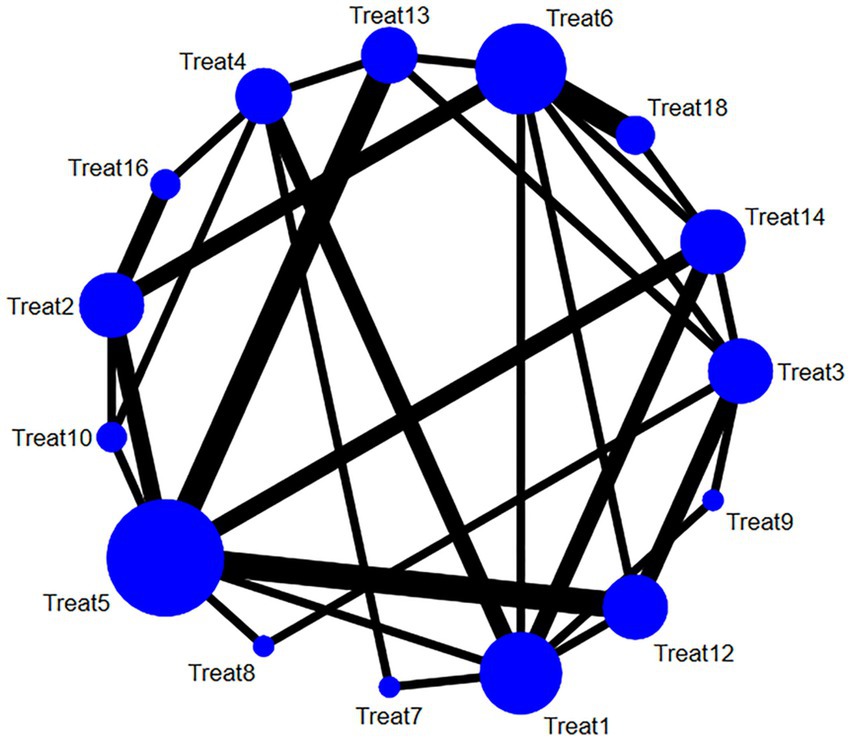
Figure 3. Network relationship diagram of the VAS pain relief of multiple acupuncture methods for post-stroke SHS (the larger the dot in the figure, the more samples it contains; the thicker the line between two dots, the more documents are compared between the two groups).
4.1.2 Synthesized results
The studies included in this analysis met the overall consistency hypothesis test (p > 0.05), so we used a consistency model for Bayesian network meta-analysis. The results of the analysis show that compared to the routine intervention Treat 1 (rehabilitation), Treat 10 (floating needle), Treat 16 (rehabilitation + catgut embedding), Treat 13 (other multi-needle acupuncture combinations), Treat 12 (special needle operation and technique), Treat 14 (acupuncture on the non-affected limb), Treat 8 (fire needling), Treat 7 (warming needle), Treat 4 (rehabilitation + acupuncture), Treat 6 (electroacupuncture), Treat 5 (western medicine + rehabilitation + acupuncture), and Treat 3 (routine acupuncture) could significantly reduce VAS score, (p < 0.05) as shown in Figure 4.
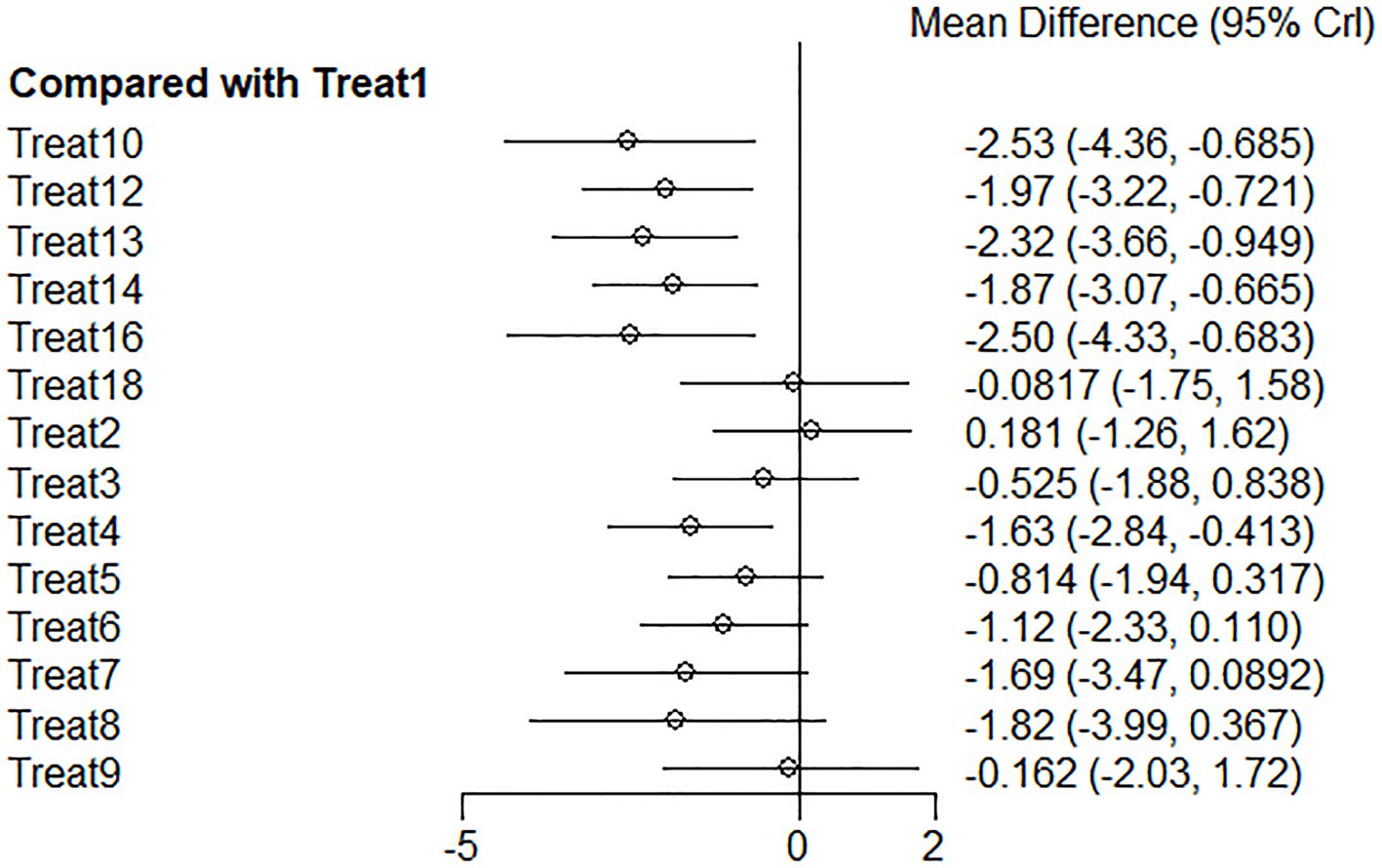
Figure 4. VAS forest plot of network meta-analysis of acupuncture treatments versus rehabilitation therapy for post-stroke shoulder-hand syndrome [the left side of the picture represents the results obtained after comparing various intervention methods with the conventional group Treat 1 (rehabilitation). The horizontal line for each intervention represents the confidence interval for estimating the effect size. If the confidence interval does not contain a null line, the difference is statistically significant].
Among these effective intervention methods, the top three were Treat 10 (floating needle), Treat 16 (rehabilitation + catgut embedding), and Treat 13 (other multi-needle acupuncture combinations), with ranking probabilities of 0.84, 0.83, and 0.82, respectively. At the same time, compared to routine rehabilitation, their improvements in VAS were Treat 10 (floating needle) −2.54 (95% CI: −4.37 to −0.69), Treat 16 (rehabilitation + catgut embedding) −2.51 (95% CI: −4.33 to −0.68), and Treat 13 (other multi-needle acupuncture combinations) −2.32 (95% CI: −3.68 to −0.94), with significant differences. The detailed results of pairwise comparisons are shown in Table 2.
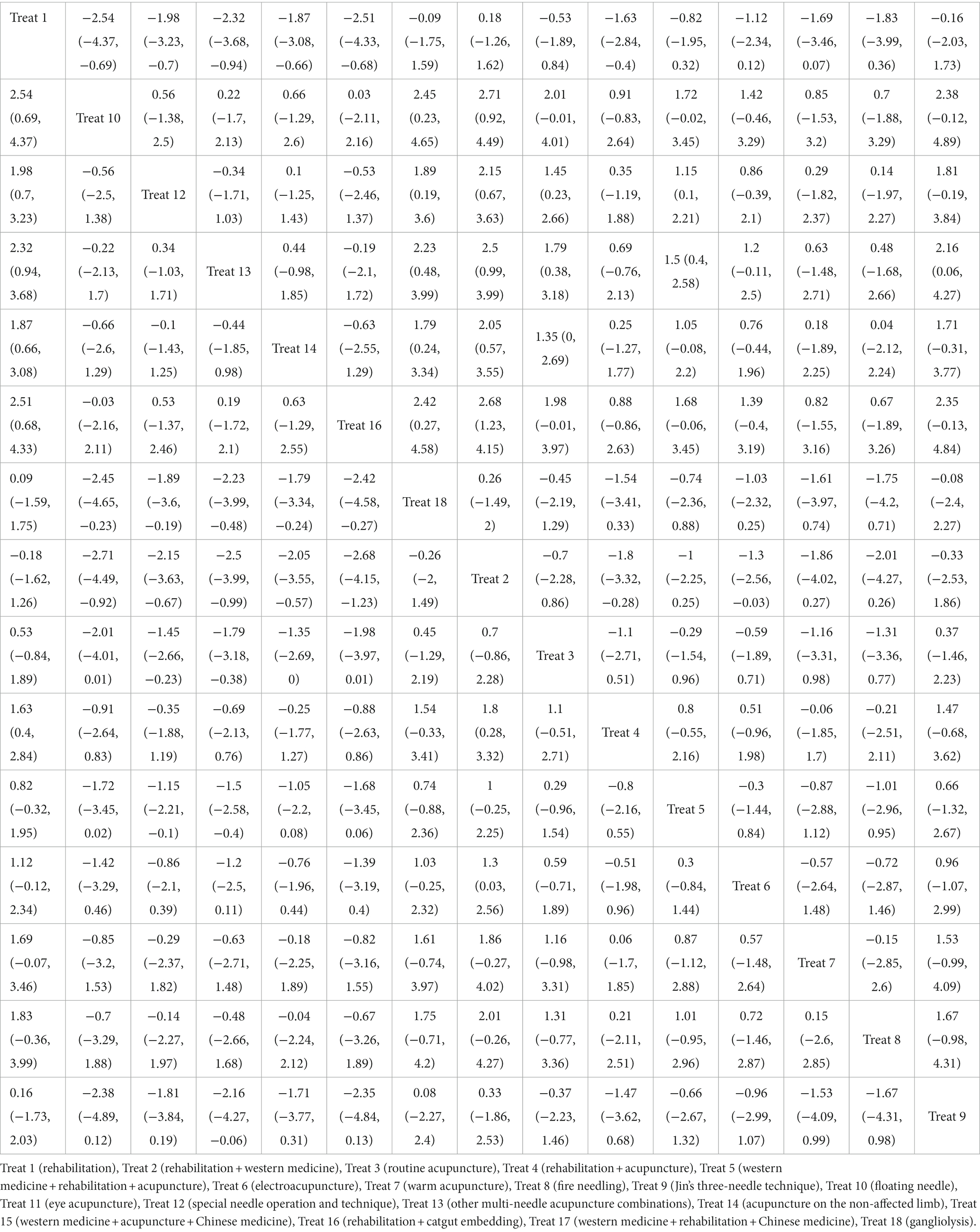
Table 2. Fugl–Meyer league table of network meta-analysis of acupuncture treatment for post-stroke SHS.
4.1.3 Reporting biases
There appears to be no significant publication bias, as shown in the funnel plot (shown in Figure 5).
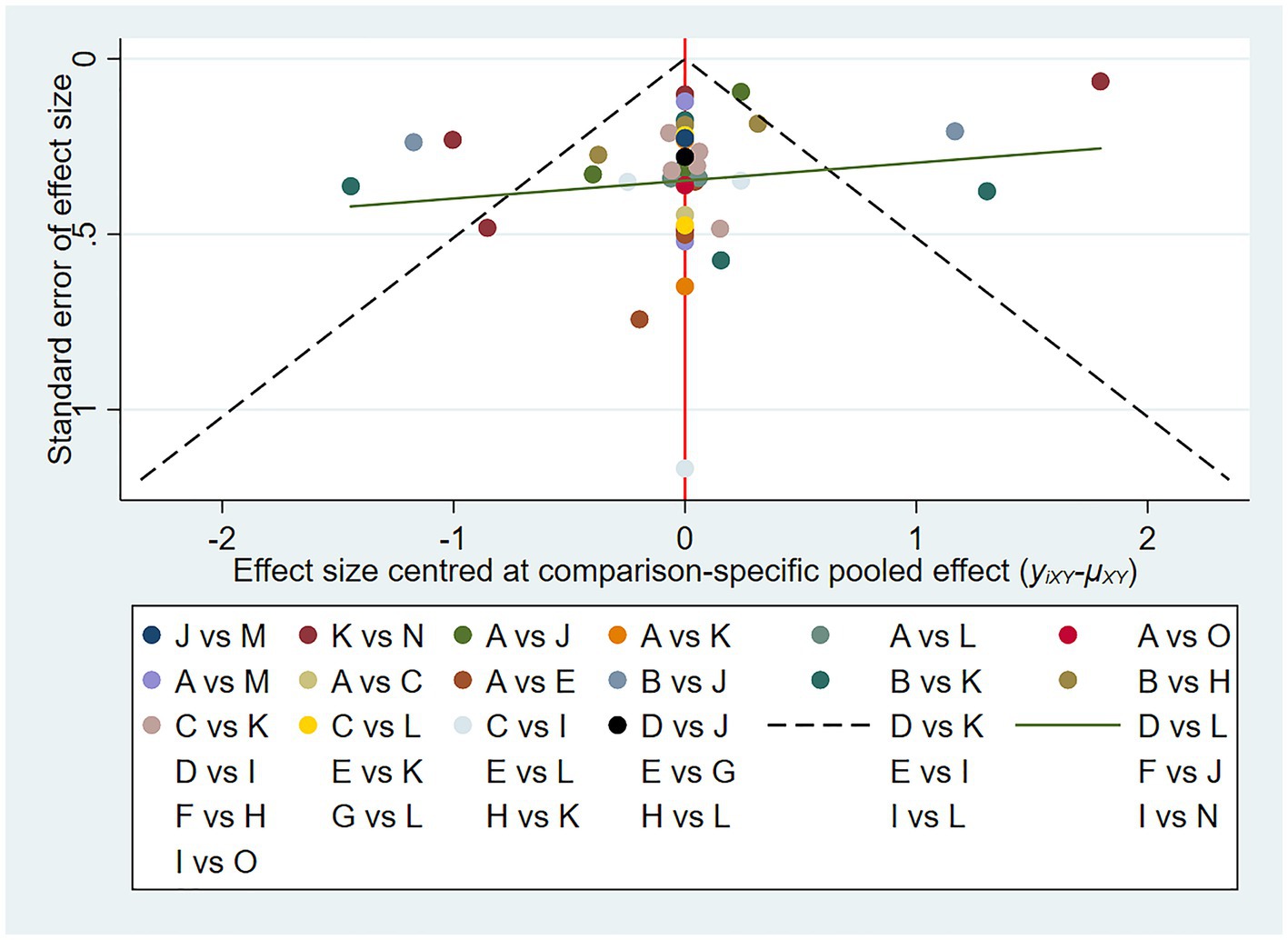
Figure 5. VAS funnel plot of network meta-analysis of acupuncture treatment for post-stroke shoulder-hand syndrome (each dot represents the study we included, and the horizontal axis represents the effect size).
4.2 Fugl–Meyer
4.2.1 Correlation between intervention methods
A total of 48 studies (18–32, 34–41, 43–47, 49–67) reported the effect of multiple acupuncture methods on the upper limb motor function of the Fugl–Meyer score in SHS after stroke. The main intervention methods consisted of Treat 1 (rehabilitation), Treat 4 (rehabilitation + acupuncture), Treat 5 (western medicine + rehabilitation + acupuncture), Treat 6 (electroacupuncture), Treat 12 (special needle operation and technique). With the application and development of acupuncture in recent years, some special acupuncture therapies have gradually emerged and have been used in the recovery of upper limb motor function in SHS after stroke, such as Treat 8 (fire needling), Treat 9 (Jin’s three-needle technique), Treat 10 (floating needle), Treat 11 (eye acupuncture), and Treat 15 (western medicine + acupuncture + Chinese medicine). A detailed comparison of the intervention methods is presented in Figure 6.
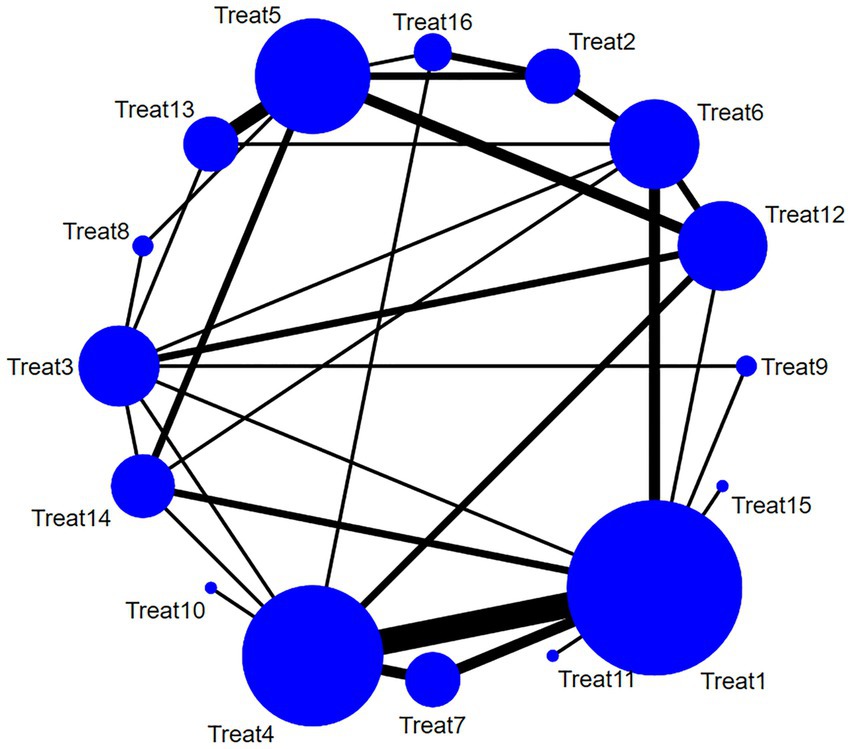
Figure 6. Network diagram of diversified acupuncture treatment plans for the improvement of Fugl–Meyer in post-stroke shoulder-hand syndrome (the larger the dot in the figure, the more samples it contains; the thicker the line between two dots, the more documents are compared between the two groups).
4.2.2 Synthesized results
The included studies met the overall consistency hypothesis test (p > 0.05), so we used a consistency model for Bayesian network meta-analysis. The results of the analysis show that compared to Treat 1 (rehabilitation), Treat 11 (eye acupuncture), Treat 13 (other multi-needle acupuncture combinations), Treat 15 (western medicine + acupuncture + Chinese medicine), Treat 7 (warm acupuncture), Treat 12 (special needle operation and technique), Treat 16 (rehabilitation + catgut embedding), Treat 10 (floating needle), Treat 6 (electroacupuncture), Treat 14 (acupuncture on the non-affected limb), Treat 9 (Jin’s three-needle), Treat 4 (rehabilitation + acupuncture), Treat 8 (fire needling), Treat 5 (western medicine + rehabilitation + acupuncture), and Treat 3 (routine acupuncture) (Figure 7) could significantly increase the Fugl–Meyer score (p < 0.05).
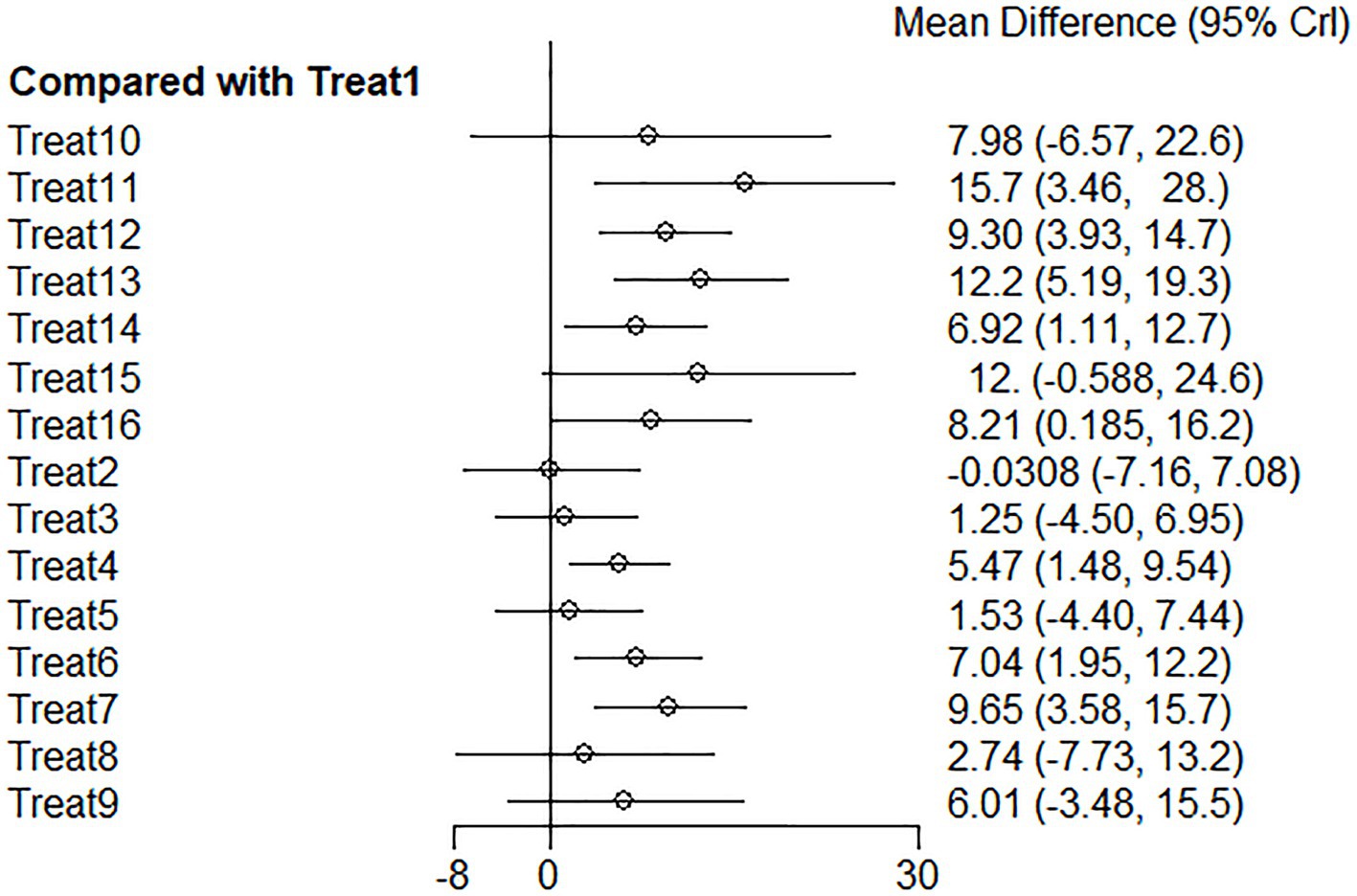
Figure 7. Fugl–Meyer forest plot of network meta-analysis of acupuncture treatments versus rehabilitation therapy for post-stroke shoulder-hand syndrome [the left side of the picture represents the results obtained by comparing various intervention methods with the conventional group Treat 1 (rehabilitation). The horizontal line corresponding to each intervention method represents the confidence interval of the estimated effect. If the confidence interval does not contain a null line, the difference is statistically significant].
Among these effective intervention methods, the top three are Treat 11 (eye acupuncture), Treat 13 (other multi-needle acupuncture combinations), and Treat 15 (western medicine + acupuncture + Chinese medicine), with ranking probabilities of 0.88, 0.84, and 0.75, respectively. At the same time, compared to routine rehabilitation, their improvements in Fugl–Meyer scores were Treat 11 (eye needle) 15.73 (95% CI: 3.4627.95), Treat 13 (other multi-needle acupuncture combinations) 12.22 (95% CI: 5.1919.34), and Treat 15 (western medicine + acupuncture + Chinese medicine) 11.96 (95% CI: −0.59 to 24.63). There was a significant difference between the first two, while Treat 11 (eye needle) showed good therapeutic effects. However, due to the small sample size, this result should be interpreted cautiously. The degree of improvement of the intervention method Treat 15 (western medicine + acupuncture + Chinese medicine) was not significant. The detailed results of pairwise comparisons are provided in Table 3.
4.2.3 Reporting biases
There was no significant publication bias, as shown in the funnel plot (shown in Figure 8).
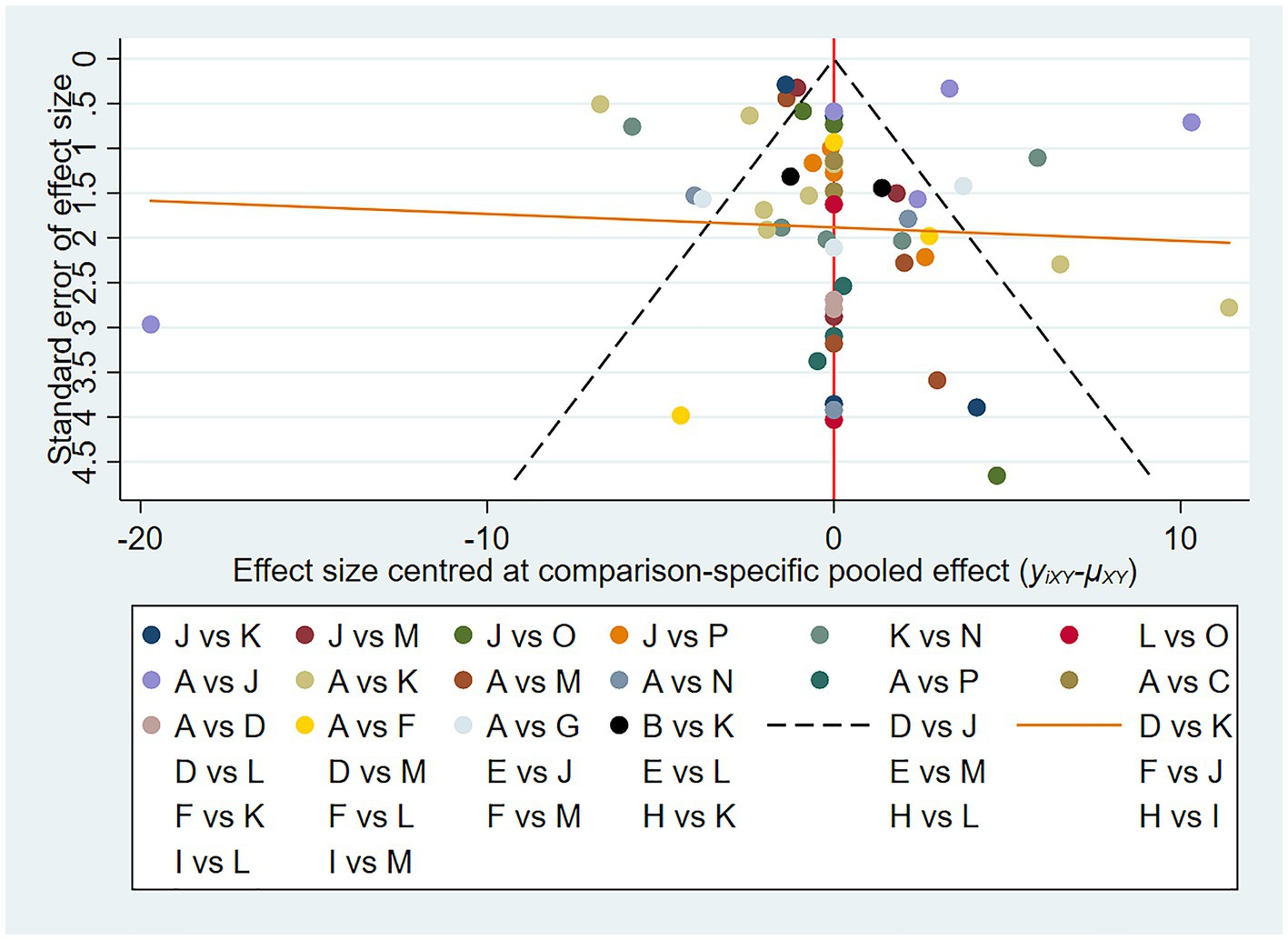
Figure 8. Fugl–Meyer funnel plot of network meta-analysis of acupuncture treatment for post-stroke shoulder-hand syndrome (each dot represents the study we included, and the horizontal axis represents the effect size).
4.3 Secondary outcome measures
We also analyzed the secondary outcome measures of Barthel index and SHSS. Compared to conventional treatment, various interventions did not significantly improve Barthel index or SHSS. The analysis results of secondary outcome measures are presented in Appendix 1.
5 Discussion
5.1 Summary of the main findings
Our network meta-analysis found that the top five interventions for improving pain according to the VAS scale are floating needle, rehabilitation + catgut embedding, other multi-needle acupuncture combinations, special needle operation and technique, and acupuncture on non-affected limb, which have a significant effect on pain relief. The best five interventions for the Fugl–Meyer score are eye needle, other multi-needle acupuncture combinations, western medicine + acupuncture + traditional Chinese medicine, warming needles, and special needle operation and technique, which could significantly improve upper limb motor function.
We found that rehabilitation + catgut embedding was effective in pain relief. Previous studies have also reviewed this intervention, and the analgesic principle may be a continuous stimulation by absorbable surgical sutures at acupoints, leading to a sterile inflammatory response, and ultimately promoting tissue regeneration (66, 68).
5.2 Comparison with previous studies (other reviews)
Although previous studies have also attempted to analyze the effects of acupuncture treatment on post-stroke SHS, some of them only explored the relative effectiveness of a single type of acupuncture or a certain acupuncture combination with rehabilitation and the control group (69–72). Post-stroke SHS is caused by multiple etiologies. Single therapy may not achieve the ideal pain relief. The clinical practice tends to combine multiple intervention methods, which can help explore more reasonable and effective treatment options. The number of types of acupuncture and studies included in existing network meta-analyses is limited (73), but there are many types of acupuncture. Furthermore, the above studies did not consider the existing types of acupuncture or combined acupuncture treatment methods to comprehensively compare various acupuncture interventions.
The mainstream treatment for post-stroke SHS is still rehabilitation therapy. As an indispensable intervention for treating this disease, it focuses on function recovery. Meanwhile, the obstacles affecting function recovery should be tackled to reduce the chances of patients refusing rehabilitation. Aerobic exercise of the upper limbs is found to reduce pain during the day and during exercise (74, 75). Some studies have reported that the combination of two or more therapies may be more effective than rehabilitation alone. Acupuncture combined with rehabilitation training can significantly help in reducing pain scores, promoting limb motor function recovery, and improving overall effectiveness (69–71, 76).
Drug therapy includes oral calcium channel modulators, anti-inflammatory, analgesic, antidepressants, or invasive injections of corticosteroids, bisphosphonates, and botulinum toxin (77, 78). Although drug treatment is convenient and quick, it has limited effects, and long-term use can produce adverse reactions such as hepatorenal and cardiac toxicity, excessive sedation, and drug resistance (79). Some drugs also have the possibility of recurrence after withdrawal and cannot fundamentally control and treat this disease (78, 80–83). In contrast, acupuncture has the advantages of high safety and no toxic side effects and is more easily accepted by patients with heart, liver, and kidney damage.
Neural stimulation, nerve block, and ganglion radiofrequency ablation can avoid the adverse systemic effects induced by drug treatment. Nonetheless, invasive surgery has certain adverse reactions and risks, and the implanted stimulation device may also have problems such as wire disconnection, requiring regular battery replacement (78, 84). A study has even found that the effects of standard high-frequency neurostimulation may be worse than acupuncture or other types of electrical stimulation, and acupuncture can become a promising treatment method for patients with drug-resistant neuropathic pain (84). The nerve block needs to be carried out under ultrasound guidance to improve safety. After a single treatment session, 61.8% of patients still have pain recurrence within 3 months. For chronic pain, it cannot achieve fundamental relief (78, 85–87). Ganglion radiofrequency ablation may cause risks of sensory and motor dysfunction and nerve damage, with small clinical improvement in the VAS score of patients with chronic root pain (88). Its long-term therapeutic effects are still controversial.
The treatment of post-stroke SHS is to relieve pain in the early stage of the disease without affecting the motor function and rehabilitation process of the affected limb. Conventional analgesic drugs, such as opioids and anti-inflammatory drugs, have a variety of side effects such as reduced motor function, induced hyperalgesia, and lethargy (89). At present, acupuncture is widely used for stroke rehabilitation and various pain-related diseases in China, the United States, Europe, and North America. Although acupuncture is an invasive treatment, the incidence of acupuncture-induced adverse reactions is significantly lower than that of many drugs or other recognized medical interventions according to the consensus report for the NIH Conference (90). Acupuncture can reduce the excitability of the pain pathway by reducing excitatory neurotransmitters and promoting inhibitory neurotransmitters (91, 92). Electroacupuncture has been shown to induce peripheral opioid receptors in rats, producing long-term analgesic effects for up to 144 h, improving motor function, and normalizing neurotransmitter metabolism (93). A preclinical study has also shown that acupuncture’s antihyperalgesic effects are associated with 10 peripheral receptors and 8 neurotransmitters (94).
5.3 Advantages and limitations of the study
This systematic review is the first to focus on the advantages of different acupuncture treatment plans to broaden the selection of feasible treatment options in clinical practice. The advantages of different acupuncture treatments are different. There are currently no studies comparing the effectiveness of various types of acupuncture for post-stroke SHS directly or indirectly. Our network meta-analysis includes a large number of studies, integrating various acupuncture intervention methods and comparing the improvement of different acupuncture therapies for post-stroke SHS based on VAS, Fugl–Meyer, Barthel, and SHSS scales. The aim is to provide more comprehensive clinical practice references for acupuncture treatment for post-stroke SHS.
However, there are also several limitations. Since acupuncture is a traditional Chinese treatment method, its promotion in the world is still limited to some extent. The included studies are mainly from China and lack ethnic diversity. Therefore, research and exploration outside China are required to enhance clinical promotion and applicability. The multi-center studies included in our research are relatively few. To acquire more convincing evidence, future studies are desired to verify these results.
6 Conclusion
From the results, we found that the combination of acupuncture and rehabilitation is more effective in improving the overall effectiveness of post-stroke SHS than simple rehabilitation intervention, especially in relieving pain and improving motor function. Floating needle acupuncture and catgut embedding + rehabilitation show good performance in pain relief, but the sample size of floating needle acupuncture is small. Large sample sizes and high-quality studies are required for verification in the future. Most notably, other multi-needle acupuncture combinations and special needle operations and techniques all demonstrate good effects in pain relief and upper limb motor function recovery. This could be related to the inclusion of special needle operation and technique and the combination with the patient’s limb activity during the acupuncture treatment. For patients who fear rehabilitation exercise due to pain, these two acupuncture methods can be considered as the first options. Western medicine + acupuncture + traditional Chinese medicine is also effective in improving Fugl–Meyer, Barthel, and SHSS scores. However, since it is not reflected in the VAS scale, there is currently a lack of effective exploration of its pain relief effect. It is recommended that future research could supplement this gap.
In conclusion, multiple acupuncture treatments have significant effects in treating pain and improving upper limb motor function after a stroke, with fewer adverse events. Hence, acupuncture can be promoted as a treatment method. More high-quality, multi-center collaborative, large-sample studies are warranted to verify our results in future.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
TH: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Validation, Visualization, Writing – original draft. HY: Data curation, Funding acquisition, Investigation, Project administration, Supervision, Writing – review & editing. JH: Formal analysis, Investigation, Supervision, Writing – review & editing. NW: Conceptualization, Data curation, Formal analysis, Resources, Writing – review & editing. CZ: Data curation, Formal analysis, Investigation, Writing – review & editing. XH: Data curation, Investigation, Writing – review & editing. XT: Data curation, Investigation, Writing – review & editing. YaL: Data curation, Investigation, Writing – review & editing. YJ: Data curation, Investigation, Project administration, Writing – review & editing. XW: Data curation, Investigation, Project administration, Writing – review & editing. YY: Resources, Supervision, Writing – review & editing. YiL: Funding acquisition, Project administration, Resources, Supervision, Writing – review & editing. SY: Data curation, Investigation, Writing – review & editing. YM: Data curation, Investigation, Writing – review & editing. SL: Data curation, Investigation, Writing – review & editing. JZ: Data curation, Investigation, Writing – review & editing. YH: Conceptualization, Funding acquisition, Resources, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research was supported by the National Natural Science Foundation of China (NSFC): Study on the analgesic mechanism of NPP by Tui Na from the regulation of miR-342-3p/IER3 by LNCRNAH19 (No. 82160943) and the Innovation Project of Guangxi Graduate Education of GXUCM:P2X7/NLRP3-based regulation of cellular pyroptosis Exploring the analgesic mechanism of acupressure on neuropathic pain in rats analgesic mechanism in rats with neuropathic pain (No. YCBXJ2023002).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2023.1268626/full#supplementary-material
References
1. Sung, H, Ferlay, J, Siegel, RL, Laversanne, M, Soerjomataram, I, Jemal, A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2021) 71:209–49. doi: 10.3322/caac.21660
2. Pu, L, Wang, L, Zhang, R, Zhao, T, Jiang, Y, and Han, L. Projected global trends in ischemic stroke incidence, deaths and disability-adjusted life years from 2020 to 2030. Stroke. (2023) 54:1330–9. doi: 10.1161/strokeaha.122.040073
3. Kim, JY, Yoon, SY, Kim, J, Jeong, YH, and Kim, YW. Neural substrates for poststroke complex regional pain syndrome type I: a retrospective case-control study using voxel-based lesion symptom mapping analysis. Pain. (2020) 161:1311–20. doi: 10.1097/j.pain.0000000000001816
4. Zyluk, A, and Zyluk, B. Shoulder-hand syndrome in patients after stroke. Neurol Neurochir Pol. (1999) 33:131–42.
5. Wales, C, Matthews, LR, and Donelly, M. Medically unexplained chronic pain in Australia: difficulties for rehabilitation providers and workers in pain. Work. (2010) 36:167–79. doi: 10.3233/wor-2010-1018
6. Backonja, MM, and Serra, J. Pharmacologic management part 2: lesser-studied neuropathic pain diseases. Pain Med. (2004) 5:S48–59. doi: 10.1111/j.1526-4637.2004.04021.x
7. Lee, SK, Yang, DS, Lee, JW, and Choy, WS. Four treatment strategies for complex regional pain syndrome type 1. Orthopedics. (2012) 35:e834–42. doi: 10.3928/01477447-20120525-21
8. Iolascon, G, and Moretti, A. Pharmacotherapeutic options for complex regional pain syndrome. Expert Opin Pharmacother. (2019) 20:1377–86. doi: 10.1080/14656566.2019.1612367
9. Samen, CDK, Sutton, OM, Rice, AE, Zaidi, MA, Siddarthan, IJ, Crimmel, SD, et al. Correlation between temperature rise after sympathetic block and pain relief in patients with complex regional pain syndrome. Pain Med. (2022) 23:1679–89. doi: 10.1093/pm/pnac035
10. Wan, R, Fan, Y, Zhao, A, Xing, Y, Huang, X, Zhou, L, et al. Comparison of efficacy of acupuncture-related therapy in the treatment of rheumatoid arthritis: a network meta-analysis of randomized controlled trials. Front Immunol. (2022) 13:829409. doi: 10.3389/fimmu.2022.829409
11. Feng, Z, Cui, S, Yang, H, Wang, Y, Zhou, X, Wong, J, et al. Acupuncture for neuropathic pain: a meta-analysis of randomized control trials. Front Neurol. (2022) 13:1076993. doi: 10.3389/fneur.2022.1076993
12. Birch, S, and Robinson, N. Acupuncture as a post-stroke treatment option: a narrative review of clinical guideline recommendations. Phytomedicine. (2022) 104:154297. doi: 10.1016/j.phymed.2022.154297
13. Prosperity, L. Acupuncture and moxibustion (seven-year planning textbook forhigher Chinese medicine schools in the new century). China Traditional Chinese Medicine Press (2012). 165p,176p,180p and 186p.
14. Neurology CMA. The 2016 edition of the Chinese cerebrovascular disease diagnosis and consensus, vol. 106 People’s Medical Publishing House (2016). 150 p.
15. Hongshi, L, and Pulian, Z. Rehabilitation assessment and treatment of stroke. Huaxia Publishing House (1996) 149–150. 60p and 83p.
16. Hutton, B, Salanti, G, Caldwell, DM, Chaimani, A, Schmid, CH, Cameron, C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. (2015) 162:777–84. doi: 10.7326/m14-2385
17. Higgins, JPT, Savović, J, Page, MJ, Elbers, RG, and Sterne, JAC. Chapter 8: assessing risk of bias in a randomized trial In: JPT Higgins, J Thomas, J Chandler, M Cumpston, T Li, and MJ Page, et al., editors. Cochrane handbook for systematic reviews of interventions version 6.1 (updated September 2020) : The Cochrane Collaboration (2020)
18. Yin, W, Tao, Y, Yufeng, G, Yuanshi, L, Baojuan, G, Wentai, X, et al. Observation on therapeutic effects of different acupoint selection methods combined with systematical rehabilitation on shoulder-hand syndrome after apoplexy. Chin Acupunct Moxibust. (2002) 2:12–4. doi: 10.13703/j.0255-2930.2002.02.005
19. Yongqiang, H, Tieming, M, Yunfa, X, and Lei, W. Immediate effect study and FMRI study of electroacupuncture on scalp acupuncture treatment of shoulder-hand syndrome after stroke. Chin Arch Tradit Chin Med. (2022) 40:161–4. doi: 10.13193/j.issn.1673-7717.2022.01.038
20. Xinru, L, Desong, Z, Xiaoguang, W, and Xinhong, X. Clinical observation on warm acupuncture and moxibustion for trigger points in patients with stage I shoulder-hand syndrome after stroke. China J Tradit Chin Med Pharm. (2021) 36:5671–3.
21. Juan, Y, Quan, D, and Nenggui, X. Curative effect observation of fire needle on post-stroke shoulder-hand syndrome in early stage. China J Tradit Chin Med Pharm. (2011) 26:967–71.
22. Qin, X, Lixing, Z, Jun, H, and Dexiong, H. Effects of Jin’s three-needle acupuncture therapy combined with rehabilitation training in patients with shoulder-hand syndrome after stroke. Chin J Rehabil Med. (2011) 26:720–3. doi: 10.3969/j.issn.1001-1242.2011.08.006
23. Xiaoqiong, H, Yanjie, L, Hewei, Q, Kun, R, Shuchen, Z, and Haoyuan, L. Clinical study on treatment of qi deficiency and blood stasis syndrome of shoulder-hand syndrome after stroke with wax-mud Moxibustion. J Beijing Univ Tradit Chin Med. (2022) 45:738–44. doi: 10.3969/j.issn.1006-2157.2022.07.015
24. Liang, Z, Genying, Z, Tongcai, T, Junjie, S, and Xiangming, Y. Effects of acupuncture from Tiaokou to Chenshan and exercise on shoulder-hand syndrome at stage I after stroke. Chin J Rehabil Theory Pract. (2016) 22:95–7. doi: 10.3969/j.issn.1006-9771.2016.01.021
25. Feilin, N, Changping, C, Hui, X, Fengmei, Q, and Qun, H. Effect of warm-unblocking therapy using moving cupping and acupoints moxibustion in stroke patients with shoulder-hand syndrome. Chin J Integr West Med. (2021) 41:456–60. doi: 10.7661/j.cjim.20201008.189
26. Qingbo, J, and Pengqin, W. Clinical research on the treatment of shoulder hand syndrome after stroke by eye-acupuncture cooperated with ironing analgesia. J Basic Chin Med. (2016) 22:960–96. doi: 10.19945/j.cnki.issn.1006-3250.2016.07.035
27. Wenjun, N, Zhaoxia, D, Ping, A, Yuhua, W, Yanyun, L, Xiuhong, X, et al. Effect of silver needle with systematical rehabilitation on shoulder-hand syndrome after stroke. Chin J Rehabil Theory Pract. (2012) 18:107–10. doi: 10.3969/j.issn.1006-9771.2012.02.003
28. Yimo, F, and Sulan, M. Acupuncture combined with infrared acupoint irradiation and rehabilitation treatment of 126 cases of clinical observation on shoulder hand syndrome after stroke. Laser J. (2015) 36:195–7. doi: 10.14016/j.cnki.jgzz.2015.04.195
29. Xianping, H, and Zichao, W. Effect of acupuncture combined with rehabilitation exercise on Fugl–Meyer score and quality of life in patients with shoulder-hand syndrome after stroke. Chin Arch Tradit Chin Med. (2017) 35:2199–202. doi: 10.13193/j.issn.1673-7717.2017.08.077
30. Ranwei, L, Jun, G, Jin, D, Ying, Y, Shuang, L, Weihong, S, et al. Effect of the contralateral needling therapy on post-stroke shoulder-hand syndrome. Acupunct Res. (2020) 45:152–6. doi: 10.13702/j.1000-0607.190478
31. Lijuan, C, Yan, T, Wei, Z, Yuan, L, Hai, H, Qian, L, et al. Analysis of the clinical effect on post-stroke shoulder hand syndrome stage I treated with the along-meridian trochar acupuncture therapy. Acupunct Res. (2020) 45:657–61. doi: 10.13702/j.1000-0607.200164
32. Ronghua, Z, Mei, Y, Junlong, D, Xinhan, Z, Hui, B, Lei, S, et al. Treatment of stroke patients with shoulder-wrist syndrome by acupoint catgut embedding and surface electromyogram biofeedback therapy. Acupunct Res. (2018) 43:380–3. doi: 10.13702/j.1000-0607.170491
33. Xiongjie, C, Xiao, G, Xuexia, G, Yanli, X, and Shiqiu, D. Clinical efficacy on post-stroke shoulder-hand syndrome (stage 1) treated byelectro-acupuncture at dorsal root of auric Le. J Clin Acupunct Moxibust. (2015) 31:22–4. doi: 10.3969/j.issn.1005-0779.2015.08.009
34. Huang, Z, Pei, J, Wang, W, Song, Y, Han, Z, Song, Y, et al. Clinical observation of acupuncture plus medicine and function training for post-stroke shoulder-hand syndrome. Shanghai J Acupunct Moxibust. (2015) 34:511–4. doi: 10.13460/j.issn.1005-0957.2015.06.0511
35. Miaojun, L, Haofeng, G, Qiaoging, H, and Rundong, T. Clinical observation on the treatment of post-stroke shoulder-hand syndrome by Fuyang buried thread method. Shanghai J Acupunct Moxibust. (2016) 35:1162–5. doi: 10.13460/j.issn.1005-0957.2016.10.1162
36. Liwen, X, Qun, L, and Jingqing, S. Clinical observation on penetration needling combined with electroacupuncture for treatment of poststroke shoulder-hand syndrome. Chin Acupunct Moxibust. (2007) 7:491–3. doi: 10.13703/j.0255-2930.2007.07.007
37. Ruiqing, L, Yiying, W, Tingqin, M, Lihong, Z, Jianyun, Z, Jingwen, L, et al. Clinical observation on wrist-ankle acupuncture for shoulder-hand syndrome phase I after stroke. Chin Acupunct Moxibust. (2022) 42:721–5. doi: 10.13703/j.0255-2930.20210813-k0001
38. Yanjie, S, Chengcheng, M, Yuying, C, Dongsheng, W, and Lingli, K. Clinical study on acupuncture combined with rehabilitation therapy for treatment of Poststroke shoulder-hand syndrome. Chin Acupunct Moxibust. (2008) 5:331–3. doi: 10.13703/j.0255-2930.2008.05.017
39. Zhan, J, Ai, Y, Zhan, L, Pan, R, Wang, Y, Dong, C, et al. Effect of abdominal acupuncture combined with routine rehabilitation training on shoulder-hand syndrome after stroke: a randomized controlled trial. Integr Med Res. (2022) 11:100805. doi: 10.1016/j.imr.2021.100805
40. Fanying, M, and Jin, W. Effect of warm acupuncture stimulation of Waiguan (Te 5) on post-stroke shoulder-hand syndrome. Acupunct Res. (2014) 39:228–31. doi: 10.13702/j.1000-0607.2014.03.012
41. Tang, XL, and Pan, HY. Muscle regions of meridians warm needling method plus pricking Jing-well points for blood-letting in the treatment of shoulder-hand syndrome after stroke. J Acupunct Tuina Sci. (2021) 19:291–9. doi: 10.1007/s11726-021-1260-x
42. Jun, W, Xiao, C, Huanhuan, N, Chunshui, H, Cuiwen, Z, Ji, W, et al. The efficacy of floating stabbing combined with rehabilitation training for the treatment of shoulder pain in shoulder-hand syndrome after stroke. Chin Acupunct Moxibust. (2013) 33:294–8. doi: 10.13703/j.0255-2930.2013.04.005
43. Jinbiao, H, Pengjie, S, Yiqin, Y, Shouxiang, Y, and Zenghui, Y. Observation on therapeutic effect of opposing needling for treatment of poststroke shoulder-hand syndrome. Chin Acupunct Moxibust. (2009) 29:205–8. doi: 10.13703/j.0255-2930.2009.03.013
44. Zhang Qian, SX, Wenpeng, W, and Pengyu, Z. Observations on the efficacy of along-meridian distal point selection in treating post-cerebral infarction shoulder-hand syndrome. Shanghai J Acupunct Moxibust. (2015) 34:297–9. doi: 10.13460/j.issn.1005-0957.2015.04.0297
45. Bing, Y, Lixiong, W, Nenggui, X, Yongfeng, L, Zhuoxin, Y, Ling, W, et al. Observations on the efficacy of Jin’s three needles plus twelve Jing-well points in treating post-stroke shoulder-hand syndrome. Shanghai J Acupunct Moxibust. (2015) 34:605–8. doi: 10.13460/j.issn.1005-0957.2015.07.0605
46. Tongbo, J, Tongyan, M, and Bing, W. Observations on the efficacy of superficial needling plus external washing with Chinese herbal medicine in treating post-stroke shoulder-hand syndrome. Shanghai J Acupunct Moxibust. (2016) 35:789–91. doi: 10.13460/j.issn.1005-0957.2016.07.0789
47. Chunshui, H, Wenzhao, F, Ansheng, Y, Xiao, C, and Ji, W. Penetration acupuncture at Baxie(EX-UE 9) combined with rehabilitation for swelling hand of post-stroke shoulder-hand syndrome. Chin Acupunct Moxibust. (2017) 37:121–4. doi: 10.13703/j.0255-2930.2017.02.004
48. Zhaohui, Z, Lixing, Z, Zhenhu, C, Jianying, L, Yanhui, L, Ganghui, J, et al. Post-stroke shoulder-hand syndrome treated with floating-needle therapy combined with rehabilitation training: a randomized controlled trial. Chin Acupunct Moxibust. (2014) 34:636–40. doi: 10.13703/j.0255-2930.2014.07.006
49. Wenrong, W, Tianlei, W, Shaolu, C, Yinlong, Z, Wei, Z, Qiuyan, W, et al. Acupuncture combined with rehabilitation for post-stroke shoulder-hand syndrome: a randomized controlled study. Chin Acupunct Moxibust. (2013) 33:970–4. doi: 10.13703/j.0255-2930.2013.11.026
50. Bingfeng, X, Min, H, Xin, Z, Kaina, Z, Shengpeng, D, and Honghong, W. Short-term and long-term efficacy of PGLA thread-embedding therapy in treatment of stagei post-stroke shoulder-hand syndrome. Acupunct Res. (2019) 44:762–5. doi: 10.13702/j.1000-0607.180805
51. Ning, Li, and, Fengwei, Tian, Wang, Chengwei, Yu, Pengming, Zhou, Xi, and Wen, Qian, and,, et al. Therapeutic effect of acupuncture and massage for shoulder-hand syndrome in hemiplegia patients: a clinical two-center randomized controlled trial J Tradit Chin Med. (2012) 32:343–349, doi: 10.1016/S0254-6272(13)60035-7
52. Jingchun, Y, Guoping, Z, Guihua, Z, and Hongqiao, F. Therapeutic observation of acupuncture at the interiorly-exteriorly related meridians plus rehabilitation training for post-stroke shoulder-hand syndrome. Shanghai J Acupunct Moxibust. (2015) 34:7–10. doi: 10.13460/j.issn.1005-0957.2015.01.0007
53. Jingjun, X, and Jinxia, L. Therapeutic observation of electroacupuncture plus rehabilitation for post-stroke shoulder-hand syndrome. Shanghai J Acupunct Moxibust. (2016) 35:1423–5. doi: 10.13460/j.issn.1005-0957.2016.12.1423
54. Gao Sen, MX, Chunying, L, Jie, S, and Haikuo, Y. Wang Ju-Yi’s meridian diagnosis method combined with Bobath rehabilitation training for post-stroke shoulder-hand syndrome type I. Chin Acupunct Moxibust. (2022) 42:28–32. doi: 10.13703/j.0255-2930.20210202-k0011
55. Zhihong, Z, Yulei, W, Jian, L, and Jun, W. Effect of white tiger shaking head needling combined with rehabilitation training on pain and upper limb motor function in the treatment of Shsas. J Clin Acupunct Moxibust. (2021) 37:19–25. doi: 10.19917/j.cnki.1005-0779.021238
56. Xue-Ping, Y, Hong-Tao, C, and Hui-Hui, M. Therapeutic effect of Baihu Yaotou needling on post-stroke shoulder-hand syndrome. J Clin Acupunct Moxibust. (2017) 33:21–4. doi: 10.3969/j.issn.1005-0779.2017.02.007
57. Wang Shurong, LG. Application research of spoon needle acupressure combined with shoulder triple needling in treatment of post-stroke SHS. J Clin Acupunct Moxibust. (2022) 38:37–40. doi: 10.19917/j.cnki.1005-0779.022073
58. Mingming, W, Baoqiang, W, Shengzhao, C, and Xiang, T. Clinical observation of electro-acupuncture combined with medicated cake moxibustion treating post-stroke shoulder-hand syndrome of phase I. J Clin Acupunct Moxibust. (2018) 34:12–5. doi: 10.3969/j.issn.1005-0779.2018.02.004
59. Weidong, Y, and Yanjie, M. Therapeutic observation of electroacupuncture plus mirror therapy for shoulder-hand syndrome stage I after cerebral stroke. Shanghai J Acupunct Moxibust. (2019) 38:492–6. doi: 10.13460/j.issn.1005-0957.2019.05.0492
60. Yang, W, Yuju, Y, Zhongmei, D, Naihao, H, Fan, Y, and Jiu, L. Efficacy observation of surrounding electro-acupuncture combined with Tcm fumigation on post-stroke shoulder-hand syndrome. J Clin Acupunct Moxibust. (2019) 35:32–5. doi: 10.3969/j.issn.1005-0779.2019.07.010
61. Shengsan, H, and Shiyi, G. Evaluation of abdominal acupuncture and rehabilitation treatment for shoulder-hand syndrome (period I) after stroke. J Clin Acupunct Moxibust. (2016) 32:11–3. doi: 10.19917/j.cnki.1005-0779.2016.09.004
62. Changjin, H, Yingjie, H, and Yanhua, W. Clinical observations on fire needle acupuncture at muscular attachments for the treatment of post-stroke shoulder-hand syndrome. Shanghai J Acupunct Moxibust. (2013) 32:627–9. doi: 10.3969/j.issn.1005-0957.2013.08.627
63. Youhua, Z, Yehua, B, Fang, G, Min, Z, and Yina, W. Clinical observation of Ling Gui Ba Fa for post-stroke shoulder-hand syndrome stage I. Shanghai J Acupunct Moxibust. (2019) 38:1326–9. doi: 10.13460/j.issn.1005-0957.2019.12.1326
64. Ting, Z, Jieyu, W, and Yaoxiang, M. Clinical effects of balanced acupuncture combined with Bobath therapy on post-stroke shoulder-hand syndrome. J Clin Acupunct Moxibust. (2019) 35:23–6.
65. Fei, H. Clinical study of thumb-tack needling combined with electro-acupuncture and rehabilitation treating post-stoke shoulder-hand syndrome. J Clin Acupunct Moxibust. (2018) 34:25–8. doi: 10.3969/j.issn.1005-0779.2018.10.008
66. Guoqi, C, Haiyan, Z, Xinyi, W, and Liming, Y. Clinical observation of point-to-point scalp acupuncture combined with body acupuncture in the treatment of shoulder-hand syndrome after stroke. J Clin Acupunct Moxibust. (2018) 34:29–31.
67. Xin, T, Dandan, L, Yan, W, and Yujue, W. Therapeutic observation of early-stage shoulder-hand syndrome after ischemic stroke treated with acupuncture at distal points plus exercise. Shanghai J Acupunct Moxibust. (2014) 33:607–9. doi: 10.13460/j.issn.1005-0957.2014.07.0607
68. Leem, J, Kim, H, Jo, HG, Jeon, SR, Hong, Y, Park, Y, et al. Efficacy and safety of thread embedding acupuncture combined with conventional acupuncture for chronic low Back pain: a study protocol for a randomized, controlled, Assessor-blinded, multicenter clinical trial. Medicine. (2018) 97:e10790. doi: 10.1097/md.0000000000010790
69. Wei, X, He, L, Liu, J, Ai, Y, Liu, Y, Yang, Y, et al. Electroacupuncture for reflex sympathetic dystrophy after stroke: a meta-analysis. J Stroke Cerebrovasc Dis. (2019) 28:1388–99. doi: 10.1016/j.jstrokecerebrovasdis.2019.02.010
70. Lei, S, Dai, F, Xue, F, Hu, G, Zhang, Y, Xu, X, et al. Acupuncture for shoulder-hand syndrome after stroke: an overview of systematic reviews. Medicine. (2022) 101:e31847. doi: 10.1097/md.0000000000031847
71. Liu, S, Zhang, CS, Cai, Y, Guo, X, Zhang, AL, Xue, CC, et al. Acupuncture for post-stroke shoulder-hand syndrome: a systematic review and meta-analysis. Front Neurol. (2019) 10:433. doi: 10.3389/fneur.2019.00433
72. Peng, L, Zhang, C, Zhou, L, Zuo, HX, He, XK, and Niu, YM. Traditional manual acupuncture combined with rehabilitation therapy for shoulder hand syndrome after stroke within the Chinese healthcare system: a systematic review and meta-analysis. Clin Rehabil. (2018) 32:429–39. doi: 10.1177/0269215517729528
73. Wang, RQ, Wu, QZ, Huang, CH, and Rao, WF. Network meta-analysis of 4 acupuncture therapies for shoulder hand syndrome after stroke. Zhongguo Zhen Jiu. (2021) 41:563–9. doi: 10.13703/j.0255-2930.20200325-k0011
74. Topcuoglu, A, Gokkaya, NK, Ucan, H, and Karakuş, D. The effect of upper-extremity aerobic exercise on complex regional pain syndrome type I: a randomized controlled study on subacute stroke. Top Stroke Rehabil. (2015) 22:253–61. doi: 10.1179/1074935714z.0000000025
75. Smart, KM, Wand, BM, and O’Connell, NE. Physiotherapy for pain and disability in adults with complex regional pain syndrome (Crps) types I and ii. Cochrane Database Syst Rev. (2016) 2:CD010853. doi: 10.1002/14651858.CD010853.pub2
76. Feng, S, Tang, M, Huang, G, Wang, J, He, S, Liu, D, et al. Emg biofeedback combined with rehabilitation training may be the best physical therapy for improving upper limb motor function and relieving pain in patients with the post-stroke shoulder-hand syndrome: a Bayesian network meta-analysis. Front Neurol. (2022) 13:1056156. doi: 10.3389/fneur.2022.1056156
77. Chauvineau, V, Codine, P, Hérisson, C, Pellas, F, and Pélissier, J. What is the place of diphosphonates in the treatment of complex regional pain syndrome I? Ann Readapt Med Phys. (2005) 48:150–7. doi: 10.1016/j.annrmp.2004.11.004
78. Berthelot, JM. Current management of reflex sympathetic dystrophy syndrome (complex regional pain syndrome type I). Joint Bone Spine. (2006) 73:495–9. doi: 10.1016/j.jbspin.2005.11.022
79. Sendrasoa, FA, Ranaivo, IM, Raherivelo, AJ, Rapelanoro Rabenja, F, and Ramarozatovo, LS. Adverse effects of long-term oral corticosteroids in the Department of Dermatology, Antananarivo, Madagascar. Clin Cosmet Investig Dermatol. (2021) 14:1337–41. doi: 10.2147/ccid.S332201
80. Kalita, J, Misra, U, Kumar, A, and Bhoi, SK. Long-term prednisolone in post-stroke complex regional pain syndrome. Pain Physician. (2016) 19:565–74. doi: 10.36076/ppj/2016.19.565
81. Corrado, A, Santoro, N, and Cantatore, FP. Extra-skeletal effects of bisphosphonates. Joint Bone Spine. (2007) 74:32–8. doi: 10.1016/j.jbspin.2006.06.005
82. Santamato, A, Ranieri, M, Panza, F, Solfrizzi, V, Frisardi, V, Stolfa, I, et al. Role of biphosphonates and lymphatic drainage type Leduc in the complex regional pain syndrome (shoulder-hand syndrome). Pain Med. (2009) 10:179–85. doi: 10.1111/j.1526-4637.2008.00539.x
83. Matayoshi, S, Shimodozono, M, Hirata, Y, Ueda, T, Horio, S, and Kawahira, K. Use of calcitonin to prevent complex regional pain syndrome type I in severe hemiplegic patients after stroke. Disabil Rehabil. (2009) 31:1773–9. doi: 10.1080/09638280902795573
84. Cruccu, G, Aziz, TZ, Garcia-Larrea, L, Hansson, P, Jensen, TS, Lefaucheur, JP, et al. Efns guidelines on neurostimulation therapy for neuropathic pain. Eur J Neurol. (2007) 14:952–70. doi: 10.1111/j.1468-1331.2007.01916.x
85. Taskaynatan, MA, Ozgul, A, Tan, AK, Dincer, K, and Kalyon, TA. Bier block with methylprednisolone and lidocaine in CRPS type I: a randomized, double-blinded, placebo-controlled study. Reg Anesth Pain Med. (2004) 29:408–12. doi: 10.1016/j.rapm.2004.05.007
86. Han, KR, Kim, C, Chae, YJ, and Kim, DW. Efficacy and safety of high concentration lidocaine for trigeminal nerve block in patients with trigeminal neuralgia. Int J Clin Pract. (2008) 62:248–54. doi: 10.1111/j.1742-1241.2007.01568.x
87. Kanaan, T, Abusaleh, R, Abuasbeh, J, Al Jammal, M, Al-Haded, S, Al-Rafaiah, S, et al. The efficacy of therapeutic selective nerve block in treating lumbar radiculopathy and avoiding surgery. J Pain Res. (2020) 13:2971–8. doi: 10.2147/jpr.S276331
88. Albayrak, I, Apiliogullari, S, Onal, O, Gungor, C, Saltali, A, and Levendoglu, F. Pulsed radiofrequency applied to the dorsal root ganglia for treatment of post-stroke complex regional pain syndrome: a case series. J Clin Anesth. (2016) 33:192–7. doi: 10.1016/j.jclinane.2016.03.059
89. Rowbotham, MC, and Wallace, M. Evolution of analgesic tolerance and opioid-induced hyperalgesia over 6 months: double-blind randomized trial incorporating experimental pain models. J Pain. (2020) 21:1031–46. doi: 10.1016/j.jpain.2020.01.005
90. NIN Consensus Development Panel on Acupuncture. Acupuncture. JAMA. (1998) 280:1518–24. doi: 10.1001/jama.280.17.1518
91. Belskaya, GN, Stepanova, SB, Makarova, LD, Sergienko, DA, Krylova, LG, and Antimonova, KV. Acupuncture in the prevention and treatment of stroke: a review of foreign studies. Vopr Kurortol Fizioter Lech Fiz Kult. (2020) 97:68–77. doi: 10.17116/kurort20209702168
92. Dou, B, Li, Y, Ma, J, Xu, Z, Fan, W, Tian, L, et al. Role of neuroimmune crosstalk in mediating the anti-inflammatory and analgesic effects of acupuncture on inflammatory pain. Front Neurosci. (2021) 15:695670. doi: 10.3389/fnins.2021.695670
93. Wang, Y, Hackel, D, Peng, F, and Rittner, HL. Long-term antinociception by electroacupuncture is mediated via peripheral opioid receptors in free-moving rats with inflammatory hyperalgesia. Eur J Pain. (2013) 17:1447–57. doi: 10.1002/j.1532-2149.2013.00325.x
Keywords: acupuncture, post-stroke shoulder-hand syndrome, pain relief, systematic review, Bayesian network meta-analysis
Citation: Huang T, Yao H, Huang J, Wang N, Zhou C, Huang X, Tan X, Li Y, Jie Y, Wang X, Yang Y, Liang Y, Yue S, Mao Y, Lai S, Zheng J and He Y (2023) Effectiveness of acupuncture for pain relief in shoulder-hand syndrome after stroke: a systematic evaluation and Bayesian network meta-analysis. Front. Neurol. 14:1268626. doi: 10.3389/fneur.2023.1268626
Edited by:
Massimiliano Valeriani, Bambino Gesù Children’s Hospital (IRCCS), ItalyReviewed by:
Mostafa Meshref, Al-Azhar University, EgyptLeonardo Pellicciari, IRCCS Institute of Neurological Sciences of Bologna (ISNB), Italy
Copyright © 2023 Huang, Yao, Huang, Wang, Zhou, Huang, Tan, Li, Jie, Wang, Yang, Liang, Yue, Mao, Lai, Zheng and He. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yufeng He, aGV5ZkBneHRjbXUuZWR1LmNu
†These authors have contributed equally to this work
 Ting Huang
Ting Huang Hongfang Yao2†
Hongfang Yao2†