- College of Korean Medicine, Dongguk University, Seoul, Republic of Korea
Chronic neck pain is a leading health issue affecting a significant proportion of the global population. Multiple treatment options for chronic neck pain include anti-inflammatory drugs and analgesics. Acupuncture has been widely used for the treatment of chronic pain. In this study, we aimed to determine the efficacy of acupuncture for female patients with chronic neck pain. Twenty-three participants were enrolled in the study, and participants waited 4 weeks without acupuncture treatment and then received 4 weeks of treatment. One-way ANOVA with repeated measures was used to determine differences in the visual analogue scale (VAS), neck disability index (NDI), and substance P (SP) over time. The subjects’ pain intensity and degree of disability due to neck pain were measured as primary outcomes. SP in the blood was also analyzed as a secondary outcome. There was no significant difference between the VAS score and NDI value of baseline and after 4 weeks waiting. However, there was an improvement in both VAS and NDI after 4 weeks treatment. SP level was decreased after 4 weeks treatment. We could conclude that acupuncture is effective in alleviating chronic neck pain. Moreover, our findings revealed the efficacy of acupuncture on chronic pain with potential underlying biological mechanisms.
1. Introduction
Neck pain is a highly prevalent musculoskeletal disorder affecting individuals, families and healthcare systems of countries with substantial economic burdens. The Global Burden of Disease Study between 1990 and 2017 studied trends and prevalence of neck pain, and neck pain was reported as a serious public health problem, still affecting a significant proportion of the global population (1, 2). Popular analgesics such as non-steroidal anti-inflammatory drugs, acetaminophen, and cyclooxygenase 2 inhibitors relieve pain by suppressing the inflammatory process and have been commonly used as pharmacological interventions for musculoskeletal diseases, including neck pain (3, 4).
There are also non-pharmacological treatments such as physiotherapy, manual treatment, and massage therapy (5–7). Acupuncture has been gaining increasing interest for its favorable clinical outcomes in various chronic pains (8–10). Studies have shown a significant improvement in the visual analogue scale (VAS) score in subjects with acute or chronic musculoskeletal diseases such as low back pain after receiving acupuncture treatments (11–13). Nevertheless, there are still controversies over the clinical mechanisms by which insertion and stimulation by needles alleviate chronic pain.
Substance P (SP) is a mediator involved in various physiological processes, such as neuroinflammation and pain transmission (14, 15). It is broadly distributed in both the central and peripheral nervous system, and some studies have reported control of diseases, such as inflammatory muscle pain, cancer, and colitis, by mediating SP levels in animal models (16, 17). It has been hypothesized that neurological stimulation by needles at acupoints would cause physiological changes, mediating SP in serum (18).
The effect of acupuncture on chronic neck pain and its underlying mechanism is not well explored. In this study, we aimed to investigate the effect of acupuncture on chronic neck pain with different measurements and to further examine the potential biological connection between pain and SP level.
2. Methods
2.1. Study participants
Participant recruitment was performed through advertisement using local flyers in Goyang City, Gyeonggi-do and Seoul City, South Korea, from April 2018 to February 2019. A pre-screening survey was conducted on volunteered participants by assessing numeric pain scale (0–10 points), current medication, and questionnaires based on inclusion and exclusion criteria. Eligible participants were women aged between 40 to 60 years having neck pain for more than 12 weeks (VAS score ≥30.0 mm) (19). The inclusion criteria for participation were the absence of radiating pain and medication or other pain-related treatments. The exclusion criteria were pregnancy, spondylolisthesis, spondylitis, and infectious diseases, potentially affecting the treatment outcome.
2.2. Ethical approval and consent
Ethical approval for this study was obtained from the Institutional Review Board of Kyonggi University (KGU-20171222-HR-026). This study was registered with the Korean Clinical Trial Registry and WHO Clinical Trial Registry (KCT0005363, registered April 3rd, 2018, https://cris.nih.go.kr/cris/en/). The study procedures and potential risks were explained to each participant, and written informed consent was obtained prior to the study enrollment.
2.3. Study procedures
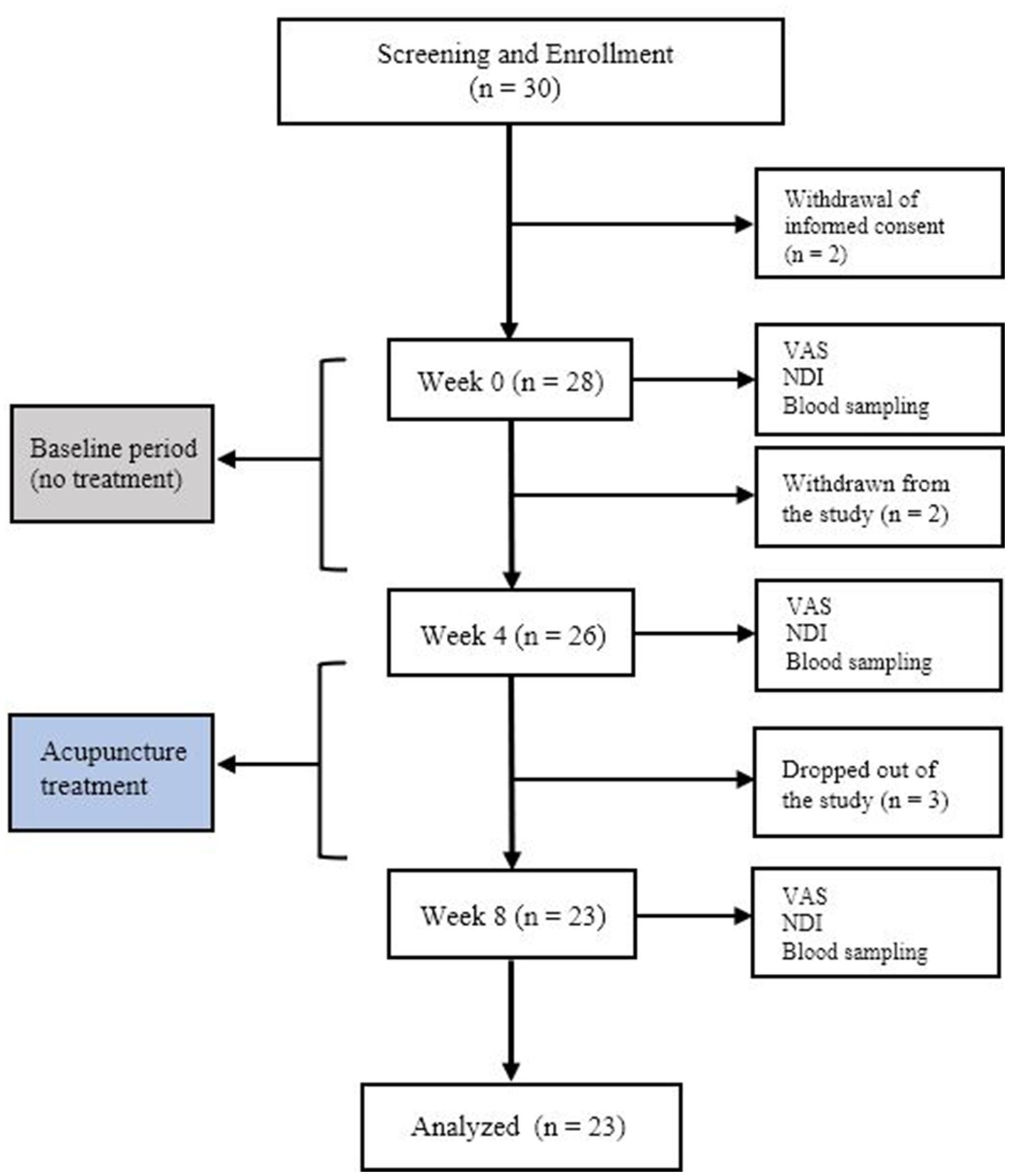
We primarily screened 29 participants to be enrolled in the study. After the first blood sampling (20), two participants dropped out due to perceived discomfort in blood sampling. Four participants withdrew from the study due to not being able to comply with the treatment schedule. Twenty-three subjects were ultimately included in the study and the further outcome analysis (Figure 1). All the outcome measures were assessed by an independent investigator. The investigator was also blinded to the treatment procedure and each patient’s treatment.
2.4. Acupuncture protocol
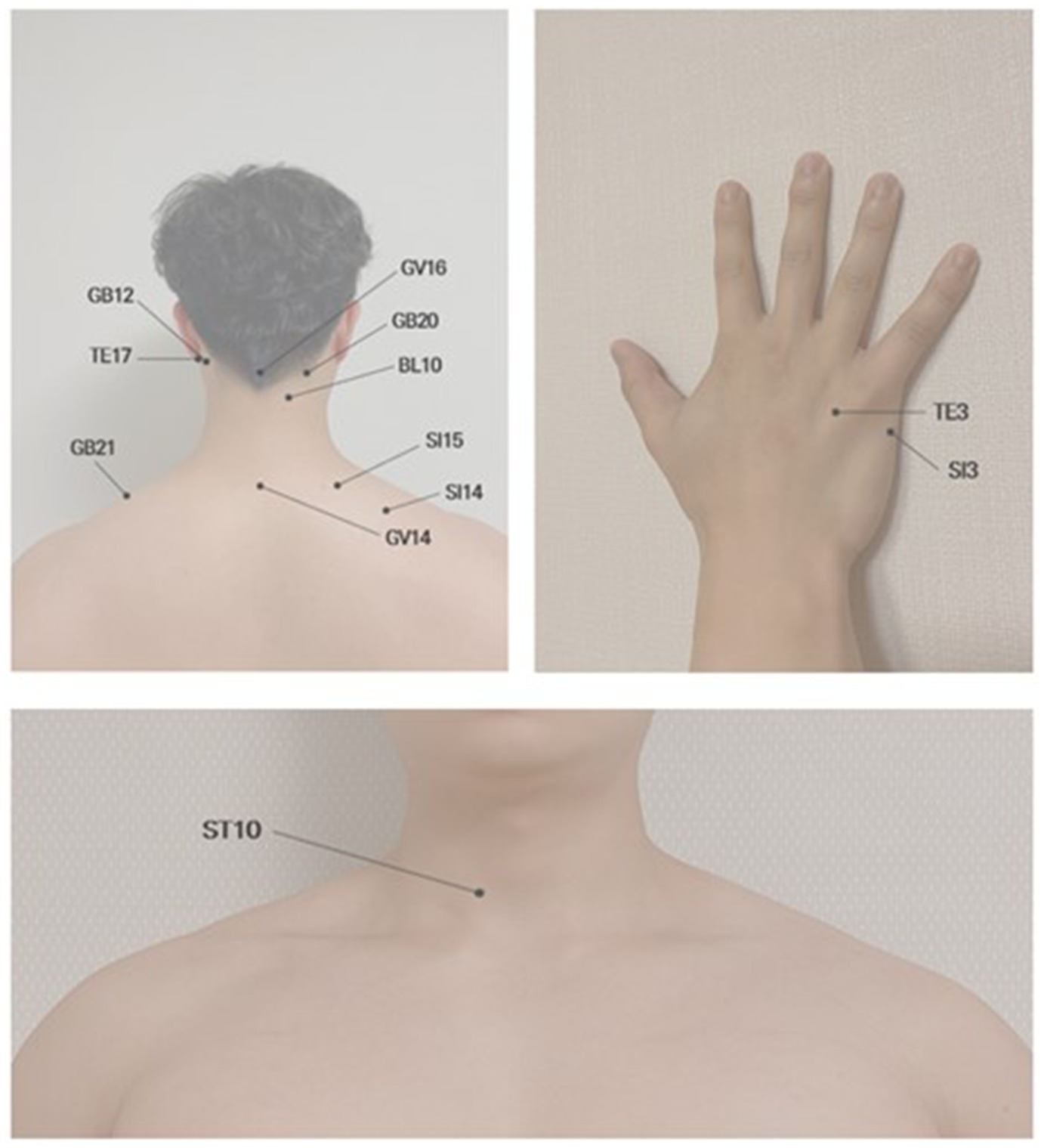
All the subjects received acupuncture treatment at two proximal acupoints (GV14 and GV16) and ten acupoints (BL10, GB20, GB12, GB21, TE3, TE17, ST10, SI3, SI14, and SI15), which are bilaterally symmetric. Acupoints were located near the head, cervical vertebrae, neck and shoulder (Figure 2). The practitioner used disposable sterile needles (0.25 × 0.30 mm) and inserted the needles to a depth of 10–20 mm using a guide tube. The needles remained in the acupoints for 15 min, and each treatment session took approximately 20 min, with relaxation time before and after each treatment. A licensed oriental medicine doctor performed all the acupuncture treatments.
2.5. Primary outcome measures
2.5.1. Visual analogue scale
Neck pain intensity was evaluated using VAS. Patients marked the point on a 10 cm horizontal line that best estimated their intensity of pain. The left end (0.0 cm) represented “no pain,” and the right end (10.0 cm) represented “extreme pain” (21). The measurements from the left end of the scale to the patients’ marks were recorded in centimeters and analyzed as their pain intensity.
2.5.2. Neck disability index
Neck pain-related disability was assessed by the Korean version of NDI to determine patients’ perceived pain levels and degree of interference with daily activities (22). The NDI questionnaire covers ten items: pain intensity, personal care, lifting, reading, headaches, concentration, work, driving, sleeping, and recreation. Each item is scored on a 0 (no disability) to 5 (full disability) scale with a maximum total score of 50 points or 100% (23). If a subject responded that they do not drive, we recorded the NDI out of 45 and converted the score to a percentage.
The VAS and NDI measures were completed by each subject before the 4 weeks waiting (baseline), after the 4 weeks waiting (week 4), and after the 4 weeks treatment (week 8).
2.6. Secondary outcome measures
Blood sampling was conducted at three different time points (baseline, week 4, and week 8). The blood from each subject was collected into anticoagulant (EDTA)-treated tubes and prepared by centrifuging the whole blood at 3000 RPM for 15 min at 4°C. Plasma was then transferred into a new microtube and stored at −80°C until analysis. Serum SP levels were measured by enzyme-linked immunosorbent assay (ELISA) (KGE007, R&D, United States) and multimode plate reader (VICTOR Nivo, PerkinElmer, United States).
2.7. Statistical analysis
All data were analyzed using SPSS version 24.0 (IBM SPSS Statistics, Armonk, NY, United States). Statistical significance was set at p < 0.05 for all analyses. An independent t-test or chi-square test was performed to compare all variables at baseline between groups. One-way ANOVA with repeated measures at three different time points as main factors were used to test whether pain level significantly differed from baseline in VAS, NDI, and serum SP levels. When a group-by-time interaction was significant, the significance of the difference from baseline was tested by paired t-test in each group. The Greenhouse–Geisser correction was applied upon violating the assumption of Mauchly’s test of sphericity.
3. Results
3.1. Baseline characteristics
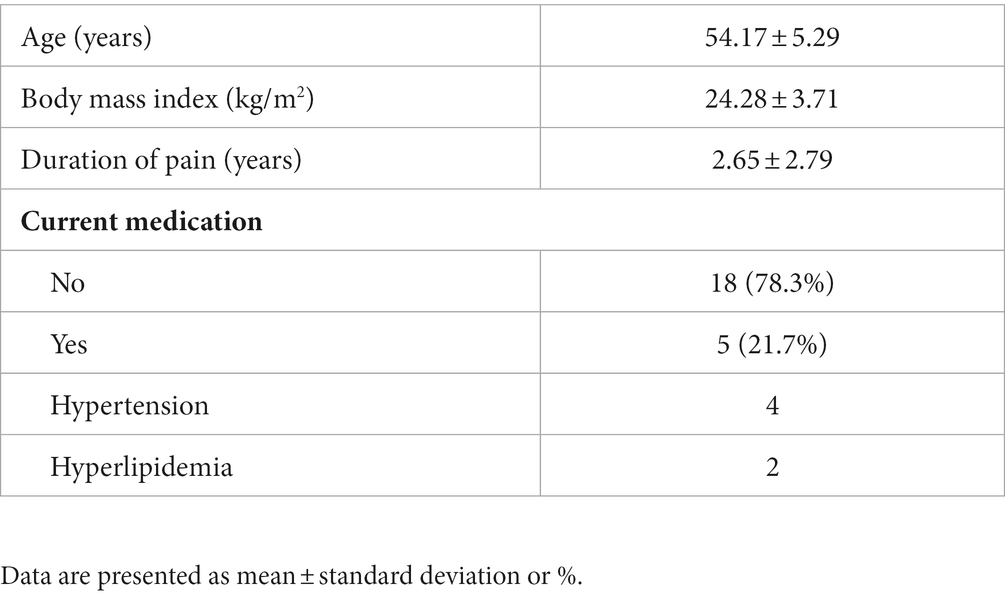
Baseline characteristics of the subjects, including age, body mass index (BMI), current medication, and duration of neck pain, are displayed in Table 1. The average age of the subjects (n = 23) was 54.17, and the average BMI was 24.28. Duration of neck pain was less than 3 years for all the subjects, with a mean of 2.65 years. Eighteen subjects (78.3%) were not on any medications, and the types of medication that five subjects (21.7%) had been taking were hypertension and hyperlipidemia medicine.
3.2. Primary outcomes
Pain intensity measured using VAS showed no significant differences between measurement values at baseline and week 4 (p = 0.102). There was also no significant difference between the baseline NDI score and the score after 4 weeks-waiting (p = 0.618). According to the test of within-subjects effect for VAS result, a significant improvement in pain was observed after 4 weeks-treatment compared to the value after 4 weeks-waiting (p < 0.001). In addition, there was also a significant difference in NDI score between the score measured after 4 weeks-waiting and after 4 weeks-treatment (p < 0.001) (Figures 3A,B).
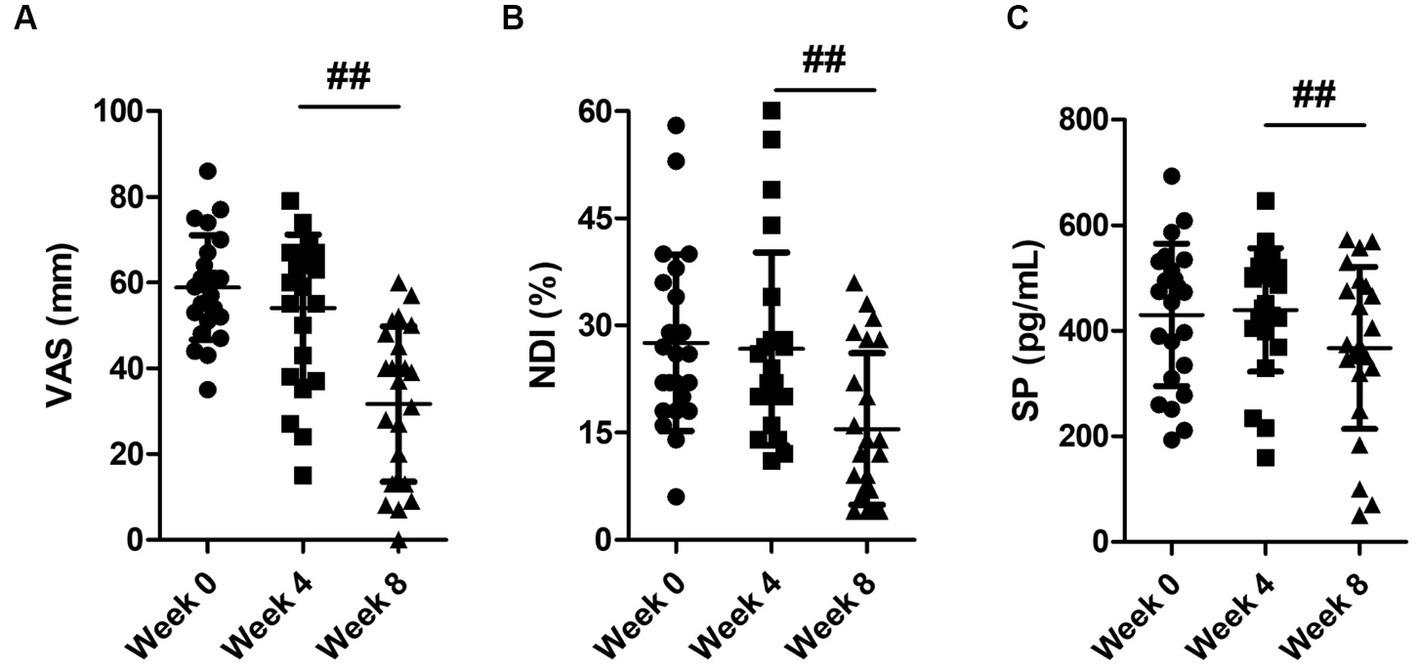
Figure 3. Changes in (A) visual analogue scale (VAS), (B) neck disability index (NDI), and (C) substance P (SP) level. Data are presented as mean ± standard deviation. The significance of the within-subject factor (time) was tested by one-way ANOVA with repeated measures. ##p < 0.001: week 4 vs. week 8.
3.3. Secondary outcome
The results of one-way ANOVA with repeated measures showed no significantly different changes in SP between baseline value and after the 4 weeks-waiting (p = 0.736). However, there was a significant change in SP value after 4 weeks-treatment compared to the value examined prior to the treatments (p < 0.05) (Figure 3C).
4. Discussion
We observed efficacy of acupuncture on chronic neck pain by assessing perceived pain and changes of SP level in serum. There was no significant difference in the comparison of VAS score at baseline vs. after 4 weeks-waiting. After 4 weeks-acupuncture intervention on the subjects with chronic neck pain, there was significant alleviation in pain intensity as VAS decreased from 53.96 mm to 31.65 mm. Subjects also reported that their overall disability level in daily life had diminished after treatments (15.46 ± 10.65) compared to before treatments (26.69 ± 13.45). For pain assessment, patient-reported outcome measures have been widely applied in clinical trials. By self-evaluating pain intensity, patients can subjectively detect their pain over time (24). Our primary outcome data obtained from VAS and NDI also shows how effectively acupuncture improved pain in patients with chronic neck pain.
A growing number of studies demonstrate reliable evidence of the effect of acupuncture on various diseases despite ongoing controversies over acupuncture treatment. Several studies examined the effect of acupuncture treatment on different types of pain. Acupuncture treatment significantly decreased VAS score in Whiplash patients compared to the no-treatment control group (25). In our study, the VAS and NDI were decreased by an average of −22.31 mm and −11.24%, respectively, after 4 weeks of acupuncture intervention. According to the results we obtain from two different self-evaluations, the pain-relief effect of acupuncture on acute pain is also evident in chronic neck pain.
In previous pain-related research, a multitude of biomarkers have been studied to understand complex neurobiological mechanisms of pain. SP is an undecapeptide belonging to the tachykinin peptide family. It is widely distributed in the central and peripheral nervous systems and released upon nociceptive stimulation. SP is involved in numerous neuronal signaling pathways and plays a pivotal role as a neurotransmitter and a neuromodulator (26, 27). However, the effect of acupuncture on SP has not been well understood in patients with chronic neck pain. Inflammatory biomarkers often reflect the degree of inflammation. We explored the change in SP level to objectively measure pain and make a reliable connection between pain modulation and acupuncture treatment for chronic neck pain. The painful perception can occur by various factor, which means it could stimulate different neural pathways. Interestingly, in this study, SP levels significantly decreased after acupuncture intervention in subjects with chronic neck pain, whereas there was no significant difference in SP levels between baseline and week 4. Based on both primary and secondary outcomes, a correlation between the effect of acupuncture and changes in SP levels can be suggested. However, there were limited subjects and healthy comparison group to further suggest more concrete underlying mechanism. We still need to further investigate how acupuncture played a regulatory role in central sensitization which led to SP level changes and also identify whether SP level is directly or indirectly involved in potential therapeutic mechanisms of acupuncture such as segmental inhibition, release of endogenous opioid, and adrenergic and 5 HT pathway.
This study assessed the impact of acupuncture treatment chronic neck pain in a single group over time. It allowed us to minimize subjects’ variation and to compare pain modulation. Although more studies with larger sample sizes and the inclusion of a healthy control group are expected to provide more reliable evidence of the effect of acupuncture on pain regulation in general, our findings suggested the beneficial effect of acupuncture on chronic neck pain and potential pain relief mechanism.
5. Conclusion
The present study suggests that acupuncture alleviates chronic neck pain by managing pain intensity and improving neck pain-induced disabilities in daily life. However, it is still necessary to further investigate the biological mechanism underlying the role of acupuncture in pain relief based on the secondary outcome of this study.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Institutional Review Board of Kyonggi University (KGU-20171222-HR-026). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
JK: Investigation, Writing – original draft. S-NK: Conceptualization, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the National Research Foundation of Korea, funded by the Korean Government (MSIT) (NRF-2020R1C1C1004107) the Korea Institute of Oriental Medicine (Grant K18182) and from the Ministry of Health & Welfare through the Korea Health Industry Development Institute (KHIDI) (Grant No. HF21C0018).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Safiri, S, Kolahi, AA, Hoy, D, Buchbinder, R, Mansournia, MA, Bettampadi, D, et al. Global, regional, and national burden of neck pain in the general population, 1990-2017: systematic analysis of the Global Burden of Disease Study 2017. BMJ. (2020) 368:m791. doi: 10.1136/bmj.m791
2. Mokdad, AH, Ballestros, K, Echko, M, Glenn, S, Olsen, HE, Mullany, E, et al. The state of US health, 1990–2016: burden of diseases, injuries, and risk factors among US states. JAMA. (2018) 319:1444–72. doi: 10.1001/jama.2018.0158
3. Huang, JF, Meng, Z, Zheng, XQ, Qin, Z, Sun, XL, Zhang, K, et al. Real-world evidence in prescription medication use among U.S.adults with neck pain. Pain Ther. (2020) 9:637–55. doi: 10.1007/s40122-020-00193-1
4. Saragiotto, BT, Machado, GC, Ferreira, ML, Pinheiro, MB, Abdel Shaheed, C, and Maher, CG. Paracetamol for low back pain. Cochrane Database Syst Rev. (2016) 2019:Cd012230. doi: 10.1002/14651858.Cd012230
5. Damgaard, P, Bartels, EM, Ris, I, Christensen, R, and Juul-Kristensen, B. Evidence of physiotherapy interventions for patients with chronic neck pain: a systematic review of randomised controlled trials. ISRN Pain. (2013) 2013:567175:1–23. doi: 10.1155/2013/567175
6. Miller, J, Gross, A, D'Sylva, J, Burnie, SJ, Goldsmith, CH, Graham, N, et al. Manual therapy and exercise for neck pain: a systematic review. Man Ther. (2010) 15:334–54. doi: 10.1016/j.math.2010.02.007
7. Sherman, KJ, Cherkin, DC, Hawkes, RJ, Miglioretti, DL, and Deyo, RA. Randomized trial of therapeutic massage for chronic neck pain. Clin J Pain. (2009) 25:233–8. doi: 10.1097/AJP.0b013e31818b7912
8. Vickers, AJ, Vertosick, EA, Lewith, G, MacPherson, H, Foster, NE, Sherman, KJ, et al. Acupuncture for chronic pain: update of an individual patient data meta-analysis. J Pain. (2018) 19:455–74. doi: 10.1016/j.jpain.2017.11.005
9. Irnich, D, Behrens, N, Molzen, H, König, A, Gleditsch, J, Krauss, M, et al. Randomised trial of acupuncture compared with conventional massage and “sham” laser acupuncture for treatment of chronic neck pain. BMJ. (2001) 322:1574–8. doi: 10.1136/bmj.322.7302.1574
10. Chen, YJ, Shimizu Bassi, G, and Yang, YQ. Classic Chinese acupuncture versus different types of control groups for the treatment of chronic pain: review of randomized controlled trials (2000–2018). Evid Based Complement Alternat Med. (2019) 2019:6283912. doi: 10.1155/2019/6283912
11. Witt, CM, Jena, S, Selim, D, Brinkhaus, B, Reinhold, T, Wruck, K, et al. Pragmatic randomized trial evaluating the clinical and economic effectiveness of acupuncture for chronic low back pain. Am J Epidemiol. (2006) 164:487–96. doi: 10.1093/aje/kwj224
12. Molsberger, AF, Mau, J, Pawelec, DB, and Winkler, J. Does acupuncture improve the orthopedic management of chronic low back pain—a randomized, blinded, controlled trial with 3 months follow up. Pain. (2002) 99:579–87. doi: 10.1016/s0304-3959(02)00269-5
13. Weiss, J, Quante, S, Xue, F, Muche, R, and Reuss-Borst, M. Effectiveness and acceptance of acupuncture in patients with chronic low back pain: results of a prospective, randomized, controlled trial. J Altern Complement Med. (2013) 19:935–41. doi: 10.1089/acm.2012.0338
14. Lorente, L, Martín, MM, Almeida, T, Hernández, M, Ramos, L, Argueso, M, et al. Serum substance P levels are associated with severity and mortality in patients with severe traumatic brain injury. Crit Care. (2015) 19:192. doi: 10.1186/s13054-015-0911-z
15. Lisowska, B, Lisowski, A, and Siewruk, K. Substance P and chronic pain in patients with chronic inflammation of connective tissue. PLoS One. (2015) 10:e0139206. doi: 10.1371/journal.pone.0139206
16. Lin, CC, Chen, WN, Chen, CJ, Lin, YW, Zimmer, A, and Chen, CC. An antinociceptive role for substance P in acid-induced chronic muscle pain. Proc Natl Acad Sci U S A. (2012) 109:E76–83. doi: 10.1073/pnas.1108903108
17. Engel, MA, Leffler, A, Niedermirtl, F, Babes, A, Zimmermann, K, Filipović, MR, et al. TRPA1 and substance P mediate colitis in mice. Gastroenterology. (2011) 141:1346–58. doi: 10.1053/j.gastro.2011.07.002
18. Fan, Y, Kim, DH, Gwak, YS, Ahn, D, Ryu, Y, Chang, S, et al. The role of substance P in acupuncture signal transduction and effects. Brain Behav Immun. (2020) 91:683–94. doi: 10.1016/j.bbi.2020.08.016
19. Collins, SL, Moore, RA, and McQuay, HJ. The visual analogue pain intensity scale: what is moderate pain in millimetres? Pain. (1997) 72:95–7. doi: 10.1016/s0304-3959(97)00005-5
20. Hu, Y, Mulot, C, Bourreau, C, Martin, D, Laurent-Puig, P, Radoi, L, et al. Biochemically tracked variability of blood plasma thawed-state exposure times in a multisite collection study. Biopreserv Biobank. (2020) 18:376-88. doi: 10.1089/bio.2019.0137
21. Haefeli, M, and Elfering, A. Pain assessment. Eur Spine J. (2006) 15:S17–24. doi: 10.1007/s00586-005-1044-x
22. Song, KJ, Choi, BW, Choi, BR, and Seo, GB. Cross-cultural adaptation and validation of the Korean version of the neck disability index. Spine. (2010) 35:E1045–9. doi: 10.1097/BRS.0b013e3181df78e9
23. Lee, H, Nicholson, LL, Adams, RD, Maher, CG, Halaki, M, and Bae, SS. Development and psychometric testing of Korean language versions of 4 neck pain and disability questionnaires. Spine. (2006) 31:1841–5. doi: 10.1097/01.brs.0000227268.35035.a5
24. Holmes, MM, Lewith, G, Newell, D, Field, J, and Bishop, FL. The impact of patient-reported outcome measures in clinical practice for pain: a systematic review. Qual Life Res. (2017) 26:245–57. doi: 10.1007/s11136-016-1449-5
25. Moon, TW, Posadzki, P, Choi, TY, Park, TY, Kim, HJ, Lee, MS, et al. Acupuncture for treating whiplash associated disorder: a systematic review of randomised clinical trials. Evid Based Complement Alternat Med. (2014) 2014:870271. doi: 10.1155/2014/870271
26. Zieglgänsberger, W. Substance P and pain chronicity. Cell Tissue Res. (2019) 375:227–41. doi: 10.1007/s00441-018-2922-y
Keywords: acupuncture, chronic neck pain, substance P, middle-aged women, neck disability index
Citation: Ko JH and Kim S-N (2023) Effect of acupuncture on pain and substance P levels in middle-aged women with chronic neck pain. Front. Neurol. 14:1267952. doi: 10.3389/fneur.2023.1267952
Edited by:
Qinhong Zhang, Heilongjiang University of Chinese Medicine, ChinaReviewed by:
Hee Young Kim, Yonsei University, Republic of KoreaFeng Han, University of California, Berkeley, United States
Copyright © 2023 Ko and Kim. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Seung-Nam Kim, c25raW1AZG9uZ2d1ay5lZHU=
†Present address: Jade Heejae Ko, Department of Neurosurgery, Stanford University School of Medicine, Stanford, CA, United States
 Jade Heejae Ko†
Jade Heejae Ko† Seung-Nam Kim
Seung-Nam Kim