
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Neurol. , 05 September 2023
Sec. Stroke
Volume 14 - 2023 | https://doi.org/10.3389/fneur.2023.1219679
This article is part of the Research Topic Reviews in: Stroke View all 25 articles
Purpose: Ischemic stroke (IS) has a considerable impact on the health-related quality of life (HRQoL) of patients. A systematic review was conducted to summarize and synthesize the HRQoL reported from IS patients.
Methods: An electronic search was performed in PubMed, Web of Science, ScienceDirect, Embase, and Cochrane Library databases from inception to February 2022 for studies measuring utility values in IS patients. Basic information about the studies, patient characteristics, measurement of the utility values, and utility values were extracted and summarized. Utility values were pooled according to the time of evaluation, and disease severity was classified with modified Rankin Scale (mRS) scores. The quality of the studies was assessed according to key criteria recommended by the National Institute for Health and Care Excellence.
Results: A total of 39 studies comprising 30,853 participants were included in the study. Measured with EQ-5D-3L, the pooled utility values were 0.42 [95% confidential interval (CI): 0.13 to 0.71], 0.55 (95% CI: 0.43 to 0.68), 0.65 (95% CI: 0.52 to 0.78), 0.60 (95% CI: 0.43 to 0.78), and 0.67 (95% CI: 0.60 to 0.74) for patients diagnosed with IS within 1, 3, 6, 12, and 24 months or above among poststroke patients. Four studies reported utility values classified by mRS scores where synthesized estimates stratified by mRS scores ranged from 0.91 (95% CI: 0.85 to 0.97) for patients with an mRS score of 1 to−0.04 (95% CI:−0.18 to 0.11) for those with an mRS score of 5. As for the health dimension profiles, usual activity was the most impacted dimension, while self-care was the least impacted one.
Conclusion: This study indicated that the utility values in IS patients kept increasing from stroke onset and became relatively stabilized at 6 months poststroke. Health utility values decreased significantly as mRS scores increased. These results facilitate economic evaluations in utility retrieval and selection. Further exploration was required regarding the factors that affect the HRQoL of IS patients.
Stroke continues to be one of the leading causes of death and disability worldwide; with 12.2 million strokes that occurred in 2019, ischemic stroke (IS) accounted for 62.4% (1). The disease burden of IS increases continuously in China, where the number of incident cases was estimated to reach 2.8 million in 2019 (2). Despite the advances in early management and secondary prevention, deaths from stroke have increased by 43.0% over the last three decades (1, 3, 4). Additionally, patients who survive IS often experience long-term disability (5), cognitive impairment (6), and emotional problems (7), leading to compromised health-related quality of life (HRQoL).
HRQoL can be defined as how well a person functions in their life and his or her perceived wellbeing in physical, mental, and social domains of health and can be presented using utility (8), which ranges from 0 to 1, where 0 represents death and 1 represents perfect health, and a negative utility value represents health states that are worse than death (9). There are various methods to directly and indirectly measure utility values; these methods can be performed among patients, their caregivers, or the general public. Direct evaluation methods such as time trade-off (TTO), standard gamble (SG), and rating scale (RS) elicit values directly from respondents who make their assignment with respect to specific health states or are required to report their preferences toward some hypothetical scenarios. However, these evaluation methods take more time and may involve problems regarding cognitive understanding and interviewer effects (10, 11). Indirect valuation methods such as the EuroQol 5-dimensional (12) (EQ-5D), Short Form 6 Dimensions (13) (SF-6D), 15D (14), and Health Utility Value Index (15) (HUI) are questionnaires that are easier to administer and thus can be included as a part of clinical trials or routine follow-up without increasing respondent burden (16). In the questionnaires, respondents specify their health states in multiple dimensions, and the questionnaire responses are then converted to utility values by means of “tariffs” (17). The “tariffs” are obtained from previous studies in which values for possible health states were elicited from the general population using methods such as TTO (12, 17).
Utility can also be applied to estimate quality-adjusted life years (QALYs) gained for cost-effectiveness analysis by multiplying by the time of survival in a certain health state. With the launch of new medical techniques, the use of cost-effective analysis to compare the potential benefits, harms, and costs between new interventions and existing interventions is an important technique for healthcare decision-makers and has been widely adopted in many countries to help better allocate medical resources (18).
Given the important role of health utility values in summarizing HRQoL and supporting cost-effectiveness analysis, this systematic review aimed to identify and summarize studies reporting utility values in IS and provide the pooled utility values of the IS population at different times of measurement and disease severities.
This systematic review was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement (19).
The PubMed, Embase, Cochrane Library, Web of Science, and ScienceDirect databases were searched from inception to February 2022. Search terms included “ischemic stroke,” “ischaemic stroke,” “patient reported outcomes,” “quality of life,” “QoL” and “HRQoL.” Detailed information on search items in the abovementioned database is shown in Supplementary Table 1.
According to the PICOS framework, both clinical trials and observational studies that reported outcomes on utility values in IS patients were included. There were no restrictions on interventions and comparators. In order to decrease the heterogeneity and uncertainty, studies were excluded if they met any of the following criteria: (a) only abstracts or studies with full-text unavailable; (b) systematic review; (c) economic evaluation; (d) not published in English; (e) reported utility values for a mixed cohort of patients with IS and hemorrhagic stroke; and (f) non-original study that did not provide additional information on health utility.
The characteristics of the included studies were extracted independently by two reviewers, with disagreements resolved through discussion or a third reviewer. The following data were extracted from the included studies: study characteristics (year of publication, country or region, study design, sample size, and intervention/grouping), demographic characteristics of patients (age and gender), methodology of HRQoL measurement (survey method, evaluation time, and tariff), and utility values.
To observe the long-term changes in utility values in the IS population, mean utility values elicited with the EQ-5D were synthesized by meta-analysis according to the appropriate time of evaluation. Since few studies reported the mean utility values using EQ-5D-5L, only mean utility values measured using EQ-5D-3L were pooled. Considering the short duration of stay, days from discharge were regarded as days from poststroke. Additionally, the difference in synthesized utility values between each evaluation time was compared with minimally important differences (MIDs) in the EQ-5D-3L in stroke. The MID in the EQ-5D was 0.08 to 0.12 (20), and a 0.1-point increase or decrease in utility was considered an important change in our study. Furthermore, the utility values stratified by the modified Rankin Scale (mRS) were also pooled to describe utility weights for individuals with different mRS scores. The mRS is a commonly used clinician-reported scale that assesses changes in disability after stroke, with scores ranging from 0 to 6 (21).
Notably, this study aimed to synthesize utility values for IS population, and utility values derived from patients who entered the randomized controlled studies and received the specific treatments (e.g., intensive lipid rather than guideline lipid) or participated in some therapeutic programs (e.g., home rehabilitation program, which was a home-based exercise program provided by a physical therapist) tend to generate better health states with higher utility values and could not represent the general population. Similarly, the utility values for IS patients with specific poststroke complications (e.g., spasticity) were not included. Pooled utility values of compared groups from clinical trials were also excluded. For multiple publications from the same study population, the article that reported utility values appropriate for meta-analysis or covered a larger sample size was included. For any study reporting utility values applying diverse tariffs from multiple countries, to eliminate the additive effect, only the utility value calculated using investigators' country-specific tariff was included in the meta-analysis.
If the standard deviation (SD) around the mean utility value was not available in the article, estimations from the standard error or 95% confidential interval (CI) were applied. The heterogeneity among the included studies was assessed using the I2 statistic, and fixed effects models were employed if the value of I2 was smaller than 50%; otherwise, random effects models were used. The meta-analysis was conducted in R software version 4.2.1 using the “meta” package.
Since there were no agreed criteria specific for assessing the quality of utility studies, we assessed the quality of the included studies based on the criteria recommended in the National Institute for Health and Clinical Excellence guidance on a systematic review of utility values (22) and additional two criteria (uncertainty measurement and appropriateness of tariff) applied in the study by Mok et al. (23).
The flowchart of study selection and the inclusion process is presented in Figure 1. Our search initially identified 4,106 references. After removing duplicates, 1,911 records were further screened by titles and abstracts. Finally, 91 articles were subject to full-text screening, where 55 were excluded mostly because they did not involve utility evaluation. Three additional studies were identified from the reference lists of relevant publications. A total of 39 studies were included, and 17 studies were selected for meta-analysis.
The basic characteristics of the included studies are summarized in Table 1. A total of 39 identified studies were published between 1999 (24) and 2022 (25), with most of studies (n = 8) (26–33) published in 2017. The included studies covered different regions around the world. Five of the studies were multinational (26, 31, 34–36), 18 studies in Europe (24, 27, 28, 30, 32, 33, 37–48), 8 studies in Asia (25, 49–55), 7 studies in North America (29, 56–61), and 1 study in Australia (62). In terms of study design, 22 of the 39 (56.4%) studies were observational, while the rest were randomized controlled studies to assess the effectiveness of treatment. In the randomized controlled studies, endovascular treatment (EVT) was the most common therapy (25, 28, 31–33, 35, 43, 54). Other treatments included a rehabilitation program, alteplase, citicoline, intravenous tissue plasminogen activator (t-PA), lipid management, and blood pressure management. Studies included 30,853 participants (adjustment has been made for the overlapping populations), and the sample size ranged from 11 to 4,016. The average or median age of the study population was >60 years in most of the studies. The proportion of males ranged from 36.0 to 81.6%.
The evaluation methods are presented in Table 2. For methods applied, three studies (40, 42, 46) did not specify the survey method, while nine studies (25, 28, 34, 36, 44, 45, 53, 54, 61) used more than one method. The survey methods included telephone interviews (n = 16, 41.0%), face-to-face interviews (n = 11, 28.2%), questionnaires during the follow-up visit (n = 10, 25.6%), and postal questionnaires (n = 4, 10.3%). As for the respondents, only one study involved a normal population (24), in which they were asked to imagine their preference for certain scenarios as IS survivors. Among the studies that reported specific information on respondents, the percentage of proxies in the reported studies ranged from 12 to 56%. Regarding the utility score elicitation method, only one study used direct methods where TTO, SG, and RS were adopted simultaneously (24). For the indirect methods, the vast majority of studies (n = 37) used the EQ-5D, most of which (n = 31) used the EQ-5D-3L, 4 studies used EQ-5D-5L, and 2 studies did not mention the EQ-5D-3L/EQ-5D-5L version. In addition, the time point of evaluation for IS patients in the included studies ranged from the stroke onset to 7 years poststroke. A total of 3, 6, 12, and 24 months after stroke/discharge were the most frequently adopted evaluation time points. For tariffs to calculate utility values, 20 studies did not specify the tariffs, and 2 of 5 multinational studies (26, 34) used tariffs from multiple countries of the study population.
We synthesized the utility values by the baseline (within 1 month after stroke/discharge), 3, 6, 12, and 24 months or above among poststroke patients, as illustrated in Figure 2. For patients at the baseline of stroke onset, the utility values were reported in five studies, ranging from−0.11 to 0.67. Accordingly, the pooled estimate as utility value for the acute stroke phase was 0.42 (95% CI: 0.13 to 0.71), with significant heterogeneity (I2 = 100%), as presented in Figure 2A. When measured at 3 months after stroke, the utility values were increased and ranged from 0.34 to 0.71 in six studies. The synthesized utility value was 0.55 (95% CI: 0.43 to 0.68). When measured at 6 months after stroke, the utility values ranged from 0.34 to 0.82 in six studies, and the pooled utility value was 0.65 (95% CI: 0.52 to 0.78). A slight decrease could be observed at 12 months poststroke, where the estimated utility values were 0.60 (95% CI: 0.43 to 0.78). The synthesized utility values were 0.67 (95% CI: 0.60 to 0.74) at 24 months and above poststroke, indicating a relatively steady HRQoL among patients. Health utility values kept increasing from stroke onset to 6 months poststroke, and MID could be observed between the baseline and 3 months as well as 3 and 6 months. Therefore, it is concluded that the utility values reached a relatively stable level after 6 months poststroke. The utility values after 6 months were further combined and estimated to be 0.66 (95% CI: 0.59 to 0.72), as presented in Supplementary Figure 1. The trend of change in utility values was similar to that of most of the included longitudinal studies (Figure 3).
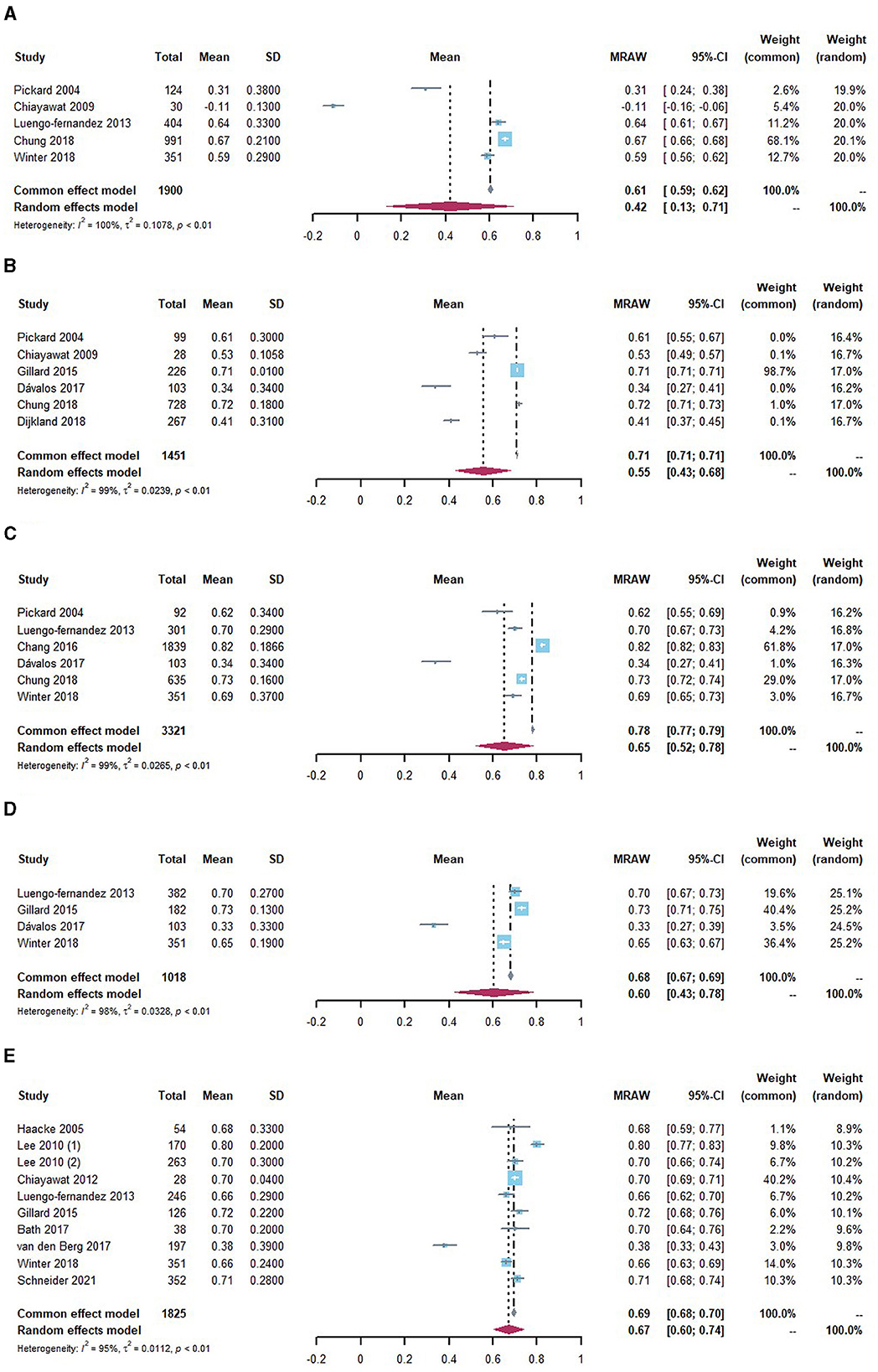
Figure 2. Utility values stratified by evaluation time for IS population (A) within 1 month of poststroke, (B) at 3 months of poststroke, (C) at 6 months of poststroke, (D) at 12 months of poststroke, and (E) 24 months and above of poststroke.
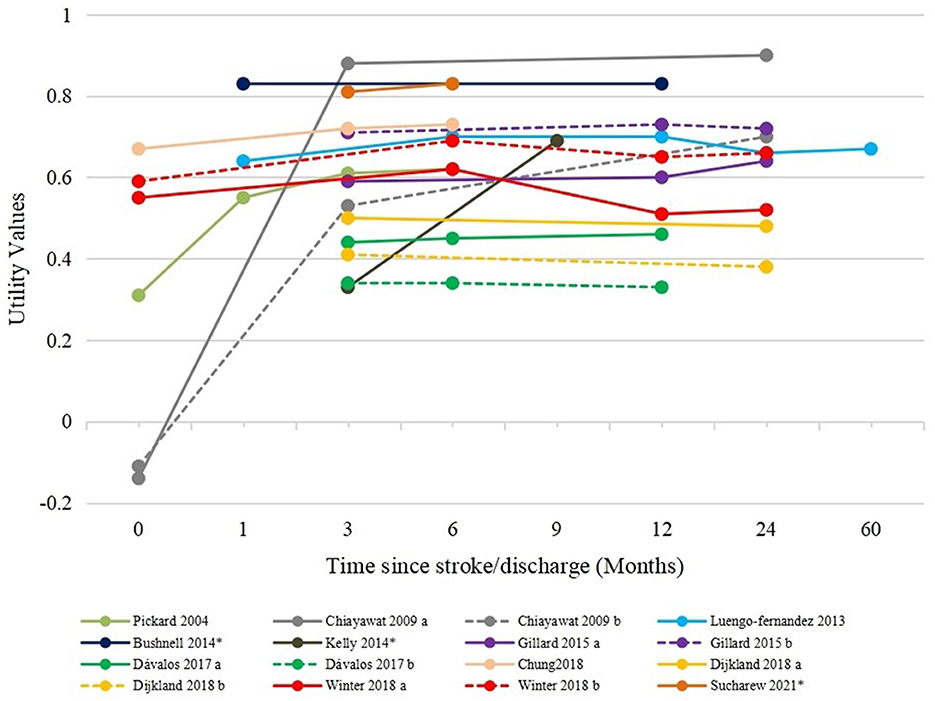
Figure 3. Utility values in longitudinal studies. Chiayawat 2009 a, rehabilitation program; Chiayawat 2009 b, usual care; Gillard 2015 a, patients with spasticity; Gillard 2015 b, patients without spasticity; Dávalos 2017 a, endovascular treatment + medical treatment; Dávalos 2017 b, medical treatment; Dijkland 2018 a, EVT + usual care; Dijkland 2018 b, usual care; Winter 2018 a, patients with poststroke epilepsy; Winter 2018 b, patients with poststroke epilepsy. *Utility values were reported as median values in these studies.
Eight studies reported utility values stratified by mRS scores (as shown in Table 3), of which three reported utility values for dichotomized mRS scores (24, 37, 62) (classified as “independence” and “severe disability”) and one study reported the utility index as median values (31). Thus, these four studies were excluded, and the other four studies reported mean values (26, 36, 43, 44) were included in the pooled analysis. With considerable heterogeneity, the pooled effect estimates for mRS scores from 0 to 5 were 0.91, 0.85, 0.73, 0.54, 0.26, and−0.04, respectively, as shown in Figure 4. The MID in utility values was seen between all mRS levels except mRS 0 and mRS 1.
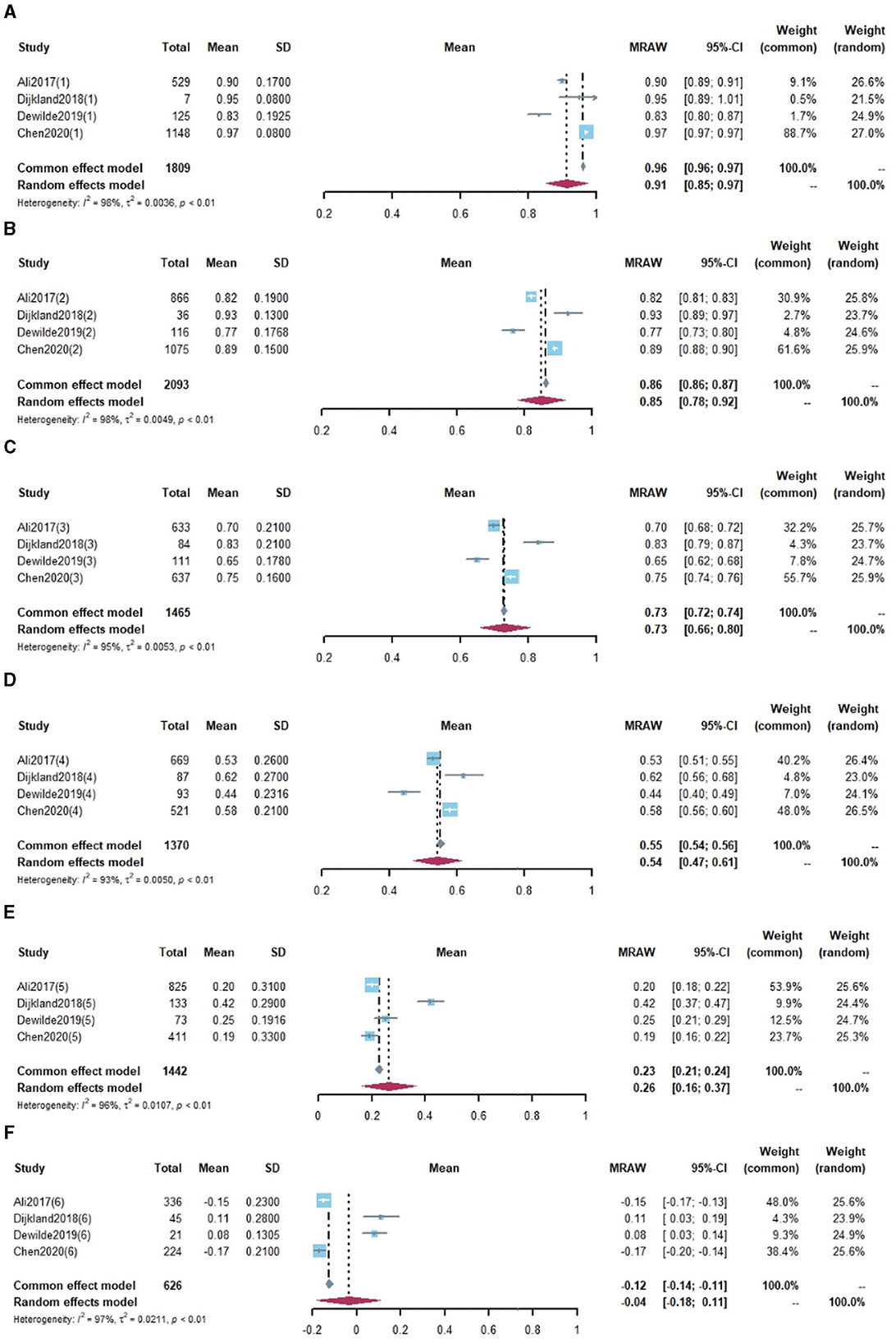
Figure 4. Utility values by modified Rankin Scale for IS population. (A) mRS = 0, (B) mRS = 1, (C) mRS = 2, (D) mRS = 3, (E) mRS = 4, (F) mRS = 5.
The utility of the IS population is affected by many factors. Some of the studies reported utility values for specific subgroups of IS populations. For example, four studies reported utility values for male and female IS patients, and all suggested that men had better HRQoL as measured by the EQ-5D-3L than women (37, 40, 55, 58). In addition, one study reported utility values stratified by National Institutes of Health Stroke Scale (NIHSS) scores, which was another scale for disease severity. It was indicated that utility values at 3 months for NIHSS 0–4, NIHSS 5–11, NIHSS 12–19, and NIHSS ≥ 20 were 0.86, 0.77, 0.59, and 0.52, respectively (35).
Poststroke complications also played an important role in affecting utility values, and it was reported that IS patients with poststroke spasticity had lower scores on the EQ-5D (0.63 vs. 0.71) (59). Similarly, patients with poststroke epilepsy reported worse HRQoL in the long term (42).
Moreover, the utility values were affected by the valuation instrument. In four studies that reported instrument-specific utility values, the utility values elicited by EQ-5D were lower than those elicited by 15D (38, 41) but higher than those elicited by HUI3 (37, 56). Additionally, the utility was mediated by respondents due to differences in the perception of HRQoL between patients and their proxies, in two studies that reported the utility of specific respondents, both suggested that the utility was slightly lower for proxies than for patient self-assessments (56, 61).
Nine studies (16 groups) reported the responses to EQ-5D dimensions. The overall information on responses to five dimensions is illustrated in Figure 5. Given the differences in baseline characteristics, disease severity of the study population, and evaluation time, the proportion of patients reporting “no problems” in each dimension varied greatly. Nevertheless, by comparing the dimensions, 12 groups suggested that the proportion of patients who reported “no problems” in the self-care dimension was higher than that of other dimensions. Additionally, six groups showed that the proportion of patients who reported “no problems” in the usual activity dimension was lower than that of other dimensions. In general, the most impaired health dimension was usual activity, while self-care was the least impacted dimension. Anxiety/depression, pain/discomfort, and mobility dimensions were moderately affected.
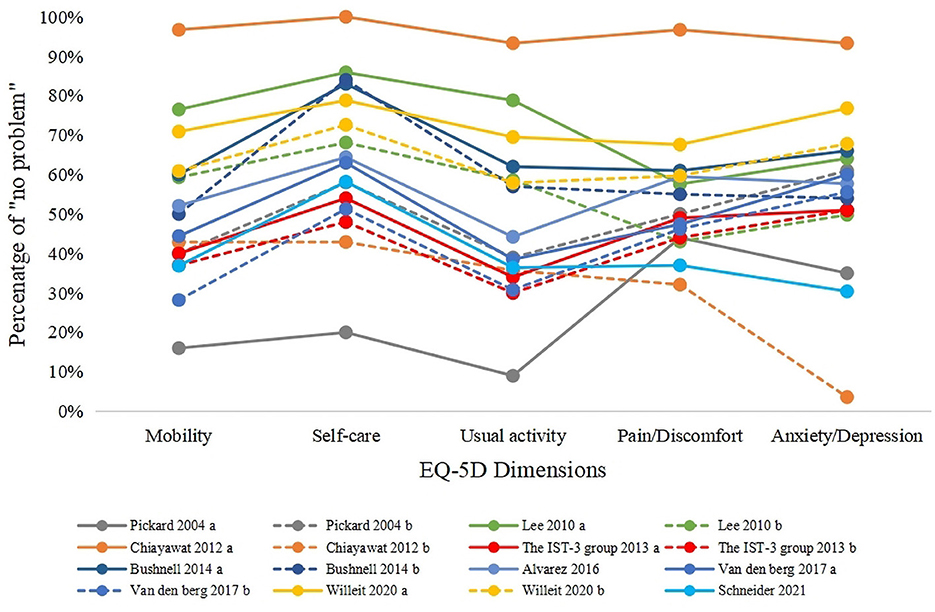
Figure 5. Responses to EQ-5D dimensions. Pickard 2004 a, within 2 weeks of stroke (baseline); Pickard 2004 b, 6 months after baseline; Lee 2010 a, lacunar infarction; Lee 2010 b, non-lacunar infarction; Chiayawat 2012 a, rehabilitation program; Chiayawat 2012 b, usual care; The IST-3 group a, alteplase + standard care; The IST-3 group b, standard care; Bushnell 2014 a, male; Bushnell 2014 b, female; Van den berg 2017 a, endovascular treatment plus usual care; Van den berg 2017 b, usual care.
The quality assessment of the included studies is presented in Supplementary Table 2. Many studies did not provide sufficient information on evaluation methodology or utility results to be assessed by several criteria, such as response rates to instruments and missing data. More specifically, in terms of sample size, the utility values were elicited from fewer than 100 participants in five studies (27, 37, 49, 51, 57). The sample size was smaller within the studies focused on specific patients such as those who underwent hemicraniectomy or who had specific complications. The recruitment and inclusion criteria were given in most of the included studies, and since most of the studies applied restrictions on age, disease severity, medical history, and so on and excluded the most severe patients, an overestimate of utility may be induced.
Regarding the results reporting, 22 studies (56.4%) reported their response rates to utility instruments, and none of them were lower than 60%. In addition, in eight included longitudinal studies, only one study (42) did not report information on lost follow-up. However, it remained unclear whether patient characteristics with lost follow-up were similar to those of patients followed up for the rest of the studies indicating a potential risk of bias. Information on missing data was reported in a limited number of studies (n = 12), and eight of them stated the techniques of handling missing data, such as multiple imputation (39, 45) and analysis based on only complete data (52, 58). The studies that did not report missing data or the corresponding solution could also cause potential biased estimates.
The measures to elicit utility values were all considered valid in all included studies because they all used well-established instruments. For the uncertainty measurements, most of the studies reported SD or interquartile range (IQR) as uncertain estimates, and only two studies (31, 62) reported median utility values without uncertain estimates. Information on tariffs remained unclear in more than 35% of the included studies, and three studies (48, 50, 56) might apply inappropriate tariffs that did not match the country/region of origin of the HRQoL respondents mainly because localized tariffs were not established at the time their studies were conducted.
HRQoL plays an important role in measuring and assessing the total wellbeing of poststroke patients. This study aimed to summarize the HRQoL among patients with IS by a systematic review of previous studies. It could be found that EQ-5D-3L was still the most frequently used tool for measuring HRQoL in IS. Additionally, the meta-analysis was performed according to different times of evaluation poststroke and mRS scores. Thereafter, the results could not only observe and discuss the long-term changes in preference-based HRQoL of IS but also provide utility within each mRS level, both of which could be applied in future economic evaluations. When pooling according to the time of evaluation, the results showed that the mean utility values across the included studies increased gradually over time and then reached a stable level at 6 months poststroke. This made sense because the health condition of patients was expected to be improved after the treatment even though IS could make them suffer from long-term disability. However, the utility values were consistently lower than the matched non-stroke population in the long-term observation (30, 48). When stratified by mRS levels, the utility estimates significantly declined by increasing the mRS levels, and the utility for mRS 5 was negative in our review, suggesting that patients had health states that were worse than death. The summary of utility values for specific groups and the response to EQ-5D dimensions might also provide additional information to researchers. Specifically, female patients and patients with poststroke complications had worse HRQoL, which suggested that more attention should be paid to these patients in disease management. Moreover, since self-care dimension was relatively less impacted, efforts to improve patients' HRQoL should focus on usual activity, anxiety/depression, pain or discomfort, and mobility dimensions.
While there have been numerous studies of HRQoL in patients with IS, to the best of our knowledge, very few studies have reviewed utility values regarding IS. Previous reviews included hemorrhagic stroke and were published almost 2 decades ago (64–66), which might not be representative of the current perception in HRQoL. The recently published review (67), focusing on observational studies, synthesized utility values by the evaluation time points and found that a great increase in utility values between acute care and < 4-month follow-up, which was consistent with our findings. Moreover, we used an additional time point (2 years and above) for pooled utility values because economic evaluations of cardiovascular disease often include health states for 2-year poststroke (68, 69). In comparison with this review, the present systematic review focuses on a certain type of stroke without much restriction on the study design and therefore provides more applicable evidence. Moreover, our findings serve as an update for a current assessment of the evidence on the HRQoL in IS patients.
The study also has several limitations to be considered. First, there was a significant heterogeneity in reported utility values although we followed a rational approach to pool comparable studies that applied EQ-5D-3L to similar evaluation time or disease severity and employed random effects models. Heterogeneity in utility may be induced by the differences in characteristics of participants, including age, gender, and complications. Treatments that were assigned to patients, evaluation methods, and tariffs would also contribute to heterogeneity. Second, there was a poor representation of studies from Central and South America, so it could affect the generalizability of the combined results for these regions. Third, our study may be subject to selection bias since the included studies were limited to those published in English. However, given that English is widely used and well accepted around the world, such influence may be mitigated. Fourth, with limited applicable mean utility values measured with EQ-5D-5L, only mean values measured with EQ-5D-3L were included in the meta-analysis. Furthermore, with a limited number of studies assessing the utility values for subgroups, subgroup analysis was not feasible.
There are some arrears that require further investigation in future research. For instance, utility values stratified by time since IS were important to economic evaluations of cardiovascular disease, our findings might be useful when there were no suitable or appropriate sources, and future evidence on long-term changes in utility values among IS patients from longitudinal studies could be more reliable. Additionally, utility estimates for IS patients with complications needed further explanation since poststroke complication has a negative influence on utility, but few studies have investigated on this. Furthermore, few studies have focused on the impact of IS on utility for caregivers or families, which has been evidenced as a source of significant burden (70). Finally, future HRQoL studies would be more informative if considering the appropriate sample size, evaluation method, reporting the missing data, uncertainty around utility results, and so on. These could facilitate future research studies, health decision–making, and improvement of health policies by providing high-quality data and evidence.
IS has a substantial effect on patients' HRQoL. This study provided a comprehensive summary of the characteristics of HRQoL research in IS, synthesized health utility values both at different time poststroke and mRS levels, and assessed the quality of studies. The findings from this study will be informative for HRQoL research, economic evaluations, and health decision-making.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
LW and AM contributed to the conception of the study. LW and JZ completed the database search. JZ, QW, HH, and WL conducted the screening, data extraction, and quality assessment, under the guidance of LW, XG, and AM. JZ and LW performed the meta-analysis and interpreted the data. JZ, QW, and LW contributed to the writing and revised the manuscript. All authors approved the final manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2023.1219679/full#supplementary-material
1. GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet Neurol. (2021) 20:795–820. doi: 10.1016/S1474-4422(21)00252-0
2. Sun T, Chen S, Wu K, Sun M, Zhang X, You C. Trends in incidence and mortality of stroke in China from 1990 to 2019. Front Neurol. (2021) 12:759221. doi: 10.3389/fneur.2021.759221
3. Edwards JD, Kapral MK, Fang J, Swartz RH. Trends in long-term mortality and morbidity in patients with no early complications after stroke and transient ischemic attack. J Stroke Cerebrovasc Dis. (2017) 26:1641–5. doi: 10.1016/j.jstrokecerebrovasdis.2016.09.038
4. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American heart association/American stroke association. Stroke. (2019) 50:e344–418. doi: 10.1161/STR.0000000000000211
5. Hasan TF, Hasan H, Kelley RE. Overview of acute ischemic stroke evaluation and management. Biomedicines. (2021) 9:1486. doi: 10.3390/biomedicines9101486
6. Mellon L, Brewer L, Hall P, Horgan F, Williams D, Hickey A, et al. Cognitive impairment six months after ischaemic stroke: a profile from the ASPIRE-S study. BMC Neurol. (2015) 15:31. doi: 10.1186/s12883-015-0288-2
7. Hackett ML, Pickles K. Part I: frequency of depression after stroke: an updated systematic review and meta-analysis of observational studies. Int J Stroke. (2014) 9:1017–25. doi: 10.1111/ijs.12357
8. Torrance GW. Utility approach to measuring health-related quality of life. J Chronic Dis. (1987) 40:593–603. doi: 10.1016/0021-9681(87)90019-1
9. Torrance GW. Measurement of health state utility value for economic appraisal. J Health Econ. (1986) 5:1–30. doi: 10.1016/0167-6296(86)90020-2
10. Stiggelbout AM, de Haes JC. Patient preference for cancer therapy: an overview of measurement approaches. J Clin Oncol. (2001) 19:220–30. doi: 10.1200/JCO.2001.19.1.220
11. Lugnér AK, Krabbe PFM. An overview of the time trade-off method: concept, foundation, and the evaluation of distorting factors in putting a value on health. Expert Rev Pharmacoecon Outcomes Res. (2020) 20:331–42. doi: 10.1080/14737167.2020.1779062
12. Rabin R, de Charro F. EQ-5D: a measure of health status from the EuroQol group. Ann Med. (2001) 33:337–43. doi: 10.3109/07853890109002087
13. Brazier J, Roberts J, Deverill M. The estimation of a preference-based measure of health from the SF-36. J Health Econ. (2002) 21:271–92. doi: 10.1016/S0167-6296(01)00130-8
14. Sintonen H. The 15D instrument of health-related quality of life: properties and applications. Ann Med. (2001) 33:328–36. doi: 10.3109/07853890109002086
15. Horsman J, Furlong W, Feeny D, Torrance G. The Health Utilities Index (HUI): concepts, measurement properties and applications. Health Qual Life Outcomes. (2003) 1:54. doi: 10.1186/1477-7525-1-54
16. Brazier J, Ara R, Rowen D, Chevrou-Severac H. A review of generic preference-based measures for use in cost-effectiveness models. Pharmacoeconomics. (2017) 35:21–31. doi: 10.1007/s40273-017-0545-x
17. Arnold D, Girling A, Stevens A, Lilford R. Comparison of direct and indirect methods of estimating health state utilities for resource allocation: review and empirical analysis. BMJ. (2009) 339:b2688. doi: 10.1136/bmj.b2688
18. Sanders GD, Maciejewski ML, Basu A. Overview of cost-effectiveness analysis. JAMA. (2019) 321:1400–1. doi: 10.1001/jama.2019.1265
19. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
20. Kim SK, Kim SH, Jo MW, Lee SI. Estimation of minimally important differences in the EQ-5D and SF-6D indices and their utility in stroke. Health Qual Life Outcomes. (2015) 13:32. doi: 10.1186/s12955-015-0227-3
21. Wilson JT, Hareendran A, Grant M, Baird T, Schulz UG, Muir KW, et al. Improving the assessment of outcomes in stroke: use of a structured interview to assign grades on the modified Rankin Scale. Stroke. (2002) 33:2243–6. doi: 10.1161/01.STR.0000027437.22450.BD
22. Papaioannou D, Brazier, J, Paisley, S,. NICE Decision Support Unit Technical Support Document 9: The Identification, Review Synthesis of Health State Utility Values From the Literature. (2010). Available online at: http://nicedsu.org.uk/wp-content/uploads/2016/03/TSD9-HSUV-values_FINAL.pdf (accessed October 17, 2022).
23. Mok CH, Kwok HHY, Ng CS, Leung GM, Quan J. Health state utility values for type 2 diabetes and related complications in east and Southeast Asia: a systematic review and meta-analysis. Value Health. (2021) 24:1059–67. doi: 10.1016/j.jval.2020.12.019
24. Hallan S, Asberg A, Indredavik B, Widerøe TE. Quality of life after cerebrovascular stroke: a systematic study of patients' preferences for different functional outcomes. J Intern Med. (1999) 246:309–16. doi: 10.1046/j.1365-2796.1999.00531.x
25. Zhang P, Shen HJ, Chen L, Zhu X, Zhang MM, Jiang Y, et al. Patient-reported anxiety/depression after endovascular thrombectomy: a post-hoc analysis of direct-MT trial. Front Neurol. (2022) 13:811629. doi: 10.3389/fneur.2022.811629
26. Ali M, MacIsaac R, Quinn TJ, Bath PM, Veenstra DL, Xu Y, et al. Dependency and health utilities in stroke: data to inform cost-effectiveness analyses. Eur Stroke J. (2017) 2:70–6. doi: 10.1177/2396987316683780
27. Bath PM, Scutt P, Blackburn DJ, Ankolekar S, Krishnan K, Ballard C, et al. Intensive versus guideline blood pressure and lipid lowering in patients with previous stroke: main results from the pilot 'prevention of decline in cognition after stroke trial' (PODCAST) randomised controlled trial. PLoS ONE. (2017) 12:e0164608. doi: 10.1371/journal.pone.0164608
28. Dávalos A, Cobo E, Molina CA, Chamorro A, de Miquel MA, Román LS, et al. Safety and efficacy of thrombectomy in acute ischaemic stroke (REVASCAT): 1-year follow-up of a randomised open-label trial. Lancet Neurol. (2017) 16:369–76. doi: 10.1016/S1474-4422(17)30047-9
29. Katzan IL, Thompson NR, Lapin B, Uchino K. Added value of patient-reported outcome measures in stroke clinical practice. J Am Heart Assoc. (2017) 6:e005356. doi: 10.1161/JAHA.116.005356
30. Persson J, Levin LÅ, Holmegaard L, Redfors P, Jood K, Jern C, et al. Stroke survivors' long-term QALY-weights in relation to their spouses' QALY-weights and informal support: a cross-sectional study. Health Qual Life Outcomes. (2017) 15:150. doi: 10.1186/s12955-017-0724-7
31. Rangaraju S, Haussen D, Nogueira RG, Nahab F, Frankel M. Comparison of 3-month stroke disability and quality of life across modified rankin scale categories. Interv Neurol. (2017) 6:36–41. doi: 10.1159/000452634
32. Schreuders J, van den Berg LA, Fransen PS, Berkhemer OA, Beumer D, Lingsma HF, et al. Quality of life after intra-arterial treatment for acute ischemic stroke in the MR CLEAN trial-Update. Int J Stroke. (2017) 12:708–12. doi: 10.1177/1747493017706244
33. van den Berg LA, Dijkgraaf MG, Berkhemer OA, Fransen PS, Beumer D, Lingsma HF, et al. Two-year outcome after endovascular treatment for acute ischemic stroke. N Engl J Med. (2017) 376:1341–9. doi: 10.1056/NEJMoa1612136
34. IST-3 Collaborative Group. Effect of thrombolysis with alteplase within 6 h of acute ischaemic stroke on long-term outcomes (the third International Stroke Trial [IST-3]): 18-month follow-up of a randomised controlled trial. Lancet Neurol. (2013) 12:768–76. doi: 10.1016/S1474-4422(13)70130-3
35. Rangaraju S, Frankel M, Jovin TG. Prognostic value of the 24-hour neurological examination in anterior circulation ischemic stroke: a post hoc analysis of two randomized controlled stroke trials. Interv Neurol. (2016) 4:120–9. doi: 10.1159/000443801
36. Chen X, Wang X, Delcourt C, Li J, Arima H, Hackett ML, et al. Ethnicity and other determinants of quality of functional outcome in acute ischemic stroke: the ENCHANTED trial. Stroke. (2020) 51:588–93. doi: 10.1161/STROKEAHA.119.027639
37. Haacke C, Althaus A, Spottke A, Siebert U, Back T, Dodel R. Long-term outcome after stroke: evaluating health-related quality of life using utility measurements. Stroke. (2006) 37:193–8. doi: 10.1161/01.STR.0000196990.69412.fb
38. Naess H, Lunde L, Brogger J. The effects of fatigue, pain, and depression on quality of life in ischemic stroke patients: the Bergen stroke study. Vasc Health Risk Manag. (2012) 8:407–13. doi: 10.2147/VHRM.S32780
39. Luengo-Fernandez R, Gray AM, Bull L, Welch S, Cuthbertson F, Rothwell PM, et al. Quality of life after TIA and stroke: ten-year results of the oxford vascular study. Neurology. (2013) 81:1588–95. doi: 10.1212/WNL.0b013e3182a9f45f
40. Alvarez-Sabín J, Santamarina E, Maisterra O, Jacas C, Molina C, Quintana M, et al. Long-term treatment with citicoline prevents cognitive decline and predicts a better quality of life after a first ischemic stroke. Int J Mol Sci. (2016) 17:390. doi: 10.3390/ijms17030390
41. Sand KM, Wilhelmsen G, Naess H, Midelfart A, Thomassen L, Hoff JM. Vision problems in ischaemic stroke patients: effects on life quality and disability. Eur J Neurol. (2016) 23:1–7. doi: 10.1111/ene.12848
42. Winter Y, Daneshkhah N, Galland N, Kotulla I, Krüger A, Groppa S. Health-related quality of life in patients with poststroke epilepsy. Epilepsy Behav. (2018) 80:303–6. doi: 10.1016/j.yebeh.2017.12.037
43. Dijkland SA, Voormolen DC, Venema E, Roozenbeek B, Polinder S, Haagsma JA, et al. Utility-weighted modified rankin scale as primary outcome in stroke trials: a simulation study. Stroke. (2018) 49:965–71. doi: 10.1161/STROKEAHA.117.020194
44. Dewilde S, Annemans L, Lloyd A, Peeters A, Hemelsoet D, Vandermeeren Y, et al. The combined impact of dependency on caregivers, disability, and coping strategy on quality of life after ischemic stroke. Health Qual Life Outcomes. (2019) 17:31. doi: 10.1186/s12955-018-1069-6
45. Oemrawsingh A, van Leeuwen N, Venema E, Limburg M, de Leeuw FE, Wijffels MP, et al. Value-based healthcare in ischemic stroke care: case-mix adjustment models for clinical and patient-reported outcomes. BMC Med Res Methodol. (2019) 19:229. doi: 10.1186/s12874-019-0864-z
46. Jarosławski S, Jarosławska B, Błaszczyk B, Auqier P, Toumi M. Health-related quality of life of patients after ischaemic stroke treated in a provincial hospital in Poland. J Mark Access Health Policy. (2020) 8:1775933. doi: 10.1080/20016689.2020.1775933
47. Willeit P, Toell T, Boehme C, Krebs S, Mayer L, Lang C, et al. STROKE-CARD care to prevent cardiovascular events and improve quality of life after acute ischaemic stroke or TIA: a randomised clinical trial. EClinicalMedicine. (2020) 25:100476. doi: 10.1016/j.eclinm.2020.100476
48. Schneider S, Taba N, Saapar M, Vibo R, Kõrv J. Determinants of long-term health-related quality of life in young ischemic stroke patients. J Stroke Cerebrovasc Dis. (2021) 30:105499. doi: 10.1016/j.jstrokecerebrovasdis.2020.105499
49. Chaiyawat P, Kulkantrakorn K, Sritipsukho P. Effectiveness of home rehabilitation for ischemic stroke. Neurol Int. (2009) 1:e10. doi: 10.4081/ni.2009.e10
50. Lee HY, Hwang JS, Jeng JS, Wang JD. Quality-adjusted life expectancy (QALE) and loss of QALE for patients with ischemic stroke and intracerebral hemorrhage: a 13-year follow-up. Stroke. (2010) 41:739–44. doi: 10.1161/STROKEAHA.109.573543
51. Chaiyawat P, Kulkantrakorn K. Effectiveness of home rehabilitation program for ischemic stroke upon disability and quality of life: a randomized controlled trial. Clin Neurol Neurosurg. (2012) 114:866–70. doi: 10.1016/j.clineuro.2012.01.018
52. Chang WH, Sohn MK, Lee J, Kim DY, Lee SG, Shin YI, et al. Predictors of functional level and quality of life at 6 months after a first-ever stroke: the KOSCO study. J Neurol. (2016) 263:1166–77. doi: 10.1007/s00415-016-8119-y
53. Chung PW, Yoon BW, Lee YB, Shin BS, Kim HY, Park JH, et al. Medication adherence of statin users after acute ischemic stroke. Eur Neurol. (2018) 80:106–14. doi: 10.1159/000493530
54. Yang P, Zhang Y, Zhang L, Zhang Y, Treurniet KM, Chen W, et al. Endovascular thrombectomy with or without intravenous alteplase in acute stroke. N Engl J Med. (2020) 382:1981–93. doi: 10.1056/NEJMoa2001123
55. She R, Yan Z, Hao Y, Zhang Z, Du Y, Liang Y, et al. Health-related quality of life after first-ever acute ischemic stroke: associations with cardiovascular health metrics. Qual Life Res. (2021) 30:2907–17. doi: 10.1007/s11136-021-02853-x
56. Pickard AS, Johnson JA, Feeny DH, Shuaib A, Carriere KC, Nasser AM. Agreement between patient and proxy assessments of health-related quality of life after stroke using the EQ-5D and health utilities index. Stroke. (2004) 35:607–12. doi: 10.1161/01.STR.0000110984.91157.BD
57. Kelly ML, Rosenbaum BP, Kshettry VR, Weil RJ. Comparing clinician- and patient-reported outcome measures after hemicraniectomy for ischemic stroke. Clin Neurol Neurosurg. (2014) 126:24–9. doi: 10.1016/j.clineuro.2014.08.007
58. Bushnell CD, Reeves MJ, Zhao X, Pan W, Prvu-Bettger J, Zimmer L, et al. Sex differences in quality of life after ischemic stroke. Neurology. (2014) 82:922–31. doi: 10.1212/WNL.0000000000000208
59. Gillard PJ, Sucharew H, Kleindorfer D, Belagaje S, Varon S, Alwell K, et al. The negative impact of spasticity on the health-related quality of life of stroke survivors: a longitudinal cohort study. Health Qual Life Outcomes. (2015) 13:159. doi: 10.1186/s12955-015-0340-3
60. Romano JG, Gardener H, Campo-Bustillo I, Khan Y, Tai S, Riley N, et al. Predictors of outcomes in patients with mild ischemic stroke symptoms: MaRISS. Stroke. (2021) 52:1995–2004. doi: 10.1161/STROKEAHA.120.032809
61. Sucharew H, Kleindorfer D, Khoury JC, Alwell K, Haverbusch M, Stanton R, et al. Deriving place of residence, modified rankin scale, and EuroQol-5D scores from the medical record for stroke survivors. Cerebrovasc Dis. (2021) 50:567–73. doi: 10.1159/000516571
62. Parameshwaran B, Cordato D, Parsons M, Cheung A, Manning N, Wenderoth J, et al. The benefit of endovascular thrombectomy for stroke on functional outcome is sustained at 12 months. Cerebrovasc Dis Extra. (2021) 11:81–6. doi: 10.1159/000517929
63. Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. (2011) 20:1727–36. doi: 10.1007/s11136-011-9903-x
64. Post PN, Stiggelbout AM, Wakker PP. The utility of health states after stroke: a systematic review of the literature. Stroke. (2001) 32:1425–9. doi: 10.1161/01.STR.32.6.1425
65. Tengs TO, Lin TH. A meta-analysis of quality-of-life estimates for stroke. Pharmacoeconomics. (2003) 21:191–200. doi: 10.2165/00019053-200321030-00004
66. Tengs TO, Yu M, Luistro E. Health-related quality of life after stroke a comprehensive review. Stroke. (2001) 32:964–72. doi: 10.1161/01.STR.32.4.964
67. Joundi RA, Adekanye J, Leung AA, Ronksley P, Smith EE, Rebchuk AD, et al. Health state utility values in people with stroke: a systematic review and meta-analysis. J Am Heart Assoc. (2022) 11:e024296. doi: 10.1161/JAHA.121.024296
68. Grégoire J, Champsi S, Jobin M, Martinez L, Urbich M, Rogoza RM, et al. Cost-effectiveness analysis of evolocumab in adult patients with atherosclerotic cardiovascular disease in Canada. Adv Ther. (2022) 39:3262–79. doi: 10.1007/s12325-022-02130-4
69. Desai NR, Campbell C, Electricwala B, Petrou M, Trueman D, Woodcock F, et al. Cost effectiveness of inclisiran in atherosclerotic cardiovascular patients with elevated low-density lipoprotein cholesterol despite statin use: a threshold analysis. Am J Cardiovasc Drugs. (2022) 22:545–56. doi: 10.1007/s40256-022-00534-9
Keywords: ischemic stroke, health-related quality of life, utility value, EQ-5D, systematic review
Citation: Zhou J, Wei Q, Hu H, Liu W, Guan X, Ma A and Wang L (2023) A systematic review and meta-analysis of health utility values among patients with ischemic stroke. Front. Neurol. 14:1219679. doi: 10.3389/fneur.2023.1219679
Received: 09 May 2023; Accepted: 16 August 2023;
Published: 05 September 2023.
Edited by:
Jean-Claude Baron, University of Cambridge, United KingdomReviewed by:
Veronica Olavarria, Clínica Alemana, ChileCopyright © 2023 Zhou, Wei, Hu, Liu, Guan, Ma and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Aixia Ma, YWl4aWFtYTczQDEyNi5jb20=; Luying Wang, bHV5aW5nX3dAMTYzLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.